Articles
- Page Path
- HOME > Restor Dent Endod > Volume 39(3); 2014 > Article
- Case Report The use of platelet rich plasma in the treatment of immature tooth with periapical lesion: a case report
- Günseli Güven Polat1, Ceren Yıldırım1, Özlem Martı Akgün1, Ceyhan Altun1, Didem Dinçer2, Cansel Köse Özkan3
-
2014;39(3):-234.
DOI: https://doi.org/10.5395/rde.2014.39.3.230
Published online: June 2, 2014
1Department of Pediatric Dentistry, Center for Dental Sciences, Gulhane Medical Academy, Ankara, Turkey.
2Department of Dermatology, Gulhane Medical Academy, Ankara, Turkey.
3Center for Pharmaceutical Sciences, Gulhane Medical Academy, Ankara, Turkey.
- Correspondence to Günseli Güven Polat, DDS, PhD. Associate Professor, Department of Pediatric Dentistry, Gulhane Medical Academy, General Tevfik Saglam Cad. No:1, Ankara, Turkey. TEL, +903123046039; FAX, +903123046020; guvengunseli@gmail.com
• Received: January 22, 2014 • Accepted: April 23, 2014
©Copyights 2014. The Korean Academy of Conservative Dentistry.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 1,693 Views
- 8 Download
- 17 Crossref
Abstract
- This study describes the treatment of an immature permanent tooth with periapical lesion which was treated with regenerative approach using platelet rich plasma (PRP). The root canal of immature human permanent tooth with periapical lesion was gently debrided of necrotic tissue and disinfected with 2.5% NaOCl, and then medicated with triple antibiotic paste comprised of ciprofloxacin, metronidazole, and tetracycline. When the tooth was asymptomatic, PRP and mineral trioxide aggregate (MTA) were placed into the root canal. Six months after PRP treatment, radiographical examination revealed resolution of the radiolucency and progressive thickening of the root wall and apical closure. Our findings suggest that PRP can be used for the treatment of immature permanent teeth with periapical lesion, as part of a regenerative endodontic treatment procedure.
Introduction
Pulp necrosis, which eventually causes arrested root formation, is the most common complication in immature teeth. Immature teeth with apical periodontitis may be treated using several different procedures.1 Among these, calcium hydroxide was the most commonly used intracanal medicament for apexification that produced an apical barrier. However, it was found that long-term application of calcium hydroxide produces weaker dentinal walls and leaves the dentin more vulnerable to fractures.2,3 Alternative methods of endodontic regenerative procedures have been devised in order to allow root development in immature teeth with apical periodontitis.4,5 The aim of this procedure is to create and deliver new tissues to replace the necrotic pulp. There are two major concepts in the regenerative endodontics: tissue regeneration and tissue engineering.6 Tissue engineering is a procedure which utilizes specific stem cells, three dimensional scaffolds and growth factors to regenerate pulp-dentin complex.7 As for tissue regeneration, the procedures involves disinfection by irrigation solution, placement of three antibiotics into the root canal thus eliminating microorganisms from it, and revascularization of the pulp-dentin complex. Disinfection of root canal systems plays an important role in regeneration processes, promoting proliferation of the newly formed matrix and maintaining root development.8
Platelet rich plasma (PRP) is blood plasma that has been enriched with platelets. It contains various growth factors that are highly effective in promoting cell proliferation and differentiation.9 In the literature there are several case reports which use PRP in the treatment of tooth with necrotic pulp and open apex.10,11 This case report describes regenerative endodontic treatment using PRP in immature tooth with apical periodontitis.
Case report
10-year-old female patient was referred to the Department of Pediatric Dentistry complaining of swelling of the left permanent mandibular second premolar. Radiographic examination of this tooth revealed an open apex associated with a large radiolucency (Figure 1). According to intraoral examination, the tooth had enamel hypoplasia and caries. A buccal sinus tract was present, which traced to the apex of the tooth. Negative responses to electric pulp test (EPT) and cold sensivity test were recorded. Response to percussion and palpation were within normal limits. It was decided that the PRP procedure was appropriate in this case because positive results can be obtained in a short time using PRP. The procedure was explained to the parents and informed consent was obtained. A treatment plan was formulated which included the use of PRP as an internal matrix and mineral trioxide aggregate (MTA) as an apical barrier. The treatment plan was explained to the parents, and a customized informed consent form was subsequently signed.
The tooth was isolated with rubber dam under local anesthesia. The pulp tissue comprising approximately 1/3 of the root length of the tooth was removed mechanically, and the root canal was disinfected with 2.5% NaOCl. Root canal instrumentation was not performed, and the canal was dried with paper points followed with application of ciprofloxacin (Ciloxan, Alcon, Istanbul, Turkey), metronidazole (Roza, Orva, Izmir, Turkey), and tetracycline (Tetra, Mustafa Nevzat, Istanbul, Turkey). Access cavity was filled with glass ionomer cement (Ketac Nano Light-Curing Glass Ionomer Restorative, 3M ESPE, St. Paul, MN, USA) and light-cured for 20 seconds. The patient was followed up 2 weeks later, and the antibacterial paste was changed. The antibacterial paste was changed every 2 weeks until symptoms were subsided. At the 2-month recall, the tooth was asymptomatic and not sensitive to percussion or palpation.
The preparation of PRP was performed for the patient by the Department of Dermatology of our hospital 30 minutes prior to administration. First, the blood sample was collected into 10 mL tubes containing acid-citrate-dextrose solution. The citrated blood was then centrifuged promptly in a standard laboratory centrifuge for 15 minutes at 3,000 rpm. After the first spin, the lower red blood cell portion was discarded and the supernatant was again centrifuged for 5 minutes at 3,000 rpm. The resulting thrombocyte pellet resuspended in 1.0 mL of plasma constituted the PRP.
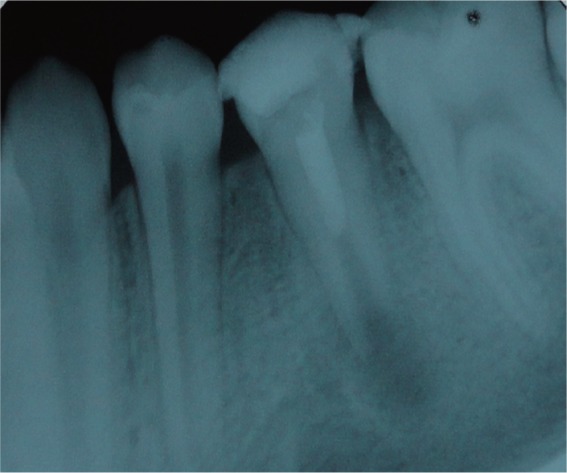
The root canal was irrigated with sterile saline solution and dried with sterile paper points under rubber dam isolation. Then, PRP was injected gently into the root canal to the level of cemento-enamel junction (CEJ) using an insulin syringe, and allowed to clot for 10 minutes. MTA (Pro-Root MTA, Dentsply Maillefer, Baillagues, Switzerland) was then placed into the root canal with a wet cotton pellet placed over. The cotton pellet was removed after 10 minutes. Glass ionomer cement was placed against the MTA, and adhesive (Excite DSC, Ivoclar Vivadent AG, Schaan, Liechtenstein) was applied according to the manufacturer's instructions. Finally, composite restoration was completed with Tetric Ceram (Ivoclar Vivadent AG) using the incremental technique, followed by occlusal adjustment (Figure 2). The patient was asymptomatic six months after the treatment. The radiographic presentation of the radiolucency was healed and the root continued to develop (Figure 3). At the 2-year recall, the root of the tooth was fully developed (Figure 4).
Discussion
One of the most serious potential complications of traumatic dental injury is pulp necrosis.12 Pulp necrosis of permanent immature teeth interrupts root formation and apical closure.13 Traditionally, the preferred method for treatment of immature permanent teeth with pulp necrosis has been apexification.14 The American Association of Endodontists defines apexification as a method to induce a calcified barrier in a root with an open apex or the continued apical development of an incomplete root in teeth with necrotic pulp.15 In the apexification procedure, calcium hydroxide, which was first introduced by Kaiser in 1964, has gained the widest acceptance for apical barrier formation.16,17 Recently, the regenerative procedures have been investigated for the treatment of immature permanent teeth due to the disadvantages associated with apexification procedures such as thin canal walls, discontinued root development, and vulnerability to fracture.6,17 According to the regenerative theory, if the canal space can be adequately disinfected and the coronal tooth structure is sealed to minimize bacterial contamination, regeneration is possible when a suitable matrix for new tissue growth exists.6 Successful results have been obtained in studies where this procedure has been applied.6,10,18,19 Petrino et al., Ding et al., and Torabinejad et al. reported resolution of periapical lesion, countinued root development, thickening of the dentinal walls and closure of apex following the regenerative procedures.10,18,19 In these studies, intracanal irrigants (NaOCl and chlorhexidine) and antibiotics such as the ciprofloxacin/metronidazole/minocycline paste described by Hoshio et al. were used for several weeks for the disinfection of immature teeth with apical periodontitis.6,18,19,20 In our case, a paste prepared using ciprofloxacin, metronidazole, and tetracycline was used for disinfection of root canal after irrigation with 2.5% NaOCl. The intracanal dressing was changed every 15 days for 2 months until tooth symptoms disappeared.
The tetracyclines represent a large group of antibacterials that were first discovered in the late 1940s which exhibit activity against a wide range of microorganisms including gram-positive and gram-negative bacteria, chlamydiae, mycoplasmas, rickettsiae, and protozoan parasites.21 In general, the tetracyclines can be divided into 3 groups on the basis of their pharmacokinetic and antibacterial properties. Group 1 (tetracycline, oxytetracycline, chlortetracycline etc.) consists of the older drugs, which have reduced absorption and lipophilicity as compared to the newer drugs in Group 2 (doxycycline, minocycline etc.). Group 2 drugs are almost completely absorbed, and are 3 - 5 times more lipophilic than Group 1 drugs. Group 3 includes the developmental compounds aminomethylcyclines.22 Although minocycline has a broader spectrum of activity as compared to other members of the group, we selected tetracycline instead of minocycline in the present case because it is easily available and affordable. It was found to be effective in our case. Kim et al., and Reynolds et al. used dentine bonding agents to seal the dentinal tubules of access cavity in order to prevent tooth discoloration resulting from use of minocycline/tetracycline.23,24 Also tooth discoloration might be reduced by using white MTA instead of grey MTA. This complication was not observed in our case.
MTA was first recommended as an artificial apical barrier by Torabinejad and Chivian in 1999.25 Since then MTA's popularity has grown steadily due to its high biocompatibility, highly alkaline pH (Bacteriostatic), excellent sealing ability, and low solubility. In most of the studies in which revascularization procedures were applied, MTA was preferred due to its sealing ability and biocompatibility.4,26 In the present case, MTA was placed into the root canal after PRP to obtain tight coronal seal as it is hydrophilic and needs moisture to set. This is a favorable property when there is potential moisture contamination in the clinical setting. Also MTA by itself provides signaling molecules for the growth of the stem cells.27 Platelets (or thrombocytes) are small, irregularly shaped clear cell fragments, which are derived from fragmentation of precursor megakaryocytes. They are a natural source of growth factors such as transforming growth factor, vascular endothelial growth factor, and platelet-derived growth factor.28 The use of platelet concentrates, particularly PRP and platelet rich fibrin (PRF) is a current treatment approach in oral and maxillofacial surgery, particularly in implant dentistry.29 The main purpose of the use of PRP is to increase the speed of healing of the soft and hard tissue.
In recent years, only one study has been conducted investigating the impact of PRP on the proliferation of pulpal cells. Liu et al. showed that PRP stimulates cell proliferation and differentiation of the dentin-pulp complex, which suggested that PRP could be used as a scaffold for pulp capping.30 Therefore, we believed that PRP can be used in the treatment of regenerative endodontic therapies. The use of PRP in immature teeth with periapical lesion has been firstly reported by Torabinejad and Turman, describing the case of an 11-year-old boy with a maxillary second premolar tooth with pulpal necrosis and symptomatic apical periodontitis.10 Torabinejad and Faras reported that regenaration of pulp-like tissue in a tooth root canal with the use of PRP in regenerative endodontic treatments.31 Jadhav et al. reported three cases that were followed-up clinically and radiographically at 6 and 12 months.32 According to the results of their study, there was a marked difference in periapical healing, apical closure and dentinal wall thickening of teeth treated by revascularization with PRP. In the case presented herein, only 2 months after PRP therapy, resolution of radiolucency and continued root development of the teeth were evident upon radiographic examination. The reason behind the success of the presented case may be that the PRP provokes proliferation of human dental pulp cells and increases the protein expression of osteoprotegerin (OPG) and alkaline phosphatase (ALP) activity. The potential diffuculty of using these procedure is the collecting of the blood sample, especially in children. For this reason, the procedure should be preferred to apply in cooperative children.
Conclusions
The results of our study suggest that PRP is a very effective preparation for use in regenerative endodontic therapies. Additionally, positive results can be obtained in a very short time. Although an observation in our case has extended to 2 years thus far, there is a need for long-term follow-up to observe whether or not any pathology will develop.
- 1. Fouad AF. The microbial challenge to pulp regeneration. Adv Dent Res 2011;23:285-289.ArticlePubMedPMCPDF
- 2. Gomes-Filho JE, Duarte PC, de Oliveira CB, Watanabe S, Lodi CS, Cintra LT, Bernabé PF. Tissue reaction to a triantibiotic paste used for endodontic tissue self-regeneration of nonvital immature permanent teeth. J Endod 2012;38:91-94.ArticlePubMed
- 3. Villat C, Grosgogeat B, Seux D, Farge P. Conservative approach of a symptomatic carious immature permanent tooth using a tricalcium silicate cement (Biodentine): a case report. Restor Dent Endod 2013;38:258-262.ArticlePubMedPMC
- 4. Banchs F, Trope M. Revascularization of immature permanent teeth with apical periodontitis: new treatment protocol? J Endod 2004;30:196-200.ArticlePubMed
- 5. Forghani M, Parisay I, Maghsoudlou A. Apexogenesis and revascularization treatment procedures for two traumatized immature permanent maxillary incisors: a case report. Restor Dent Endod 2013;38:178-181.ArticlePubMedPMC
- 6. Murray PE, Garcia-Godoy F, Hargreaves KM. Regenerative endodontics: a review of current status and a call for action. J Endod 2007;33:377-390.ArticlePubMed
- 7. Huang GT. Pulp and dentin tissue engineering and regeneration: current progress. Regen Med 2009;4:697-707.ArticlePubMed
- 8. Akgun OM, Altun C, Guven G. Use of triple antibiotic paste as a disinfectant for a traumatized immature tooth with a periapical lesion: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;108:e62-e65.ArticlePubMed
- 9. Ogino Y, Ayukawa Y, Kukita T, Koyano K. The contribution of platelet-derived growth factor, transforming growth factor-beta1, and insulin-like growth factor-I in platelet-rich plasma to the proliferation of osteoblast-like cells. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;101:724-729.PubMed
- 10. Torabinejad M, Turman M. Revitalization of tooth with necrotic pulp and open apex by using platelet-rich plasma: a case report. J Endod 2011;37:265-268.ArticlePubMed
- 11. Bezgin T, Yilmaz AD, Celik BN, Sönmez H. Concentrated platelet-rich plasma used in root canal revascularization: 2 case reports. Int Endod J 2014;47:41-49.ArticlePubMed
- 12. Andreasen FM. Pulpal healing following acute dental trauma: clinical and radiographic review. Pract Proced Aesthet Dent 2001;13:315-322.PubMed
- 13. Beslot-Neveu A, Bonte E, Baune B, Serreau R, Aissat F, Quinquis L, Grabar S, Lasfargues JJ. Mineral trioxide aggregate versus calcium hydroxide in apexification of non vital immature teeth: study protocol for a randomized controlled trial. Trials 2011;12:174.PubMedPMC
- 14. Chen MY, Chen KL, Chen CA, Tayebaty F, Rosenberg PA, Lin LM. Responses of immature permanent teeth with infected necrotic pulp tissue and apical periodontitis/abscess to revascularization procedures. Int Endod J 2012;45:294-305.ArticlePubMed
- 15. American Association of Endodontists. Glossary of endodontic terms. 7th ed. Chicago: American Association of Endodontists; 2003.
- 16. Walia T, Chawla HS, Gauba K. Management of wide open apices in non-vital permanent teeth with Ca(OH)2 paste. J Clin Pediatr Dent 2000;25:51-56.ArticlePubMedPDF
- 17. Rafter M. Apexification: a review. Dent Traumatol 2005;21:1-8.ArticlePubMed
- 18. Petrino JA, Boda KK, Shambarger S, Bowles WR, McClanahan SB. Challenges in regenerative endodontics: a case series. J Endod 2010;36:536-541.ArticlePubMed
- 19. Ding RY, Cheung GS, Chen J, Yin XZ, Wang QQ, Zhang CF. Pulp revascularization of immature teeth with apical periodontitis: a clinical study. J Endod 2009;35:745-749.ArticlePubMed
- 20. Hoshino E, Kurihara-Ando N, Sato I, Uematsu H, Sato M, Kota K, Iwaku M. In-vitro antibacterial susceptibility of bacteria taken from infected root dentine to a mixture of ciprofloxacin, metronidazole and minocycline. Int Endod J 1996;29:125-130.ArticlePubMed
- 21. Chopra I, Roberts M. Tetracycline antibiotics: mode of action, applications, molecular biology, and epidemiology of bacterial resistance. Microbiol Mol Biol Rev 2001;65:232-260.ArticlePubMedPMCPDF
- 22. Agwuh KN, MacGowan A. Pharmacokinetics and pharmacodynamics of the tetracyclines including glycylcyclines. J Antimicrob Chemother 2006;58:256-265.ArticlePubMed
- 23. Kim JH, Kim Y, Shin SJ, Park JW, Jung IY. Tooth discoloration of immature permanent incisor associated with triple antibiotic therapy: a case report. J Endod 2010;36:1086-1091.ArticlePubMed
- 24. Reynolds K, Johnson JD, Cohenca N. Pulp revascularization of necrotic bilateral bicuspids using a modified novel technique to eliminate potential coronal discoloration: a case report. Int Endod J 2009;42:84-92.PubMed
- 25. Torabinejad M, Chivian N. Clinical applications of mineral trioxide aggregate. J Endod 1999;25:197-205.ArticlePubMed
- 26. Cotti E, Mereu M, Lusso D. Regenerative treatment of an immature, traumatized tooth with apical periodontitis: report of a case. J Endod 2008;34:611-616.ArticlePubMed
- 27. Rudagi KB, Rudagi B. One-step apexification in immature tooth using grey mineral trioxide aggregate as an apical barrier and autologus platelet rich fibrin membrane as an internal matrix. J Conserv Dent 2012;15:196-199.ArticlePubMedPMC
- 28. Shivashankar VY, Johns DA, Vidyanath S, Kumar MR. Platelet rich fibrin in the revitalization of tooth with necrotic pulp and open apex. J Conserv Dent 2012;15:395-398.ArticlePubMedPMC
- 29. Hotwani K, Sharma K. Platelet rich fibrin - a novel acumen into regenerative endodontic therapy. Restor Dent Endod 2014;39:1-6.ArticlePubMedPMC
- 30. Liu ZN, Jiang T, Wang YX. Platelet-riched plasma promotes potential mineralizing capacity of human dental pulp cells in vivo. Beijing Da Xue Xue Bao 2011;43:276-279.PubMed
- 31. Torabinejad M, Faras H. A clinical and histological report of a tooth with an open apex treated with regenerative endodontics using platelet-rich plasma. J Endod 2012;38:864-868.ArticlePubMed
- 32. Jadhav GR, Shah N, Logani A. Comparative outcome of revascularization in bilateral, non-vital, immature maxillary anterior teeth supplemented with or without platelet rich plasma: a case series. J Conserv Dent 2013;16:568-572.ArticlePubMedPMC
REFERENCES
Tables & Figures
REFERENCES
Citations
Citations to this article as recorded by 

- Evaluation of postoperative pain and healing following regenerative endodontics using platelet‐rich plasma versus conventional endodontic treatment in necrotic mature mandibular molars with chronic periapical periodontitis. A randomized clinical trial
Yassmin Elsayed Ahmed, Geraldine Mohamed Ahmed, Angie Galal Ghoneim
International Endodontic Journal.2023; 56(4): 404. CrossRef - Different Approaches to the Regeneration of Dental Tissues in Regenerative Endodontics
Anna M. Krupińska, Katarzyna Skośkiewicz-Malinowska, Tomasz Staniowski
Applied Sciences.2021; 11(4): 1699. CrossRef - Coronal tooth discoloration induced by regenerative endodontic treatment using different scaffolds and intracanal coronal barriers: a 6-month ex vivo study
Noushin Shokouhinejad, Hassan Razmi, Maryam Farbod, Marzieh Alikhasi, Josette Camilleri
Restorative Dentistry & Endodontics.2019;[Epub] CrossRef - Efficacy of Autologous Platelet Concentrates in Regenerative Endodontic Treatment: A Systematic Review of Human Studies
Joanna Metlerska, Irini Fagogeni, Alicja Nowicka
Journal of Endodontics.2019; 45(1): 20. CrossRef - Bone, Periodontal and Dental Pulp Regeneration in Dentistry: A Systematic Scoping Review
Luiz Alexandre Chisini, Marcus Cristian Muniz Conde, Guillermo Grazioli, Alissa Schmidt San Martin, Rodrigo Varella de Carvalho, Letícia Regina Morello Sartori, Flávio Fernando Demarco
Brazilian Dental Journal.2019; 30(2): 77. CrossRef - Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview – part II: other clinical applications and complications
M. Torabinejad, M. Parirokh, P. M. H. Dummer
International Endodontic Journal.2018; 51(3): 284. CrossRef - Alternative to Avoid Tooth Discoloration after Regenerative Endodontic Procedure: A Systematic Review
Luciane Geanini Pena dos Santos, Luiz Alexandre Chisini, Camila Guerner Springmann, Beatriz Dulcineia Mendes de Souza, Fernanda Geraldo Pappen, Flávio Fernando Demarco, Mara Cristina Santos Felippe, Wilson Tadeu Felippe
Brazilian Dental Journal.2018; 29(5): 409. CrossRef - Influence of Apical Diameter on the Outcome of Regenerative Endodontic Treatment in Teeth with Pulp Necrosis: A Review
Yanjun Fang, Xinhuan Wang, Jingjing Zhu, Chaonan Su, Ying Yang, Liuyan Meng
Journal of Endodontics.2018; 44(3): 414. CrossRef - A scoping review of root canal revascularization: relevant aspects for clinical success and tissue formation
M. C. M. Conde, L. A. Chisini, R. Sarkis‐Onofre, H. S. Schuch, J. E. Nör, F. F. Demarco
International Endodontic Journal.2017; 50(9): 860. CrossRef - Effects of Epigallocatechin Gallate, an Antibacterial Cross-linking Agent, on Proliferation and Differentiation of Human Dental Pulp Cells Cultured in Collagen Scaffolds
Young-Sun Kwon, Hee-Jin Kim, Yun-Chan Hwang, Vinicius Rosa, Mi-Kyung Yu, Kyung-San Min
Journal of Endodontics.2017; 43(2): 289. CrossRef - Regenerative Endodontics
Kristina Feigin, Bonnie Shope
Journal of Veterinary Dentistry.2017; 34(3): 161. CrossRef - Regenerative Endodontic Treatment or Mineral Trioxide Aggregate Apical Plug in Teeth with Necrotic Pulps and Open Apices: A Systematic Review and Meta-analysis
Mahmoud Torabinejad, Ali Nosrat, Prashant Verma, Oyoyo Udochukwu
Journal of Endodontics.2017; 43(11): 1806. CrossRef - Platelet concentrates for revitalization of immature necrotic teeth: a systematic review of the clinical studies
Alessandra Lolato, Cristina Bucchi, Silvio Taschieri, Ahmed El Kabbaney, Massimo Del Fabbro
Platelets.2016; 27(5): 383. CrossRef - Regenerative endodontics—Creating new horizons
Harnoor Dhillon, Mamta Kaushik, Roshni Sharma
Journal of Biomedical Materials Research Part B: Applied Biomaterials.2016; 104(4): 676. CrossRef - The impact of autologous platelet concentrates on endodontic healing: a systematic review
Nastaran Meschi, Ana B. Castro, Katleen Vandamme, Marc Quirynen, Paul Lambrechts
Platelets.2016; 27(7): 613. CrossRef - Pulp and Periodontal Regeneration of an Avulsed Permanent Mature Incisor Using Platelet-rich Plasma after Delayed Replantation: A 12-month Clinical Case Study
Harini Priya M, Pavan B. Tambakad, Jaya Naidu
Journal of Endodontics.2016; 42(1): 66. CrossRef - Platelet preparations in dentistry: How? Why? Where? When?
Luigi Fabrizio Rodella
World Journal of Stomatology.2015; 4(2): 39. CrossRef
The use of platelet rich plasma in the treatment of immature tooth with periapical lesion: a case report
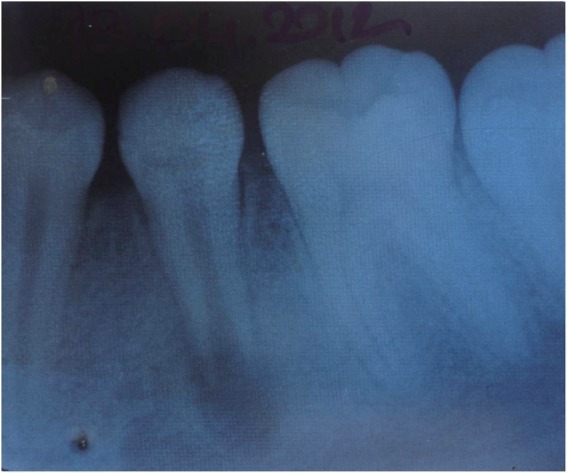
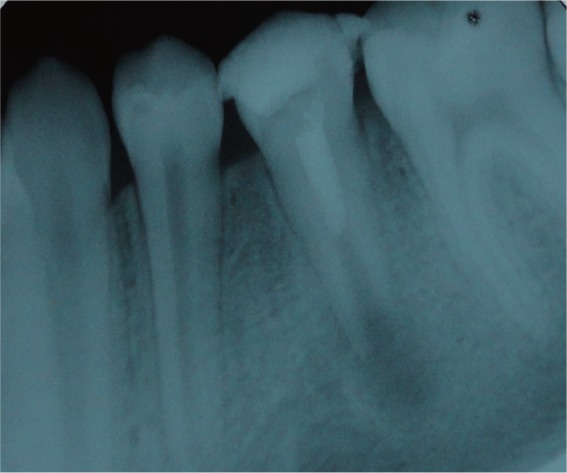


Figure 1 Periapical radiograph of the left permanent mandibular second premolar before treatment.
Figure 2 Immediate post-operative periapical radiograph of the left permanent mandibular second premolar.
Figure 3 Periapical radiograph of the left permanent mandibular second premolar six months after treatment.
Figure 4 Periapical radiograph of the left permanent mandibular second premolar two years after treatment.
Figure 1
Figure 2
Figure 3
Figure 4
The use of platelet rich plasma in the treatment of immature tooth with periapical lesion: a case report

 KACD
KACD



 ePub Link
ePub Link Cite
Cite

