Search
- Page Path
- HOME > Search
- Assessment of mechanical allodynia in healthy teeth adjacent and contralateral to endodontically diseased teeth: a clinical study
- Vaishnavi Ratnakar Patankar, Ashish K Jain, Rahul D Rao, Prajakta R Rao
- Restor Dent Endod 2024;49(3):e31. Published online July 29, 2024
- DOI: https://doi.org/10.5395/rde.2024.49.e31
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
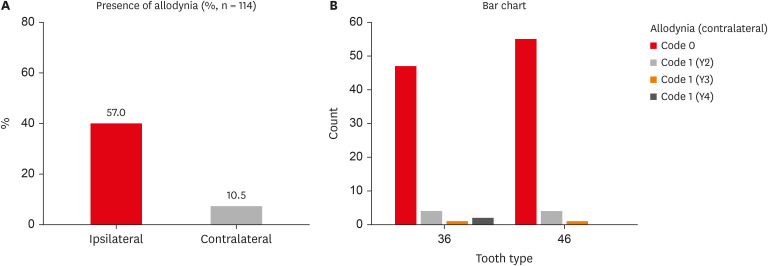
ePub Objectives The present study investigated the prevalence of mechanical allodynia (MA) in healthy teeth adjacent and contralateral to endodontically diseased teeth.
Materials and Methods This cross-sectional study included 114 patients with symptomatic irreversible pulpitis and apical periodontitis in permanent mandibular first molars who possessed healthy teeth adjacent and contralateral to the endodontically diseased tooth. The mechanical sensitivity of the teeth was determined by percussion testing. The presence or absence of pain on percussion in the teeth adjacent and contralateral to the endodontically diseased tooth and the tooth distal to the contralateral symmetrical tooth was recorded according to coding criteria. The prevalence of MA was computed as a percentage, and binary logistic regression analysis was done. The Fisher exact test and Mann-Whitney
U test were used for binary and ordinal data.Results Age and sex did not influence the prevalence of MA. An increased prevalence of MA was found in patients with higher levels of spontaneous pain (
p < 0.001). The prevalence of allodynia was 57% in teeth adjacent to endodontically diseased teeth and 10.5% in teeth contralateral to endodontically diseased teeth. In addition, on the ipsilateral side, there were more painful sensations distal to the diseased tooth than mesially.Conclusions Despite being disease-free, teeth adjacent and contralateral to endodontically diseased teeth exhibited pain on percussion. There was a direct association between the severity of the patient’s pain and the presence of MA.
- 2,807 View
- 89 Download

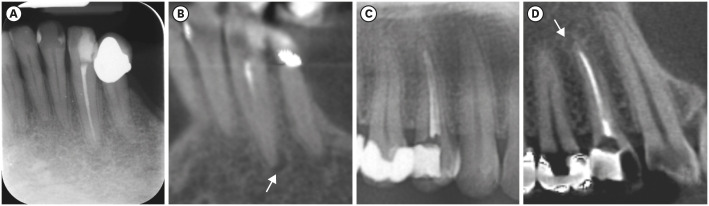
- Endodontic characteristics of mandibular premolar with dens evaginatus: a retrospective study
- Minjin Kim, Sujin Jeon, Min-Seock Seo
- Restor Dent Endod 2024;49(3):e28. Published online July 11, 2024
- DOI: https://doi.org/10.5395/rde.2024.49.e28
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
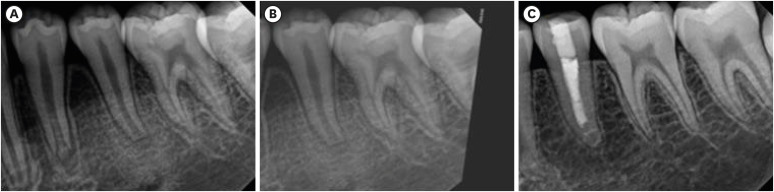
ePub Objectives This study aimed to investigate the endodontic characteristics of mandibular premolars with dens evaginatus (DE) that require endodontic treatment.
Materials and Methods Patients who underwent endodontic treatment were enrolled. The inclusion criteria were patients who underwent root canal treatment in the lower permanent teeth with DE and were followed up for at least 1 year. Preoperative clinical and radiographic variables were obtained. The frequency distribution of the preoperative variables was compared using the χ2 or Fisher’s exact tests. The significance of the change in periapical health index (PAI) and root development stages before and after treatment was examined using the Wilcoxon signed-rank test.
Results A total of 150 teeth of 134 patients with an average age of 15.3 years were included. The percentage distribution comparison of the preoperative variables and obturation techniques revealed significant differences in pulpal and periapical diagnosis, and percussion, and especially regarding age, root development stage, and PAI. Age was the only statistically significant preoperative variable associated with root growth (
p < 0.05).Conclusions Approximately, 60% of DEs requiring endodontic treatment had immature roots. Age being the most significant predisposing factor, early treatment provides the greatest opportunity for full root development.
-
Citations
Citations to this article as recorded by- A tooth with multiple supernumerary cusps and taurodontism concurrently accompanied with other taurodont teeth: a rare case report
Zihui Tang, Hongchen Zhang, Rongrong Dang, Qiushi Zhang, Yan Huang, Yanwei Yang
Surgical and Radiologic Anatomy.2025;[Epub] CrossRef
- A tooth with multiple supernumerary cusps and taurodontism concurrently accompanied with other taurodont teeth: a rare case report
- 3,118 View
- 102 Download
- 1 Web of Science
- 1 Crossref

- Radiographic patterns of periosteal bone reactions associated with endodontic lesions
- Poorya Jalali, Jessica Riccobono, Robert A. Augsburger, Mehrnaz Tahmasbi-Arashlow
- Restor Dent Endod 2023;48(3):e23. Published online June 8, 2023
- DOI: https://doi.org/10.5395/rde.2023.48.e23
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
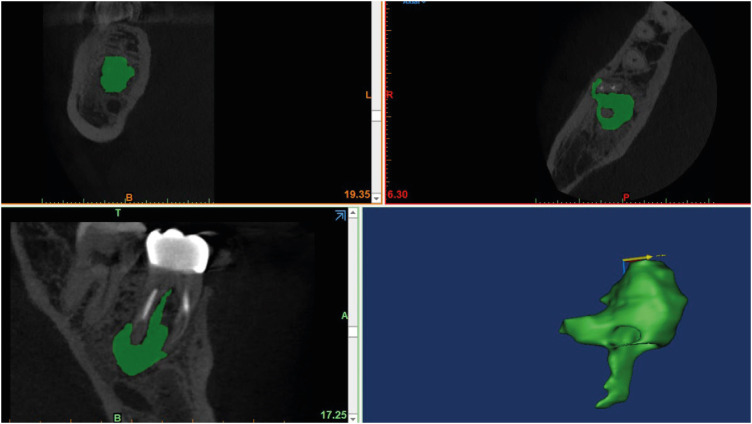
ePub Objectives The formation of new bone by periosteum due to an insult is called periosteal bone reaction (PBR). This study assessed the cone beam computed tomography (CBCT) patterns of periosteal bone reactions associated with periapical inflammatory lesion (apical periodontitis/periapical rarefying osteitis).
Materials and Methods Twenty-two small field of view CBCT images of patients with PBR were selected from a database of a private practice limited to endodontics. The volume of the periapical inflammatory lesion, the presence of cortical fenestration, the distance of the root apices to the affected cortex, and the location, pattern, and longest diameter of the periosteal reaction were recorded. Statistical analysis was performed using Wilcoxon Ranksum, Fischer’s exact, Spearman Correlation Coefficient, and paired
t -test.Results In all cases, periosteal bone reaction manifested as either parallel (90.9%) or irregular (9.1%). No correlation was found between periapical inflammatory lesion volume and the periosteal reaction's longest diameter (
p > 0.05). Cortical fenestration was noted in 72.7% of the cases. In addition, the findings showed that periosteal reactions were located mostly on the buccal and were present 53.8% and 100% of the time in the mandible and maxilla, respectively.Conclusions The periosteal reactions of endodontic origin had a nonaggressive form (
i.e ., parallel or irregular), and none of the lesions resulted in a periosteal reaction with an ominous Codman’s triangle or spicule pattern.-
Citations
Citations to this article as recorded by- The influence of endodontic treatment quality on periapical lesions' architecture in cone‐beam computed tomography
Ewa Mackiewicz, Tobias Bonsmann, Krzysztof Safranow, Patrycja Nowicka, Janusz Kołecki, Alicja Nowicka
Australian Endodontic Journal.2025; 51(1): 36. CrossRef - Novel radiographic pattern of maxillary periostitis induced by endodontic inflammation: A case report
Pai-Chun Huang, I-Hao Su, Meng-Ling Chiang, Jyh-Kwei Chen
Journal of Dental Sciences.2025; 20(3): 1982. CrossRef - Garre’s osteomyelitis of the mandible managed by nonsurgical re-endodontic treatment
Heegyun Kim, Jiyoung Kwon, Hyun-Jung Kim, Soram Oh, Duck-Su Kim, Ji-Hyun Jang
Restorative Dentistry & Endodontics.2024;[Epub] CrossRef
- The influence of endodontic treatment quality on periapical lesions' architecture in cone‐beam computed tomography
- 4,799 View
- 79 Download
- 3 Web of Science
- 3 Crossref

- Interplay of collagen and mast cells in periapical granulomas and periapical cysts: a comparative polarizing microscopic and immunohistochemical study
- Deepty Bansal, Mala Kamboj, Anjali Narwal, Anju Devi, Nisha Marwah
- Restor Dent Endod 2022;47(1):e12. Published online February 14, 2022
- DOI: https://doi.org/10.5395/rde.2022.47.e12
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives This pilot study aimed to establish the interrelationship between collagen and mast cells in periapical granulomas and periapical cysts.
Materials and Methods An observational cross-sectional study was conducted on the paraffin-embedded tissue sections of 68 specimens (34 periapical granulomas and 34 periapical cysts). The specimens were stained with picrosirius to observe collagen fiber birefringence and anti-tryptase antibody to evaluate the mast cell count immunohistochemically. The mean number and birefringence of collagen fibers, as well as the mean number of mast cells (total, granulated, and degranulated), and the mean inflammatory cell density were calculated. The data obtained were analyzed using the Kruskal Wallis test, Mann Whitney
U test, and Spearman correlation test (p < 0.05).Results The mean number of thick collagen fibers was higher in periapical cysts, while that of thin fibers was higher in granulomas (
p = 0.00). Cysts emitted orange-yellow to red birefringence, whereas periapical granulomas had predominantly green fibers (p = 0.00). The mean inflammatory cell density was comparable in all groups (p = 0.129). The number of total, degranulated, and granulated mast cells exhibited significant results (p = 0.00) in both groups. Thick cyst fibers showed significant inverse correlations with inflammation and degranulated mast cells (p = 0.041, 0.04 respectively).Conclusions Mast cells and inflammatory cells influenced the nature of collagen fiber formation and its birefringence. This finding may assist in the prediction of the nature, pathogenesis, and biological behavior of periapical lesions.
-
Citations
Citations to this article as recorded by- The Mystifying Role of Mast Cells in the Pathogenesis of Periapical Pathologies - A Systematic Review
Mala Kamboj, Shashibala Malik, R. Keerthika, Anjali Narwal, Anju Devi, Gopikrishnan Vijayakumar, Adarsh Kumar
Journal of Endodontics.2025; 51(7): 845. CrossRef - Immunohistochemical Analysis of CD117 in the Mast Cells of Odontogenic Keratocysts
Sujatha Varma, Shameena PM, Plakkil Viswanathan Deepthi, Indu G
Cureus.2024;[Epub] CrossRef - Immunohistochemical evaluation of cyclooxygenase‐2 and mast cell density in periapical lesions
Shashibala Malik, Mala Kamboj, Anjali Narwal, Anju Devi
International Endodontic Journal.2023; 56(8): 980. CrossRef
- The Mystifying Role of Mast Cells in the Pathogenesis of Periapical Pathologies - A Systematic Review
- 2,095 View
- 21 Download
- 2 Web of Science
- 3 Crossref

- Which factors related to apical radiolucency may influence its radiographic detection? A study using CBCT as reference standard
- Rocharles Cavalcante Fontenele, Eduarda Helena Leandro Nascimento, Hugo Gaêta-Araujo, Laís Oliveira de Araujo Cardelli, Deborah Queiroz Freitas
- Restor Dent Endod 2021;46(3):e43. Published online July 21, 2021
- DOI: https://doi.org/10.5395/rde.2021.46.e43
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives This study aimed to evaluate the detection rate of apical radiolucencies in 2-dimensional images using cone-beam computed tomography (CBCT) as the reference standard, and to determine which factors related to the apical radiolucencies and the teeth could influence its detection.
Materials and Methods The sample consisted of exams of patients who had panoramic (PAN) and/or periapical (PERI) radiography and CBCT. The exams were assessed by 2 oral radiologists and divided into PAN+CBCT (227 teeth–285 roots) and PERI+CBCT (94 teeth–115 roots). Radiographic images were evaluated for the presence of apical radiolucency, while CBCT images were assessed for presence, size, location, and involvement of the cortical bone (thinning, expansion, and destruction). Diagnostic values were obtained for PERI and PAN.
Results PERI and PAN presented high accuracy (0.83 and 0.77, respectively) and specificity (0.89 and 0.91, respectively), but low sensitivity, especially for PAN (0.40 vs. 0.65 of PERI). The size of the apical radiolucency was positively correlated with its detection in PERI and PAN (
p < 0.001). For PAN, apical radiolucencies were 3.93 times more frequently detected when related to single-rooted teeth (p = 0.038). The other factors did not influence apical radiolucency detection (p > 0.05).Conclusions PERI presents slightly better accuracy than PAN for the detection of apical radiolucency. The size is the only factor related to radiolucency that influences its detection, for both radiographic exams. For PAN, apical radiolucency is most often detected in single-rooted teeth.
-
Citations
Citations to this article as recorded by- Radiomics-based classification of pediatric dental trauma in periapical radiographs: a preliminary study
Mengtian Peng, Bin Yu, Juan Hu, Xiaoxin Xie, Jihong He
BMC Medical Imaging.2025;[Epub] CrossRef - Increasing Diagnostic Acumen in Endodontics
Shilpa Thakkar, Dana Mominkhan
Dental Clinics of North America.2025; 69(4): 479. CrossRef - Three-dimensional clinical assessment for MRONJ risk in oncologic patients following tooth extractions
Catalina Moreno Rabie, Rocharles Cavalcante Fontenele, Nicolly Oliveira Santos, Fernanda Nogueira Reis, Tim Van den Wyngaert, Reinhilde Jacobs
Dentomaxillofacial Radiology.2023;[Epub] CrossRef - Quality of techniques used to assess clinical outcomes of regenerative endodontic treatment in necrotic mature teeth
Roy George
Evidence-Based Dentistry.2022; 23(3): 98. CrossRef
- Radiomics-based classification of pediatric dental trauma in periapical radiographs: a preliminary study
- 2,711 View
- 21 Download
- 3 Web of Science
- 4 Crossref

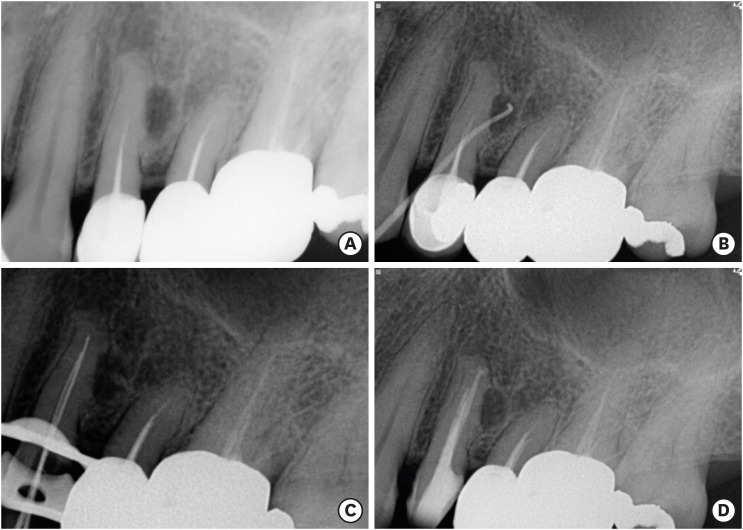
- Surgical management of an accessory canal in a maxillary premolar: a case report
- Hee-Jin Kim, Mi-Kyung Yu, Kwang-Won Lee, Kyung-San Min
- Restor Dent Endod 2019;44(3):e30. Published online July 29, 2019
- DOI: https://doi.org/10.5395/rde.2019.44.e30
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub We report the surgical endodontic treatment of a maxillary first premolar with a lateral lesion that originated from an accessory canal. Although lesions originating from accessory canals frequently heal with simple conventional endodontic therapy, some lesions may need additional and different treatment. In the present case, conventional root canal retreatment led to incomplete healing with the need for further treatment (
i.e. , surgery). Surgical endodontic management with a fast-setting calcium silicate cement was performed on the accessory canal using a dental operating microscope. At the patient's 9-month recall visit, the lesion was resolved upon radiography.-
Citations
Citations to this article as recorded by- Predictive analysis of root canal morphology in relation to root canal treatment failures: a retrospective study
Mohmed Isaqali Karobari, Vishnu Priya Veeraraghavan, P. J. Nagarathna, Sudhir Rama Varma, Jayaraj Kodangattil Narayanan, Santosh R. Patil
Frontiers in Dental Medicine.2025;[Epub] CrossRef - Endodontic management of internal replacement resorption of two maxillary central incisors with the aid of cone-beam computed tomography as the diagnostic tool: a case report and review of literature
Fatemeh Eskandari, Safoora Sahebi, Negar Ghorbani Jahandizi, Hossein Mofidi
Journal of Medical Case Reports.2025;[Epub] CrossRef - The Impact of the Preferred Reporting Items for Case Reports in Endodontics (PRICE) 2020 Guidelines on the Reporting of Endodontic Case Reports
Sofian Youssef, Phillip Tomson, Amir Reza Akbari, Natalie Archer, Fayjel Shah, Jasmeet Heran, Sunmeet Kandhari, Sandeep Pai, Shivakar Mehrotra, Joanna M Batt
Cureus.2023;[Epub] CrossRef - Main and Accessory Canal Filling Quality of a Premixed Calcium Silicate Endodontic Sealer According to Different Obturation Techniques
Su-Yeon Ko, Hae Won Choi, E-Deun Jeong, Vinicius Rosa, Yun-Chan Hwang, Mi-Kyung Yu, Kyung-San Min
Materials.2020; 13(19): 4389. CrossRef
- Predictive analysis of root canal morphology in relation to root canal treatment failures: a retrospective study
- 1,493 View
- 16 Download
- 4 Crossref

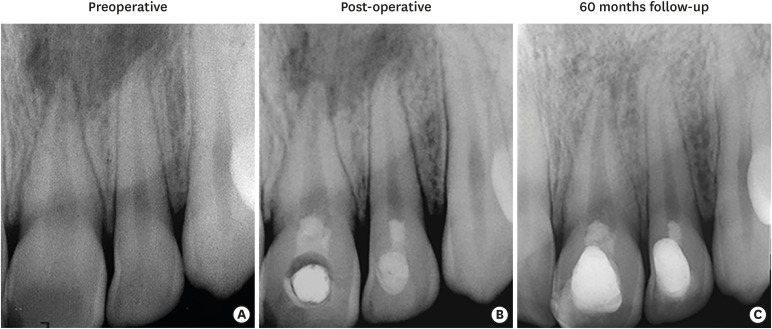
- Revitalization of necrotic mature permanent incisors with apical periodontitis: a case report
- Emre Nagas, M. Ozgur Uyanik, Zafer C. Cehreli
- Restor Dent Endod 2018;43(3):e31. Published online July 5, 2018
- DOI: https://doi.org/10.5395/rde.2018.43.e31
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Despite considerable focus on the regenerative endodontic treatment of immature teeth with necrotic infected pulps and apical periodontitis, little data exist with regard to its possible implementation in necrotic permanent teeth with complete apical and radicular development. The present report describes the procedures and outcome of a regenerative endodontic treatment approach in 2 previously-traumatized incisors with closed apex with apical periodontitis. A 2-visit treatment procedure was employed. At initial visit, the root canals were copiously irrigated, followed by placement of a triple antibiotic paste containing ciprofloxacin, metronidazole, and clindamycin into the root canals. After 4 weeks, the antibiotic paste was removed, and apical bleeding was initiated with size 10 hand files beyond the apices. The root canals were coronally sealed with mineral trioxide aggregate, and the access cavities were restored with bonded resin composite. At post-operative 60 months, both teeth were remained asymptomatic, with the recall radiographs showing complete resolution of apical radiolucency and reestablishment of periradicular tissues. In both teeth, the dimensions of root space remained unchanged as verified by image analysis. The revitalization protocol utilizing root canal disinfection and induced apical bleeding in necrotic, closed-apex incisors may offer a clinically acceptable alternative to conventional root canal treatment.
-
Citations
Citations to this article as recorded by- Regenerative potential of concentrated growth factor compared to platelet-rich fibrin in treatment of necrotic mature teeth: a randomized clinical trial
Taghreed Salah, Wael Hussein, Heba Abdelkafy
BDJ Open.2025;[Epub] CrossRef - Efficacy of Pulp Revascularization in the Treatment of Apical Periodontitis in Mature Necrotic Teeth: An Umbrella Review
Wanderson Limeira de Sousa Barbosa, Luiz Renato Paranhos, Márcia Valente de Brito Dantas, Rômulo Dias Jesuino, João Marcos da Costa Ribeiro, Walbert A. Vieira, Felipe de Souza Matos
Australian Endodontic Journal.2025; 51(2): 495. CrossRef - Clinical and radiographic outcomes of non-surgical retreatment of mature maxillary incisors using two regenerative endodontic techniques in adolescents: a 24-month randomized clinical trial
Ahmad Abdel Hamid Elheeny, Sherif Shafik EL Bahnasy, Yassmin Mohamed ElMakawi, Mohammed Turky, Eman Farouk Ahmed, Norhan Khaled Omar Wahba
BDJ Open.2025;[Epub] CrossRef - Effect of chitosan medicaments loaded with green-synthesized silver nanoparticles on basic fibroblast growth factor release from infected dentin
Dilek Hancerliogullari, Zehra Gun Gok, Nebahat Aytuna Cerci, Eray Ceylanoglu, Bengisu Ozturk, Ozum Hekim Harput, Sevda Durust Baris, Filiz Kiper, Ali Erdemir
Odontology.2025;[Epub] CrossRef - Revolutionizing Endodontics: Innovative Approaches for Treating Mature Teeth With Closed Apices and Apical Lesions: A Report of Two Cases
Claudia Brizuela, Gastón Meza, Maroun Khoury
Journal of Endodontics.2024; 50(5): 596. CrossRef - Current Aspects of Regenerative Endodontics: A Systematic Review
A. V. Mitronin, K. A. Archakov, D. A. Ostanina, Yu. A. Mitronin, T. V. Khizrieva
Endodontics Today.2024; 21(4): 287. CrossRef - Correlation between pulp sensibility and magnetic resonance signal intensity following regenerative endodontic procedures in mature necrotic teeth- a retrospective cohort study
Noha Mohamed El-Kateb, Amr Mohamed Abdallah, Rania Noaman ElBackly
BMC Oral Health.2024;[Epub] CrossRef - Influence of periapical lesion size on healing outcome following regenerative endodontic procedures: a clinical investigation
Noha Mohamed El Kateb, Mahmoud Mostafa Fata
Oral Radiology.2022; 38(4): 480. CrossRef - Do alternative scaffolds used in regenerative endodontics promote better root development than that achieved with blood clots?
Letícia de Araújo, Taynara Santos Goulart, Ana Clara Kuerten Gil, Daniela Peressoni Vieira Schuldt, Beatriz Serrato Coelho, Daniela de Rossi Figueiredo, Lucas da Fonseca Roberti Garcia, Josiane de Almeida
Brazilian Dental Journal.2022; 33(2): 22. CrossRef - Endodontic Regenerative Procedures in Necrotic Adult Teeth
Sara Garrido-Parada, Pablo Castelo-Baz, Nancy Feijoo-Pato, José Gaviño-Orduña, Benjamín Martín-Biedma
Applied Sciences.2022; 12(9): 4212. CrossRef - Combined conventional and regenerative treatment in molars with coexistent closed and open apices: A case series
Zafer C. Cehreli, Gizem Erbas Unverdi, Pinar Eymirli, Irem Mergen, Ezgihan Arslan, Gulce Esenturk
Australian Endodontic Journal.2022; 48(1): 197. CrossRef - Regenerative Endodontic Procedures for the Treatment of Necrotic Mature Teeth with Apical Periodontitis: A Systematic Review and Meta-analysis of Randomized Controlled Trials
Antonios Glynis, Federico Foschi, Ismini Kefalou, Despina Koletsi, Giorgos N. Tzanetakis
Journal of Endodontics.2021; 47(6): 873. CrossRef - Different Approaches to the Regeneration of Dental Tissues in Regenerative Endodontics
Anna M. Krupińska, Katarzyna Skośkiewicz-Malinowska, Tomasz Staniowski
Applied Sciences.2021; 11(4): 1699. CrossRef - Quantitative Assessment of Intracanal Regenerated Tissues after Regenerative Endodontic Procedures in Mature Teeth Using Magnetic Resonance Imaging: A Randomized Controlled Clinical Trial
Noha Mohamed El-Kateb, Rania Noaman El-Backly, Wessam Mohamed Amin, Amr Mohamed Abdalla
Journal of Endodontics.2020; 46(5): 563. CrossRef
- Regenerative potential of concentrated growth factor compared to platelet-rich fibrin in treatment of necrotic mature teeth: a randomized clinical trial
- 2,264 View
- 26 Download
- 14 Crossref

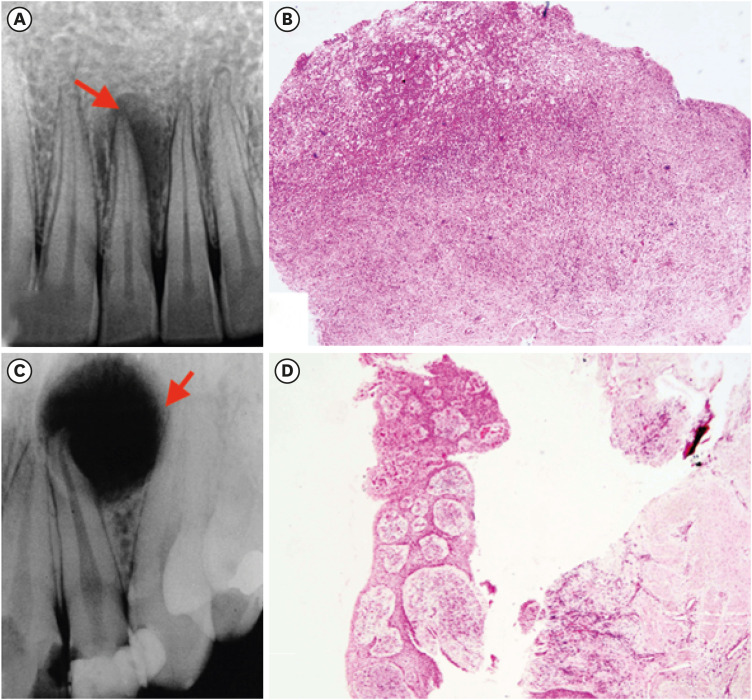
- Differential diagnosis of periapical cyst using collagen birefringence pattern of the cyst wall
- Hyo Jin Ji, Se-Hee Park, Kyung-Mo Cho, Suk Keun Lee, Jin Woo Kim
- Restor Dent Endod 2017;42(2):111-117. Published online February 9, 2017
- DOI: https://doi.org/10.5395/rde.2017.42.2.111
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives Periapical lesions, including periapical cyst (PC), periapical granuloma (PG), and periapical abscess (PA), are frequently affected by chemical/physical damage during root canal treatment or severe bacterial infection, and thus, the differential diagnosis of periapical lesions may be difficult due to the presence of severe inflammatory reaction. The aim of this study was to make differential diagnosis among PC, PG, and PA under polarizing microscope.
Materials and Methods The collagen birefringence patterns of 319 cases of PC (
n = 122), PG (n = 158), and PA (n = 39) obtained using a polarizing microscope were compared. In addition, 6 cases of periodontal fibroma (PF) were used as positive controls.Results Collagen birefringence was condensed with a thick, linear band-like pattern in PC, but was short and irregularly scattered in PG, and scarce or absent in PA. PF showed intense collagen birefringence with a short, palisading pattern but no continuous band-like pattern. The linear band-like birefringence in PC was ascribed to pre-existing expansile tensile stress of the cyst wall.
Conclusions In this study all PCs (
n = 122) were distinguishable from PGs and PAs by their characteristic birefringence, despite the absence of lining epithelium (n = 20). Therefore, the authors suggest that the presence of linear band-like collagen birefringence of the cyst wall aids the diagnostic differentiation of PC from PG and PA.-
Citations
Citations to this article as recorded by- Interplay of collagen and mast cells in periapical granulomas and periapical cysts: a comparative polarizing microscopic and immunohistochemical study
Deepty Bansal, Mala Kamboj, Anjali Narwal, Anju Devi, Nisha Marwah
Restorative Dentistry & Endodontics.2022;[Epub] CrossRef
- Interplay of collagen and mast cells in periapical granulomas and periapical cysts: a comparative polarizing microscopic and immunohistochemical study
- 1,819 View
- 6 Download
- 1 Crossref

- Healing outcomes of root canal treatment for C-shaped mandibular second molars: a retrospective analysis
- Hye-Ra Ahn, Young-Mi Moon, Sung-Ok Hong, Min-Seock Seo
- Restor Dent Endod 2016;41(4):262-270. Published online August 29, 2016
- DOI: https://doi.org/10.5395/rde.2016.41.4.262
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives This study aimed to evaluate the healing rate of non-surgical endodontic treatment between C-shaped and non-C-shaped mandibular second molars.
Materials and Methods Clinical records and radiological images of patients who had undergone endodontic treatment on mandibular second molars between 2007 and 2014 were screened. The periapical index scoring system was applied to compare healing outcomes. Information about preoperative and postoperative factors as well as the demographic data of the patients was acquired and evaluated using chi-square and multinomial logistic regression tests.
Results The total healing rate was 68.4%. Healing rates for the mandibular second molar were 70.9% in C-shaped canals (
n = 79) and 66.6% in non-C-shaped ones (n = 117). The difference was not statistically significant.Conclusions The presence of a C-shaped canal in the mandibular second molar did not have a significantly negative effect on healing after treatment. Instead, proper pulpal diagnosis and final restoration were indicated as having significantly greater influence on the healing outcomes of C-shaped and non-C-shaped canals, respectively.
-
Citations
Citations to this article as recorded by- Predicting early endodontic treatment failure following primary root canal treatment
Young-Eun Jang, Yemi Kim, Sin-Young Kim, Bom Sahn Kim
BMC Oral Health.2024;[Epub] CrossRef - Factors Influencing Non-Surgical Root Canal Treatment Outcomes in Mandibular Second Molars: A Retrospective Cone-Beam Computed Tomography Analysis
Da-Min Park, Woo-Hyun Seok, Ji-Young Yoon
Journal of Clinical Medicine.2024; 13(10): 2931. CrossRef - Retrospective Assessment of Healing Outcome of Endodontic Treatment for Mandibular Molars with C-shaped Root Canal
Kishore Kumar Majety, Basanta Kumar Choudhury, Anika Bansal, Achla Sethi, Jaina Panjabi
The Journal of Contemporary Dental Practice.2017; 18(7): 591. CrossRef
- Predicting early endodontic treatment failure following primary root canal treatment
- 1,718 View
- 19 Download
- 3 Crossref

- The use of platelet rich plasma in the treatment of immature tooth with periapical lesion: a case report
- Günseli Güven Polat, Ceren Yıldırım, Özlem Martı Akgün, Ceyhan Altun, Didem Dinçer, Cansel Köse Özkan
- Restor Dent Endod 2014;39(3):230-234. Published online June 2, 2014
- DOI: https://doi.org/10.5395/rde.2014.39.3.230
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub This study describes the treatment of an immature permanent tooth with periapical lesion which was treated with regenerative approach using platelet rich plasma (PRP). The root canal of immature human permanent tooth with periapical lesion was gently debrided of necrotic tissue and disinfected with 2.5% NaOCl, and then medicated with triple antibiotic paste comprised of ciprofloxacin, metronidazole, and tetracycline. When the tooth was asymptomatic, PRP and mineral trioxide aggregate (MTA) were placed into the root canal. Six months after PRP treatment, radiographical examination revealed resolution of the radiolucency and progressive thickening of the root wall and apical closure. Our findings suggest that PRP can be used for the treatment of immature permanent teeth with periapical lesion, as part of a regenerative endodontic treatment procedure.
-
Citations
Citations to this article as recorded by- Evaluation of postoperative pain and healing following regenerative endodontics using platelet‐rich plasma versus conventional endodontic treatment in necrotic mature mandibular molars with chronic periapical periodontitis. A randomized clinical trial
Yassmin Elsayed Ahmed, Geraldine Mohamed Ahmed, Angie Galal Ghoneim
International Endodontic Journal.2023; 56(4): 404. CrossRef - Different Approaches to the Regeneration of Dental Tissues in Regenerative Endodontics
Anna M. Krupińska, Katarzyna Skośkiewicz-Malinowska, Tomasz Staniowski
Applied Sciences.2021; 11(4): 1699. CrossRef - Coronal tooth discoloration induced by regenerative endodontic treatment using different scaffolds and intracanal coronal barriers: a 6-month ex vivo study
Noushin Shokouhinejad, Hassan Razmi, Maryam Farbod, Marzieh Alikhasi, Josette Camilleri
Restorative Dentistry & Endodontics.2019;[Epub] CrossRef - Efficacy of Autologous Platelet Concentrates in Regenerative Endodontic Treatment: A Systematic Review of Human Studies
Joanna Metlerska, Irini Fagogeni, Alicja Nowicka
Journal of Endodontics.2019; 45(1): 20. CrossRef - Bone, Periodontal and Dental Pulp Regeneration in Dentistry: A Systematic Scoping Review
Luiz Alexandre Chisini, Marcus Cristian Muniz Conde, Guillermo Grazioli, Alissa Schmidt San Martin, Rodrigo Varella de Carvalho, Letícia Regina Morello Sartori, Flávio Fernando Demarco
Brazilian Dental Journal.2019; 30(2): 77. CrossRef - Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview – part II: other clinical applications and complications
M. Torabinejad, M. Parirokh, P. M. H. Dummer
International Endodontic Journal.2018; 51(3): 284. CrossRef - Alternative to Avoid Tooth Discoloration after Regenerative Endodontic Procedure: A Systematic Review
Luciane Geanini Pena dos Santos, Luiz Alexandre Chisini, Camila Guerner Springmann, Beatriz Dulcineia Mendes de Souza, Fernanda Geraldo Pappen, Flávio Fernando Demarco, Mara Cristina Santos Felippe, Wilson Tadeu Felippe
Brazilian Dental Journal.2018; 29(5): 409. CrossRef - Influence of Apical Diameter on the Outcome of Regenerative Endodontic Treatment in Teeth with Pulp Necrosis: A Review
Yanjun Fang, Xinhuan Wang, Jingjing Zhu, Chaonan Su, Ying Yang, Liuyan Meng
Journal of Endodontics.2018; 44(3): 414. CrossRef - A scoping review of root canal revascularization: relevant aspects for clinical success and tissue formation
M. C. M. Conde, L. A. Chisini, R. Sarkis‐Onofre, H. S. Schuch, J. E. Nör, F. F. Demarco
International Endodontic Journal.2017; 50(9): 860. CrossRef - Effects of Epigallocatechin Gallate, an Antibacterial Cross-linking Agent, on Proliferation and Differentiation of Human Dental Pulp Cells Cultured in Collagen Scaffolds
Young-Sun Kwon, Hee-Jin Kim, Yun-Chan Hwang, Vinicius Rosa, Mi-Kyung Yu, Kyung-San Min
Journal of Endodontics.2017; 43(2): 289. CrossRef - Regenerative Endodontics
Kristina Feigin, Bonnie Shope
Journal of Veterinary Dentistry.2017; 34(3): 161. CrossRef - Regenerative Endodontic Treatment or Mineral Trioxide Aggregate Apical Plug in Teeth with Necrotic Pulps and Open Apices: A Systematic Review and Meta-analysis
Mahmoud Torabinejad, Ali Nosrat, Prashant Verma, Oyoyo Udochukwu
Journal of Endodontics.2017; 43(11): 1806. CrossRef - Platelet concentrates for revitalization of immature necrotic teeth: a systematic review of the clinical studies
Alessandra Lolato, Cristina Bucchi, Silvio Taschieri, Ahmed El Kabbaney, Massimo Del Fabbro
Platelets.2016; 27(5): 383. CrossRef - Regenerative endodontics—Creating new horizons
Harnoor Dhillon, Mamta Kaushik, Roshni Sharma
Journal of Biomedical Materials Research Part B: Applied Biomaterials.2016; 104(4): 676. CrossRef - The impact of autologous platelet concentrates on endodontic healing: a systematic review
Nastaran Meschi, Ana B. Castro, Katleen Vandamme, Marc Quirynen, Paul Lambrechts
Platelets.2016; 27(7): 613. CrossRef - Pulp and Periodontal Regeneration of an Avulsed Permanent Mature Incisor Using Platelet-rich Plasma after Delayed Replantation: A 12-month Clinical Case Study
Harini Priya M, Pavan B. Tambakad, Jaya Naidu
Journal of Endodontics.2016; 42(1): 66. CrossRef - Platelet preparations in dentistry: How? Why? Where? When?
Luigi Fabrizio Rodella
World Journal of Stomatology.2015; 4(2): 39. CrossRef
- Evaluation of postoperative pain and healing following regenerative endodontics using platelet‐rich plasma versus conventional endodontic treatment in necrotic mature mandibular molars with chronic periapical periodontitis. A randomized clinical trial
- 1,517 View
- 6 Download
- 17 Crossref

- Mental nerve paresthesia secondary to initiation of endodontic therapy: a case report
- Syed Mukhtar-Un-Nisar Andrabi, Sharique Alam, Afaf Zia, Masood Hasan Khan, Ashok Kumar
- Restor Dent Endod 2014;39(3):215-219. Published online May 8, 2014
- DOI: https://doi.org/10.5395/rde.2014.39.3.215
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Whenever endodontic therapy is performed on mandibular posterior teeth, damage to the inferior alveolar nerve or any of its branches is possible. Acute periapical infection in mandibular posterior teeth may also sometimes disturb the normal functioning of the inferior alveolar nerve. The most common clinical manifestation of these insults is the paresthesia of the inferior alveolar nerve or mental nerve paresthesia. Paresthesia usually manifests as burning, prickling, tingling, numbness, itching or any deviation from normal sensation. Altered sensation and pain in the involved areas may interfere with speaking, eating, drinking, shaving, tooth brushing and other events of social interaction which will have a disturbing impact on the patient. Paresthesia can be short term, long term or even permanent. The duration of the paresthesia depends upon the extent of the nerve damage or persistence of the etiology. Permanent paresthesia is the result of nerve trunk laceration or actual total nerve damage. Paresthesia must be treated as soon as diagnosed to have better treatment outcomes. The present paper describes a case of mental nerve paresthesia arising after the start of the endodontic therapy in left mandibular first molar which was managed successfully by conservative treatment.
-
Citations
Citations to this article as recorded by- Evolving Paradigms in the Management of Trigeminal Nerve Injuries Post Oral Surgery: A Comprehensive Narrative Review
Saanvi Tank, Amit Patil, Tejal Patil, Minal M Kshirsagar, Aarti S Bedia, Sanpreet S Sachdev, Vyshnavi Mundada
Cureus.2025;[Epub] CrossRef - Separated Surgical Instrument During the Extraction of a Third Molar: A Case Report
Abdulaziz A Mahdi, Abdullah I Alkharji, Safa A Alburayh, Bader A Fatani, Osama A Alharbi
Cureus.2025;[Epub] CrossRef - Treatment of paresthesia induced by periapical lesions: a case report
Hyo Jin Jo, Jung-Hong Ha
Journal of Dental Rehabilitation and Applied Science.2024; 40(4): 305. CrossRef - İMPLANT CERRAHİSİ SONRASI HİPOESTEZİ-6 AYLIK TAKİP: VAKA SERİSİ
Sefa AYDINDOĞAN, Emine Elif MUTAFCİLAR VELİOĞLU, Yunus Emre BALABAN
Selcuk Dental Journal.2023; 10(4): 350. CrossRef - Mental Nerve Paraesthesia: A Report of Two Cases Associated with Endodontic Etiology
Neeta Patel, Akshayraj Langaliya, Shikha Kanodia, Aravind Kumbhar, Aastha Buch, Aarshvi Shah, Himani Bhatt, Drashti Panchal, Sharan Shah, Jinali Shah, Darko Macan
Case Reports in Dentistry.2021;[Epub] CrossRef - Anatomic Danger Zones of the Head and Neck
Guy Talmor, Andy Trang, Omeed Ahadiat, Boris Paskhover, Ashley Wysong
Dermatologic Surgery.2020; 46(12): 1549. CrossRef - The anatomical relationship between the roots of erupted permanent teeth and the mandibular canal: a systematic review
Michał Puciło, Mariusz Lipski, Magdalena Sroczyk-Jaszczyńska, Aleksandra Puciło, Alicja Nowicka
Surgical and Radiologic Anatomy.2020; 42(5): 529. CrossRef - Endodontic-related inferior alveolar nerve injuries: A review and a therapeutic flow chart
R. Castro, M. Guivarc'h, J.M. Foletti, J.H. Catherine, C. Chossegros, L. Guyot
Journal of Stomatology, Oral and Maxillofacial Surgery.2018; 119(5): 412. CrossRef - Neuropathy of Trigeminal Nerve Branches After Oral and Maxillofacial Treatment
Jimoh Olubanwo Agbaje, Elke Van de Casteele, Marjolein Hiel, Ciska Verbaanderd, Ivo Lambrichts, Constantinus Politis
Journal of Maxillofacial and Oral Surgery.2016; 15(3): 321. CrossRef - Facial nerve paralysis following endodontic treatment of lower first molar
Umut Demetoglu, Gokhan Ozkan, Hasan Onur Simsek
Journal of Oral and Maxillofacial Surgery, Medicine, and Pathology.2016; 28(3): 267. CrossRef - Broken Endodontic Instrument Caused Inferior Alveolar Nerve Paraesthesia: A Case Report.
M. Ozbek Selcuk, Kaman Süleyman, Ozgur Demiralp Kemal
Journal of Dentistry And Oral Implants.2016; 1(1): 21. CrossRef
- Evolving Paradigms in the Management of Trigeminal Nerve Injuries Post Oral Surgery: A Comprehensive Narrative Review
- 2,797 View
- 12 Download
- 11 Crossref

- Misdiagnosis of florid cemento-osseous dysplasia leading to unnecessary root canal treatment: a case report
- Jong-Ki Huh, Su-Jung Shin
- Restor Dent Endod 2013;38(3):160-166. Published online August 23, 2013
- DOI: https://doi.org/10.5395/rde.2013.38.3.160
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub This case report demonstrates an unnecessary endodontic treatment of teeth with florid cemento-osseous dysplasia (FCOD) due to a misdiagnosis as periapical pathosis and emphasizes the importance of correct diagnosis to avoid unnecessary treatment. A 30-year-old woman was referred to our institution for apicoectomies of the mandibular left canine and both the lateral incisors. The periapical lesions associated with these teeth had failed to resolve after root canal treatment over a 3-year period. Radiographic examinations revealed multiple lesions on the right canine, the second premolar, and both first molars as well as the anterior region of the mandible. Based on clinical, radiographic and histological evaluations, the patient condition was diagnosed as FCOD. The patient has been monitored for 2 years. To avoid unnecessary invasive treatment, accurate diagnosis is essential before treatment is carried out in managing FCOD.
-
Citations
Citations to this article as recorded by- Periapical cemento‐osseous dysplasia masquerading as asymptomatic chronic apical periodontitis in a Chinese woman: A case report
Yunjing Ma, Dong Fang, Mei Ji
Clinical Case Reports.2024;[Epub] CrossRef - Benign Fibro-Osseous Lesions of The Jaw: A Retrospective Analysis
Saim Yanık, Mehmet Emrah Polat
European Journal of Therapeutics.2024; 30(5): 760. CrossRef - Radiological follow-up of cemento-osseous dysplasia on cone-beam computed tomography
Stefan F. Nemec, Steffen Schneider, Klaus M. Friedrich, Michael Weber, Ursula Schwarz-Nemec
Journal of Cranio-Maxillofacial Surgery.2024; 52(5): 644. CrossRef - Cemento osseous dysplasia(COD) of the mandibular teeth misdiagnosed as periapical lesion; cone beam CT-based case report
Won-Jeong Han
The Journal of The Korean Dental Association.2024; 62(7): 432. CrossRef - Surgical Management of Infection Secondary to Cemento-osseous Dysplasia
Farin Ebrahimi, Faraz Ebrahimi, Jingang An
Journal of Craniofacial Surgery.2023; 34(6): e614. CrossRef - Florid osseous dysplasia mimicking odontogenic infections: A report of two cases and literature review
A. Wajdi Bin Mohammed, Mohammed Mubarak Aldosari, Osama A. Alharbi, Ahmed Alzahrani, Abdullah M. Alsoghier
Saudi Journal of Oral Sciences.2023; 10(3): 195. CrossRef - Radiolucent lesions that may resemble inflammatory periapical lesions: A review article
Hamad Albagieh, Mohammed Aldosari, Abdulmajeed Alkhathlan, Nawaf Alfawaz, Mohammed Almutairi
The Saudi Dental Journal.2023; 35(8): 916. CrossRef - Cemento-Osseous Dysplasia: A Detailed Comparison of the 2005 and 2017 WHO Classifications and Case Analysis
Jiankang Zhang, Yunbo Yu, Wei Tang, Jian Pan, Wei Jing
Cureus.2023;[Epub] CrossRef - The bony changes after mandibular incisors retraction on a severe skeletal Class II bimaxillary protrusion extraction patient with periapical cemento-osseous dysplasia
Huijuan Wang, Yiwen Zhou, Baochao Li, Ling Huang, Huang Li
AJO-DO Clinical Companion.2022; 2(5): 496. CrossRef - Cemento-ossøs dysplasi – en diagnostisk utfordring
Stig Løvold, Sivakami Rethnam Haug
Den norske tannlegeforenings Tidende.2022; 132(11): 938. CrossRef - A retrospective cone beam computed tomography analysis of cemento-osseous dysplasia
Birsay Gumru, Melda Pelin Akkitap, Sevilay Deveci, Ender Idman
Journal of Dental Sciences.2021; 16(4): 1154. CrossRef - Florid Cemento-osseous Dysplasia: A Report of Two Cases and Literature Review
Prashanth Panta, Imran Shahid, Mukund Seshadri
The Journal of Contemporary Dental Practice.2021; 22(3): 304. CrossRef - Natural history of florid osseous dysplasia of the jaws with important clinical implications
Camile S. Farah, Marie Anne T. Matias
Australian Endodontic Journal.2021; 47(3): 684. CrossRef - Clinical assessment of cemento‐osseous dysplasia based on three‐dimensional diagnostic imaging: A case report
Naoki Shibata, Kyoko Inamoto, Munetaka Naitoh, Eiichiro Ariji
Australian Endodontic Journal.2021; 47(1): 105. CrossRef - Odontogenic Cysts
Arvind Babu Rajendra Santosh
Dental Clinics of North America.2020; 64(1): 105. CrossRef - Difficulties in the diagnosis of periapical translucencies and in the classification of cemento-osseous dysplasia
Andrea Brody, Attila Zalatnai, Krisztian Csomo, Andrea Belik, Csaba Dobo-Nagy
BMC Oral Health.2019;[Epub] CrossRef - Florid Cemento-Osseous Dysplasia of Osteolytic Stage Showing Cyst-Like Findings on CT and MRI: A Case Report
Kotaro Ito, Naohisa Hirahara, Norihito Iizuka, Eri Sawada, Shunya Okada, Masaaki Suemitsu, Kayo Kuyama, Takashi Kaneda
International Journal of Oral-Medical Sciences.2019; 17(3-4): 137. CrossRef - Oral management of a patient with cemento-osseous dysplasia: a case report
Camila de Nazaré Alves de Oliveira KATO, Juliana Diogo de Almeida SAMPAIO, Tânia Mara Pimenta do AMARAL, Lucas Guimarães ABREU, Cláudia Borges BRASILEIRO, Ricardo Alves MESQUITA
RGO - Revista Gaúcha de Odontologia.2019;[Epub] CrossRef - Cemento-osseous dysplasia: Re-visited
International Journal of Dental Research and Oral Health.2019;[Epub] CrossRef - Retrospective Study of 383 Cases of Fibro-Osseous Lesions of the Jaws
Camila de Nazaré Alves de Oliveira Kato, Laiz Fernandes Mendes Nunes, Loliza Luiz Figueiredo Houri Chalub, Adriana Etges, Tarcília Aparecida Silva, Ricardo Alves Mesquita
Journal of Oral and Maxillofacial Surgery.2018; 76(11): 2348. CrossRef - Successful Implant Placement in a Case of Florid Cemento-Osseous Dysplasia: A Case Report and Literature Review
Nasrin Esfahanizadeh, Hila Yousefi
Journal of Oral Implantology.2018; 44(4): 275. CrossRef - Recurrent symptomatic cemento-osseous dysplasia: A case report
Chang-Ki Min, Kwang-Joon Koh, Kyoung-A Kim
Imaging Science in Dentistry.2018; 48(2): 131. CrossRef - Cemento-Osseous Dysplasias: Imaging Features Based on Cone Beam Computed Tomography Scans
Paulo Henrique Pereira Cavalcanti, Eduarda Helena Leandro Nascimento, Maria Luiza dos Anjos Pontual, Andréa dos Anjos Pontual, Priscylla Gonçalves Correia Leite de Marcelos, Danyel Elias da Cruz Perez, Flávia Maria de Moraes Ramos-Perez
Brazilian Dental Journal.2018; 29(1): 99. CrossRef - Florid cemento-osseous dysplasia: a contraindication to orthodontic treatment in compromised areas
Alberto Consolaro, Sergio Rafael Baggio Paschoal, Jose Burgos Ponce, Dario A. Oliveira Miranda
Dental Press Journal of Orthodontics.2018; 23(3): 26. CrossRef - Clinical, demographic, and radiographic analysis of 82 patients affected by florid osseous dysplasia: an international collaborative study
Débora Lima Pereira, Fábio Ramôa Pires, Márcio Ajudarte Lopes, Román Carlos, John Marshal Wright, Paras Patel, Willie van Heerden, Andre Uys, Pablo Agustin Vargas
Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology.2016; 122(2): 250. CrossRef - Cone beam CT as an aid to diagnosing mixed radiopaque radiolucent lesions in the mandibular incisor region
Unni Krishnan, Manal Al Maslamani, Alex J Moule
BMJ Case Reports.2015; 2015: bcr2014207617. CrossRef - Benign Fibro-Osseous Lesions of the Craniofacial Area in Children and Adolescents: A Review
D.V. Rogozhin, F. Bertoni, D. Vanel, M. Gambarotti, A. Righi, I.V. Bulycheva, D.M. Konovalov, A.G. Talalaev, V.Yu. Roshin, A.P. Ektova, M.V. Bolotin, A.V. Lopatin
Arkhiv patologii.2015; 77(4): 63. CrossRef - Dysplasie osseuse floride mandibulaire : un cas de découverte fortuite et revue de la littérature
Eugénie Massereau, Ugo Ordioni, Maud Guivarc’h, Guillaume Royer, Jean-Hugues Catherine
Médecine Buccale Chirurgie Buccale.2015; 21(2): 101. CrossRef
- Periapical cemento‐osseous dysplasia masquerading as asymptomatic chronic apical periodontitis in a Chinese woman: A case report
- 2,192 View
- 18 Download
- 28 Crossref

- Vital tooth with periapical lesion: spontaneous healing after conservative treatment
- Hyun-Joo Kim, Seung-Jong Lee, Il-Young Jung, Sung-Ho Park
- Restor Dent Endod 2012;37(2):123-126. Published online May 18, 2012
- DOI: https://doi.org/10.5395/rde.2012.37.2.123
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub It is often presumed that apical periodontitis follows total pulp necrosis, and consequently root canal treatment is commonly performed. Periapical lesion development is usually caused by bacteria and its byproduct which irritate pulp, develop pulpitis, and result in necrosis through an irreversible process. Afterwards, apical periodontitis occurs. This phenomenon is observed as an apical radiolucency in radiographic view. However, this unusual case presents a spontaneous healing of periapical lesion, which has developed without pulp necrosis in a vital tooth, through conservative treatment.
- 1,903 View
- 29 Download

- Effects of canal enlargement and irrigation needle depth on the cleaning of the root canal system at 3 mm from the apex
- Ho-Jin Moon, Chan-Ui Hong
- Restor Dent Endod 2012;37(1):24-28. Published online March 2, 2012
- DOI: https://doi.org/10.5395/rde.2012.37.1.24
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives The aim of this study was to test the hypothesis, that the effectiveness of irrigation in removing smear layer in the apical third of root canal system is dependent on the depth of placement of the irrigation needle into the root canal and the enlargement size of the canal.
Materials and Methods Eighty sound human lower incisors were divided into eight groups according to the enlargement size (#25, #30, #35 and #40) and the needle penetration depth (3 mm from working length, WL-3 mm and 9 mm from working length, WL-9 mm). Each canal was enlarged to working length with Profile.06 Rotary Ni-Ti files and irrigated with 5.25% NaOCl. Then, each canal received a final irrigation with 3 mL of 3% EDTA for 4 min, followed by 5 mL of 5.25% NaOCl at different level (WL-3 mm and WL-9 mm) from working length. Each specimen was prepared for the scanning electron microscope (SEM). Photographs of the 3mm area from the apical constriction of each canal with a magnification of ×250, ×500, ×1,000, ×2,500 were taken for the final evaluation.
Results Removal of smear layer in WL-3 mm group showed a significantly different effect when the canal was enlarged to larger than #30. There was a significant difference in removing apical smear layer between the needle penetration depth of WL-3 mm and WL-9 mm.
Conclusions Removal of smear layer from the apical portion of root canals was effectively accomplished with apical instrumentation to #35/40 06 taper file and 3 mm needle penetration from the working length.
-
Citations
Citations to this article as recorded by- Numerical Evaluation of Flow Pattern for Root Canal Irrigation Including icrobubbles
Joon Hyun Kim, Chan U Lee, Inwhan Lee, Jaeyong Sung
Journal of the Korean Society of Manufacturing Technology Engineers.2023; 32(5): 251. CrossRef
- Numerical Evaluation of Flow Pattern for Root Canal Irrigation Including icrobubbles
- 1,073 View
- 5 Download
- 1 Crossref

- A retrospective study of the intentionally replanted mandibular second molars with C-shaped root canal configurations
- Won-Jun Shon, Kee-Yeon Kum, Seung-Ho Baek, Woo-Cheol Lee
- J Korean Acad Conserv Dent 2011;36(1):19-25. Published online January 31, 2011
- DOI: https://doi.org/10.5395/JKACD.2011.36.1.19
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives The purpose of this retrospective study was to evaluate the success rate of intentionally replanted mandibular second molar with C-shaped canal configurations and to access the impact of preoperative periapical lesion on the success of intentional replantation procedure.
Materials and Methods This retrospective chart review study evaluated 52 intentionally replanted mandibular second molar teeth treated at Seoul National University Dental Hospital Department of Conservative Dentistry from January 2005 to December 2007. Seventeen teeth were lost for the follow-up, and another 6 teeth did not meet inclusion criteria of C-shaped root canal configurations. Healing outcome such as success, uncertain healing, and failure after follow-up was evaluated by clinical criteria and radiographs.
Results The overall success rate was 72.4% for the 29 intentionally replanted C-shaped mandibular second molars. The success rate of replanted teeth with preoperative periapical lesions was similar to that of replanted teeth which have no periapical lesions.
Conclusions Therefore, root canal treatment failure on C-shaped mandibular second molar can be predictably treated by intentional replantation regardless of the presence of periapical lesion.
- 1,087 View
- 6 Download

- Prognostic factors influencing clinical outcome of nonsurgical endodontic treatment
- Seonah Kim
- J Korean Acad Conserv Dent 2010;35(6):436-444. Published online November 30, 2010
- DOI: https://doi.org/10.5395/JKACD.2010.35.6.436
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives This study aimed to assess prospectively the clinical outcome of nonsurgical endodontic treatment and identify patient- and tooth-related factors, rather than treatment-related factors, that were the best predictors of this outcome.
Materials and Methods The inception cohort comprised 441 teeth (320 patients) and 175 teeth (123 patients) were followed up for 1-2 years. Age, gender, presence of medical disease, number of canals, previous endodontic treatment, presence of sensitivity and pain, pulp vitality, swelling or sinus tract of pulpal origin on the gingiva, periapical radiolucency and tendency of unilateral bite on the affected tooth were recorded at treatment start.
Results The outcome was classified on the basis of periapical radiolucency as healed or non healed. The overall healed rate in these cases, including nonsurgical retreatment, was 81.1%. Four tooth-related factors had a negative impact in the bivariate analysis: previous endodontic treatment, necrotic pulp, preoperative gingival swelling or sinus tract of pulpal origin, and preoperative periapical radiolucency. Stepwise logistic regression analysis including patient-, tooth-related factors and level of the root canal filling as a treatment-related factor showed that preoperative gingival lesion (odds ratio [OR]: 4.4;
p = 0.005), preoperative periapical radiolucency (OR: 3.6;p = 0.011), and ≤ 1-2 mm under root filling length (OR: 9.6;p = 0.012) were significant predictors of failure.Conclusions A preoperative gingival lesion of pulpal origin can influence the outcome of nonsurgical endodontic treatment in addition to preoperative periapical radiolucency.
-
Citations
Citations to this article as recorded by- A retrospective study on the prognostic factors and success, survival, and failure outcomes of treated endodontic‐periodontal lesions
Ingar Wong, An Ton, Amiel J. Cassidy, Nicolette Fozzard, Lavanya Ajay Sharma, Robert M. Love, Ajay Sharma
Clinical and Experimental Dental Research.2024;[Epub] CrossRef - Evaluation of gutta-percha removal from the dentinal tubules using different instrumentation techniques with or without solvent: An In vitro study
MukeshKumar Hasija, Babita Meena, Deepti Wadhwa, KulvinderKaur Wadhwani, Virender Yadav
Journal of the International Clinical Dental Research Organization.2020; 12(1): 27. CrossRef - Surgical endodontic management of infected lateral canals of maxillary incisors
Ji-Hyun Jang, Jung-Min Lee, Jin-Kyu Yi, Sung-Baik Choi, Sang-Hyuk Park
Restorative Dentistry & Endodontics.2015; 40(1): 79. CrossRef - Single visit nonsurgical endodontic therapy for periapical cysts: A clinical study
Ipsita Maity, N. Meena, R. Anitha Kumari
Contemporary Clinical Dentistry.2014; 5(2): 195. CrossRef
- A retrospective study on the prognostic factors and success, survival, and failure outcomes of treated endodontic‐periodontal lesions
- 4,125 View
- 34 Download
- 4 Crossref

- The relationship of radiographic lesion size and characteristics to diagnosis of periapical cysts and granulomas
- Ho-Sik Choi, Woo-Cheol Lee, Won-Jun Shon, Kee-Yeon Kum, Kwang-Shik Bae, Seung-Ho Baek
- J Korean Acad Conserv Dent 2010;35(1):24-29. Published online January 31, 2010
- DOI: https://doi.org/10.5395/JKACD.2010.35.1.024
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub The purpose of this study was to find out the relationship of radiographic lesion size, gender, age of patients and radiographic character to the diagnosis of periapical cyst and granuloma.
The data was collected from 187 periapical lesions of 167 patients who undergone apical surgery at Department of Conservative Dentistry, Seoul National University Dental Hospital from 2003 to 2005. The lesion were surgically removed and send for biopsy to the Oral Pathology Laboratory. From the initial radiograph, lesion size was calculated using PiViewSTAR® (INFINITT, Korea) program. The obtained data were statistically evaluated using SPSS (p < 0.05).
The result were as followings:
From 187 biopsy samples, the incidence of periapical cyst was 28.34% and granuloma was 65.24%.
There was a significant correlation between periapical cyst and the size of radiographic lesion (p < 0.01).
There were no significant correlations between age, gender, location of lesion and the final diagnosis (p > 0.05).
There was a significant correlation between the non-demarcation of the lesion and the incidence of periapical granuloma (p < 0.01).
- 1,977 View
- 17 Download

- The role of Type 2 Diabetes as a predisposing risk factor on the pulpo-periapical pathogenesis: review article
- Jin-Hee Kim, Kwang-shik Bae, Deog-Gyu Seo, Sung-Tae Hong, Yoon Lee, Sam-Pyo Hong, Kee-Yeon Kum
- J Korean Acad Conserv Dent 2009;34(3):169-176. Published online May 31, 2009
- DOI: https://doi.org/10.5395/JKACD.2009.34.3.169
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Diabetes Mellitus (DM) is a syndrome accompanied with the abnormal secretion or function of insulin, a hormone that plays a vital role in controlling the blood glucose level (BGL). Type 1and 2 DM are most common form and the prevalence of the latter is recently increasing. The aim of this article was to assess whether Type 2 DM could act as a predisposing risk factor on the pulpo-periapical pathogenesis. Previous literature on the pathologic changes of blood vessels in DM was thoroughly reviewed. Furthermore, a histopathologic analysis of artificially-induced periapical specimens obtained from Type 2 diabetic and DM-resistant rats was compared. Histopathologic results demonstrate that the size of periapical bone destruction was larger and the degree of pulpal inflammation was more severe in diabetic rats, indicating that Type 2 DM itself can be a predisposing risk factor that makes the host more susceptible to pulpal infection. The possible reasons may be that in diabetic state the lumen of pulpal blood vessels are thickened by atheromatous deposits, and microcirculation is hindered. The function of polymorphonuclear leukocyte is also impaired and the migration of immune cells is blocked, leading to increased chance of pulpal infection. Also, lack of collateral circulation of pulpal blood vessels makes the pulp more susceptible to infection. These decrease the regeneration capacity of pulpal cells or tissues, delaying the healing process. Therefore, when restorative treatment is needed in Type 2 DM patients, dentists should minimize irritation to the pulpal tissue un der control of BGL.
-
Citations
Citations to this article as recorded by- Pulp necrosis following luxated injury to teeth in a patient with uncontrolled type II diabetes mellitus: a case report
Haneol Shin, Seung-Jong Lee, Il-Young Jung, Chan-Young Lee
Restorative Dentistry & Endodontics.2012; 37(1): 61. CrossRef
- Pulp necrosis following luxated injury to teeth in a patient with uncontrolled type II diabetes mellitus: a case report
- 1,054 View
- 9 Download
- 1 Crossref

-
Reconsideration of treatment protocol on the reduction of
Enterococcus faecalis associated with failed root canal treatment - Woo Cheol Lee, Seong-Tae Hong, WonJun Shon
- J Korean Acad Conserv Dent 2008;33(6):560-569. Published online November 30, 2008
- DOI: https://doi.org/10.5395/JKACD.2008.33.6.560
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Microorganism survived in the root canal after root canal cleaning and shaping procedure is a main cause of root canal treatment failure. There are several mechanisms for the bacteria to survive in the root canal after chemomechanical preparation and root canal irrigation. Bacteria organized as biofilm has been suggested as an etiology of persistent periapical lesion. Recent studies were focus on removal of
Enterococcus faecalis biofilm due to the report that the persistence of this bacteria after root canal treatment may be associated with its ability to form biofilm. Several investigations demonstrated that current root canal treatment protocol including use of NaOCl, EDTA and Chlorhexidine as irrigants is quite effective in eliminatingE. faecalis biofilm. However, this microorganism still can survive in inaccessible areas of root canal system and evade host immune response, suppress immune activity and produce biofilm. Up to date, there is no possible clinical method to completely get rid of bacteria from the root canal. Once the root canal treatment failure occurred, and conventional treatment incorporating current therapeutic protocol has failed, periapical surgery or extraction should be considered rather than prolong the ineffected retreatment procedure.
- 1,001 View
- 4 Download

- Isolation and identification of bacteria from the root canal of the teeth diagnosed as the acute pulpitis and acute periapical abscess
- Yeon-Jae Lee, Mi-Kwang Kim, Ho-Keel Hwang, Joong-Ki Kook
- J Korean Acad Conserv Dent 2005;30(5):409-422. Published online September 30, 2005
- DOI: https://doi.org/10.5395/JKACD.2005.30.5.409
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub The aim of this study was to identify the bacteria isolated from acute endodontic lesions by cell culture and 16S rDNA sequencing. The necrotic pulpal tissue was collected from 17 infected root canals, which were diagnosed as being either an acute pulpitis or acute periapical abscess. Samples were collected aseptically from the infected pulpal tissue of the infected root canals using a barbed broach and a paper point. The cut barbed broaches and paper points were transferred to an eppendorf tube containing 500 ul of 1 X PBS. The sample solution was briefly mixed and plated onto a BHI-agar plate containing 5% sheep blood. The agar plates were incubated in a 37℃ anaerobic chamber for 7 days. The bacteria growing on the agar plate were identified by 16S rRNA coding gene (rDNA) cloning and sequencing at the species level. Among the 71 colonies grown on the agar plates, 56 strains survived and were identified. In dental caries involving the root canals,
Streptococcus spp. were mainly isolated.Actinomyces ,Clostridia ,Bacteroides andFusobacteria were isolated in the periapical lesion without dental caries. Interestingly, two newActinomyces spp. (ChDC B639 and ChDC B631) were isolated in this study. These results showed that there was diversity among the species in endodontic lesions. This suggests that an endodontic infection is a mixed infection with a polymicrobial etiology. These results may offer the bacterial strains for pathogenesis studies related to an endodontic infection.-
Citations
Citations to this article as recorded by- Microorganism penetration in dentinal tubules of instrumented and retreated root canal walls.In vitroSEM study
Saad Al-Nazhan, Alaa Al-Sulaiman, Fellwa Al-Rasheed, Fatimah Alnajjar, Bander Al-Abdulwahab, Abdulhakeem Al-Badah
Restorative Dentistry & Endodontics.2014; 39(4): 258. CrossRef - Microbial profile of asymptomatic and symptomatic teeth with primary endodontic infections by pyrosequencing
Sang-Min Lim, Tae-Kwon Lee, Eun-Jeong Kim, Jun-Hong Park, Yoon Lee, Kwang-Shik Bae, Kee-Yeon Kum
Journal of Korean Academy of Conservative Dentistry.2011; 36(6): 498. CrossRef
- Microorganism penetration in dentinal tubules of instrumented and retreated root canal walls.In vitroSEM study
- 1,260 View
- 10 Download
- 2 Crossref

- Diagnosis of periapical cemental dysplasia
- Soon-Young Lee, Chan-Young Lee, Byoung-Duck Roh
- J Korean Acad Conserv Dent 2005;30(1):66-71. Published online January 31, 2005
- DOI: https://doi.org/10.5395/JKACD.2005.30.1.066
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Periapical cemental dysplasia(PCD) is a condition most commonly seen in the mandibular incisor region. Radiographically it passes through the three phases(osteolytic stage, intermediate stage, and mature stage). At osteolytic stage, the lesion is similar to features associated with granuloma or cyst that arise following pulpal necrosis. So, it is important to confirm the vitality of the pulp to diagnosis.
In this case, it is difficult to confirm the vitality of involved tooth because the tooth was covered with PFG bridge. And it is unusual that the PCD lesion at mandibular incisors has occurred at first and the lesion of mandibular canine and mandibular premolar were occurred afterward.
- 1,450 View
- 10 Download

- Distribution of oral pathogens in infections of endodontic origin
- Seung-Yoon Kim, Ho-Young Choi, Sang-Hyuk Park, Gi-Woon Choi
- J Korean Acad Conserv Dent 2003;28(4):303-313. Published online July 31, 2003
- DOI: https://doi.org/10.5395/JKACD.2003.28.4.303
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub It has been documented that periodontopathic bacteria are also implicated in endodontic infections. 16S rDNA gene-directed PCR was to examine the prevalence of periodontopathic bacteria including
Actinobacillus actinomycetemcomitans (Aa ),Prevotella intermedia (Pi ),Prevotella nigrescens (Pn ),Porphyromonas gingivalis (Pg ),Porphyromonas endodontalis (Pe ), andTreponema denticola (Td ) in the root canals of 36 endodontically infected teeth having apical lesions with or without clinical symptoms like pain, swelling, and fistula.In 36 infected root canals, most frequently detected bacterial species was
Pg (61.1%), followed byTd (52.8%) andPe (38.9%).Of 36 infected root canals,
Aa was detected in 6 canals (16.7%) of the teeth, all of which showed clinical symptoms.Of 36 infected root canals,
Pi andPn were found in 4 (13.9%) and 5 (33.3%), respectively. Notably, prevalence ofPn in the symptomatic teeth was 50.0%.One of black-pigmented anaerobic bacteria (BPB) including
Pi ,Pn ,Pe , andPg was detected in all of the teeth that showed pain or especially swelling but not fistula. It was, however, found that prevalence of BPB in the asymptomatic teeth or the teeth with fistula was only 40%.Pe andPg were detected in the teeth regardless of the presence or absence of symptoms.Td was detected in the teeth regardless of the presence or absence of symptoms.High prevalence of BPB in the symptomatic teeth but low in the asymptomatic teeth suggests that BPB may play an important role in the pathogenesis of periapical lesions.
-
Citations
Citations to this article as recorded by- Isolation of Propionibacterium acnes among the microbiota of primary endodontic infections with and without intraoral communication
Sadia Ambreen Niazi, Hana Suleiman Al Kharusi, Shanon Patel, Kenneth Bruce, David Beighton, Federico Foschi, Francesco Mannocci
Clinical Oral Investigations.2016; 20(8): 2149. CrossRef - Antimicrobial Activity of Isothiocyanates (ITCs) Extracted from Horseradish (Armoracia rusticana) Root against Oral Microorganisms
HO-WON PARK, KYU-DUCK CHOI, IL-SHIK SHIN
Biocontrol Science.2013; 18(3): 163. CrossRef - Microbial profile of asymptomatic and symptomatic teeth with primary endodontic infections by pyrosequencing
Sang-Min Lim, Tae-Kwon Lee, Eun-Jeong Kim, Jun-Hong Park, Yoon Lee, Kwang-Shik Bae, Kee-Yeon Kum
Journal of Korean Academy of Conservative Dentistry.2011; 36(6): 498. CrossRef
- Isolation of Propionibacterium acnes among the microbiota of primary endodontic infections with and without intraoral communication
- 1,160 View
- 2 Download
- 3 Crossref


 KACD
KACD

 First
First Prev
Prev


