Articles
- Page Path
- HOME > Restor Dent Endod > Volume 41(1); 2016 > Article
- Research Article Analysis of C-shaped root canal configuration in maxillary molars in a Korean population using cone-beam computed tomography
- Hyoung-Hoon Jo, Jeong-Bum Min, Ho-Keel Hwang
-
2016;41(1):-62.
DOI: https://doi.org/10.5395/rde.2016.41.1.55
Published online: January 29, 2016
Department of Conservative Dentistry, School of Dentistry, Chosun University, Gwangju, Korea.
- Correspondence to Ho-Keel Hwang, DDS, PhD. Professor, Department of Conservative Dentistry, School of Dentistry, Chosun University, 309 Pilmun-daero, Dong-gu, Gwangju, Korea 61452. TEL, +82-62-220-3840; FAX, +82-62-223-9064; rootcanal@hanmail.net
©Copyrights 2016. The Korean Academy of Conservative Dentistry.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 1,915 Views
- 14 Download
- 26 Crossref
Abstract
-
Objectives The purpose of this study was to investigate the incidence of root fusion and C-shaped root canals in maxillary molars, and to classify the types of C-shaped canal by analyzing cone-beam computed tomography (CBCT) in a Korean population.
-
Materials and Methods Digitized CBCT images from 911 subjects were obtained in Chosun University Dental Hospital between February 2010 and July 2012 for orthodontic treatment. Among them, a total of selected 3,553 data of maxillary molars were analyzed retrospectively. Tomography sections in the axial, coronal, and sagittal planes were displayed by PiViewstar and Rapidia MPR software (Infinitt Co.). The incidence and types of root fusion and C-shaped root canals were evaluated and the incidence between the first and the second molar was compared using Chi-square test.
-
Results Root fusion was present in 3.2% of the first molars and 19.5% of the second molars, and fusion of mesiobuccal and palatal root was dominant. C-shaped root canals were present in 0.8% of the first molars and 2.7% of the second molars. The frequency of root fusion and C-shaped canal was significantly higher in the second molar than the first molar (p < 0.001).
-
Conclusions In a Korean population, maxillary molars showed total 11.3% of root fusion and 1.8% of C-shaped root canals. Furthermore, root fusion and C-shaped root canals were seen more frequently in the maxillary second molars.
Introduction
Materials and Methods
Results
Discussion
Conclusions
- 1. Cooke HG 3rd, Cox FL. C-shaped canal configurations in mandibular molars. J Am Dent Assoc 1979;99:836-839.ArticlePubMed
- 2. Gulabivala K, Opasanon A, Ng YL, Alavi A. Root and canal morphology of Thai mandibular molars. Int Endod J 2002;35:56-62.ArticlePubMed
- 3. Bolger WL, Schindler WG. A mandibular first molar with a C-shaped root configuration. J Endod 1988;14:515-519.ArticlePubMed
- 4. Baisden MK, Kulild JC, Weller RN. Root canal configuration of the mandibular first premolar. J Endod 1992;18:505-508.ArticlePubMed
- 5. Newton CW, McDonald S. A C-shaped canal configuration in a maxillary first molar. J Endod 1984;10:397-399.ArticlePubMed
- 6. Melton DC, Krell KV, Fuller MW. Anatomical and histological features of C-shaped canals in mandibular second molars. J Endod 1991;17:384-388.ArticlePubMed
- 7. Fan B, Cheung GS, Fan M, Gutmann JL, Bian Z. C-shaped canal system in mandibular second molars: part I - anatomical features. J Endod 2004;30:899-903.ArticlePubMed
- 8. Jerome CE. C-shaped root canal systems: diagnosis, treatment, and restoration. Gen Dent 1994;42:424-427.PubMed
- 9. Trope M, Elfenbein L, Tronstad L. Mandibular premolars with more than one root canal in different race groups. J Endod 1986;12:343-345.ArticlePubMed
- 10. Weine FS, Hayami S, Hata G, Toda T. Canal configuration of the mesiobuccal root of the maxillary first molar of a Japanese sub-population. Int Endod J 1999;32:79-87.ArticlePubMed
- 11. Seo MS, Park DS. C-shaped root canals of mandibular second molars in a Korean population: clinical observation and in vitro analysis. Int Endod J 2004;37:139-144.ArticlePubMed
- 12. Yang ZP, Yang SF, Lin YC, Shay JC, Chi CY. C-shaped root canals in mandibular second molars in a Chinese population. Endod Dent Traumatol 1988;4:160-163.ArticlePubMed
- 13. Ross IF, Evanchik PA. Root fusion in molars: incidence and sex linkage. J Periodontol 1981;52:663-667.ArticlePubMed
- 14. Zheng QH, Wang Y, Zhou XD, Wang Q, Zheng GN, Huang DM. A cone-beam computed tomography study of maxillary first permanent molar root and canal morphology in a Chinese population. J Endod 2010;36:1480-1484.ArticlePubMed
- 15. Ng YL, Aung TH, Alavi A, Gulabivala K. Root and canal morphology of Burmese maxillary molars. Int Endod J 2001;34:620-630.ArticlePubMedPDF
- 16. Alavi AM, Opasanon A, Ng YL, Gulabivala K. Root and canal morphology of Thai maxillary molars. Int Endod J 2002;35:478-485.ArticlePubMed
- 17. Neelakantan P, Subbarao C, Ahuja R, Subbarao CV, Gutmann JL. Cone-beam computed tomography study of root and canal morphology of maxillary first and second molars in an Indian population. J Endod 2010;36:1622-1627.ArticlePubMed
- 18. Zhang R, Yang H, Yu X, Wang H, Hu T, Dummer PM. Use of CBCT to identify the morphology of maxillary permanent molar teeth in a Chinese subpopulation. Int Endod J 2011;44:162-169.ArticlePubMed
- 19. Kim Y, Lee SJ, Woo J. Morphology of maxillary first and second molars analyzed by cone-beam computed tomography in a korean population: variations in the number of roots and canals and the incidence of fusion. J Endod 2012;38:1063-1068.ArticlePubMed
- 20. Yang ZP, Yang SF, Lee G. The root and root canal anatomy of maxillary molars in a Chinese population. Endod Dent Traumatol 1988;4:215-218.ArticlePubMed
- 21. al Shalabi RM, Omer OE, Glennon J, Jennings M, Claffey NM. Root canal anatomy of maxillary first and second permanent molars. Int Endod J 2000;33:405-414.ArticlePubMed
- 22. Pécora JD, Woelfel JB, Sousa Neto MD. Morphologic study of the maxillary molars. 1. External anatomy. Braz Dent J 1991;2:45-50.PubMed
- 23. De Moor RJ. C-shaped root canal configuration in maxillary first molars. Int Endod J 2002;35:200-208.ArticlePubMed
- 24. Dankner E, Friedman S, Stabholz A. Bilateral C shape configuration in maxillary first molars. J Endod 1990;16:601-603.ArticlePubMed
- 25. Yilmaz Z, Tuncel B, Serper A, Calt S. C-shaped root canal in a maxillary first molar: a case report. Int Endod J 2006;39:162-166.ArticlePubMed
- 26. Singla M, Aggarwal V. C-Shaped palatal canal in maxillary second molar mimicking two palatal canals diagnosed with the aid of spiral computerized tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010;109:e92-e95.Article
- 27. Kottoor J, Velmurugan N, Ballal S, Roy A. Four-rooted maxillary first molar having C-shaped palatal root canal morphology evaluated using cone-beam computerized tomography: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2011;111:e41-e45.ArticlePubMed
- 28. Manning SA. Root canal anatomy of mandibular second molars. Part II. C-shaped canals. Int Endod J 1990;23:40-45.PubMed
- 29. Haddad GY, Nehme WB, Ounsi HF. Diagnosis, classification, and frequency of C-shaped canals in mandibular second molars in the Lebanese population. J Endod 1999;25:268-271.ArticlePubMed
- 30. Tachibana H, Matsumoto K. Applicability of X-ray computerized tomography in endodontics. Endod Dent Traumatol 1990;6:16-20.ArticlePubMed
REFERENCES
Classification of root fusion in maxillary first and second molars
Type and number of root fusion in maxillary first and second molars
' – ' means fusion of roots (ie, "MB-P" means mesiobuccal root fused with palatal root).
Values within parentheses are percentages of the total number of teeth in each column.
MB, mesiobuccal root; DB, distobuccal root; B, buccal root; P, palatal root; MP, mesiopalatal root; DP, distopalatal root.
*The difference between maxillary first molar and second molar was statistically significant (p < 0.05).
Classification of C-shaped root canal in maxillary first and second molars
Type and number of C-shaped root canal in maxillary first and second molars
' - 'means fusion of root canals that make C-shape.
Values within parentheses are percentages of the total number of teeth in each column.
MB, mesiobuccal root canal; DB, distobuccal root canal; P, palatal root canal; MP, mesiopalatal root canal; DP, distopalatal root canal.
*The difference between maxillary first molar and second molar was statistically significant (p < 0.05).
Tables & Figures
REFERENCES
Citations

- Prevalence of C‐Shaped Canals in Maxillary Molars in an Iranian Population: A Cone‐Beam Computed Tomography Analysis
Amin Salem Milani, Shahin Namvar Asl Amirkhizi, Tahmineh Razi, Ahmad Nouroloyouni, Pouya Sabanik, Nikhat Kaura
International Journal of Clinical Practice.2026;[Epub] CrossRef - Prevalence of c-shaped canal morphology in premolar and molar teeth assessed by cone-beam computed tomography: systematic review and meta-analysis
Faezeh Yousefi, Younes Mohammadi, Elham Shokri
BMC Oral Health.2025;[Epub] CrossRef - A Cone‐Beam Computed Tomography Evaluation of C‐Shaped Canal Configuration in Maxillary Molars Among an Iranian Population
Nafiseh Nikkerdar, Mohammad Moslehi, Amin Golshah, Mario Dioguardi
International Journal of Dentistry.2024;[Epub] CrossRef - Endodontic treatment of a C‐shaped mandibular second molar with narrow dentinal thickness: A case report
Mina Mehrjouei, Hamid Jafarzadeh, Pourya Esmaeelpour, Maryam Khorasanchi
Clinical Case Reports.2024;[Epub] CrossRef - Evaluation of 2- and 3-dimensional anatomic parameters of C-shaped root canals with cone beam computed tomography, microcomputed tomography, and nanocomputed tomography
Miguel Angel Ventura Molina, Giovane Oliveira Silva, Amanda Pelegrin Candemil, Rafael Verardino de Camargo, Ruben Pauwels, Reinhilde Jacobs, Manoel Damião Sousa-Neto, Jardel Francisco Mazzi-Chaves
Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology.2023; 136(6): 759. CrossRef - Cone-Beam Computed Tomography (CBCT) Analysis of an Unusual Configuration of the Upper First Molar With a C-shaped Canal With Apically Fused Roots: A Case Report
Kapil D Wahane, Anand V Bansod, Sudha mattigatti, Rushikesh Mahaparale, Yuvraj B Rote, Mayur B Wanjari
Cureus.2023;[Epub] CrossRef - Assessment of C-Shaped Canal Morphology in Mandibular and Maxillary Second Molars in an Iraqi Subpopulation Using Cone-Beam Computed Tomography
Kazhan Abdalrahman, Ranjdar Talabani, Sara Kazzaz, Dlsoz Babarasul, Berndt Koslowski
Scanning.2022; 2022: 1. CrossRef - Root and canal-specific features of maxillary first molars with fused roots
Katarina Beljic-Ivanovic, Branislav Karadzic
Vojnosanitetski pregled.2022; 79(11): 1092. CrossRef - Diagnosis and treatment of maxillary molar with abnormality
Kkot-Byeol Bae, Bin-Na Lee, Hoon-Sang Chang, In-Nam Hwang, Won-Mann Oh, Yun-Chan Hwang
Oral Biology Research.2022; 46(4): 195. CrossRef - Endodontic treatment of the maxillary first molar with palatal canal variations: A case report and review of literature
Kai Chen, Xing Ran, Yan Wang
World Journal of Clinical Cases.2022; 10(32): 12036. CrossRef - Evaluation of C-shaped canals in maxillary molars in a Chinese population using CBCT
Yuyan Qian, Yamei Li, Jukun Song, Ping Zhang, Zhu Chen
BMC Medical Imaging.2022;[Epub] CrossRef - Comprehensive evaluation of root and root canal morphology of mandibular second molars in a Saudi subpopulation evaluated by cone-beam computed tomography
Moazzy I. Almansour, Saad M. Al‑Zubaidi, Abdulmjeed S. Enizy, Ahmed A. Madfa
BMC Oral Health.2022;[Epub] CrossRef - Evaluation of C-shaped canal configuration in maxillary molars: A retrospective cone-beam computed tomography study
Emre KÖSE, Rüya AK
Clinical and Experimental Health Sciences.2021; 11(3): 444. CrossRef - Maxillary First Molars with Two Palatal Root Canals
Kun-Hwa Sung, Ho-Keel Hwang, Hyoung-Hoon Jo, Konstantinos Michalakis
Case Reports in Dentistry.2021;[Epub] CrossRef - Preferred Reporting Items for Epidemiologic Cross-sectional Studies on Root and Root Canal Anatomy Using Cone-beam Computed Tomographic Technology: A Systematized Assessment
Jorge N.R. Martins, Anil Kishen, Duarte Marques, Emmanuel João Nogueira Leal Silva, João Caramês, António Mata, Marco A. Versiani
Journal of Endodontics.2020; 46(7): 915. CrossRef - Evaluation of root and root canal morphology of elderly Korean patients maxillary molars using cone-beam computed tomography
Tae-Yong Lee, Mi-Yeon Kim, Sun-Ho Kim, Jeong-Hee Kim
The Journal of Korean Academy of Prosthodontics.2020; 58(2): 95. CrossRef - Second mesiobuccal root canal in maxillary molars—A systematic review and meta-analysis of prevalence studies using cone beam computed tomography
Jorge N.R. Martins, Duarte Marques, Emmanuel João Nogueira Leal Silva, João Caramês, António Mata, Marco A. Versiani
Archives of Oral Biology.2020; 113: 104589. CrossRef - Prevalência estimada de canais “C- Shaped”: Uma revisão sistemática e meta-análise
Natália Pereira da Silva Falcão, Sandro Junio de Oliveira Tavares, Ludmila Silva Guimarães, Katherine Azevedo Batistela Rodrigues Thuller, Leonardo dos Santos Antunes, Estefano Borgo Sarmento, Fellipe Navarro Azevedo de Azevedo, Cinthya Cristina Gomes, Ca
Revista Científica Multidisciplinar Núcleo do Conhecimento.2020; : 91. CrossRef - Evaluation of the internal anatomy of paramolar tubercles using cone-beam computed tomography
G. Colakoglu, I. Kaya Buyukbayram, M. A. Elcin, M. Kazak, H. Sezer
Surgical and Radiologic Anatomy.2020; 42(1): 15. CrossRef - Analysis of Prevalence of Pyramidal Molars in Adolescent
Woojin Kwon, Hyung-Jun Choi, Jaeho Lee, Je Seon Song
THE JOURNAL OF THE KOREAN ACADEMY OF PEDTATRIC DENTISTRY.2020; 47(4): 389. CrossRef - Prevalence Studies on Root Canal Anatomy Using Cone-beam Computed Tomographic Imaging: A Systematic Review
Jorge N.R. Martins, Duarte Marques, Emmanuel João Nogueira Leal Silva, João Caramês, Marco A. Versiani
Journal of Endodontics.2019; 45(4): 372. CrossRef - Fused roots of maxillary molars: characterization and prevalence in a Latin American sub-population: a cone beam computed tomography study
Maytté Marcano-Caldera, Jose Luis Mejia-Cardona, María del Pilar Blanco-Uribe, Elena Carolina Chaverra-Mesa, Didier Rodríguez-Lezama, Jose Hernán Parra-Sánchez
Restorative Dentistry & Endodontics.2019;[Epub] CrossRef - An original micro‐CT study and meta‐analysis of the internal and external anatomy of maxillary molars—implications for endodontic treatment
Iwona M. Tomaszewska, Anna Jarzębska, Bendik Skinningsrud, Przemysław A. Pękala, Sebastian Wroński, Joe Iwanaga
Clinical Anatomy.2018; 31(6): 838. CrossRef - A Cone-beam Computed Tomographic Study of Root and Canal Morphology of Maxillary First and Second Permanent Molars in a Thai Population
Roserin Ratanajirasut, Anchana Panichuttra, Soontra Panmekiate
Journal of Endodontics.2018; 44(1): 56. CrossRef - Retrospective Assessment of Healing Outcome of Endodontic Treatment for Mandibular Molars with C-shaped Root Canal
Kishore Kumar Majety, Basanta Kumar Choudhury, Anika Bansal, Achla Sethi, Jaina Panjabi
The Journal of Contemporary Dental Practice.2017; 18(7): 591. CrossRef - The morphology of maxillary first and second molars analyzed by cone-beam computed tomography in a polish population
Katarzyna Olczak, Halina Pawlicka
BMC Medical Imaging.2017;[Epub] CrossRef
- Related articles
-
- Determination of optimal horizontal beam angulations for canal separation in mandibular molars using cone-beam computed tomography: a retrospective image-based analysis
- Dentin thickness of C-shaped root canal walls in mandibular premolars based on cone-beam computed tomography: a retrospective cross-sectional study
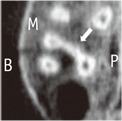
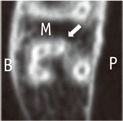
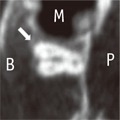
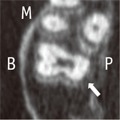
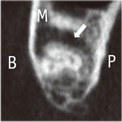
Classification of root fusion in maxillary first and second molars
| Type of root fusion | CBCT Image representing the type | Description | |
|---|---|---|---|
| Fusion of 2 roots | MB-P | Mesiobuccal root fused with palatal root | |
| DB-P | Distobuccal root fused with palatal root | ||
| MB-DB | Mesiobuccal root fused with distobuccal root | ||
| Fusion of 3 roots | MB-DB-P | Mesiobuccal root fused with distobuccal root and palatal root | |
| DB-MB-P | Distobuccal root fused with mesiobuccal root and palatal root | ||
| MB-P-DB (V shape) | Mesiobuccal root fused with palatal root and distobuccal root | ||
| All root (Y or cone shape) | All 3 roots are fused to apical direction without any sequence | ||
| Other types of root fusion | B-P (teeth with 2 root) | Single buccal root fused with palatal root | |
| MB-MP and DB-DP | Mesiobuccal root fused with mesiopalatal root and distobuccal root fused with distopalatal root | ||
In the CBCT image, the arrows indicate the fusion of examined teeth, the capital letter indicate each aspect.
CBCT, cone-beam computed tomography; M, Mesial; B, Buccal; P, Palatal.
Type and number of root fusion in maxillary first and second molars
| Type of root fusion | Total (n = 3,553) | Maxillary first molar (n = 1,786) | Maxillary second molar (n = 1,767) | ||
|---|---|---|---|---|---|
| Fusion of 2 roots | MB-P | 217 (6.1) | 129 (3.6) | 6 (0.3) | 123 (7.0) |
| DB-P | 16 (0.4) | 11 (0.6) | 5 (0.3) | ||
| MB-DB | 72 (2.0) | 31 (1.7) | 41 (2.3) | ||
| Fusion of 3 roots | MB-DB-P | 124 (3.4) | 7 (0.2) | 6 (0.3) | 1 (0.1) |
| DB-MB-P | 40 (1.1) | 0 (0.0) | 40 (2.3) | ||
| MB-P-DB (V shape) | 15 (0.4) | 2 (0.1) | 13 (0.7) | ||
| All root (Y or cone shape) | 62 (1.7) | 0 (0.0) | 62 (3.5) | ||
| Other types of root fusion | B-P (teeth with 2 root) | 61 (1.7) | 60 (1.68) | 1 (0.1) | 59 (3.3) |
| MB-MP and DB-DP | 1 (0.03) | 0 (0.0) | 1 (0.1) | ||
| Total | 402 (11.3) | 57 (3.2)* | 345 (19.5)* | ||
' – ' means fusion of roots (ie, "MB-P" means mesiobuccal root fused with palatal root).
Values within parentheses are percentages of the total number of teeth in each column.
MB, mesiobuccal root; DB, distobuccal root; B, buccal root; P, palatal root; MP, mesiopalatal root; DP, distopalatal root.
*The difference between maxillary first molar and second molar was statistically significant (p < 0.05).
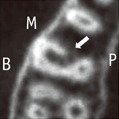
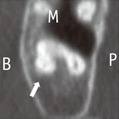
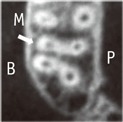
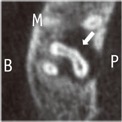
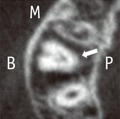
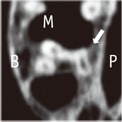
Classification of C-shaped root canal in maxillary first and second molars
| Type of C-shaped root canal | CBCT Image representing the type | Description | |
|---|---|---|---|
| Type I Fusion of 2 root canals | Subtype A MB-P | mesiobuccal root canal fused with palatal root canal (fusion of 2 roots) | |
| mesiobuccal root canal fused with palatal root canal (fusion of 3 roots) | |||
| Subtype B DB-P | distobuccal root canal fused with palatal root cana | ||
| Subtype C MB-DB | mesiobuccal root canal fused with distobuccal root canal (fusion of 2 roots) | ||
| mesiobuccal root canal fused with distobuccal root canal (fusion of 3 roots) | |||
| Type II Fusion of 3 root canals | Subtype A DB-MB-P | distobuccal root canal fused with mesiobuccal root canal and palatal root canal | |
| Subtype B MB-P-DB (V shape) | mesiobuccal root canal fused with palatal root canal and distobuccal root canal | ||
| Type III Other type of root canal fusion | MP-DP (tooth with 4 root canals) | mesiopalatal root canal fused with distopalatal root canal | |
In the CBCT image, the arrows indicate the C-shaped root canal of examined teeth, the capital letter indicate each aspect.
M, Mesial; B, Buccal; P, Palatal.
Type and number of C-shaped root canal in maxillary first and second molars
| Type of C-shaped root canal | Total (n = 3,553) | Maxillary first molar (n = 1,786) | Maxillary second molar (n = 1,767) | ||
|---|---|---|---|---|---|
| Type I Fusion of 2 roots | Subtype A: MB-P | 57 (1.6) | 11 (0.3) | 0 (0.0) | 11 (0.6) |
| Subtype B: DB-P | 2 (0.06) | 0 (0.0) | 2 (0.1) | ||
| Subtype C: MB-DB | 44 (1.2) | 15 (0.8) | 29 (1.6) | ||
| Type II Fusion of 3 roots | Subtype A: DB-MB-P | 5 (0.14) | 3 (0.08) | 0 (0.0) | 3 (0.2) |
| Subtype B: MB-P-DB (V shape) | 2 (0.06) | 0 (0.0) | 2 (0.1) | ||
| Type III Other type of root canal fusion | MP-DP (teeth with 4 root canals) | 1 (0.03) | 0 (0.0) | 1 (0.1) | |
| Total | 63 (1.8) | 15 (0.8)* | 48 (2.7)* | ||
' - 'means fusion of root canals that make C-shape.
Values within parentheses are percentages of the total number of teeth in each column.
MB, mesiobuccal root canal; DB, distobuccal root canal; P, palatal root canal; MP, mesiopalatal root canal; DP, distopalatal root canal.
*The difference between maxillary first molar and second molar was statistically significant (p < 0.05).
In the CBCT image, the arrows indicate the fusion of examined teeth, the capital letter indicate each aspect. CBCT, cone-beam computed tomography; M, Mesial; B, Buccal; P, Palatal.
' – ' means fusion of roots (ie, "MB-P" means mesiobuccal root fused with palatal root). Values within parentheses are percentages of the total number of teeth in each column. MB, mesiobuccal root; DB, distobuccal root; B, buccal root; P, palatal root; MP, mesiopalatal root; DP, distopalatal root. *The difference between maxillary first molar and second molar was statistically significant (
In the CBCT image, the arrows indicate the C-shaped root canal of examined teeth, the capital letter indicate each aspect. M, Mesial; B, Buccal; P, Palatal.
' - 'means fusion of root canals that make C-shape. Values within parentheses are percentages of the total number of teeth in each column. MB, mesiobuccal root canal; DB, distobuccal root canal; P, palatal root canal; MP, mesiopalatal root canal; DP, distopalatal root canal. *The difference between maxillary first molar and second molar was statistically significant (

 KACD
KACD






 ePub Link
ePub Link Cite
Cite

