Search
- Page Path
- HOME > Search
- Determination of optimal horizontal beam angulations for canal separation in mandibular molars using cone-beam computed tomography: a retrospective image-based analysis
- Benedikt Schneider, Tamina Tepe, Daniel Rapp, Wilhelm Frank, Maria Lessani, Constantin von See, Sebastian Fitzek, Jörg Philipp Tchorz
- Restor Dent Endod 2026;51(1):e9. Published online February 26, 2026
- DOI: https://doi.org/10.5395/rde.2026.51.e9
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Objectives
Two-dimensional intraoral radiographs often obscure canals due to superimposition, especially in mandibular molars with complex anatomy. This cone-beam computed tomography (CBCT) study identified the horizontal beam angles at which first and second molar canals overlap and derived clinically applicable angulations for enhanced canal separation.
Methods
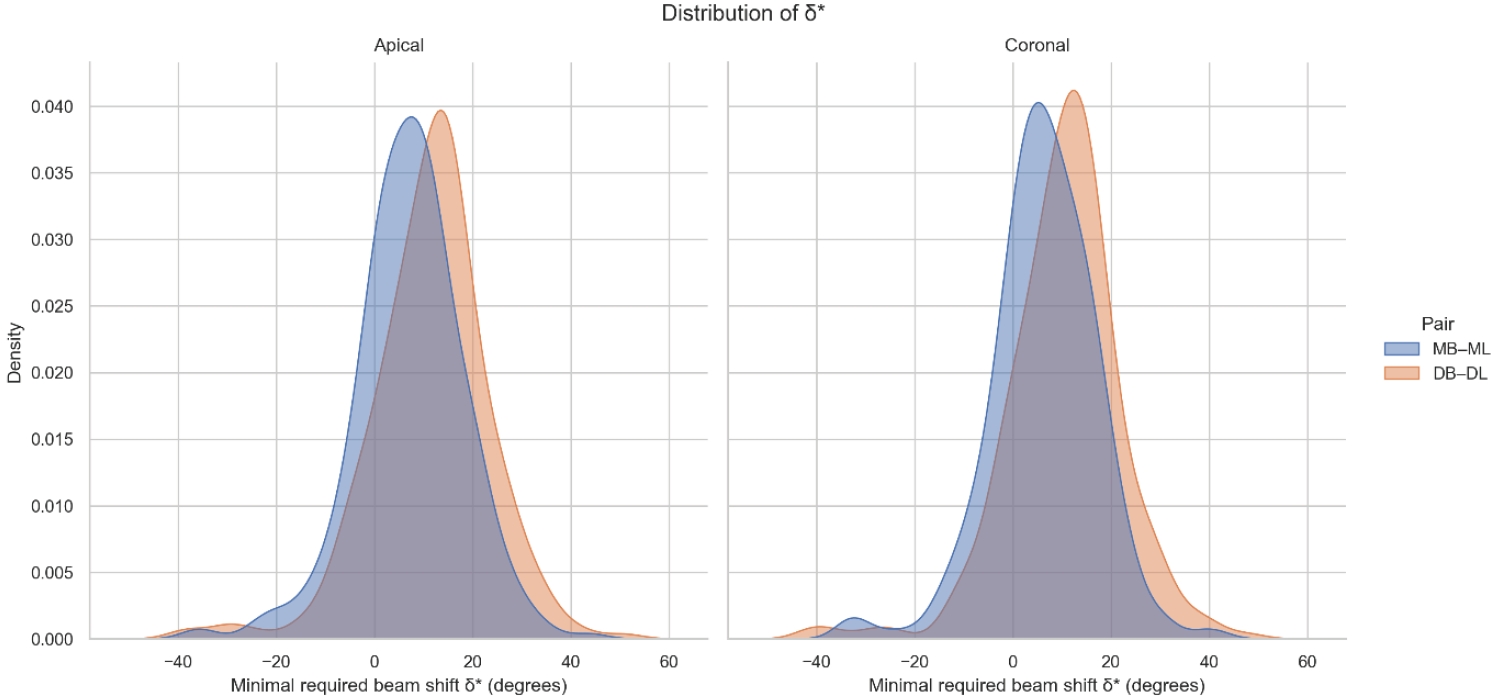
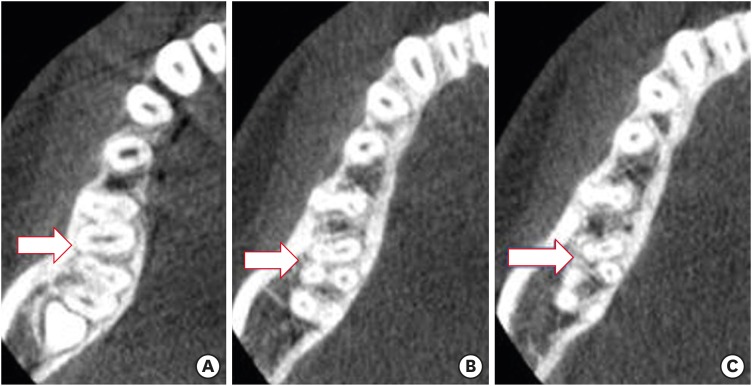
Eighty-five CBCT datasets from 100 patients met the inclusion criteria, yielding 318 mandibular molars (160 first, 158 second). Using ImageJ, absolute horizontal overlap angles (α) were measured to determine the corresponding theoretical separation angles defined as δ* = 90° – α. Separability was modeled across horizontal beam angulation increments from −45° to +45° in five steps, and Wilson’s 95% confidence intervals were computed. Group comparisons used the Mann-Whitney U and independent t-tests (p ≤ 0.05)
Results
Minimal mesial beam angulations for effective canal separability (δ* = 90° − α) ranged from approximately 7° to 15° for mesial roots and approximately 10° to 13° for distal roots. No significant mesial differences were observed between first and second molars (p > 0.30). Distal roots of second molars exhibited significantly higher angulations (p = 0.003 coronal, p < 0.001 apical). Mesial canals achieved ≥95% separability at approximately 25° and ≥99% at approximately 35°; distal canals required approximately 30° and approximately 40°.
Conclusions
A mesial beam angulation of 30° to 35° provides probable canal differentiation in mandibular molars, separating mesial canals in ≥99% and distal canals in ≥95% of cases. This range refines previous recommendations and supports the as low as reasonably achievable (ALARA) principle.
- 375 View
- 13 Download

- Cone-beam computed tomography analysis of maxillary premolar canal anatomy: Ahmed’s versus Vertucci’s classifications in a Jordanian cohort
- Raidan Ba-Hattab, Muna M. Shaweesh, Nessrin A. Taha, Elham S. Abu Alhaija
- Restor Dent Endod 2026;51(1):e11. Published online February 26, 2026
- DOI: https://doi.org/10.5395/rde.2026.51.e11
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Objectives
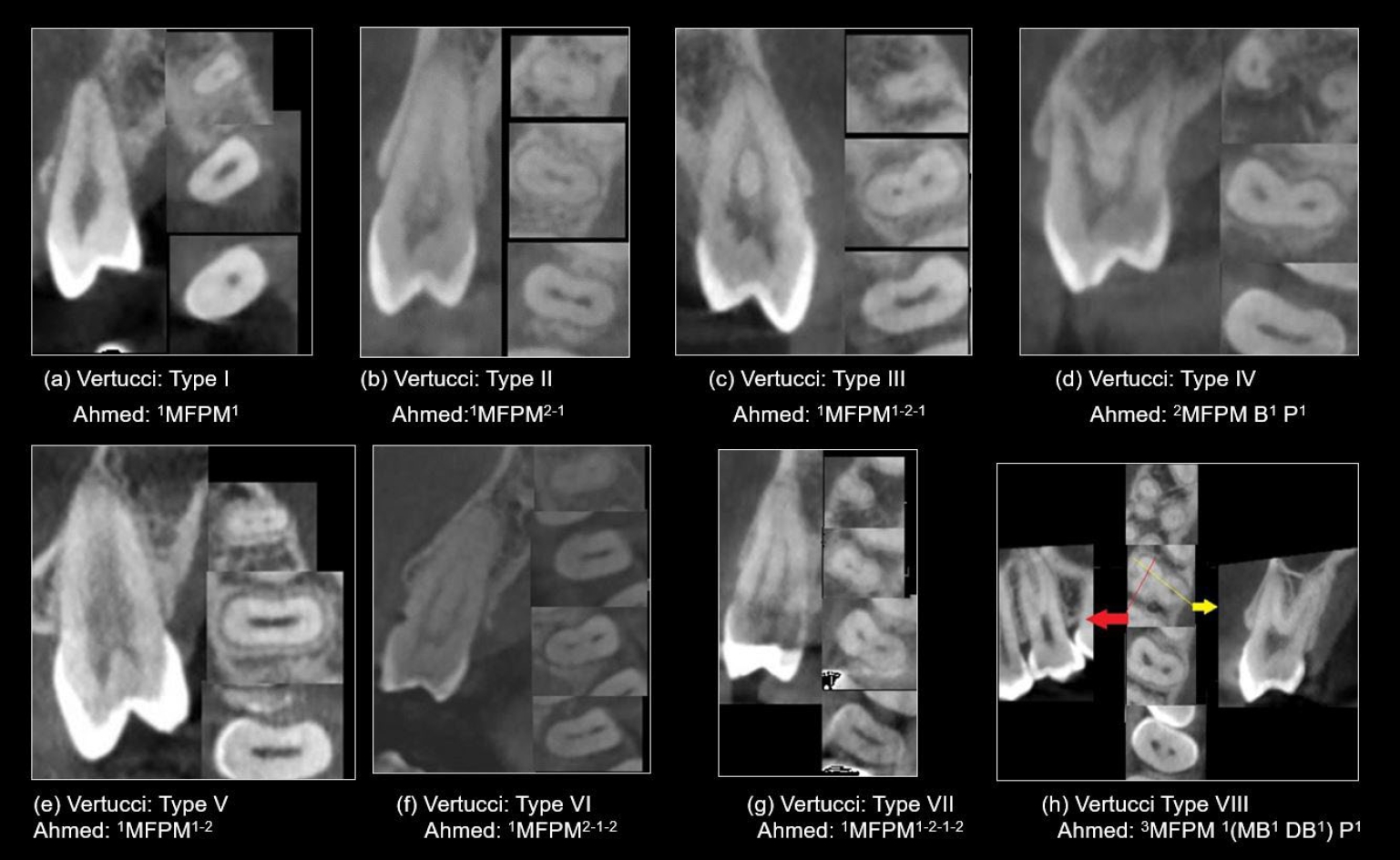
This study analyzed the root and canal configurations of maxillary premolars in a Jordanian subpopulation using cone-beam computed tomography (CBCT) and classified them based on Vertucci’s and Ahmed’s systems.
Methods
Two hundred CBCT scans of 800 maxillary premolars were retrospectively assessed for root morphology, canal configurations, and root canal divergence and merging. Data was statistically analyzed.
Results
The study included 70 males and 130 females. Most right and left maxillary first premolars (RFPM, LFPM) had two roots (59.0% and 58.5%), with a significant association between sex and root number for RFPM and LFPM (p < 0.05). In contrast, the right and left maxillary second premolars (RSPM, LSPM) mostly had a single root (87.5% and 88.5%), with no association with sex. Vertucci’s classification showed type IV as the predominant configuration in first premolars (RFPM, 65.0% and LFPM, 67.0%) and type I in second premolars (RSPM, 44.0% and LSPM, 49.0%). A significant sex association was found only with RSPM. Ahmed’s classification revealed that maxillary premolar with two separated roots and two separated canals (2MP B1 P1) was mostly found in first premolars (RFPM, 58.0% and LFPM, 56.0%), and maxillary premolar with one root and one canal (1MP1) in second premolars (RSPM, 44.0% and LSPM, 49.0%), with a significant sex association for RSPM and LSPM (p < 0.05). Age had no impact, and symmetry was observed between the right and left sides. Three-rooted premolars were identified in four cases. Almost all of Vertucci’s types and numerous codes from Ahmed’s classification were documented.
Conclusions
CBCT revealed diverse anatomical variations in the Jordanian subpopulation, with Ahmed’s classification providing more detailed canal configurations than Vertucci’s, uncovering previously overlooked variations.
- 166 View
- 16 Download

- Analysis of thermal profiles on tooth structure and insert during one-piece or adapter-coupled ultrasonic insert use: an in vitro experimental study
- Gabriela Loewen Brotto, Bruno Monguilhott Crozeta, Bruno Marques-da-Silva, Alysson Nunes Diógenes, Emmanuel João Nogueira Leal da Silva, Flávia Sens Fagundes Tomazinho
- Restor Dent Endod 2025;50(3):e24. Published online July 11, 2025
- DOI: https://doi.org/10.5395/rde.2025.50.e24
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Objectives
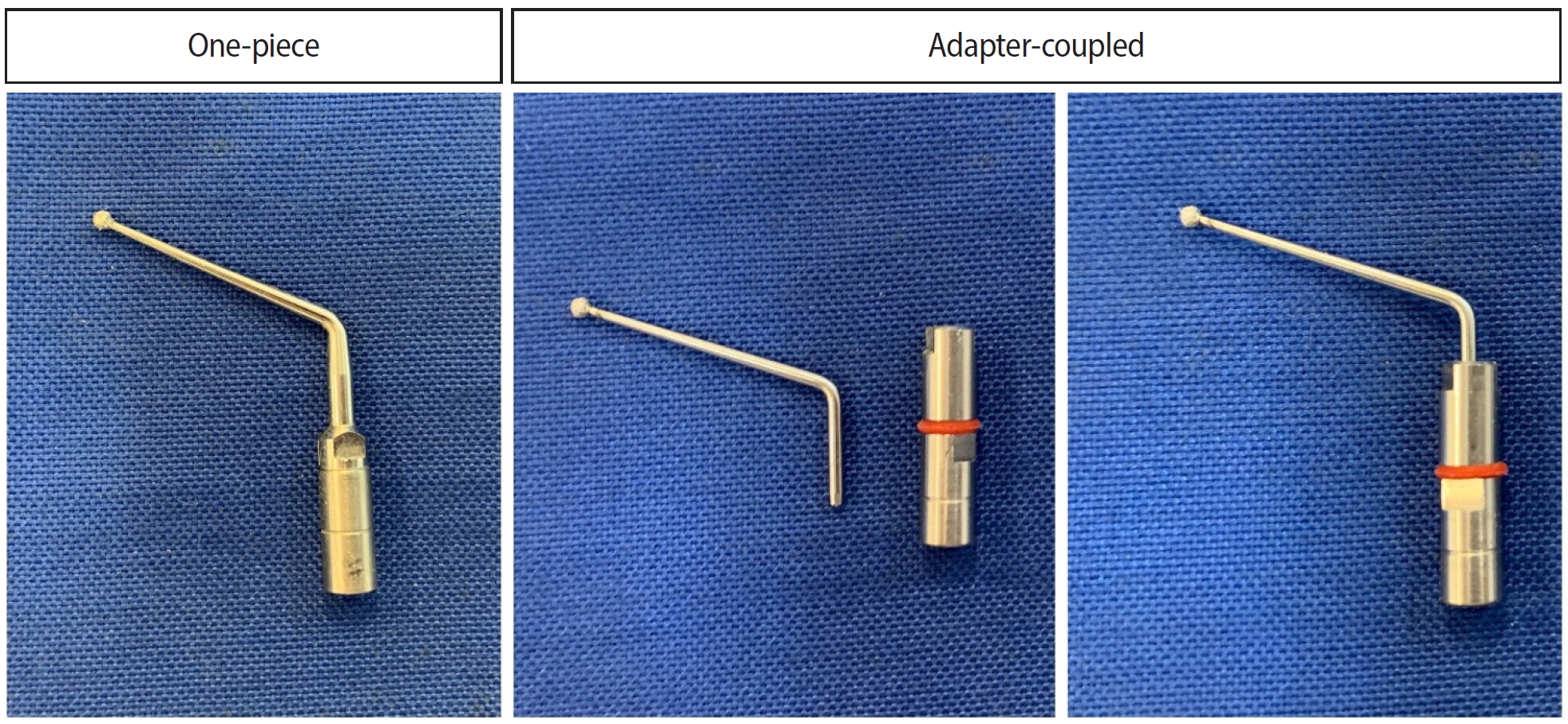
This in vitro study aimed to evaluate temperature variation on the external surface of mandibular molars and within ultrasonic inserts when using adapter-coupled versus one-piece inserts.
Methods
Twenty-four extracted human mandibular molars were divided into two groups based on the type of ultrasonic insert used: adapter-coupled and one-piece inserts. Temperature on the external surface of each tooth was measured with a thermocouple probe positioned in the furcation area, capturing data continuously. The temperature of the ultrasonic inserts was monitored in real-time using a thermal imaging camera. Measurements were taken in a controlled environment without cooling for over 120 seconds. Statistical analysis was conducted using analysis of variance (ANOVA) and two-way ANOVA with repeated measures to evaluate temperature variations between groups and over time, with significance set at 5%.
Results
In the external tooth surface temperature measurements, no significant differences were observed between the groups during the initial 15 seconds (p = 0.185) and 30 seconds (p = 0.067). However, significant differences emerged at 60 seconds (p = 0.025), 90 seconds (p = 0.024), and 120 seconds (p = 0.020), with the one-piece insert group demonstrating higher temperatures in the furcation region. Thermal imaging of the inserts revealed a significant difference at all time points (p < 0.001), with adapter-coupled inserts showing greater heating.
Conclusions
The use of ultrasonic inserts leads to a gradual rise in temperature on the external tooth surface. One-piece inserts generated higher temperatures on the tooth, while adapter-coupled inserts exhibited greater heating within the insert.
- 1,809 View
- 95 Download

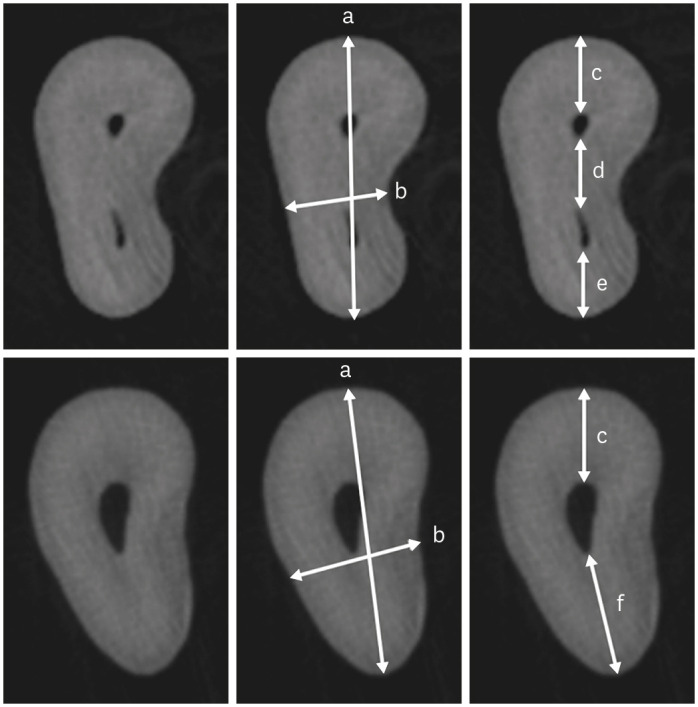
- Dentin thickness of C-shaped root canal walls in mandibular premolars based on cone-beam computed tomography: a retrospective cross-sectional study
- Elif Aslan, Ali Canberk Ulusoy, Bilge Hakan Sen, B. Guniz Baksi, Erinc Onem, Ali Mert
- Restor Dent Endod 2025;50(2):e18. Published online May 15, 2025
- DOI: https://doi.org/10.5395/rde.2025.50.e18
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Objectives
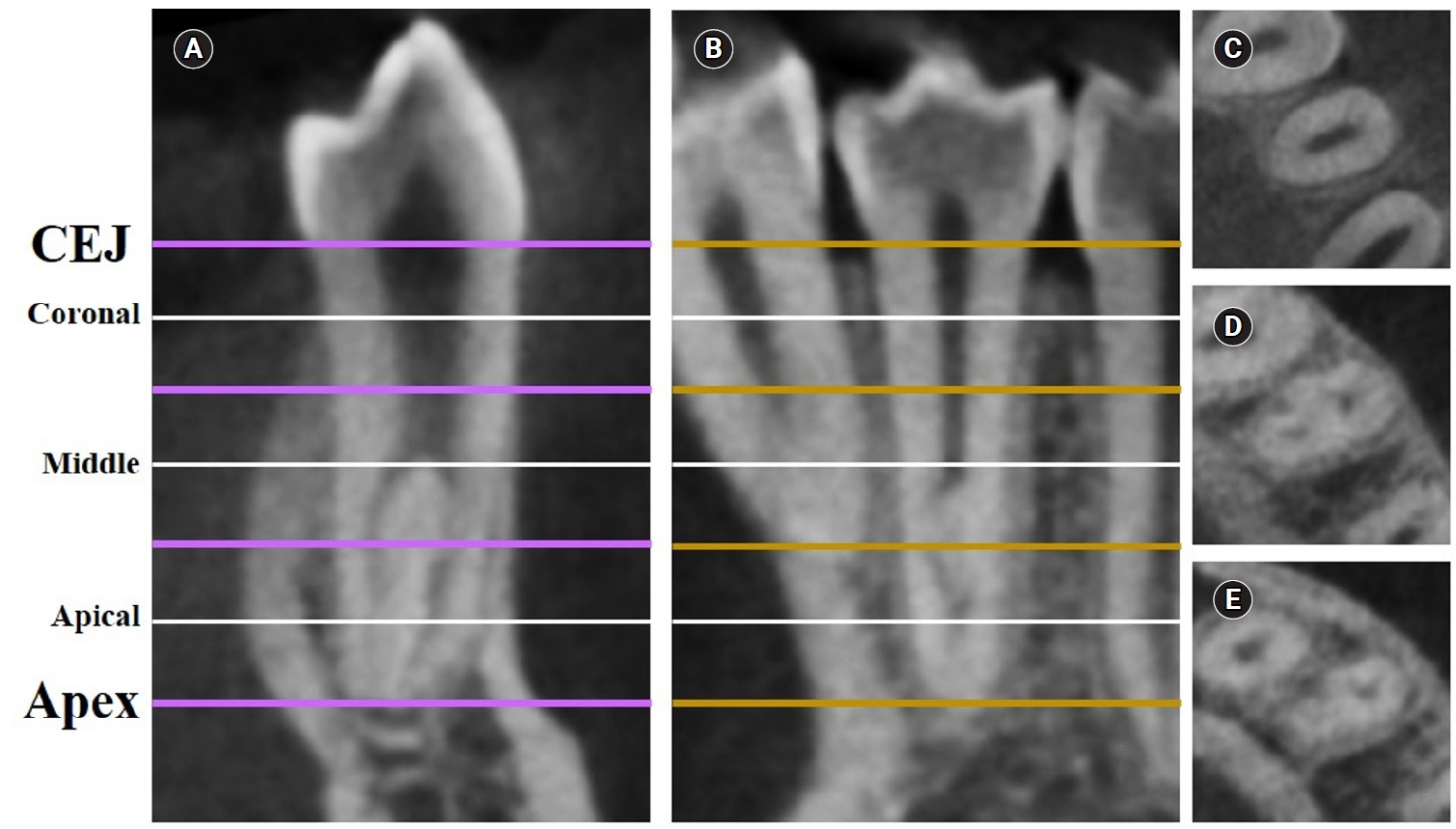
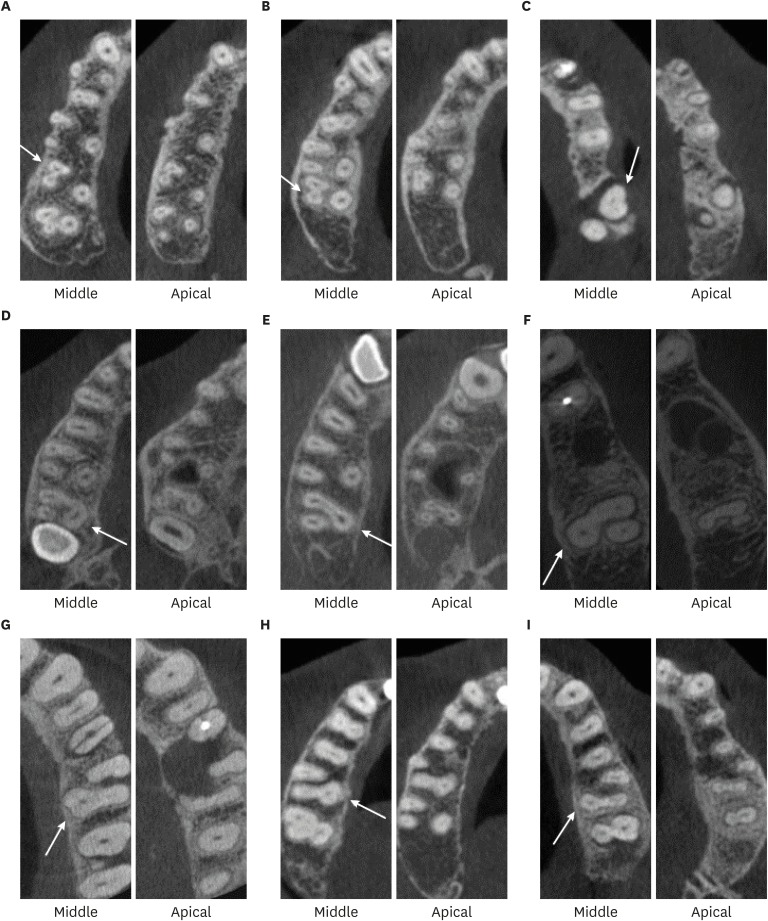
This study aimed to measure the dentin thickness of C-shaped canals in mandibular first and second premolars at coronal, middle, and apical root levels using cone-beam computed tomography (CBCT).
Methods
Dentin thicknesses of buccal, lingual, mesial, and distal root walls of 41 C-shaped premolars were measured at three different root levels on axial CBCT slices. The measurements were made at the midpoint of each third, along with 1 mm below and above the midpoint. C-shape configurations of the premolar root canals were also recorded. Analysis of variance, Kruskal-Wallis, and the independent samples t-tests were used for the comparisons (p = 0.05).
Results
The thickest walls for both premolars were buccal and lingual walls at all three root levels (p < 0.05). The thinnest walls for the first premolar teeth were mesial and distal walls of the lingual canal, while it was the mesial end of the buccal and lingual canals for the second premolars (p < 0.05). Dentin wall thicknesses at the mesial end of buccal and lingual canals of C1-shaped first premolars were thinner than C2-shaped first premolars at the apical level (p < 0.05).
Conclusions
Danger zones for C-shaped mandibular first and second premolars are predominantly mesial walls facing the radicular groove and distal wall of the lingual canal. CBCT imaging during endodontic treatment is recommended to avoid complications. -
Citations
Citations to this article as recorded by- Anatomical complexity in mandibular second molars: prevalence of C-shaped canals, radicular grooves, taurodontism, and radices molarum in Saudi population
Ahmed A. Madfa, Abdullah F. Alshammari, Eyad Almagadawyi, Ebtsam A. Aledaili, Afaf Al-Haddad
Scientific Reports.2025;[Epub] CrossRef
- Anatomical complexity in mandibular second molars: prevalence of C-shaped canals, radicular grooves, taurodontism, and radices molarum in Saudi population
- 3,556 View
- 135 Download
- 1 Web of Science
- 1 Crossref

- Assessment of mechanical allodynia in healthy teeth adjacent and contralateral to endodontically diseased teeth: a clinical study
- Vaishnavi Ratnakar Patankar, Ashish K Jain, Rahul D Rao, Prajakta R Rao
- Restor Dent Endod 2024;49(3):e31. Published online July 29, 2024
- DOI: https://doi.org/10.5395/rde.2024.49.e31
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives The present study investigated the prevalence of mechanical allodynia (MA) in healthy teeth adjacent and contralateral to endodontically diseased teeth.
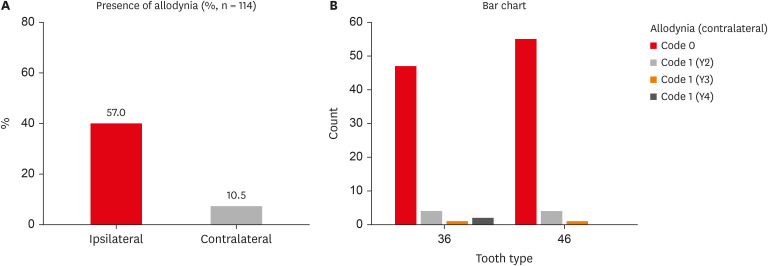
Materials and Methods This cross-sectional study included 114 patients with symptomatic irreversible pulpitis and apical periodontitis in permanent mandibular first molars who possessed healthy teeth adjacent and contralateral to the endodontically diseased tooth. The mechanical sensitivity of the teeth was determined by percussion testing. The presence or absence of pain on percussion in the teeth adjacent and contralateral to the endodontically diseased tooth and the tooth distal to the contralateral symmetrical tooth was recorded according to coding criteria. The prevalence of MA was computed as a percentage, and binary logistic regression analysis was done. The Fisher exact test and Mann-Whitney
U test were used for binary and ordinal data.Results Age and sex did not influence the prevalence of MA. An increased prevalence of MA was found in patients with higher levels of spontaneous pain (
p < 0.001). The prevalence of allodynia was 57% in teeth adjacent to endodontically diseased teeth and 10.5% in teeth contralateral to endodontically diseased teeth. In addition, on the ipsilateral side, there were more painful sensations distal to the diseased tooth than mesially.Conclusions Despite being disease-free, teeth adjacent and contralateral to endodontically diseased teeth exhibited pain on percussion. There was a direct association between the severity of the patient’s pain and the presence of MA.
- 3,008 View
- 91 Download

- Predictor factors of 1-rooted mandibular second molars on complicated root and canal anatomies of other mandibular teeth
- Hakan Aydın, Hatice Harorlı
- Restor Dent Endod 2024;49(1):e2. Published online January 3, 2024
- DOI: https://doi.org/10.5395/rde.2024.49.e2
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
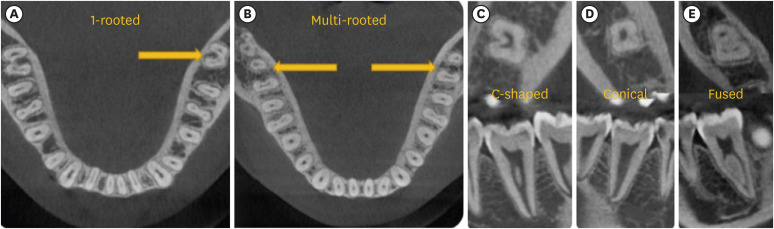
ePub Objectives This study aimed to determine the effects of 1-rooted mandibular second molar (MnSM) teeth on root canal anatomy complexities of the mandibular central incisor (MnCI), mandibular lateral incisor (MnLI), mandibular canine (MnCn), mandibular first premolar (MnFP), mandibular second premolar (MnSP), and mandibular first molar (MnFM) teeth.
Materials and Methods Cone-beam computed tomography images of 600 patients with full lower dentition were examined. Individuals with 1-rooted MnSMs were determined, and the complexity of root canal anatomy of other teeth was compared with individuals without 1-rooted MnSMs (Group-1; subjects with at least one 1-rooted MnSM, Group-2; subjects with more than a single root in both MnSMs). A second canal in MnCIs, MnLIs, MnCns, MnFPs, and MnSPs indicated a complicated root canal. The presence of a third root in MnFMs was recorded as complicated.
Results The prevalence of 1-rooted MnSMs was 12.2%, with the C-shaped root type being the most prevalent (9%). There were fewer complicated root canals in MnCIs (
p = 0.02), MnLIs (p < 0.001), and MnFPs (p < 0.001) in Group 1. The other teeth showed no difference between the groups (p > 0.05). According to logistic regression analysis, 1-rooted right MnSMs had a negative effect on having complex canal systems of MnLIs and MnFPs. Left MnSMs were explanatory variables on left MnLIs and both MnFPs.Conclusions In individuals with single-rooted MnSMs, a less complicated root canal system was observed in all teeth except the MnFMs.
-
Citations
Citations to this article as recorded by- Repair of furcal perforations using different calcium silicate cements: An in vitro study
Ariana Esperanza Apolo Aguilar, Maria Soledad Peñaherrera Manosalvas, Henry Paul Valverde Haro
Journal of Conservative Dentistry and Endodontics.2025; 28(10): 1007. CrossRef
- Repair of furcal perforations using different calcium silicate cements: An in vitro study
- 1,925 View
- 62 Download
- 1 Crossref

- The clinical success of ART restorations and Hall technique in primary molars: a randomized 18-month follow-up study
- Esra Oz, Zuhal Kırzıoglu, Canan Kale
- Restor Dent Endod 2023;48(2):e19. Published online May 1, 2023
- DOI: https://doi.org/10.5395/rde.2023.48.e19
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
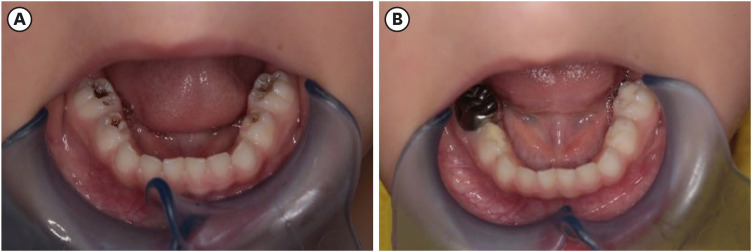
ePub Objectives The aim of the study was to evaluate the clinical and radiographic success of the Hall technique (HT) and atraumatic restorative treatment (ART) restorations using high-viscosity glass-ionomer cement for the management of occlusal carious lesions in primary molars.
Materials and Methods This randomized clinical study observed 40 children (aged 5–6 years). For each child, one tooth was treated with HT and one with ART. The primary outcome measures for HT restorations were successful, minor, and major failure rates. Clinical evaluations of ART restorations were performed according to the modified United States Public Health Service criteria during 18-month follow-up. McNemar test was used for statistical analysis.
Results Thirty of 40 (75%) participants returned for 18 months of follow-up. In the clinical evaluations of teeth that were treated with HT, the patients did not have complaints of pain or other symptoms, all crowns remained in the oral cavity, the gums were healthy, and the teeth were functional in all evaluations. At the end of the 18-month follow-up, the surface texture and marginal integrity criteria of ART restorations were recorded as 26.7% and 33.3%, respectively. In the radiographic evaluation of 30 patients treated with ART and HT, all restorations were considered successful.
Conclusions The 18-month clinical and radiographic results after treatments applied to single-surface cavities in anxious children showed that both treatment methods were successful.
-
Citations
Citations to this article as recorded by- Two-year outcomes of hall technique and modified hall technique in deep carious lesions of primary molars: a randomized clinical trial
Sumeyye Konukman Turker, Ayse Isil Cihan
BMC Oral Health.2026;[Epub] CrossRef - Success rate of Hall Technique for restoring carious primary molars - systematic review and meta-analysis
Tamara Kerber Tedesco, Nicola Patricia Innes, Claudia Lopez Gallegos, Gabriela Seabra Silva, Thais Gimenez, Mariana Minatel Braga, Mariana Pinheiro Araujo, Jayakumar Jayaraman, Waraf Al-yaseen, Daniela Prócida Raggio
Evidence-Based Dentistry.2025; 26(1): 65. CrossRef - Effectiveness of Dental Restorative Materials in the Atraumatic Treatment of Carious Primary Teeth in Pediatric Dentistry: A Systematic Review
Gianna Dipalma, Angelo Michele Inchingolo, Lucia Casamassima, Paola Nardelli, Danilo Ciccarese, Paolo De Sena, Francesco Inchingolo, Andrea Palermo, Marco Severino, Cinzia Maria Norma Maspero, Alessio Danilo Inchingolo
Children.2025; 12(4): 511. CrossRef - Clinical, radiographic, and microhardness evaluation of caries in primary molars managed with modified Hall technique
Eman El Sayed El Bedewy, Nahed A.A. Abohamila, Shereen A. M. Ali, Shimaa M.M. Hadwa
Tanta Dental Journal.2025; 22(1): 133. CrossRef - Pain Perception During Minimally Invasive Caries Removal in Children: A Randomized Clinical Trial Comparing Chemo-Mechanical Caries Removal
Dhirja Goel, Neha Awasthi, Yanina Singh, Sukhdeep Singh, Nenung Yirang
Journal of International Society of Preventive and Community Dentistry.2025; 15(4): 348. CrossRef - Clinical and histological evaluation of hall technique with and without silver diamine fluoride in the treatment of carious primary molars
Marwa M.A.Z. Abd-Elhaleium, Fatma A.-A. El-Hendawy, Lamis A. El-Ghareb, Sara Y. AboAli
Tanta Dental Journal.2025; 22(2): 351. CrossRef - Comparative success of minimally invasive treatments for cavitated caries in primary teeth: a network meta-analysis
Rasoul Sahebalam, Mahsa Ghorbani, Alireza Sarraf Shirazi, Motahareh Khosrojerdi, Mana Mowji
BMC Oral Health.2025;[Epub] CrossRef
- Two-year outcomes of hall technique and modified hall technique in deep carious lesions of primary molars: a randomized clinical trial
- 6,491 View
- 115 Download
- 6 Web of Science
- 7 Crossref

- Proximity of maxillary molar apexes to the cortical bone surface and the maxillary sinus
- Han Shin Lee, Dokyung Kim, Sung Kyo Kim
- Restor Dent Endod 2022;47(3):e33. Published online August 8, 2022
- DOI: https://doi.org/10.5395/rde.2022.47.e33
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
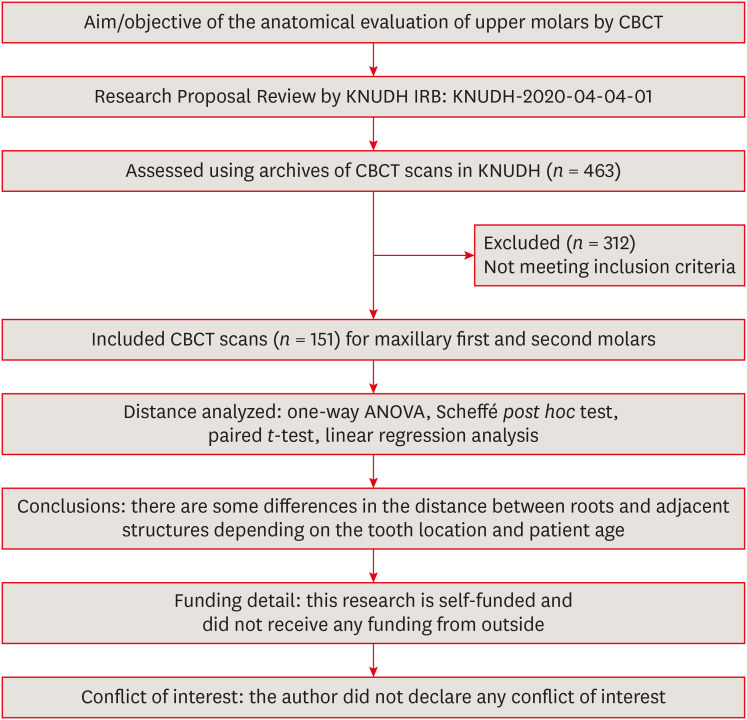
ePub Objectives This study aimed to analyze the proximity of maxillary molar roots to their overlying cortical bone surfaces and the maxillary sinus.
Materials and Methods Cone-beam computed tomographic images of 151 patients with completely erupted upper molars that had 3 separate roots were studied. The following distances were measured: from the root apex to the cortical plate and maxillary sinus floor, and from the apical 3-mm level of the root to the cortical plate. Differences between groups were analyzed with 1-way analysis of variance and the Scheffé
post hoc test, the significance of differences between cone-beam computed tomography views with the pairedt -test, and the significance of differences among age groups with linear regression analysis. The significance level was set atp < 0.05.Results The mesiobuccal and distobuccal root apexes of maxillary second molars were more distant from the buccal cortical plate than the maxillary first molars (
p < 0.05). The apical 3-mm level of the mesiobuccal root of the first molar was closer to the buccal cortical bone than the second molar (p < 0.05). In the maxillary first molars, the thickness of the buccal cortical bone decreased in all roots with age (p < 0.05). In all root apexes of both molars, the difference in the vertical level between the maxillary sinus floor and the root apex increased with age (p < 0.05).Conclusions Awareness of the anatomical profile of maxillary molar apices in relation to the cortical bones and maxillary sinus will be beneficial for apical surgery.
-
Citations
Citations to this article as recorded by- Proximity of maxillary molar palatal roots to adjacent structures for endodontic microsurgery: a cone-beam computed tomography study
Xiaoxiang Huang, Jun Xu, Benxiang Hou, Ying Wang
BMC Oral Health.2025;[Epub] CrossRef - Periapical bone loss configuration in sub-Saudi patients afflicted with periapical abscesses: A 3D cone-beam computed tomography analysis
Swati A. Srivastava, Rahaf A. Alawajy, Rehab Abdelaziz, Elzahraa A. Eldwakhly, Selma A. Saadaldin, Rahaf A. Almohareb, Fahda Nabeel Algahtani, Mai Salah Soliman, Manal M. Abdelhafeez
Saudi Endodontic Journal.2025; 15(2): 144. CrossRef
- Proximity of maxillary molar palatal roots to adjacent structures for endodontic microsurgery: a cone-beam computed tomography study
- 3,247 View
- 29 Download
- 1 Web of Science
- 2 Crossref

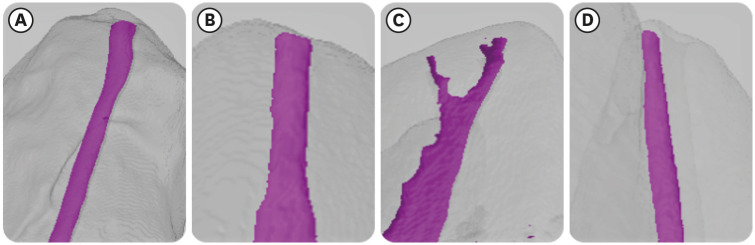
- Morphotypes of the apical constriction of maxillary molars: a micro-computed tomographic evaluation
- Jeffrey Wen-Wei Chang, Kuzhanchinathan Manigandan, Lakshman Samaranayake, Chellapandian NandhaKumar, Pazhamalai AdhityaVasun, Johny Diji, Angambakkam Rajasekharan PradeepKumar
- Restor Dent Endod 2022;47(2):e19. Published online March 24, 2022
- DOI: https://doi.org/10.5395/rde.2022.47.e19
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives The aim of this study was to evaluate and compare the apical constriction (AC) and apical canal morphology of maxillary first and second molars, using micro-computed tomography (micro-CT).
Materials and Methods The anatomical features of 313 root canals from 41 maxillary first molars and 57 maxillary second molars of patients with known age and sex were evaluated using micro-CT, with a resolution of 26.7 µm. The factors evaluated were the presence or absence of AC, the morphotypes, bucco-lingual dimension, mesio-distal dimension, and the profile (shape) of AC and the apical root canal. The apical root canal dimensions, location of the apical foramen (AF), AC to AF distance, and presence of accessory canals in the apical 5 mm were also assessed. Descriptive and analytical statistics were used for data evaluation.
Results AC was present in all 313 root canals. Patients’ age and sex did not significantly impact either AC or the apical canal dimensions. The most common AC morphotype detected was the traditional (single) constriction (52%), followed by the parallel (29%) morphotype. The mean AC dimensions in maxillary first molars were not significantly different from those in maxillary second molars. Sixty percent of AF were located within 0.5 mm from the anatomic apex.
Conclusions The most common morphotype of AC detected was the traditional constriction. Neither patients’ age nor sex had a significant impact on the dimensions of the AC or the apical root canal. The majority of AF (60%) were located within 0.5 mm from the anatomic apex.
-
Citations
Citations to this article as recorded by- In Vivo and In Vitro Accuracy and Precision Evaluations of Mini Electronic Apex Locators
Özlem Kara, Rüstem Kemal Sübay
Australian Endodontic Journal.2025; 51(2): 329. CrossRef - Effect of Coronal Flaring on Initial Apical File Size Estimation in Curved Canals Using Three Distinct Rotary Instruments: A Comparative In Vitro Study
Vinodhini Varatharajan, Muhammed Abdul Rahman Thazhathveedan, Mohammed Salman Kuttikkodan, Ismail Puzhangaraillath Mundanatayil, Amrutha Ravindran Thazhe Mangool, Ashraf Karumbil
Cureus.2024;[Epub] CrossRef - In Vitro Evaluation of the Accuracy of Three Electronic Apex Locators Using Different Sodium Hypochlorite Concentrations
Sanda Ileana Cîmpean, Radu Marcel Chisnoiu, Adela Loredana Colceriu Burtea, Rareș Rotaru, Marius Gheorghe Bud, Ada Gabriela Delean, Ioana-Sofia Pop-Ciutrilă
Medicina.2023; 59(5): 918. CrossRef - Cone beam computed tomography analysis of the root and canal morphology of the maxillary second molars in a Hail province of the Saudi population
Ahmed A. Madfa, Moazzy I. Almansour, Saad M. Al-Zubaidi, Albandari H. Alghurayes, Safanah D. AlDAkhayel, Fatemah I. Alzoori, Taif F. Alshammari, Abrar M. Aldakhil
Heliyon.2023; 9(9): e19477. CrossRef
- In Vivo and In Vitro Accuracy and Precision Evaluations of Mini Electronic Apex Locators
- 2,363 View
- 47 Download
- 6 Web of Science
- 4 Crossref

- Morphological characteristics of the mesiobuccal root in the presence of a second mesiobuccal canal: a micro-CT study
- Lucas P. Lopes Rosado, Matheus Lima Oliveira, Karla Rovaris, Deborah Queiroz Freitas, Frederico Sampaio Neves
- Restor Dent Endod 2022;47(1):e6. Published online January 18, 2022
- DOI: https://doi.org/10.5395/rde.2022.47.e6
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives This study investigated the internal morphology of mesiobuccal (MB) roots of maxillary molars with a second mesiobuccal (MB2) canal.
Materials and Methods Forty-seven maxillary first or second molars from Brazilians were scanned using micro-computed tomography. The following measurements were obtained from the MB roots: root thickness, root width, and dentin thickness of the buccal aspect of the first mesiobuccal (MB1) canal, between the MB1 and MB2 canals, and the palatal aspect of the MB2 and MB1 canals at 3 mm from the root apex and in the furcation region. For statistical analysis, the Student’s
t -test and analysis of variance with thepost-hoc Tukey test were used (α = 0.05).Results In maxillary molars with an MB2 canal, MB roots were significantly thicker (
p = 0.0014) and narrower (p = 0.0016) than in maxillary molars without an MB2 canal. The dentin thickness of the palatal aspect of the MB1 canal was also significantly greater than that of MB roots without an MB2 canal at 3 mm from the root apex (p = 0.0007) and in the furcation region (p < 0.0001). In the furcation region of maxillary molars with an MB2 canal, the dentin thickness between the MB1 and MB2 canals was significantly smaller than that in the buccal and palatal aspects (p < 0.0001).Conclusions The internal morphology of MB roots of maxillary molars with an MB2 canal revealed differences in dentin thickness, root diameter, and distance between the canals when compared with maxillary molars without an MB2 canal.
-
Citations
Citations to this article as recorded by- Effectiveness and safety of three NiTi systems in endodontic retreatment of MB1 and MB2 root canals: a micro-CT and CBCT combined analysis
Airton Oliveira Santos-Junior, Rocharles Cavalcante Fontenele, Karina Ines Medina Carita Tavares, Fernanda Ferrari Esteves Torres, Jáder Camilo Pinto, Pedro Luis Busto Rosim, Andréa Gonçalves, Marco Antonio Hungaro Duarte, Juliane Maria Guerreiro-Tanomaru
Clinical Oral Investigations.2025;[Epub] CrossRef - Cone-beam computed tomography evaluation of root and canal morphology of maxillary molars in a Chinese kazakh population
Shuchun Yang, Chenye Li, Hui Shi, Ming Liu, Xu Wang
BMC Oral Health.2025;[Epub] CrossRef - Can maxillary molar dimensions predict the presence of the second mesiobuccal canal?
Lucas P. Lopes Rosado, Deborah Queiroz Freitas, Karla Rovaris, Matheus L. Oliveira, Frederico Sampaio Neves
Oral Radiology.2023; 39(3): 482. CrossRef - Can the detection of second mesiobuccal canals be enhanced based on the volume of adjacent canals?
Lucas P. Lopes Rosado, Deborah Q. Freitas, Karla Rovaris, Matheus L. Oliveira, Frederico S. Neves
Archives of Oral Biology.2023; 146: 105604. CrossRef - Assessment of the coronal root canal morphology of permanent maxillary first molars using digital 3D-reconstruction technology based on micro-computed tomography data
Mudan Wang, Yuxuan Gao, Qi Deng, Yuan Gao, Dongzhe Song, Dingming Huang
Journal of Dental Sciences.2023; 18(2): 586. CrossRef
- Effectiveness and safety of three NiTi systems in endodontic retreatment of MB1 and MB2 root canals: a micro-CT and CBCT combined analysis
- 1,804 View
- 36 Download
- 6 Web of Science
- 5 Crossref

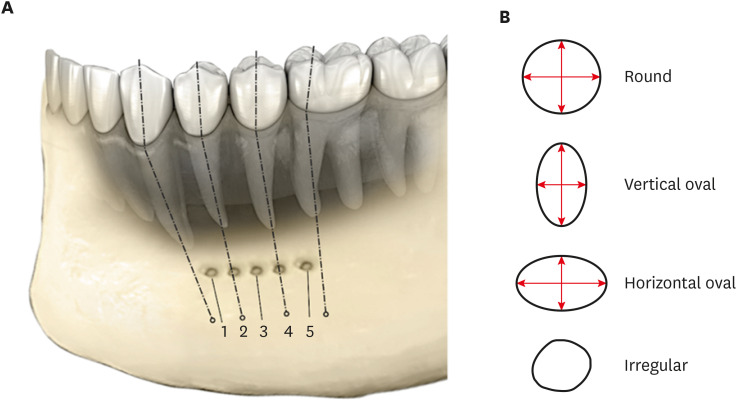
- Shape and anatomical relationship of the mental foramen to the mandibular premolars in an Indian sub-population: a retrospective CBCT analysis
- Komal Sheth, Kulvinder Singh Banga, Ajinkya M. Pawar, James L. Gutmann, Hyeon-Cheol Kim
- Restor Dent Endod 2022;47(1):e1. Published online December 13, 2021
- DOI: https://doi.org/10.5395/rde.2022.47.e1
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives This study assessed the shape and anatomical relationship of the mental foramen (MF) to mandibular posterior teeth in an Indian sub-population.
Materials and Methods In total, 475 existing cone-beam computed tomography records exhibiting 950 MFs and including the bilateral presence of mandibular premolars and first molars were assessed. Images were evaluated 3-dimensionally to ascertain the position, shape, and anatomical proximity of MFs to mandibular teeth. The position and shape of MFs were measured and calculated. The Pythagorean theorem was used to calculate the distance between the root apex of the mandibular teeth and the MF.
Results MFs exhibited a predominantly round shape (left: 67% and right: 65%) followed by oval (left: 30% and right: 31%) in both males and females and in different age groups. The root apices of mandibular second premolars (left: 71% and right: 62%) were closest to the MF, followed by distal to the first premolars and mesial to the second premolars. The mean vertical distance between the MF and the nearest tooth apex calculated on sagittal sections was 2.20 mm on the right side and 2.32 mm on the left side; no significant difference was found according to sex or age. The distance between the apices of the teeth and the MF was ≥ 4 mm (left; 4.09 ± 1.27 mm and right; 4.01 ± 1.15 mm).
Conclusions These findings highlight the need for clinicians to be aware of the location of the MF in treatment planning and while performing non-surgical and surgical endodontic procedures.
-
Citations
Citations to this article as recorded by- Anatomical and radiographic assessment of variations of the mental foramen and their impact on success of local anaesthesia administration
Isratul Jannat, M. Ummay Salma, Nipu Rani Chowdhury, Kulsum Nahar, Dilruba Binte Mostafa, Khandokar Emanuzzaman Emon, Shahela Sarmin
International Journal of Research in Medical Sciences.2026; 14(3): 823. CrossRef - Optimising Treatment Strategies: Labial versus Labio-inferior Plating Using Three-dimensional Miniplates for Mandibular Symphysis and Parasymphysis Fractures
Akash P Muralidharan, Kalyani Bhate, K Mithun Nilgiri, Sumithra S Nair, Lakshmi Shetty, Rose Johnson
Advances in Human Biology.2025; 15(2): 242. CrossRef - Morphometric analysis of mental foramen in retained cadaveric specimens of mandibles of Sri Lankan population
Dadallage Tharanga De Silva, Usliyanage Clifford Priyantha Perera
Anatomical Science International.2025;[Epub] CrossRef - A Cross-Sectional CBCT Study of Anterior Loop, Accessory Mental Foramen, and Lingual Foramina in Patients’ Mandibles: Implications for Safer Implant Planning
Abbas Shokri, Mohammad Mahdi Maleki, Leili Tapak
Journal of Maxillofacial and Oral Surgery.2025;[Epub] CrossRef - Radiographic Recognition of Mental Nerve for Secured Dental Implant Placement by Cone-Beam Computed Tomography in Mosul City Population
Asmaa B. Al-Saffar, Mekdad H. Alrigbo, Rawaa Y. Al-Rawee
Journal of Craniofacial Surgery.2024; 35(7): 2049. CrossRef - Accuracy of Implant Size Prediction Based on Edentulous Ridge Dimension on Cone-beam Computed Tomography - A Retrospective Study
Hunter R. Jolicoeur, Gerard A. Camargo, Tamara G. Stephenson, Wenjian Zhang
Annals of Maxillofacial Surgery.2024; 14(2): 187. CrossRef - Mental Foramenin Panoramik Radyografi ve Konik Işınlı Bilgisayarlı Tomografi Görüntüleri Üzerinde Morfolojik Analizi
Ezgi UZUN, Burak Kerem APAYDIN, Ayşen TİL
Selcuk Dental Journal.2023; 10(3): 540. CrossRef - Evaluation of the Possible Relationship between the Curvature and
Horizontal Course of the Inferior Alveolar Canal
Cansu G. Koca, M. Fatih Çiçek, Sanaz Sadry, Ozan Yenidünya, Fatma Akkoca Kaplan, Aras Erdil
Current Medical Imaging Formerly Current Medical Imaging Reviews.2023;[Epub] CrossRef
- Anatomical and radiographic assessment of variations of the mental foramen and their impact on success of local anaesthesia administration
- 2,993 View
- 50 Download
- 8 Web of Science
- 8 Crossref

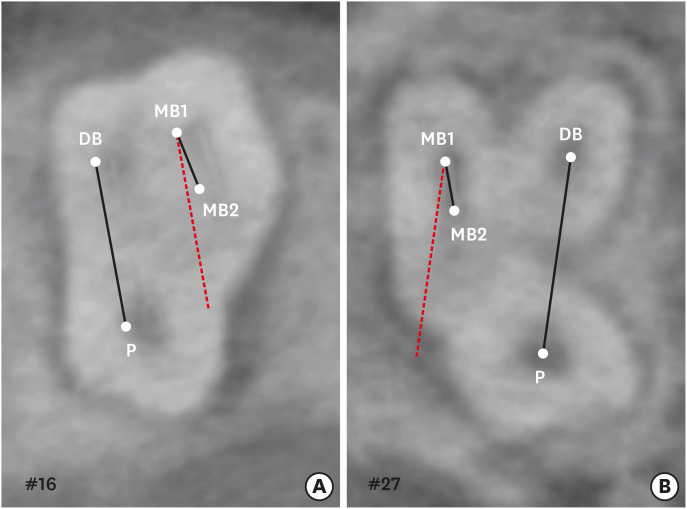
- A cone-beam computed tomography study of the prevalence and location of the second mesiobuccal root canal in maxillary molars
- Seong-Ju Lee, Eun-Hye Lee, Se-Hee Park, Kyung-Mo Cho, Jin-Woo Kim
- Restor Dent Endod 2020;45(4):e46. Published online September 3, 2020
- DOI: https://doi.org/10.5395/rde.2020.45.e46
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives This study aimed to investigate the incidence and location of the second mesiobuccal root (MB2) canal in maxillary molars with the aid of various measuring points and lines using cone-beam computed tomography (CT).
Materials and Methods A total of 205 images of patients who underwent cone-beam CT examinations between 2011 and 2015 as part of their dental diagnosis and treatment were included. There were 76 images of the maxillary first molar and 135 images of the maxillary second molar. Canal orifices were detected at −1 mm from the top of the pulpal floor on cone-beam CT images. Image assessment was performed by 2 observers in reformatted image planes using software. Assessments included measurement of the distance between the MB1 and MB2 canals, and the angles between the lines connecting the MB1-MB2 and distobuccal (DB)-palatal (P) canals. The data were analyzed using the student's
t -test.Results The prevalence of the MB2 canal was 86.8% in the first molar and 28.9% in the second molar. The angle between the lines connecting the MB1-MB2 and DB-P canals was 2.3° ± 5.7° in the first molar and −3.95° ± 7.73° in the second molar. The distance between the MB1 and MB2 canals was 2.1 ± 0.44 mm in the first molar and 1.98 ± 0.42 mm in the second molar.
Conclusions The angles between the lines connecting the MB1-MB2 and DB-P canals was almost parallel. These findings may aid in the prediction of the location of the MB2 canal orifice.
-
Citations
Citations to this article as recorded by- Position of Second Mesiobuccal Canal Relative to Distobuccal and Palatal Canals of Maxillary Molars in an Iranian Population
Sina Mosadeghian, Azadeh Torkzadeh, Parisa Ranjbarian, Roya Asaadi
Journal of Research in Dental and Maxillofacial Sciences.2025; 10(1): 34. CrossRef - Machine Learning Models in the Detection of MB2 Canal Orifice in CBCT Images
Shishir Shetty, Meliz Yuvali, Ilker Ozsahin, Saad Al-Bayatti, Sangeetha Narasimhan, Mohammed Alsaegh, Hiba Al-Daghestani, Raghavendra Shetty, Renita Castelino, Leena R David, Dilber Uzun Ozsahin
International Dental Journal.2025; 75(3): 1640. CrossRef - EVALUATION OF THE PREVALENCE AND LOCATION OF SECOND MESIOBUCCAL CANALS IN 2100 UPPER FIRST AND SECOND MOLAR TEETH: A CONE BEAM COMPUTED TOMOGRAPHY STUDY
Bahar Kaplan, Özkan Adıgüzel, Ayşe Gül Öner Talmaç, Elif Meltem Aslan
İnönü Üniversitesi Sağlık Hizmetleri Meslek Yüksek Okulu Dergisi.2025; 13(3): 752. CrossRef - A novel method for the precise second mesiobuccal canal orifice location: A combined strategy for enhanced clinical practice
Yuhan Wang, Lingyun Li, Lu Zhang, Xiaoyan Wang
Journal of Dental Sciences.2025;[Epub] CrossRef - Study on the Geometric Location Method of the Danger Zone in the Mesial Roots of Mandibular First Molars
Jinjie Yan, Yuanling Peng, Jing Yang, Jie Liu, Linxian Wang, Tingyuan Zhao, Jian Zhang, Kehua Que
Journal of Endodontics.2025;[Epub] CrossRef - The Correlation between Intraorifice Distance and the Anatomical Characteristics of the Second Mesiobuccal Canal of Maxillary Molars: A CBCT Study
Isabella Perondi, Silvio Taschieri, Martino Baruffaldi, Roberto Fornara, Luca Francetti, Stefano Corbella, Deepa Gurunathan
International Journal of Dentistry.2024;[Epub] CrossRef - Endodontic management of type I maxillary first molar with two palatal roots using cone-beam computed tomography
Nuha Alghamdi
Dental Journal.2024; 57(1): 1. CrossRef - 3D geometric analysis of second mesiobuccal canal in permanent maxillary first molar tooth
Indrani Khadilkar, Divya Nangia, Amrita Chawla, Sidhartha Sharma, Vijay Kumar, Shalini Gupta, Ajay Logani
Australian Endodontic Journal.2023; 49(1): 140. CrossRef - Prevalence of mesiobuccal-2 canals in maxillary first and second molars among the Bruneian population—CBCT analysis
Hui Yi Onn, Malissa Siao Yun Abdullah Sikun, Hanif Abdul Rahman, Jagjit Singh Dhaliwal
BDJ Open.2022;[Epub] CrossRef - Location angle of second mesio-buccal canal in maxillary molars of an Indian population: an in vivo retrospective CBCT evaluation and proposal of a new classification
Kishor Vhorkate, Kulvinder Banga, Ajinkya M. Pawar, Shugufta Mir, Suraj Arora, Dian Agustin Wahjuningrum, Anuj Bhardwaj, Alexander Maniangat Luke
PeerJ.2022; 10: e14234. CrossRef - Maxillary molar root and canal morphology of Neolithic and modern Chinese
H.Y. Ren, K.Y. Kum, Y.S. Zhao, Y.J. Yoo, J.S. Jeong, Hiran Perinpanayagam, X.Y. Wang, G.J. Li, F. Wang, H. Fang, Y. Gu
Archives of Oral Biology.2021; 131: 105272. CrossRef
- Position of Second Mesiobuccal Canal Relative to Distobuccal and Palatal Canals of Maxillary Molars in an Iranian Population
- 4,085 View
- 45 Download
- 11 Crossref

- The prevalence of radix molaris in the mandibular first molars of a Saudi subpopulation based on cone-beam computed tomography
- Hassan AL-Alawi, Saad Al-Nazhan, Nassr Al-Maflehi, Mazen A. Aldosimani, Mohammed Nabil Zahid, Ghadeer N. Shihabi
- Restor Dent Endod 2020;45(1):e1. Published online November 14, 2019
- DOI: https://doi.org/10.5395/rde.2020.45.e1
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives The purpose of this study was to determine the incidence of radix molaris (RM) (entomolaris and paramolaris) in the mandibular first permanent molars of a sample Saudi Arabian subpopulation using cone-beam computed tomography (CBCT).
Materials and Methods A total of 884 CBCT images of 427 male and 457 female Saudi citizens (age 16 to 70 years) were collected from the radiology department archives of 4 dental centers. A total of 450 CBCT images of 741 mature mandibular first molars that met the inclusion criteria were reviewed. The images were viewed at high resolution by 3 examiners and were analyzed with Planmeca Romexis software (version 5.2).
Results Thirty-three (4.5%) mandibular first permanent molars had RM, mostly on the distal side. The incidence of radix entomolaris (EM) was 4.3%, while that of radix paramolaris was 0.3%. The RM roots had one canal and occurred more unilaterally. No significant difference in root configuration was found between males and females (
p > 0.05). Types I and III EM root canal configurations were most common, while type B was the only RP configuration observed.Conclusions The incidence of RM in the mandibular first molars of this Saudi subpopulation was 4.5%. Identification of the supernumerary root can avoid missing the canal associated with the root during root canal treatment.
-
Citations
Citations to this article as recorded by- Evaluation of the variations of mandibular molars and the distance from root apex to the inferior alveolar nerve in Saudi Sub-population: Three-dimensional radiographic evaluation
Tariq Mohammed Aqili, Esam Sami Almuzaini, Abdulbari Saleh Aljohani, Ahmed Khaled Al Saeedi, Hassan Abdulmuti Hammudah, Muath Alassaf, Muhannad M. Hakeem, Mohmed Isaqali Karobari
PLOS ONE.2025; 20(2): e0317053. CrossRef - Prevalence of radix molaris in mandibular molars of a subpopulation of Brazil’s Northeast region: a cross-sectional CBCT study
Yasmym Martins Araújo de Oliveira, Maria Clara Mendes Gomes, Maria Fernanda da Silva Nascimento, Ricardo Machado, Danna Mota Moreira, Hermano Camelo Paiva, George Táccio de Miranda Candeiro
Scientific Reports.2025;[Epub] CrossRef - Prevalence of radix entomolaris and distolingual canals and their association with the incidence of middle mesial canals in mandibular first molars of a Saudi subpopulation
Ahmed A. Madfa, Abdullah F. Alshammari, Eyad Almagadawyi, Afaf Al-Haddad, Ebtsam A. Aledaili
Scientific Reports.2025;[Epub] CrossRef - Assessment of the root and canal morphology in the permanent dentition of Saudi Arabian population using cone beam computed and micro-computed tomography – a systematic review
Mohammed Mustafa, Rumesa Batul, Mohmed Isaqali Karobari, Hadi Mohammed Alamri, Abdulaziz Abdulwahed, Ahmed A. Almokhatieb, Qamar Hashem, Abdullah Alsakaker, Mohammad Khursheed Alam, Hany Mohamed Aly Ahmed
BMC Oral Health.2024;[Epub] CrossRef - Prevalence of radix accesoria dentis in a northern Peruvian population evaluated by cone-beam tomography
Karla Renata León-Almanza, Anthony Adrián Jaramillo-Nuñez, Catherin Angélica Ruiz-Cisneros, Paul Martín Herrera-Plasencia
Heliyon.2024; 10(16): e35919. CrossRef - Radix molaris is a hidden truth of mandibular first permanent molars: A descriptive- analytic study using cone beam computed tomography
Mohammed A. Alobaid, Saurabh Chaturvedi, Ebtihal Mobarak S. Alshahrani, Ebtsam M. Alshehri, Amal S. Shaiban, Mohamed Khaled Addas, Giuseppe Minervini
Technology and Health Care.2023; 31(5): 1957. CrossRef - Prevalence of Radix Entomolaris in Mandibular Permanent Molars Analyzed by Cone-Beam CT in the Saudi Population of Ha'il Province
Moazzy I Almansour, Ahmed A Madfa, Adhwaa F Algharbi, Reem Almuslumani, Noeer K Alshammari, Ghufran M Al Hussain
Cureus.2023;[Epub] CrossRef - Prevalence of radix entomolaris in India and its comparison with the rest of the world
Sumit MOHAN, Jyoti THAKUR
Minerva Dental and Oral Science.2022;[Epub] CrossRef - Radix Paramolaris an Endodontic Challenge: A Case Report
Ashwini B Prasad, Deepak Raisingani, Ridhima Gupta, Rimjhim Jain
Journal of Mahatma Gandhi University of Medical Sciences and Technology.2022; 7(1): 32. CrossRef - Evaluation of Radix Entomolaris and Middle Mesial Canal in Mandibular Permanent First Molars in an Iraqi Subpopulation Using Cone‐Beam Computed Tomography
Ranjdar Mahmood Talabani, Kazhan Omer Abdalrahman, Rawa Jamal Abdul, Dlsoz Omer Babarasul, Sara Hilmi Kazzaz, Heng Bo Jiang
BioMed Research International.2022;[Epub] CrossRef - Evaluation of Root Canal Configuration of Maxillary and Mandibular First Molar by CBCT: A Retrospective Cross-Sectional Study
Rakan Rafdan Alhujhuj, Rizwan Jouhar, Muhammad Adeel Ahmed, Abdullatif Abdulrahman Almujhim, Mohammed Tariq Albutayh, Necdet Adanir
Diagnostics.2022; 12(9): 2121. CrossRef - Ethnical Anatomical Differences in Mandibular First Permanent Molars between Indian and Saudi Arabian Subpopulations: A Retrospective Cross-sectional Study
Abdulwahab Alamir, Mohammed Mashyakhy, Apathsakayan Renugalakshmi, Thilla S Vinothkumar, Anandhi S Arthisri, Ahmed Juraybi
The Journal of Contemporary Dental Practice.2021; 22(5): 484. CrossRef
- Evaluation of the variations of mandibular molars and the distance from root apex to the inferior alveolar nerve in Saudi Sub-population: Three-dimensional radiographic evaluation
- 2,523 View
- 36 Download
- 12 Crossref

- Fused roots of maxillary molars: characterization and prevalence in a Latin American sub-population: a cone beam computed tomography study
- Maytté Marcano-Caldera, Jose Luis Mejia-Cardona, María del Pilar Blanco-Uribe, Elena Carolina Chaverra-Mesa, Didier Rodríguez-Lezama, Jose Hernán Parra-Sánchez
- Restor Dent Endod 2019;44(2):e16. Published online April 22, 2019
- DOI: https://doi.org/10.5395/rde.2019.44.e16
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives The upper molars generally have three roots; therefore, different combinations of fusion can occur, increasing the possibility of finding more complex root canal systems. The purpose of this study was to evaluate the prevalence and characterization of fused roots in first and second maxillary molars using cone-beam computed tomography (CBCT) in a Colombian population.
Materials and Methods A total of 1274 teeth were evaluated, of which 534 were maxillary first molars and 740 were maxillary second molars. Axial sections were made at the cervical, middle, and apical levels to determine the prevalence of root fusion and the types of fusion.
Results Overall, 43% of the molars (
n = 551) presented some type of fused root. Root fusion was present in 23.4% of the maxillary first molars. The most frequent type of fused root was type 3 (distobuccal-palatal; DB-P) (58.9%). Root fusion was observed in 57.6% of the maxillary second molars, and the most prevalent type of fused root was type 6 (cone-shaped) (45.2%). Of the maxillary molars, 12.5% were classified as C-shaped.Conclusion Within the limitations of this study, there was a high prevalence of fused roots in maxillary molars in the Colombian population, mainly in the maxillary second molars. In first molars, the most common type of fused root was type 3 (DB-P) and in second molars, the most common type was type 6 (cone-shaped). Additionally, molars with root fusion presented variation at different levels of the radicular portion, with implications for treatment quality.
-
Citations
Citations to this article as recorded by- Intentional Tooth Replantation: Current Evidence and Future Research Directions for Case Selection, Extraction Approaches, and Post-Operative Management
Rahul Minesh Shah, Thomas Manders, Georgios Romanos
Dentistry Journal.2026; 14(1): 59. CrossRef - Management of a rare bilateral maxillary first molar with six canals using a cone-beam computed tomography: Report of two cases
Aishwarya D. Jain, Nimisha Chinmay Shah, Abhya Jain, Shreya S. Volety
Saudi Endodontic Journal.2025; 15(2): 186. CrossRef - Assessment of root and root canal morphology in maxillary molars with fused roots using Cone Beam Computer Tomography (CBCT) in a Sri Lankan population
Ruvienath Daham Weerasinghe Rajapaksa, Manil Christopher Nishan Fonseka, Ruwan Duminda Jayasinghe, Rasika Manori Jayasinghe
Journal of Oral Biology and Craniofacial Research.2025; 15(6): 1297. CrossRef - Cone-beam computed tomography evaluation of root and canal morphology of maxillary molars in a Chinese kazakh population
Shuchun Yang, Chenye Li, Hui Shi, Ming Liu, Xu Wang
BMC Oral Health.2025;[Epub] CrossRef - A Twisted Tale of Dilacerated Fused Roots Mimicking Radicular Dens Invaginatus
Rashmi D Sathe, Preeti P. Nair, Richa Bajpai, Bidushi Mishra
Journal of the International Clinical Dental Research Organization.2025; 17(2): 214. CrossRef - Exploring the sex-associated differences in molars fused roots
Maria Eduarda Nunis Locks, Erika Calvano Küchler, Leonardo Santos Antunes, Alice Corrêa Silva-Sousa, Natanael Henrique Ribeiro Mattos, Camila Paiva Perin, Paulo Henrique Condeixa França, Peter Proff, Christian Kirschneck, Flares Baratto-Filho
Annals of Anatomy - Anatomischer Anzeiger.2024; 254: 152245. CrossRef - Cone beam computed tomography analysis of the root and canal morphology of the maxillary second molars in a Syrian subpopulation
Safaa Allawi, Mouhammad Al-Tayyan, Hassan Achour, Eyad Al-Toutangy, Yasser Alsayed Tolibah
BMC Oral Health.2024;[Epub] CrossRef - Prevalence of root fusion in canine maxillary second molar teeth using cone-beam computed tomography
Kristin Linder, Scott MacGee, Loren Schultz
Frontiers in Veterinary Science.2023;[Epub] CrossRef - Dentine thickness in maxillary fused molars depends on the fusion type: An ex vivo micro‐computed tomography study
Cangül Keskin, Defne Toplu, Ali Keleş
International Endodontic Journal.2023; 56(5): 637. CrossRef - Root and canal-specific features of maxillary first molars with fused roots
Katarina Beljic-Ivanovic, Branislav Karadzic
Vojnosanitetski pregled.2022; 79(11): 1092. CrossRef - Micro-CT Analysis of the Root Canal Configuration of Maxillary Second Molars with Fusion
Cangül KESKİN, Özgür ÖZDEMİR, Ali KELEŞ
European Annals of Dental Sciences.2022; 49(Suppl 1): 25. CrossRef - Assessment of C-Shaped Canal Morphology in Mandibular and Maxillary Second Molars in an Iraqi Subpopulation Using Cone-Beam Computed Tomography
Kazhan Abdalrahman, Ranjdar Talabani, Sara Kazzaz, Dlsoz Babarasul, Berndt Koslowski
Scanning.2022; 2022: 1. CrossRef - Analysis of Root and Canal Morphology of Fused and Separate Rooted Maxillary Molar Teeth in Turkish Population
H Aydin
Nigerian Journal of Clinical Practice.2021; 24(3): 435. CrossRef - Investigating prevalence of dental anomalies in Eastern Province of Saudi Arabia through digital orthopantomogram
Jehan ALHumaid, Maryam Buholayka, Arishiya Thapasum, Muhanad Alhareky, Maha Abdelsalam, Amr Bughsan
Saudi Journal of Biological Sciences.2021; 28(5): 2900. CrossRef - Preferred Reporting Items for Epidemiologic Cross-sectional Studies on Root and Root Canal Anatomy Using Cone-beam Computed Tomographic Technology: A Systematized Assessment
Jorge N.R. Martins, Anil Kishen, Duarte Marques, Emmanuel João Nogueira Leal Silva, João Caramês, António Mata, Marco A. Versiani
Journal of Endodontics.2020; 46(7): 915. CrossRef - Second mesiobuccal root canal in maxillary molars—A systematic review and meta-analysis of prevalence studies using cone beam computed tomography
Jorge N.R. Martins, Duarte Marques, Emmanuel João Nogueira Leal Silva, João Caramês, António Mata, Marco A. Versiani
Archives of Oral Biology.2020; 113: 104589. CrossRef
- Intentional Tooth Replantation: Current Evidence and Future Research Directions for Case Selection, Extraction Approaches, and Post-Operative Management
- 1,954 View
- 14 Download
- 16 Crossref

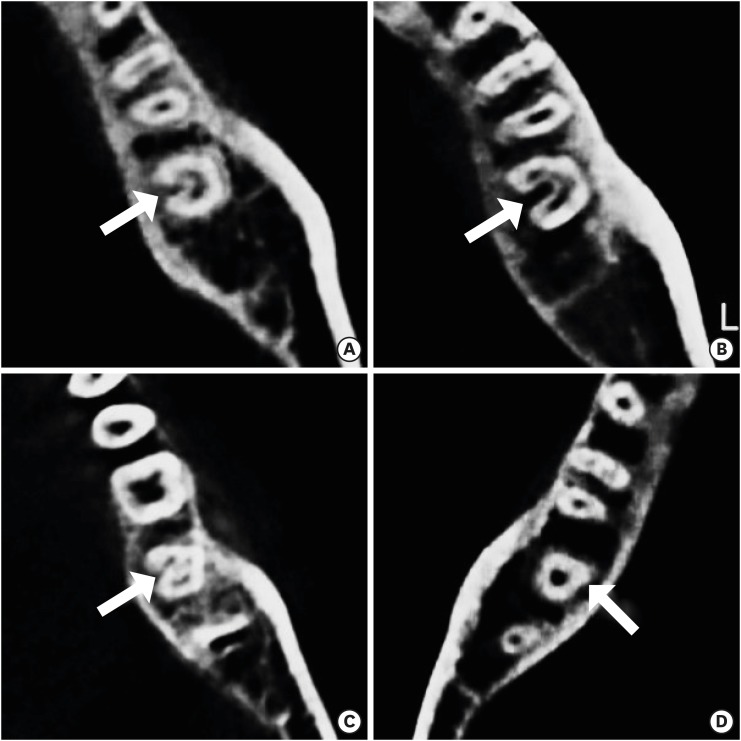
- C-shaped root canals of mandibular second molars in a Korean population: a CBCT analysis
- Hee-Sun Kim, Daun Jung, Ho Lee, Yoon-Sic Han, Sohee Oh, Hye-Young Sim
- Restor Dent Endod 2018;43(4):e42. Published online November 1, 2018
- DOI: https://doi.org/10.5395/rde.2018.43.e42
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives The purpose of this study was to investigate the C-shaped root canal anatomy of mandibular second molars in a Korean population.
Materials and Methods A total of 542 teeth were evaluated using cone-beam computed tomography (CBCT). The canal shapes were classified according to a modified version of Melton's method at the level where the pulp chamber floor became discernible.
Results Of the 542 mandibular second molars, 215 (39.8%) had C-shaped canals, 330 (53%) had 3 canals, 17 (3.3%) had 2 canals, 12 (2.2%) had 4 canals, and 8 (1.7%) had 1 canal. The prevalence of C-shaped canals was 47.8% in females and 28.4% in males. Seventy-seven percent of the C-shaped canals showed a bilateral appearance. The prevalence of C-shaped canals showed no difference according to age or tooth position. Most teeth with a C-shaped canal system presented Melton's type II (45.6%) and type III (32.1%) configurations.
Conclusions There was a high prevalence of C-shaped canals in the mandibular second molars of the Korean population studied. CBCT is expected to be useful for endodontic diagnosis and treatment planning of mandibular second molars.
-
Citations
Citations to this article as recorded by- A cone-beam computed tomography-based morphometric comparison of mandibular molars between Han Chinese and Malays
Jacob John, Wei Cheong Ngeow, Ting-Chun Shen, Lih-Jyh Fuh, Phrabhakaran Nambiar, Yen-Wen Shen, Jui-Ting Hsu
Journal of Dental Sciences.2026; 21(1): 265. CrossRef - Prevalence of C‐Shaped Canals in Maxillary Molars in an Iranian Population: A Cone‐Beam Computed Tomography Analysis
Amin Salem Milani, Shahin Namvar Asl Amirkhizi, Tahmineh Razi, Ahmad Nouroloyouni, Pouya Sabanik, Nikhat Kaura
International Journal of Clinical Practice.2026;[Epub] CrossRef - Evaluation of mandibular and maxillary second molar root canal anatomy in a Turkish subpopulation using CBCT: comparison of Briseno-Marroquin and Vertucci classifications
Hüseyin Gürkan Güneç, İpek Öreroğlu, Kemal Çağlar, Kader Cesur Aydin
BMC Medical Imaging.2025;[Epub] CrossRef - Dentin thickness of C-shaped root canal walls in mandibular premolars based on cone-beam computed tomography: a retrospective cross-sectional study
Elif Aslan, Ali Canberk Ulusoy, Bilge Hakan Sen, B. Guniz Baksi, Erinc Onem, Ali Mert
Restorative Dentistry & Endodontics.2025; 50(2): e18. CrossRef - Prevalence of c-shaped canal morphology in premolar and molar teeth assessed by cone-beam computed tomography: systematic review and meta-analysis
Faezeh Yousefi, Younes Mohammadi, Elham Shokri
BMC Oral Health.2025;[Epub] CrossRef - Anatomical complexity in mandibular second molars: prevalence of C-shaped canals, radicular grooves, taurodontism, and radices molarum in Saudi population
Ahmed A. Madfa, Abdullah F. Alshammari, Eyad Almagadawyi, Ebtsam A. Aledaili, Afaf Al-Haddad
Scientific Reports.2025;[Epub] CrossRef - Imaging Findings of Clinical Significance in Endodontics During Cone Beam Computed Tomography Scanning of the Upper Airway—The Anterior, Bilateral, C-Shaped, Dual of Mandibular Root Canals: A Brief Case Report
Edgar García-Torres, Diana Laura Grissel Guerrero-Falcón, Hugo Alejandro Bojórquez-Armenta, Oscar Eduardo Almeda-Ojeda, Víctor Hiram Barajas-Pérez, Luis Javier Solís-Martínez
Diagnostics.2025; 15(24): 3157. CrossRef - Frequency of C-Shaped Root Canals in Permanent Mandibular Second Molars in a Sample of Pakistani Population using Cone Beam Computed Tomography
Syed Nabeel Ahmed, Muhammad Mansoor Majeed, Sakina Kazmi, Muhammad Omar Ansari
Pakistan Journal of Health Sciences.2024; : 109. CrossRef - ANÁLISE DAS VARIAÇÕES ANATÔMICAS DE CANAIS C-SHAPED NOS MOLARES INFERIORES: UMA REVISÃO INTEGRATIVA DA LITERATURA
Larissa Eulália Pereira, Thayana Karla Guerra Lira dos Santos
Revista Contemporânea.2024; 4(5): e4264. CrossRef - External Validation of the Effect of the Combined Use of Object Detection for the Classification of the C-Shaped Canal Configuration of the Mandibular Second Molar in Panoramic Radiographs: A Multicenter Study
Sujin Yang, Kee-Deog Kim, Yoshitaka Kise, Michihito Nozawa, Mizuho Mori, Natsuho Takata, Akitoshi Katsumata, Yoshiko Ariji, Wonse Park, Eiichiro Ariji
Journal of Endodontics.2024; 50(5): 627. CrossRef - A Cone‐Beam Computed Tomography Evaluation of C‐Shaped Canal Configuration in Maxillary Molars Among an Iranian Population
Nafiseh Nikkerdar, Mohammad Moslehi, Amin Golshah, Mario Dioguardi
International Journal of Dentistry.2024;[Epub] CrossRef - Root and canal morphology of mandibular second molars in an Egyptian subpopulation: a cone-beam computed tomography study
Shehabeldin Mohamed Saber, Mohammed abou El Seoud, Shaimaa Mohamed Abu el Sadat, Nawar Naguib Nawar
BMC Oral Health.2023;[Epub] CrossRef - Comprehensive evaluation of root and root canal morphology of mandibular second molars in a Saudi subpopulation evaluated by cone-beam computed tomography
Moazzy I. Almansour, Saad M. Al‑Zubaidi, Abdulmjeed S. Enizy, Ahmed A. Madfa
BMC Oral Health.2022;[Epub] CrossRef - Assessment of C-Shaped Canal Morphology in Mandibular and Maxillary Second Molars in an Iraqi Subpopulation Using Cone-Beam Computed Tomography
Kazhan Abdalrahman, Ranjdar Talabani, Sara Kazzaz, Dlsoz Babarasul, Berndt Koslowski
Scanning.2022; 2022: 1. CrossRef - Cone-beam computed tomography evaluation of C-shaped root canal system in mandibular second molars in kuwaiti sub-population
AbdullahJassim Alenezi, Saad Al-Nazhan, Nassr Al-Maflehi, MazenA Aldosimani
Saudi Endodontic Journal.2022; 12(3): 283. CrossRef - Prevalence and morphology of C‐shaped and non‐C‐shaped root canal systems in mandibular second molars
T Fenelon, P Parashos
Australian Dental Journal.2022;[Epub] CrossRef - Evaluation of C-shaped canals in mandibular second molars of a selected patient group using cone beam computed tomography: prevalence, configuration and radicular groove types
Sema Sönmez Kaplan, Tuna Kaplan, Güzide Pelin Sezgin
Odontology.2021; 109(4): 949. CrossRef - Prevalência estimada de canais “C- Shaped”: Uma revisão sistemática e meta-análise
Natália Pereira da Silva Falcão, Sandro Junio de Oliveira Tavares, Ludmila Silva Guimarães, Katherine Azevedo Batistela Rodrigues Thuller, Leonardo dos Santos Antunes, Estefano Borgo Sarmento, Fellipe Navarro Azevedo de Azevedo, Cinthya Cristina Gomes, Ca
Revista Científica Multidisciplinar Núcleo do Conhecimento.2020; : 91. CrossRef - Preferred Reporting Items for Epidemiologic Cross-sectional Studies on Root and Root Canal Anatomy Using Cone-beam Computed Tomographic Technology: A Systematized Assessment
Jorge N.R. Martins, Anil Kishen, Duarte Marques, Emmanuel João Nogueira Leal Silva, João Caramês, António Mata, Marco A. Versiani
Journal of Endodontics.2020; 46(7): 915. CrossRef - Clinical and radiological assessment of the anatomical and topographic structure of the root canals of teeth in patients of different age groups
N.B. Petrukhina, O.A. Zorina, O.A. Boriskina, I.S. Berkutova, V.A. Venediktova, R.R. Saltovets
Stomatologiya.2020; 99(5): 32. CrossRef
- A cone-beam computed tomography-based morphometric comparison of mandibular molars between Han Chinese and Malays
- 2,347 View
- 13 Download
- 20 Crossref

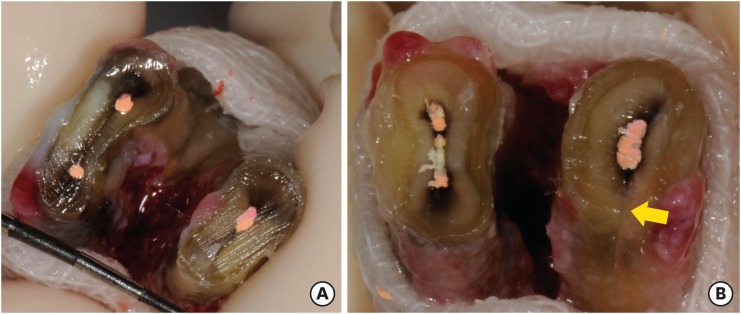
- Anatomical analysis of the resected roots of mandibular first molars after failed non-surgical retreatment
- Jiyoung Yoon, Byeong-Hoon Cho, Jihyun Bae, Yonghoon Choi
- Restor Dent Endod 2018;43(2):e16. Published online March 5, 2018
- DOI: https://doi.org/10.5395/rde.2018.43.e16
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives Understanding the reason for an unsuccessful non-surgical endodontic treatment outcome, as well as the complex anatomy of the root canal system, is very important. This study examined the cross-sectional root canal structure of mandibular first molars confirmed to have failed non-surgical root canal treatment using digital images obtained during intentional replantation surgery, as well as the causative factors of the failed conventional endodontic treatments.
Materials and Methods This study evaluated 115 mandibular first molars. Digital photographic images of the resected surface were taken at the apical 3 mm level and examined. The discolored dentin area around the root canal was investigated by measuring the total surface area, the treated areas as determined by the endodontic filling material, and the discolored dentin area.
Results Forty 2-rooted teeth showed discolored root dentin in both the mesial and distal roots. Compared to the original filled area, significant expansion of root dentin discoloration was observed. Moreover, the mesial roots were significantly more discolored than the distal roots. Of the 115 molars, 92 had 2 roots. Among the mesial roots of the 2-rooted teeth, 95.7% of the roots had 2 canals and 79.4% had partial/complete isthmuses and/or accessory canals.
Conclusions Dentin discoloration that was not visible on periapical radiographs and cone-beam computed tomography was frequently found in mandibular first molars that failed endodontic treatment. The complex anatomy of the mesial roots of the mandibular first molars is another reason for the failure of conventional endodontic treatment.
-
Citations
Citations to this article as recorded by- In vitro evaluation of the sealing ability of combined use of iRoot BP Plus and iRoot SP for root-end filling
Xu Dong, Qian Xie, Xin Xu
Clinical Oral Investigations.2023; 27(6): 2969. CrossRef - The Impact of the Preferred Reporting Items for Case Reports in Endodontics (PRICE) 2020 Guidelines on the Reporting of Endodontic Case Reports
Sofian Youssef, Phillip Tomson, Amir Reza Akbari, Natalie Archer, Fayjel Shah, Jasmeet Heran, Sunmeet Kandhari, Sandeep Pai, Shivakar Mehrotra, Joanna M Batt
Cureus.2023;[Epub] CrossRef - Clinical diagnostic approach in the treatment of chronic periodontitis in mandibular molars: Clinical cases
M. A. Postnikov, A. M. Golovachev, S. E. Chigarina, D. N. Kudryashov, I. A. Zakharova, S. A. Burakshaev
Kuban Scientific Medical Bulletin.2023; 30(5): 100. CrossRef - Evaluation of interorifice distance in permanent mandibular first molar with middle mesial canal in Bengaluru city, Karnataka: A cone-beam computed tomography study
Shruthika Mahajan, N. Meena, Anithakumari Rangappa, Ali Mohammed Mashood, Chethana Murthy, M. Lokapriya
Endodontology.2023; 35(2): 100. CrossRef - A comparative study of the effects of gutta‐percha solvents on human osteoblasts and murine fibroblasts
Gul Ipek Gundogan, Sare Durmus, Gulgun Cansu Ozturk, Nazmi Kucukyesil, Yasin Talat Acar, Rumeysa Balaban, Cenk Kig
Australian Endodontic Journal.2021; 47(3): 569. CrossRef - Endodontic retreatment of curved root canals using the dual wavelength erbium, chromium:yttrium, scandium, gallium, garnet, and diode 940-nm lasers and the XP-Endoshaper/finisher technique
Riman Nasher, Ralf-Dieter Hilgers, Norbert Gutknecht
Lasers in Dental Science.2020; 4(4): 211. CrossRef - Evaluation of gutta-percha removal from the dentinal tubules using different instrumentation techniques with or without solvent: An In vitro study
MukeshKumar Hasija, Babita Meena, Deepti Wadhwa, KulvinderKaur Wadhwani, Virender Yadav
Journal of the International Clinical Dental Research Organization.2020; 12(1): 27. CrossRef
- In vitro evaluation of the sealing ability of combined use of iRoot BP Plus and iRoot SP for root-end filling
- 1,607 View
- 10 Download
- 7 Crossref

- Management of large class II lesions in molars: how to restore and when to perform surgical crown lengthening?
- Ana Belén Dablanca-Blanco, Juan Blanco-Carrión, Benjamín Martín-Biedma, Purificación Varela-Patiño, Alba Bello-Castro, Pablo Castelo-Baz
- Restor Dent Endod 2017;42(3):240-252. Published online August 3, 2017
- DOI: https://doi.org/10.5395/rde.2017.42.3.240
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub The restoration of endodontic tooth is always a challenge for the clinician, not only due to excessive loss of tooth structure but also invasion of the biological width due to large decayed lesions. In this paper, the 7 most common clinical scenarios in molars with class II lesions ever deeper were examined. This includes both the type of restoration (direct or indirect) and the management of the cavity margin, such as the need for deep margin elevation (DME) or crown lengthening. It is necessary to have the DME when the healthy tooth remnant is in the sulcus or at the epithelium level. For caries that reaches the connective tissue or the bone crest, crown lengthening is required. Endocrowns are a good treatment option in the endodontically treated tooth when the loss of structure is advanced.
-
Citations
Citations to this article as recorded by- Awareness and Practice of Deep Margin Elevation among Dental Practitioners in India: A Cross-Sectional Survey
Mythri Padaru, Preethesh Shetty, Namith Rai, Raksha Bhat
Pesquisa Brasileira em Odontopediatria e Clínica Integrada.2025;[Epub] CrossRef - Rubber dam isolation to optimise intraoral scanning and the restoration of teeth with subgingival margins
Renato Lardin Sartori Sanchez, Gisele Lie Fukuoka, Nathália Pereira Censi Stapani, Isabella Neme Ribeiro dos Reis
BMJ Case Reports.2025; 18(4): e264082. CrossRef - Impact of spacers and thermocycling on porosity and gaps in class II endodontic temporary restorations evaluated by microcomputed tomography
Fahda N. Algahtani, Manal Alkadi, Hiba R. Talic, Sarah S. AlShalawi, Lujain M. Alqarni, Reem M. Barakat, Rasha Haridy, Sara M. ElKhateeb, Rahaf A. Almohareb
Scientific Reports.2025;[Epub] CrossRef - Deep Margin Elevation: Current Evidence and a Critical Approach to Clinical Protocols—A Narrative Review
Athanasios Karageorgiou, Maria Fostiropoulou, Maria Antoniadou, Eftychia Pappa
Adhesives.2025; 1(3): 10. CrossRef - Deep margin elevation in restorative dentistry: A scoping review
Anna Taylor, Lorna Burns
Journal of Dentistry.2024; 146: 105066. CrossRef - Effect of cervical margin relocation on marginal adaptation and microleakage of indirect ceramic restorations
Marwa Adel, Amina Hamdy, Ahmed Sabet, Kamal Ebeid
Journal of Prosthodontics.2024; 33(4): 374. CrossRef - Application of one-piece endodontic crowns fabricated with CAD-CAM system to molars
Haruto Hiraba, Kensuke Nishio, Yoshimasa Takeuchi, Takashi Ito, Tetsuo Yamamori, Atsushi Kamimoto
Japanese Dental Science Review.2024; 60: 81. CrossRef - Structurally compromised teeth. Part II: A novel approach to peripheral build up procedures
Guido Fichera, Claudia Mazzitelli, Vincenzo Picciariello, Tatjana Maravic, Uros Josic, Annalisa Mazzoni, Lorenzo Breschi
Journal of Esthetic and Restorative Dentistry.2024; 36(1): 20. CrossRef - Biomimetic Restorative Dentistry: an evidence-based discussion of common myths
Alessandra REIS, Victor Pinheiro FEITOSA, Ana Cláudia CHIBINSKI, Michael Willian FAVORETO, Mario Felipe GUTIERREZ, Alessandro Dourado LOGUERCIO
Journal of Applied Oral Science.2024;[Epub] CrossRef - Comparative clinical evaluation of correct anatomic contour and tight contact in Class II direct composite restoration using two newer contact forming instruments
Jaimini Patel, Nimisha C. Shah, Meetkumar Dedania, Deebah Choudhary, Nidhi Bharti, Aishwarya Jain
Journal of Conservative Dentistry and Endodontics.2024; 27(11): 1135. CrossRef - Effect of Deep Margin Elevation on the Pulpal and Periodontal Health of Teeth: A Systematic Review
S Srirama, S Jain, B Arul, K Prabakar, V Natanasabapathy
Operative Dentistry.2024; 49(4): 388. CrossRef - New Technique for Wedge Selection in Direct Class II Restorations: A Pilot Study
Tania Gancedo-Gancedo, Benjamín Martín-Biedma, Javier Domínguez-Cachón, Sara Garrido-Parada, Victoria Ababii, Patricia Pereira-Lores, Sandra García-Varela, Pablo Castelo-Baz
Journal of Clinical Medicine.2024; 13(5): 1324. CrossRef - Different Designs of Deep Marginal Elevation and Its Influence on Fracture Resistance of Teeth with Monolith Zirconia Full-Contour Crowns
Ali Robaian, Abdullah Alqahtani, Khalid Alanazi, Abdulrhman Alanazi, Meshal Almalki, Anas Aljarad, Refal Albaijan, Ahmed Maawadh, Aref Sufyan, Mubashir Baig Mirza
Medicina.2023; 59(4): 661. CrossRef - M-i-M for DME: matrix-in-a-matrix technique for deep margin elevation
Pascal Magne
The Journal of Prosthetic Dentistry.2023; 130(4): 434. CrossRef - A New Concept of Posterior Mini-invasive Restorations: Clinical Procedures and Requirements—Case Report
Zeineb Riahi, Belhassen Harzallah, Mounir Cherif, Dalenda Hadyaoui, Imen Kalghoum, Oumayma Mejri
CODS - Journal of Dentistry.2023; 14(2): 61. CrossRef - Evaluation of biologic width re-establishment using CHU aesthetic gauges in crown lengthening cases- a clinical study
Avantika Rani, Shiva Shankar Gummaluri, Hirak S. Bhattacharya, Preeti Bhattacharya, Sumbul Saifi, saummya singh
Journal of Oral Biology and Craniofacial Research.2023; 13(2): 138. CrossRef - Interfacial integrity of bulk-fill resin composite restorations in deep Class-II cavities
Rana Abdelrehim SEDKY, Hooi Pin CHEW, Khaled Aly NOUR, Shaimaa Mohamed ABUELSADAT, Dina ELSHERBINI, Alex Siu Lun FOK
Dental Materials Journal.2023; 42(5): 692. CrossRef - Biological evaluation of indirect restorations in endodontically treated posterior teeth with deeply located proximal margins following deep margin elevation versus surgical crown lengthening: a randomized controlled trial
Ahmed Tarek Farouk, Olfat El Sayed Hassanein, Ola Ibrahim Fahmy, Ahmed M. Elkady, Hani ElNahass
Clinical Oral Investigations.2023;[Epub] CrossRef - Deep Margin Elevation: Current Concepts and Clinical Considerations: A Review
Majed Aldakheel, Khalid Aldosary, Shatha Alnafissah, Rahaf Alaamer, Anwar Alqahtani, Nora Almuhtab
Medicina.2022; 58(10): 1482. CrossRef - Deep Margin Elevation: A Literature Review
Theodora Kalliopi Samartzi, Dimokritos Papalexopoulos, Panagiotis Ntovas, Christos Rahiotis, Markus B. Blatz
Dentistry Journal.2022; 10(3): 48. CrossRef - Examination of caries‐affected dentin and composite‐resin interface after different caries removal methods: A scanning electron microscope study
Nazmiye Donmez, Magrur Kazak, Zeynep Buket Kaynar, Yesim Sesen Uslu
Microscopy Research and Technique.2022; 85(6): 2212. CrossRef - Clinical performance of indirect restorations with cervical margin relocation in posterior teeth: A systematic review
Ghaida Alhumaidan, Raghad Alammar, Dhafer Al Asmari, Ali Alenezi
Dentistry Review.2022; 2(1): 100034. CrossRef - Current Strategies to Control Recurrent and Residual Caries with Resin Composite Restorations: Operator- and Material-Related Factors
Moataz Elgezawi, Rasha Haridy, Moamen A. Abdalla, Katrin Heck, Miriam Draenert, Dalia Kaisarly
Journal of Clinical Medicine.2022; 11(21): 6591. CrossRef - Survival and success of endocrowns: A systematic review and meta-analysis
Raghad A. Al-Dabbagh
The Journal of Prosthetic Dentistry.2021; 125(3): 415.e1. CrossRef - The Relationships Between Tooth‐Supported Fixed Dental Prostheses and Restorations and the Periodontium
Carlo Ercoli, Dennis Tarnow, Carlo E. Poggio, Alexandra Tsigarida, Marco Ferrari, Jack G. Caton, Konstantinos Chochlidakis
Journal of Prosthodontics.2021; 30(4): 305. CrossRef - Placement of Posterior Composite Restorations: A Cross-Sectional Study of Dental Practitioners in Al-Kharj, Saudi Arabia
Mohamed M. Awad, Mansour Alradan, Nawaf Alshalan, Ali Alqahtani, Feras Alhalabi, Mohammed Ali Salem, Ahmed Rabah, Ali Alrahlah
International Journal of Environmental Research and Public Health.2021; 18(23): 12408. CrossRef - Microleakage of Direct Restorations-Comparisonbetween Bulk-Fill and Traditional Composite Resins:Systematic Review and Meta-Analysis
Francesca Zotti, Edoardo Falavigna, Giorgia Capocasale, Daniele De Santis, Massimo Albanese
European Journal of Dentistry.2021; 15(04): 755. CrossRef - Assessment of knowledge, attitude, and practice regarding Deep Margin Elevation (DME) among dental practitioners in Riyadh, Saudi Arabia
Sultan R. Binalrimal, Weam M. Banjar, Sara H. Alyousef, Mada I. Alawad, Ghalia I. Alawad
Journal of Family Medicine and Primary Care.2021; 10(5): 1931. CrossRef - Treatment Prognosis of Restored Teeth with Crown Lengthening vs. Deep Margin Elevation: A Systematic Review
Maryam H. Mugri, Mohammed E. Sayed, Binoy Mathews Nedumgottil, Shilpa Bhandi, A. Thirumal Raj, Luca Testarelli, Zohaib Khurshid, Saurabh Jain, Shankargouda Patil
Materials.2021; 14(21): 6733. CrossRef - Direct resin composite restoration of endodontically-treated permanent molars in adolescents: bite force and patient-specific finite element analysis
Monise de Paula RODRIGUES, Priscilla Barbosa Ferreira SOARES, Márcio Alex Barros GOMES, Renata Afonso PEREIRA, Daranee TANTBIROJN, Antheunis VERSLUIS, Carlos Jose SOARES
Journal of Applied Oral Science.2020;[Epub] CrossRef - Up to 12 years clinical evaluation of 197 partial indirect restorations with deep margin elevation in the posterior region
R.A. Bresser, D. Gerdolle, I.A. van den Heijkant, L.M.A. Sluiter-Pouwels, M.S. Cune, M.M.M. Gresnigt
Journal of Dentistry.2019; 91: 103227. CrossRef - How biomechanics can affect the endodontic treated teeth and their restorative procedures?
Carlos José Soares, Monise de Paula Rodrigues, André Luis Faria-e-Silva, Paulo Cesar Freitas Santos-Filho, Crisnicaw Veríssimo, Hyeon-Cheol Kim, Antheunis Versluis
Brazilian Oral Research.2018;[Epub] CrossRef
- Awareness and Practice of Deep Margin Elevation among Dental Practitioners in India: A Cross-Sectional Survey
- 3,291 View
- 108 Download
- 32 Crossref

- Maxillary first molar with 7 root canals diagnosed using cone-beam computed tomography
- Evaldo Rodrigues, Antônio Henrique Braitt, Bruno Ferraz Galvão, Emmanuel João Nogueira Leal da Silva
- Restor Dent Endod 2017;42(1):60-64. Published online August 29, 2016
- DOI: https://doi.org/10.5395/rde.2017.42.1.60
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Root canal anatomy is complex, and the recognition of anatomic variations could be a challenge for clinicians. This case report describes the importance of cone beam computed tomographyic (CBCT) imaging during endodontic treatment. A 23 year old woman was referred by her general dental practitioner with the chief complaint of spontaneous pain in her right posterior maxilla. From the clinical and radiographic findings, a diagnosis of symptomatic irreversible pulpitis was made and endodontic treatment was suggested to the patient. The patient underwent CBCT examination, and CBCT scan slices revealed seven canals: three mesiobuccal (MB1, MB2, and MB3), two distobuccal (DB1 and DB2), and two palatal (P1 and P2). Canals were successfully treated with reciprocating files and filled using single-cone filling technique. Precise knowledge of root canal morphology and its variation is important during root canal treatment. CBCT examination is an excellent tool for identifying and managing these complex root canal systems.
-
Citations
Citations to this article as recorded by- KONİK IŞINLI BİLGİSAYARLI TOMOGRAFİ İLE DOĞRULANMIŞ OLAĞANDIŞI ÜST BİRİNCİ BÜYÜK AZI DİŞİN ENDODONTİK TEDAVİSİ
Didem Seda Gültekin, Funda Kont Çobankara
Journal of International Dental Sciences.2025; 11(1): 46. CrossRef - Clinical Significance of Mesiobuccal and Distobuccal Canal Variations in Maxillary Molars: A Case Series and a Mini Review
Mohsen Aminsobhani, Somayeh Majidi, Vlaho Brailo
Case Reports in Dentistry.2025;[Epub] CrossRef - An Unusual Case of Maxillary First Molar: A Case Report
Reetu Shrestha
International Journal of Innovative Science and Research Technology (IJISRT).2024; : 1330. CrossRef - Root canal therapy of maxillary first molar with seven canals diagnosed using cone beam computed tomography – a case report
Saini Rashmi, Saini V. Kumar
Tanta Dental Journal.2022; 19(3): 169. CrossRef - Four-Rooted Maxillary First Molars: A Systematic Review and Meta-Analysis
Gabriel Magnucki, Sven V. K. Mietling, Sreekanth Kumar Mallineni
International Journal of Dentistry.2021; 2021: 1. CrossRef - Endodontic treatment of various palatal roots in maxillary molars
Chengshi Wei, Keyi Li, Lili Shen, Guangliang Bai, Xiufen Tian
The Journal of the American Dental Association.2021; 152(12): 1044. CrossRef - Diversity of root canal morphology of maxillary first molars
Juhász Kincső-Réka, Kovács Mónika, Pop Mihai, Pop Silvia, Kerekes-Máthé Bernadette
Bulletin of Medical Sciences.2021; 94(1): 63. CrossRef - Endodontic Management of Maxillary First Molar with Seven Root Canals Diagnosed Using Cone-beam Computed Tomography: A Case Report
Ravindranath Megha, Venkatachalam Prakash
World Journal of Dentistry.2021; 12(1): 89. CrossRef - Endodontic management of the maxillary first molar with special root canals: A case report and review of the literature
Zhi-Hui Zhang, Hai-Lin Yao, Yan Zhang, Xiao Wang
World Journal of Clinical Cases.2020; 8(12): 2590. CrossRef - Management of a permanent maxillary first molar with unusual crown and root anatomy: a case report
Prateeksha Chowdhry, Pallavi Reddy, Mamta Kaushik
Restorative Dentistry & Endodontics.2018;[Epub] CrossRef - Usefulness of cone beam computed tomography in perplexing endodontic cases
Amandeep Kaur, Ajay Logani
Endodontology.2018; 30(2): 187. CrossRef - Endodontic management of a maxillary first molar with seven root canal systems evaluated using cone-beam computed tomography scanning
VijayReddy Venumuddala, Sridhar Moturi, SV Satish, BKalyan Chakravarthy, Sudhakar Malapati
Journal of International Society of Preventive and Community Dentistry.2017; 7(5): 297. CrossRef
- KONİK IŞINLI BİLGİSAYARLI TOMOGRAFİ İLE DOĞRULANMIŞ OLAĞANDIŞI ÜST BİRİNCİ BÜYÜK AZI DİŞİN ENDODONTİK TEDAVİSİ
- 2,428 View
- 15 Download
- 12 Crossref

- Healing outcomes of root canal treatment for C-shaped mandibular second molars: a retrospective analysis
- Hye-Ra Ahn, Young-Mi Moon, Sung-Ok Hong, Min-Seock Seo
- Restor Dent Endod 2016;41(4):262-270. Published online August 29, 2016
- DOI: https://doi.org/10.5395/rde.2016.41.4.262
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives This study aimed to evaluate the healing rate of non-surgical endodontic treatment between C-shaped and non-C-shaped mandibular second molars.
Materials and Methods Clinical records and radiological images of patients who had undergone endodontic treatment on mandibular second molars between 2007 and 2014 were screened. The periapical index scoring system was applied to compare healing outcomes. Information about preoperative and postoperative factors as well as the demographic data of the patients was acquired and evaluated using chi-square and multinomial logistic regression tests.
Results The total healing rate was 68.4%. Healing rates for the mandibular second molar were 70.9% in C-shaped canals (
n = 79) and 66.6% in non-C-shaped ones (n = 117). The difference was not statistically significant.Conclusions The presence of a C-shaped canal in the mandibular second molar did not have a significantly negative effect on healing after treatment. Instead, proper pulpal diagnosis and final restoration were indicated as having significantly greater influence on the healing outcomes of C-shaped and non-C-shaped canals, respectively.
-
Citations
Citations to this article as recorded by- Predicting early endodontic treatment failure following primary root canal treatment
Young-Eun Jang, Yemi Kim, Sin-Young Kim, Bom Sahn Kim
BMC Oral Health.2024;[Epub] CrossRef - Factors Influencing Non-Surgical Root Canal Treatment Outcomes in Mandibular Second Molars: A Retrospective Cone-Beam Computed Tomography Analysis
Da-Min Park, Woo-Hyun Seok, Ji-Young Yoon
Journal of Clinical Medicine.2024; 13(10): 2931. CrossRef - Retrospective Assessment of Healing Outcome of Endodontic Treatment for Mandibular Molars with C-shaped Root Canal
Kishore Kumar Majety, Basanta Kumar Choudhury, Anika Bansal, Achla Sethi, Jaina Panjabi
The Journal of Contemporary Dental Practice.2017; 18(7): 591. CrossRef
- Predicting early endodontic treatment failure following primary root canal treatment
- 1,938 View
- 20 Download
- 3 Crossref

- Radix mesiolingualis and radix distolingualis: a case report of a tooth with an unusual morphology
- Gurudutt Nayak, Himanshu Aeran, Inderpreet Singh
- Restor Dent Endod 2016;41(4):322-331. Published online July 14, 2016
- DOI: https://doi.org/10.5395/rde.2016.41.4.322
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Variation in the root and canal morphology of the maxillary first molars is quite common. The most common configuration is 3 roots and 3 or 4 canals. Nonetheless, other possibilities still exist. The presence of an additional palatal root is rather uncommon and has been reported to have an incidence of 0.06 - 1.6% in varying populations studied. Whenever two palatal roots exist, one of them is the normal palatal root, the other is a supernumerary structure which can be located either mesiolingually (radix mesiolingualis) or distolingually (radix distolingualis). This case report describes successful endodontic treatment of a maxillary first molar with radix mesiolingualis and radix distolingualis. Identification of this variation was done through clinical examination along with the aid of multiangled radiographs, and an accurate assessment of this morphology was made with the help of a cone-beam computed tomography imaging. In addition to the literature review, this article also discusses the epidemiology, classifications, morphometric features, guidelines for diagnosis, and endodontic management of a maxillary first molar with extra-palatal root.
-
Citations
Citations to this article as recorded by- Four-Rooted Maxillary First Molars: A Systematic Review and Meta-Analysis
Gabriel Magnucki, Sven V. K. Mietling, Sreekanth Kumar Mallineni
International Journal of Dentistry.2021; 2021: 1. CrossRef
- Four-Rooted Maxillary First Molars: A Systematic Review and Meta-Analysis
- 1,956 View
- 9 Download
- 1 Crossref

- Proximity of the mandibular molar root apex from the buccal bone surface: a cone-beam computed tomographic study
- Dokyung Kim, Jung-Hong Ha, Myoung-Uk Jin, Young-Kyung Kim, Sung Kyo Kim
- Restor Dent Endod 2016;41(3):182-188. Published online July 14, 2016
- DOI: https://doi.org/10.5395/rde.2016.41.3.182
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives The purpose of this study was to evaluate the proximity of the mandibular molar apex to the buccal bone surface in order to provide anatomic information for apical surgery.
Materials and Methods Cone-beam computed tomography (CBCT) images of 127 mandibular first molars and 153 mandibular second molars were analyzed from 160 patients' records. The distance was measured from the buccal bone surface to the root apex and the apical 3.0 mm on the cross-sectional view of CBCT.
Results The second molar apex and apical 3 mm were located significantly deeper relative to the buccal bone surface compared with the first molar (
p < 0.01). For the mandibular second molars, the distance from the buccal bone surface to the root apex was significantly shorter in patients over 70 years of age (p < 0.05). Furthermore, this distance was significantly shorter when the first molar was missing compared to nonmissing cases (p < 0.05). For the mandibular first molars, the distance to the distal root apex of one distal-rooted tooth was significantly greater than the distance to the disto-buccal root apex (p < 0.01). In mandibular second molar, the distance to the apex of C-shaped roots was significantly greater than the distance to the mesial root apex of non-C-shaped roots (p < 0.01).Conclusions For apical surgery in mandibular molars, the distance from the buccal bone surface to the apex and apical 3 mm is significantly affected by the location, patient age, an adjacent missing anterior tooth, and root configuration.
-
Citations
Citations to this article as recorded by- Expert consensus on intentional tooth replantation
Zhengmei Lin, Dingming Huang, Shuheng Huang, Zhi Chen, Qing Yu, Benxiang Hou, Lihong Qiu, Wenxia Chen, Jiyao Li, Xiaoyan Wang, Zhengwei Huang, Jinhua Yu, Jin Zhao, Yihuai Pan, Shuang Pan, Deqin Yang, Weidong Niu, Qi Zhang, Shuli Deng, Jingzhi Ma, Xiuping
International Journal of Oral Science.2025;[Epub] CrossRef - Outcome of intentional replantation of endodontically treated teeth with periapical pathosis: A systematic review and meta‐analysis
Faizan Javed, Kamil Zafar, Farhan R. Khan
Australian Endodontic Journal.2023; 49(S1): 494. CrossRef - Proximity of maxillary molar apexes to the cortical bone surface and the maxillary sinus
Han Shin Lee, Dokyung Kim, Sung Kyo Kim
Restorative Dentistry & Endodontics.2022;[Epub] CrossRef - Alveolar bone thickness overlying healthy maxillary and mandibular teeth: A systematic review and meta-analysis
Marziyeh Shafizadeh, Azita Tehranchi, Armin Shirvani, Saeed Reza Motamedian
International Orthodontics.2021; 19(3): 389. CrossRef - Relationship between the anatomic structures and mandibular posterior teeth for endodontic surgery in a Turkish population: a cone-beam computed tomographic analysis
Zeliha Uğur Aydın, Duygu Göller Bulut
Clinical Oral Investigations.2019; 23(9): 3637. CrossRef
- Expert consensus on intentional tooth replantation
- 2,223 View
- 5 Download
- 5 Crossref

- Analysis of C-shaped root canal configuration in maxillary molars in a Korean population using cone-beam computed tomography
- Hyoung-Hoon Jo, Jeong-Bum Min, Ho-Keel Hwang
- Restor Dent Endod 2016;41(1):55-62. Published online January 29, 2016
- DOI: https://doi.org/10.5395/rde.2016.41.1.55
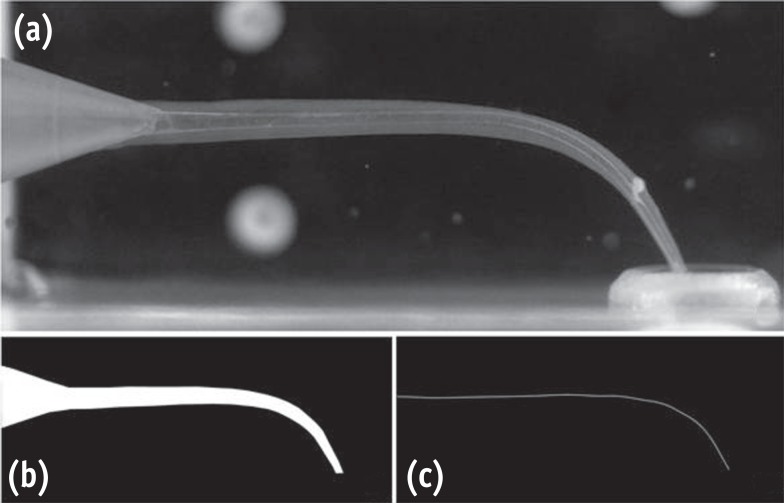
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives The purpose of this study was to investigate the incidence of root fusion and C-shaped root canals in maxillary molars, and to classify the types of C-shaped canal by analyzing cone-beam computed tomography (CBCT) in a Korean population.
Materials and Methods Digitized CBCT images from 911 subjects were obtained in Chosun University Dental Hospital between February 2010 and July 2012 for orthodontic treatment. Among them, a total of selected 3,553 data of maxillary molars were analyzed retrospectively. Tomography sections in the axial, coronal, and sagittal planes were displayed by PiViewstar and Rapidia MPR software (Infinitt Co.). The incidence and types of root fusion and C-shaped root canals were evaluated and the incidence between the first and the second molar was compared using Chi-square test.
Results Root fusion was present in 3.2% of the first molars and 19.5% of the second molars, and fusion of mesiobuccal and palatal root was dominant. C-shaped root canals were present in 0.8% of the first molars and 2.7% of the second molars. The frequency of root fusion and C-shaped canal was significantly higher in the second molar than the first molar (
p < 0.001).Conclusions In a Korean population, maxillary molars showed total 11.3% of root fusion and 1.8% of C-shaped root canals. Furthermore, root fusion and C-shaped root canals were seen more frequently in the maxillary second molars.
-
Citations
Citations to this article as recorded by- Prevalence of C‐Shaped Canals in Maxillary Molars in an Iranian Population: A Cone‐Beam Computed Tomography Analysis
Amin Salem Milani, Shahin Namvar Asl Amirkhizi, Tahmineh Razi, Ahmad Nouroloyouni, Pouya Sabanik, Nikhat Kaura
International Journal of Clinical Practice.2026;[Epub] CrossRef - Prevalence of c-shaped canal morphology in premolar and molar teeth assessed by cone-beam computed tomography: systematic review and meta-analysis
Faezeh Yousefi, Younes Mohammadi, Elham Shokri
BMC Oral Health.2025;[Epub] CrossRef - A Cone‐Beam Computed Tomography Evaluation of C‐Shaped Canal Configuration in Maxillary Molars Among an Iranian Population
Nafiseh Nikkerdar, Mohammad Moslehi, Amin Golshah, Mario Dioguardi
International Journal of Dentistry.2024;[Epub] CrossRef - Endodontic treatment of a C‐shaped mandibular second molar with narrow dentinal thickness: A case report
Mina Mehrjouei, Hamid Jafarzadeh, Pourya Esmaeelpour, Maryam Khorasanchi
Clinical Case Reports.2024;[Epub] CrossRef - Evaluation of 2- and 3-dimensional anatomic parameters of C-shaped root canals with cone beam computed tomography, microcomputed tomography, and nanocomputed tomography
Miguel Angel Ventura Molina, Giovane Oliveira Silva, Amanda Pelegrin Candemil, Rafael Verardino de Camargo, Ruben Pauwels, Reinhilde Jacobs, Manoel Damião Sousa-Neto, Jardel Francisco Mazzi-Chaves
Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology.2023; 136(6): 759. CrossRef - Cone-Beam Computed Tomography (CBCT) Analysis of an Unusual Configuration of the Upper First Molar With a C-shaped Canal With Apically Fused Roots: A Case Report
Kapil D Wahane, Anand V Bansod, Sudha mattigatti, Rushikesh Mahaparale, Yuvraj B Rote, Mayur B Wanjari
Cureus.2023;[Epub] CrossRef - Assessment of C-Shaped Canal Morphology in Mandibular and Maxillary Second Molars in an Iraqi Subpopulation Using Cone-Beam Computed Tomography
Kazhan Abdalrahman, Ranjdar Talabani, Sara Kazzaz, Dlsoz Babarasul, Berndt Koslowski
Scanning.2022; 2022: 1. CrossRef - Root and canal-specific features of maxillary first molars with fused roots
Katarina Beljic-Ivanovic, Branislav Karadzic
Vojnosanitetski pregled.2022; 79(11): 1092. CrossRef - Diagnosis and treatment of maxillary molar with abnormality
Kkot-Byeol Bae, Bin-Na Lee, Hoon-Sang Chang, In-Nam Hwang, Won-Mann Oh, Yun-Chan Hwang
Oral Biology Research.2022; 46(4): 195. CrossRef - Endodontic treatment of the maxillary first molar with palatal canal variations: A case report and review of literature
Kai Chen, Xing Ran, Yan Wang
World Journal of Clinical Cases.2022; 10(32): 12036. CrossRef - Evaluation of C-shaped canals in maxillary molars in a Chinese population using CBCT
Yuyan Qian, Yamei Li, Jukun Song, Ping Zhang, Zhu Chen
BMC Medical Imaging.2022;[Epub] CrossRef - Comprehensive evaluation of root and root canal morphology of mandibular second molars in a Saudi subpopulation evaluated by cone-beam computed tomography
Moazzy I. Almansour, Saad M. Al‑Zubaidi, Abdulmjeed S. Enizy, Ahmed A. Madfa
BMC Oral Health.2022;[Epub] CrossRef - Evaluation of C-shaped canal configuration in maxillary molars: A retrospective cone-beam computed tomography study
Emre KÖSE, Rüya AK
Clinical and Experimental Health Sciences.2021; 11(3): 444. CrossRef - Maxillary First Molars with Two Palatal Root Canals
Kun-Hwa Sung, Ho-Keel Hwang, Hyoung-Hoon Jo, Konstantinos Michalakis
Case Reports in Dentistry.2021;[Epub] CrossRef - Preferred Reporting Items for Epidemiologic Cross-sectional Studies on Root and Root Canal Anatomy Using Cone-beam Computed Tomographic Technology: A Systematized Assessment
Jorge N.R. Martins, Anil Kishen, Duarte Marques, Emmanuel João Nogueira Leal Silva, João Caramês, António Mata, Marco A. Versiani
Journal of Endodontics.2020; 46(7): 915. CrossRef - Evaluation of root and root canal morphology of elderly Korean patients maxillary molars using cone-beam computed tomography
Tae-Yong Lee, Mi-Yeon Kim, Sun-Ho Kim, Jeong-Hee Kim
The Journal of Korean Academy of Prosthodontics.2020; 58(2): 95. CrossRef - Second mesiobuccal root canal in maxillary molars—A systematic review and meta-analysis of prevalence studies using cone beam computed tomography
Jorge N.R. Martins, Duarte Marques, Emmanuel João Nogueira Leal Silva, João Caramês, António Mata, Marco A. Versiani
Archives of Oral Biology.2020; 113: 104589. CrossRef - Prevalência estimada de canais “C- Shaped”: Uma revisão sistemática e meta-análise
Natália Pereira da Silva Falcão, Sandro Junio de Oliveira Tavares, Ludmila Silva Guimarães, Katherine Azevedo Batistela Rodrigues Thuller, Leonardo dos Santos Antunes, Estefano Borgo Sarmento, Fellipe Navarro Azevedo de Azevedo, Cinthya Cristina Gomes, Ca
Revista Científica Multidisciplinar Núcleo do Conhecimento.2020; : 91. CrossRef - Evaluation of the internal anatomy of paramolar tubercles using cone-beam computed tomography
G. Colakoglu, I. Kaya Buyukbayram, M. A. Elcin, M. Kazak, H. Sezer
Surgical and Radiologic Anatomy.2020; 42(1): 15. CrossRef - Analysis of Prevalence of Pyramidal Molars in Adolescent
Woojin Kwon, Hyung-Jun Choi, Jaeho Lee, Je Seon Song
THE JOURNAL OF THE KOREAN ACADEMY OF PEDTATRIC DENTISTRY.2020; 47(4): 389. CrossRef - Prevalence Studies on Root Canal Anatomy Using Cone-beam Computed Tomographic Imaging: A Systematic Review
Jorge N.R. Martins, Duarte Marques, Emmanuel João Nogueira Leal Silva, João Caramês, Marco A. Versiani
Journal of Endodontics.2019; 45(4): 372. CrossRef - Fused roots of maxillary molars: characterization and prevalence in a Latin American sub-population: a cone beam computed tomography study
Maytté Marcano-Caldera, Jose Luis Mejia-Cardona, María del Pilar Blanco-Uribe, Elena Carolina Chaverra-Mesa, Didier Rodríguez-Lezama, Jose Hernán Parra-Sánchez
Restorative Dentistry & Endodontics.2019;[Epub] CrossRef - An original micro‐CT study and meta‐analysis of the internal and external anatomy of maxillary molars—implications for endodontic treatment
Iwona M. Tomaszewska, Anna Jarzębska, Bendik Skinningsrud, Przemysław A. Pękala, Sebastian Wroński, Joe Iwanaga
Clinical Anatomy.2018; 31(6): 838. CrossRef - A Cone-beam Computed Tomographic Study of Root and Canal Morphology of Maxillary First and Second Permanent Molars in a Thai Population
Roserin Ratanajirasut, Anchana Panichuttra, Soontra Panmekiate
Journal of Endodontics.2018; 44(1): 56. CrossRef - Retrospective Assessment of Healing Outcome of Endodontic Treatment for Mandibular Molars with C-shaped Root Canal
Kishore Kumar Majety, Basanta Kumar Choudhury, Anika Bansal, Achla Sethi, Jaina Panjabi
The Journal of Contemporary Dental Practice.2017; 18(7): 591. CrossRef - The morphology of maxillary first and second molars analyzed by cone-beam computed tomography in a polish population
Katarzyna Olczak, Halina Pawlicka
BMC Medical Imaging.2017;[Epub] CrossRef
- Prevalence of C‐Shaped Canals in Maxillary Molars in an Iranian Population: A Cone‐Beam Computed Tomography Analysis
- 1,914 View
- 14 Download
- 26 Crossref

- Endodontic treatment of a C-shaped mandibular second premolar with four root canals and three apical foramina: a case report
- Thikamphaa Bertrand, Sahng Gyoon Kim
- Restor Dent Endod 2016;41(1):68-73. Published online January 19, 2016
- DOI: https://doi.org/10.5395/rde.2016.41.1.68
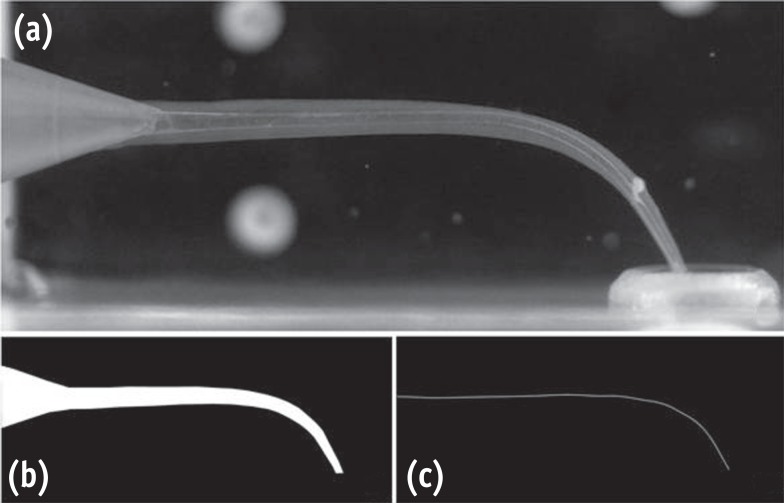
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub This case report describes a unique C-shaped mandibular second premolar with four canals and three apical foramina and its endodontic management with the aid of cone-beam computer tomography (CBCT). C-shaped root canal morphology with four canals was identified under a dental operating microscope. A CBCT scan was taken to evaluate the aberrant root canal anatomy and devise a better instrumentation strategy based on the anatomy. All canals were instrumented to have a 0.05 taper using 1.0 mm step-back filing with appropriate apical sizes determined from the CBCT scan images and filled using a warm vertical compaction technique. A C-shaped mandibular second premolar with multiple canals is an anatomically rare case for clinicians, yet its endodontic treatment may require a careful instrumentation strategy due to the difficulty in disinfecting the canals in the thin root area without compromising the root structure.
-
Citations
Citations to this article as recorded by- Unique root anatomy of mandibular second premolars: clinical strategies for effective disinfection and preservation of dentine structure in root canal treatment—a case report
Ji Wook Jeong, Erika Silguero Gonzalez, Scott R. Makins, Timothy Kirkpatrick
Frontiers in Dental Medicine.2024;[Epub] CrossRef - PRICE 2020 guidelines for reporting case reports in Endodontics: explanation and elaboration
V. Nagendrababu, B. S. Chong, P. McCabe, P. K. Shah, E. Priya, J. Jayaraman, S. J. Pulikkotil, P. M. H. Dummer
International Endodontic Journal.2020; 53(7): 922. CrossRef - A cone-beam computed tomography study of C-shaped root canal systems in mandibular second premolars in a Taiwan Chinese subpopulation
Yi-Chin Chen, Chia-Lun Tsai, Yi-Chen Chen, Gin Chen, Shue-Fen Yang
Journal of the Formosan Medical Association.2018; 117(12): 1086. CrossRef - Anatomic Comparison of Contralateral Premolars
Gaute Floer Johnsen, Sazan Dara, Sameenah Asjad, Pia Titterud Sunde, Håvard Jostein Haugen
Journal of Endodontics.2017; 43(6): 956. CrossRef - Endodontic Management of Dilacerated Maxillary Central Incisor fused to a Supernumerary Tooth using Cone Beam Computed Tomography: An Unusual Clinical Presentation
Thilla S Vinothkumar, Deivanayagam Kandaswamy, Ganesh Arathi, Sathishkumar Ramkumar, Gnanasekaran Felsypremila
The Journal of Contemporary Dental Practice.2017; 18(6): 522. CrossRef
- Unique root anatomy of mandibular second premolars: clinical strategies for effective disinfection and preservation of dentine structure in root canal treatment—a case report
- 2,752 View
- 15 Download
- 5 Crossref

- Endodontic management of a maxillary first molar with three roots and seven root canals with the aid of cone-beam computed tomography
- Gurudutt Nayak, Kamal Krishan Singh, Rhitu Shekhar
- Restor Dent Endod 2015;40(3):241-248. Published online June 3, 2015
- DOI: https://doi.org/10.5395/rde.2015.40.3.241
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Variation in root canal morphology, especially in maxillary first molar presents a constant challenge for a clinician in their detection and management. This case report describes the successful root canal treatment of a three rooted right maxillary first molar presenting with three canals each in the mesiobuccal and distobuccal roots and one canal in the palatal root. The clinical detection of this morphologic aberration was made using a dental operating microscope, and the canal configuration was established after correlating and computing the clinical, radiographic and cone-beam computed tomography (CBCT) scan findings. CBCT images confirmed the configuration of the canals in the mesiobuccal and distobuccal roots to be Al-Qudah and Awawdeh type (3-2) and type (3-2-1), respectively, whereas the palatal root had a Vertucci type I canal pattern. This report reaffirms the importance of careful examination of the floor of the pulp chamber with a dental operating microscope and the use of multiangled preoperative radiographs along with advanced diagnostic aids such as CBCT in identification and successful management of aberrant canal morphologies.
-
Citations
Citations to this article as recorded by- Inhibition potential of rhamnolipid biosurfactant against Corynespora cassiicola – a phytopathogen of king chilli
Nilam Sarma, Suresh Deka, Hemen Deka
Studia Biologica.2025; 19(3): 153. CrossRef - Endodontic Management of Maxillary First Molar with Seven Root Canals Diagnosed Using Cone-beam Computed Tomography: A Case Report
Ravindranath Megha, Venkatachalam Prakash
World Journal of Dentistry.2021; 12(1): 89. CrossRef - The MB3 canal in maxillary molars: a micro-CT study
Ronald Ordinola-Zapata, Jorge N. R. Martins, Hugo Plascencia, Marco A. Versiani, Clovis M. Bramante
Clinical Oral Investigations.2020; 24(11): 4109. CrossRef - Maxillary first molar with 7 root canals diagnosed using cone-beam computed tomography
Evaldo Rodrigues, Antônio Henrique Braitt, Bruno Ferraz Galvão, Emmanuel João Nogueira Leal da Silva
Restorative Dentistry & Endodontics.2017; 42(1): 60. CrossRef - Endodontic management of a maxillary first molar with seven root canal systems evaluated using cone-beam computed tomography scanning
VijayReddy Venumuddala, Sridhar Moturi, SV Satish, BKalyan Chakravarthy, Sudhakar Malapati
Journal of International Society of Preventive and Community Dentistry.2017; 7(5): 297. CrossRef
- Inhibition potential of rhamnolipid biosurfactant against Corynespora cassiicola – a phytopathogen of king chilli
- 2,313 View
- 12 Download
- 5 Crossref

- Use of cone-beam computed tomography and three-dimensional modeling for assessment of anomalous pulp canal configuration: a case report
- Alper Sinanoglu, Dilek Helvacioglu-Yigit, Ibrahim Mutlu
- Restor Dent Endod 2015;40(2):161-165. Published online December 4, 2014
- DOI: https://doi.org/10.5395/rde.2015.40.2.161
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Three-dimensional (3D) reconstruction of cone-beam computed tomography (CBCT) scans appears to be a valuable method for assessing pulp canal configuration. The aim of this report is to describe endodontic treatment of a mandibular second premolar with aberrant pulp canal morphology detected by CBCT and confirmed by 3D modeling. An accessory canal was suspected during endodontic treatment of the mandibular left second premolar in a 21 year old woman with a chief complaint of pulsating pain. Axial cross-sectional CBCT scans revealed that the pulp canal divided into mesiobuccal, lingual, and buccal canals in the middle third and ended as four separate foramina. 3D modeling confirmed the anomalous configuration of the fused root with a deep lingual groove. Endodontic treatment of the tooth was completed in two appointments. The root canals were obturated using lateral compaction of gutta-percha and root canal sealer. The tooth remained asymptomatic and did not develop periapical pathology until 12 months postoperatively. CBCT and 3D modeling enable preoperative evaluation of aberrant root canal systems and facilitate endodontic treatment.
-
Citations
Citations to this article as recorded by- Exploring Technological Progress in Three-Dimensional Imaging for Root Canal Treatments: A Systematic Review
Kanwalpreet Kaur, Ravinder S. Saini, Sunil Kumar Vaddamanu, Shashit Shetty Bavabeedu, Vishwanath Gurumurthy, Shan Sainudeen, Vinod Babu Mathew, Shafait Ullah Khateeb, Aida Mokhlesi, Seyed Ali Mosaddad, Artak Heboyan
International Dental Journal.2025; 75(2): 1097. CrossRef - Root Canal Treatment of Oehlers Type III Dens Invaginatus in Maxillary Lateral Incisor and Remote Sinus Tract Using Dental Surgical Microscope and Cone-Beam Computed Tomography
Rie Fujii, Tomohiro Asai, Masashi Yamada, Ryo Sako, Yoshiki Tamiya, Masahiro Furusawa
The Bulletin of Tokyo Dental College.2023; 64(2): 67. CrossRef - CBCT and Micro-CT analysis of the mandibular first premolars with C-shaped canal system in a Chinese population author
Yimeng Zhang, Xunben Weng, Yu Fu, Xuekai Qi, Yihuai Pan, Yu Zhao
BMC Oral Health.2023;[Epub] CrossRef
- Exploring Technological Progress in Three-Dimensional Imaging for Root Canal Treatments: A Systematic Review
- 1,425 View
- 9 Download
- 3 Crossref

- Endodontic treatment of a mandibular first molar with 8 canals: a case report
- Ankit Arora, Shashi Rashmi Acharya, Padmaja Sharma
- Restor Dent Endod 2015;40(1):75-78. Published online October 13, 2014
- DOI: https://doi.org/10.5395/rde.2015.40.1.75
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Presented here is a case where 8 canals were located in a mandibular first molar. A patient with continuing pain in mandibular left first molar even after completion of biomechanical preparation was referred by a dentist. Following basic laws of the pulp chamber floor anatomy, 8 canals were located in three steps with 4 canals in each root. In both of the roots, 4 separate canals commenced which joined into two canals and exited as two separate foramina. At 6 mon follow-up visit, the tooth was found to be asymptomatic and revealed normal radiographic periapical area. The case stresses on the fact that understanding the laws of pulp chamber anatomy and complying with them while attempting to locate additional canals can prevent missing canals.
-
Citations
Citations to this article as recorded by- How Do Different Image Modules Impact the Accuracy of Working Length Measurements in Digital Periapical Radiography? An In Vitro Study
Vahide Hazal Abat, Rabia Figen Kaptan
Diagnostics.2025; 15(3): 305. CrossRef - Determinants of the Number of Main Canals in a Tooth: Deciphering Potential Mechanisms
Andrea Alejandra Moreno Robalino, José Luis Álvarez Vásquez
Universitas Odontologica.2023;[Epub] CrossRef - Application Of Cone-Beam Computed Tomography In Diagnosis And Treatment Of Multiple Canals– A Case Report
Gyanendra Pratap Singh, Shruthi H Attavar, Sivaji Kavuri
Annals of Dental Specialty.2022; 10(2): 15. CrossRef - Four distal root canals in a two-rooted permanent mandibular first molar
Urvashi M. Ujariya, Foram H. Patel, Rajendra P. Bharatiya, Anjali K. Kothari
Endodontology.2022; 34(3): 212. CrossRef - Utilizing Cone-Beam Computed Tomography for Identifying and Managing Multiple Canals: A Case Report
Gyanendra Pratap Singh, Shruthi H Attavar, Sivaji Kavuri
Journal of Current Research in Oral Surgery.2022; 2(1): 37. CrossRef - Morphology and prevalence of middle canals in the mandibular molars: A systematic review
Rashmi Bansal, Sapna Hegde, Madhusudan Astekar
Journal of Oral and Maxillofacial Pathology.2018; 22(2): 216. CrossRef - Endodontic management of a permanent mandibular first molar with unusual root canal configurations: Two case reports
Mohammad Ahmad Alenezi, Mustafa Aldajani, Hind O. Al-Qathami, Seraj Al-Shommrani
Saudi Endodontic Journal.2017; 7(3): 181. CrossRef
- How Do Different Image Modules Impact the Accuracy of Working Length Measurements in Digital Periapical Radiography? An In Vitro Study
- 4,746 View
- 31 Download
- 7 Crossref

- Endodontic management of a mandibular second molar with radix entomolaris: a case report
- Rosaline Hannah, Deivanayagam Kandaswamy, Nachimuthu Jayaprakash
- Restor Dent Endod 2014;39(2):132-136. Published online March 21, 2014
- DOI: https://doi.org/10.5395/rde.2014.39.2.132
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub The presence of radix entomolaris (RE) in a mandibular first molar is a common occurrence in certain ethnic groups, but the presence of RE in a mandibular second molar is a rare occurrence. In the present case, RE was identified from preoperative radiographs and confirmed using cone-beam computed tomography (CBCT). The access cavity was modified to locate the RE. Cleaning and shaping were performed with nickel-titanium rotary instruments. Obturation was completed with gutta-percha cones using AH Plus (Dentsply Detrey GmbH) as sealer. From the CBCT axial images, the RE was determined to have a Type III curvature by the De Moor classification, Type B separate RE by the Carlsen and Alexandersen classification, and radiographically, a Type i image by the Wang classification. The presence of RE in the mandibular second molar makes it essential to anticipate and treat the distolingual root canal. This case report highlights the usefulness of CBCT for assessing RE in the mandibular second molar, which can help the clinician in making a confirmatory diagnosis and assessing the morphology of the root canal.
-
Citations
Citations to this article as recorded by- Three-Dimensional Observation and Classification of Root and Root Canal Morphology in Japanese Mandibular Third Molars
Tomoyuki Inose, Satoru Matsunaga, Norio Kasahara, Masashi Yamada, Shinichi Abe, Masahiro Furusawa
Journal of Hard Tissue Biology.2026; 35(1): 7. CrossRef - Endodontic Treatment of a Mandibular Second Molar Featuring Vertucci Type V Configuration in the Distal Root: A Case Report
He Liu, Ya Shen
Cureus.2024;[Epub] CrossRef - Endodontic management of a case of radix entomolaris: A case report
Priyanka Shorey, Kitty Sidhu
IP Indian Journal of Conservative and Endodontics.2022; 7(1): 39. CrossRef - Endodontic treatment of tooth with morphological anomalies using cone-beam computed tomography
Sung-Hyeon Choi, Na-Kyung Yoon, Ji-Hyun Jang, Young-Hoon Kim, Hoon-Sang Chang, Yun-Chan Hwang, In-Nam Hwang, Won-Mann Oh, Bin-Na Lee
Oral Biology Research.2018; 42(1): 53. CrossRef - Unusual root morphology in second mandibular molar with a radix entomolaris, and comparison between cone-beam computed tomography and digital periapical radiography: a case report
Elisardo López-Rosales, Pablo Castelo-Baz, Roland De Moor, Manuel Ruíz-Piñón, Benjamín Martín-Biedma, Purificación Varela-Patiño
Journal of Medical Case Reports.2015;[Epub] CrossRef
- Three-Dimensional Observation and Classification of Root and Root Canal Morphology in Japanese Mandibular Third Molars
- 2,196 View
- 11 Download
- 5 Crossref

- Asymmetry in mesial root number and morphology in mandibular second molars: a case report
- Gurudutt Nayak, Shashit Shetty, Rhitu Shekhar
- Restor Dent Endod 2014;39(1):45-50. Published online January 20, 2014
- DOI: https://doi.org/10.5395/rde.2014.39.1.45
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Ambiguity in the root morphology of the mandibular second molars is quite common. The most common root canal configuration is 2 roots and 3 canals, nonetheless other possibilities may still exist. The presence of accessory roots is an interesting example of anatomic root variation. While the presence of radix entomolaris or radix paramolaris is regarded as a typical clinical finding of a three-rooted mandibular second permanent molar, the occurrence of an additional mesial root is rather uncommon and represents a possibility of deviation from the regular norms. This case report describes successful endodontic management of a three-rooted mandibular second molar presenting with an unusual accessory mesial root, which was identified with the aid of multiangled radiographs and cone-beam computed tomography imaging. This article also discusses the prevalence, etiology, morphological variations, clinical approach to diagnosis, and significance of supernumerary roots in contemporary clinical dentistry.
- 2,015 View
- 6 Download

- Dilemmas pertaining to three canals in the mesiobuccal root of a maxillary second molar: a case report
- Ankit Arora, Shashi Rashmi Acharya, Muliya Vidya Saraswathi, Padmaja Sharma, Amber Ather
- Restor Dent Endod 2013;38(3):172-177. Published online August 23, 2013
- DOI: https://doi.org/10.5395/rde.2013.38.3.172
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub The mesiobuccal root of the maxillary molars is well known to pose a hindrance during endodontic therapy. Presented here is a case of a maxillary left second molar where three canals were located in its mesiobuccal root with the use of visual and diagnostic aids. Difficulties encountered during the process of unveiling the tooth's internal anatomy were discussed. The dilemmas encountered pertained to the root canal configuration, the nomenclature of the extra canals, and the justification for the presence of a third canal. The root canal configuration of 3-2-1 was confirmed for the mesiobuccal root using information gained from clinical, radiographic, and multi-detector computed tomography (MDCT) scan findings. This case demonstrates the need for efforts to locate extra canals in the mesiobuccal root of the maxillary molars as their internal anatomy remains a mystery.
-
Citations
Citations to this article as recorded by- Clinical Significance of Mesiobuccal and Distobuccal Canal Variations in Maxillary Molars: A Case Series and a Mini Review
Mohsen Aminsobhani, Somayeh Majidi, Vlaho Brailo
Case Reports in Dentistry.2025;[Epub] CrossRef - A case report on endodontic management of the rarest Vertucci's Type VIII configuration in maxillary second molar with three mesiobuccal canals
ShrustiAjay Govil, Geeta Asthana, Shikha Kanodia, Abhishek Parmar
Journal of Conservative Dentistry.2021; 24(4): 404. CrossRef - The MB3 canal in maxillary molars: a micro-CT study
Ronald Ordinola-Zapata, Jorge N. R. Martins, Hugo Plascencia, Marco A. Versiani, Clovis M. Bramante
Clinical Oral Investigations.2020; 24(11): 4109. CrossRef - Three Root Canals in the Mesiobuccal Root of Maxillary Molars: Case Reports and Literature Review
Ibrahim Ali Ahmad, Anas Al-Jadaa
Journal of Endodontics.2014; 40(12): 2087. CrossRef
- Clinical Significance of Mesiobuccal and Distobuccal Canal Variations in Maxillary Molars: A Case Series and a Mini Review
- 1,693 View
- 8 Download
- 4 Crossref

- Endodontic management of a C-shaped maxillary first molar with three independent buccal root canals by using cone-beam computed tomography
- Lorena Karanxha, Hee-Jin Kim, Sung-Ok Hong, Wan Lee, Pyung-Sik Kim, Kyung-San Min
- Restor Dent Endod 2012;37(3):175-179. Published online August 29, 2012
- DOI: https://doi.org/10.5395/rde.2012.37.3.175
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub The aim of this study was to present a method for endodontic management of a maxillary first molar with unusual C-shaped morphology of the buccal root verified by cone-beam computed tomography (CBCT) images. This rare anatomical variation was confirmed using CBCT, and nonsurgical endodontic treatment was performed by meticulous evaluation of the pulpal floor. Posttreatment image revealed 3 independent canals in the buccal root obturated efficiently to the accepted lengths in all 3 canals. Our study describes a unique C-shaped variation of the root canal system in a maxillary first molar, involving the 3 buccal canals. In addition, our study highlights the usefulness of CBCT imaging for accurate diagnosis and management of this unusual canal morphology.
-
Citations
Citations to this article as recorded by- Nonsurgical endodontic retreatment of C-shaped maxillary molars: case reports and review of literature
Ming Liu, Yanling Huang, Yixuan Wu, Yi Zhang, Zhisheng Zhang, Qianju Wu
BMC Oral Health.2024;[Epub] CrossRef - Analysis of Fused Rooted Maxillary First and Second Molars with Merged and C-shaped Canal Configurations: Prevalence, Characteristics, and Correlations in a Saudi Arabian Population
Mohammed Mashyakhy, Hemant Ramesh Chourasia, Ahmad Jabali, Abdulmajeed Almutairi, Gianluca Gambarini
Journal of Endodontics.2019; 45(10): 1209. CrossRef - C-shaped root canals of mandibular second molars in a Korean population: a CBCT analysis
Hee-Sun Kim, Daun Jung, Ho Lee, Yoon-Sic Han, Sohee Oh, Hye-Young Sim
Restorative Dentistry & Endodontics.2018;[Epub] CrossRef - Prevalence and Characteristics of the Maxillary C-shaped Molar
Jorge N.R. Martins, António Mata, Duarte Marques, Craig Anderson, João Caramês
Journal of Endodontics.2016; 42(3): 383. CrossRef - Use of cone-beam computed tomography and three-dimensional modeling for assessment of anomalous pulp canal configuration: a case report
Alper Sinanoglu, Dilek Helvacioglu-Yigit, Ibrahim Mutlu
Restorative Dentistry & Endodontics.2015; 40(2): 161. CrossRef - Endodontic management of a mandibular second molar with radix entomolaris: a case report
Rosaline Hannah, Deivanayagam Kandaswamy, Nachimuthu Jayaprakash
Restorative Dentistry & Endodontics.2014; 39(2): 132. CrossRef
- Nonsurgical endodontic retreatment of C-shaped maxillary molars: case reports and review of literature
- 1,415 View
- 4 Download
- 6 Crossref

- An evaluation of canal curvature at the apical one third in type II mesial canals of mandibular molars
- Hye-Rim Yun, Dong-Kyun Lee, Ho-Keel Hwang
- Restor Dent Endod 2012;37(2):104-109. Published online May 18, 2012
- DOI: https://doi.org/10.5395/rde.2012.37.2.104
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives The purpose of this study was to evaluate the buccolingual curvature at the apical one third in type II mesial canals of mandibular molars using the radius and angle of curvature.
Materials and Methods Total 100 mandibular molars were selected. Following an endodontic access in the teeth, their distal roots were removed. #15 H- or K-files (Dentsply Maillefer) were inserted into the mesiobuccal and mesiolingual canals of the teeth. Radiographs of the teeth were taken for the proximal view. Among them, type II canals were selected and divided into two subgroups, IIa and IIb. In type IIa, two separate canals merged into one canal before reaching the apex and in type IIb, two separate canals merged into one canal within the apical foramen. The radius and angle of curvature of specimens were examined.
Results In type II, mean radius of curvature in mesiolingual and mesiobuccal canals were 2.82 mm and 3.58 mm, respectively. The radius of the curvature of mesiolingual canals were significantly smaller than that of mesiobuccal canals in type II, and especially in type IIa. However, there were no statistically significant differences in radius of curvature between mesiobuccal and mesiolingual canals in type IIb and there were no significant differences in angle of curvature between type IIa and IIb.
Conclusion In this study, type II mesial canals of mandibular molars showed severe curvature in the proximal view. Especially, mesiolingual canals of type IIa had more abrupt curvature than mesiobuccal canals at the apical one third.
- 1,148 View
- 2 Download

- A retrospective study of the intentionally replanted mandibular second molars with C-shaped root canal configurations
- Won-Jun Shon, Kee-Yeon Kum, Seung-Ho Baek, Woo-Cheol Lee
- J Korean Acad Conserv Dent 2011;36(1):19-25. Published online January 31, 2011
- DOI: https://doi.org/10.5395/JKACD.2011.36.1.19
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives The purpose of this retrospective study was to evaluate the success rate of intentionally replanted mandibular second molar with C-shaped canal configurations and to access the impact of preoperative periapical lesion on the success of intentional replantation procedure.
Materials and Methods This retrospective chart review study evaluated 52 intentionally replanted mandibular second molar teeth treated at Seoul National University Dental Hospital Department of Conservative Dentistry from January 2005 to December 2007. Seventeen teeth were lost for the follow-up, and another 6 teeth did not meet inclusion criteria of C-shaped root canal configurations. Healing outcome such as success, uncertain healing, and failure after follow-up was evaluated by clinical criteria and radiographs.
Results The overall success rate was 72.4% for the 29 intentionally replanted C-shaped mandibular second molars. The success rate of replanted teeth with preoperative periapical lesions was similar to that of replanted teeth which have no periapical lesions.
Conclusions Therefore, root canal treatment failure on C-shaped mandibular second molar can be predictably treated by intentional replantation regardless of the presence of periapical lesion.
- 1,227 View
- 6 Download

- Study of endodontic working length of Korean posterior teeth
- Jeong-Yeob Kim, Sang-Hoon Lee, Gwang-Hee Lee, Sang-Hyuk Park
- J Korean Acad Conserv Dent 2010;35(6):429-435. Published online November 30, 2010
- DOI: https://doi.org/10.5395/JKACD.2010.35.6.429
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives The aim of this study was to investigate average working lengths of Korean posterior teeth and evaluate validity of endodontic file length.
Materials and Methods The endodontic working length of the posterior teeth of 670 Korean patients were measured than each mean value and standard deviation were investigated than the frequency deviation and standard deviation per each length were calculated.
Results Among the canals of premolar, 66.5% of canal length was marked under 20 mm by endodontic working length and 95.4% could be measured under 22 mm and Among the canals of molars, 95.5% of canal length was marked under 20 mm endodontic working length.
Conclusions With the result of measurement of endodontic working length of premolars of Korean, it suggested that 23 mm endodontic file is more proper than the 21 mm and 25 mm file on the market.
-
Citations
Citations to this article as recorded by- A Rare Case of Nonsyndromic Generalized Radiculomegaly with a Literature Review
Mohammad Al-Obaida, Kevin Seymour
Case Reports in Dentistry.2020;[Epub] CrossRef - Fluoride Release and Recharge Properties of Several Fluoride-Containing Restorative Materials
Dongyun Lee, Jongsoo Kim, Miran Han, Jisun Shin
THE JOURNAL OF THE KOREAN ACADEMY OF PEDTATRIC DENTISTRY.2020; 47(2): 196. CrossRef - Comparison of Microhardness and Compressive Strength of Alkasite and Conventional Restorative Materials
Kunho Lee, Jongsoo Kim, Jisun Shin, Miran Han
THE JOURNAL OF THE KOREAN ACADEMY OF PEDTATRIC DENTISTRY.2020; 47(3): 320. CrossRef - Fluoride Release of Giomer and Compomer Through the Dental Adhesive Layer
Minseon Hwang, Howon Park, Juhyun Lee, Hyunwoo Seo
THE JOURNAL OF THE KOREAN ACADEMY OF PEDTATRIC DENTISTRY.2017; 44(2): 180. CrossRef
- A Rare Case of Nonsyndromic Generalized Radiculomegaly with a Literature Review
- 6,189 View
- 37 Download
- 4 Crossref

- Root canal treatment of a mandibular second premolar with three separate root canals
- Seok-Ryun Lee, Seol-Hee Shin, Sung-Ok Hong, Chang-Kyu Song, Hoon-Sang Chang, Kyung-San Min
- J Korean Acad Conserv Dent 2010;35(4):302-305. Published online July 31, 2010
- DOI: https://doi.org/10.5395/JKACD.2010.35.4.302
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Mandibular premolars show a wide variety of root canal anatomy. Especially, the occurrence of three canals with three separate foramina in mandibular second premolars is very rare. This case report describes the root canal treatment of an unusual morphological configuration of the root canal system and supplements previous reports of the existence of such configuration in mandibular second premolar.
-
Citations
Citations to this article as recorded by- Effective management of mandibular second premolar with root anomalies
Ashwaq Faia Asiri
Saudi Endodontic Journal.2023; 13(1): 28. CrossRef
- Effective management of mandibular second premolar with root anomalies
- 1,941 View
- 10 Download
- 1 Crossref

- A retrospective study on incidence of C-shaped canals in mandibular second molars
- Hee-Sun Kim
- J Korean Acad Conserv Dent 2009;34(4):346-349. Published online July 31, 2009
- DOI: https://doi.org/10.5395/JKACD.2009.34.4.346
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Mandibular second molars have many variations in canal configuration. Technical modifications in cleaning, shaping and obturation are required. The purpose of this study was to investigate the root canal anatomy of mandibular second molars. 86 teeth of 85 patients were accessed and evaluated with taking radiographs for working length determination. 27 teeth(31.4%) had C-shaped canals, 43 teeth(50%) had 3 canals, 11 teeth(12.7%) had 4 canals, 5 teeth(5.8%) had 2 canals. Incidence of C-shaped canal was 31.7% in male and 31.1% in female. 30.9% of left mandibular second molar and 31.8% of right mandibular second molar showed C-shaped canals.
- 791 View
- 1 Download

- Morphology of the apical root canal system in Korean mandibular first molar
- Hyeon Jeong, Sang-jin Park, Sang-Hyuk Park, Gi-Woon Choi
- J Korean Acad Conserv Dent 2009;34(2):137-144. Published online March 31, 2009
- DOI: https://doi.org/10.5395/JKACD.2009.34.2.137
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub The aim of this study was to investigate the shapes and diameters of the physiological foramen and anatomy of the root canal at 3mm from apex in mandibular first molars.
Sixty mandibular first molars were randomly selected. The apical anatomy of 60 mandibular first molars was investigated by means of a stereomicroscope (60x magnification).
The results were as follows;
1. There was a high percentage of two physiological foramina in mesial (61.67%) and one foramen in distal(71.66%) roots of mandibular first molars.
2.There was a high frequency of accessory foramina in mesial roots with one foramen (26.07%).
3. The diameters of physiological foramen was as follows:
0.329mm in single mesial foramen
0.266mm in mesiobuccal foramen and 0.246mm in mesiolingual foramen
0.375mm in single distal foramen
0.291mm in distobuccal foramen and 0.237mm in distolingual foramen
4. The most common physiological foramen shape was oval (69.93%).
5. The incidence of isthmus in mesial root at 3mm from apex was 55%. The 3mm-sections contained a complete isthmus 31.66% and a partial isthmus 23.34%.
6. 3mm from the apex, the most common canal shape was oval (50.64%).
Knowledge of the apical anatomy of mandibular first molar would be necessary for success of surgical and nonsurgical endodontic treatment.
-
Citations
Citations to this article as recorded by- Variations in Canal Morphology, Shapes, and Positions of Major Foramen in Maxillary and Mandibular Teeth
B. Swathika, Md. Kalim Ullah, S. Ganesan, Prabu Muthusamy, Prasanna Vuyyuru, Kongkana Kalita, C. Swarnalatha, Suresh J. Babu, Abhishek Singh Nayyar
Journal of Microscopy and Ultrastructure.2021; 9(4): 190. CrossRef - Assessment of Root and Root Canal Morphology of Human Primary Molars using CBCT
Yoomin Choi, Seonmi Kim, Namki Choi
THE JOURNAL OF THE KOREAN ACADEMY OF PEDTATRIC DENTISTRY.2020; 47(1): 25. CrossRef - An evaluation of canal curvature at the apical one third in type II mesial canals of mandibular molars
Hye-Rim Yun, Dong-Kyun Lee, Ho-Keel Hwang
Restorative Dentistry & Endodontics.2012; 37(2): 104. CrossRef
- Variations in Canal Morphology, Shapes, and Positions of Major Foramen in Maxillary and Mandibular Teeth
- 1,209 View
- 1 Download
- 3 Crossref

- Stress distribution of endodontically treated maxillary second premolars restored with different methods: Three-dimensional finite element analysis
- Dong-Yeol Lim, Hyeon-Cheol Kim, Bock Hur, Kwang-Hoon Kim, Kwon Son, Jeong-Kil Park
- J Korean Acad Conserv Dent 2009;34(1):69-79. Published online January 31, 2009
- DOI: https://doi.org/10.5395/JKACD.2009.34.1.069
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub The purpose of this study was to evaluate the influence of elastic modulus of restorative materials and the number of interfaces of post and core systems on the stress distribution of three differently restored endodontically treated maxillary second premolars using 3D FE analysis. Model 1, 2 was restored with a stainless steel or glass fiber post and direct composite resin. A PFG or a sintered alumina crown was considered. Model 3 was restored by EndoCrown. An oblique 500 N was applied on the buccal (Load A) and palatal (Load B) cusp. The von Mises stresses in the coronal and root structure of each model were analyzed using ANSYS. The elastic modulus of the definitive restorations rather than the type of post and core system was the primary factor that influenced the stress distribution of endodontically treated maxillary premolars. The stress concentration at the coronal structure could be lowered through the use of definitive restoration of high elastic modulus. The stress concentration at the root structure could be lowered through the use of definitive restoration of low elastic modulus.
-
Citations
Citations to this article as recorded by- How loss of tooth structure impacts the biomechanical behavior of a single-rooted maxillary premolar: FEA
Roaa Abdelwahab Abdelfattah, Nawar Naguib Nawar, Engy M. Kataia, Shehabeldin Mohamed Saber
Odontology.2024; 112(1): 279. CrossRef - Effect of Proximal Caries-driven Access on the Biomechanical Behavior of Endodontically Treated Maxillary Premolars
Nawar Naguib Nawar, Roaa Abdelwahab Abdelfattah, Mohamed Kataia, Shehabeldin Mohamed Saber, Engy Medhat Kataia, Hyeon-Cheol Kim
Journal of Endodontics.2023; 49(10): 1337. CrossRef - Survival and success of endocrowns: A systematic review and meta-analysis
Raghad A. Al-Dabbagh
The Journal of Prosthetic Dentistry.2021; 125(3): 415.e1. CrossRef - Influence of Cavity Design on Stress Distribution in Second Premolar Tooth Using Finite Element Analysis
Z. Parlar, E.U. Gökçek, K. Yildirim, A. Kahyaoglu
Acta Physica Polonica A.2017; 132(3-II): 949. CrossRef - Influence of post types and sizes on fracture resistance in the immature tooth model
Jong-Hyun Kim, Sung-Ho Park, Jeong-Won Park, Il-Young Jung
Journal of Korean Academy of Conservative Dentistry.2010; 35(4): 257. CrossRef
- How loss of tooth structure impacts the biomechanical behavior of a single-rooted maxillary premolar: FEA
- 1,759 View
- 8 Download
- 5 Crossref

- Cross-sectional morphology and minimum canal wall widths in C-shaped root of mandibular molars
- Byung-Chul Song, Yong-Bum Cho
- J Korean Acad Conserv Dent 2007;32(1):37-46. Published online January 31, 2007
- DOI: https://doi.org/10.5395/JKACD.2007.32.1.037
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub The C-shaped canal system is an anatomical variation mostly seen in mandibular second molars, although it can also occur in maxillary and other mandibular molars. The main anatomical feature of C-shaped canals is the presence of fins or web connecting the individual root canals. The complexity of C-shaped canals prevents these canals from being cleaned, shaped, and obturated effectively during root canal therapy, and sometimes it leads to an iatrogenic perforation from the extravagant preparation.
The purpose of this study was to provide further knowledge of the anatomical configuration and the minimal thickness of dentinal wall according to the level of the root.
Thirty extracted mandibular second molars with fused roots and longitudinal grooves on lingual or buccal surface of the root were collected from a native Korean population. The photo images and radiographs from buccal, lingual, apical direction were taken. After access cavity was prepared, teeth were placed in 5.25% sodium hypochlorite solution for 2 hours to dissolve the organic tissue of the root surface and from the root canal system. After bench dried and all the teeth were embedded in a self-curing resin. Each block was sectioned using a microtome (Accutom-50, Struers, Denmark) at interval of 1 mm. The sectioned surface photograph was taken using a digital camera (Coolpix 995, Nikon, Japan) connected to the microscope. 197 images were evaluated for canal configurations and the minimal thickness of dentinal wall between canal and external wall using' Root Thickness Gauge Program' designed with Visual Basic.
The results were as follows:
1. At the orifice level of all teeth, the most frequent observed configuration was Melton's Type C I (73%), however the patterns were changed to type C II and C III when the sections were observed at the apical third. On the other hand, the type C III was observed at the orifice level of only 2 teeth but this type could be seen at apical region of the rest of the teeth.
2. The C-shaped canal showed continuous and semi-colon shape at the orifice level, but at the apical portion of the canal there was high possibility of having 2 or 3 canals.
3. Lingual wall was thinner than buccal wall at coronal, middle, apical thirds of root but there was no statistical differences.
- 935 View
- 1 Download

- Effects of occlusal load on the cervical stress distribution: A three-dimensional finite element study
- Hyeong-Mo Lee, Bock Hur, Hyeon-Cheol Kim, Sung-Gwan Woo, Kwang-Hoon Kim, Kwon Son, Jeong-Kil Park
- J Korean Acad Conserv Dent 2006;31(6):427-436. Published online November 30, 2006
- DOI: https://doi.org/10.5395/JKACD.2006.31.6.427
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub The objective of this study was to investigate the effects of various occlusal loads on the stress distribution of the buccal cervical region of a normal maxillary second premolar, using a three dimensional finite element analysis (3D FEA).
After 3D FE modeling of maxillary second premolar, a static load of 500N of three load cases was applied. Stress analysis was performed using ANSYS (Swanson Analysis Systems, Inc., Houston, USA). The maximum principal stresses and minimum principal stresses were sampled at thirteen nodal points in the buccal cervical enamel for each four horizontal planes, 1.0 mm above CEJ, 0.5 mm above CEJ, CEJ, 0.5 mm under CEJ.
The results were as follows
1. The peak stress was seen at the cervical enamel surface of the mesiobuccal line angle area, asymmetrically.
2. The values of compressive stresses were within the range of the failure stress of enamel. But the values of tensile stresses exceeded the range of the failure stress of enamel.
3. The tensile stresses from the perpendicular load at the buccal incline of palatal cusp may be shown to be the primary etiological factors of the NCCLs.
-
Citations
Citations to this article as recorded by- Biomechanical and Occlusal Factors Influencing the Longevity of Single-Unit Restorations: A Comprehensive Review
Wedad S Alaida, Safa A Gadi, Rokia E Al-Ghannam, Moayad F Alamri, Feras I Mirdad, Ruba M Argaibeh, Bushra A Alqahtani, Abdulrahman M Alqahtani, Abdulelah A Al Jaban, Turki M Alkuraydimi, Abdulrahman S Alamari
Cureus.2025;[Epub] CrossRef - Effect of restoration type on the stress distribution of endodontically treated maxillary premolars; Three-dimensional finite element study
Heun-Sook Jung, Hyeon-Cheol Kim, Bock Hur, Kwang-Hoon Kim, Kwon Son, Jeong-Kil Park
Journal of Korean Academy of Conservative Dentistry.2009; 34(1): 8. CrossRef - Stress distribution of endodontically treated maxillary second premolars restored with different methods: Three-dimensional finite element analysis
Dong-Yeol Lim, Hyeon-Cheol Kim, Bock Hur, Kwang-Hoon Kim, Kwon Son, Jeong-Kil Park
Journal of Korean Academy of Conservative Dentistry.2009; 34(1): 69. CrossRef
- Biomechanical and Occlusal Factors Influencing the Longevity of Single-Unit Restorations: A Comprehensive Review
- 1,764 View
- 4 Download
- 3 Crossref

- The canal system in the mesiobuccal root of the maxillary first molar
- Dong-Hyun Cho, Ho-Young Choi, Sang-Hyuk Park, Gi-Woon Choi
- J Korean Acad Conserv Dent 2003;28(3):232-240. Published online May 31, 2003
- DOI: https://doi.org/10.5395/JKACD.2003.28.3.232
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub This study is to investigate the canal system in the mesiobuccal root of the maxillry first molar.
61 maxillary first molars were randomly selected. Serial transverse sections were made perpendicular to the long axis of the mesiobuccal root. Each section was placed in 3% sodium hypochlorite for 24 hours and rinsed in water and dried. The resected surface was stained with 2% methylene blue dye and examined with stereomicroscope.
Canal configuration analysis showed that 36.1% of the specimen classified as type I, 16.4% as type II, 37.7% as type III and 9.8% as type IV.
Type II canal was merged in one canal within 1 to 4mm of the apex. 40% of type II canal converged at 2mm of the apex.
Type IV canal was divided into two canal within 2 to 4mm of the apex. 66.6% of type IV canal branched off at 2mm of the apex.
None of the sections had more than two main root canal.
48.4% of the sections in 3mm with two canals contained an isthmusand more than 70% with two canals has isthmus at 4 to 5mm sections.
63.9% of the mesiobuccal root of maxillary first molar had two canaland 76.5% of sections with two canals in 5 MM had an isthmus. Because of this complexity the clinician should always search for extra canal carefullyand root canal system, including an isthmus, should be cleaned and shaped completelyand obturated three dimensionally for successful endodontic treatment.
- 1,072 View
- 4 Download


 KACD
KACD

 First
First Prev
Prev


