Abstract
-
Objectives
This study aimed to determine the effects of 1-rooted mandibular second molar (MnSM) teeth on root canal anatomy complexities of the mandibular central incisor (MnCI), mandibular lateral incisor (MnLI), mandibular canine (MnCn), mandibular first premolar (MnFP), mandibular second premolar (MnSP), and mandibular first molar (MnFM) teeth.
-
Materials and Methods
Cone-beam computed tomography images of 600 patients with full lower dentition were examined. Individuals with 1-rooted MnSMs were determined, and the complexity of root canal anatomy of other teeth was compared with individuals without 1-rooted MnSMs (Group-1; subjects with at least one 1-rooted MnSM, Group-2; subjects with more than a single root in both MnSMs). A second canal in MnCIs, MnLIs, MnCns, MnFPs, and MnSPs indicated a complicated root canal. The presence of a third root in MnFMs was recorded as complicated.
-
Results
The prevalence of 1-rooted MnSMs was 12.2%, with the C-shaped root type being the most prevalent (9%). There were fewer complicated root canals in MnCIs (p = 0.02), MnLIs (p < 0.001), and MnFPs (p < 0.001) in Group 1. The other teeth showed no difference between the groups (p > 0.05). According to logistic regression analysis, 1-rooted right MnSMs had a negative effect on having complex canal systems of MnLIs and MnFPs. Left MnSMs were explanatory variables on left MnLIs and both MnFPs.
-
Conclusions
In individuals with single-rooted MnSMs, a less complicated root canal system was observed in all teeth except the MnFMs.
-
Keywords: Cone-beam computed tomography; Cross-sectional studies; C-shaped; Lower second molar; Mandibular second molar; Root canal anatomy
INTRODUCTION
Mandibular second molar (MnSM) teeth are differentiated from adjacent first molars by root and canal anatomy deviations [
1]. Due to their later eruption, the number of roots may vary to adapt to variations in osteometric mandibular form features [
2]. Although MnSMs mostly show a 2-root morphological structure, they can exhibit more than 2 roots or be 1-rooted due to root fusion [
3,
4]. In teeth with root fusion, inter-canal connections depend on the degree of root fusion [
5]. In mild fusion, the canals are distinct and separate, such as the 2-independent rooted/3-canal version with non-C-shaped floors and canal system, while an increase in the intensity of fusion shows web and fin entities partial or along the root or in the canal course between the canals. A complete fusion between the mesial and distal roots is accompanied by a complete union of the canals, with a single wide oval canal throughout the length [
5]. The most common and clinically significant 1-root type in epidemiological studies is the C-shaped root and canal configuration [
2]. C-shaped root and canal structure with specific morphology has been the subject of many studies, especially in East-Asian countries, due to a high frequency of occurrence [
6,
7]. Reports suggest that root fusion and C-shaped morphology in MnSM teeth is an adaptation to fit teeth in narrow jaws, and Aydın [
2] showed that the most influential factor is the anteroposterior distance of the mandible [
2,
7].
One-rooted and C-shaped root canal anatomy, more common in women and ethnically diverse, has its own peculiarities [
4]. Few studies have evaluated correlations between anatomical variations observed in different tooth groups within the same or the opposing dental arch [
8,
9,
10,
11,
12]. Studies have focused on radix entomolaris in mandibular first molar (MnFM) teeth and the complex root-canal anatomies of other mandibular tooth groups. According to these studies, patients with distolingual roots in MnFMs were found to be more likely to have other mandibular teeth with complex roots and canals [
8,
9,
11,
12,
13].
Limited data exists on C-shaped teeth and their correlations with other tooth groups, with only 2 studies addressing this topic [
10,
14]. One of these studies observed that C-shaped MnSMs and distolingually rooted MnFMs were more common in the Mongolian race compared to other populations [
10]. Based on the data from this study, the unilateral distolingual root group showed the highest occurrence of C-shaped MnSMs [
10]. The second study investigated the correlation between C-shaped MnSMs and MnFMs and mandibular premolars [
14]. The study involving limited participants did not find C-shaped teeth in any patient at the same time. As the study focused solely on the correlation between C-shapes, it was unable to assess changes in the complex root structure of mandibular premolars in patients with C-shaped MnSMs. Limited information is available regarding how 1-rooted or C-shaped morphotypes in MnSM teeth impact root canal complexities in other mandibular teeth. Despite numerous studies in the literature on C-shaped MnSM teeth, this issue has received relatively little attention [
4,
15]. Accurate diagnosis of C-shaped canal morphology is essential for the effective implementation of endodontic treatment. Radiographic evaluation, particularly through cone-beam computed tomography (CBCT) images, is commonly employed to identify these canal shapes [
15].
Therefore, this study aimed to determine the effects of 1-rooted and C-shaped MnSMs on the complexity of root canal systems of other mandibular teeth using CBCT images in the Turkish subpopulation. Null hypotheses were that the presence of C-shaped configurations in MnSM teeth does not affect the root canal system of i) mandibular central incisor (MnCI), ii) mandibular lateral incisor (MnLI), iii) mandibular canine (MnCn), iv) mandibular first premolar (MnFP), v) mandibular second premolar (MnSP), and vi) MnFM teeth.
MATERIALS AND METHODS
Subjects and study size
Before this retrospective observational study, the minimum sample size was calculated by power analysis, and the number of 430 was determined, providing a working power of 0.90 for epidemiological studies (Java Applets for sample size and power,
http://www.stat.uiowa.edu/~rlenth/Power). Considering the low frequency of MnSMs in Turkish society, the study involved 600 individuals (300 male, 300 female). Ethics committee approval was obtained for the project and protocols (Akdeniz University Faculty of Medicine Clinical Trials Ethics Committee, KAEK-614). Root and canal anatomies of the participants were analyzed using CBCT. The analyzed images of patients were obtained from the database of a private dental clinic (Ballıpınar Dental Center Antalya/Turkey) between May 2016 and May 2022 during dental treatment, and no additional images were obtained. In the design and presentation of this research, ‘‘preferred reporting items for epidemiologic cross-sectional studies for root and canal anatomy using CBCT’’ and ‘‘STROBE statement/checklist of items in reports of cross-sectional studies’’ (
https://www.strobe-statement.org/checklists) guide was taken and all information was provided [
16].
Images were taken with Sirona Orthophos XG3D (Sirona Dental Systems GmbH, Bensheim, Germany) CBCT machine with 5 kV, 6.0 mA, 0.160 mm3 voxel size, and full-arc (8 × 8 image field) and analyzed with the integrated Sidexis 4 (Sirona, Charlotte, NC, USA) software in multiplanar axial, coronal, and sagittal sections. Analyses were performed by a single experienced examiner (HA, 7-year endodontist).
Inclusion and exclusion criteria
The study included individuals with complete mandibular dentition, excluding lower wisdom teeth. A total of 8,400 mandibular teeth were examined, with 1,200 teeth symmetrically selected from each tooth group. The included teeth had no history of root canal treatment, posts, prosthetic restorations, internal and external resorption, or apical periodontitis. Patients under 16 years of age with incomplete apical root development were excluded from the study. Additionally, low-quality radiographs that did not allow for a detailed examination of root and canal anatomy were also excluded.
The study evaluated a total of 7,982 CBCTs to reach the determined sample size of 600. The reasons for receiving CBCT in these 600 patients were as follows: 385 for presurgical assessment of the relationship between impacted wisdom molars and the mandibular canal, 165 for maxillary comprehensive implant surgery, 24 for orthodontic evaluation, 14 for surgical procedures such as maxillofacial tumors and cysts, and 12 for endodontic evaluation.
Morphological analysis and classification of tooth groups
First, the root and canal anatomies were examined for all mandibular teeth. In each tooth group, the teeth were divided into the following groups according to their root and canal anatomy:
-
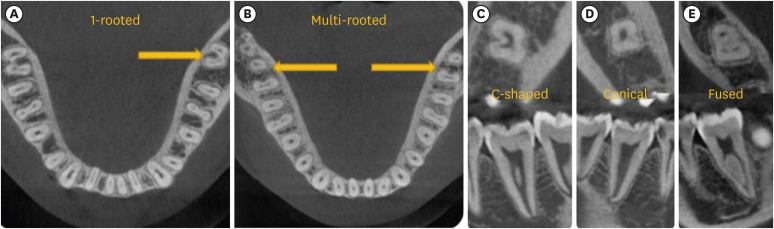
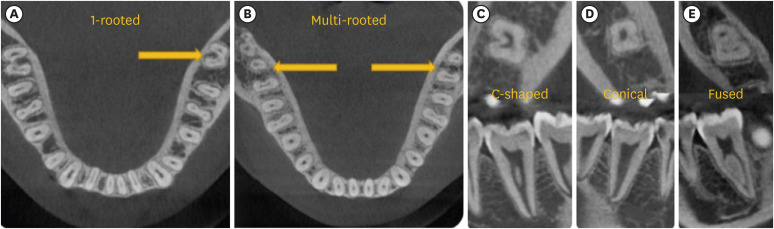
1. MnSMs: According to the number of roots, this tooth group was divided into 1-, 2-, and 3-rooted teeth; 2- and 3-rooted teeth were named multi-rooted, and no further classification was made. Teeth with one root, i.e., a fused or non-divided root, were divided into the following subgroups (Figure 1) [2]:
C-shaped: Having a prominent radicular groove between the roots and exhibiting C1, C2, and C3 configurations in axial cross-section according to Fan classification [6].
Fused: Teeth that are simply notched without the presence of a distinct radicular groove between the roots.
Conical: A single, large, oval, or long oval configuration of the root canal system from the canal orifice to the root tip (C4 configuration).
-
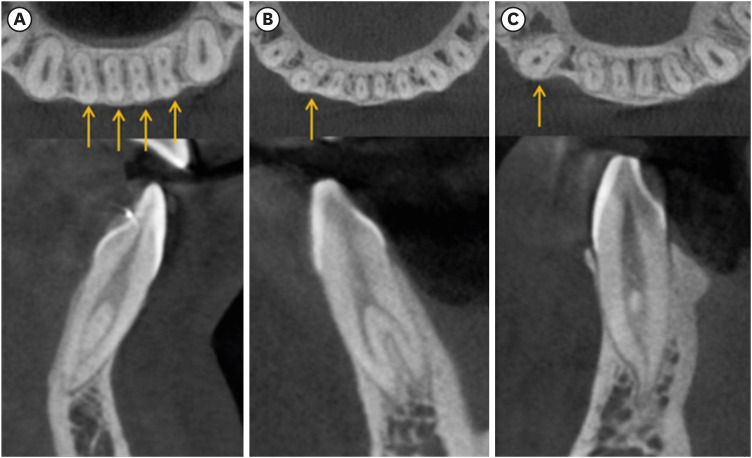
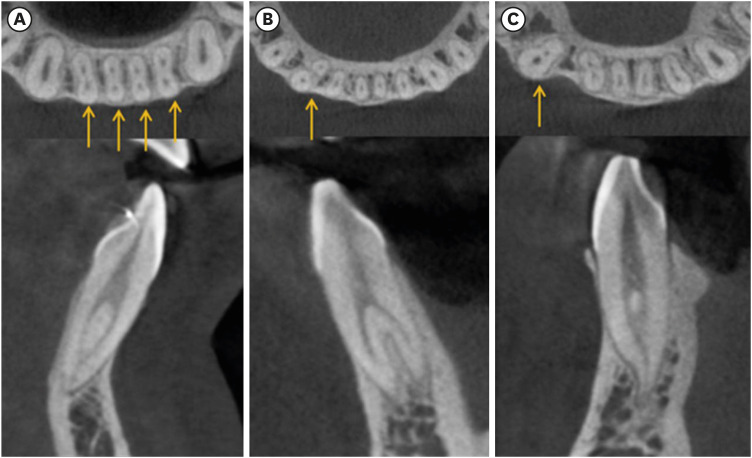
2. Mandibular central and lateral incisors (Figure 2A) [9,13]:
-
3. MnCns (Figure 2B and 2C) [17]:
-
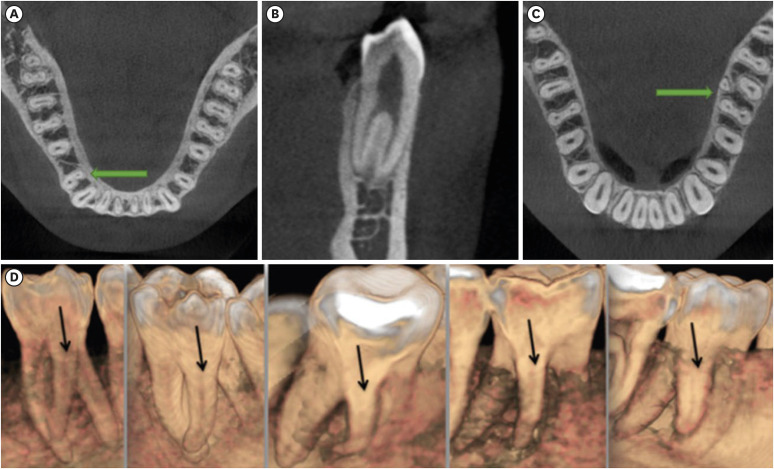
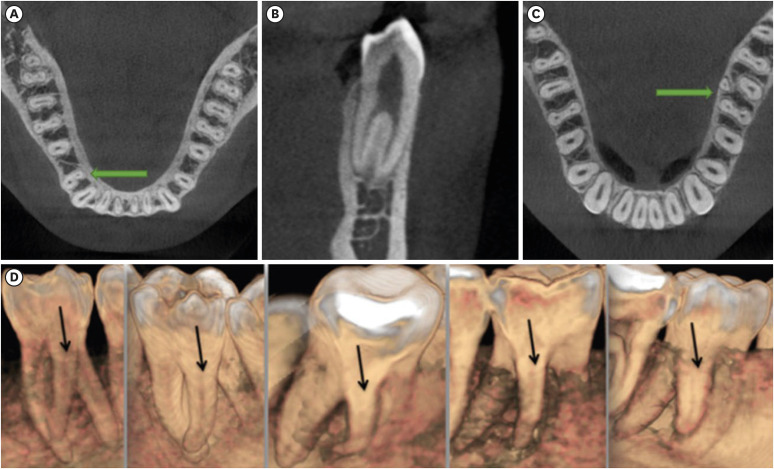
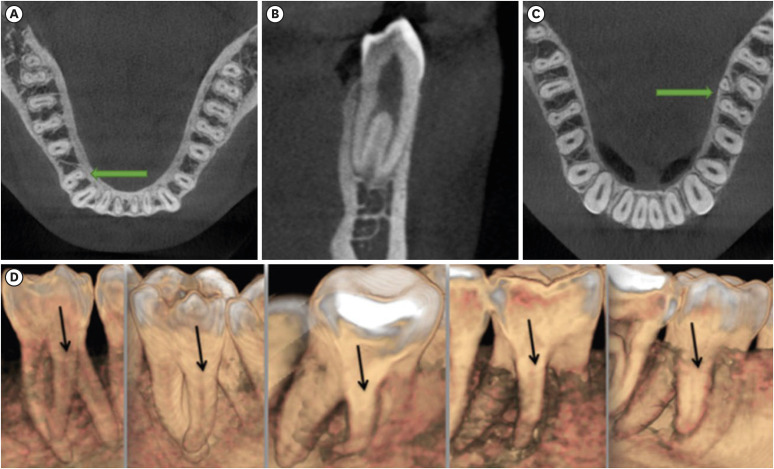
4. Mandibular premolars (Figure 3A and 3B) [8]:
5. MnFMs (Figure 3C and 3D) [8]: These teeth were categorized as 2-rooted and 3-rooted. Three-rooted teeth were considered to have a complicated root structure.
Figure 1Examples of (A) 1-rooted, and (B) multi-rooted MnSM teeth and 1-rooted types, (C) C-shaped, (D) conical, (E) fused.
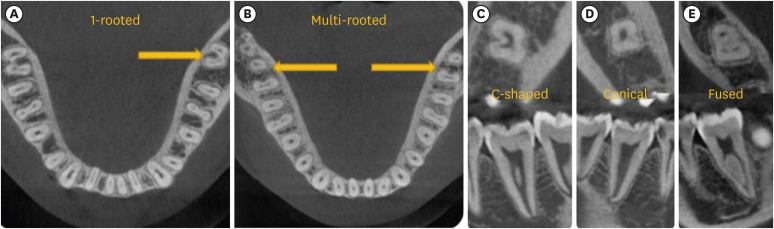
Figure 2(A) Mandibular central and lateral incisors with complicated root canals, (B) 2-rooted mandibular canine, (C) 1-rooted/complicated canal mandibular canine.
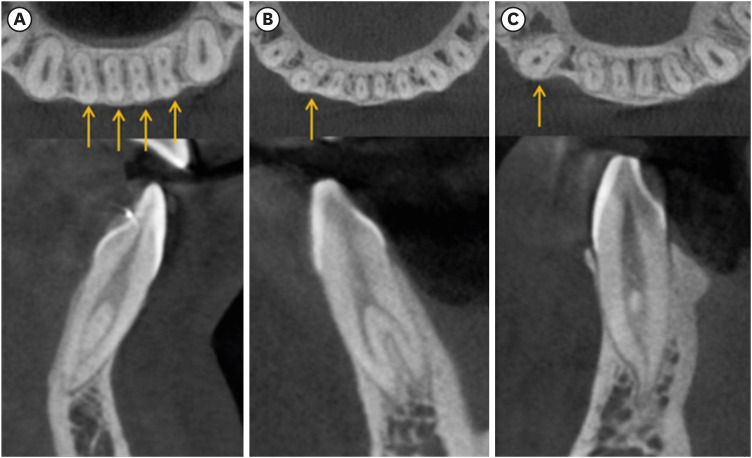
Figure 3(A, B) Mandibular first premolar with complicated root canals, (C, D) examples of radix entomolaris in the mandibular first molar tooth.
Examined root and canal morphologies were determined separately according to sex and tooth groups. The symmetry pattern of the individuals was based on the root number of MnSMs. Individuals with bilateral and unilateral 1-rooted MnSMs were combined under one group (due to the low number of individuals with 1-rooted MnSMs). Individuals without 1-rooted MnSMs were assigned as multi-rooted individuals. Then, it was calculated the number and percentages of root and canal anatomies of the other teeth in these 2 groups (as described above) and examined the differences between these groups.
Statistical analysis
Data were introduced to the SPSS program (SPSS version 23.0, IBM SPSS Statistics, Chicago, IL, USA), and all statistical analyses were conducted at the 5% significance level. The images of 100 patients were re-evaluated after 3 weeks, and the measurement agreement between the 2 evaluations was found using the Cohen kappa test. Sex and tooth position differences were subjected to χ2 (Pearson’s or Fischer’s exact) tests. The effects of 1-rooted MnSM teeth on the complexity of root and canal anatomy of other teeth were determined using binary logistic regression analysis.
RESULTS
The mean age of 600 patients participating in this study was 33.6 ± 10.1 (32 ± 9.6 for women, 35.15 ± 10.37 for men). Intra-rater reliability was 0.98 for MnSMs, and between 0.88 and 0.94 for other teeth and showed a perfect agreement. At least one MnSM tooth was 1-rooted in 86 (14.3%) of 600 patients. The sample number of this group was 86, and the sample number of the group that did not have 1-root MnSM teeth was 514 (85.7%).
Root and root canal anatomies of MnSMs
The numbers and percentages of root numbers and 1-rooted types in MnSMs and their distribution by tooth position and sex are presented in
Table 1. The prevalence of 1-rooted MnSMs was 12.2% (95% confidence interval [CI], 10.4%–14.1%). The most common 1-rooted type was C-shaped canal configuration (9% [95% CI, 7.5%–10.8%]). There was no difference in the number of root and 1-rooted types based on tooth position (
p > 0.05). The frequency of 1-rooted MnSMs was higher in females (
p < 0.001). The symmetry pattern in MnSMs is shown in
Table 2. Of 86 patients with 1-rooted MnSM teeth, 57 (66.3%) had bilateral consistency.
Table 1Numbers and percentages of root numbers and 1-rooted types in mandibular second molars, and their distribution by tooth position and sex
|
Characteristics |
Total (n = 1,200) |
Tooth position |
Sex |
p value |
|
Right (n = 600) |
Left (n = 600) |
Female (n = 600) |
Male (n = 600) |
|
Root numbers |
|
|
|
|
|
|
|
1-rooted |
146 (12.2) |
78 (13) |
68 (11.3) |
96 (16)*
|
50 (8.3) |
< 0.001 |
|
2-rooted |
1,009 (84.1) |
497 (82.8) |
512 (85.3) |
479 (79.8)*
|
530 (88.3) |
< 0.001 |
|
3-rooted |
45 (3.8) |
25 (4.2) |
20 (3.3) |
25 (4.2) |
20 (3.3) |
0.577 |
|
1-rooted type |
|
|
|
|
|
|
|
C-shaped |
108 (9) |
57 (9.5) |
51 (8.5) |
63 (10.5) |
45 (7.5) |
0.069 |
|
Fused |
22 (1.8) |
12 (2) |
10 (1.7) |
19 (3.2)*
|
3 (0.5) |
< 0.001 |
|
Conical |
16 (1.3) |
9 (1.5) |
7 (1.2) |
14 (2.3)*
|
2 (0.3) |
0.003 |
Table 2Symmetry pattern of subjects according to root numbers
|
Symmetry pattern |
Subjects number (%) |
|
1R-1R |
57 (9.5) |
|
1R-2R |
29 (4.8) |
|
2R-2R |
476 (79.3) |
|
2R-3R |
34 (5.7) |
|
3R-3R |
4 (0.7) |
|
Total |
600 (100) |
Root and root canal anatomies of MnCI, MnLI, and MnCn teeth
The numbers and percentages of root and canal types of MnCI, MnLI, and MnCn teeth and their distribution by tooth position and sex are summarized in
Table 3. Second canal occurrence rate in MnCI, MnLI, and MnCn teeth was 41.8% (95% CI, 39.1%–44.7%), 38.5% (95% CI, 35.8%–41.3%), and 8.4% (95% CI, 7.0%–10.1%), respectively. There was no difference in the presence of additional canals for tooth position (
p > 0.05). Males had a higher prevalence of complicated canals in MnCI (
p = 0.005) and MnLI (
p = 0.009) teeth, while females had a higher frequency of complicated MnCn (
p < 0.001).
Table 3Distribution of mandibular central incisor (MnCI), mandibular lateral incisor (MnLI), mandibular canine (MnCn), mandibular first premolar (MnFP), mandibular second premolar (MnSP), and mandibular first molar (MnFM) teeth by number and percentage of root and canal types, tooth position, and sex
|
Characteristics |
Total (n = 1,200) |
Tooth position |
Sex |
p value |
|
Right (n = 600) |
Left (n = 600) |
Female (n = 600) |
Male (n = 600) |
|
MnCI |
|
|
|
|
|
|
|
1-rooted/1-canal |
698 (58.2) |
351 (58.5) |
347 (57.8) |
373 (62.2)*
|
325 (54.2) |
0.005 |
|
Complicated |
502 (41.8) |
249 (41.5) |
253 (42.2) |
227 (37.8)*
|
275 (45.8) |
0.005 |
|
MnLI |
|
|
|
|
|
|
|
1-rooted/1-canal |
738 (61.5) |
378 (63) |
360 (60) |
391 (65.2)*
|
347 (57.8) |
0.009 |
|
Complicated |
462 (38.5) |
222 (37) |
240 (40) |
209 (34.8)*
|
253 (42.2) |
0.009 |
|
MnCn |
|
|
|
|
|
|
|
1-rooted/1-canal |
1,099 (91.6) |
547 (91.2) |
552 (92) |
532 (88.7)*
|
567 (94.5) |
< 0.001 |
|
Complicated |
101 (8.4) |
53 (8.8) |
48 (8) |
68 (11.3)*
|
33 (5.5) |
< 0.001 |
|
|
1-rooted/multicanal |
60 (5) |
34 (5.7) |
26 (4.3) |
37 (6.1) |
23 (3.8) |
0.064 |
|
|
2-rooted |
41 (3.4) |
19 (3.2) |
22 (3.7) |
31 (5.2)*
|
10 (1.7) |
< 0.001 |
|
MnFP |
|
|
|
|
|
|
|
1-rooted/1-canal |
890 (74.2) |
444 (74) |
446 (74.3) |
489 (81.5)*
|
401 (66.8) |
< 0.001 |
|
Complicated |
310 (25.8) |
156 (26) |
154 (25.7) |
111 (18.5)*
|
199 (33.2) |
< 0.001 |
|
MnSP |
|
|
|
|
|
|
|
1-rooted/1-canal |
1,153 (96.1) |
574 (95.7) |
579 (96.5) |
592 (98.7)*
|
561 (93.5) |
< 0.001 |
|
Complicated |
47 (3.9) |
26 (4.3) |
21 (3.5) |
8 (1.3)*
|
39 (6.5) |
< 0.001 |
|
MnFM |
|
|
|
|
|
|
|
2-rooted |
1,168 (97.3) |
580 (96.7) |
588 (98) |
579 (96.5) |
589 (98.2) |
0.073 |
|
3-rooted |
32 (2.7) |
20 (3.3) |
12 (2) |
21 (3.5) |
11 (1.8) |
0.073 |
Root and root canal anatomies of mandibular premolars
The numbers and percentages of root and canal types of MnFPs and MnSPs and their distribution by tooth position and sex are tabulated in
Table 3. The prevalence of complicated canals was 25.8% (95% CI, 23.4%–28.4%) in MnFPs and only 3.9% (95% CI, 3%–5.2%) in MnSPs. There was no difference in tooth position in both MnFPs and MnSPs (
p > 0.05), but a higher percentage was observed in males in both tooth types in terms of complicated canals (
p < 0.001 for both premolars).
The root numbers and percentages of MnFMs and their distribution by tooth position and sex are presented in
Table 3. Only 2.7% (95% CI, 1.9%–3.7%) of all MnFMs had extra roots. In terms of an extra root, there was no difference in sex and tooth position (
p > 0.05).
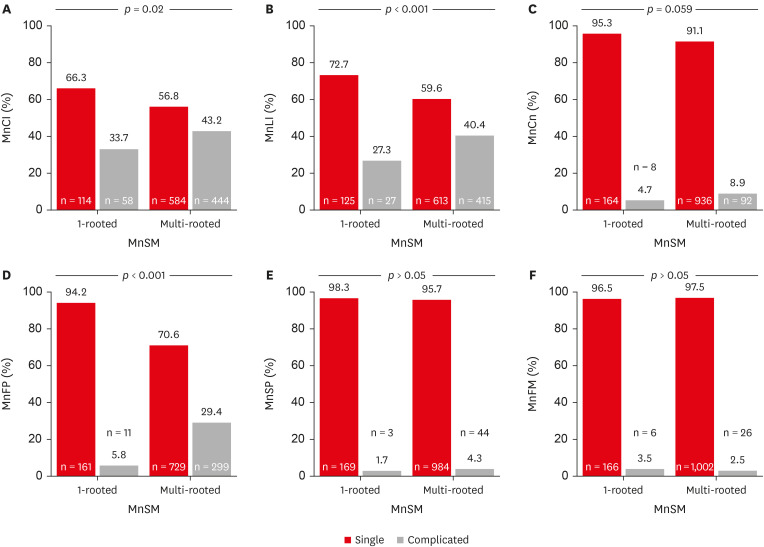
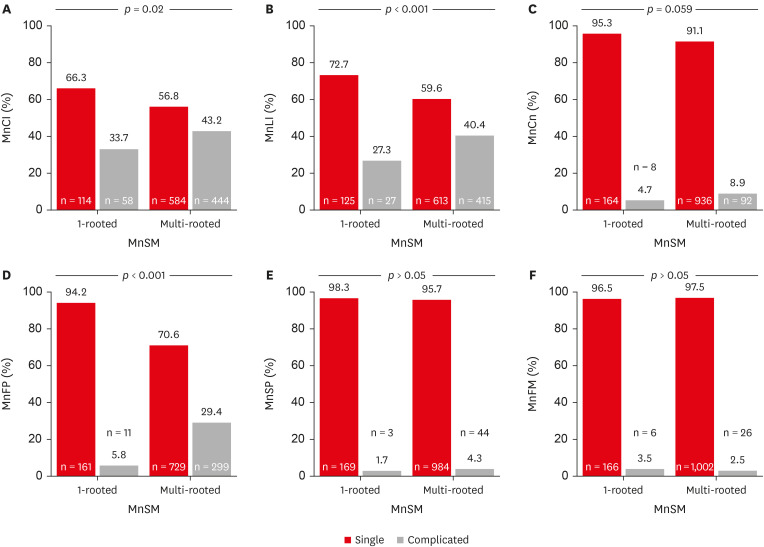
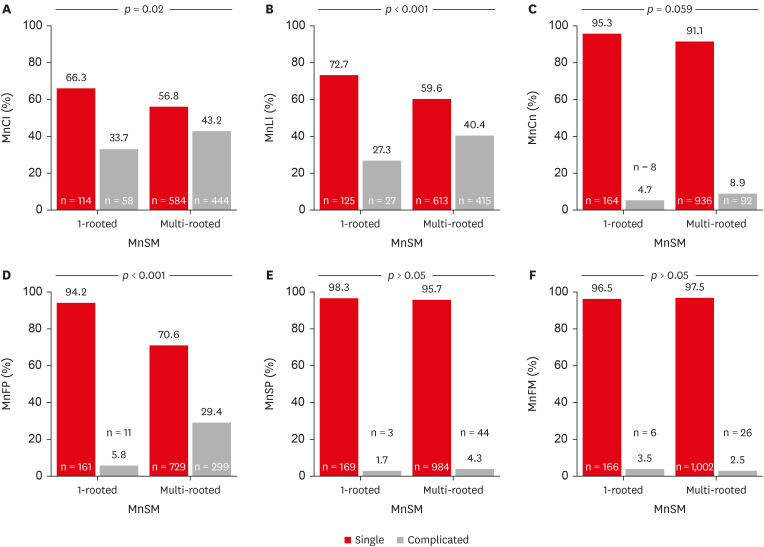
The differences between root and canal morphologies of mandibular teeth in individuals with 1-rooted and multi-rooted MnSMs are shown in
Figure 4. Less complicated root and canal morphology was observed in individuals with 1-rooted MnSMs in all tooth group types except MnFMs. This difference was significant in MnCI (
p = 0.02), MnLI (
p < 0.001), and MnFP tooth types (
p < 0.001) but not in MnCns and MnSPs (
p > 0.05).
Figure 4In individuals with 1-rooted and multi-rooted mandibular second molar (MnSM) teeth, the number, percentages, and p values of the root anatomy of other teeth separately. (A) Mandibular central incisor (MnCI), (B) mandibular lateral incisor (MnLI), (C) mandibular canine (MnCn), (D) mandibular first premolar (MnFP), (E) mandibular second premolar (MnSP), (F) mandibular first molar (MnFM).
Predictive effects of root numbers of MnSM teeth on root-canal anatomy of other teeth
Logistic regression analysis results for right and left 1-rooted MnSM teeth and their predictive effects on the other teeth’ complicated root and canal anatomy, odds ratio, and CIs are listed in
Table 4. In cases where the right MnSM tooth had one root, the root canal systems of both MnLI (
p = 0.49 and
p = 0.006 for right and left MnLI teeth, respectively) and both MnFP teeth (
p < 0.001 for both MnFP teeth) were found to be significantly less complicated. Similarly, in cases where the left MnSM teeth had one root, it was observed that the complex root canal systems of the left MnLI (
p = 0.002) and both MnFPs (
p < 0.001 for both MnFP teeth) were reduced.
Table 4Predictive effects of right and left mandibular second molars (MnSMs) with 1 root on complicated root and canal anatomy of other teeth, according to logistic regression analysis
|
Characteristics |
Right MnSM (independent explanatory variable) |
Left MnSM (independent explanatory variable) |
|
OR (95% CI) |
p value |
OR (95% CI) |
p value |
|
MnCI |
|
|
|
|
|
Right |
0.6 (0.37–1.04) |
> 0.05 |
0.64 (0.37–1.09) |
> 0.05 |
|
Left |
0.65 (0.39–1.07) |
> 0.05 |
0.72 (0.42–1.22) |
> 0.05 |
|
MnLI |
|
|
|
|
|
Right |
0.58 (0.34–0.99) |
0.49*
|
0.68 (0.39–1.18) |
> 0.05 |
|
Left |
0.47 (0.27–0.81) |
0.006*
|
0.38 (0.21–0.7) |
0.002*
|
|
MnCn |
|
|
|
|
|
Right |
0.37 (0.11–1.24) |
> 0.05 |
0.28 (0.07–1.2) |
> 0.05 |
|
Left |
0.6 (0.21–1.72) |
> 0.05 |
0.71 (0.24–2.05) |
> 0.05 |
|
MnFP |
|
|
|
|
|
Right |
0.13 (0.05–0.7) |
< 0.001*
|
0.16 (0.06–0.43) |
< 0.001*
|
|
Left |
0.17 (0.07–0.43) |
< 0.001*
|
0.12 (0.04–0.38) |
< 0.001*
|
|
MnSP |
|
|
|
|
|
Right |
0.26 (0.03–1.93) |
> 0.05 |
0.64 (0.14–2.77) |
> 0.05 |
|
Left |
- |
> 0.05 |
0.38 (0.05–2.89) |
> 0.05 |
|
MnFM |
|
|
|
|
|
Right |
1.18 (0.34–4.15) |
> 0.05 |
1.39 (0.4–4.9) |
> 0.05 |
|
Left |
2.28 (0.6–8.61) |
> 0.05 |
2.68 (0.71–10.16) |
> 0.05 |
DISCUSSION
The failure of Hertwig’s epithelial root sheath (which plays the role of a regulator and inducer in root growth and affects radicular properties, such as root number and shape on the buccal or lingual root surface) is the primary factor in the fusion of MnSM roots [
6,
18]. However, Martins
et al. [
19] noted a high prevalence of root fusion in MnSM teeth in Asians, drawing attention to human genetic lineage tracing hundreds of thousands of years ago, and argued that hereditary and environmental influences shaped the size and shape of jaws and teeth and that Asians with smaller mandibles showed a higher tendency for root fusion than other ethnicities. A higher C-shaped MnSM prevalence of 51.5% was detected in the ancient Chinese people in the Neolithic era, about 5 millennia ago, compared to the modern control human group [
20]. This finding implied that dental morphological characters were regulated by genes. Moreover, environmental factors could create random genetic drift with minimal effect [
20]. Furthermore, the smaller volume of the mandible in women showing sexual dimorphism and the fact that women have more 1-rooted MnSM teeth suggest the effect of mandible form and volume [
19]. In the only recent study that aimed to identify the mandibular dentoalveolar anatomical features influencing 1-rooted MnSMs, the anteroposterior mandibular distance was shorter in the group of individuals with bilateral 1-rooted MnSM teeth [
2].
The endodontic literature on MnSMs has numerous qualitative and quantitative studies on epidemiological, general, and specific issues related to C-shaped teeth owing to their clinical significance [
15,
21,
22]. Internal and external metric and non-metric odontometric features, such as C-shaped configuration in a cross-sectional section from canal orifice level to root apex, location of longitudinal grooves, radicular longitudinal groove depth, radiological appearance, negotiation of C-shaped system according to the type of pulp chamber floor and dentin fusion location, minimum root wall thicknesses, and orientation of the thinnest root wall areas were studied extensively with
ex vivo and
in vivo modality using morphological and histological criteria [
6,
14,
15,
22,
23,
24,
25]. Therefore, the main aim of this study was not to examine the prevalence or biometric characteristics of C-shaped in the Turkish subpopulation in the context of demographic factors but to analyze the implications of this phenomenon on the root canal complexity of other teeth in the mandible when 1-rooted MnSM teeth are detected in the clinic. Roots and canals missed in endodontic treatment led to catastrophic results, risking the long-term success of endodontic treatment [
7]. Undoubtedly, predicting complicated root canal variants in practice can help clinicians.
CBCT analysis has been shown in numerous studies to be beneficial for examining root canal anatomy [
1,
4,
15]. CBCT offers an advantage over traditional 2-dimensional radiographs as it allows for a comprehensive 3-dimensional assessment of root canal systems. Additional CBCT is a noninvasive method, and gender differences and the bilateral prevalence of anatomic variants may be easily compared with CBCT images [
4]. All the data in this study were obtained from an existing CBCT imaging database, allowing for an analysis of a large sample size for all the teeth without exposing the patients to unnecessary radiation.
The frequency of bilateral 1-rooted and/or C-shaped MnSMs can be as high as 80%, especially in Asian populations [
22]. 1-rooted and/or C-shaped teeth are more likely to be bilaterally symmetrical, and the bilateral discrepancy was only 33.7% in the current study, consistent with the literature [
4,
7]. Bilateral presence has high clinical importance as the dentist is more aware of the possibility of root number in the contralateral tooth in cases where bilateral MnSM teeth require treatment. However, the contralateral tooth and other tooth groups in the same arch may need therapy in clinical practice. Thus, the explanatory effects of developmental root differences, such as 1-rooted MnSMs, on root and canal numbers of other teeth increase intraoperative relevance by increasing or decreasing the probability of preoperative estimation, although all possible scenarios are considered.
In the current study, there were significant differences between the root canal forms of the other tooth groups between patients with 1-rooted and multi-rooted MnSMs, and simpler canal anatomies were observed in the 1-rooted group in all tooth groups except the MnFM tooth group. MnFMs are another group of ethnically heterogeneous teeth-related root numbers [
1]. Like 1-rooted and/or C-shaped MnSMs, the frequency of the third root in Asians is much higher than worldwide [
1]. The high prevalence of 1-root and/or C-shaped MnSM and radix entomolaris, which are genetically determined racial dental radicular traits, are considered Asiatic traits [
4,
8]. Distolingual root frequency is less than 5% in non-Asian populations and around 25% in Asians [
1,
3,
8,
26]. The overall prevalence of distolingual roots in MnFMs in the present study was 3.3%, consistent with previous Turkish population studies [
5,
12]. Although there was no significant difference between the 1-rooted and multi-rooted groups, the 1-rooted group had a slightly higher percentage of distolingual roots. This finding is partially consistent with a study by Wu
et al. [
10]. However, some of their findings differed because they divided the groups into bilateral and unilateral distolingual roots. They encountered C-shaped MnSMs most frequently in unilateral radix entomolaris cases, while bilateral radix entomolaris cases showed the lowest occurrence, thus precluding a complete comparison. The null hypothesis for MnFMs was accepted.
In the present study, the frequency of the second canal in MnFPs and MnSPs was 25.8% and 3.9%, respectively, consistent with the literature [
1,
12,
26]. MnFPs exhibit more complex root canals than MnSPs, and their treatment should not be underestimated. In the present study, MnFPs were most often associated with 1-rooted MnSMs. The second canal prevalence was 29.1% in the multi-rooted group, compared to only 6.4% in the 1-rooted group. Logistic regression analysis revealed that odds ratios for MnFMs in the right and left 1-rooted MnSM teeth varied between 0.12 and 0.17. Thus, the incidence of a second canal in MnFPs in the 1-rooted group was approximately 8 times less. For MnSPs, the frequency of complex canals was less in the 1-rooted group, but there was no significant difference. The findings presented on MnFPs are the first information in the literature. The null hypothesis for MnFPs was rejected and accepted for MnSPs.
Unlike other mandibular incisors, MnCns have a higher probability of a second root in the complex root and canal system. While all the mandibular incisors in this study were single-rooted, 41 teeth (3.42%) were bifurcated with 2 separate roots. Therefore, complex root canal systems of this group included both 1-rooted/multi-canal and 2-rooted teeth, and 8.4% did not exhibit a single canal. This incidence is consistent with the literature for Caucasians but higher than that for Asians [
1,
17]. The incidence of additional canals was 4.7% in the 1-rooted MnSM group and 9.7% in the multi-rooted MnSM group. However, the difference was statistically insignificant. Notably, the incidence was less common in the 1-rooted group. The null hypothesis was accepted for MnCns. However, mandibular incisors are tooth groups with more frequent canal separations in the buccal-lingual direction than MnCns, and a second canal is frequently encountered [
1]. In the present study, the complicated canal configuration in the MnCI and MnLI tooth groups was 41.8% and 38.5%, respectively, and was substantial. The prevalence of complicated canals in MnCI and MnLI teeth was lower in the 1-rooted MnSM group and null hypotheses were rejected.
This study had some limitations. Only a single CBCT image database was used in the study. This prevents the generalization of the acquired data to the entire Turkish population. Only mandibular teeth were considered in the study design. Future studies should investigate the effect of 1-rooted and C-shaped root canal anatomy on maxillary teeth. Another limitation was that the bilateral and unilateral groups were combined into a single group in the 1-rooted group. The low incidence of 1-rooted MnSMs in the studied population limited the number of individuals with this radicular morphology. Differences in bilateral and unilateral involvement can be examined by conducting the same study in an Asian population, ensuring a larger sample size of the 1-rooted MnSM tooth group.
CONCLUSIONS
This study investigated the impact of 1-rooted MnSMs on root and canal anatomies of other mandibular teeth. The prevalence of 1-rooted and C-shaped MnSMs in the Turkish subpopulation was 12.2% and 9%, respectively. Subjects with 1-rooted MnSMs had less complicated root canal systems than those with multi-rooted MnSMs in all tooth groups except MnFMs, but it was statistically insignificant in MnCns and MnSPs. Notably, the study underscores the significance of considering these features of MnSMs when planning endodontic treatments to achieve optimal outcomes.
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Aydın H.
Data curation: Aydın H.
Formal analysis: Aydın H.
Funding acquisition: Aydın H.
Investigation: Aydın H.
Methodology: Aydın H.
Project administration: Aydın H.
Resources: Aydın H.
Software: Aydın H.
Supervision: Aydın H, Harorlı H.
Validation: Aydın H, Harorlı H.
Visualization: Aydın H.
Writing - original draft: Aydın H.
Writing - review & editing: Aydın H, Harorlı H.
REFERENCES
- 1. Martins JNR, Gu Y, Marques D, Francisco H, Caramês J. Differences on the root and root canal morphologies between Asian and White ethnic groups analyzed by cone-beam computed tomography. J Endod 2018;44:1096-1104.ArticlePubMed
- 2. Aydın H.. Predictor mandibular dentoalveolar features on the occurrence of 1-rooted/C-shaped mandibular second molar teeth. Eur Endod J 2023 Nov 7 [Epub].
- 3. Martins JN, Mata A, Marques D, Caramês J. Prevalence of root fusions and main root canal merging in human upper and lower molars: a cone-beam computed tomography in vivo study. J Endod 2016;42:900-908.PubMed
- 4. Kim SY, Kim BS, Kim Y. Mandibular second molar root canal morphology and variants in a Korean subpopulation. Int Endod J 2016;49:136-144.ArticlePubMed
- 5. Aydın H, Mobaraki S. Comparison of root and canal anatomy of taurodont and normal molar teeth: a retrospective cone-beam computed tomography study. Arch Oral Biol 2021;130:105242.ArticlePubMed
- 6. Fan B, Cheung GS, Fan M, Gutmann JL, Bian Z. C-shaped canal system in mandibular second molars: part I--anatomical features. J Endod 2004;30:899-903.ArticlePubMed
- 7. Kato A, Ziegler A, Higuchi N, Nakata K, Nakamura H, Ohno N. Aetiology, incidence and morphology of the C-shaped root canal system and its impact on clinical endodontics. Int Endod J 2014;47:1012-1033.ArticlePubMedPMCPDF
- 8. Wu YC, Su CC, Tsai YC, Cheng WC, Chung MP, Chiang HS, et al. Complicated root canal configuration of mandibular first premolars is correlated with the presence of the distolingual root in mandibular first molars: a cone-beam computed tomographic study in Taiwanese individuals. J Endod 2017;43:1064-1071.ArticlePubMed
- 9. Wu YC, Cheng WC, Chung MP, Su CC, Weng PW, Cathy Tsai YW, et al. Complicated root canal morphology of mandibular lateral incisors is associated with the presence of distolingual root in mandibular first molars: a cone-beam computed tomographic study in a Taiwanese population. J Endod 2018;44:73-79.e1.ArticlePubMed
- 10. Wu YC, Su WS, Mau LP, Cheng WC, Weng PW, Tsai YC, et al. Association between the presence of distolingual root in mandibular first molars and the presence of C-shaped mandibular second molars: a CBCT study in a Taiwanese population. Quintessence Int 2020;51:798-807.PubMed
- 11. Yang Y, Jiang C, Chen M, Zeng J, Wu B. Vertucci’s root canal configuration of 11,376 mandibular anteriors and its relationship with distolingual roots in mandibular first molars in a Cantonese population: a cone-beam computed tomography study. BMC Oral Health 2022;22:130.ArticlePubMedPMCPDF
- 12. Aydın H. Correlations between additional roots in maxillary second molars, maxillary first premolars, mandibular first molars and mandibular first premolars: a retrospective cone-beam computed tomography analysis. Odontology 2022;110:584-595.ArticlePubMedPDF
- 13. Wu YC, Cheng WC, Weng PW, Chung MP, Su CC, Chiang HS, et al. The presence of distolingual root in mandibular first molars is correlated with complicated root canal morphology of mandibular central incisors: a cone-beam computed tomographic study in a Taiwanese population. J Endod 2018;44:711-716.e1.ArticlePubMed
- 14. Mashyakhy MH, Chourasia HR, Jabali AH, Bajawi HA, Jamal H, Testarelli L, et al. C-shaped canal configuration in mandibular premolars and molars: prevalence, correlation, and differences: an in vivo study using cone-beam computed tomography. Niger J Clin Pract 2020;23:232-239.ArticlePubMed
- 15. Sinanoglu A, Helvacioglu-Yigit D. Analysis of C-shaped canals by panoramic radiography and cone-beam computed tomography: root-type specificity by longitudinal distribution. J Endod 2014;40:917-921.ArticlePubMed
- 16. Martins JNR, Kishen A, Marques D, Nogueira Leal Silva EJ, Caramês J, Mata A, et al. Preferred reporting items for epidemiologic cross-sectional studies on root and root canal anatomy using cone-beam computed tomographic technology: a systematized assessment. J Endod 2020;46:915-935.ArticlePubMed
- 17. Aydın H. Comparing the crown and root metric properties of double-rooted and single-rooted mandibular canine teeth. Oral Radiol 2023;39:301-311.ArticlePubMedPDF
- 18. Aydin H, Çiloglu Ö. Relationship between root canal merging and presence of C-shaped canal in fused rooted maxillary molar teeth. Braz Dent Sci 2022;25:e2964.Article
- 19. Martins JNR, Marques D, Silva EJNL, Caramês J, Mata A, Versiani MA. Prevalence of C-shaped canal morphology using cone beam computed tomography - a systematic review with meta-analysis. Int Endod J 2019;52:1556-1572.ArticlePubMedPDF
- 20. Ren HY, Zhao YS, Yoo YJ, Zhang XW, Fang H, Wang F, et al. Mandibular molar C-shaped root canals in 5th millennium BC China. Arch Oral Biol 2020;117:104773.ArticlePubMed
- 21. Melton DC, Krell KV, Fuller MW. Anatomical and histological features of C-shaped canals in mandibular second molars. J Endod 1991;17:384-388.ArticlePubMed
- 22. Zheng Q, Zhang L, Zhou X, Wang Q, Wang Y, Tang L, et al. C-shaped root canal system in mandibular second molars in a Chinese population evaluated by cone-beam computed tomography. Int Endod J 2011;44:857-862.ArticlePubMed
- 23. Fan B, Cheung GS, Fan M, Gutmann JL, Fan W. C-shaped canal system in mandibular second molars: part II--radiographic features. J Endod 2004;30:904-908.ArticlePubMed
- 24. Fan B, Min Y, Lu G, Yang J, Cheung GS, Gutmann JL. Negotiation of C-shaped canal systems in mandibular second molars. J Endod 2009;35:1003-1008.ArticlePubMed
- 25. Seo DG, Gu Y, Yi YA, Lee SJ, Jeong JS, Lee Y, et al. A biometric study of C-shaped root canal systems in mandibular second molars using cone-beam computed tomography. Int Endod J 2012;45:807-814.ArticlePubMed
- 26. Martins JNR, Marques D, Mata A, Caramês J. Root and root canal morphology of the permanent dentition in a Caucasian population: a cone-beam computed tomography study. Int Endod J 2017;50:1013-1026.ArticlePubMedPDF
 , Hatice Harorlı2
, Hatice Harorlı2


 KACD
KACD
 ePub Link
ePub Link Cite
Cite

