Articles
- Page Path
- HOME > Restor Dent Endod > Volume 42(1); 2017 > Article
- Case Report Retreatment of failed regenerative endodontic of orthodontically treated immature permanent maxillary central incisor: a case report
- Musaed Fahad Al-Tammami1, Saad A. Al-Nazhan2
-
2016;42(1):-71.
DOI: https://doi.org/10.5395/rde.2017.42.1.65
Published online: October 28, 2016
1Security Force Hospital, Dental Department, Riyadh, Saudi Arabia.
2Department of Restorative Dental Science, Division of Endodontics, King Saudi University, College of Dentistry, Riyadh, Saudi Arabia.
- Correspondence to Saad A. Al-Nazhan, BDS, MSD. Professor, Department of Restorative Dental Science, Division of Endodontics, King Saudi University, College of Dentistry, P.O. Box 60169, Riyadh, Saudi Arabia 11545. TEL, +966-14677420; FAX, +966-14677329; snazhan@ksu.edu.sa
• Received: July 5, 2016 • Accepted: August 30, 2016
©Copyrights 2017. The Korean Academy of Conservative Dentistry.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 1,823 Views
- 15 Download
- 12 Crossref
Abstract
- A revascularization procedure was shown to be the best alternative therapy for immature teeth with necrotic pulp and apical infection. A 12 year old female with a history of trauma to her upper central incisor and a sinus tract was referred for endodontic treatment. She was an active orthodontic patient and had undergone regenerative endodontic treatment for the past 2 years. Clinical examination revealed no response to sensibility, percussion, and palpation tests. The preoperative radiograph showed an open apex and apical rarefaction. The case was diagnosed as previously treated tooth with asymptomatic apical periodontitis. Regenerative endodontic retreatment was performed, and the case was followed for 3 years. Clinical, radiographic, and cone-beam computed tomography follow-up examination revealed an asymptomatic tooth, with evidence of periapical healing and root maturation.
Introduction
Dental trauma is the most common cause of cessation of root development in permanent teeth.1 The management of the immature teeth is one of the most challenging situations in endodontics. In such cases, chemomechanical debridement as well as placement of filling materials to seal the root apex cannot be performed due to weak roots. Calcium hydroxide multiple-visit apexification followed by a one-visit mineral trioxide aggregate (MTA) apical plug used to be the treatment of choice.2,3,4 Although the success rate was high,5,6 the long-term use of calcium hydroxide was reported to increase the risk of root fracture.7 In contrast, the use of MTA prevents dentin weakening.8 Limited potential for further development of the root with the use of calcium hydroxide and MTA has been demonstrated.9 Thus, regenerative endodontic treatment was proposed in which the infected root canal is disinfected, followed by induction of bleeding through irritation of periradicular tissue and a coronal seal.10,11,12 It is recommended for patients between 8 and 16 years old.3 This procedure promotes root development with a 100% survival rate.14 However, failure of the therapy has been reported, with successful retreatment.15
Trauma to anterior teeth may cause pulpal necrosis and displacement of the teeth, requiring endodontic as well as orthodontic treatment. Andreasen et al.16 reported that endodontic treatment should be performed prior to orthodontic treatment in traumatized teeth with necrotic pulp. This report presents a case of retreatment of failed revascularization of an orthodontically treated immature traumatized permanent maxillary incisor.
Case Report
A 12 year old girl was referred from an orthodontic clinic to evaluate and treat the maxillary right central incisor (tooth #11). Her previous dental history was that the patient had trauma at age 9 years that affected her maxillary central incisors. She was referred by an orthodontist to a pedodontist in a private clinic to evaluate the traumatized teeth. An apexification was done for the maxillary left central incisor (tooth #21) using calcium hydroxide (Figure 1a) then she was referred back to her orthodontist who started the orthodontic treatment after one year. The patient developed buccal swelling one week after initiating the orthodontic treatment and the orthodontist sent the patient back to the pedodontist for the treatment on tooth #11. A regenerative endodontic retreatment was performed using MTA on tooth #11.
When this patient visited our clinic, she was an active orthodontic patient (Figure 1b). The tooth was asymptomatic and had a buccal sinus tract (Figure 1c). The medical history was unremarkable. Radiographic evaluation showed an immature open apex, with a large periradicular rarefaction and radiopaque material inside the root canal (Figure 1d). The intra-oral exam revealed an asymptomatic tooth #11 with an associated draining sinus tract. Clinical examination revealed no response to percussion and palpation tests. The tooth showed no mobility, and periodontal probing was within normal limits. The clinical diagnosis was previously treated asymptomatic periapical periodontitis.
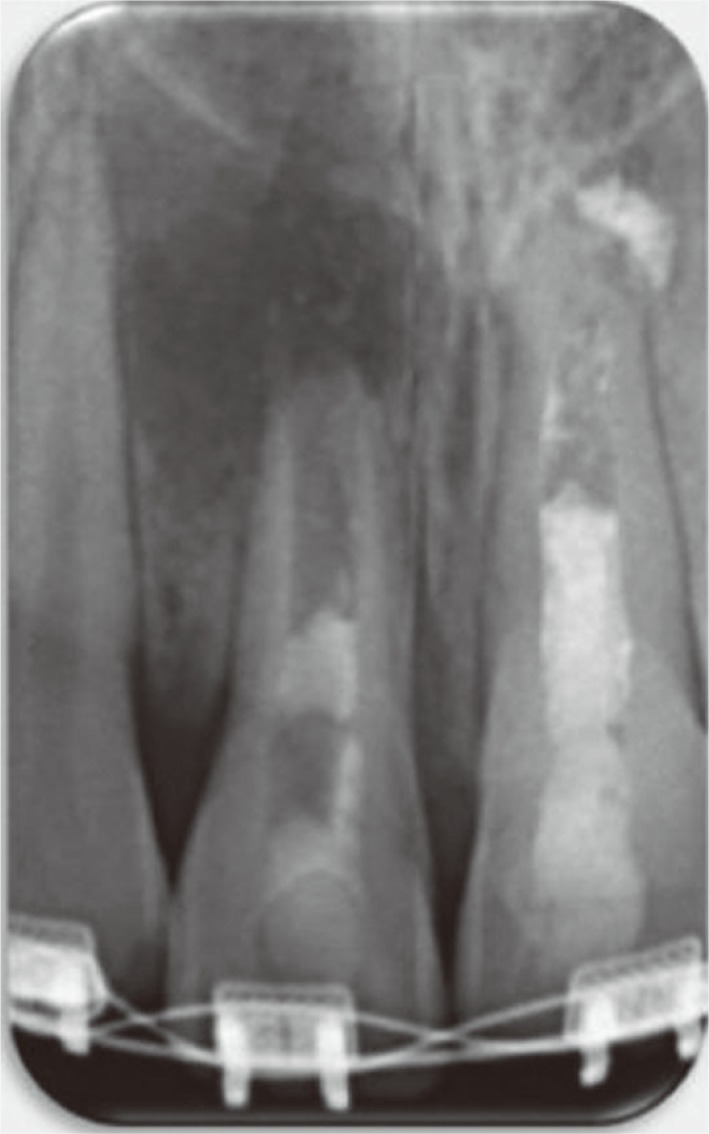
The treatment options were discussed with the patient's mother. It was decided that the patient would benefit from another revascularization procedure rather than regular apexification or an apical plug. A consent form was signed after approval of the proposed protocol to initiate revascularization treatment. A rubber dam was applied, and the tooth was accessed following local anesthesia (1.8 mL of 2% lidocaine with 1:100,000 epinephrine) administration using a dental operating microscope (Global Surgical Corp., St. Louis, MO, USA). The MTA root canal filling was removed with CPR ultrasonic tips (Obtura Spartan Endodontics, Algonquin, IL, USA) set at low power. The vibration of the CPR ultrasonic tips caused the MTA filling materials to break up into pieces, and then the canal was flushed with saline to remove root canal filling debris, irrigated with 20 mL of 5.25% sodium hypochlorite (Henry Schein, Melville, NY, USA), and then rinsed with sterile saline solution. The pulp chamber was carefully dried with paper points and filled with double antibiotic paste (DAP) consisting of a mixture of ciprofloxacin (Ciprobay, Bayer Pharma, Leverkusen, Germany) and metronidazole (Flagyl, Sanofi Aventis, Frankfurt, Germany) in a 1:1 ratio prepared with saline (wt/vol 2.5:1) using a lentulo spiral (Dentsply, Maillefer, Ballaigues, Switzerland). Access was sealed with temporary filling material (Cavit, 3M ESPE, St. Paul, MN, USA), and a radiograph was taken (Figure 2).
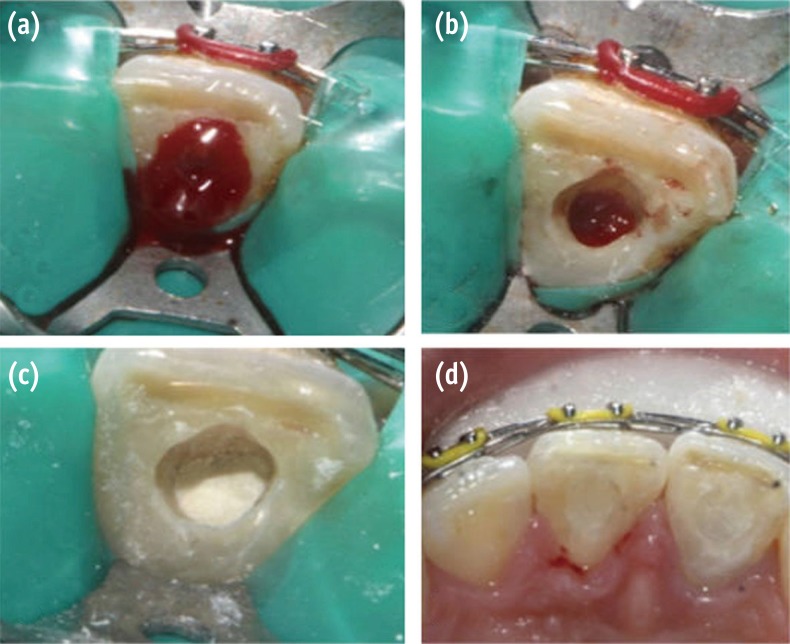
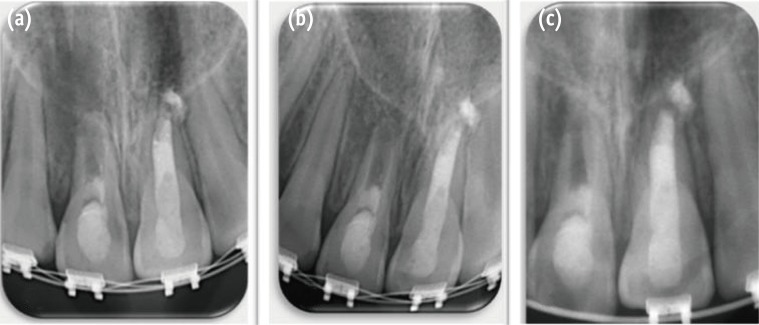
Two weeks later, the tooth was still asymptomatic, and the sinus tract had healed. The tooth was anesthetized with 3% mepivacaine hydrochlor ide without a vasoconstrictor (Polocaine dental, Dentsply Pharmaceutical, York, PA, USA). A rubber dam was placed, and the canal was irrigated with 20 mL of 5.25% sodium hypochlorite to remove the DAP and then rinsed with sterile saline solution and 10 mL of 0.12% chlorhexidine gluconate (Vista Dental, Racine, WI, USA) for 5 minutes. The canal was dried with paper points, and bleeding was induced by gentle irritation of the canal apical tissue with a size 70 K-file (Dentsply Maillefer) (Figure 3a). A layer of 'CollaPlug' resorbable matrix (Zimmer Dental, Carlsbad, CA, USA) was coronally placed over the blood clot to act as a barrier (Figure 3b). A 3 mm thick layer of white MTA (MTA-Angelus, Angelus, Londrina, PR, Brazil) was gently condensed over the CollaPlug matrix to seal the canal system (Figure 3c). A moistened cotton pellet was placed over the MTA, and the access cavity was temporized. The patient returned after 1 week for placement of the final restoration of bonded composite resin (Filtek Z250 XT, 3M ESPE) after removal of the wet cotton pellet and checking the setting of the MTA with an explorer (Figure 3d). The root canal of tooth #21 was cleaned and the apical third was plugged with MTA and the remaining canal was filled with gutta-percha and AH26 sealer (Dentsply De Trey GmbH, Konstanz, Germany). The coronal access was sealed with bonded composite resin.
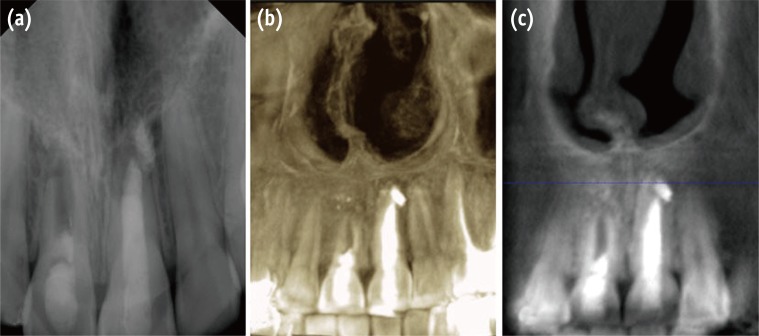
At 3 and 6 months follow-up, the patient was asymptomatic, and slight healing of the apical radiolucency was noticed (Figures 4a and 4b). The orthodontist was advised to use no force on the tooth. At the 12 months follow-up appointment, the patient remained asymptomatic, and the orthodontic appliances were removed. Radiographic examination demonstrated evidence of periradicular bone healing (Figure 4c). At the 3 year recall appointment, the patient was asymptomatic, and a periapical radiograph showed disappearance of the apical radiolucency and closure of the root apex (Figure 5a). The treatment outcome was confirmed with cone beam computed tomography (CBCT) images (Figures 5b and 5c).
Discussion
The treatment outcome of regenerative endodontics is usually determined by the status of the pulp tissue and size of the apical opening.17,18 Unfavorable outcomes, including poor or no root development and coronal discoloration, have been reported.10,19
In the case presented here, the radiographic and CBCT images demonstrated disappearance of periapical radiolucency and closure of the apical foramen without any significant increase in root length or root wall thickness. Similar findings have been reported previously.18,19,20,21 The periapical radiolucency usually disappears within 1 year of successful pulp revascularization,11,22,23,24 as was found in the present case. Healing of the periapical lesion after regenerative endodontic treatment has been demonstrated by Lenzi and Trope25 regardless of the absence of vital tissue inside the canal space. They attributed this to the disinfection protocol used during regenerative endodontic treatments. Closure of the apical foramen in immature teeth treated with regenerative endodontic procedures is achieved by growth of the periodontal ligament tissue as well as the deposition of cementum inside the canal space.26 In addition, Lin et al.27 and Shi et al.28 reported that the survival of postnatal dental pulp stem cells is facilitated by a rich apical blood supply at the open apex. These cells reside in the tissue of the dental pulp regardless of the status of the periapical tissue. The failure of root development was likely related to the previous trauma, persistent apical pathosis, poor endodontic management, and force applied in orthodontic treatment. It is believed that this causes the Hertwig epithelial root sheath, which is associated with root development, to lose its vitality.18,19,26,29,30 Chen et al.18 evaluated root developmental patterns with conventional radiographs. They reported that five types of root development pattern can occur as a result of regenerative endodontic procedures, all of which are based on survival of the Hertwig epithelial root sheath. The type 2 root development pattern, described as 'no significant continuation of root development with the root apex becoming blunt and closed', was seen radiographically and was confirmed with CBCT in the present case. This was achieved through good management of the failed treatment. Similar findings have been reported previously.19
The patient in the current case was under active orthodontic treatment. Such treatment does not interfere with root development if performed in immature vital teeth,31 but it delays the healing of periapical lesions of endodontically treated teeth.32 However, in cases of traumatized immature necrotic teeth with periapical pathosis requiring endodontic treatment, the applied orthodontic force exerts an additional inflammatory stimulus to the tooth that might prolong the destructive phase acting on the cementum.33 This may interfere with root development, causing failure of the regenerative procedure. Therefore, orthodontic treatment should be delayed for at least 1 year to enable observation of periradicular healing as well as root development.33,34,35
In the present case, the root canal was irrigated with 5.25% sodium hypochlorite and medicated with DAP. Minocycline was not used, as it causes discoloration of the tooth.36 Triple antibiotic paste (TAP) has been recommended by the American Association of Endodontists as a disinfectant for pulp revascularization.37 Its high concentration was reported to be detrimental to dental stem cell survival.38,39 In addition, TAP has a low pH compared to DAP,40 and the presence of minocycline in TAP was suggested to chelate calcium and demineralize dental hard tissues.41
Chlorhexidine was used before initiating bleeding. It is an effective antimicrobial irrigant that is frequently used in nonsurgical root canal treatment.42 However, it has been reported that its use in immature teeth might be detrimental to the survival of stem cells.43 This might be one of the reasons for incomplete apical closure. Collagen matrix (CollaPlug) was reported to be useful for the controlled placement of MTA.10 A double seal of MTA and composite resin restoration was placed over the CollaPlug material to provide a tight coronal seal against bacterial leakage. This is very important for the successful outcome of regenerative endodontics.21,44 MTA releases calcium ions, which react with environmental phosphorus, leading to the formation of hydroxyapatite crystals on the surface of the MTA as well as the MTA-dentin interface.45,46
Conclusions
In conclusion, retreatment of failed regenerative endodontics performed on an orthodontically active patient achieved healing of the periapical radiolucency and continuation of root development without thickening of the canal walls.
- 1. Andreasen JO, Ravn JJ. Epidemiology of traumatic dental injuries to primary and permanent teeth in a Danish population sample. Int J Oral Surg 1972;1:235-239.ArticlePubMed
- 2. Morse DR, O'Larnic J, Yesilsoy C. Apexification: review of the literature. Quintessence Int 1990;21:589-598.PubMed
- 3. Pace R, Giuliani V, Pini Prato L, Baccetti T, Pagavino G. Apical plug technique using mineral trioxide aggregate: results from a case series. Int Endod J 2007;40:478-484.ArticlePubMed
- 4. Chala S, Abouqal R, Rida S. Apexification of immature teeth with calcium hydroxide or mineral trioxide aggregate: systematic review and meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2011;112:e36-e42.Article
- 5. Sheehy EC, Roberts GJ. Use of calcium hydroxide for apical barrier formation and healing in non-vital immature permanent teeth: a review. Br Dent J 1997;183:241-246.ArticlePubMedPDF
- 6. Simon S, Rillard F, Berdal A, Machtou P. The use of mineral trioxide aggregate in one visit apexification treatment: a prospective study. Int Endod J 2007;40:186-197.ArticlePubMed
- 7. Andreason JO, Farik B, Munksgaard EC. Long-term calcium hydroxide as a root canal dressing may increase risk of root fracture. Dent Traumatol 2002;18:134-137.ArticlePubMedPDF
- 8. Andreasen JO, Munksgaard EC, Bakland LK. Comparison of fracture resistance in root canals of immature sheep teeth after filling with calcium hydroxide or MTA. Dent Traumatol 2006;22:154-156.ArticlePubMed
- 9. Nagy MM, Tawfik HE, Hashem AA, Abu-Seida AM. Regenerative potential of immature permanent teeth with necrotic pulps after different regenerative protocols. J Endod 2014;40:192-198.ArticlePubMed
- 10. Petrino JA, Boda KK, Shambarger S, Bowles WR, McClanahan SB. Challenges in regenerative endodontics: a case series. J Endod 2010;36:536-541.ArticlePubMed
- 11. Cehreli ZC, Isbitiren B, Sara S, Erbas G. Regenerative endodontic treatment (revascularization) of immature necrotic molars medicated with calcium hydroxide: a case series. J Endod 2011;37:1327-1330.ArticlePubMed
- 12. Al-Ghamdi NS, Al-Nazhan S. Pulp revascularization of immature maxillary first premolar. J Conserv Dent 2015;18:496-499.ArticlePubMedPMC
- 13. Garcia-Godoy F, Murray PE. Recommendations for using regenerative endodontic procedures in permanent immature traumatized teeth. Dent Traumatol 2012;28:33-41.ArticlePubMed
- 14. Jeeruphan T, Jantarat J, Yanpiset K, Suwannapan , Khewsawai P, Hargreaves KM. Mahidol study 1: comparison of radiographic and survival outcomes of immature teeth treated with either regenerative endodontic or apexification methods: a retrospective study. J Endod 2012;38:1330-1336.ArticlePubMed
- 15. Miltiadous ME, Floratos SG. Regenerative endodontic treatment as a retreatment option for a tooth with open apex - a case report. Braz Dent J 2015;26:552-556.ArticlePubMed
- 16. Andreasen JO, Bakland LK, Flores MT, Andreasen FM, Andersson L. Traumatic dental injuries: a manual. 3rd ed. West Sussex: Wiley-Blackwell; 2011. p. 12. p. 29. p. 35. p. 63-72.
- 17. Iwaya SI, Ikawa M, Kubota M. Revascularization of an immature permanent tooth with apical periodontitis and sinus tract. Dent Traumatol 2001;17:185-187.ArticlePubMedPDF
- 18. Chen MY, Chen KL, Chen CA, Tayebaty F, Rosenberg PA, Lin LM. Responses of immature permanent teeth with infected necrotic pulp tissue and apical periodontitis/abscess to revascularization procedures. Int Endod J 2012;45:294-305.ArticlePubMed
- 19. Nosrat A, Homayounfar N, Oloomi K. Drawbacks and unfavorable outcomes of regenerative endodontic treatments of necrotic immature teeth: a literature review and report of a case. J Endod 2012;38:1428-1434.ArticlePubMed
- 20. Bose R, Nummikoski P, Hargreaves K. A retrospective evaluation of radiographic outcomes in immature teeth with necrotic root canal systems treated with regenerative endodontic procedures. J Endod 2009;35:1343-1349.ArticlePubMed
- 21. Wang Y, Zhu X, Zhang C. Pulp revascularization on permanent teeth with open apices in a middle-aged patient. J Endod 2015;41:1571-1575.ArticlePubMed
- 22. Jadhav G, Shah N, Logani A. Revascularization with and without platelet-rich plasma in nonvital, immature, anterior teeth: a pilot clinical study. J Endod 2012;38:1581-1587.ArticlePubMed
- 23. Bezgin T, Yilmaz AD, Celik BN, Sönmez H. Concentrated platelet-rich plasma used in root canal revascularization: 2 case reports. Int Endod J 2014;47:41-49.ArticlePubMed
- 24. Kim JH, Kim Y, Shin SJ, Park JW, Jung IY. Tooth discoloration of immature permanent incisor associated with triple antibiotic therapy: a case report. J Endod 2010;36:1086-1091.ArticlePubMed
- 25. Lenzi R, Trope M. Revitalization procedures in two traumatized incisors with different biological outcomes. J Endod 2012;38:411-414.ArticlePubMed
- 26. Thibodeau B, Teixeira F, Yamauchi M, Caplan DJ, Trope M. Pulp revascularization of immature dog teeth with apical periodontitis. J Endod 2007;33:680-689.ArticlePubMed
- 27. Lin L, Shovlin F, Skribner J, Langeland K. Pulp biopsies from the teeth associated with periapical radiolucency. J Endod 1984;10:436-448.ArticlePubMed
- 28. Shi S, Gronthos S. Perivascular niche of postnatal mesenchymal stem cells in human bone marrow and dental pulp. J Bone Miner Res 2003;18:696-704.ArticlePubMedPDF
- 29. Nosrat A, Li KL, Vir K, Hicks ML, Fouad AF. Is pulp regeneration necessary for root maturation? J Endod 2013;39:1291-1295.ArticlePubMed
- 30. Lin LM, Rosenberg PA. Repair and regeneration in endodontics. Int Endod J 2011;44:889-906.ArticlePubMed
- 31. Mavragani M, Bøe OE, Wisth PJ, Selvig KA. Changes in root length during orthodontic treatment: advantages for immature teeth. Eur J Orthod 2002;24:91-97.ArticlePubMed
- 32. de Souza RS, Gandini LG Jr, de Souza V, Holland R, Dezan E Jr. Influence of orthodontic dental movement on the healing process of teeth with periapical lesions. J Endod 2006;32:115-119.ArticlePubMed
- 33. Beck VJ, Stacknik S, Chandler NP, Farella M. Orthodontic tooth movement of traumatised or root-canal-treated teeth: a clinical review. N Z Dent J 2013;109:6-11.PubMed
- 34. Drysdale C, Gibbs SL, Ford TR. Orthodontic management of root-filled teeth. Br J Orthod 1996;23:255-260.ArticlePubMedPDF
- 35. Malmgren O, Malmgren B. Orthodontic management of the traumatised dentition. In: Andreasen JO, Andreasen FM, Andersson L, editors. Textbook and color atlas of traumatic injuries to the teeth. 4th ed. Oxford: Blackwell; 2007. p. 669-715.
- 36. Nagata JY, Gomes BP, Rocha Lima TF, Murakami LS, de Faria DE, Campos GR, de Souza-Filho FJ, Soares Ade J. Traumatized immature teeth treated with 2 protocols of pulp revascularization. J Endod 2014;40:606-612.ArticlePubMed
- 37. American Association of Endodontists: Clinical resources, regenerative endodontics. AAE clinical considerations for a regenerative procedure. updated Oct 9, 2016]. Available from: http://www.aae.org/uploadedfiles/publications_and_research/research/currentregenerativeendodonticconsiderations.pdf.
- 38. Ruparel NB, Teixeira FB, Ferraz CC, Diogenes A. Direct effect of intracanal medicaments on survival of stem cells of the apical papilla. J Endod 2012;38:1372-1375.ArticlePubMed
- 39. Chuensombat S, Khemaleelakul S, Chattipakorn S, Srisuwan T. Cytotoxic effects and antibacterial efficacy of a 3-antibiotic combination: an in vitro study. J Endod 2013;39:813-819.ArticlePubMed
- 40. Yassen GH, Chu TM, Eckert G, Platt JA. Effect of medicaments used in endodontic regeneration technique on the chemical structure of human immature radicular dentin: an in vitro study. J Endod 2013;39:269-273.ArticlePubMed
- 41. Maruyama H, Aoki A, Sasaki KM, Takasaki AA, Iwasaki K, Ichinose S, Oda S, Ishikawa I, Izumi Y. The effect of chemical and/or mechanical conditioning on the Er:YAG laser-treated root cementum: analysis of surface morphology and periodontal ligament fibroblast attachment. Lasers Surg Med 2008;40:211-222.ArticlePubMed
- 42. Gomes BP, Vianna ME, Zaia AA, Almeida JF, Souza-Filho FJ, Ferraz CC. Chlorhexidine in endodontics. Braz Dent J 2013;24:89-102.ArticlePubMed
- 43. Trevino EG, Patwardhan AN, Henry MA, Perry G, Dybdal-Hargreaves N, Hargreaves KM, Diogenes A. Effect of irrigants on the survival of human stem cells of the apical papilla in a platelet-rich plasma scaffold in human root tips. J Endod 2011;37:1109-1115.ArticlePubMed
- 44. Forghani M, Parisay I, Maghsoudlou A. Apexogenesis and revascularization treatment procedures for two traumatized immature permanent maxillary incisors: a case report. Restor Dent Endod 2013;38:178-181.ArticlePubMedPMC
- 45. Asgary S, Eghbal MJ, Parirokh M, Ghoddusi J. Effect of two storage solutions on surface topography of two root-end fillings. Aust Endod J 2009;35:147-152.ArticlePubMed
- 46. Sarkar NK, Caicedo R, Ritwik P, Moiseyeva R, Kawashima I. Physicochemical basis of the biologic properties of mineral trioxide aggregate. J Endod 2005;31:97-100.ArticlePubMed
REFERENCES
Figure 1
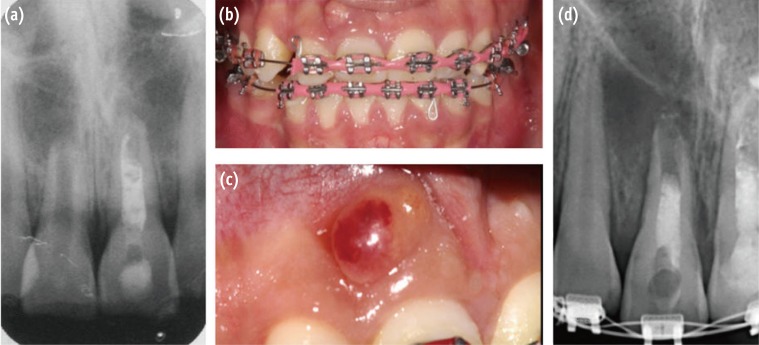
(a) Diagnostic radiograph of the maxillary right central incisor (tooth #11) demonstrated incomplete root formation with diffuse periapical radiolucency and poor root canal filling; (b and c) Preoperative clinical photograph illustrates orthodontic treatment and the sinus tract related to tooth #11; (d) Periapical radiograph during orthodontic examination and before regenerative endodontic treatment that shows an open apex with apical rarefaction.
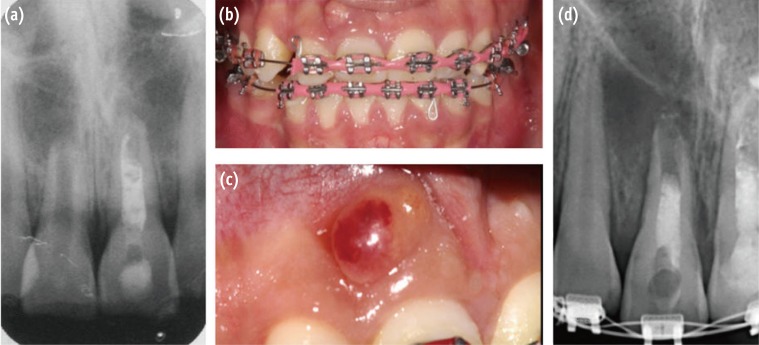
Figure 3
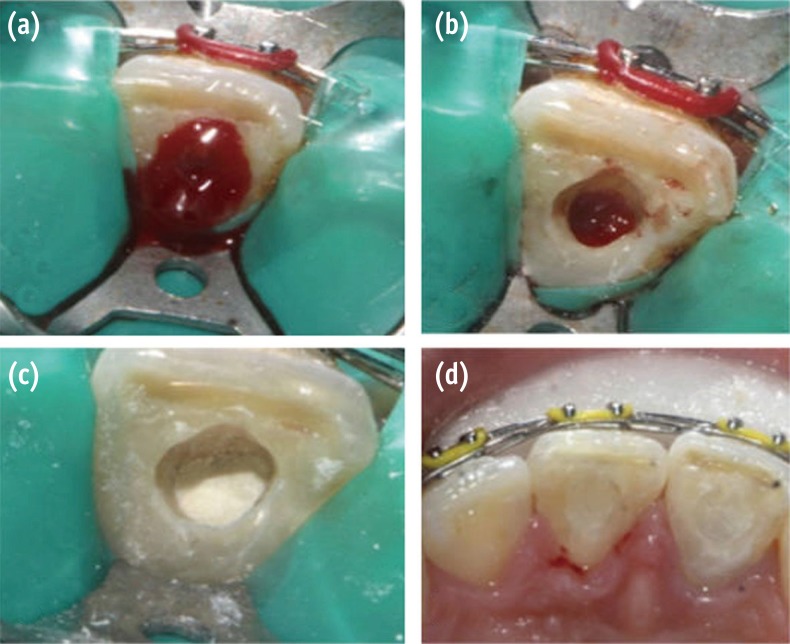
Second appointment. (a) Bleeding created by overinstrumentation; (b) Bleeding stopped 3 mm from CEJ; (c) Collagen membrane placed on top of the blood clot and placement of white MTA; (d) Access cavity restored with composite resin restoration. CEJ, cementoenamel junction; MTA, mineral trioxide aggregate.
Tables & Figures
REFERENCES
Citations
Citations to this article as recorded by 

- Revascularization of Non-Vital, Immature, Permanent Teeth with Two Bioceramic Cements: A Randomized Controlled Trial
Alaa Shaker, Mohamed Salem Rekab, Mohammad Alharissy, Naji Kharouf
Ceramics.2024; 7(1): 86. CrossRef - Orthodontically induced external apical root resorption considerations of root-filled teeth vs vital pulp teeth: a systematic review and meta-analysis
Danning Zhao, Kun Xue, Jiayuan Meng, Meijing Hu, Fei Bi, Xuelian Tan
BMC Oral Health.2023;[Epub] CrossRef - Regenerative Endodontic Therapy for Management of an Immature Permanent Tooth with Recurrent Post-treatment Apical Periodontitis
Renato Lenzi, Sandra R Hernández, Flávio R F Alves, Isabela N Ro[Combining Circumflex Accent]c[COMBINING CEDILLA]as, Jose[Combining Acute Accent] F Siqueira
Journal of International Society of Preventive and Community Dentistry.2022; 12(4): 468. CrossRef - Rejeneratif Endodontik Tedavi: Bir Literatür Derlemesi
Enes Mustafa AŞAR, Murat Selim BOTSALI
Selcuk Dental Journal.2022; 9(1): 335. CrossRef - Clinical and radiographic outcomes of regenerative endodontic treatment performed by endodontic postgraduate students: a retrospective study
Hadi Rajeh Alfahadi, Saad Al-Nazhan, Fawaz Hamad Alkazman, Nassr Al-Maflehi, Nada Al-Nazhan
Restorative Dentistry & Endodontics.2022;[Epub] CrossRef - Endodontic Regenerative Procedures in Necrotic Adult Teeth
Sara Garrido-Parada, Pablo Castelo-Baz, Nancy Feijoo-Pato, José Gaviño-Orduña, Benjamín Martín-Biedma
Applied Sciences.2022; 12(9): 4212. CrossRef - Different Approaches to the Regeneration of Dental Tissues in Regenerative Endodontics
Anna M. Krupińska, Katarzyna Skośkiewicz-Malinowska, Tomasz Staniowski
Applied Sciences.2021; 11(4): 1699. CrossRef - Histologic, Radiographic, and Micro-Computed Tomography Evaluation of Experimentally Enlarged Root Apices in Dog Teeth with Apical Periodontitis after Regenerative Treatment
Mohammed S. Alenazy, Saad Al-Nazhan, Hezekiah A Mosadomi
Current Therapeutic Research.2021; 94: 100620. CrossRef - Revitalizing previously treated teeth with open apices: A case report and a literature review
Ali Nosrat, Behnam Bolhari, Shima Saber Tahan, Omid Dianat, Paul Michael Howell Dummer
International Endodontic Journal.2021; 54(10): 1782. CrossRef - PRICE 2020 guidelines for reporting case reports in Endodontics: explanation and elaboration
V. Nagendrababu, B. S. Chong, P. McCabe, P. K. Shah, E. Priya, J. Jayaraman, S. J. Pulikkotil, P. M. H. Dummer
International Endodontic Journal.2020; 53(7): 922. CrossRef - Regenerative Endodontics: A Systematic Analysis of the Failed Cases
Waleed Almutairi, Ghaeth H. Yassen, Anita Aminoshariae, Kristin A. Williams, Andre Mickel
Journal of Endodontics.2019; 45(5): 567. CrossRef - Alternative to Avoid Tooth Discoloration after Regenerative Endodontic Procedure: A Systematic Review
Luciane Geanini Pena dos Santos, Luiz Alexandre Chisini, Camila Guerner Springmann, Beatriz Dulcineia Mendes de Souza, Fernanda Geraldo Pappen, Flávio Fernando Demarco, Mara Cristina Santos Felippe, Wilson Tadeu Felippe
Brazilian Dental Journal.2018; 29(5): 409. CrossRef
Retreatment of failed regenerative endodontic of orthodontically treated immature permanent maxillary central incisor: a case report
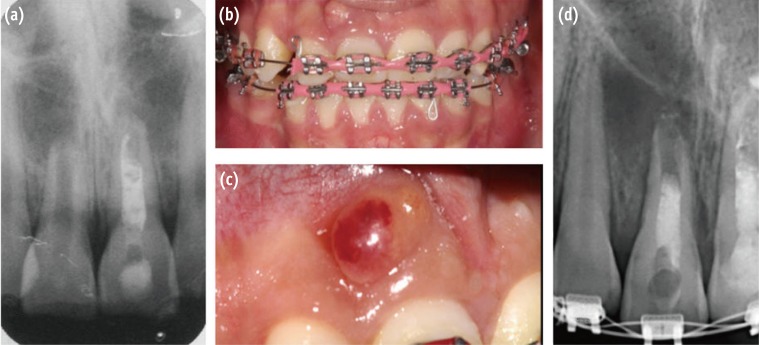
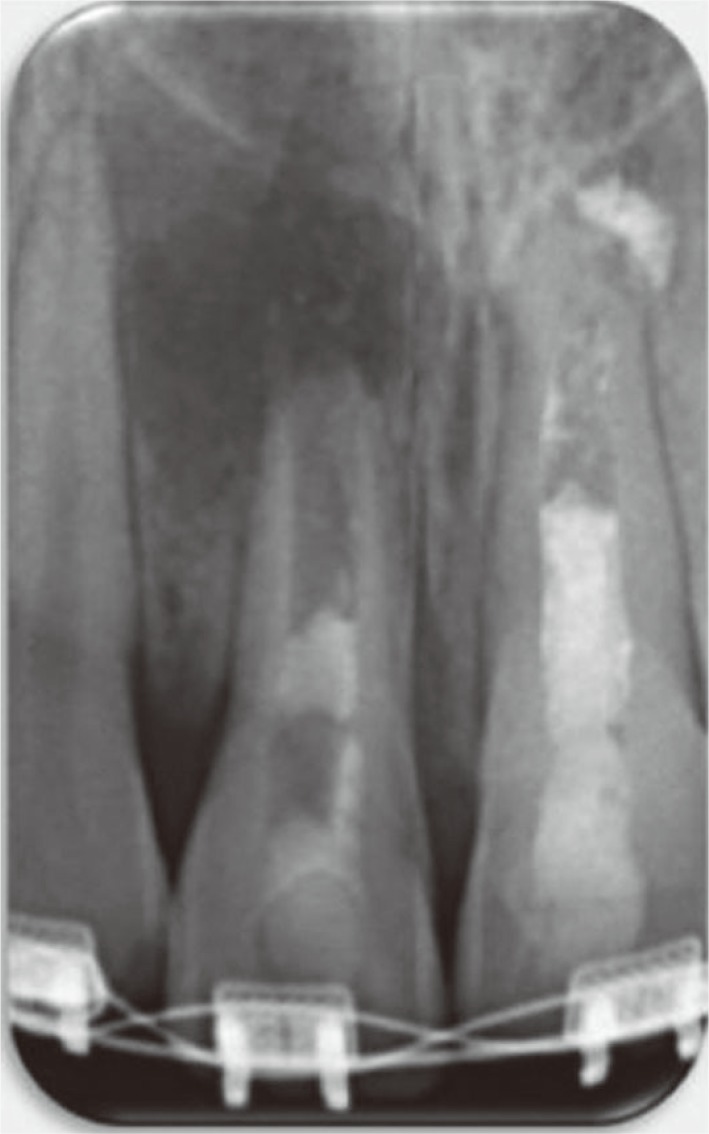
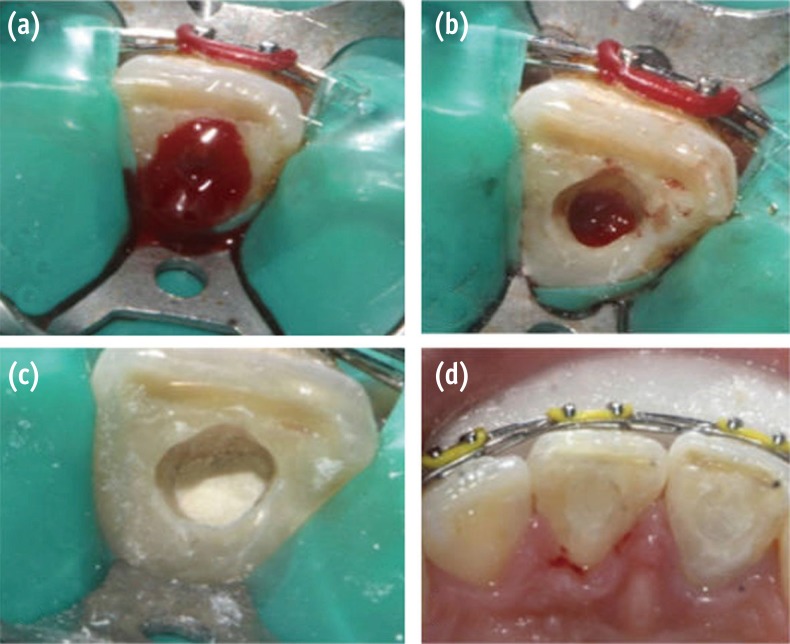
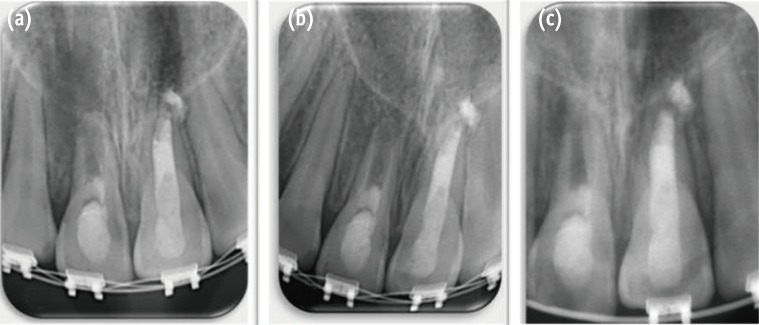
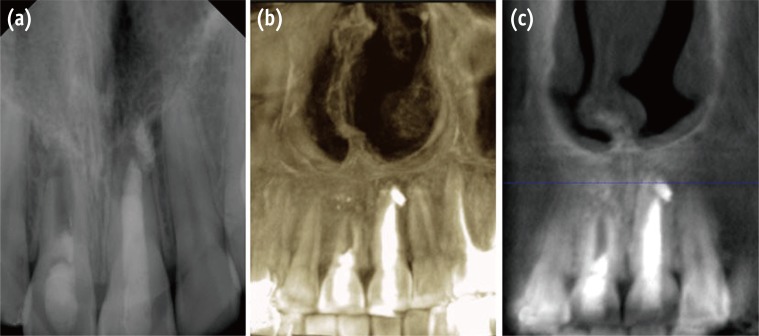
Figure 1 (a) Diagnostic radiograph of the maxillary right central incisor (tooth #11) demonstrated incomplete root formation with diffuse periapical radiolucency and poor root canal filling; (b and c) Preoperative clinical photograph illustrates orthodontic treatment and the sinus tract related to tooth #11; (d) Periapical radiograph during orthodontic examination and before regenerative endodontic treatment that shows an open apex with apical rarefaction.
Figure 2 Periapical radiograph after placement of double antibiotic paste (DAP).
Figure 3 Second appointment. (a) Bleeding created by overinstrumentation; (b) Bleeding stopped 3 mm from CEJ; (c) Collagen membrane placed on top of the blood clot and placement of white MTA; (d) Access cavity restored with composite resin restoration. CEJ, cementoenamel junction; MTA, mineral trioxide aggregate.
Figure 4 Follow-up radiographs of tooth #11 at (a) 3 months; (b) 6 months; (c) 12 months.
Figure 5 Three year follow-up confirming the healing process. (a) Conventional radiograph; (b) CBCT three-dimensional reconstruction; (c) CBCT buccal view. CBCT, cone beam computed tomography.
Figure 1
Figure 2
Figure 3
Figure 4
Figure 5
Retreatment of failed regenerative endodontic of orthodontically treated immature permanent maxillary central incisor: a case report

 KACD
KACD
 ePub Link
ePub Link Cite
Cite

