Search
- Page Path
- HOME > Search
- Evaluation of platelet concentrates in regenerative endodontics: a systematic review and meta-analysis
- Anna Tsiolaki, Dimitrios Theocharis, Nikolaos Tsitsipas, Anastasia Fardi, Konstantinos Kodonas
- Restor Dent Endod 2025;50(4):e38. Published online November 28, 2025
- DOI: https://doi.org/10.5395/rde.2025.50.e38
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - Objectives
The aim of this systematic review is to compare the effectiveness of advanced platelet concentrates as regenerative endodontic therapeutic alternatives to blood clot (BC) revascularization in immature permanent necrotic teeth.
Methods
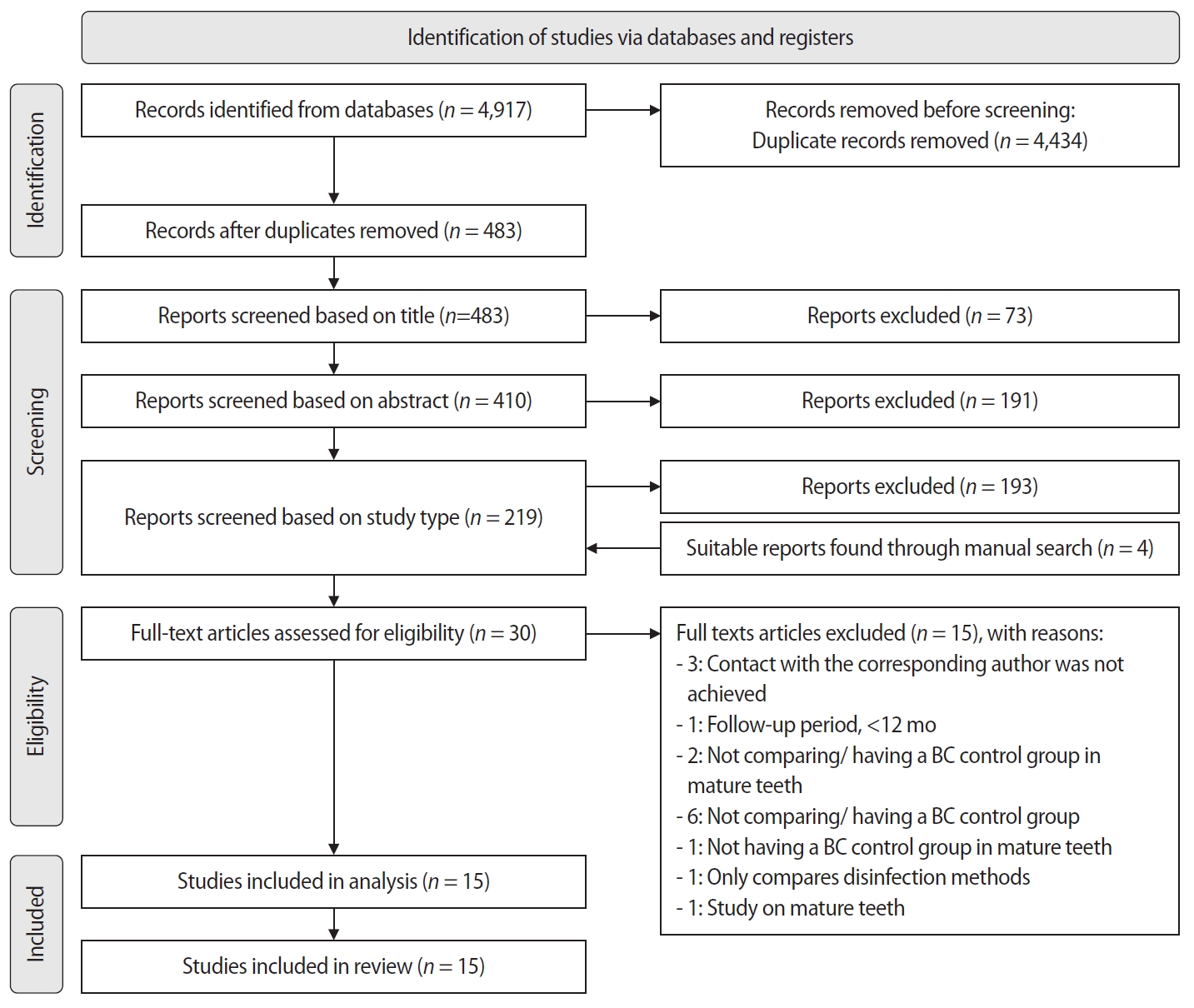
Randomized controlled trials (RCTs) comparing regenerative endodontic therapies using platelet-rich plasma (PRP), platelet-rich fibrin (PRF), or platelet pellet (PP) with the BC revascularization approach in immature permanent necrotic teeth were systematically searched in PubMed, Scopus, Cochrane Library, and Web of Science until May 2025. Data was extracted and analyzed both qualitatively and quantitatively. Study quality was assessed using the Cochrane Risk of Bias tool. A meta-analysis was conducted using IBM SPSS software (version 29.0), with success rates expressed as risk ratios and 95% confidence intervals (CIs).
Results
The initial search yielded 4,917 studies. After removing duplicates and applying eligibility criteria, 15 RCTs were included. Meta-analysis indicated no significant difference in the risk ratio (RR), as the BC method has similar success rates with PRP (10 studies; RR = 1.01; 95% CI, 0.94–1.09; p = 0.76) and PRF (8 studies; RR = 0.98; 95% CI, 0.89–1.08; p = 0.65) at 12 months. The primary outcomes evaluated were based on clinical and radiographic success.
Conclusions
Current evidence suggests PRP, PRF, and BC are all effective in treating immature permanent necrotic teeth with similar success rates. However, further research is needed to assess long-term outcomes.
- 878 View
- 50 Download

- Stem cell-derived exosomes for dentin-pulp complex regeneration: a mini-review
- Dina A. Hammouda, Alaa M Mansour, Mahmoud A. Saeed, Ahmed R. Zaher, Mohammed E. Grawish
- Restor Dent Endod 2023;48(2):e20. Published online May 3, 2023
- DOI: https://doi.org/10.5395/rde.2023.48.e20
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub This mini-review was conducted to present an overview of the use of exosomes in regenerating the dentin-pulp complex (DPC). The PubMed and Scopus databases were searched for relevant articles published between January 1, 2013 and January 1, 2023. The findings of basic
in vitro studies indicated that exosomes enhance the proliferation and migration of mesenchymal cells, as human dental pulp stem cells, via mitogen-activated protein kinases and Wingless-Int signaling pathways. In addition, they possess proangiogenic potential and contribute to neovascularization and capillary tube formation by promoting endothelial cell proliferation and migration of human umbilical vein endothelial cells. Likewise, they regulate the migration and differentiation of Schwann cells, facilitate the conversion of M1 pro-inflammatory macrophages to M2 anti-inflammatory phenotypes, and mediate immune suppression as they promote regulatory T cell conversion. Basicin vivo studies have indicated that exosomes triggered the regeneration of dentin-pulp–like tissue, and exosomes isolated under odontogenic circumstances are particularly strong inducers of tissue regeneration and stem cell differentiation. Exosomes are a promising regenerative tool for DPC in cases of small pulp exposure or for whole-pulp tissue regeneration.-
Citations
Citations to this article as recorded by- Extracellular vesicles derived from dental mesenchymal stem cells for regenerative medicine: a scoping review
Maria Emília Mota, Márcia Martins Marques, Thaís Gimenez, Suely Kunimi Kubo Ariga, Tiago Góss dos Santos, Fábio Abreu Alves, Maria Stella Moreira
Molecular Biology Reports.2026;[Epub] CrossRef - Cell Homing Strategies in Regenerative Endodontic Therapy
David Kim, Sahng G. Kim
Cells.2025; 14(3): 201. CrossRef - Impact of dental pulp cells-derived small extracellular vesicles on the properties and behavior of dental pulp cells: an in-vitro study
Dina A. Hammouda, Alaa M. Mansour, Ahmed R. Zaher, Mohammed E. Grawish
BMC Oral Health.2025;[Epub] CrossRef - Methodological Approaches for Economic Comparison of Mesenchymal Stem Cell and Exosome-based Therapies with Conventional Endodontic Treatments in Regenerative Endodontics
Madina A. Kurmanalina Kurmanalina, Nadiar M. Mussin, Aigul M. Sumanova, Violetta R. Detochkina, Maryam Mardani, Nader Tanideh, Amin Tamadon
West Kazakhstan Medical Journal.2025; 67(2): 188. CrossRef - Exosomal circ_0003057 promotes osteo/odontogenic differentiation of hDPSCs by binding with EIF4A3 through upregulated parental gene ANKH
Bingtao Wang, Yuanyuan Kong, Huixian Dong, Feng Lai, Zixin Guo, Liecong Lin, Jingyi Xu, Jingkun Zhang, Yiguo Jiang, Qianzhou Jiang
International Endodontic Journal.2025; 58(9): 1433. CrossRef - Mechanistic insights into dental stem cells‐derived exosomes in regenerative endodontics
Paras Ahmad, Nathan Estrin, Nima Farshidfar, Yufeng Zhang, Richard J. Miron
International Endodontic Journal.2025; 58(9): 1384. CrossRef - Development and characterization of an exosome-loaded biomimetic hydroxyapatite/gelatin scaffold for enhanced dental pulp regeneration
Yuen-Shan Tsai, Shih-Jung Cheng, Tsao-Li Chuang, Shu-Fang Chang, Feng-Huei Lin, Chun-Pin Lin
Journal of Dental Sciences.2025;[Epub] CrossRef - Exosomes as Promising Therapeutic Tools for Regenerative Endodontic Therapy
Qingyue Kong, Yujie Wang, Nan Jiang, Yifan Wang, Rui Wang, Xiaohan Hu, Jing Mao, Xin Shi
Biomolecules.2024; 14(3): 330. CrossRef - Role and Molecular Mechanism of miR-586 in the Differentiation of Dental Pulp Stem Cells into Odontoblast-like Cells
Gang Pan, Qianwen Zhou, Chenhua Pan, Yingxue Zhang
Cell Biochemistry and Biophysics.2024; 83(1): 507. CrossRef
- Extracellular vesicles derived from dental mesenchymal stem cells for regenerative medicine: a scoping review
- 4,714 View
- 94 Download
- 8 Web of Science
- 9 Crossref

- Dentinal tubule penetration of sodium hypochlorite in root canals with and without mechanical preparation and different irrigant activation methods
- Renata Aqel de Oliveira, Theodoro Weissheimer, Gabriel Barcelos Só, Ricardo Abreu da Rosa, Matheus Albino Souza, Rodrigo Gonçalves Ribeiro, Marcus Vinicius Reis Só
- Restor Dent Endod 2023;48(1):e1. Published online December 1, 2022
- DOI: https://doi.org/10.5395/rde.2023.48.e1
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives This study evaluated the dentinal penetration depth of 2.5% sodium hypochlorite (NaOCl) in root canals with and without preparation and different irrigant activation protocols.
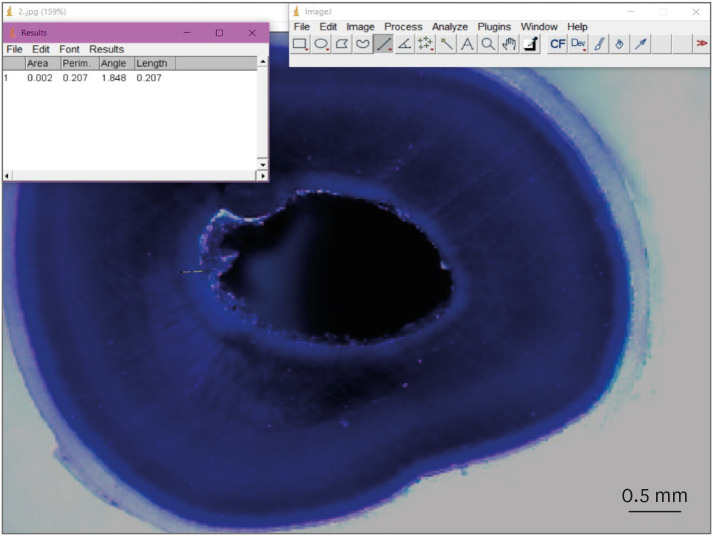
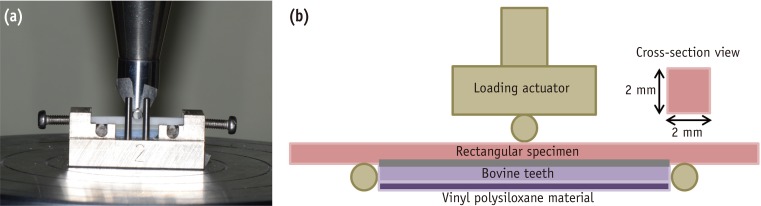
Materials and Methods Sixty-three bovine mandibular incisors were randomly allocated to 6 groups (
n = 10): G1, preparation + conventional needle irrigation (CNI); G2, preparation + passive ultrasonic irrigation (PUI); G3, preparation + Odous Clean (OC); G4, no preparation + CNI; G5, no preparation + PUI; G6, no preparation + OC; and CG (negative control;n = 3). Samples were filled with crystal violet for 72 hours. Irrigant activation was performed. Samples were sectioned perpendicularly along the long axis, 3 mm and 7 mm from the apex. Images of the root thirds of each block were captured with a stereomicroscope and analyzed with an image analysis software. One-way analysis of variance, followed by the Tukeypost hoc test, and the Student’st -test were used for data analysis, with a significance level of 5%.Results The NaOCl penetration depth was similar when preparation was performed, regardless of the method of irrigation activation (
p > 0.05). In the groups without preparation, G6 showed greater NaOCl penetration depth (p < 0.05). The groups without preparation had a greater NaOCl penetration depth than those with preparation (p = 0.0019).Conclusions The NaOCl penetration depth was similar in groups with root canal preparation. Without root canal preparation, OC allowed deeper NaOCl penetration. The groups without preparation had greater NaOCl penetration than those undergoing root canal preparation.
-
Citations
Citations to this article as recorded by- Novel approaches involving curcumin in endodontic and periodontal diseases: a scoping review
Yuxi Xing, Yanbing Zhu, Yukai Shen, Yuou Xu, Ziman Xu, Mengxue Wang, Xudong Ma, Lehua Liu, Shu Chen
BMC Oral Health.2026;[Epub] CrossRef - Influence of passive ultrasonic irrigation cycles on the penetration depth of sodium hypochlorite into root dentin
Hüseyin Gündüz, Esin Özlek, Züleyha Baş
Scientific Reports.2025;[Epub] CrossRef - Evaluating the Effects of Various Antioxidants on Dentinal Tubule Penetrability of a Resin-Based Sealer: A Confocal Laser Microscopic Study
Sanjeev Srivastava, Shijita Sinha, Abhishek Singh, Aditya Singh, Pragyan Paliwal, Syed H Mehdii
Cureus.2025;[Epub] CrossRef - Impact of different activation procedures on sodium hypochlorite penetration into dentinal tubules after endodontic retreatment via confocal laser scanning microscopy
Betul Gunes, Kübra Yeşildal Yeter, Yasin Altay
BMC Oral Health.2024;[Epub] CrossRef - Debridement ability of the WaveOne Gold and TruNatomy systems in the apical third of root canals: ex vivo assessment
Sara Carvalho Avelar de Oliveira, Carlos Eduardo da Silveira Bueno, Rina Andréa Pelegrine, Carlos Eduardo Fontana, Alexandre Sigrist de Martin, Carolina Pessoa Stringheta
Brazilian Dental Journal.2024;[Epub] CrossRef - Combined effect of electrical energy and graphene oxide on Enterococcus faecalis biofilms
Myung-Jin LEE, Mi-Ah KIM, Kyung-San MIN
Dental Materials Journal.2023; 42(6): 844. CrossRef
- Novel approaches involving curcumin in endodontic and periodontal diseases: a scoping review
- 2,369 View
- 63 Download
- 4 Web of Science
- 6 Crossref

- Evaluation of blood clot, platelet-rich plasma, and platelet-rich fibrin–mediated regenerative endodontic procedures in teeth with periapical pathology: a CBCT study
- Swati Markandey, Haridas Das Adhikari
- Restor Dent Endod 2022;47(4):e41. Published online October 21, 2022
- DOI: https://doi.org/10.5395/rde.2022.47.e41
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
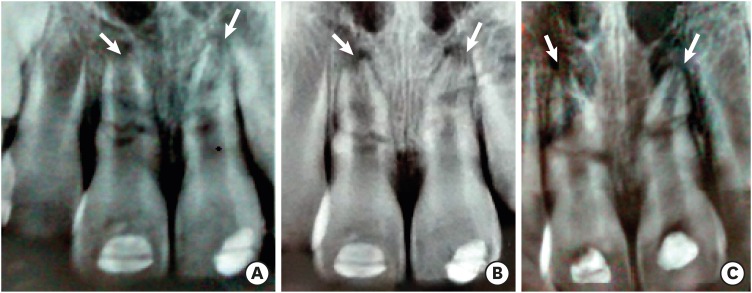
ePub Objectives This study compared the clinical and radiological outcomes of regenerative endodontic procedures (REPs) using blood clots (BCs), platelet-rich plasma (PRP), and platelet-rich fibrin (PRF) through intraoral periapical radiography (IOPAR) and cone-beam computed tomography (CBCT).
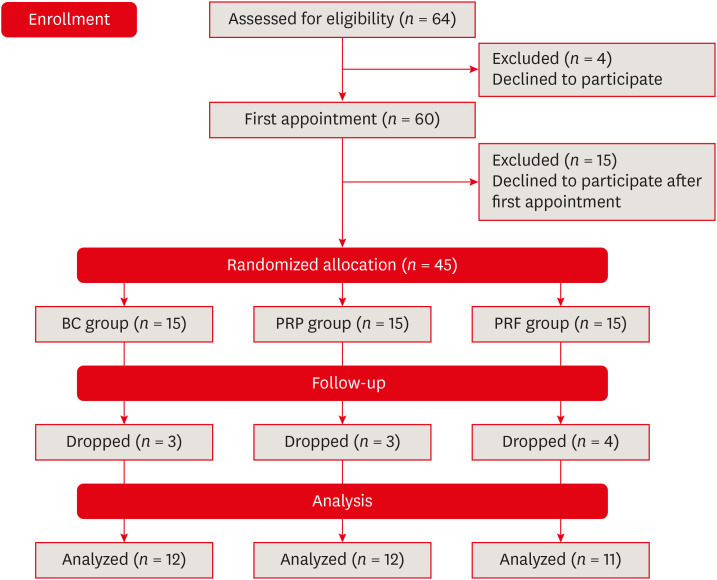
Materials and Methods Forty-five single-rooted necrotic teeth with periapical pathology were randomly allocated to receive BC, PRP, or PRF as an individual scaffold. Outcomes were evaluated in 35 teeth in 23 patients with a follow-up period of 12–24 months through qualitative IOPAR scoring and quantitative CBCT measurements. Healing of periapical lesions and in immature teeth, changes in the apical foramen diameter (AFD), root wall thickness (RWT), and root length (RL) were assessed. A
p value less than 0.05 was considered to indicate statistical significance.Results All teeth were asymptomatic except 1 in the PRP group. Periapical lesion healing was seen in all except 2 teeth in the BC group and 3 in the PRP group. Both IOPAR and CBCT revealed no significant differences in bone healing or changes in AFD, RWT, and RL among the 3 groups. A positive pulp sensibility response to the cold test was seen in 2 teeth in the BC group, but none to the electric pulp test. Intracanal calcification (ICC) was evident in more teeth in the BC group than in the PRP and PRF groups, and was also significantly higher in immature teeth.
Conclusions Our results revealed that BC, PRP, and PRF have similar potential as scaffolds in REPs, and ICC may be a concern for long-term outcomes.
-
Citations
Citations to this article as recorded by- Regenerative potential of concentrated growth factor compared to platelet-rich fibrin in treatment of necrotic mature teeth: a randomized clinical trial
Taghreed Salah, Wael Hussein, Heba Abdelkafy
BDJ Open.2025;[Epub] CrossRef - Clinical and radiographic outcomes of non-surgical retreatment of mature maxillary incisors using two regenerative endodontic techniques in adolescents: a 24-month randomized clinical trial
Ahmad Abdel Hamid Elheeny, Sherif Shafik EL Bahnasy, Yassmin Mohamed ElMakawi, Mohammed Turky, Eman Farouk Ahmed, Norhan Khaled Omar Wahba
BDJ Open.2025;[Epub] CrossRef - Clinical and Radiographic Outcomes of Autologous Platelet-Rich Products in Regenerative Endodontics: A Systematic Review and Meta-Analysis
Raewyn Huang, Wei Chen, Matthew Fang, Ove A. Peters, Sepanta Hosseinpour
Dentistry Journal.2025; 13(6): 236. CrossRef - Regenerative Endodontics in the Treatment of Periapical Lesions of Endodontic Origin: A Systematic Review of Randomized Controlled Trials
BelHaj Salah Kawthar, Berrima Fatma, Boukhris Hanen, Gnaba Imen, Ben Youssef Souha
The Journal of Contemporary Dental Practice.2025; 26(6): 623. CrossRef - Advanced Platelet-Rich Fibrin Plus Sealed Exclusively with Glass Ionomer Cement: Setting a New Standard for Healing, Aesthetics and Predictive Modelling in Regenerative Endodontics
Dubravka Turjanski, Dragutin Lisjak, Petra Bučević Sojčić, Jelena Valpotić, Tea Borojević Renić, Kristina Goršeta, Domagoj Glavina
Materials.2025; 18(18): 4421. CrossRef - Evaluation of different scaffolds and intracanal medications in revascularization of nonvital immature permanent teeth
Mona M. A. Sameia, Abeer M. Darrag, Neveen A. Shaheen, Dina A. Attia
Tanta Dental Journal.2025; 22(4): 693. CrossRef - Biomimetic pulp scaffolds prepared from extracellular matrix derived from stem cells from human exfoliated deciduous teeth promote pulp–dentine complex regeneration
Ning Yang, Rou Shen, Wenxiao Yang, Shengcai Zhang, Tianxing Gong, Yao Liu
International Endodontic Journal.2024; 57(9): 1279. CrossRef - Arrest and Repair of Inflammatory Root Resorption After an Endodontic Regeneration Procedure – A Hypothesis and Case Report
Arieh Y. Kaufman, Bill Kahler
Journal of Endodontics.2024; 50(12): 1743. CrossRef - Effect of Platelet Rich Plasma in Regenerative Endodontic Treatment: A Review of Clinical Trials
Hojat Rezazadeh, Mehrnaz Okhovatfard
Research Journal of Pharmacy and Technology.2023; : 5562. CrossRef
- Regenerative potential of concentrated growth factor compared to platelet-rich fibrin in treatment of necrotic mature teeth: a randomized clinical trial
- 4,357 View
- 108 Download
- 6 Web of Science
- 9 Crossref

- Clinical and radiographic outcomes of regenerative endodontic treatment performed by endodontic postgraduate students: a retrospective study
- Hadi Rajeh Alfahadi, Saad Al-Nazhan, Fawaz Hamad Alkazman, Nassr Al-Maflehi, Nada Al-Nazhan
- Restor Dent Endod 2022;47(2):e24. Published online May 9, 2022
- DOI: https://doi.org/10.5395/rde.2022.47.e24
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives Regenerative endodontic treatment is a clinical procedure aimed at biologically regenerating damaged root canal tissue of immature permanent teeth. This study aimed to report the outcomes of regenerative endodontic treatment performed by endodontic postgraduate students.
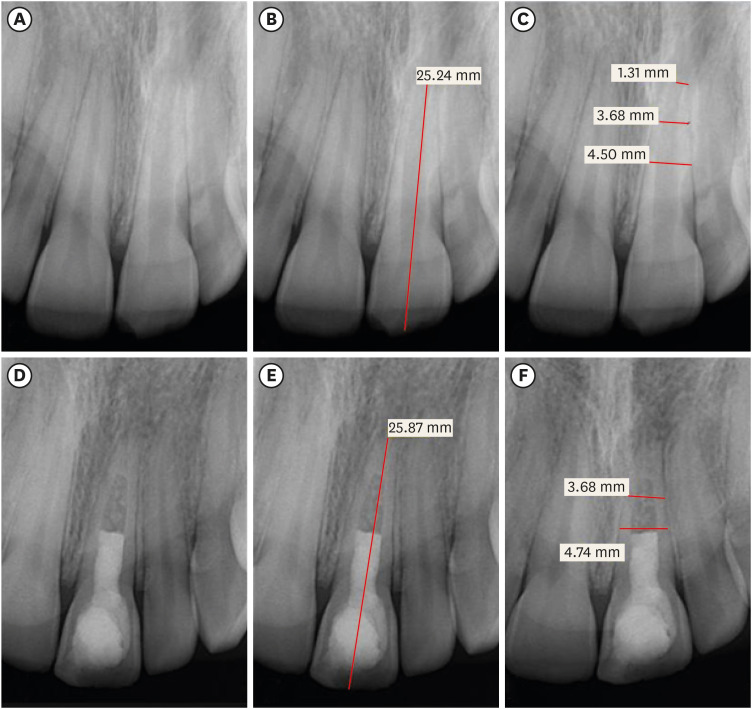
Materials and Methods Clinical and radiographic data of 27 patients, aged 10–22 years, who underwent regenerative treatment of immature permanent teeth from 2015 to 2019 were followed up, wherein clinical and radiographic examinations were performed for each patient. Postoperative success rate and tooth survival were analyzed, and the postoperative radiographic root area changes were quantified.
Results A total of 23 patients attended the dental appointments, showing that all teeth survived and were asymptomatic. Specifically, 7 periapical pathosis cases were completely healed, 12 were incompletely healed, and 4 cases failed. Moreover, significant differences were found between discolored and non-discolored teeth, and between the presence or absence of periapical radiolucency. Additionally, 3 anterior teeth showed complete closure of the apical foramen, while the apical foramen width was reduced in 17 teeth and failed in 3 teeth. Root length was also found to have been increased in 7 anterior and 4 posterior teeth, and the average length ranged from 4.00–0.63 mm in the anterior teeth, 2.85–1.48 mm of the mesial root, and 2.73–2.16 mm of the molar teeth distal root. Furthermore, calcified tissue deposition was observed in 7 teeth.
Conclusions A favorable outcome of regenerative endodontic treatment of immature permanent teeth with necrotic pulp was achieved with a high survival rate.
-
Citations
Citations to this article as recorded by- Pre‐Operative Factors on Prognosis of Regenerative Endodontic Procedures: A Systematic Review and Meta‐Analysis
Filipe Colombo Vitali, Alexandre Henrique dos Reis‐Prado, Pablo Silveira Santos, Ana Paula Portes Zeno, Patrícia de Andrade de Risso, Lucianne Cople Maia, Francine Benetti, Cleonice da Silveira da Teixeira
International Endodontic Journal.2025; 58(12): 1814. CrossRef - Clinical, radiographic, and biomarker perspectives of low-level laser therapy during regenerative endodontic procedures in necrotic immature young teeth: a randomized clinical study
Pragya Pandey, Neha Jasrasaria, Ramesh Bharti, Rakesh Kumar Yadav, Monika Kumari, Abinia Vaishnavi, Rahul Pandey
Lasers in Medical Science.2025;[Epub] CrossRef - Allogeneic Bone Marrow Mesenchymal Stromal Cell Transplantation Induces Dentin Pulp Complex-like Formation in Immature Teeth with Pulp Necrosis and Apical Periodontitis
Jose Francisco Gomez-Sosa, José E. Cardier, Olga Wittig, Dylana Díaz-Solano, Eloisa Lara, Kharelys Duque, Giselle Ramos-González
Journal of Endodontics.2024; 50(4): 483. CrossRef - Radiographic assessment of dental post and core placement at different educational levels in an undergraduate student clinic: a 4-year retrospective study
Turki Alshehri, Nourhan M. Aly, Raand Altayyar, Deena Alghamdi, Shahad Alotaibi, Passent Ellakany
F1000Research.2024; 12: 976. CrossRef - Evaluation of the efficacy of injectable platelet‐rich fibrin versus platelet‐rich plasma in the regeneration of traumatized necrotic immature maxillary anterior teeth: A randomized clinical trial
Maha Mohamed Abo‐Heikal, Jealan M. El‐Shafei, Samia A. Shouman, Nehal N. Roshdy
Dental Traumatology.2024; 40(1): 61. CrossRef - Radiographical assessment of post and core placement errors encountered by Saudi dental students at different educational levels
Turki Alshehri, Nourhan M. Aly, Raand Altayyar, Deena Alghamdi, Shahad Alotaibi, Passent Ellakany
F1000Research.2023; 12: 976. CrossRef
- Pre‐Operative Factors on Prognosis of Regenerative Endodontic Procedures: A Systematic Review and Meta‐Analysis
- 3,866 View
- 69 Download
- 6 Web of Science
- 6 Crossref

- Comparative analysis of bond strength to root dentin and compression of bioceramic cements used in regenerative endodontic procedures
- Maykely Naara Morais Rodrigues, Kely Firmino Bruno, Ana Helena Gonçalves de Alencar, Julyana Dumas Santos Silva, Patrícia Correia de Siqueira, Daniel de Almeida Decurcio, Carlos Estrela
- Restor Dent Endod 2021;46(4):e59. Published online November 9, 2021
- DOI: https://doi.org/10.5395/rde.2021.46.e59
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives This study compared the Biodentine, MTA Repair HP, and Bio-C Repair bioceramics in terms of bond strength to dentin, failure mode, and compression.
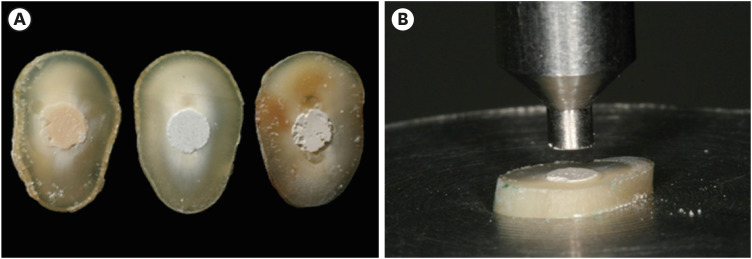
Materials and Methods Fifty-four slices obtained from the cervical third of 18 single-rooted human mandibular premolars were randomly distributed (
n = 18). After insertion of the bioceramic materials, the push-out test was performed. The failure mode was analyzed using stereomicroscopy. Another set of cylindrically-shaped bioceramic samples (n = 10) was prepared for compressive strength testing. The normality of data distribution was analyzed using the Shapiro-Wilk test. The Kruskal-Wallis and Friedman tests were used for the push-out test data, while compressive strength was analyzed with analysis of variance and the Tukey test, considering a significance level of 0.05.Results Biodentine presented a higher median bond strength value (14.79 MPa) than MTA Repair HP (8.84 MPa) and Bio-C Repair (3.48 MPa), with a significant difference only between Biodentine and Bio-C Repair. In the Biodentine group, the most frequent failure mode was mixed (61%), while in the MTA Repair HP and Bio-C Repair groups, it was adhesive (94% and 72%, respectively). Biodentine showed greater resistance to compression (29.59 ± 8.47 MPa) than MTA Repair HP (18.68 ± 7.40 MPa) and Bio-C Repair (19.96 ± 3.96 MPa) (
p < 0.05).Conclusions Biodentine showed greater compressive strength than MTA Repair HP and Bio-C Repair, and greater bond strength than Bio-C Repair. The most frequent failure mode of Biodentine was mixed, while that of MTA Repair HP and Bio-C Repair was adhesive.
-
Citations
Citations to this article as recorded by- Comparación de la resistencia compresiva entre el Agregado Trióxido Mineral y BiodentineTM en perforaciones de furca de molares inferiores permanentes
Jheymy Gerardo Huatuco-Granda, John Paul Torres-Navarro, Rosa Josefina Roncal-Espinoza
Revista Facultad de Odontología.2024;[Epub] CrossRef - Effects of different calcium-silicate based materials on fracture resistance of immature permanent teeth with replacement root resorption and osteoclastogenesis
Gabriela Leite de Souza, Gabrielle Alves Nunes Freitas, Maria Tereza Hordones Ribeiro, Nelly Xiomara Alvarado Lemus, Carlos José Soares, Camilla Christian Gomes Moura
Restorative Dentistry & Endodontics.2023;[Epub] CrossRef - Evaluation the Marginal Adaptation for the Bio C Repair and Other Root end Filling Material by Using Scanning Electron Microscope (A Comparative In Vitro Study)
Fatimah HAMADHİ, Zainab M.
Cumhuriyet Dental Journal.2023; 26(3): 261. CrossRef - Dentin Bond Strength of Calcium Silicate-Based Materials: A Systematic Review of In Vitro Studies
Natalia Radulica, José Luis Sanz, Adrián Lozano
Applied Sciences.2023; 14(1): 104. CrossRef - Evaluation Of The Push-out Bond Strength Of The Bio-C Repair And Compare It With The Mineral Trioxide Aggregate And Amalgam When Used As Root-end Filling Material
Fatimah R. Hammadi, Zainab M Abdul-Ameer
Dental Hypotheses.2023; 14(2): 62. CrossRef - Effect of different root canal irrigants on push-out bond strength of two novel root-end filling materials
Nada Omar, Rasha M. Abdelraouf, Tamer M. Hamdy
BMC Oral Health.2023;[Epub] CrossRef - Effect of irrigation systems on the bond strength of calcium-silicate-based cement used as pulp barrier in regenerative endodontic treatment
Cihan Hascizmeci, Burak Buldur
Journal of Adhesion Science and Technology.2023; 37(23): 3393. CrossRef
- Comparación de la resistencia compresiva entre el Agregado Trióxido Mineral y BiodentineTM en perforaciones de furca de molares inferiores permanentes
- 2,988 View
- 65 Download
- 4 Web of Science
- 7 Crossref

- Effect of hydrogel-based antibiotic intracanal medicaments on crown discoloration
- Rayan B. Yaghmoor, Jeffrey A. Platt, Kenneth J. Spolnik, Tien Min Gabriel Chu, Ghaeth H. Yassen
- Restor Dent Endod 2021;46(4):e52. Published online October 5, 2021
- DOI: https://doi.org/10.5395/rde.2021.46.e52
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
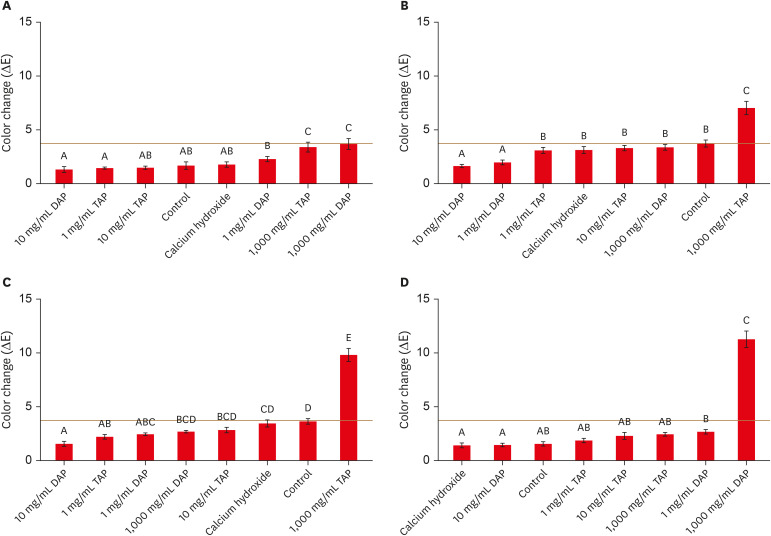
ePub Objectives This study evaluated the effects of low and moderate concentrations of triple antibiotic paste (TAP) and double antibiotic paste (DAP) loaded into a hydrogel system on crown discoloration and explored whether application of an adhesive bonding agent prevented crown discoloration.
Materials and Methods Intact human molars (
n = 160) were horizontally sectioned 1 mm apical to the cementoenamel junction. The crowns were randomized into 8 experimental groups (calcium hydroxide, Ca[OH]2; 1, 10, and 1,000 mg/mL TAP and DAP; and no medicament. The pulp chambers in half of the samples were coated with an adhesive bonding agent before receiving the intracanal medicament. Color changes (ΔE) were detected by spectrophotometry after 1 day, 1 week, and 4 weeks, and after 5,000 thermal cycles, with ΔE = 3.7 as a perceptible threshold. The 1-samplet -test was used to determine the significance of color changes relative to 3.7. Analysis of variance was used to evaluate the effects of treatment, adhesive, and time on color change, and the level of significance wasp < 0.05.Results Ca(OH)2 and 1 and 10 mg/mL DAP did not cause clinically perceivable tooth discoloration. Adhesive agent use significantly decreased tooth discoloration in the 1,000 mg/mL TAP group up to 4 weeks. However, adhesive use did not significantly improve coronal discoloration after thermocycling when 1,000 mg/mL TAP was used.
Conclusions Ca(OH)2 and 1 and 10 mg/mL DAP showed no clinical discoloration. Using an adhesive significantly improved coronal discoloration up to 4 weeks with 1,000 mg/mL TAP.
-
Citations
Citations to this article as recorded by- Tooth discoloration caused by nanographene oxide as an irrigant and intracanal medicament in the endodontic treatment of extracted single-rooted teeth: An ex-vivo study
Abbas Abbaszadegan, Zeinab Rafiee, Bahar Asheghi, Ahmad Gholami, Mohmed Isaqali Karobari
PLOS One.2025; 20(6): e0325430. CrossRef - Root development of immature necrotic permanent teeth following regenerative endodontic process: Case series
Abbasali Khademi, Pedram Iranmanesh, Ali Akhavan, Movahed Ghassem Yeganeh, Samira Khalifezade Esfahani
Dental Research Journal.2025;[Epub] CrossRef - Root Canal Dentin Microhardness after Contact with Antibiotic Medications: An In Vitro Study
Amanda Palmeira Arruda Nogueira, Renata Grazziotin-Soares, Adriana Marques Mesquita Leal, Sérgio Alves Guida Freitas Júnior, Bruna Laís Lins Gonçalves, José Bauer, Meire Coelho Ferreira, Ceci Nunes Carvalho
Dentistry Journal.2024; 12(7): 201. CrossRef - Potential Crown Discoloration Induced by the Combination of Various Intracanal Medicaments and Scaffolds Applied in Regenerative Endodontic Therapy
NB Altun, A Turkyilmaz
Nigerian Journal of Clinical Practice.2024; 27(7): 897. CrossRef
- Tooth discoloration caused by nanographene oxide as an irrigant and intracanal medicament in the endodontic treatment of extracted single-rooted teeth: An ex-vivo study
- 1,961 View
- 31 Download
- 4 Web of Science
- 4 Crossref

- A novel antimicrobial-containing nanocellulose scaffold for regenerative endodontics
- Victoria Kichler, Lucas Soares Teixeira, Maick Meneguzzo Prado, Guilherme Colla, Daniela Peressoni Vieira Schuldt, Beatriz Serrato Coelho, Luismar Marques Porto, Josiane de Almeida
- Restor Dent Endod 2021;46(2):e20. Published online March 16, 2021
- DOI: https://doi.org/10.5395/rde.2021.46.e20
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
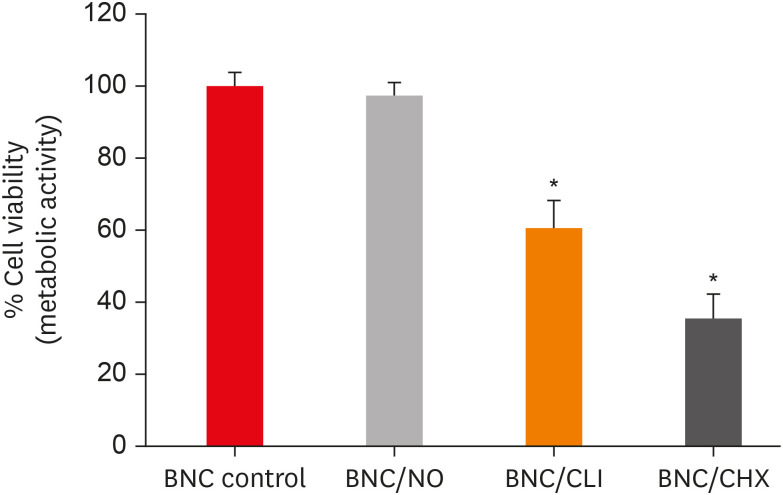
ePub Objectives The aim of this study was to evaluate bacterial nanocellulose (BNC) membranes incorporated with antimicrobial agents regarding cytotoxicity in fibroblasts of the periodontal ligament (PDLF), antimicrobial activity, and inhibition of multispecies biofilm formation.
Materials and Methods The tested BNC membranes were BNC + 1% clindamycin (BNC/CLI); BNC + 0.12% chlorhexidine (BNC/CHX); BNC + nitric oxide (BNC/NO); and conventional BNC (BNC; control). After PDLF culture, the BNC membranes were positioned in the wells and maintained for 24 hours. Cell viability was then evaluated using the MTS calorimetric test. Antimicrobial activity against
Enterococcus faecalis ,Actinomyces naeslundii , andStreptococcus sanguinis (S. sanguinis ) was evaluated using the agar diffusion test. To assess the antibiofilm activity, BNC membranes were exposed for 24 hours to the mixed culture. After sonicating the BNC membranes to remove the remaining biofilm and plating the suspension on agar, the number of colony-forming units (CFU)/mL was determined. Data were analyzed by 1-way analysis of variance and the Tukey, Kruskal-Wallis, and Dunn tests (α = 5%).Results PDLF metabolic activity after contact with BNC/CHX, BNC/CLI, and BNC/NO was 35%, 61% and 97%, respectively, compared to BNC. BNC/NO showed biocompatibility similar to that of BNC (
p = 0.78). BNC/CLI showed the largest inhibition halos, and was superior to the other BNC membranes againstS. sanguinis (p < 0.05). The experimental BNC membranes inhibited biofilm formation, with about a 3-fold log CFU reduction compared to BNC (p < 0.05).Conclusions BNC/NO showed excellent biocompatibility and inhibited multispecies biofilm formation, similarly to BNC/CLI and BNC/CHX.
-
Citations
Citations to this article as recorded by- Topic: Perspectives on Success and Failure of Endodontic Treatments
Ilma Robo, Manola Kelmendi, Eva Habazaj, Kleves Elezi, Rialda Xhizdari, Nevila Alliu
SN Comprehensive Clinical Medicine.2025;[Epub] CrossRef - Data about application of chlorhexidine as a periodontal irrigant –
Systematic Review.
Ilma Robo, Manola Kelmendi , Eva Habazaj , Kristi Sulanjaku , Nevila Alliu
Acta Stomatologica Marisiensis Journal.2025; 8(1): 6. CrossRef - Aqueous‐Phase Surface Amidation of TEMPO‐CNF Films for Improved Adsorption of Organic Pollutants in Water
Domenico Santandrea, Cécile Sillard, Valentina Beghetto, Julien Bras
ChemPlusChem.2025;[Epub] CrossRef - Materials design of gas-releasing nanoplatforms: strategies for precision delivery in oral healthcare
Haodong Zhong, Weiming Tan, Jian Zhang, Xiongwei Huang, Haizhan Chen, Jiyuan Zou, Yuxin Ye, Tao Wang, Xuechao Yang, Jiang Li, Li Yang, Lvhua Guo, Tao Luo
Materials & Design.2025; 258: 114704. CrossRef - Pushing the limits of bacterial cellulose for biomedicine: a review
Cristina Campano, Virginia Rivero-Buceta, Ana M. Hernandez-Arriaga, Maria T. Manoli, M. Auxiliadora Prieto
International Journal of Biological Macromolecules.2025; 323: 146701. CrossRef - Prospective and applications of bacterial nanocellulose in dentistry
Yasmin Alimardani, Esmaeel Mirzakhani, Fereshteh Ansari, Hadi Pourjafar, Nadia Sadeghi
Cellulose.2024; 31(13): 7819. CrossRef - Bacterial nanocelluloses as sustainable biomaterials for advanced wound healing and dressings
Atefeh Zarepour, Bahar Gok, Yasemin Budama-Kilinc, Arezoo Khosravi, Siavash Iravani, Ali Zarrabi
Journal of Materials Chemistry B.2024; 12(48): 12489. CrossRef - Sulfated endospermic nanocellulose crystals prevent the transmission of SARS-CoV-2 and HIV-1
Enrique Javier Carvajal-Barriga, Wendy Fitzgerald, Emilios K. Dimitriadis, Leonid Margolis, R. Douglas Fields
Scientific Reports.2023;[Epub] CrossRef - A Novel Approach for the Fabrication of 3D-Printed Dental Membrane Scaffolds including Antimicrobial Pomegranate Extract
Hatice Karabulut, Songul Ulag, Basak Dalbayrak, Elif Arisan, Turgut Taskin, Mehmet Guncu, Burak Aksu, Alireza Valanezhad, Oguzhan Gunduz
Pharmaceutics.2023; 15(3): 737. CrossRef - Current advances of nanocellulose application in biomedical field
M.Y. Leong, Y.L. Kong, M.Y. Harun, C.Y. Looi, W.F. Wong
Carbohydrate Research.2023; 532: 108899. CrossRef - Bacterial cellulose as a potential biopolymer in biomedical applications: a state-of-the-art review
Prachi Shrivastav, Sheersha Pramanik, Gayatri Vaidya, Mohamed A. Abdelgawad, Mohammed M. Ghoneim, Ajeet Singh, Bassam M. Abualsoud, Larissa Souza Amaral, Mohammed A. S. Abourehab
Journal of Materials Chemistry B.2022; 10(17): 3199. CrossRef - Nanocelluloses as new generation materials: natural resources, structure-related properties, engineering nanostructures, and technical challenges
Ahmed Barhoum, Vibhore K. Rastogi, Bhupender K. Mahur, Amit Rastogi, Fatehy M. Abdel-Haleem, Pieter Samyn
Materials Today Chemistry.2022; 26: 101247. CrossRef - The current natural/chemical materials and innovative technologies in periodontal diseases therapy and regeneration: A narrative review
Peyman Esmaeili Fard Barzegar, Reza Ranjbar, Mohsen Yazdanian, Elahe Tahmasebi, Mostafa Alam, Kamyar Abbasi, Hamid Tebyaniyan, Keyvan Esmaeili Fard Barzegar
Materials Today Communications.2022; 32: 104099. CrossRef
- Topic: Perspectives on Success and Failure of Endodontic Treatments
- 1,961 View
- 30 Download
- 14 Web of Science
- 13 Crossref

- Pulp revascularization with and without platelet-rich plasma in two anterior teeth with horizontal radicular fractures: a case report
- Edison Arango-Gómez, Javier Laureano Nino-Barrera, Gustavo Nino, Freddy Jordan, Henry Sossa-Rojas
- Restor Dent Endod 2019;44(4):e35. Published online August 20, 2019
- DOI: https://doi.org/10.5395/rde.2019.44.e35
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Pulp revascularization is an alternative treatment in immature traumatized teeth with necrotic pulp. However, this procedure has not been reported in horizontal root fractures. This is a case report of a 9-year-old patient with multiple horizontal root fractures in 2 upper central incisors that were successfully treated with pulp revascularization. The patient presented for treatment 2 years after the initial trauma, and revascularization was attempted after the initial treatment with calcium hydroxide had failed. Prior to pulp revascularization, cone-beam computed tomography and autoradiograms demonstrated multiple horizontal fractures in the middle and apical thirds of the roots of the 2 affected teeth. Revascularization was performed in both teeth; platelet-rich plasma (PRP) was used in one tooth (#11) and the conventional method (blood clot) was used in the other tooth (#21). Clinical and radiographic follow-up over 4 years demonstrated pulp calcification in the PRP-treated tooth. Neither of the 2 teeth were lost, and the root canal calcification of tooth #11 was greater than that of tooth #21. This case suggests that PRP-based pulp revascularization may be an alternative for horizontal root fractures.
-
Citations
Citations to this article as recorded by- Platelet-Rich Plasma and Platelet-Rich Fibrin in Endodontics: A Scoping Review
Simão Rebimbas Guerreiro, Carlos Miguel Marto, Anabela Paula, Joana Rita de Azevedo Pereira, Eunice Carrilho, Manuel Marques-Ferreira, Siri Vicente Paulo
International Journal of Molecular Sciences.2025; 26(12): 5479. CrossRef - Dental pulp mesenchymal stem cells-response to fibrin hydrogel reveals ITGA2 and MMPs expression
David Tong, Stéphanie Gobert, Alicia Reuzeau, Jean-Christophe Farges, Marianne Leveque, Marie Bolon, Arthur Costantini, Marielle Pasdeloup, Jérôme Lafont, Maxime Ducret, Mourad Bekhouche
Heliyon.2024; 10(13): e32891. CrossRef - Pulp regeneration treatment using different bioactive materials in permanent teeth of pediatric subjects
Dina Abdellatif, Alfredo Iandolo, Giuseppina De Benedetto, Francesco Giordano, Davide Mancino, Edouard Euvrard, Massimo Pisano
Journal of Conservative Dentistry and Endodontics.2024; 27(5): 458. CrossRef - Retreatment of a Failed Regenerative Endodontic Treatment in an Immature Tooth with a Horizontal Root Fracture: A Case Report
Zaher Marjy, Iris Slutzky-Goldberg
International Journal of Clinical Pediatric Dentistry.2024; 17(10): 1168. CrossRef - The Impact of the Preferred Reporting Items for Case Reports in Endodontics (PRICE) 2020 Guidelines on the Reporting of Endodontic Case Reports
Sofian Youssef, Phillip Tomson, Amir Reza Akbari, Natalie Archer, Fayjel Shah, Jasmeet Heran, Sunmeet Kandhari, Sandeep Pai, Shivakar Mehrotra, Joanna M Batt
Cureus.2023;[Epub] CrossRef - Evaluation of postoperative pain and healing following regenerative endodontics using platelet‐rich plasma versus conventional endodontic treatment in necrotic mature mandibular molars with chronic periapical periodontitis. A randomized clinical trial
Yassmin Elsayed Ahmed, Geraldine Mohamed Ahmed, Angie Galal Ghoneim
International Endodontic Journal.2023; 56(4): 404. CrossRef - Regenerative endodontic procedures for two traumatized mature anterior teeth with transverse root fractures
Jing Lu, Bill Kahler
BMC Oral Health.2022;[Epub] CrossRef - Are platelet concentrate scaffolds superior to traditional blood clot scaffolds in regeneration therapy of necrotic immature permanent teeth? A systematic review and meta-analysis
Qianwei Tang, Hua Jin, Song Lin, Long Ma, Tingyu Tian, Xiurong Qin
BMC Oral Health.2022;[Epub] CrossRef - Platelet-Rich Fibrin Used as a Scaffold in Pulp Regeneration: Case Series
Ceren ÇİMEN, Selin ŞEN, Elif ŞENAY, Tuğba BEZGİN
Cumhuriyet Dental Journal.2021; 24(1): 113. CrossRef - Plasma rico en plaquetas en Odontología: Revisión de la literatura
Hugo Anthony Rosas Rozas, Hugo Leoncio Rosas Cisneros
Yachay - Revista Científico Cultural.2021; 10(1): 536. CrossRef
- Platelet-Rich Plasma and Platelet-Rich Fibrin in Endodontics: A Scoping Review
- 2,432 View
- 41 Download
- 10 Crossref

- Retreatment of failed regenerative endodontic of orthodontically treated immature permanent maxillary central incisor: a case report
- Musaed Fahad Al-Tammami, Saad A. Al-Nazhan
- Restor Dent Endod 2017;42(1):65-71. Published online October 28, 2016
- DOI: https://doi.org/10.5395/rde.2017.42.1.65
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub A revascularization procedure was shown to be the best alternative therapy for immature teeth with necrotic pulp and apical infection. A 12 year old female with a history of trauma to her upper central incisor and a sinus tract was referred for endodontic treatment. She was an active orthodontic patient and had undergone regenerative endodontic treatment for the past 2 years. Clinical examination revealed no response to sensibility, percussion, and palpation tests. The preoperative radiograph showed an open apex and apical rarefaction. The case was diagnosed as previously treated tooth with asymptomatic apical periodontitis. Regenerative endodontic retreatment was performed, and the case was followed for 3 years. Clinical, radiographic, and cone-beam computed tomography follow-up examination revealed an asymptomatic tooth, with evidence of periapical healing and root maturation.
-
Citations
Citations to this article as recorded by- Revascularization of Non-Vital, Immature, Permanent Teeth with Two Bioceramic Cements: A Randomized Controlled Trial
Alaa Shaker, Mohamed Salem Rekab, Mohammad Alharissy, Naji Kharouf
Ceramics.2024; 7(1): 86. CrossRef - Orthodontically induced external apical root resorption considerations of root-filled teeth vs vital pulp teeth: a systematic review and meta-analysis
Danning Zhao, Kun Xue, Jiayuan Meng, Meijing Hu, Fei Bi, Xuelian Tan
BMC Oral Health.2023;[Epub] CrossRef - Regenerative Endodontic Therapy for Management of an Immature Permanent Tooth with Recurrent Post-treatment Apical Periodontitis
Renato Lenzi, Sandra R Hernández, Flávio R F Alves, Isabela N Ro[Combining Circumflex Accent]c[COMBINING CEDILLA]as, Jose[Combining Acute Accent] F Siqueira
Journal of International Society of Preventive and Community Dentistry.2022; 12(4): 468. CrossRef - Rejeneratif Endodontik Tedavi: Bir Literatür Derlemesi
Enes Mustafa AŞAR, Murat Selim BOTSALI
Selcuk Dental Journal.2022; 9(1): 335. CrossRef - Clinical and radiographic outcomes of regenerative endodontic treatment performed by endodontic postgraduate students: a retrospective study
Hadi Rajeh Alfahadi, Saad Al-Nazhan, Fawaz Hamad Alkazman, Nassr Al-Maflehi, Nada Al-Nazhan
Restorative Dentistry & Endodontics.2022;[Epub] CrossRef - Endodontic Regenerative Procedures in Necrotic Adult Teeth
Sara Garrido-Parada, Pablo Castelo-Baz, Nancy Feijoo-Pato, José Gaviño-Orduña, Benjamín Martín-Biedma
Applied Sciences.2022; 12(9): 4212. CrossRef - Different Approaches to the Regeneration of Dental Tissues in Regenerative Endodontics
Anna M. Krupińska, Katarzyna Skośkiewicz-Malinowska, Tomasz Staniowski
Applied Sciences.2021; 11(4): 1699. CrossRef - Histologic, Radiographic, and Micro-Computed Tomography Evaluation of Experimentally Enlarged Root Apices in Dog Teeth with Apical Periodontitis after Regenerative Treatment
Mohammed S. Alenazy, Saad Al-Nazhan, Hezekiah A Mosadomi
Current Therapeutic Research.2021; 94: 100620. CrossRef - Revitalizing previously treated teeth with open apices: A case report and a literature review
Ali Nosrat, Behnam Bolhari, Shima Saber Tahan, Omid Dianat, Paul Michael Howell Dummer
International Endodontic Journal.2021; 54(10): 1782. CrossRef - PRICE 2020 guidelines for reporting case reports in Endodontics: explanation and elaboration
V. Nagendrababu, B. S. Chong, P. McCabe, P. K. Shah, E. Priya, J. Jayaraman, S. J. Pulikkotil, P. M. H. Dummer
International Endodontic Journal.2020; 53(7): 922. CrossRef - Regenerative Endodontics: A Systematic Analysis of the Failed Cases
Waleed Almutairi, Ghaeth H. Yassen, Anita Aminoshariae, Kristin A. Williams, Andre Mickel
Journal of Endodontics.2019; 45(5): 567. CrossRef - Alternative to Avoid Tooth Discoloration after Regenerative Endodontic Procedure: A Systematic Review
Luciane Geanini Pena dos Santos, Luiz Alexandre Chisini, Camila Guerner Springmann, Beatriz Dulcineia Mendes de Souza, Fernanda Geraldo Pappen, Flávio Fernando Demarco, Mara Cristina Santos Felippe, Wilson Tadeu Felippe
Brazilian Dental Journal.2018; 29(5): 409. CrossRef
- Revascularization of Non-Vital, Immature, Permanent Teeth with Two Bioceramic Cements: A Randomized Controlled Trial
- 1,795 View
- 14 Download
- 12 Crossref

- Biocompatibility of two experimental scaffolds for regenerative endodontics
- Dephne Jack Xin Leong, Frank C. Setzer, Martin Trope, Bekir Karabucak
- Restor Dent Endod 2016;41(2):98-105. Published online March 28, 2016
- DOI: https://doi.org/10.5395/rde.2016.41.2.98
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives The biocompatibility of two experimental scaffolds for potential use in revascularization or pulp regeneration was evaluated.
Materials and Methods One resilient lyophilized collagen scaffold (COLL), releasing metronidazole and clindamycin, was compared to an experimental injectable poly(lactic-co-glycolic) acid scaffold (PLGA), releasing clindamycin. Human dental pulp stem cells (hDPSCs) were seeded at densities of 1.0 × 104, 2.5 × 104, and 5.0 × 104. The cells were investigated by light microscopy (cell morphology), MTT assay (cell proliferation) and a cytokine (IL-8) ELISA test (biocompatibility).
Results Under microscope, the morphology of cells coincubated for 7 days with the scaffolds appeared healthy with COLL. Cells in contact with PLGA showed signs of degeneration and apoptosis. MTT assay showed that at 5.0 × 104 hDPSCs, COLL demonstrated significantly higher cell proliferation rates than cells in media only (control,
p < 0.01) or cells co-incubated with PLGA (p < 0.01). In ELISA test, no significant differences were observed between cells with media only and COLL at 1, 3, and 6 days. Cells incubated with PLGA expressed significantly higher IL-8 than the control at all time points (p < 0.01) and compared to COLL after 1 and 3 days (p < 0.01).Conclusions The COLL showed superior biocompatibility and thus may be suitable for endodontic regeneration purposes.
-
Citations
Citations to this article as recorded by- Advances in scaffolds used forpulp–dentinecomplex tissue engineering: A narrative review
Parisa Noohi, Mohammad J. Abdekhodaie, Mohammad H. Nekoofar, Kerstin M. Galler, Paul M. H. Dummer
International Endodontic Journal.2022; 55(12): 1277. CrossRef - In vitro performance of a nanobiocomposite scaffold containing boron-modified bioactive glass nanoparticles for dentin regeneration
Reza Moonesi Rad, Engin Pazarçeviren, Elif Ece Akgün, Zafer Evis, Dilek Keskin, Sıla Şahin, Ayşen Tezcaner
Journal of Biomaterials Applications.2019; 33(6): 834. CrossRef - Biological effects of silk fibroin 3D scaffolds on stem cells from human exfoliated deciduous teeth (SHEDs)
M. Collado-González, M. P. Pecci-Lloret, D. García-Bernal, S. Aznar-Cervantes, R. E. Oñate-Sánchez, J. M. Moraleda, J. L. Cenis, F. J. Rodríguez-Lozano
Odontology.2018; 106(2): 125. CrossRef - Pulp Regeneration Concepts for Nonvital Teeth: From Tissue Engineering to Clinical Approaches
Valérie Orti, Pierre-Yves Collart-Dutilleul, Sofía Piglionico, Orsolya Pall, Frédéric Cuisinier, Ivan Panayotov
Tissue Engineering Part B: Reviews.2018; 24(6): 419. CrossRef - Investigation of Human Dental Pulp Cells on a Potential Injectable Poly(lactic-co-glycolic acid) Microsphere Scaffold
Huiru Zou, Guanhua Wang, Fang Song, Xudong Shi
Journal of Endodontics.2017; 43(5): 745. CrossRef - Biocompatibility of hydrogel-based scaffolds for tissue engineering applications
Sheva Naahidi, Mousa Jafari, Megan Logan, Yujie Wang, Yongfang Yuan, Hojae Bae, Brian Dixon, P. Chen
Biotechnology Advances.2017; 35(5): 530. CrossRef
- Advances in scaffolds used forpulp–dentinecomplex tissue engineering: A narrative review
- 1,533 View
- 10 Download
- 6 Crossref

- Effect of dentin treatment on proliferation and differentiation of human dental pulp stem cells
- Minjeong Park, Nan-Sim Pang, Il-Young Jung
- Restor Dent Endod 2015;40(4):290-298. Published online September 23, 2015
- DOI: https://doi.org/10.5395/rde.2015.40.4.290
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives Sodium hypochlorite (NaOCl) is an excellent bactericidal agent, but it is detrimental to stem cell survival, whereas intracanal medicaments such as calcium hydroxide (Ca[OH]2) promote the survival and proliferation of stem cells. This study evaluated the effect of sequential NaOCl and Ca[OH]2 application on the attachment and differentiation of dental pulp stem cells (DPSCs).
Materials and Methods DPSCs were obtained from human third molars. All dentin specimens were treated with 5.25% NaOCl for 30 min. DPSCs were seeded on the dentin specimens and processed with additional 1 mg/mL Ca[OH]2, 17% ethylenediaminetetraacetic acid (EDTA) treatment, file instrumentation, or a combination of these methods. After 7 day of culture, we examined DPSC morphology using scanning electron microscopy and determined the cell survival rate with 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide assay. We measured cell adhesion gene expression levels after 4 day of culture and odontogenic differentiation gene expression levels after 4 wk using quantitative real-time polymerase chain reaction.
Results DPSCs did not attach to the dentin in the NaOCl-treated group. The gene expression levels of fibronectin-1 and secreted phosphoprotein-1 gene in both the Ca[OH]2- and the EDTA-treated groups were significantly higher than those in the other groups. All Ca[OH]2-treated groups showed higher expression levels of dentin matrix protein-1 than that of the control. The dentin sialophosphoprotein level was significantly higher in the groups treated with both Ca[OH]2 and EDTA.
Conclusions The application of Ca[OH]2 and additional treatment such as EDTA or instrumentation promoted the attachment and differentiation of DPSCs after NaOCl treatment.
-
Citations
Citations to this article as recorded by- Effect of Intracanal Medications on the Viability of Human Periodontal Ligament‐Derived Mesenchymal Stem Cells
Arian Braido, Walbert de Andrade Vieira, Bruno Cazotti Pereira, Karina Gonzales Silvério, Paulo Henrique Gabriel, Aline Cristine Gomes Matta, Emerson Alves Martins, Adriana de Jesus Soares
Australian Endodontic Journal.2025;[Epub] CrossRef - Effect of erbium yttrium aluminium garnet laser dentin conditioning on dental pulp stem cells viability
Aryan Jafari, Mehdi Vatanpour, Nooshin Barikrow, Pouyan Razavi, Sohrab Tour Savadkouhi
Heliyon.2024; 10(5): e26954. CrossRef - Comparison of the effect of NaOCL, curcumin, and EDTA on differentiation, proliferation, and adhesion of dental pulp stem cells
Vahid Zand, Amin Salem Milani, Carolyn Primus, Marzie Aghazade, Hadi Mokhtari, Sabete Bagheri Sabzevar, Pardis Tehranchi
Journal of Oral Biology and Craniofacial Research.2023; 13(2): 347. CrossRef - Differential Effects of Extracellular Matrix Glycoproteins Fibronectin and Laminin-5 on Dental Pulp Stem Cell Phenotypes and Responsiveness
Hyungbin Lee, Allen Bae, John Kim, Karl Kingsley
Journal of Functional Biomaterials.2023; 14(2): 91. CrossRef - Assessment of the Influence of Various Concentrations of Sodium Hypochlorite on Stem Cell Derived From Human Exfoliated Deciduous Teeth (SHED) Proliferation and Differentiation
Viral Maru, Ashwini KB, Manisha Madkaikar, R K Sarada Devi, Ashita Gada, Salil Bapat
Cureus.2022;[Epub] CrossRef - Effects of sodium hypochlorite and ethylenediaminetetraacetic acid on proliferation, osteogenic/odontogenic differentiation, and mechanosensitive gene expression of human dental pulp stem cells
Yuejun Li, Changlong Jin, Shouliang Zhao, Han Xie
Tissue and Cell.2022; 79: 101955. CrossRef - Influence of ethylenediaminetetraacetic acid on regenerative endodontics: A systematic review
Alexandre H. dos Reis‐Prado, Lucas G. Abreu, Rogéria R. Fagundes, Sabrina de C. Oliveira, Marco C. Bottino, Antônio P. Ribeiro‐Sobrinho, Francine Benetti
International Endodontic Journal.2022; 55(6): 579. CrossRef - An in-vitro Comparative Evaluation of Quantitative Release of Transforming Growth Factor β-1 from Dentin upon the Action of Endodontic Irrigants, Medicaments, Ultrasonic Activation, and Low-Level Laser Irradiation
Anilkumar Akhila, V. P. Prabath Singh, Kerala R. Varma, Senthil V. Vasudevan, V. Sukhithasri, Salu Sasikumar
Amrita Journal of Medicine.2021; 17(2): 34. CrossRef - Non-Thermal Atmospheric Pressure Plasma-Conditioned Root Dentin Promotes Attraction and Attachment of Primary Human Dental Pulp Stem Cells in Real-Time Ex Vivo
Yeon-Jee Yoo, Min-Ji Kang, Hiran Perinpanayagam, Joo-Cheol Park, Seung-Ho Baek, Kee-Yeon Kum
Applied Sciences.2021; 11(15): 6836. CrossRef - The Effects of Intracanal Irrigants and Medicaments on Dental-Derived Stem Cells Fate in Regenerative Endodontics: An update
Sara Ayoub, Ali Cheayto, Sanaa Bassam, Mehdi Najar, Antoine Berbéri, Mohammad Fayyad-Kazan
Stem Cell Reviews and Reports.2020; 16(4): 650. CrossRef - An Immunofluorescence Study to Analyze Wound Healing Outcomes of Regenerative Endodontics in an Immature Premolar with Chronic Apical Abscess
Jeen Nee Lui, Wen Yi Lim, Domenico Ricucci
Journal of Endodontics.2020; 46(5): 627. CrossRef - Dynamic Irrigation Promotes Apical Papilla Cell Attachment in an Ex Vivo Immature Root Canal Model
Sanupong Prompreecha, Thanapat Sastraruji, Phumisak Louwakul, Tanida Srisuwan
Journal of Endodontics.2018; 44(5): 744. CrossRef - Odontoblast-like differentiation and mineral formation of pulpsphere derived cells on human root canal dentin in vitro
Jörg Neunzehn, Sandra Pötschke, Christian Hannig, Hans-Peter Wiesmann, Marie-Theres Weber
Head & Face Medicine.2017;[Epub] CrossRef - Effects of Epigallocatechin Gallate, an Antibacterial Cross-linking Agent, on Proliferation and Differentiation of Human Dental Pulp Cells Cultured in Collagen Scaffolds
Young-Sun Kwon, Hee-Jin Kim, Yun-Chan Hwang, Vinicius Rosa, Mi-Kyung Yu, Kyung-San Min
Journal of Endodontics.2017; 43(2): 289. CrossRef
- Effect of Intracanal Medications on the Viability of Human Periodontal Ligament‐Derived Mesenchymal Stem Cells
- 1,562 View
- 6 Download
- 14 Crossref

- A review of the regenerative endodontic treatment procedure
- Bin-Na Lee, Jong-Wook Moon, Hoon-Sang Chang, In-Nam Hwang, Won-Mann Oh, Yun-Chan Hwang
- Restor Dent Endod 2015;40(3):179-187. Published online March 16, 2015
- DOI: https://doi.org/10.5395/rde.2015.40.3.179
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Traditionally, apexification has been used to treat immature permanent teeth that have lost pulp vitality. This technique promotes the formation of an apical barrier to close the open apex so that the filling materials can be confined to the root canal. Because tissue regeneration cannot be achieved with apexification, a new technique called regenerative endodontic treatment was presented recently to treat immature permanent teeth. Regenerative endodontic treatment is a treatment procedure designed to replace damaged pulp tissue with viable tissue which restores the normal function of the pulp-dentin structure. After regenerative endodontic treatment, continued root development and hard tissue deposition on the dentinal wall can occur under ideal circumstances. However, it is difficult to predict the result of regenerative endodontic treatment. Therefore, the purpose of this study was to summarize multiple factors effects on the result of regenerative endodontic treatment in order to achieve more predictable results. In this study, we investigated the features of regenerative endodontic treatment in comparison with those of other pulp treatment procedures and analyzed the factors that have an effect on regenerative endodontic treatment.
-
Citations
Citations to this article as recorded by- Evaluation of the Clinical Outcomes of Regenerative Endodontic Procedures Using Autologous Platelet Concentrate: A Systematic Review and Meta-Analysis
Elnaz Mousavi, Navid Nasrabadi, Samira Jamali, Arian Haddadi
Pesquisa Brasileira em Odontopediatria e Clínica Integrada.2025;[Epub] CrossRef - Antimicrobial 3D printed gelatin scaffolds for root canal disinfection in regenerative endodontics procedures
Mateo Dallos Ortega, Jenny Aveyard, Raghda Magdy Abdelgawad, Reem El-Gendy, Alexander Ciupa, David Whetnall, Julia Behnsen, Robert J. Poole, Raechelle A. D'Sa
Biomaterials Science.2025; 13(14): 3795. CrossRef - Regenerative Endodontic Therapies: Harnessing Stem Cells, Scaffolds, and Growth Factors
Rosana Farjaminejad, Samira Farjaminejad, Franklin Garcia-Godoy
Polymers.2025; 17(11): 1475. CrossRef - Effects of combining hyaluronic acid hydrogel with injectable platelet rich fibrin on apical papilla stem cells proliferation and differentiation
Azal H. Al-Masoody, Nasrin Asadi, Hadiseh Mohammadpour, Mahshid Hodjat, Tahereh Sadat Jafarzadeh Kashi
BMC Oral Health.2025;[Epub] CrossRef - Experts consensus on management of tooth luxation and avulsion
Ruijie Huang, Chenchen Zhou, Ling Zhan, Yuan Liu, Xian Liu, Qin Du, Jun Wang, Wei Zhao, Guangtai Song, Li-an Wu, Beizhan Jiang, Yanhong Li, Hongmei Zhang, Jing Zou
International Journal of Oral Science.2024;[Epub] CrossRef - A review of tissue engineering in regenerative endodontic treatment
Eric Priyo Prasetyo, Dian Agustin Wahjuningrum, Galih Sampoerno, Wilson Sukandar, Shafy Shariz Bin Sharizal, Nurfahira Paidal, Menza Fadiyan Amriel, Nathania Elita Gunawan, Ketut Suardita, Evelyn Tjendronegoro
Conservative Dentistry Journal.2024; 14(1): 1. CrossRef - Innovative Paradigms and Established Strategies in Tooth Revitalization: A Review
Ahmad Shah Khan, Zahid Mehmood Khan, Palwasha Ishaque, Muhammad Zubair, Syeda Fatima Tu Zahra, Sana Ashfaq
Dental Update.2024; 51(8): 570. CrossRef - Explore the most recent developments and upcoming outlooks in the field of dental nanomaterials
Ali Alsuraifi, Zainab M. Sulaiman, Noor Alhuda R. Mohammed, Jassim Mohammed, Sarah Kareem Ali, Yousef Husam Abdualihamaid, Fatimah Husam, Abdullah Ayad
Beni-Suef University Journal of Basic and Applied Sciences.2024;[Epub] CrossRef - Recent Advances in Regenerative Endodontics: A Review of Current Techniques and Future Directions
Firas A Alothman, Lamia S Hakami, Ali Alnasser, Faris M AlGhamdi, Abdullah A Alamri, Basel M Almutairii
Cureus.2024;[Epub] CrossRef - Regenerative Potential of Dental Pulp Stem Cells in Response to a Bioceramic Dental Sealer and Photobiomodulation: An In Vitro Study
Hamed A Alshawkani, Mohamed Mansy, Mahmoud Al Ankily, Mohamed Shamel
The Journal of Contemporary Dental Practice.2024; 25(4): 313. CrossRef - Marginal adaptation of customized gutta percha cone with calcium silicate based sealer versus MTA and biodentine apical plugs in simulated immature permanent teeth (an in vitro study)
Mary M. Mina, Sybel M. Moussa, Mahmoud R. Aboelseoud
BMC Oral Health.2024;[Epub] CrossRef - GelMA‐based hydrogel biomaterial scaffold: A versatile platform for regenerative endodontics
Lei Huang, Xuan Chen, XiaoXia Yang, Yinchun Zhang, Xiaoling Qiu
Journal of Biomedical Materials Research Part B: Applied Biomaterials.2024;[Epub] CrossRef - Regenerative Endodontic Treatment in Dentinogenesis Imperfecta‐Induced Apical Periodontitis
Ying Liao, Ting Pan, Xianghui Xing, Sivakumar Nuvvula
Case Reports in Dentistry.2024;[Epub] CrossRef - In vitro and in vivo evaluation of iRoot BP Plus as a coronal sealing material for regenerative endodontic procedures
Ning Yang, Wenxiao Yang, Rou Shen, Shengcai Zhang, Tianchi Ma, Yao Liu
Clinical Oral Investigations.2024;[Epub] CrossRef - Comparative evaluation of pH and Ca+ ion release from MTA on interaction with platelet-rich fibrin and blood clot: an in vitro study
Sonia Khatri, Sylvia Mathew, Shruthi Nagaraja, Swaroop Hegde, Soumyadeep Ghosh, Kavimalar Ravichandran
F1000Research.2023; 12: 364. CrossRef - Photobiomodulation Therapy and Pulp-Regenerative Endodontics: A Narrative Review
Jiawen Yong, Sabine Gröger, Zuping Wu, Sabine Ruf, Yuer Ye, Xiaoyan Chen
Bioengineering.2023; 10(3): 371. CrossRef - Efficacy of disinfection procedures performed prior to regenerative endodontic therapy: An integrative review
Ketillyn da Silva Magalhães, Ana Clara Kuerten Gil, Taynara Santos Goulart, Daniela Peressoni Vieira Schuldt, Beatriz Serrato Coelho, Daniela de Rossi Figueiredo, Lucas da Fonseca Roberti Garcia, Josiane de Almeida
Australian Endodontic Journal.2023; 49(2): 418. CrossRef - Newer Prospects of Regenerative Endodontics: A Comprehensive and Updated Review of Literature
Mohammad Kamran Khan, Mahendra Kumar Jindal
Journal of the Scientific Society.2023; 50(3): 299. CrossRef - Comparative evaluation of pH and Ca+ ion release from MTA on interaction with platelet-rich fibrin and blood clot: an in vitro study
Sonia Khatri, Sylvia Mathew, Shruthi Nagaraja, Swaroop Hegde, Soumyadeep Ghosh, Kavimalar Ravichandran
F1000Research.2023; 12: 364. CrossRef - Effects of CEM cement and emdogain on proliferation and differentiation of human stem cells from the apical papilla: a comparative in vitro study
Elham Khoshbin, Leila Ghasemi, Rezvan Najafi, Hamed Karkehabadi
Biotechnology Letters.2023; 45(1): 69. CrossRef - Comparative Evaluation of the Regenerative Potential of Blood Clot and Platelet-rich Fibrin in Young Permanent Teeth Based on the Revised American Academy of Endodontics Clinical Considerations for Regenerative Procedure: 2016
Saraswathi V Naik, Prabhakar Attiguppe, Aarathi J Prakash
International Journal of Clinical Pediatric Dentistry.2023; 16(S2): S149. CrossRef - Biomechanical characterization of a fibrinogen–blood hydrogel for human dental pulp regeneration
Sofia Silvia Piglionico, Bela Varga, Orsolya Pall, Olivier Romieu, Csilla Gergely, Frédéric Cuisinier, Bernard Levallois, Ivan Vladislavov Panayotov
Biomaterials Science.2023; 11(20): 6919. CrossRef - Intracellular bacterial eradication using a novel peptide in vitro
Wing Nok Isaac Ng, Shanthini Kalimuthu, Carmen Oi Kwan Law, Angeline Hui Cheng Lee, Terrence Chi Kong Lau, Yiu Yan Leung, Gary Shun Pan Cheung, Prasanna Neelakantan
International Endodontic Journal.2023; 56(11): 1360. CrossRef - Regenerative Endodontic Treatment of Previously Treated Mature Permanent Tooth: A Case Report with 3-year Follow Up
Myung-Jin Lee
The Korean Journal of Oral and Maxillofacial Pathology.2023; 47(6): 133. CrossRef - Clinical Outcome and Comparison of Regenerative and Apexification Intervention in Young Immature Necrotic Teeth—A Systematic Review and Meta-Analysis
Pratima Panda, Lora Mishra, Shashirekha Govind, Saurav Panda, Barbara Lapinska
Journal of Clinical Medicine.2022; 11(13): 3909. CrossRef - Evaluation of Attitude and Knowledge of Endodontic, Pedodontic and SBARD Residents in Saudi Arabia toward Regenerative Endodontics—A National Survey
Ali A. Assiry, Mohmed Isaqali Karobari, Niher Tabassum Snigdha, Roshan Noor Mohamed, Syed Nahid Basheer, Mohammed Zameer
Medicina.2022; 58(4): 545. CrossRef - Effects of Intracanal Antimicrobials on Viability and Differentiation of Stem Cells From the Apical Papilla: An In Vitro Study
Gavin Raddall, Isabel Mello, Brendan M. Leung
Journal of Endodontics.2022; 48(7): 880. CrossRef - Awareness and Acceptance of Vital Pulp Therapy and Regenerative Endodontic Procedures among Dental Professionals in India: A Web-based Survey
Saloni Rathi, Priya Chauhan, Suparna Ganguly Saha, Rolly Agarwal, Simar Kaur Manocha, Mrinali Chaddha
Journal of Research and Advancement in Dentistry.2022; 14(1): 10. CrossRef - Exosomes as Biochemistry Tools for Stem Cell Differentiation: A Novel Cell-Based Treatment for Diseases
Saeed Azandeh, Darioush Bijan Nejad, Samaneh Karimi, Fereshtesadat Fakhredini
Jentashapir Journal of Cellular and Molecular Biology.2022;[Epub] CrossRef - Effect of biodentine coated with emdogain on proliferation and differentiation of human stem cells from the apical papilla
Hamed Karkehabadi, Erfan Ahmadyani, Rezvan Najafi, Elham Khoshbin
Molecular Biology Reports.2022; 49(5): 3685. CrossRef - Evaluation of the Effectiveness of Laser‐Assisted Bleaching of the Teeth Discolored due to Regenerative Endodontic Treatment
Noushin Shokouhinejad, Mehrfam Khoshkhounejad, Fatemeh Hamidzadeh, Murilo Baena Lopes
International Journal of Dentistry.2022;[Epub] CrossRef - Triple Antibiotic Paste: A Suitable Medicament for Intracanal Disinfection
Krutika Malu, Monika Khubchandani
Cureus.2022;[Epub] CrossRef - A Comparative Evaluation of Microhardness and Chemical Structure of Radicular Dentin with Two Combinations of TAP and MTAP: An In Vitro Study
P Niharika, Saigeeta Kondamadugu, Nagireddy Venugopal Reddy, Muthumula Daneswari, Annie P Chris, Nikhila V Reddy
International Journal of Clinical Pediatric Dentistry.2022; 15(S2): S151. CrossRef - Comparing Antibiotic Pastes with Electrospun Nanofibers as Modern Drug Delivery Systems for Regenerative Endodontics
Nura Brimo, Dilek Çökeliler Serdaroğlu, Busra Uysal
Current Drug Delivery.2022; 19(9): 904. CrossRef - The Advances of Blood Clots Used as Biomaterials in Regenerative Medicine
Eliza VanZweden, Rachael Tolsma, Victor Hung, Peter Awad, Robert Sawyer, Yong Li
Regenerative Medicine.2022; 17(12): 957. CrossRef - Microstructure and color stability of calcium silicate-based dental materials exposed to blood or platelet-rich fibrin
Noushin Shokouhinejad, Ibrahim Abu Tahun, Shima Saber Tahan, Fatemeh Mohandes, Mohammad H. Nekoofar, Paul M. H. Dummer
Clinical Oral Investigations.2022; 27(3): 1193. CrossRef - Results of “proroot mta” application in treatment of chronic periodontitis in teeth with incomplete root formation
N.M. Korneeva, E.A. Novikova, D.S. Popova, K.S. Rabadanova, L.Ya Rzaeva
Stomatology for All / International Dental review.2022; (2(99)): 10. CrossRef - Antimicrobial Effect of Calcium Hydroxide Combined with Electrolyzed Superoxidized Solution at Neutral pH on Enterococcus faecalis Growth
Héctor Armando Jimenez-Gonzalez, María Argelia Akemi Nakagoshi-Cepeda, Sergio Eduardo Nakagoshi-Cepeda, Víctor Hugo Urrutia-Baca, Myriam Angélica De La Garza-Ramos, Juan Manuel Solis-Soto, Ricardo Gomez-Flores, Patricia Tamez-Guerra, Yeliz Guven
BioMed Research International.2021;[Epub] CrossRef - Unpredictable Outcomes of a Regenerative Endodontic Treatment
Zahra Mohammadi, Hadi Assadian, Behnam Bolhari, Mohammadreza Sharifian, Mehrfam Khoshkhounejad, Nazanin Chitsaz, Andrea Scribante
Case Reports in Dentistry.2021;[Epub] CrossRef - Revascularization of nonvital immature incisor with asymptomatic apical periodontitis
Ema Mulyawati, Pribadi Santosa, Tunjung Nugraheni
Scientific Dental Journal.2020; 4(3): 134. CrossRef - Comparative analysis of calcium hydroxide apexification and regenerative endodontic procedure for root dentine growth stimulation in immature incisors with pulp necrosis
M.S. Rakhmanova, M.V. Korolenkova
Stomatologiya.2020; 99(6): 55. CrossRef - Antimicrobial Efficacy of a Novel Antibiotic‐Eluting Injectable Platelet‐Rich Fibrin Scaffold against a Dual‐Species Biofilm in an Infected Immature Root Canal Model
Azade Rafiee, Mahtab Memarpour, Yasaman Najibi, Bahman Khalvati, Sedigheh Kianpour, Mohammad Hossein Morowvat, Sung-Hwan Choi
BioMed Research International.2020;[Epub] CrossRef - Exosomes Derived from Stem Cells from the Apical Papilla Promote Dentine-Pulp Complex Regeneration by Inducing Specific Dentinogenesis
Xueying Zhuang, Lingli Ji, Huan Jiang, Yao Liu, Xuemei Liu, Jing Bi, Weidong Zhao, Zhenjiang Ding, Xu Chen
Stem Cells International.2020; 2020: 1. CrossRef - Injectable Biomaterials for Dental Tissue Regeneration
Håvard Jostein Haugen, Poulami Basu, Mousumi Sukul, João F Mano, Janne Elin Reseland
International Journal of Molecular Sciences.2020; 21(10): 3442. CrossRef - Viability and Stimulation of Human Stem Cells from the Apical Papilla (hSCAPs) Induced by Silicate-Based Materials for Their Potential Use in Regenerative Endodontics: A Systematic Review
José Luis Sanz, Leopoldo Forner, Alicia Almudéver, Julia Guerrero-Gironés, Carmen Llena
Materials.2020; 13(4): 974. CrossRef - An Innovative Drug Delivery System Loaded with a Modified Combination of Triple Antibiotics for Use in Endodontic Applications
Ardavan Parhizkar, Hanieh Nojehdehian, Fahimeh Tabatabaei, Saeed Asgary
International Journal of Dentistry.2020; 2020: 1. CrossRef - Defining Endodontic Residents' Clinical Experiences: A National Survey
Jonathan D. Blacher, Kamran E. Safavi, Robert H. Aseltine, Blythe M. Kaufman
Journal of Dental Education.2019; 83(5): 504. CrossRef - Coronal tooth discoloration induced by regenerative endodontic treatment using different scaffolds and intracanal coronal barriers: a 6-month ex vivo study
Noushin Shokouhinejad, Hassan Razmi, Maryam Farbod, Marzieh Alikhasi, Josette Camilleri
Restorative Dentistry & Endodontics.2019;[Epub] CrossRef - Comparative Study between Revitalization of Necrotic Immature Permanent Anterior Teeth with and without Platelet Rich Fibrin: A Randomized Controlled Trial
Rasha Adel Ragab, Amr Ezzat Abd El Lattif, Norhan Abd El Wahab El Dokky
Journal of Clinical Pediatric Dentistry.2019; 43(2): 78. CrossRef - Biomaterials and Scaffold Design Strategies for Regenerative Endodontic Therapy
Gavin Raddall, Isabel Mello, Brendan M. Leung
Frontiers in Bioengineering and Biotechnology.2019;[Epub] CrossRef - Iloprost Induces Dental Pulp Angiogenesis in a Growth Factor–free 3-Dimensional Organ Culture System
Sonntana Seang, Prasit Pavasant, Chalida N. Limjeerajarus
Journal of Endodontics.2018; 44(5): 759. CrossRef - Ratio and Rate of Induced Root Growth in Necrotic Immature Teeth
Eun Jung Sang, Ji-Soo Song, Teo Jeon Shin, Young-Jae Kim, Jung-Wook Kim, Ki-Taeg Jang, Sang-Hoon Lee, Hong-Keun Hyun
THE JOURNAL OF THE KOREAN ACADEMY OF PEDTATRIC DENTISTRY.2018; 45(2): 225. CrossRef - Triple antibiotic paste: momentous roles and applications in endodontics: a review
Ardavan Parhizkar, Hanieh Nojehdehian, Saeed Asgary
Restorative Dentistry & Endodontics.2018;[Epub] CrossRef - Traumatic avulsion and delayed replantation of maxillary incisors in an eleven-year-old child
Gokcen Deniz Bayrak
Edorium Journal of Dentistry.2018; 5(1): 1. CrossRef - Influence of Apical Diameter on the Outcome of Regenerative Endodontic Treatment in Teeth with Pulp Necrosis: A Review
Yanjun Fang, Xinhuan Wang, Jingjing Zhu, Chaonan Su, Ying Yang, Liuyan Meng
Journal of Endodontics.2018; 44(3): 414. CrossRef - Assessment of Regaining Pulp Sensibility in Mature Necrotic Teeth Using a Modified Revascularization Technique with Platelet-rich Fibrin: A Clinical Study
Mohamed Nageh, Geraldine M. Ahmed, Alaa A. El-Baz
Journal of Endodontics.2018; 44(10): 1526. CrossRef - Local drug delivery in endodontics: A literature review
Shin Hye Chung, Young-Seok Park
Journal of Drug Delivery Science and Technology.2017; 39: 334. CrossRef - Regenerative Endodontics
Kristina Feigin, Bonnie Shope
Journal of Veterinary Dentistry.2017; 34(3): 161. CrossRef - Intentional Replantation of an Avulsed Immature Permanent Incisor: A Case Report
Claudio Maniglia-Ferreira, Fabio de Almeida Gomes, Marcelo de Morais Vitoriano
Journal of Endodontics.2017; 43(8): 1383. CrossRef - Effect of acidic solutions on the microhardness of dentin and set OrthoMTA and their cytotoxicity on murine macrophage
Soram Oh, Hiran Perinpanayagam, Yoon Lee, Jae-Won Kum, Yeon-Jee Yoo, Sang-Min Lim, Seok Woo Chang, Won-Jun Shon, Woocheol Lee, Seung-Ho Baek, Kee-Yeon Kum
Restorative Dentistry & Endodontics.2016; 41(1): 12. CrossRef - Questioning the spot light on Hi-tech endodontics
Jojo Kottoor, Denzil Albuquerque
Restorative Dentistry & Endodontics.2016; 41(1): 80. CrossRef - Effects of a Bioactive Scaffold Containing a Sustained Transforming Growth Factor-β1–releasing Nanoparticle System on the Migration and Differentiation of Stem Cells from the Apical Papilla
Craig Bellamy, Suja Shrestha, Calvin Torneck, Anil Kishen
Journal of Endodontics.2016; 42(9): 1385. CrossRef - Effects of Novel 3-dimensional Antibiotic-containing Electrospun Scaffolds on Dentin Discoloration
Margaret Louise A. Porter, Eliseu A. Münchow, Maria T.P. Albuquerque, Kenneth J. Spolnik, Anderson T. Hara, Marco C. Bottino
Journal of Endodontics.2016; 42(1): 106. CrossRef
- Evaluation of the Clinical Outcomes of Regenerative Endodontic Procedures Using Autologous Platelet Concentrate: A Systematic Review and Meta-Analysis
- 6,580 View
- 101 Download
- 63 Crossref

- Platelet rich fibrin - a novel acumen into regenerative endodontic therapy
- Kavita Hotwani, Krishna Sharma
- Restor Dent Endod 2014;39(1):1-6. Published online January 20, 2014
- DOI: https://doi.org/10.5395/rde.2014.39.1.1
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Research into regenerative dentistry has added impetus onto the field of molecular biology. It can be documented as a prototype shift in the therapeutic armamentarium for dental disease. Regenerative endodontic procedures are widely being added to the current armamentarium of pulp therapy procedures. The regenerative potential of platelets has been deliberated. A new family of platelet concentrates called the platelet rich fibrin (PRF) has been recently used by several investigators and has shown application in diverse disciplines of dentistry. This paper is intended to add light on the various prospects of PRF and clinical insights to regenerative endodontic therapy.
-
Citations
Citations to this article as recorded by- Biomaterials to biofabrication: advanced scaffold technologies for regenerative endodontics
Arun Mayya, Akshatha Chatra, Vinita Dsouza, Raviraja N Seetharam, Shashi Rashmi Acharya, Kirthanashri S Vasanthan
Biomedical Physics & Engineering Express.2026; 12(1): 012001. CrossRef - Apicoectomy versus apical curettage in combination with or without L-PRF application: a randomized clinical trial
Serap Gulsever, Seyda Ersahan, Yelda Erdem Hepsenoglu, Alperen Tekin
Scientific Reports.2025;[Epub] CrossRef - Platelet-Rich Plasma and Platelet-Rich Fibrin in Endodontics: A Scoping Review
Simão Rebimbas Guerreiro, Carlos Miguel Marto, Anabela Paula, Joana Rita de Azevedo Pereira, Eunice Carrilho, Manuel Marques-Ferreira, Siri Vicente Paulo
International Journal of Molecular Sciences.2025; 26(12): 5479. CrossRef - Pulp regeneration treatment using different bioactive materials in permanent teeth of pediatric subjects
Dina Abdellatif, Alfredo Iandolo, Giuseppina De Benedetto, Francesco Giordano, Davide Mancino, Edouard Euvrard, Massimo Pisano
Journal of Conservative Dentistry and Endodontics.2024; 27(5): 458. CrossRef - Analysis of Pulp Tissue Viability and Cytotoxicity of Pulp Capping Agents
Pratima Panda, Shashirekha Govind, Sanjit Kumar Sahoo, Satabdi Pattanaik, Rachappa M. Mallikarjuna, Triveni Nalawade, Sanjay Saraf, Naseer Al Khaldi, Salma Al Jahdhami, Vinay Shivagange, Amit Jena
Journal of Clinical Medicine.2023; 12(2): 539. CrossRef - Implantation Effect of a Fibrin Matrix Associated with Mesenchymal Wharton’s Jelly Stromal Cells on the Course of an Experimental Spinal Cord Injury
V. V. Medvediev, N. P. Oleksenko, L. D. Pichkur, S. A. Verbovska, S. I. Savosko, N. G. Draguntsova, Yu. A. Lontkovskyi, V. V. Vaslovych, V. I. Tsymbalyuk
Cytology and Genetics.2023; 57(1): 19. CrossRef - Advanced Platelet-rich Fibrin-mediated Regeneration of Necrotic Immature Permanent Teeth: A Clinico-radiographic Observational Study
Ashi Chug, Sagrika Shukla, Tulika Wakhloo, Mridul Dhar
International Journal of Clinical Pediatric Dentistry.2022; 15(4): 402. CrossRef - Effect of Implantation of a Fibrin Matrix Associated with Neonatal Brain Cells on the Course of an Experimental Spinal Cord Injury
V. V. Medvediev, N. P. Oleksenko, L. D. Pichkur, S. A. Verbovska, S. I. Savosko, N. G. Draguntsova, Yu. A. Lontkovskiy, V. V. Vaslovych, V. I. Tsymbalyuk
Cytology and Genetics.2022; 56(2): 125. CrossRef - Comparison of Autologous Platelet-Rich Fibrin Matrix and Transplantation of Autologous Noncultured Epidermal Cell Suspension in the Treatment of Chronic Non Healing Ulcer
Satyendra K. Singh, Sri Rupa
Indian Journal of Dermatology.2022; 67(4): 334. CrossRef - Effect of amniotic membrane and platelet‐rich fibrin membrane on bone healing post endodontic surgery: An ultrasonographic, randomized controlled study
Saumya Johri, Promila Verma, Aseem Prakash Tikku, Rhythm Bains, Neera Kohli
Journal of Tissue Engineering and Regenerative Medicine.2022; 16(12): 1208. CrossRef - Effect of biodentine coated with emdogain on proliferation and differentiation of human stem cells from the apical papilla
Hamed Karkehabadi, Erfan Ahmadyani, Rezvan Najafi, Elham Khoshbin
Molecular Biology Reports.2022; 49(5): 3685. CrossRef - SINGLE VISIT- APEXIFICATION USING MTA AND AUTOLOGOUS PRF AS AN INTERNAL MATRIX. A CASE SERIES.
Deepika Deepika, Abhishek Sharma, Ajay Kumar Nagpal, Muhammad Mutiur Rahman
INTERNATIONAL JOURNAL OF SCIENTIFIC RESEARCH.2022; : 61. CrossRef - COMPARATIVE CLINICAL, RADIOGRAPHICAL AND HISTOLOGICAL EVALUATION OF CORONAL PULPOTOMY TECHNIQUE WITH PRF AND A NOVEL CROSSLINKED PRF AS AN ALTERNATIVE TO PULPECTOMY FOR PRESERVING THE TOOTH VITALITY IN CONTEXT OF TISSUE ENGINEERING.
Suman Kar, R. R. Paul, H. D. Adhikari, Swagata Gayen, Sandip Sinha
INTERNATIONAL JOURNAL OF SCIENTIFIC RESEARCH.2022; : 84. CrossRef - Clinical Application of Platelet-Rich Fibrin in Pediatric Dentistry
Sowndarya Gunasekaran, Soundarya Sakthivel, Shanthala B. M., George Babu, Vidhya Vijayan
Journal of Health and Allied Sciences NU.2022; 12(02): 186. CrossRef - Platelet-Rich Fibrin Used as a Scaffold in Pulp Regeneration: Case Series
Ceren ÇİMEN, Selin ŞEN, Elif ŞENAY, Tuğba BEZGİN
Cumhuriyet Dental Journal.2021; 24(1): 113. CrossRef - Treatment of Miller I Mandibular Gingival Recessions Using PRF vs. Connective Graft
Hernan S. Garzon, Camilo Alfonso, Francisco J. Vega, Andrea García, Ana Muñoz, Gustavo Jaimes, Katherine Isaza, Katherine Rivera, Gaetano Isola
International Journal of Dentistry.2021; 2021: 1. CrossRef - Human Umbilical Cord Mesenchymal Stem Cells Over Platelet Rich Fibrin Scaffold for Mandibular Cartilage Defects Regenerative Medicine
Ni Putu Mira Sumarta, David Buntoro Kamadjaja, Nike Hendrijantini, Coen Pramono Danudiningrat, Fedik Abdul Rantam
Pesquisa Brasileira em Odontopediatria e Clínica Integrada.2021;[Epub] CrossRef - Platelet-Rich Fibrin Enhances Surgical Wound Healing in Total Laryngectomy
Mirta H. Reksodiputro, Syahrial M. Hutauruk, Dini W. Widodo, Fauziah Fardizza, Dita Mutia
Facial Plastic Surgery.2021; 37(03): 325. CrossRef - Role of Platelet-Rich Fibrin (PRF) and Platelet-Rich Plasma (PRP) in Oro-Facial Tissue Regeneration: A Narrative Review
Modhi Al Deeb
Journal of Advanced Oral Research.2020; 11(1): 5. CrossRef - Efficacy of Autologous Platelet Concentrates in Regenerative Endodontic Treatment: A Systematic Review of Human Studies
Joanna Metlerska, Irini Fagogeni, Alicja Nowicka
Journal of Endodontics.2019; 45(1): 20. CrossRef - Autologous platelet-rich-fibrin-induced revascularization sequelae: Two case reports
Ahmed M Eltawila, Rania El Backly
World Journal of Stomatology.2019; 7(3): 28. CrossRef - Revascularization of a Nonvital, Immature Permanent Tooth Using Amniotic Membrane: A Novel Approach
Meghna Bajaj, Ashu J Soni
International Journal of Clinical Pediatric Dentistry.2019; 12(2): 150. CrossRef - Biomimetics in Endodontics: A Review of the Changing Trends in Endodontics
Jalak Patel, Tejal Sheth, Dhwanit Thakore, Dharmesh Dhamat
Journal of Advanced Oral Research.2018; 9(1-2): 11. CrossRef - Regenerative in endodontics: how, when and where
AL Ahmar Rima, Bassam Sanaa, Salloum Sarah, El Husseini Hassan, AL Ahmar Rima
Journal of Dental Health, Oral Disorders & Therapy.2018; 9(6): 531. CrossRef - Effects of the nitric oxide releasing biomimetic nanomatrix gel on pulp-dentin regeneration: Pilot study
Chan-Yang Moon, Ok Hyung Nam, Misun Kim, Hyo-Seol Lee, Sagar N. Kaushik, David A. Cruz Walma, Ho-Wook Jun, Kyounga Cheon, Sung Chul Choi, Jinkee Hong
PLOS ONE.2018; 13(10): e0205534. CrossRef - Growth Factors and Cell Homing in Dental Tissue Regeneration
Henry F. Duncan, Yoshifumi Kobayashi, Emi Shimizu
Current Oral Health Reports.2018; 5(4): 276. CrossRef - Use of Leukocyte Platelet (L-PRF) Rich Fibrin in Diabetic Foot Ulcer with Osteomyelitis (Three Clinical Cases Report)
Alessandro Crisci, Giuseppe Marotta, Anna Licito, Edda Serra, Giulio Benincasa, Michela Crisci
Diseases.2018; 6(2): 30. CrossRef - Pulp Regeneration Concepts for Nonvital Teeth: From Tissue Engineering to Clinical Approaches
Valérie Orti, Pierre-Yves Collart-Dutilleul, Sofía Piglionico, Orsolya Pall, Frédéric Cuisinier, Ivan Panayotov
Tissue Engineering Part B: Reviews.2018; 24(6): 419. CrossRef - Long-term cytokine and growth factor release from equine platelet-rich fibrin clots obtained with two different centrifugation protocols
Román F. Jiménez-Aristizabal, Catalina López, María E. Álvarez, Carlos Giraldo, Marta Prades, Jorge U. Carmona
Cytokine.2017; 97: 149. CrossRef - Rejeneratif Pulpa Tedavilerine Genel Bir Bakış
Elif Sungurtekin Ekçi
Cumhuriyet Dental Journal.2017; 19(3): 238. CrossRef - Three-dimensional structure and cytokine distribution of platelet-rich fibrin
Meng-Yi Bai, Ching-Wei Wang, Jyun-Yi Wang, Ming-Fang Lin, Wing P Chan
Clinics.2017; 72(2): 116. CrossRef - The impact of autologous platelet concentrates on endodontic healing: a systematic review
Nastaran Meschi, Ana B. Castro, Katleen Vandamme, Marc Quirynen, Paul Lambrechts
Platelets.2016; 27(7): 613. CrossRef - Platelet concentrates for revitalization of immature necrotic teeth: a systematic review of the clinical studies
Alessandra Lolato, Cristina Bucchi, Silvio Taschieri, Ahmed El Kabbaney, Massimo Del Fabbro
Platelets.2016; 27(5): 383. CrossRef - Endodontie in der unreifen bleibenden Dentition — Maßnahmen zur Vitalerhaltung, Apexifikation und Regeneration der Pulpa
Martin Jung
Oralprophylaxe & Kinderzahnheilkunde.2016; 38(1): 29. CrossRef - A review of the regenerative endodontic treatment procedure
Bin-Na Lee, Jong-Wook Moon, Hoon-Sang Chang, In-Nam Hwang, Won-Mann Oh, Yun-Chan Hwang
Restorative Dentistry & Endodontics.2015; 40(3): 179. CrossRef - Platelet preparations in dentistry: How? Why? Where? When?
Luigi Fabrizio Rodella
World Journal of Stomatology.2015; 4(2): 39. CrossRef - The use of platelet rich plasma in the treatment of immature tooth with periapical lesion: a case report
Günseli Güven Polat, Ceren Yıldırım, Özlem Martı Akgün, Ceyhan Altun, Didem Dinçer, Cansel Köse Özkan
Restorative Dentistry & Endodontics.2014; 39(3): 230. CrossRef
- Biomaterials to biofabrication: advanced scaffold technologies for regenerative endodontics
- 2,367 View
- 19 Download
- 37 Crossref

- Prevention of tooth discoloration associated with triple antibiotics
- Bona Kim, Min-Ju Song, Su-Jung Shin, Jeong-Won Park
- Restor Dent Endod 2012;37(2):119-122. Published online May 18, 2012
- DOI: https://doi.org/10.5395/rde.2012.37.2.119
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Regenerative endodontics has a potential to heal a partially necrotic pulp, which can be beneficial for the continued root development and strengthening of immature teeth. For this purpose, triple antibiotic mixture of ciprofloxacin, metronidazole, and minocycline was recommended as intracanal medicament in an attempt to disinfect the root canal system for revascularization of a tooth with a necrotic pulp. However, discoloration of the tooth was reported after applying this. This case shows the idea for preventing the tooth discoloration using a delivery syringe (SW-O-01, Shinwoo dental) to avoid the contact between the clinical crown and the antibiotics.
-
Citations
Citations to this article as recorded by- Non-surgical Management of a Large Periapical Lesion: A Case Study of the Successful Application of a Modified Triple Antibacterial Paste
Srushti Awghad, Joyeeta Mahapatra, Amit Reche, Ankita Burse, Aradhana Kibe
Cureus.2024;[Epub] CrossRef - Evaluation of the antimicrobial efficacy of two combinations of drugs on bacteria taken from infected primary teeth (in vitro)
R. Rafatjou, R. Yousefimashouf, M. Farhadian, S. Afzalsoltani
European Archives of Paediatric Dentistry.2019; 20(6): 609. CrossRef - Triple antibiotic paste: momentous roles and applications in endodontics: a review
Ardavan Parhizkar, Hanieh Nojehdehian, Saeed Asgary
Restorative Dentistry & Endodontics.2018;[Epub] CrossRef - Clinical Effectiveness of Different Polishing Systems and Self-Etch Adhesives in Class V Composite Resin Restorations: Two-Year Randomized Controlled Clinical Trial
J-H Jang, H-Y Kim, S-M Shin, C-O Lee, DS Kim, K-K Choi, S-Y Kim
Operative Dentistry.2017; 42(1): 19. CrossRef - Revascularization of Necrotic Immature Permanent Teeth: An Update
N Velmurugan
Journal of Operative Dentistry & Endodontics.2016; 1(1): 18. CrossRef - Treatment of non-vital immature teeth with amoxicillin-containing triple antibiotic paste resulting in apexification
Hyon-Beom Park, Bin-Na Lee, Yun-Chan Hwang, In-Nam Hwang, Won-Mann Oh, Hoon-Sang Chang
Restorative Dentistry & Endodontics.2015; 40(4): 322. CrossRef
- Non-surgical Management of a Large Periapical Lesion: A Case Study of the Successful Application of a Modified Triple Antibacterial Paste
- 1,102 View
- 3 Download
- 6 Crossref


 KACD
KACD

 First
First Prev
Prev


