Search
- Page Path
- HOME > Search
- Proximity of maxillary molar apexes to the cortical bone surface and the maxillary sinus
- Han Shin Lee, Dokyung Kim, Sung Kyo Kim
- Restor Dent Endod 2022;47(3):e33. Published online August 8, 2022
- DOI: https://doi.org/10.5395/rde.2022.47.e33
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
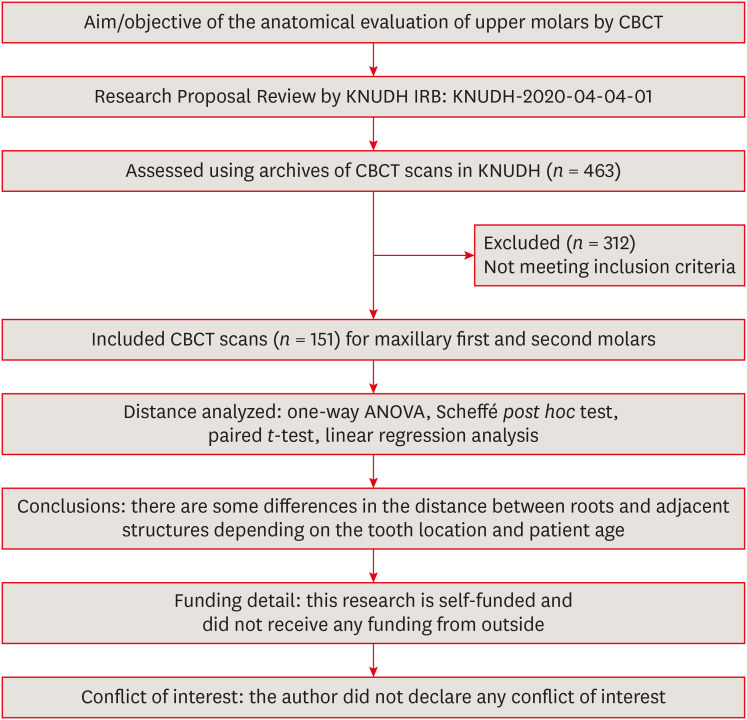
ePub Objectives This study aimed to analyze the proximity of maxillary molar roots to their overlying cortical bone surfaces and the maxillary sinus.
Materials and Methods Cone-beam computed tomographic images of 151 patients with completely erupted upper molars that had 3 separate roots were studied. The following distances were measured: from the root apex to the cortical plate and maxillary sinus floor, and from the apical 3-mm level of the root to the cortical plate. Differences between groups were analyzed with 1-way analysis of variance and the Scheffé
post hoc test, the significance of differences between cone-beam computed tomography views with the pairedt -test, and the significance of differences among age groups with linear regression analysis. The significance level was set atp < 0.05.Results The mesiobuccal and distobuccal root apexes of maxillary second molars were more distant from the buccal cortical plate than the maxillary first molars (
p < 0.05). The apical 3-mm level of the mesiobuccal root of the first molar was closer to the buccal cortical bone than the second molar (p < 0.05). In the maxillary first molars, the thickness of the buccal cortical bone decreased in all roots with age (p < 0.05). In all root apexes of both molars, the difference in the vertical level between the maxillary sinus floor and the root apex increased with age (p < 0.05).Conclusions Awareness of the anatomical profile of maxillary molar apices in relation to the cortical bones and maxillary sinus will be beneficial for apical surgery.
-
Citations
Citations to this article as recorded by- Proximity of maxillary molar palatal roots to adjacent structures for endodontic microsurgery: a cone-beam computed tomography study
Xiaoxiang Huang, Jun Xu, Benxiang Hou, Ying Wang
BMC Oral Health.2025;[Epub] CrossRef - Periapical bone loss configuration in sub-Saudi patients afflicted with periapical abscesses: A 3D cone-beam computed tomography analysis
Swati A. Srivastava, Rahaf A. Alawajy, Rehab Abdelaziz, Elzahraa A. Eldwakhly, Selma A. Saadaldin, Rahaf A. Almohareb, Fahda Nabeel Algahtani, Mai Salah Soliman, Manal M. Abdelhafeez
Saudi Endodontic Journal.2025; 15(2): 144. CrossRef
- Proximity of maxillary molar palatal roots to adjacent structures for endodontic microsurgery: a cone-beam computed tomography study
- 3,251 View
- 29 Download
- 1 Web of Science
- 2 Crossref

- Morphotypes of the apical constriction of maxillary molars: a micro-computed tomographic evaluation
- Jeffrey Wen-Wei Chang, Kuzhanchinathan Manigandan, Lakshman Samaranayake, Chellapandian NandhaKumar, Pazhamalai AdhityaVasun, Johny Diji, Angambakkam Rajasekharan PradeepKumar
- Restor Dent Endod 2022;47(2):e19. Published online March 24, 2022
- DOI: https://doi.org/10.5395/rde.2022.47.e19
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
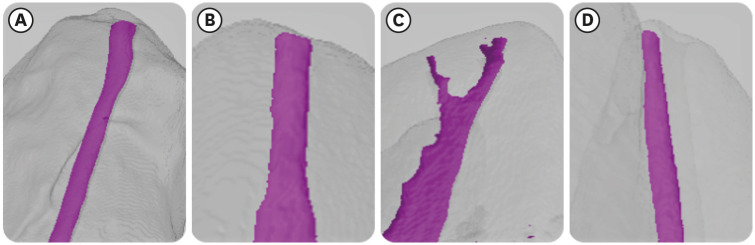
ePub Objectives The aim of this study was to evaluate and compare the apical constriction (AC) and apical canal morphology of maxillary first and second molars, using micro-computed tomography (micro-CT).
Materials and Methods The anatomical features of 313 root canals from 41 maxillary first molars and 57 maxillary second molars of patients with known age and sex were evaluated using micro-CT, with a resolution of 26.7 µm. The factors evaluated were the presence or absence of AC, the morphotypes, bucco-lingual dimension, mesio-distal dimension, and the profile (shape) of AC and the apical root canal. The apical root canal dimensions, location of the apical foramen (AF), AC to AF distance, and presence of accessory canals in the apical 5 mm were also assessed. Descriptive and analytical statistics were used for data evaluation.
Results AC was present in all 313 root canals. Patients’ age and sex did not significantly impact either AC or the apical canal dimensions. The most common AC morphotype detected was the traditional (single) constriction (52%), followed by the parallel (29%) morphotype. The mean AC dimensions in maxillary first molars were not significantly different from those in maxillary second molars. Sixty percent of AF were located within 0.5 mm from the anatomic apex.
Conclusions The most common morphotype of AC detected was the traditional constriction. Neither patients’ age nor sex had a significant impact on the dimensions of the AC or the apical root canal. The majority of AF (60%) were located within 0.5 mm from the anatomic apex.
-
Citations
Citations to this article as recorded by- In Vivo and In Vitro Accuracy and Precision Evaluations of Mini Electronic Apex Locators
Özlem Kara, Rüstem Kemal Sübay
Australian Endodontic Journal.2025; 51(2): 329. CrossRef - Effect of Coronal Flaring on Initial Apical File Size Estimation in Curved Canals Using Three Distinct Rotary Instruments: A Comparative In Vitro Study
Vinodhini Varatharajan, Muhammed Abdul Rahman Thazhathveedan, Mohammed Salman Kuttikkodan, Ismail Puzhangaraillath Mundanatayil, Amrutha Ravindran Thazhe Mangool, Ashraf Karumbil
Cureus.2024;[Epub] CrossRef - In Vitro Evaluation of the Accuracy of Three Electronic Apex Locators Using Different Sodium Hypochlorite Concentrations
Sanda Ileana Cîmpean, Radu Marcel Chisnoiu, Adela Loredana Colceriu Burtea, Rareș Rotaru, Marius Gheorghe Bud, Ada Gabriela Delean, Ioana-Sofia Pop-Ciutrilă
Medicina.2023; 59(5): 918. CrossRef - Cone beam computed tomography analysis of the root and canal morphology of the maxillary second molars in a Hail province of the Saudi population
Ahmed A. Madfa, Moazzy I. Almansour, Saad M. Al-Zubaidi, Albandari H. Alghurayes, Safanah D. AlDAkhayel, Fatemah I. Alzoori, Taif F. Alshammari, Abrar M. Aldakhil
Heliyon.2023; 9(9): e19477. CrossRef
- In Vivo and In Vitro Accuracy and Precision Evaluations of Mini Electronic Apex Locators
- 2,365 View
- 47 Download
- 6 Web of Science
- 4 Crossref

- Morphological characteristics of the mesiobuccal root in the presence of a second mesiobuccal canal: a micro-CT study
- Lucas P. Lopes Rosado, Matheus Lima Oliveira, Karla Rovaris, Deborah Queiroz Freitas, Frederico Sampaio Neves
- Restor Dent Endod 2022;47(1):e6. Published online January 18, 2022
- DOI: https://doi.org/10.5395/rde.2022.47.e6
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
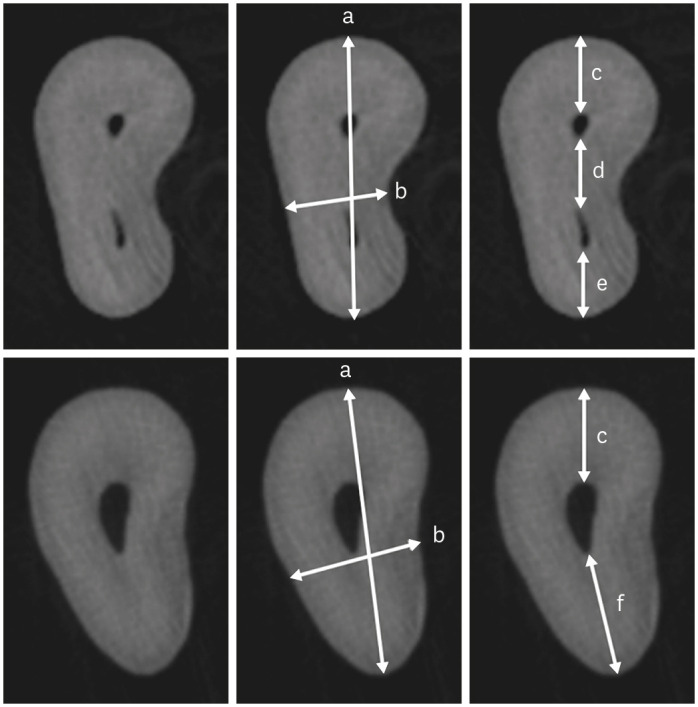
ePub Objectives This study investigated the internal morphology of mesiobuccal (MB) roots of maxillary molars with a second mesiobuccal (MB2) canal.
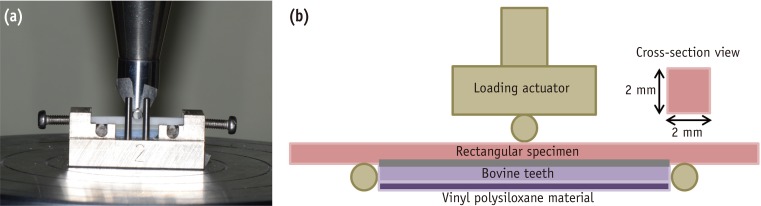
Materials and Methods Forty-seven maxillary first or second molars from Brazilians were scanned using micro-computed tomography. The following measurements were obtained from the MB roots: root thickness, root width, and dentin thickness of the buccal aspect of the first mesiobuccal (MB1) canal, between the MB1 and MB2 canals, and the palatal aspect of the MB2 and MB1 canals at 3 mm from the root apex and in the furcation region. For statistical analysis, the Student’s
t -test and analysis of variance with thepost-hoc Tukey test were used (α = 0.05).Results In maxillary molars with an MB2 canal, MB roots were significantly thicker (
p = 0.0014) and narrower (p = 0.0016) than in maxillary molars without an MB2 canal. The dentin thickness of the palatal aspect of the MB1 canal was also significantly greater than that of MB roots without an MB2 canal at 3 mm from the root apex (p = 0.0007) and in the furcation region (p < 0.0001). In the furcation region of maxillary molars with an MB2 canal, the dentin thickness between the MB1 and MB2 canals was significantly smaller than that in the buccal and palatal aspects (p < 0.0001).Conclusions The internal morphology of MB roots of maxillary molars with an MB2 canal revealed differences in dentin thickness, root diameter, and distance between the canals when compared with maxillary molars without an MB2 canal.
-
Citations
Citations to this article as recorded by- Effectiveness and safety of three NiTi systems in endodontic retreatment of MB1 and MB2 root canals: a micro-CT and CBCT combined analysis
Airton Oliveira Santos-Junior, Rocharles Cavalcante Fontenele, Karina Ines Medina Carita Tavares, Fernanda Ferrari Esteves Torres, Jáder Camilo Pinto, Pedro Luis Busto Rosim, Andréa Gonçalves, Marco Antonio Hungaro Duarte, Juliane Maria Guerreiro-Tanomaru
Clinical Oral Investigations.2025;[Epub] CrossRef - Cone-beam computed tomography evaluation of root and canal morphology of maxillary molars in a Chinese kazakh population
Shuchun Yang, Chenye Li, Hui Shi, Ming Liu, Xu Wang
BMC Oral Health.2025;[Epub] CrossRef - Can maxillary molar dimensions predict the presence of the second mesiobuccal canal?
Lucas P. Lopes Rosado, Deborah Queiroz Freitas, Karla Rovaris, Matheus L. Oliveira, Frederico Sampaio Neves
Oral Radiology.2023; 39(3): 482. CrossRef - Can the detection of second mesiobuccal canals be enhanced based on the volume of adjacent canals?
Lucas P. Lopes Rosado, Deborah Q. Freitas, Karla Rovaris, Matheus L. Oliveira, Frederico S. Neves
Archives of Oral Biology.2023; 146: 105604. CrossRef - Assessment of the coronal root canal morphology of permanent maxillary first molars using digital 3D-reconstruction technology based on micro-computed tomography data
Mudan Wang, Yuxuan Gao, Qi Deng, Yuan Gao, Dongzhe Song, Dingming Huang
Journal of Dental Sciences.2023; 18(2): 586. CrossRef
- Effectiveness and safety of three NiTi systems in endodontic retreatment of MB1 and MB2 root canals: a micro-CT and CBCT combined analysis
- 1,805 View
- 36 Download
- 6 Web of Science
- 5 Crossref

- A cone-beam computed tomography study of the prevalence and location of the second mesiobuccal root canal in maxillary molars
- Seong-Ju Lee, Eun-Hye Lee, Se-Hee Park, Kyung-Mo Cho, Jin-Woo Kim
- Restor Dent Endod 2020;45(4):e46. Published online September 3, 2020
- DOI: https://doi.org/10.5395/rde.2020.45.e46
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
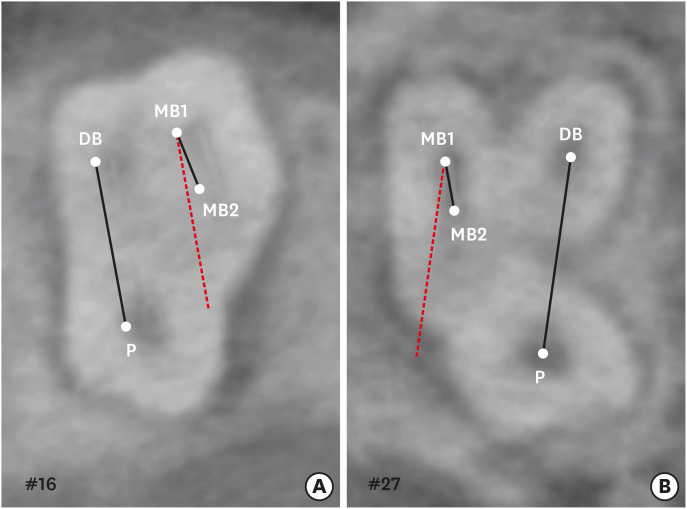
ePub Objectives This study aimed to investigate the incidence and location of the second mesiobuccal root (MB2) canal in maxillary molars with the aid of various measuring points and lines using cone-beam computed tomography (CT).
Materials and Methods A total of 205 images of patients who underwent cone-beam CT examinations between 2011 and 2015 as part of their dental diagnosis and treatment were included. There were 76 images of the maxillary first molar and 135 images of the maxillary second molar. Canal orifices were detected at −1 mm from the top of the pulpal floor on cone-beam CT images. Image assessment was performed by 2 observers in reformatted image planes using software. Assessments included measurement of the distance between the MB1 and MB2 canals, and the angles between the lines connecting the MB1-MB2 and distobuccal (DB)-palatal (P) canals. The data were analyzed using the student's
t -test.Results The prevalence of the MB2 canal was 86.8% in the first molar and 28.9% in the second molar. The angle between the lines connecting the MB1-MB2 and DB-P canals was 2.3° ± 5.7° in the first molar and −3.95° ± 7.73° in the second molar. The distance between the MB1 and MB2 canals was 2.1 ± 0.44 mm in the first molar and 1.98 ± 0.42 mm in the second molar.
Conclusions The angles between the lines connecting the MB1-MB2 and DB-P canals was almost parallel. These findings may aid in the prediction of the location of the MB2 canal orifice.
-
Citations
Citations to this article as recorded by- Position of Second Mesiobuccal Canal Relative to Distobuccal and Palatal Canals of Maxillary Molars in an Iranian Population
Sina Mosadeghian, Azadeh Torkzadeh, Parisa Ranjbarian, Roya Asaadi
Journal of Research in Dental and Maxillofacial Sciences.2025; 10(1): 34. CrossRef - Machine Learning Models in the Detection of MB2 Canal Orifice in CBCT Images
Shishir Shetty, Meliz Yuvali, Ilker Ozsahin, Saad Al-Bayatti, Sangeetha Narasimhan, Mohammed Alsaegh, Hiba Al-Daghestani, Raghavendra Shetty, Renita Castelino, Leena R David, Dilber Uzun Ozsahin
International Dental Journal.2025; 75(3): 1640. CrossRef - EVALUATION OF THE PREVALENCE AND LOCATION OF SECOND MESIOBUCCAL CANALS IN 2100 UPPER FIRST AND SECOND MOLAR TEETH: A CONE BEAM COMPUTED TOMOGRAPHY STUDY
Bahar Kaplan, Özkan Adıgüzel, Ayşe Gül Öner Talmaç, Elif Meltem Aslan
İnönü Üniversitesi Sağlık Hizmetleri Meslek Yüksek Okulu Dergisi.2025; 13(3): 752. CrossRef - A novel method for the precise second mesiobuccal canal orifice location: A combined strategy for enhanced clinical practice
Yuhan Wang, Lingyun Li, Lu Zhang, Xiaoyan Wang
Journal of Dental Sciences.2025;[Epub] CrossRef - Study on the Geometric Location Method of the Danger Zone in the Mesial Roots of Mandibular First Molars
Jinjie Yan, Yuanling Peng, Jing Yang, Jie Liu, Linxian Wang, Tingyuan Zhao, Jian Zhang, Kehua Que
Journal of Endodontics.2025;[Epub] CrossRef - The Correlation between Intraorifice Distance and the Anatomical Characteristics of the Second Mesiobuccal Canal of Maxillary Molars: A CBCT Study
Isabella Perondi, Silvio Taschieri, Martino Baruffaldi, Roberto Fornara, Luca Francetti, Stefano Corbella, Deepa Gurunathan
International Journal of Dentistry.2024;[Epub] CrossRef - Endodontic management of type I maxillary first molar with two palatal roots using cone-beam computed tomography
Nuha Alghamdi
Dental Journal.2024; 57(1): 1. CrossRef - 3D geometric analysis of second mesiobuccal canal in permanent maxillary first molar tooth
Indrani Khadilkar, Divya Nangia, Amrita Chawla, Sidhartha Sharma, Vijay Kumar, Shalini Gupta, Ajay Logani
Australian Endodontic Journal.2023; 49(1): 140. CrossRef - Prevalence of mesiobuccal-2 canals in maxillary first and second molars among the Bruneian population—CBCT analysis
Hui Yi Onn, Malissa Siao Yun Abdullah Sikun, Hanif Abdul Rahman, Jagjit Singh Dhaliwal
BDJ Open.2022;[Epub] CrossRef - Location angle of second mesio-buccal canal in maxillary molars of an Indian population: an in vivo retrospective CBCT evaluation and proposal of a new classification
Kishor Vhorkate, Kulvinder Banga, Ajinkya M. Pawar, Shugufta Mir, Suraj Arora, Dian Agustin Wahjuningrum, Anuj Bhardwaj, Alexander Maniangat Luke
PeerJ.2022; 10: e14234. CrossRef - Maxillary molar root and canal morphology of Neolithic and modern Chinese
H.Y. Ren, K.Y. Kum, Y.S. Zhao, Y.J. Yoo, J.S. Jeong, Hiran Perinpanayagam, X.Y. Wang, G.J. Li, F. Wang, H. Fang, Y. Gu
Archives of Oral Biology.2021; 131: 105272. CrossRef
- Position of Second Mesiobuccal Canal Relative to Distobuccal and Palatal Canals of Maxillary Molars in an Iranian Population
- 4,086 View
- 45 Download
- 11 Crossref

- Fused roots of maxillary molars: characterization and prevalence in a Latin American sub-population: a cone beam computed tomography study
- Maytté Marcano-Caldera, Jose Luis Mejia-Cardona, María del Pilar Blanco-Uribe, Elena Carolina Chaverra-Mesa, Didier Rodríguez-Lezama, Jose Hernán Parra-Sánchez
- Restor Dent Endod 2019;44(2):e16. Published online April 22, 2019
- DOI: https://doi.org/10.5395/rde.2019.44.e16
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives The upper molars generally have three roots; therefore, different combinations of fusion can occur, increasing the possibility of finding more complex root canal systems. The purpose of this study was to evaluate the prevalence and characterization of fused roots in first and second maxillary molars using cone-beam computed tomography (CBCT) in a Colombian population.
Materials and Methods A total of 1274 teeth were evaluated, of which 534 were maxillary first molars and 740 were maxillary second molars. Axial sections were made at the cervical, middle, and apical levels to determine the prevalence of root fusion and the types of fusion.
Results Overall, 43% of the molars (
n = 551) presented some type of fused root. Root fusion was present in 23.4% of the maxillary first molars. The most frequent type of fused root was type 3 (distobuccal-palatal; DB-P) (58.9%). Root fusion was observed in 57.6% of the maxillary second molars, and the most prevalent type of fused root was type 6 (cone-shaped) (45.2%). Of the maxillary molars, 12.5% were classified as C-shaped.Conclusion Within the limitations of this study, there was a high prevalence of fused roots in maxillary molars in the Colombian population, mainly in the maxillary second molars. In first molars, the most common type of fused root was type 3 (DB-P) and in second molars, the most common type was type 6 (cone-shaped). Additionally, molars with root fusion presented variation at different levels of the radicular portion, with implications for treatment quality.
-
Citations
Citations to this article as recorded by- Intentional Tooth Replantation: Current Evidence and Future Research Directions for Case Selection, Extraction Approaches, and Post-Operative Management
Rahul Minesh Shah, Thomas Manders, Georgios Romanos
Dentistry Journal.2026; 14(1): 59. CrossRef - Management of a rare bilateral maxillary first molar with six canals using a cone-beam computed tomography: Report of two cases
Aishwarya D. Jain, Nimisha Chinmay Shah, Abhya Jain, Shreya S. Volety
Saudi Endodontic Journal.2025; 15(2): 186. CrossRef - Assessment of root and root canal morphology in maxillary molars with fused roots using Cone Beam Computer Tomography (CBCT) in a Sri Lankan population
Ruvienath Daham Weerasinghe Rajapaksa, Manil Christopher Nishan Fonseka, Ruwan Duminda Jayasinghe, Rasika Manori Jayasinghe
Journal of Oral Biology and Craniofacial Research.2025; 15(6): 1297. CrossRef - Cone-beam computed tomography evaluation of root and canal morphology of maxillary molars in a Chinese kazakh population
Shuchun Yang, Chenye Li, Hui Shi, Ming Liu, Xu Wang
BMC Oral Health.2025;[Epub] CrossRef - A Twisted Tale of Dilacerated Fused Roots Mimicking Radicular Dens Invaginatus
Rashmi D Sathe, Preeti P. Nair, Richa Bajpai, Bidushi Mishra
Journal of the International Clinical Dental Research Organization.2025; 17(2): 214. CrossRef - Exploring the sex-associated differences in molars fused roots
Maria Eduarda Nunis Locks, Erika Calvano Küchler, Leonardo Santos Antunes, Alice Corrêa Silva-Sousa, Natanael Henrique Ribeiro Mattos, Camila Paiva Perin, Paulo Henrique Condeixa França, Peter Proff, Christian Kirschneck, Flares Baratto-Filho
Annals of Anatomy - Anatomischer Anzeiger.2024; 254: 152245. CrossRef - Cone beam computed tomography analysis of the root and canal morphology of the maxillary second molars in a Syrian subpopulation
Safaa Allawi, Mouhammad Al-Tayyan, Hassan Achour, Eyad Al-Toutangy, Yasser Alsayed Tolibah
BMC Oral Health.2024;[Epub] CrossRef - Prevalence of root fusion in canine maxillary second molar teeth using cone-beam computed tomography
Kristin Linder, Scott MacGee, Loren Schultz
Frontiers in Veterinary Science.2023;[Epub] CrossRef - Dentine thickness in maxillary fused molars depends on the fusion type: An ex vivo micro‐computed tomography study
Cangül Keskin, Defne Toplu, Ali Keleş
International Endodontic Journal.2023; 56(5): 637. CrossRef - Root and canal-specific features of maxillary first molars with fused roots
Katarina Beljic-Ivanovic, Branislav Karadzic
Vojnosanitetski pregled.2022; 79(11): 1092. CrossRef - Micro-CT Analysis of the Root Canal Configuration of Maxillary Second Molars with Fusion
Cangül KESKİN, Özgür ÖZDEMİR, Ali KELEŞ
European Annals of Dental Sciences.2022; 49(Suppl 1): 25. CrossRef - Assessment of C-Shaped Canal Morphology in Mandibular and Maxillary Second Molars in an Iraqi Subpopulation Using Cone-Beam Computed Tomography
Kazhan Abdalrahman, Ranjdar Talabani, Sara Kazzaz, Dlsoz Babarasul, Berndt Koslowski
Scanning.2022; 2022: 1. CrossRef - Analysis of Root and Canal Morphology of Fused and Separate Rooted Maxillary Molar Teeth in Turkish Population
H Aydin
Nigerian Journal of Clinical Practice.2021; 24(3): 435. CrossRef - Investigating prevalence of dental anomalies in Eastern Province of Saudi Arabia through digital orthopantomogram
Jehan ALHumaid, Maryam Buholayka, Arishiya Thapasum, Muhanad Alhareky, Maha Abdelsalam, Amr Bughsan
Saudi Journal of Biological Sciences.2021; 28(5): 2900. CrossRef - Preferred Reporting Items for Epidemiologic Cross-sectional Studies on Root and Root Canal Anatomy Using Cone-beam Computed Tomographic Technology: A Systematized Assessment
Jorge N.R. Martins, Anil Kishen, Duarte Marques, Emmanuel João Nogueira Leal Silva, João Caramês, António Mata, Marco A. Versiani
Journal of Endodontics.2020; 46(7): 915. CrossRef - Second mesiobuccal root canal in maxillary molars—A systematic review and meta-analysis of prevalence studies using cone beam computed tomography
Jorge N.R. Martins, Duarte Marques, Emmanuel João Nogueira Leal Silva, João Caramês, António Mata, Marco A. Versiani
Archives of Oral Biology.2020; 113: 104589. CrossRef
- Intentional Tooth Replantation: Current Evidence and Future Research Directions for Case Selection, Extraction Approaches, and Post-Operative Management
- 1,954 View
- 14 Download
- 16 Crossref

- Maxillary first molar with 7 root canals diagnosed using cone-beam computed tomography
- Evaldo Rodrigues, Antônio Henrique Braitt, Bruno Ferraz Galvão, Emmanuel João Nogueira Leal da Silva
- Restor Dent Endod 2017;42(1):60-64. Published online August 29, 2016
- DOI: https://doi.org/10.5395/rde.2017.42.1.60
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
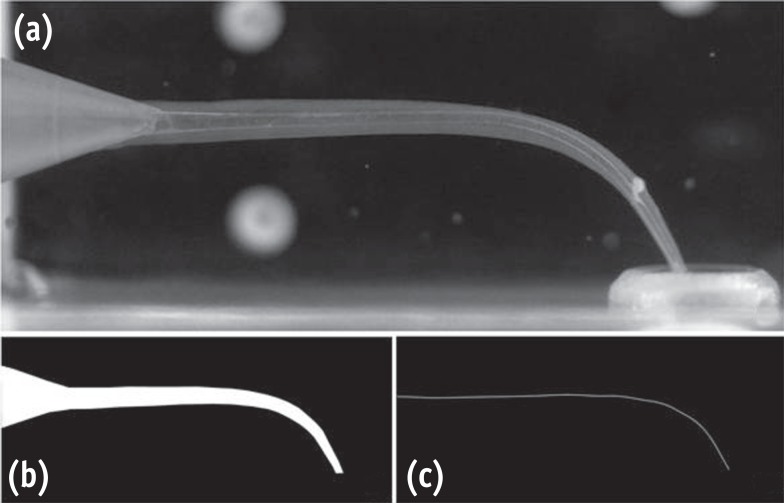
ePub Root canal anatomy is complex, and the recognition of anatomic variations could be a challenge for clinicians. This case report describes the importance of cone beam computed tomographyic (CBCT) imaging during endodontic treatment. A 23 year old woman was referred by her general dental practitioner with the chief complaint of spontaneous pain in her right posterior maxilla. From the clinical and radiographic findings, a diagnosis of symptomatic irreversible pulpitis was made and endodontic treatment was suggested to the patient. The patient underwent CBCT examination, and CBCT scan slices revealed seven canals: three mesiobuccal (MB1, MB2, and MB3), two distobuccal (DB1 and DB2), and two palatal (P1 and P2). Canals were successfully treated with reciprocating files and filled using single-cone filling technique. Precise knowledge of root canal morphology and its variation is important during root canal treatment. CBCT examination is an excellent tool for identifying and managing these complex root canal systems.
-
Citations
Citations to this article as recorded by- KONİK IŞINLI BİLGİSAYARLI TOMOGRAFİ İLE DOĞRULANMIŞ OLAĞANDIŞI ÜST BİRİNCİ BÜYÜK AZI DİŞİN ENDODONTİK TEDAVİSİ
Didem Seda Gültekin, Funda Kont Çobankara
Journal of International Dental Sciences.2025; 11(1): 46. CrossRef - Clinical Significance of Mesiobuccal and Distobuccal Canal Variations in Maxillary Molars: A Case Series and a Mini Review
Mohsen Aminsobhani, Somayeh Majidi, Vlaho Brailo
Case Reports in Dentistry.2025;[Epub] CrossRef - An Unusual Case of Maxillary First Molar: A Case Report
Reetu Shrestha
International Journal of Innovative Science and Research Technology (IJISRT).2024; : 1330. CrossRef - Root canal therapy of maxillary first molar with seven canals diagnosed using cone beam computed tomography – a case report
Saini Rashmi, Saini V. Kumar
Tanta Dental Journal.2022; 19(3): 169. CrossRef - Four-Rooted Maxillary First Molars: A Systematic Review and Meta-Analysis
Gabriel Magnucki, Sven V. K. Mietling, Sreekanth Kumar Mallineni
International Journal of Dentistry.2021; 2021: 1. CrossRef - Endodontic treatment of various palatal roots in maxillary molars
Chengshi Wei, Keyi Li, Lili Shen, Guangliang Bai, Xiufen Tian
The Journal of the American Dental Association.2021; 152(12): 1044. CrossRef - Diversity of root canal morphology of maxillary first molars
Juhász Kincső-Réka, Kovács Mónika, Pop Mihai, Pop Silvia, Kerekes-Máthé Bernadette
Bulletin of Medical Sciences.2021; 94(1): 63. CrossRef - Endodontic Management of Maxillary First Molar with Seven Root Canals Diagnosed Using Cone-beam Computed Tomography: A Case Report
Ravindranath Megha, Venkatachalam Prakash
World Journal of Dentistry.2021; 12(1): 89. CrossRef - Endodontic management of the maxillary first molar with special root canals: A case report and review of the literature
Zhi-Hui Zhang, Hai-Lin Yao, Yan Zhang, Xiao Wang
World Journal of Clinical Cases.2020; 8(12): 2590. CrossRef - Management of a permanent maxillary first molar with unusual crown and root anatomy: a case report
Prateeksha Chowdhry, Pallavi Reddy, Mamta Kaushik
Restorative Dentistry & Endodontics.2018;[Epub] CrossRef - Usefulness of cone beam computed tomography in perplexing endodontic cases
Amandeep Kaur, Ajay Logani
Endodontology.2018; 30(2): 187. CrossRef - Endodontic management of a maxillary first molar with seven root canal systems evaluated using cone-beam computed tomography scanning
VijayReddy Venumuddala, Sridhar Moturi, SV Satish, BKalyan Chakravarthy, Sudhakar Malapati
Journal of International Society of Preventive and Community Dentistry.2017; 7(5): 297. CrossRef
- KONİK IŞINLI BİLGİSAYARLI TOMOGRAFİ İLE DOĞRULANMIŞ OLAĞANDIŞI ÜST BİRİNCİ BÜYÜK AZI DİŞİN ENDODONTİK TEDAVİSİ
- 2,432 View
- 15 Download
- 12 Crossref

- Analysis of C-shaped root canal configuration in maxillary molars in a Korean population using cone-beam computed tomography
- Hyoung-Hoon Jo, Jeong-Bum Min, Ho-Keel Hwang
- Restor Dent Endod 2016;41(1):55-62. Published online January 29, 2016
- DOI: https://doi.org/10.5395/rde.2016.41.1.55
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
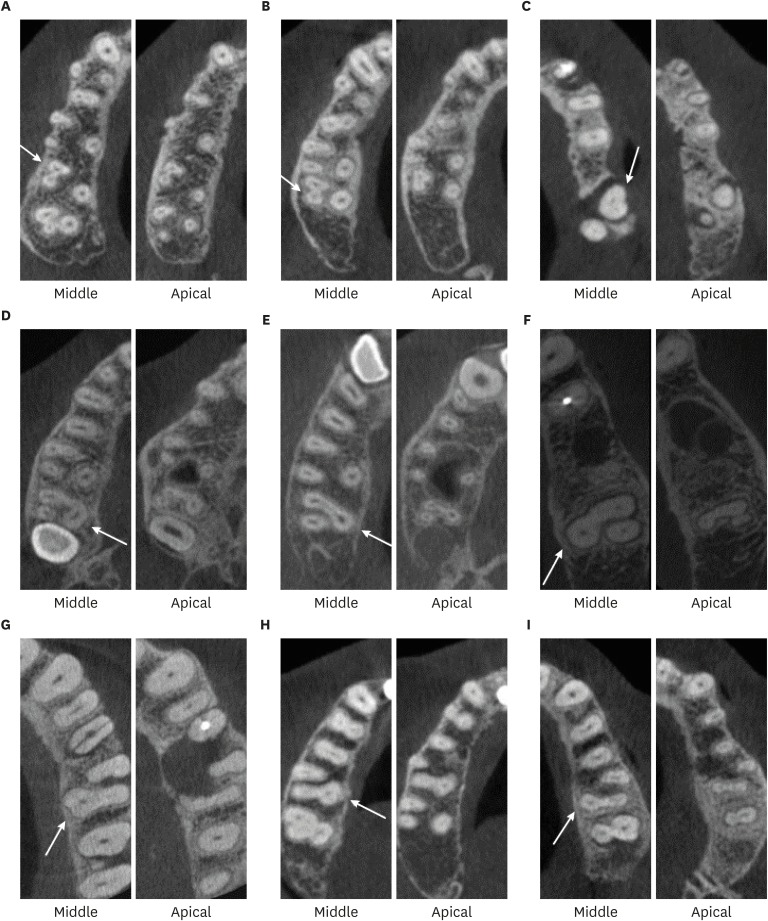
ePub Objectives The purpose of this study was to investigate the incidence of root fusion and C-shaped root canals in maxillary molars, and to classify the types of C-shaped canal by analyzing cone-beam computed tomography (CBCT) in a Korean population.
Materials and Methods Digitized CBCT images from 911 subjects were obtained in Chosun University Dental Hospital between February 2010 and July 2012 for orthodontic treatment. Among them, a total of selected 3,553 data of maxillary molars were analyzed retrospectively. Tomography sections in the axial, coronal, and sagittal planes were displayed by PiViewstar and Rapidia MPR software (Infinitt Co.). The incidence and types of root fusion and C-shaped root canals were evaluated and the incidence between the first and the second molar was compared using Chi-square test.
Results Root fusion was present in 3.2% of the first molars and 19.5% of the second molars, and fusion of mesiobuccal and palatal root was dominant. C-shaped root canals were present in 0.8% of the first molars and 2.7% of the second molars. The frequency of root fusion and C-shaped canal was significantly higher in the second molar than the first molar (
p < 0.001).Conclusions In a Korean population, maxillary molars showed total 11.3% of root fusion and 1.8% of C-shaped root canals. Furthermore, root fusion and C-shaped root canals were seen more frequently in the maxillary second molars.
-
Citations
Citations to this article as recorded by- Prevalence of C‐Shaped Canals in Maxillary Molars in an Iranian Population: A Cone‐Beam Computed Tomography Analysis
Amin Salem Milani, Shahin Namvar Asl Amirkhizi, Tahmineh Razi, Ahmad Nouroloyouni, Pouya Sabanik, Nikhat Kaura
International Journal of Clinical Practice.2026;[Epub] CrossRef - Prevalence of c-shaped canal morphology in premolar and molar teeth assessed by cone-beam computed tomography: systematic review and meta-analysis
Faezeh Yousefi, Younes Mohammadi, Elham Shokri
BMC Oral Health.2025;[Epub] CrossRef - A Cone‐Beam Computed Tomography Evaluation of C‐Shaped Canal Configuration in Maxillary Molars Among an Iranian Population
Nafiseh Nikkerdar, Mohammad Moslehi, Amin Golshah, Mario Dioguardi
International Journal of Dentistry.2024;[Epub] CrossRef - Endodontic treatment of a C‐shaped mandibular second molar with narrow dentinal thickness: A case report
Mina Mehrjouei, Hamid Jafarzadeh, Pourya Esmaeelpour, Maryam Khorasanchi
Clinical Case Reports.2024;[Epub] CrossRef - Evaluation of 2- and 3-dimensional anatomic parameters of C-shaped root canals with cone beam computed tomography, microcomputed tomography, and nanocomputed tomography
Miguel Angel Ventura Molina, Giovane Oliveira Silva, Amanda Pelegrin Candemil, Rafael Verardino de Camargo, Ruben Pauwels, Reinhilde Jacobs, Manoel Damião Sousa-Neto, Jardel Francisco Mazzi-Chaves
Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology.2023; 136(6): 759. CrossRef - Cone-Beam Computed Tomography (CBCT) Analysis of an Unusual Configuration of the Upper First Molar With a C-shaped Canal With Apically Fused Roots: A Case Report
Kapil D Wahane, Anand V Bansod, Sudha mattigatti, Rushikesh Mahaparale, Yuvraj B Rote, Mayur B Wanjari
Cureus.2023;[Epub] CrossRef - Assessment of C-Shaped Canal Morphology in Mandibular and Maxillary Second Molars in an Iraqi Subpopulation Using Cone-Beam Computed Tomography
Kazhan Abdalrahman, Ranjdar Talabani, Sara Kazzaz, Dlsoz Babarasul, Berndt Koslowski
Scanning.2022; 2022: 1. CrossRef - Root and canal-specific features of maxillary first molars with fused roots
Katarina Beljic-Ivanovic, Branislav Karadzic
Vojnosanitetski pregled.2022; 79(11): 1092. CrossRef - Diagnosis and treatment of maxillary molar with abnormality
Kkot-Byeol Bae, Bin-Na Lee, Hoon-Sang Chang, In-Nam Hwang, Won-Mann Oh, Yun-Chan Hwang
Oral Biology Research.2022; 46(4): 195. CrossRef - Endodontic treatment of the maxillary first molar with palatal canal variations: A case report and review of literature
Kai Chen, Xing Ran, Yan Wang
World Journal of Clinical Cases.2022; 10(32): 12036. CrossRef - Evaluation of C-shaped canals in maxillary molars in a Chinese population using CBCT
Yuyan Qian, Yamei Li, Jukun Song, Ping Zhang, Zhu Chen
BMC Medical Imaging.2022;[Epub] CrossRef - Comprehensive evaluation of root and root canal morphology of mandibular second molars in a Saudi subpopulation evaluated by cone-beam computed tomography
Moazzy I. Almansour, Saad M. Al‑Zubaidi, Abdulmjeed S. Enizy, Ahmed A. Madfa
BMC Oral Health.2022;[Epub] CrossRef - Evaluation of C-shaped canal configuration in maxillary molars: A retrospective cone-beam computed tomography study
Emre KÖSE, Rüya AK
Clinical and Experimental Health Sciences.2021; 11(3): 444. CrossRef - Maxillary First Molars with Two Palatal Root Canals
Kun-Hwa Sung, Ho-Keel Hwang, Hyoung-Hoon Jo, Konstantinos Michalakis
Case Reports in Dentistry.2021;[Epub] CrossRef - Preferred Reporting Items for Epidemiologic Cross-sectional Studies on Root and Root Canal Anatomy Using Cone-beam Computed Tomographic Technology: A Systematized Assessment
Jorge N.R. Martins, Anil Kishen, Duarte Marques, Emmanuel João Nogueira Leal Silva, João Caramês, António Mata, Marco A. Versiani
Journal of Endodontics.2020; 46(7): 915. CrossRef - Evaluation of root and root canal morphology of elderly Korean patients maxillary molars using cone-beam computed tomography
Tae-Yong Lee, Mi-Yeon Kim, Sun-Ho Kim, Jeong-Hee Kim
The Journal of Korean Academy of Prosthodontics.2020; 58(2): 95. CrossRef - Second mesiobuccal root canal in maxillary molars—A systematic review and meta-analysis of prevalence studies using cone beam computed tomography
Jorge N.R. Martins, Duarte Marques, Emmanuel João Nogueira Leal Silva, João Caramês, António Mata, Marco A. Versiani
Archives of Oral Biology.2020; 113: 104589. CrossRef - Prevalência estimada de canais “C- Shaped”: Uma revisão sistemática e meta-análise
Natália Pereira da Silva Falcão, Sandro Junio de Oliveira Tavares, Ludmila Silva Guimarães, Katherine Azevedo Batistela Rodrigues Thuller, Leonardo dos Santos Antunes, Estefano Borgo Sarmento, Fellipe Navarro Azevedo de Azevedo, Cinthya Cristina Gomes, Ca
Revista Científica Multidisciplinar Núcleo do Conhecimento.2020; : 91. CrossRef - Evaluation of the internal anatomy of paramolar tubercles using cone-beam computed tomography
G. Colakoglu, I. Kaya Buyukbayram, M. A. Elcin, M. Kazak, H. Sezer
Surgical and Radiologic Anatomy.2020; 42(1): 15. CrossRef - Analysis of Prevalence of Pyramidal Molars in Adolescent
Woojin Kwon, Hyung-Jun Choi, Jaeho Lee, Je Seon Song
THE JOURNAL OF THE KOREAN ACADEMY OF PEDTATRIC DENTISTRY.2020; 47(4): 389. CrossRef - Prevalence Studies on Root Canal Anatomy Using Cone-beam Computed Tomographic Imaging: A Systematic Review
Jorge N.R. Martins, Duarte Marques, Emmanuel João Nogueira Leal Silva, João Caramês, Marco A. Versiani
Journal of Endodontics.2019; 45(4): 372. CrossRef - Fused roots of maxillary molars: characterization and prevalence in a Latin American sub-population: a cone beam computed tomography study
Maytté Marcano-Caldera, Jose Luis Mejia-Cardona, María del Pilar Blanco-Uribe, Elena Carolina Chaverra-Mesa, Didier Rodríguez-Lezama, Jose Hernán Parra-Sánchez
Restorative Dentistry & Endodontics.2019;[Epub] CrossRef - An original micro‐CT study and meta‐analysis of the internal and external anatomy of maxillary molars—implications for endodontic treatment
Iwona M. Tomaszewska, Anna Jarzębska, Bendik Skinningsrud, Przemysław A. Pękala, Sebastian Wroński, Joe Iwanaga
Clinical Anatomy.2018; 31(6): 838. CrossRef - A Cone-beam Computed Tomographic Study of Root and Canal Morphology of Maxillary First and Second Permanent Molars in a Thai Population
Roserin Ratanajirasut, Anchana Panichuttra, Soontra Panmekiate
Journal of Endodontics.2018; 44(1): 56. CrossRef - Retrospective Assessment of Healing Outcome of Endodontic Treatment for Mandibular Molars with C-shaped Root Canal
Kishore Kumar Majety, Basanta Kumar Choudhury, Anika Bansal, Achla Sethi, Jaina Panjabi
The Journal of Contemporary Dental Practice.2017; 18(7): 591. CrossRef - The morphology of maxillary first and second molars analyzed by cone-beam computed tomography in a polish population
Katarzyna Olczak, Halina Pawlicka
BMC Medical Imaging.2017;[Epub] CrossRef
- Prevalence of C‐Shaped Canals in Maxillary Molars in an Iranian Population: A Cone‐Beam Computed Tomography Analysis
- 1,916 View
- 14 Download
- 26 Crossref


 KACD
KACD

 First
First Prev
Prev


