Articles
- Page Path
- HOME > Restor Dent Endod > Volume 46(3); 2021 > Article
- Research Article Which factors related to apical radiolucency may influence its radiographic detection? A study using CBCT as reference standard
-
Rocharles Cavalcante Fontenele1
 , Eduarda Helena Leandro Nascimento2
, Eduarda Helena Leandro Nascimento2 , Hugo Gaêta-Araujo3
, Hugo Gaêta-Araujo3 , Laís Oliveira de Araujo Cardelli1
, Laís Oliveira de Araujo Cardelli1 , Deborah Queiroz Freitas1
, Deborah Queiroz Freitas1
-
Restor Dent Endod 2021;46(3):e43.
DOI: https://doi.org/10.5395/rde.2021.46.e43
Published online: July 21, 2021
1Department of Oral Diagnosis, Division of Oral Radiology, Piracicaba Dental School, University of Campinas, São Paulo, Brazil.
2Department of Dentistry, Oral Radiology area, Federal University of Sergipe, Sergipe, Brazil.
3Oral Radiology section, School of Dentistry, Federal University of Alfenas, Minas Gerais, Brazil.
- Correspondence to Rocharles Cavalcante Fontenele, DDS, MSc. PhD Student, Department of Oral Diagnosis, Division of Oral Radiology, Piracicaba Dental School, University of Campinas, Av. Limeira, 901, Piracicaba, São Paulo 13414-903, Brazil. rocharlesf@gmail.com
Copyright © 2021. The Korean Academy of Conservative Dentistry
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Objectives This study aimed to evaluate the detection rate of apical radiolucencies in 2-dimensional images using cone-beam computed tomography (CBCT) as the reference standard, and to determine which factors related to the apical radiolucencies and the teeth could influence its detection.
-
Materials and Methods The sample consisted of exams of patients who had panoramic (PAN) and/or periapical (PERI) radiography and CBCT. The exams were assessed by 2 oral radiologists and divided into PAN+CBCT (227 teeth–285 roots) and PERI+CBCT (94 teeth–115 roots). Radiographic images were evaluated for the presence of apical radiolucency, while CBCT images were assessed for presence, size, location, and involvement of the cortical bone (thinning, expansion, and destruction). Diagnostic values were obtained for PERI and PAN.
-
Results PERI and PAN presented high accuracy (0.83 and 0.77, respectively) and specificity (0.89 and 0.91, respectively), but low sensitivity, especially for PAN (0.40 vs. 0.65 of PERI). The size of the apical radiolucency was positively correlated with its detection in PERI and PAN (p < 0.001). For PAN, apical radiolucencies were 3.93 times more frequently detected when related to single-rooted teeth (p = 0.038). The other factors did not influence apical radiolucency detection (p > 0.05).
-
Conclusions PERI presents slightly better accuracy than PAN for the detection of apical radiolucency. The size is the only factor related to radiolucency that influences its detection, for both radiographic exams. For PAN, apical radiolucency is most often detected in single-rooted teeth.
INTRODUCTION
MATERIALS AND METHODS
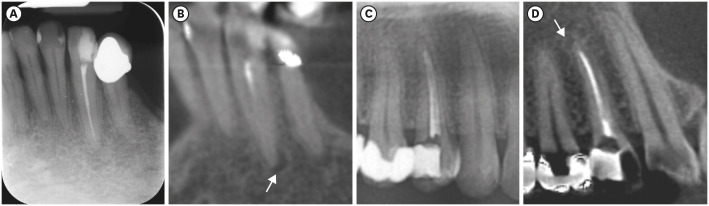
Images of PERI+CBCT and PAN+CBCT groups evaluated. Lower left canine in PERI (A) and CBCT coronal reconstruction (B). An upper right first premolar observed in cropped PAN (C) and CBCT sagittal reconstruction (D). Arrows indicate the apical radiolucencies detected in CBCT reconstructions.
Distribution of the study sample according to each image group
RESULTS
Detection of apical radiolucency on PERI and PAN images compared with CBCT images (reference standard)
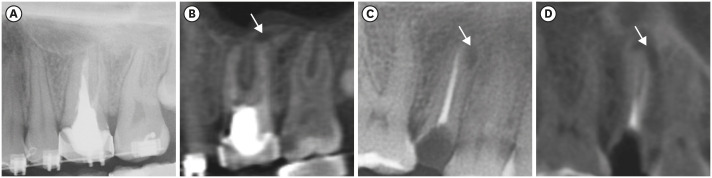
An apical radiolucency in a multi-rooted tooth that was not detected in PAN (A), but detected in the CBCT sagittal reconstruction, indicated by the arrow (B). The arrows are indicating an apical radiolucency detected on both PAN (C) and CBCT sagittal reconstruction (D) of a single-root tooth.
Diagnostic tests of accuracy, sensitivity, specificity, PPV and NPV for PERI and PAN images
| Variables | Accuracy | Sensitivity | Specificity | PPV | NPV |
|---|---|---|---|---|---|
| PERI | 0.83 | 0.65 | 0.89 | 0.63 | 0.90 |
| PAN | 0.77 | 0.40 | 0.91 | 0.63 | 0.80 |
Binomial logistic regression detailing the possible factors that influence the detection of apical radiolucency on PERI and PAN images
DISCUSSION
CONCLUSIONS
-
Funding: This study was financed in part by PIBIC/CNPq (National Council for Scientific and Technological Development) and the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001.
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Fontenele RC, Nascimento EHL, Freitas DQ.
Data curation: Gaêta-Araujo H, Cardelli LOA.
Formal analysis: Fontenele RC, Nascimento EHL, Freitas DQ.
Funding acquisition: Fontenele RC, Nascimento EHL, Gaêta-Araujo H, Freitas DQ.
Investigation: Fontenele RC, Nascimento EHL, Gaêta-Araujo H, Freitas DQ.
Methodology: Fontenele RC, Nascimento EHL, Freitas DQ.
Project administration: Fontenele RC, Nascimento EHL, Freitas DQ.
Resources: Fontenele RC, Freitas DQ.
Software: Gaêta-Araujo H, Cardelli LOA, Freitas DQ.
Supervision: Freitas DQ.
Validation: Fontenele RC, Nascimento EHL, Freitas DQ.
Visualization: Fontenele RC, Nascimento EHL, Gaêta-Araujo H, Freitas DQ.
Writing - original draft: Fontenele RC, Nascimento EHL, Gaêta-Araujo H, Cardelli LOA, Freitas DQ.
Writing - review & editing: Freitas DQ.
- 1. Estrela C, Bueno MR, Azevedo BC, Azevedo JR, Pécora JD. A new periapical index based on cone beam computed tomography. J Endod 2008;34:1325-1331.ArticlePubMed
- 2. Estrela C, Bueno MR, Leles CR, Azevedo B, Azevedo JR. Accuracy of cone beam computed tomography and panoramic and periapical radiography for detection of apical periodontitis. J Endod 2008;34:273-279.ArticlePubMed
- 3. de Freitas JV, Baratto-Filho F, Coelho BS, Tomazinho FSF, Crozeta BM, de Sousa Neto MD, Gabardo MCL. Efficacy of different cone-beam computed tomographic protocols in the identification of mesiobuccal canals of maxillary first molars: a tomographic and ex vivo study. J Endod 2017;43:810-815.ArticlePubMed
- 4. Patel S. New dimensions in endodontic imaging: part 2. Cone beam computed tomography. Int Endod J 2009;42:463-475.ArticlePubMed
- 5. Moura MS, Guedes OA, De Alencar AH, Azevedo BC, Estrela C. Influence of length of root canal obturation on apical periodontitis detected by periapical radiography and cone beam computed tomography. J Endod 2009;35:805-809.ArticlePubMed
- 6. Durack C, Patel S. Cone beam computed tomography in endodontics. Braz Dent J 2012;23:179-191.ArticlePubMed
- 7. Patel S, Brown J, Pimentel T, Kelly RD, Abella F, Durack C. Cone beam computed tomography in endodontics - a review of the literature. Int Endod J 2019;52:1138-1152.ArticlePubMedPDF
- 8. Pope O, Sathorn C, Parashos P. A comparative investigation of cone-beam computed tomography and periapical radiography in the diagnosis of a healthy periapex. J Endod 2014;40:360-365.ArticlePubMed
- 9. Nardi C, Calistri L, Pradella S, Desideri I, Lorini C, Colagrande S. Accuracy of orthopantomography for apical periodontitis without endodontic treatment. J Endod 2017;43:1640-1646.ArticlePubMed
- 10. Nardi C, Calistri L, Grazzini G, Desideri I, Lorini C, Occhipinti M, Mungai F, Colagrande S. Is panoramic radiography an accurate imaging technique for the detection of endodontically treated asymptomatic apical periodontitis? J Endod 2018;44:1500-1508.ArticlePubMed
- 11. Esposito S, Cardaropoli M, Cotti E. A suggested technique for the application of the cone beam computed tomography periapical index. Dentomaxillofac Radiol 2011;40:506-512.ArticlePubMedPMC
- 12. Kapila R, Harada N, Araki K, Sano T, Goto TK. Evaluation of juxta-apical radiolucency in cone beam CT images. Dentomaxillofac Radiol 2014;43:20130402.ArticlePubMedPMC
- 13. Patel S, Wilson R, Dawood A, Foschi F, Mannocci F. The detection of periapical pathosis using digital periapical radiography and cone beam computed tomography - part 2: a 1-year post-treatment follow-up. Int Endod J 2012;45:711-723.ArticlePubMed
- 14. Davies A, Mannocci F, Mitchell P, Andiappan M, Patel S. The detection of periapical pathoses in root filled teeth using single and parallax periapical radiographs versus cone beam computed tomography - a clinical study. Int Endod J 2015;48:582-592.ArticlePubMed
- 15. López FU, Kopper PM, Cucco C, Della Bona A, de Figueiredo JA, Vier-Pelisser FV. Accuracy of cone-beam computed tomography and periapical radiography in apical periodontitis diagnosis. J Endod 2014;40:2057-2060.ArticlePubMed
- 16. Kanagasingam S, Lim CX, Yong CP, Mannocci F, Patel S. Diagnostic accuracy of periapical radiography and cone beam computed tomography in detecting apical periodontitis using histopathological findings as a reference standard. Int Endod J 2017;50:417-426.ArticlePubMedPDF
- 17. Abella F, Patel S, Durán-Sindreu F, Mercadé M, Bueno R, Roig M. An evaluation of the periapical status of teeth with necrotic pulps using periapical radiography and cone-beam computed tomography. Int Endod J 2014;47:387-396.ArticlePubMed
- 18. Kanagasingam S, Hussaini HM, Soo I, Baharin S, Ashar A, Patel S. Accuracy of single and parallax film and digital periapical radiographs in diagnosing apical periodontitis - a cadaver study. Int Endod J 2017;50:427-436.ArticlePubMedPDF
- 19. Kruse C, Spin-Neto R, Wenzel A, Kirkevang LL. Cone beam computed tomography and periapical lesions: a systematic review analysing studies on diagnostic efficacy by a hierarchical model. Int Endod J 2015;48:815-828.ArticlePubMed
- 20. Bender IB. Factors influencing the radiographic appearance of bony lesions. J Endod 1997;23:5-14.ArticlePubMed
- 21. Bender IB, Seltzer S. Roentgenographic and direct observation of experimental lesions in bone: II. 1961. J Endod 2003;29:707-712.PubMed
REFERENCES
Tables & Figures
REFERENCES
Citations

- Radiomics-based classification of pediatric dental trauma in periapical radiographs: a preliminary study
Mengtian Peng, Bin Yu, Juan Hu, Xiaoxin Xie, Jihong He
BMC Medical Imaging.2025;[Epub] CrossRef - Increasing Diagnostic Acumen in Endodontics
Shilpa Thakkar, Dana Mominkhan
Dental Clinics of North America.2025; 69(4): 479. CrossRef - Three-dimensional clinical assessment for MRONJ risk in oncologic patients following tooth extractions
Catalina Moreno Rabie, Rocharles Cavalcante Fontenele, Nicolly Oliveira Santos, Fernanda Nogueira Reis, Tim Van den Wyngaert, Reinhilde Jacobs
Dentomaxillofacial Radiology.2023;[Epub] CrossRef - Quality of techniques used to assess clinical outcomes of regenerative endodontic treatment in necrotic mature teeth
Roy George
Evidence-Based Dentistry.2022; 23(3): 98. CrossRef
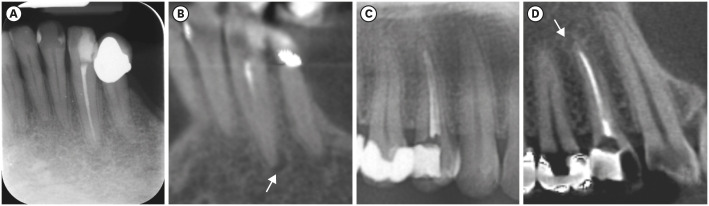
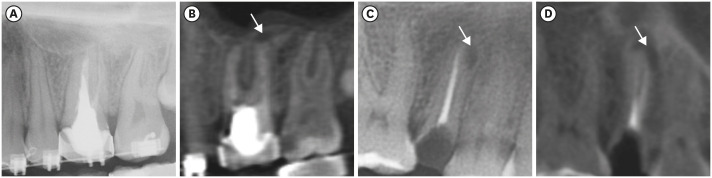
Figure 1
Figure 2
Distribution of the study sample according to each image group
| Image group | Dental arch | Region | Number of teeth (%) |
|---|---|---|---|
| PERI+CBCT | Maxilla | Anterior | 28 (29.8) |
| Posterior | 19 (20.2) | ||
| Mandible | Anterior | 28 (29.8) | |
| Posterior | 19 (20.2) | ||
| PAN+CBCT | Maxilla | Anterior | 47 (20.7) |
| Posterior | 63 (27.8) | ||
| Mandible | Anterior | 47 (20.7) | |
| Posterior | 70 (30.8) |
CBCT, cone-beam computed tomography; PAN, panoramic radiograph; PERI, periapical radiograph.
Detection of apical radiolucency on PERI and PAN images compared with CBCT images (reference standard)
| Variables | CBCT | p value* | |||
|---|---|---|---|---|---|
| Absence | Present | Total | |||
| PERI | |||||
| Absence | 79 (88.8) | 9 (34.6) | 88 (76.5) | < 0.001 | |
| Presence | 10 (11.2) | 17 (65.4) | 27 (23.5) | ||
| Total | 89 (77.4) | 26 (22.6) | 115 (100.0) | ||
| PAN | |||||
| Absence | 189 (91.3) | 47 (60.3) | 236 (82.8) | < 0.001 | |
| Presence | 18 (8.7) | 31 (39.7) | 49 (17.2) | ||
| Total | 207 (72.6) | 78 (27.4) | 285 (100.0) | ||
Bold numbers indicate agreement between imaging modalities.
CBCT, cone-beam computed tomography; PAN, panoramic radiograph; PERI, periapical radiograph.
*According to Pearson's χ2 test.
Diagnostic tests of accuracy, sensitivity, specificity, PPV and NPV for PERI and PAN images
| Variables | Accuracy | Sensitivity | Specificity | PPV | NPV |
|---|---|---|---|---|---|
| PERI | 0.83 | 0.65 | 0.89 | 0.63 | 0.90 |
| PAN | 0.77 | 0.40 | 0.91 | 0.63 | 0.80 |
NPV, negative predictive value; PAN, panoramic radiograph; PERI, periapical radiograph; PPV, positive predictive value.
Binomial logistic regression detailing the possible factors that influence the detection of apical radiolucency on PERI and PAN images
| Variables | Estimate | SE | Wald χ2 | p value | OR | 95% CI (min–max) | ||
|---|---|---|---|---|---|---|---|---|
| PERI | ||||||||
| Localization and tooth morphology | ||||||||
| Maxillary or mandibular | 1.467 | 0.913 | 2.581 | 0.108 | 4.33 | (0.72–25.94) | ||
| Anterior or posterior | −1.503 | 1.093 | 1.89 | 0.169 | 0.22 | (0.26–1.89) | ||
| Single- or multi-rooted | 1.051 | 1.152 | 0.832 | 0.362 | 2.86 | (0.29–27.37) | ||
| Apical radiolucency size | 19.152 | < 0.001 | ||||||
| Score 1 | 3.18 | 1.262 | 6.352 | 0.012 | 24.05 | (2.03–285.27) | ||
| Score 2 | 2.377 | 0.761 | 9.744 | 0.002 | 10.77 | (2.42–47.92) | ||
| Score 3 | 3.68 | 1.393 | 6.981 | 0.008 | 39.64 | (2.59–607.44) | ||
| Cortical thinning | 0.00 | 1.000 | ||||||
| Score 1 | 42.033 | 46,176.01 | 0.00 | 0.999 | - | (0.00) | ||
| Score 3 | 62.95 | 61,218.45 | 0.00 | 0.999 | - | (0.00) | ||
| Cortical expansion | −20.410 | 27,670.73 | 0.00 | 0.999 | 0.00 | (0.00) | ||
| Cortical destruction | −20.092 | 22,732.18 | 0.00 | 0.999 | 0.00 | (0.00) | ||
| PAN | ||||||||
| Localization and tooth morphology | ||||||||
| Maxillary or mandibular | −0.632 | 0.383 | 2.718 | 0.099 | 0.53 | (0.25–1.13) | ||
| Anterior or posterior | 0.211 | 0.855 | 0.061 | 0.805 | 1.24 | (0.23–6.59) | ||
| Single- or multi-rooted | −1.641 | 0.791 | 4.3 | 0.038 | 3.93 | (0.04–0.91) | ||
| Apical radiolucency size | 9.092 | 0.028 | ||||||
| Score 1 | 1.495 | 0.716 | 4.356 | 0.037 | 4.46 | (1.1–18.14) | ||
| Score 2 | 2.607 | 0.886 | 8.668 | 0.003 | 13.6 | (2.39–76.92) | ||
| Score 3 | 1.768 | 0.83 | 4.538 | 0.033 | 5.86 | (1.15–29.8) | ||
| Cortical thinning | 1.114 | 0.774 | ||||||
| Score 1 | −0.456 | 1.281 | 0.127 | 0.722 | 0.63 | (0.51–7.81) | ||
| Score 2 | 1.008 | 1.674 | 0.362 | 0.547 | 2.74 | (0.1–72.94) | ||
| Score 3 | −21.969 | 17,416.11 | 0.00 | 0.999 | 0.00 | (0.00) | ||
| Cortical expansion | −21.119 | 22,939.57 | 0.00 | 0.999 | 0.00 | (0.00) | ||
| Cortical destruction | 0.819 | 1.176 | 0.485 | 0.486 | 2.27 | (0.23–22.72) | ||
OR, odds ratio; CI, confidence interval; PAN, panoramic radiograph; PERI, periapical radiograph; SE, standard error.
CBCT, cone-beam computed tomography; PAN, panoramic radiograph; PERI, periapical radiograph.
Bold numbers indicate agreement between imaging modalities.
CBCT, cone-beam computed tomography; PAN, panoramic radiograph; PERI, periapical radiograph.
*According to Pearson's χ2 test.
NPV, negative predictive value; PAN, panoramic radiograph; PERI, periapical radiograph; PPV, positive predictive value.
OR, odds ratio; CI, confidence interval; PAN, panoramic radiograph; PERI, periapical radiograph; SE, standard error.

 KACD
KACD
 ePub Link
ePub Link Cite
Cite

