Articles
- Page Path
- HOME > Restor Dent Endod > Volume 44(2); 2019 > Article
- Research Article Fused roots of maxillary molars: characterization and prevalence in a Latin American sub-population: a cone beam computed tomography study
-
Maytté Marcano-Caldera1
 , Jose Luis Mejia-Cardona1
, Jose Luis Mejia-Cardona1 , María del Pilar Blanco-Uribe1, Elena Carolina Chaverra-Mesa1, Didier Rodríguez-Lezama2
, María del Pilar Blanco-Uribe1, Elena Carolina Chaverra-Mesa1, Didier Rodríguez-Lezama2 , Jose Hernán Parra-Sánchez3
, Jose Hernán Parra-Sánchez3
-
Restor Dent Endod 2019;44(2):e16.
DOI: https://doi.org/10.5395/rde.2019.44.e16
Published online: April 22, 2019
1Postgraduate Endodontics Program. Autonomous University of Manizales, Manizales, Colombia.
2Oral Health Department. Autonomous University of Manizales, Manizales, Colombia.
3Math and Statistics Department. National University of Colombia, Campus Palogrande, Manizales, Colombia.
- Correspondence to Maytté Marcano-Caldera, DDS. Assistant Professor, Postgraduate Endodontics, Autonomous University of Manizales, Antigua Estación del Ferrocarril, Manizales-Caldas 170002, Colombia. mayttemc@gmail.com
Copyright © 2019. The Korean Academy of Conservative Dentistry
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 1,723 Views
- 14 Download
- 14 Crossref
Abstract
-
Objectives The upper molars generally have three roots; therefore, different combinations of fusion can occur, increasing the possibility of finding more complex root canal systems. The purpose of this study was to evaluate the prevalence and characterization of fused roots in first and second maxillary molars using cone-beam computed tomography (CBCT) in a Colombian population.
-
Materials and Methods A total of 1274 teeth were evaluated, of which 534 were maxillary first molars and 740 were maxillary second molars. Axial sections were made at the cervical, middle, and apical levels to determine the prevalence of root fusion and the types of fusion.
-
Results Overall, 43% of the molars (n = 551) presented some type of fused root. Root fusion was present in 23.4% of the maxillary first molars. The most frequent type of fused root was type 3 (distobuccal-palatal; DB-P) (58.9%). Root fusion was observed in 57.6% of the maxillary second molars, and the most prevalent type of fused root was type 6 (cone-shaped) (45.2%). Of the maxillary molars, 12.5% were classified as C-shaped.
-
Conclusion Within the limitations of this study, there was a high prevalence of fused roots in maxillary molars in the Colombian population, mainly in the maxillary second molars. In first molars, the most common type of fused root was type 3 (DB-P) and in second molars, the most common type was type 6 (cone-shaped). Additionally, molars with root fusion presented variation at different levels of the radicular portion, with implications for treatment quality.
INTRODUCTION
MATERIALS AND METHODS
- Cervical: 3 mm apical to the CEJ.
- Middle: half the distance between the CEJ and the radiographic apex.
- Apical: 2 mm from the radiographic apex.
- Type 1: Mesiobuccal (MB) root fused with distobuccal (DB) root.
- Type 2: MB root fused with palatal (P) root.
- Type 3: DB root fused with P root.
- Type 4: MB root fused with DB root and P root or P root with MB and DB roots (proximal groove).
- Type 5: P root fused with MB and DB roots (vestibular groove).
- Type 6: P, MB, and DB roots fused as a cone-shaped root.
RESULTS
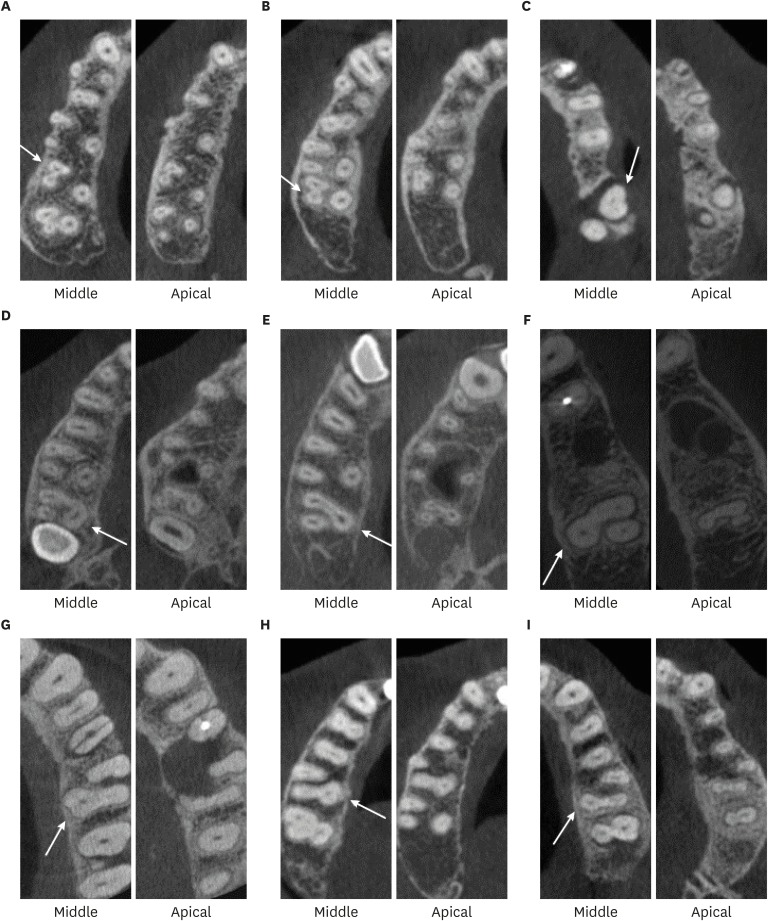
Maxillary first and second molars, fused root type 1, 2 and 3. (A-C) Variations of type 1 root fusion (MB-DB roots) (arrows); (D-F) Variations of type 2 root fusion (MB-P roots) (arrows); (G-I) Variations of type 3 root fusion (DB-P roots) (arrows).
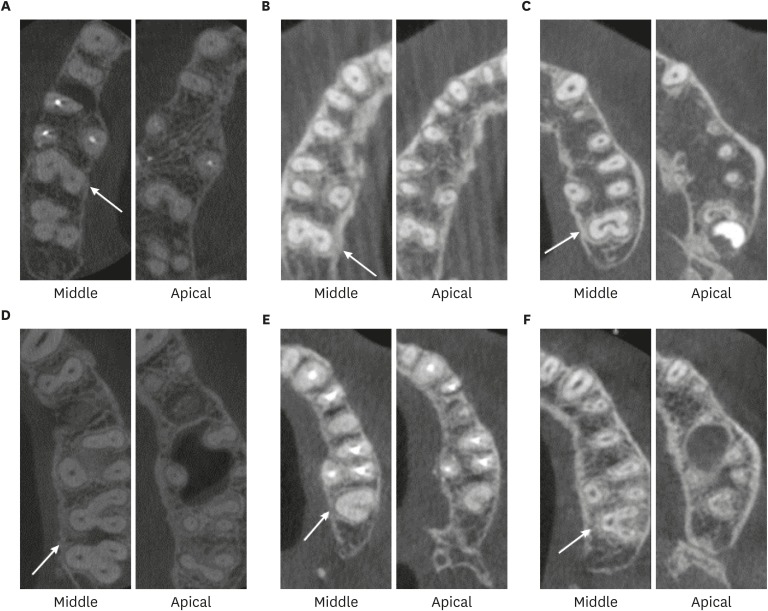
Maxillary C-shaped second molars, fused root type 4 and 5. (A-C) Variations of type 4 root fusion (MB-DB-P roots, proximal groove) (arrows); (D-F) Variations of type 5 root fusion (P-MB-DB roots, buccal groove) (arrows).
Prevalence and distribution of the different types of fusion in upper molars
| Type of fusion | No. (%) |
|---|---|
| 1 | 49 (8.9) |
| 2 | 104 (18.8) |
| 3 | 99 (18.0) |
| 4 | 24 (4.3) |
| 5 | 45 (8.2) |
| 6 | 213 (38.7) |
| Not catalogued | 17 (3.1) |
| Total | 551 (100.0) |
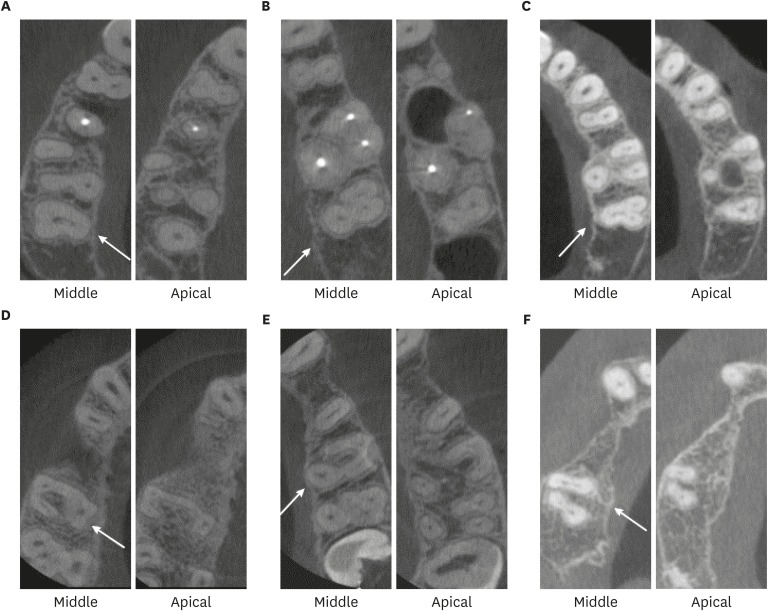
Maxillary first and second molars, fused root type 6 and not catalogued. (A-C) Variations of type 6 root fusion (single root, cone-shape root) (arrows); (D-F) Variations of not catalogued root fusion (arrows).
Comparison of the types of fusion between first and second upper molars
Variation of the continuity of the configuration from the middle third to the apical third
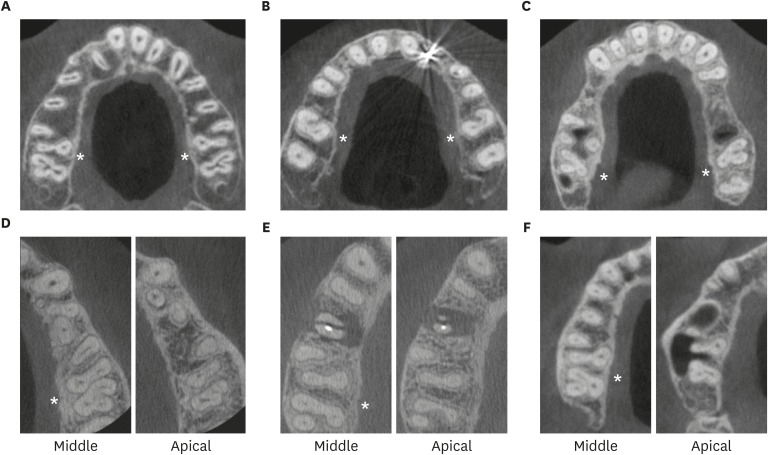
Maxillary first and second molars, symmetry and fusion in adjacent molars. (A-C) Examples of symmetry (*) between right and left maxillary molars. (D-F) Examples of root fusion in the adjacent (*) first and second maxillary molars.
DISCUSSION
CONCLUSION
ACKNOWLEDGMENTS
-
Funding: This study was supported by the Research Department of the Autonomous University of Manizales (grant No. 074-2016).
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Marcano-Caldera M, Mejia-Cardona JL.
Data curation: Marcano-Caldera M, Mejia-Cardona JL, Blanco-Uribe MP, Chaverra-Mesa EC, Rodriguez-Lezama D.
Formal analysis: Marcano-Caldera M, Mejia-Cardona JL, Parra-Sánchez JH.
Investigation: Marcano-Caldera M, Mejia-Cardona JL, Blanco-Uribe MP, Chaverra-Mesa EC.
Methodology: Marcano-Caldera M, Mejia-Cardona JL, Rodriguez-Lezama D, Parra-Sánchez JH.
Resources: Rodriguez-Lezama D, Parra-Sánchez JH.
Validation: Marcano-Caldera M, Mejia-Cardona JL, Blanco-Uribe MP, Chaverra-Mesa EC, Rodriguez-Lezama D, Parra-Sánchez JH.
Writing - original draft: Marcano-Caldera M, Mejia-Cardona JL, Blanco-Uribe MP, Chaverra-Mesa EC, Rodriguez-Lezama D.
Writing - review & editing: Marcano-Caldera M, Mejia-Cardona JL, Parra-Sánchez JH.
- 1. Vertucci FJ. Root canal anatomy of the human permanent teeth. Oral Surg Oral Med Oral Pathol 1984;58:589-599.ArticlePubMed
- 2. Melton DC, Krell KV, Fuller MW. Anatomical and histological features of C-shaped canals in mandibular second molars. J Endod 1991;17:384-388.ArticlePubMed
- 3. Peters OA, Laib A, Rüegsegger P, Barbakow F. Three-dimensional analysis of root canal geometry by high-resolution computed tomography. J Dent Res 2000;79:1405-1409.ArticlePubMedPDF
- 4. Chai WL, Thong YL. Cross-sectional morphology and minimum canal wall widths in C-shaped roots of mandibular molars. J Endod 2004;30:509-512.ArticlePubMed
- 5. Peikoff MD, Christie WH, Fogel HM. The maxillary second molar: variations in the number of roots and canals. Int Endod J 1996;29:365-369.ArticlePubMed
- 6. Fan B, Cheung GS, Fan M, Gutmann JL, Fan W. C-shaped canal system in mandibular second molars: part II—radiographic features. J Endod 2004;30:904-908.ArticlePubMed
- 7. Zhang Q, Chen H, Fan B, Fan W, Gutmann JL. Root and root canal morphology in maxillary second molar with fused root from a native Chinese population. J Endod 2014;40:871-875.ArticlePubMed
- 8. Vertucci FJ. Root canal morphology and its relationship to endodontic procedures. Endod Topics 2005;10:3-29.Article
- 9. Chen J, Li X, Su Y, Zhang D, Wen X, Nie X, An J, Liu L, Deng M. A micro-computed tomography study of the relationship between radicular grooves and root canal morphology in mandibular first premolars. Clin Oral Investig 2015;19:329-334.ArticlePubMedPDF
- 10. Simon JH, Dogan H, Ceresa LM, Silver GK. The radicular groove: its potential clinical significance. J Endod 2000;26:295-298.ArticlePubMed
- 11. Zhao H, Wang H, Pan Y, Pan C, Jin X. The relationship between root concavities in first premolars and chronic periodontitis. J Periodontal Res 2014;49:213-219.ArticlePubMedPDF
- 12. Yang ZP, Yang SF, Lee G. The root and root canal anatomy of maxillary molars in a Chinese population. Endod Dent Traumatol 1988;4:215-218.ArticlePubMed
- 13. Carlsen O, Alexandersen V, Heitmann T, Jakobsen P. Root canals in one-rooted maxillary second molars. Scand J Dent Res 1992;100:249-256.ArticlePubMed
- 14. Ordinola-Zapata R, Martins JN, Bramante CM, Villas-Boas MH, Duarte MH, Versiani MA. Morphological evaluation of maxillary second molars with fused roots: a micro-CT study. Int Endod J 2017;50:1192-1200.PubMed
- 15. Neelakantan P, Subbarao C, Ahuja R, Subbarao CV, Gutmann JL. Cone-beam computed tomography study of root and canal morphology of maxillary first and second molars in an Indian population. J Endod 2010;36:1622-1627.ArticlePubMed
- 16. Kim Y, Lee SJ, Woo J. Morphology of maxillary first and second molars analyzed by cone-beam computed tomography in a Korean population: variations in the number of roots and canals and the incidence of fusion. J Endod 2012;38:1063-1068.ArticlePubMed
- 17. Zheng QH, Wang Y, Zhou XD, Wang Q, Zheng GN, Huang DM. A cone-beam computed tomography study of maxillary first permanent molar root and canal morphology in a Chinese population. J Endod 2010;36:1480-1484.ArticlePubMed
- 18. Tian XM, Yang XW, Qian L, Wei B, Gong Y. Analysis of the root and canal morphologies in maxillary first and second molars in a Chinese population using cone-beam computed tomography. J Endod 2016;42:696-701.ArticlePubMed
- 19. Wu D, Zhang G, Liang R, Zhou G, Wu Y, Sun C, Fan W. Root and canal morphology of maxillary second molars by cone-beam computed tomography in a native Chinese population. J Int Med Res 2017;45:830-842.ArticlePubMedPMCPDF
- 20. Guo J, Vahidnia A, Sedghizadeh P, Enciso R. Evaluation of root and canal morphology of maxillary permanent first molars in a North American population by cone-beam computed tomography. J Endod 2014;40:635-639.ArticlePubMed
- 21. Silva EJ, Nejaim Y, Silva AI, Haiter-Neto F, Zaia AA, Cohenca N. Evaluation of root canal configuration of maxillary molars in a Brazilian population using cone-beam computed tomographic imaging: an in vivo study. J Endod 2014;40:173-176.ArticlePubMed
- 22. Jafarzadeh H, Wu YN. The C-shaped root canal configuration: a review. J Endod 2007;33:517-523.ArticlePubMed
- 23. Kato A, Ziegler A, Higuchi N, Nakata K, Nakamura H, Ohno N. Aetiology, incidence and morphology of the C-shaped root canal system and its impact on clinical endodontics. Int Endod J 2014;47:1012-1033.ArticlePubMedPMCPDF
- 24. Ross IF, Evanchik PA. Root fusion in molars: incidence and sex linkage. J Periodontol 1981;52:663-667.ArticlePubMed
- 25. Special Committee to Revise the Joint AAE/AAOMR Position Statement on use of CBCT in Endodontics. AAE and AAOMR joint position statement: use of cone beam computed tomography in endodontics 2015 update. Oral Surg Oral Med Oral Pathol Oral Radiol 2015;120:508-512.PubMed
- 26. Martins JN, Mata A, Marques D, Caramês J. Prevalence of root fusions and main root canal merging in human upper and lower molars: a cone-beam computed tomography in vivo study. J Endod 2016;42:900-908.ArticlePubMed
- 27. Gao Y, Fan B, Cheung GS, Gutmann JL, Fan M. C-shaped canal system in mandibular second molars part IV: 3-D morphological analysis and transverse measurement. J Endod 2006;32:1062-1065.ArticlePubMed
- 28. Martins JN, Mata A, Marques D, Anderson C, Caramês J. Prevalence and characteristics of the maxillary C-shaped molar. J Endod 2016;42:383-389.ArticlePubMed
- 29. Jo HH, Min JB, Hwang HK. Analysis of C-shaped root canal configuration in maxillary molars in a Korean population using cone-beam computed tomography. Restor Dent Endod 2016;41:55-62.ArticlePubMedPMCPDF
- 30. Ratanajirasut R, Panichuttra A, Panmekiate S. A cone-beam computed tomographic study of root and canal morphology of maxillary first and second permanent molars in a Thai population. J Endod 2018;44:56-61.ArticlePubMed
- 31. Ghobashy AM, Nagy MM, Bayoumi AA. Evaluation of root and canal morphology of maxillary permanent molars in an Egyptian population by cone-beam computed tomography. J Endod 2017;43:1089-1092.ArticlePubMed
- 32. Ng YL, Aung TH, Alavi A, Gulabivala K. Root and canal morphology of Burmese maxillary molars. Int Endod J 2001;34:620-630.ArticlePubMedPDF
REFERENCES
Tables & Figures
REFERENCES
Citations

- Management of a rare bilateral maxillary first molar with six canals using a cone-beam computed tomography: Report of two cases
Aishwarya D. Jain, Nimisha Chinmay Shah, Abhya Jain, Shreya S. Volety
Saudi Endodontic Journal.2025; 15(2): 186. CrossRef - Assessment of root and root canal morphology in maxillary molars with fused roots using Cone Beam Computer Tomography (CBCT) in a Sri Lankan population
Ruvienath Daham Weerasinghe Rajapaksa, Manil Christopher Nishan Fonseka, Ruwan Duminda Jayasinghe, Rasika Manori Jayasinghe
Journal of Oral Biology and Craniofacial Research.2025; 15(6): 1297. CrossRef - Cone-beam computed tomography evaluation of root and canal morphology of maxillary molars in a Chinese kazakh population
Shuchun Yang, Chenye Li, Hui Shi, Ming Liu, Xu Wang
BMC Oral Health.2025;[Epub] CrossRef - Exploring the sex-associated differences in molars fused roots
Maria Eduarda Nunis Locks, Erika Calvano Küchler, Leonardo Santos Antunes, Alice Corrêa Silva-Sousa, Natanael Henrique Ribeiro Mattos, Camila Paiva Perin, Paulo Henrique Condeixa França, Peter Proff, Christian Kirschneck, Flares Baratto-Filho
Annals of Anatomy - Anatomischer Anzeiger.2024; 254: 152245. CrossRef - Cone beam computed tomography analysis of the root and canal morphology of the maxillary second molars in a Syrian subpopulation
Safaa Allawi, Mouhammad Al-Tayyan, Hassan Achour, Eyad Al-Toutangy, Yasser Alsayed Tolibah
BMC Oral Health.2024;[Epub] CrossRef - Prevalence of root fusion in canine maxillary second molar teeth using cone-beam computed tomography
Kristin Linder, Scott MacGee, Loren Schultz
Frontiers in Veterinary Science.2023;[Epub] CrossRef - Dentine thickness in maxillary fused molars depends on the fusion type: An ex vivo micro‐computed tomography study
Cangül Keskin, Defne Toplu, Ali Keleş
International Endodontic Journal.2023; 56(5): 637. CrossRef - Root and canal-specific features of maxillary first molars with fused roots
Katarina Beljic-Ivanovic, Branislav Karadzic
Vojnosanitetski pregled.2022; 79(11): 1092. CrossRef - Micro-CT Analysis of the Root Canal Configuration of Maxillary Second Molars with Fusion
Cangül KESKİN, Özgür ÖZDEMİR, Ali KELEŞ
European Annals of Dental Sciences.2022; 49(Suppl 1): 25. CrossRef - Assessment of C-Shaped Canal Morphology in Mandibular and Maxillary Second Molars in an Iraqi Subpopulation Using Cone-Beam Computed Tomography
Kazhan Abdalrahman, Ranjdar Talabani, Sara Kazzaz, Dlsoz Babarasul, Berndt Koslowski
Scanning.2022; 2022: 1. CrossRef - Analysis of Root and Canal Morphology of Fused and Separate Rooted Maxillary Molar Teeth in Turkish Population
H Aydin
Nigerian Journal of Clinical Practice.2021; 24(3): 435. CrossRef - Investigating prevalence of dental anomalies in Eastern Province of Saudi Arabia through digital orthopantomogram
Jehan ALHumaid, Maryam Buholayka, Arishiya Thapasum, Muhanad Alhareky, Maha Abdelsalam, Amr Bughsan
Saudi Journal of Biological Sciences.2021; 28(5): 2900. CrossRef - Preferred Reporting Items for Epidemiologic Cross-sectional Studies on Root and Root Canal Anatomy Using Cone-beam Computed Tomographic Technology: A Systematized Assessment
Jorge N.R. Martins, Anil Kishen, Duarte Marques, Emmanuel João Nogueira Leal Silva, João Caramês, António Mata, Marco A. Versiani
Journal of Endodontics.2020; 46(7): 915. CrossRef - Second mesiobuccal root canal in maxillary molars—A systematic review and meta-analysis of prevalence studies using cone beam computed tomography
Jorge N.R. Martins, Duarte Marques, Emmanuel João Nogueira Leal Silva, João Caramês, António Mata, Marco A. Versiani
Archives of Oral Biology.2020; 113: 104589. CrossRef
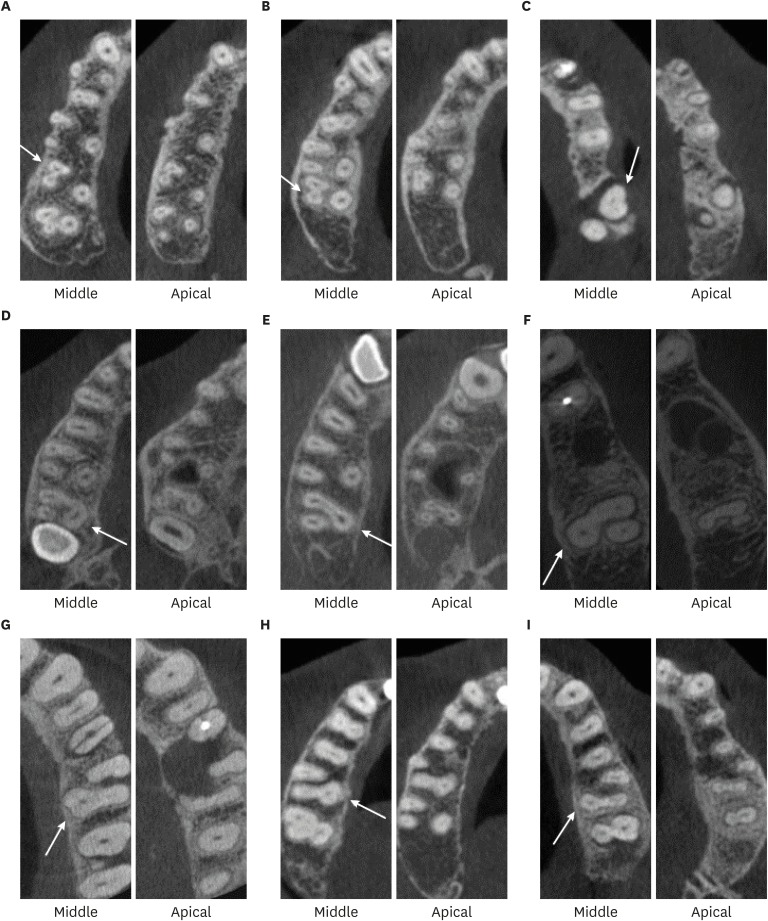
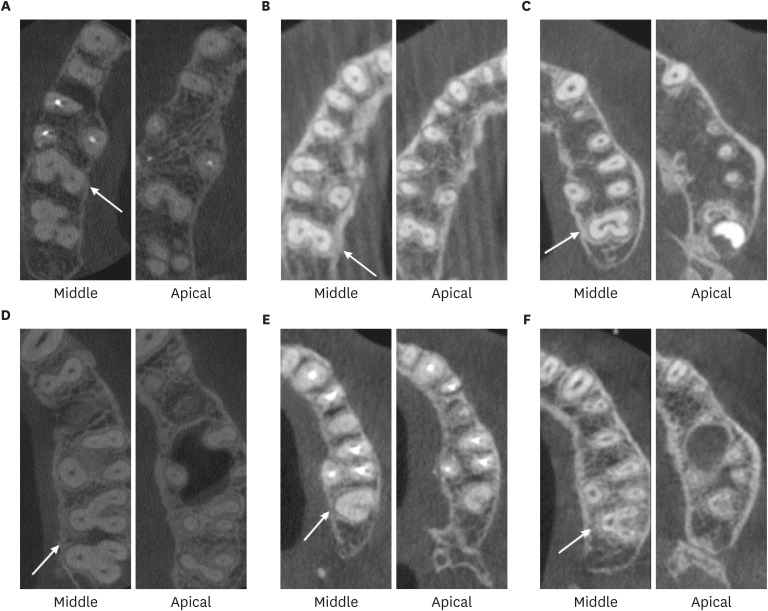
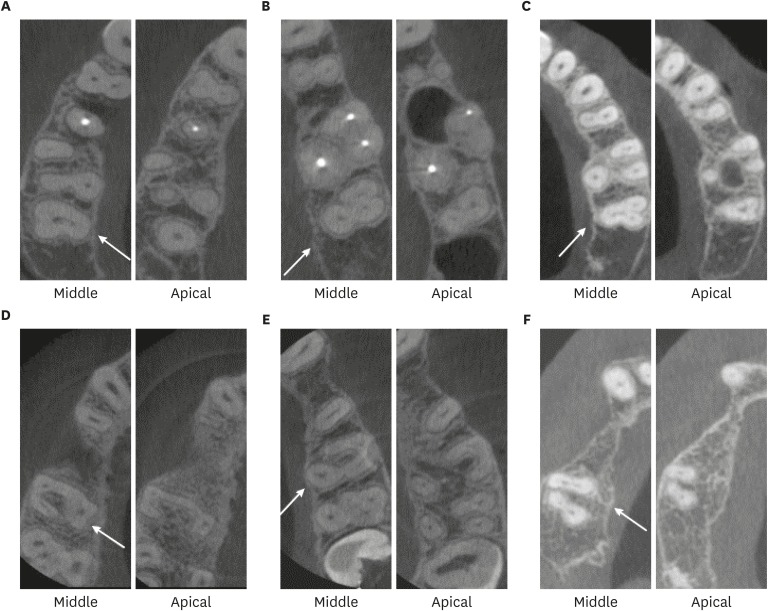
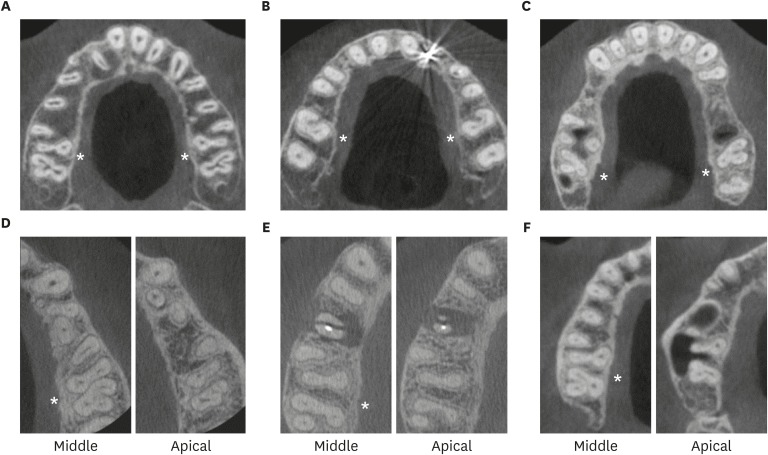
Figure 1
Figure 2
Figure 3
Figure 4
Prevalence and distribution of the different types of fusion in upper molars
| Type of fusion | No. (%) |
|---|---|
| 1 | 49 (8.9) |
| 2 | 104 (18.8) |
| 3 | 99 (18.0) |
| 4 | 24 (4.3) |
| 5 | 45 (8.2) |
| 6 | 213 (38.7) |
| Not catalogued | 17 (3.1) |
| Total | 551 (100.0) |
Comparison of the types of fusion between first and second upper molars
| Type of fusion | First molars | Second molars | Z test |
|---|---|---|---|
| 1 | 7 (5.7) | 42 (9.8) | 1.66 |
| 2 | 12 (9.7) | 92 (21.5) | 3.57* |
| 3 | 73 (58.9) | 26 (6.1) | −11.55* |
| 4 | 2 (1.6) | 22 (5.2) | 2.27* |
| 5 | 4 (3.2) | 41 (9.6) | 2.98* |
| 6 | 20 (16.1) | 193 (45.2) | 7.11* |
| Not catalogued | 6 (4.8) | 11 (2.6) | −1.09 |
| Total | 124 (100.0) | 427 (100.0) | 13.38* |
Data shown are number (%).
*Statistical difference (p < 0.05).
Variation of the continuity of the configuration from the middle third to the apical third
| Middle third | Apical third | |||||||
|---|---|---|---|---|---|---|---|---|
| T 1 | T 2 | T 3 | T 4 | T 5 | T 6 | NC | Separate | |
| T 1 (n = 49) | 38 (77.6) | 0 (0.0) | 0 (0.0) | 1 (2.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 10 (20.4) |
| T 2 (n = 104) | 11 (10.6) | 67 (64.4) | 0 (0.0) | 4 (3.8) | 0 (0.0) | 3 (2.9) | 0 (0.0) | 19 (18.3) |
| T 3 (n = 99) | 4 (4.0) | 0 (0.0) | 65 (65.7) | 2 (2.0) | 0 (0.0) | 4 (4.0) | 3 (3.0) | 21 (21.2) |
| T 4 (n = 24) | 5 (20.8) | 0 (0.0) | 0 (0.0) | 15 (62.5) | 0 (0.0) | 3 (12.5) | 0 (0.0) | 1 (4.2) |
| T 5* (n = 45) | 2 (4.4) | 7 (15.6) | 4 (8.9) | 0 (0.0) | 8 (17.8) | 17 (37.8) | 1 (2.2) | 6 (13.3) |
| T 6 (n = 213) | 27 (12.7) | 7 (3.3) | 6 (2.8) | 15 (7.0) | 6 (2.8) | 123 (57.7) | 10 (4.7) | 19 (8.9) |
| NC (n = 17) | 3 (17.6) | 1 (5.9) | 1 (5.9) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 10 (58.8) | 2 (11.8) |
Data shown are number (%).
T, type; NC, not catalogued.
*Most variability in its configuration from the middle third to the apical third.
Data shown are number (%).
*Statistical difference (
Data shown are number (%).
T, type; NC, not catalogued.
*Most variability in its configuration from the middle third to the apical third.

 KACD
KACD
 ePub Link
ePub Link Cite
Cite

