Articles
- Page Path
- HOME > Restor Dent Endod > Volume 45(4); 2020 > Article
- Research Article A cone-beam computed tomography study of the prevalence and location of the second mesiobuccal root canal in maxillary molars
-
Seong-Ju Lee1
 , Eun-Hye Lee2
, Eun-Hye Lee2 , Se-Hee Park1
, Se-Hee Park1 , Kyung-Mo Cho1
, Kyung-Mo Cho1 , Jin-Woo Kim1
, Jin-Woo Kim1
-
Restor Dent Endod 2020;45(4):e46.
DOI: https://doi.org/10.5395/rde.2020.45.e46
Published online: September 3, 2020
1Department of Conservative Dentistry, Gangneung-Wonju National University, Gangneung, Korea.
2Department of Conservative Dentistry, Hanyang University Seoul Hospital, Seoul, Korea.
- Correspondence to Jin-Woo Kim, PhD. Professor, Department of Conservative Dentistry, Gangneung-Wonju National University, 7 Jukheon-gil, Gangneung 25457, Korea. mendo7@gwnu.ac.kr
Copyright © 2020. The Korean Academy of Conservative Dentistry
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 3,785 Views
- 44 Download
- 11 Crossref
Abstract
-
Objectives This study aimed to investigate the incidence and location of the second mesiobuccal root (MB2) canal in maxillary molars with the aid of various measuring points and lines using cone-beam computed tomography (CT).
-
Materials and Methods A total of 205 images of patients who underwent cone-beam CT examinations between 2011 and 2015 as part of their dental diagnosis and treatment were included. There were 76 images of the maxillary first molar and 135 images of the maxillary second molar. Canal orifices were detected at −1 mm from the top of the pulpal floor on cone-beam CT images. Image assessment was performed by 2 observers in reformatted image planes using software. Assessments included measurement of the distance between the MB1 and MB2 canals, and the angles between the lines connecting the MB1-MB2 and distobuccal (DB)-palatal (P) canals. The data were analyzed using the student's t-test.
-
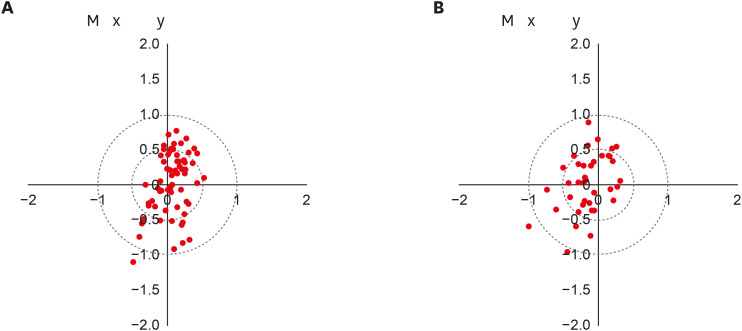
Results The prevalence of the MB2 canal was 86.8% in the first molar and 28.9% in the second molar. The angle between the lines connecting the MB1-MB2 and DB-P canals was 2.3° ± 5.7° in the first molar and −3.95° ± 7.73° in the second molar. The distance between the MB1 and MB2 canals was 2.1 ± 0.44 mm in the first molar and 1.98 ± 0.42 mm in the second molar.
-
Conclusions The angles between the lines connecting the MB1-MB2 and DB-P canals was almost parallel. These findings may aid in the prediction of the location of the MB2 canal orifice.
INTRODUCTION
MATERIALS AND METHODS
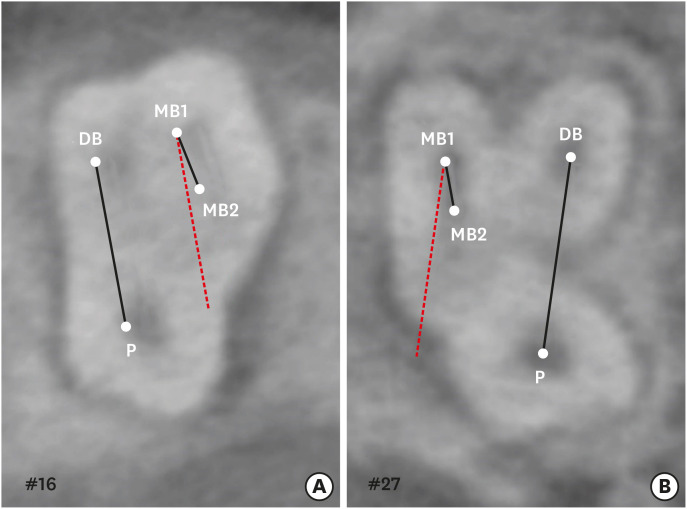
1. Angles of the lines connecting the MB1 and MB2 canals and those connecting the DB and P canals
Measurement of the angle between the line connecting the MB1-MB2 and that connecting the DB-P canals in a maxillary molar. (A) Positive angle; (B) Negative angle.
2. Distance between the MB1 and MB2 canal orifices
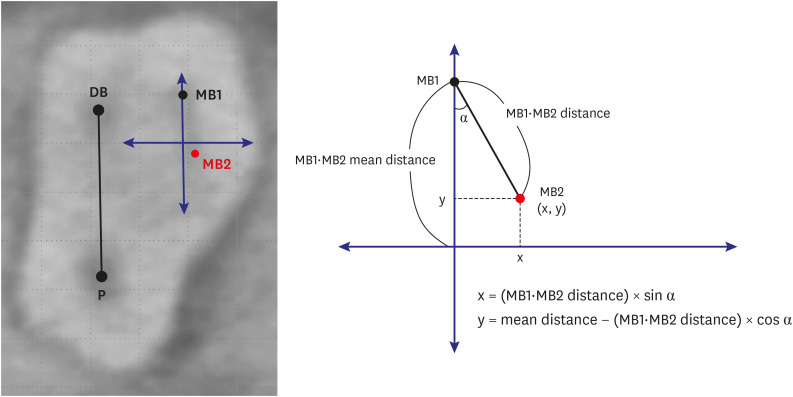
3. Distribution of MB2 canal locations
Measurement of the mean distance between the MB1 and MB2 canals in a maxillary molar. The hypothetical line that passes through the MB1 and is parallel to the line connecting the DB and P canals (mm) is the y-axis. The maximum value of the y-axis and the 0 point are assumed to be the mean distance between the MB1 and MB2 canals.
RESULTS
1. Angles between the lines connecting the MB1 and MB2 canals and those connecting the DB and P canals
Angles between the line connecting the MB1 and MB2 canals and the line connecting the DB and P canals, as well as the distances between the MB1 and MB2 canals, in the first and second maxillary molars
| Tooth type | ∠MB1·MB2 line–DB·P line (°) | Distances between the MB1-MB2 canals (mm) |
|---|---|---|
| First molar | 2.30 ± 5.70 | 2.10 ± 0.44 |
| Second molar | −3.95 ± 7.73 | 1.98 ± 0.42 |
| p value | 0.000* | 0.243 |
2. Distances between the MB1 and MB2 canal orifices
3. Distribution of the MB2 canal locations
Distribution of the second mesiobuccal root canal in the maxillary first and second molars. (A) Maxillary first molar; (B) Maxillary second molar.
DISCUSSION
CONCLUSIONS
ACKNOWLEDGEMENTS
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Kim JW.
Data curation: Lee SJ.
Formal analysis: Kim JW, Cho KM, Park SH.
Funding acquisition: Kim JW.
Investigation: Lee SJ.
Methodology: Kim JW.
Project administration: Park SH.
Resources: Lee SJ.
Software: Lee SJ, Lee EH.
Supervision: Kim JW.
Validation: Park SH.
Visualization: Lee SJ.
Writing - original draft: Lee SJ.
Writing - review & editing: Kim JW, Cho KM, Park SH.
- 1. Cantatore G, Berutti E, Castellucci A. Missed anatomy: frequency and clinical impact. Endod Topics 2006;15:3-31.Article
- 2. Vertucci FJ. Root canal anatomy of the human permanent teeth. Oral Surg Oral Med Oral Pathol 1984;58:589-599.ArticlePubMed
- 3. Huumonen S, Kvist T, Gröndahl K, Molander A. Diagnostic value of computed tomography in re-treatment of root fillings in maxillary molars. Int Endod J 2006;39:827-833.ArticlePubMed
- 4. Wolcott J, Ishley D, Kennedy W, Johnson S, Minnich S, Meyers J. A 5 yr clinical investigation of second mesiobuccal canals in endodontically treated and retreated maxillary molars. J Endod 2005;31:262-264.ArticlePubMed
- 5. Cotton TP, Geisler TM, Holden DT, Schwartz SA, Schindler WG. Endodontic applications of cone-beam volumetric tomography. J Endod 2007;33:1121-1132.ArticlePubMed
- 6. Michetti J, Maret D, Mallet JP, Diemer F. Validation of cone beam computed tomography as a tool to explore root canal anatomy. J Endod 2010;36:1187-1190.ArticlePubMed
- 7. Blattner TC, George N, Lee CC, Kumar V, Yelton CD. Efficacy of cone-beam computed tomography as a modality to accurately identify the presence of second mesiobuccal canals in maxillary first and second molars: a pilot study. J Endod 2010;36:867-870.ArticlePubMed
- 8. Vizzotto MB, Silveira PF, Arús NA, Montagner F, Gomes BP, da Silveira HE. CBCT for the assessment of second mesiobuccal (MB2) canals in maxillary molar teeth: effect of voxel size and presence of root filling. Int Endod J 2013;46:870-876.PubMed
- 9. Akbarzadeh N, Aminoshariae A, Khalighinejad N, Palomo JM, Syed A, Kulild JC, Sadeghi G, Mickel A. The association between the anatomic landmarks of the pulp chamber floor and the prevalence of middle mesial canals in mandibular first molars: an in vivo analysis. J Endod 2017;43:1797-1801.ArticlePubMed
- 10. Lofthag-Hansen S, Huumonen S, Gröndahl K, Gröndahl HG. Limited cone-beam CT and intraoral radiography for the diagnosis of periapical pathology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;103:114-119.ArticlePubMed
- 11. Matherne RP, Angelopoulos C, Kulild JC, Tira D. Use of cone-beam computed tomography to identify root canal systems in vitro . J Endod 2008;34:87-89.ArticlePubMed
- 12. Jang JH, Kim JW, Cho KM, Kim SY, Park SH. A study on Radix Entomolaris about prevalence and correlation of canal orifices location according to number of roots in mandibular first molars. J Korean Dent Assoc 2018;56:695-706.ArticlePDF
- 13. Deutsch AS, Musikant BL, Gu S, Isidro M. Morphological measurements of anatomic landmarks in pulp chambers of human maxillary furcated bicuspids. J Endod 2005;31:570-573.ArticlePubMed
- 14. Degerness RA, Bowles WR. Dimension, anatomy and morphology of the mesiobuccal root canal system in maxillary molars. J Endod 2010;36:985-989.ArticlePubMed
- 15. Martins JN, Alkhawas MA, Altaki Z, Bellardini G, Berti L, Boveda C, Chaniotis A, Flynn D, Gonzalez JA, Kottoor J, Marques MS, Monroe A, Ounsi HF, Parashos P, Plotino G, Ragnarsson MF, Aguilar RR, Santiago F, Seedat HC, Vargas W, von Zuben M, Zhang Y, Gu Y, Ginjeira A. Worldwide analyses of maxillary first molar second mesiobuccal prevalence: a multicenter cone-beam computed tomographic study. J Endod 2018;44:1641-1649.e1.ArticlePubMed
- 16. Lee YS. Prevalence and location of the second mesiobuccal canal in maxillary first molars in a Korean population. Daegu: Kyungpook National University; 2018.
- 17. Betancourt P, Navarro P, Cantín M, Fuentes R. Cone-beam computed tomography study of prevalence and location of MB2 canal in the mesiobuccal root of the maxillary second molar. Int J Clin Exp Med 2015;8:9128-9134.PubMedPMC
- 18. Lee JH, Kim KD, Lee JK, Park W, Jeong JS, Lee Y, Gu Y, Chang SW, Son WJ, Lee WC, Baek SH, Bae KS, Kum KY. Mesiobuccal root canal anatomy of Korean maxillary first and second molars by cone-beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2011;111:785-791.ArticlePubMed
- 19. Bauman R, Scarfe W, Clark S, Morelli J, Scheetz J, Farman A. Ex vivo detection of mesiobuccal canals in maxillary molars using CBCT at four different isotropic voxel dimensions. Int Endod J 2011;44:752-758.ArticlePubMed
- 20. Kim Y, Lee SJ, Woo J. Morphology of maxillary first and second molars analyzed by cone-beam computed tomography in a Korean population: variations in the number of roots and canals and the incidence of fusion. J Endod 2012;38:1063-1068.ArticlePubMed
- 21. Zhang R, Yang H, Yu X, Wang H, Hu T, Dummer PM. Use of CBCT to identify the morphology of maxillary permanent molar teeth in a Chinese subpopulation. Int Endod J 2011;44:162-169.ArticlePubMed
- 22. Kulild JC, Peters DD. Incidence and configuration of canal systems in the mesiobuccal root of maxillary first and second molars. J Endod 1990;16:311-317.ArticlePubMed
- 23. Betancourt P, Navarro P, Muñoz G, Fuentes R. Prevalence and location of the secondary mesiobuccal canal in 1,100 maxillary molars using cone beam computed tomography. BMC Med Imaging 2016;16:66.ArticlePubMedPMCPDF
- 24. Tuncer AK, Haznedaroglu F, Sert S. The location and accessibility of the second mesiobuccal canal in maxillary first molar. Eur J Dent 2010;4:12-16.ArticlePubMedPMC
REFERENCES
Tables & Figures
REFERENCES
Citations

- Position of Second Mesiobuccal Canal Relative to Distobuccal and Palatal Canals of Maxillary Molars in an Iranian Population
Sina Mosadeghian, Azadeh Torkzadeh, Parisa Ranjbarian, Roya Asaadi
Journal of Research in Dental and Maxillofacial Sciences.2025; 10(1): 34. CrossRef - Machine Learning Models in the Detection of MB2 Canal Orifice in CBCT Images
Shishir Shetty, Meliz Yuvali, Ilker Ozsahin, Saad Al-Bayatti, Sangeetha Narasimhan, Mohammed Alsaegh, Hiba Al-Daghestani, Raghavendra Shetty, Renita Castelino, Leena R David, Dilber Uzun Ozsahin
International Dental Journal.2025; 75(3): 1640. CrossRef - EVALUATION OF THE PREVALENCE AND LOCATION OF SECOND MESIOBUCCAL CANALS IN 2100 UPPER FIRST AND SECOND MOLAR TEETH: A CONE BEAM COMPUTED TOMOGRAPHY STUDY
Bahar Kaplan, Özkan Adıgüzel, Ayşe Gül Öner Talmaç, Elif Meltem Aslan
İnönü Üniversitesi Sağlık Hizmetleri Meslek Yüksek Okulu Dergisi.2025; 13(3): 752. CrossRef - A novel method for the precise second mesiobuccal canal orifice location: A combined strategy for enhanced clinical practice
Yuhan Wang, Lingyun Li, Lu Zhang, Xiaoyan Wang
Journal of Dental Sciences.2025;[Epub] CrossRef - Study on the Geometric Location Method of the Danger Zone in the Mesial Roots of Mandibular First Molars
Jinjie Yan, Yuanling Peng, Jing Yang, Jie Liu, Linxian Wang, Tingyuan Zhao, Jian Zhang, Kehua Que
Journal of Endodontics.2025;[Epub] CrossRef - The Correlation between Intraorifice Distance and the Anatomical Characteristics of the Second Mesiobuccal Canal of Maxillary Molars: A CBCT Study
Isabella Perondi, Silvio Taschieri, Martino Baruffaldi, Roberto Fornara, Luca Francetti, Stefano Corbella, Deepa Gurunathan
International Journal of Dentistry.2024;[Epub] CrossRef - Endodontic management of type I maxillary first molar with two palatal roots using cone-beam computed tomography
Nuha Alghamdi
Dental Journal.2024; 57(1): 1. CrossRef - 3D geometric analysis of second mesiobuccal canal in permanent maxillary first molar tooth
Indrani Khadilkar, Divya Nangia, Amrita Chawla, Sidhartha Sharma, Vijay Kumar, Shalini Gupta, Ajay Logani
Australian Endodontic Journal.2023; 49(1): 140. CrossRef - Prevalence of mesiobuccal-2 canals in maxillary first and second molars among the Bruneian population—CBCT analysis
Hui Yi Onn, Malissa Siao Yun Abdullah Sikun, Hanif Abdul Rahman, Jagjit Singh Dhaliwal
BDJ Open.2022;[Epub] CrossRef - Location angle of second mesio-buccal canal in maxillary molars of an Indian population: an in vivo retrospective CBCT evaluation and proposal of a new classification
Kishor Vhorkate, Kulvinder Banga, Ajinkya M. Pawar, Shugufta Mir, Suraj Arora, Dian Agustin Wahjuningrum, Anuj Bhardwaj, Alexander Maniangat Luke
PeerJ.2022; 10: e14234. CrossRef - Maxillary molar root and canal morphology of Neolithic and modern Chinese
H.Y. Ren, K.Y. Kum, Y.S. Zhao, Y.J. Yoo, J.S. Jeong, Hiran Perinpanayagam, X.Y. Wang, G.J. Li, F. Wang, H. Fang, Y. Gu
Archives of Oral Biology.2021; 131: 105272. CrossRef
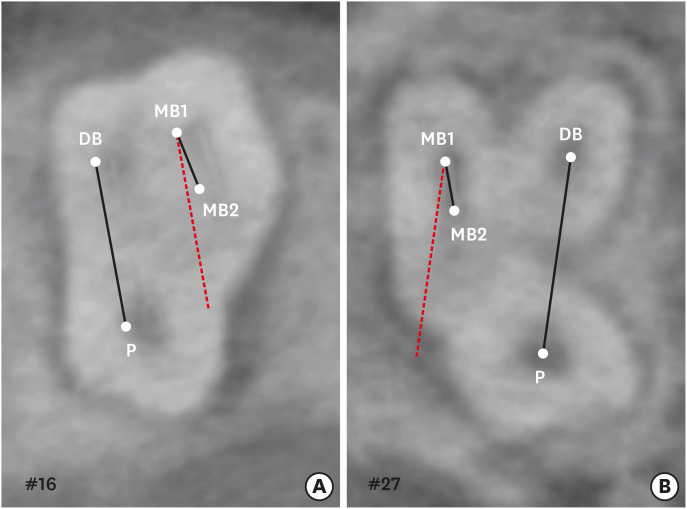
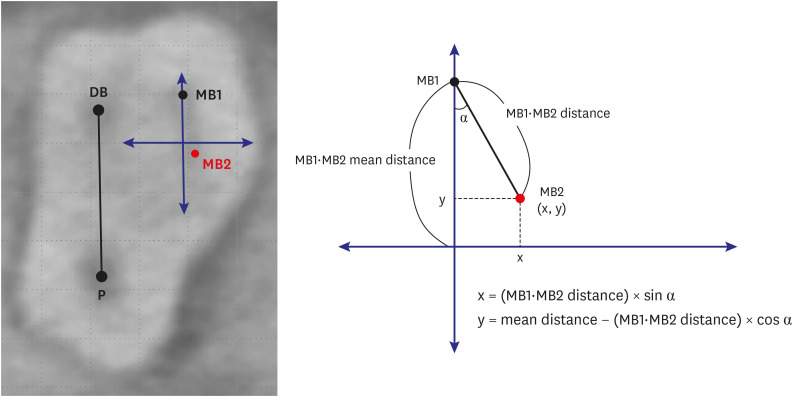
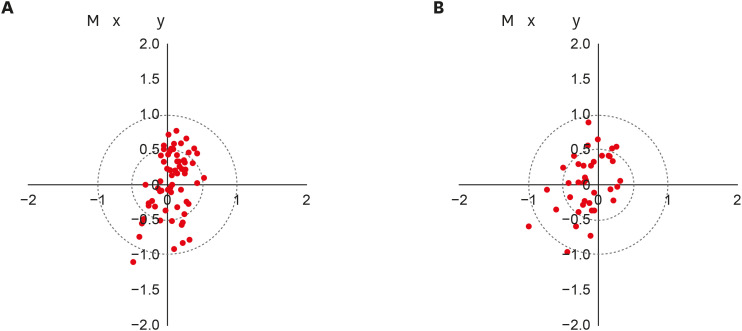
Figure 1
Figure 2
Figure 3
Angles between the line connecting the MB1 and MB2 canals and the line connecting the DB and P canals, as well as the distances between the MB1 and MB2 canals, in the first and second maxillary molars
| Tooth type | ∠MB1·MB2 line–DB·P line (°) | Distances between the MB1-MB2 canals (mm) |
|---|---|---|
| First molar | 2.30 ± 5.70 | 2.10 ± 0.44 |
| Second molar | −3.95 ± 7.73 | 1.98 ± 0.42 |
| p value | 0.000* | 0.243 |
Data are expressed as mean ± standard deviation.
MB1, first mesiobuccal root; MB2, second mesiobuccal root; DB, distobuccal; P, palatal.
Data are expressed as mean ± standard deviation.
MB1, first mesiobuccal root; MB2, second mesiobuccal root; DB, distobuccal; P, palatal.

 KACD
KACD
 ePub Link
ePub Link Cite
Cite

