-
CBCT study of mandibular first molars with a distolingual root in Koreans
-
Hee-Ho Kim, Hyoung-Hoon Jo, Jeong-Bum Min, Ho-Keel Hwang
-
Restor Dent Endod 2018;43(3):e33. Published online July 30, 2018
-
DOI: https://doi.org/10.5395/rde.2018.43.e33
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Objectives
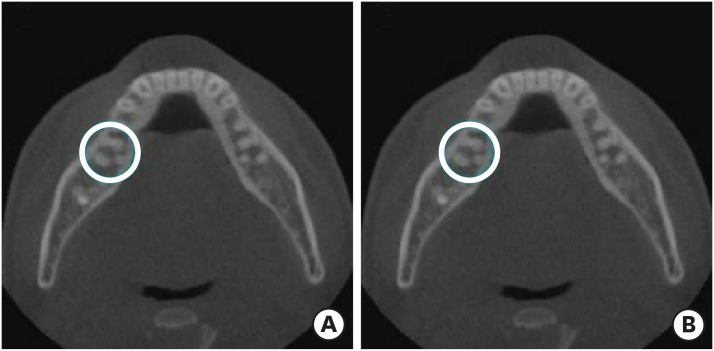
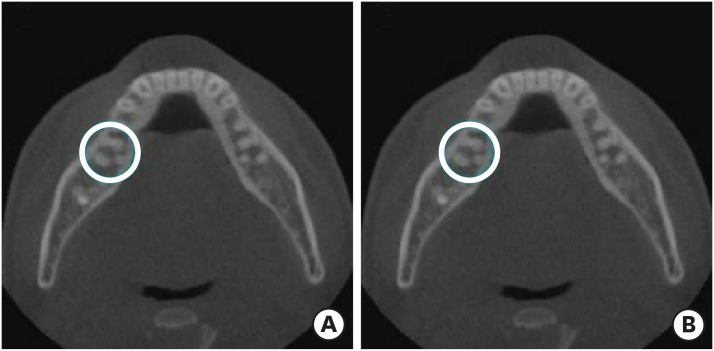
This study aimed to investigate the prevalence of a separate distolingual root and to measure the thickness of the buccal cortical bone in mandibular first molars in Koreans using cone-beam computed tomography (CBCT) images. Materials and MethodsHigh-quality CBCT data from 432 patients were analyzed in this study. The prevalence of a separate distolingual root of the mandibular first molar was investigated. The distance from the distobuccal and distolingual root apices to the outer surface of the buccal cortical bone was measured. We also evaluated the thickness of the buccal cortical bone. ResultsThe prevalence of a separate distolingual root (2 separate distal roots with 1 canal in each root; 2R2C) was 23.26%. In mandibular first molars with 2R2C, the distance from the distobuccal root apex to the outer surface of the buccal cortical bone was 5.51 mm. Furthermore, the distance from the distolingual root apex to the outer surface of the buccal cortical bone was 12.09 mm. In mandibular first molars with 2R2C morphology, the thickness of the buccal cortical bone at the distobuccal root apex of the mandibular first molar was 3.30 mm. The buccal cortical bone at the distobuccal root apex was significantly thicker in the right side (3.38 mm) than the left side (3.09 mm) (p < 0.05). ConclusionsA separate distolingual root is not rare in mandibular first molars in the Korean population. Anatomic and morphologic knowledge of the mandibular first molar can be useful in treatment planning, including surgical endodontic treatment.
-
Citations
Citations to this article as recorded by  - The association between complex root canal morphology of mandibular anteriors and distolingual roots in mandibular first molars in a Turkish population
Özge Kurt, Elif Solakoğlu
BMC Oral Health.2025;[Epub] CrossRef - Radix molaris is a hidden truth of mandibular first permanent molars: A descriptive- analytic study using cone beam computed tomography
Mohammed A. Alobaid, Saurabh Chaturvedi, Ebtihal Mobarak S. Alshahrani, Ebtsam M. Alshehri, Amal S. Shaiban, Mohamed Khaled Addas, Giuseppe Minervini
Technology and Health Care.2023; 31(5): 1957. CrossRef - Prevalence of radix entomolaris in India and its comparison with the rest of the world
Sumit MOHAN, Jyoti THAKUR
Minerva Dental and Oral Science.2022;[Epub] CrossRef - A critical analysis of laboratory and clinical research methods to study root and canal anatomy
Hany Mohamed Aly Ahmed
International Endodontic Journal.2022; 55(S2): 229. CrossRef - Three‐Rooted Permanent Mandibular First Molars: A Meta‐Analysis of Prevalence
Nyan M. Aung, Kyaw K. Myint, Luca Testarelli
International Journal of Dentistry.2022;[Epub] CrossRef - Reproducibilidad en el diagnóstico imagenológico de periodontitis apical a partir de CBCT
Sandra Milena Buitrago Rojas, Yeny Zulay Castellanos Dominguez, Jhonny Alexander Contreras Vargas, Yosdi Tomás Solano Diaz, Eder Fabián Gutierrez Argote
Acta Odontológica Colombiana.2020;[Epub] CrossRef - Assessment of Root and Root Canal Morphology of Human Primary Molars using CBCT
Yoomin Choi, Seonmi Kim, Namki Choi
THE JOURNAL OF THE KOREAN ACADEMY OF PEDTATRIC DENTISTRY.2020; 47(1): 25. CrossRef - The prevalence of radix molaris in the mandibular first molars of a Saudi subpopulation based on cone-beam computed tomography
Hassan AL-Alawi, Saad Al-Nazhan, Nassr Al-Maflehi, Mazen A. Aldosimani, Mohammed Nabil Zahid, Ghadeer N. Shihabi
Restorative Dentistry & Endodontics.2020;[Epub] CrossRef - Preferred Reporting Items for Epidemiologic Cross-sectional Studies on Root and Root Canal Anatomy Using Cone-beam Computed Tomographic Technology: A Systematized Assessment
Jorge N.R. Martins, Anil Kishen, Duarte Marques, Emmanuel João Nogueira Leal Silva, João Caramês, António Mata, Marco A. Versiani
Journal of Endodontics.2020; 46(7): 915. CrossRef - Evaluation of roots and canal systems of mandibular first molars in a vietnamese subpopulation using cone-beam computed tomography
KhoaVan Pham, AnhHoang Lan Le
Journal of International Society of Preventive and Community Dentistry.2019; 9(4): 356. CrossRef
-
1,686
View
-
10
Download
-
10
Crossref
-
Application of quantitative light-induced fluorescence to determine the depth of demineralization of dental fluorosis in enamel microabrasion: a case report
-
Tae-Young Park, Han-Sol Choi, Hee-Won Ku, Hyun-Su Kim, Yoo-Jin Lee, Jeong-Bum Min
-
Restor Dent Endod 2016;41(3):225-230. Published online June 20, 2016
-
DOI: https://doi.org/10.5395/rde.2016.41.3.225
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
Enamel microabrasion has become accepted as a conservative, nonrestorative method of removing intrinsic and superficial dysmineralization defects from dental fluorosis, restoring esthetics with minimal loss of enamel. However, it can be difficult to determine if restoration is necessary in dental fluorosis, because the lesion depth is often not easily recognized. This case report presents a method for analysis of enamel hypoplasia that uses quantitative light-induced fluorescence (QLF) followed by a combination of enamel microabrasion with carbamide peroxide home bleaching. We describe the utility of QLF when selecting a conservative treatment plan and confirming treatment efficacy. In this case, the treatment plan was based on QLF analysis, and the selected combination treatment of microabrasion and bleaching had good results. -
Citations
Citations to this article as recorded by  - Resin Infiltration for Dental Fluorosis: A Systematic Review and Meta‐Analysis of Randomized Controlled Trials on Esthetic Masking Efficacy
Hui Han, Tian Lan, Fenglan Li, Huishan Sun
Journal of Esthetic and Restorative Dentistry.2025; 37(12): 2579. CrossRef - Management of Multifactorial Stained Enamel Defects on Anterior Dentition Using a Combination Treatment of Whitening, Microabrasion, Resin Infiltration and Resin-based Composite Restoration
A Alkhazaleh, A Tsujimoto
Operative Dentistry.2023; 48(3): 251. CrossRef - Resin Infiltration and Remineralization Interventions in Management of Moderate Dental Fluorosis
Shreepriya Singhania, B. Nandlal, Raghavendra Shanbhog, Ragavee Veeramani
Indian Journal of Dental Research.2021; 32(3): 362. CrossRef - Resolution of a fluorosis case through the association of minimally invasive techniques
Danielle Ferreira Sobral de Souza, Josué Junior Araújo Pierote, Flávio Henrique Baggio Aguiar, Luís Alexandre Maffei Sartini Paulillo, Débora Alves Nunes Leite Lima
Brazilian Journal of Oral Sciences.2019; 18: e191663. CrossRef - La micro-abrasion amélaire associée à l’éclaircissement externe: intérêt dans la prise en charge de la fluorose
Laïla Azzahim, Sanaa Chala, Faïza Abdallaoui
Pan African Medical Journal.2019;[Epub] CrossRef - Methodological considerations for designing a community water fluoridation cessation study
Sonica Singhal, Julie Farmer, Lindsay McLaren
Community Dentistry and Oral Epidemiology.2017; 45(3): 193. CrossRef - Clinical validation and assessment of a modular fluorescent imaging system and algorithm for rapid detection and quantification of dental plaque
Keith Angelino, Pratik Shah, David A. Edlund, Mrinal Mohit, Gregory Yauney
BMC Oral Health.2017;[Epub] CrossRef
-
1,590
View
-
7
Download
-
7
Crossref
-
Analysis of C-shaped root canal configuration in maxillary molars in a Korean population using cone-beam computed tomography
-
Hyoung-Hoon Jo, Jeong-Bum Min, Ho-Keel Hwang
-
Restor Dent Endod 2016;41(1):55-62. Published online January 29, 2016
-
DOI: https://doi.org/10.5395/rde.2016.41.1.55
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Objectives
The purpose of this study was to investigate the incidence of root fusion and C-shaped root canals in maxillary molars, and to classify the types of C-shaped canal by analyzing cone-beam computed tomography (CBCT) in a Korean population. Materials and MethodsDigitized CBCT images from 911 subjects were obtained in Chosun University Dental Hospital between February 2010 and July 2012 for orthodontic treatment. Among them, a total of selected 3,553 data of maxillary molars were analyzed retrospectively. Tomography sections in the axial, coronal, and sagittal planes were displayed by PiViewstar and Rapidia MPR software (Infinitt Co.). The incidence and types of root fusion and C-shaped root canals were evaluated and the incidence between the first and the second molar was compared using Chi-square test. ResultsRoot fusion was present in 3.2% of the first molars and 19.5% of the second molars, and fusion of mesiobuccal and palatal root was dominant. C-shaped root canals were present in 0.8% of the first molars and 2.7% of the second molars. The frequency of root fusion and C-shaped canal was significantly higher in the second molar than the first molar (p < 0.001). ConclusionsIn a Korean population, maxillary molars showed total 11.3% of root fusion and 1.8% of C-shaped root canals. Furthermore, root fusion and C-shaped root canals were seen more frequently in the maxillary second molars.
-
Citations
Citations to this article as recorded by  - Prevalence of c-shaped canal morphology in premolar and molar teeth assessed by cone-beam computed tomography: systematic review and meta-analysis
Faezeh Yousefi, Younes Mohammadi, Elham Shokri
BMC Oral Health.2025;[Epub] CrossRef - A Cone‐Beam Computed Tomography Evaluation of C‐Shaped Canal Configuration in Maxillary Molars Among an Iranian Population
Nafiseh Nikkerdar, Mohammad Moslehi, Amin Golshah, Mario Dioguardi
International Journal of Dentistry.2024;[Epub] CrossRef - Endodontic treatment of a C‐shaped mandibular second molar with narrow dentinal thickness: A case report
Mina Mehrjouei, Hamid Jafarzadeh, Pourya Esmaeelpour, Maryam Khorasanchi
Clinical Case Reports.2024;[Epub] CrossRef - Evaluation of 2- and 3-dimensional anatomic parameters of C-shaped root canals with cone beam computed tomography, microcomputed tomography, and nanocomputed tomography
Miguel Angel Ventura Molina, Giovane Oliveira Silva, Amanda Pelegrin Candemil, Rafael Verardino de Camargo, Ruben Pauwels, Reinhilde Jacobs, Manoel Damião Sousa-Neto, Jardel Francisco Mazzi-Chaves
Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology.2023; 136(6): 759. CrossRef - Cone-Beam Computed Tomography (CBCT) Analysis of an Unusual Configuration of the Upper First Molar With a C-shaped Canal With Apically Fused Roots: A Case Report
Kapil D Wahane, Anand V Bansod, Sudha mattigatti, Rushikesh Mahaparale, Yuvraj B Rote, Mayur B Wanjari
Cureus.2023;[Epub] CrossRef - Assessment of C-Shaped Canal Morphology in Mandibular and Maxillary Second Molars in an Iraqi Subpopulation Using Cone-Beam Computed Tomography
Kazhan Abdalrahman, Ranjdar Talabani, Sara Kazzaz, Dlsoz Babarasul, Berndt Koslowski
Scanning.2022; 2022: 1. CrossRef - Root and canal-specific features of maxillary first molars with fused roots
Katarina Beljic-Ivanovic, Branislav Karadzic
Vojnosanitetski pregled.2022; 79(11): 1092. CrossRef - Diagnosis and treatment of maxillary molar with abnormality
Kkot-Byeol Bae, Bin-Na Lee, Hoon-Sang Chang, In-Nam Hwang, Won-Mann Oh, Yun-Chan Hwang
Oral Biology Research.2022; 46(4): 195. CrossRef - Endodontic treatment of the maxillary first molar with palatal canal variations: A case report and review of literature
Kai Chen, Xing Ran, Yan Wang
World Journal of Clinical Cases.2022; 10(32): 12036. CrossRef - Evaluation of C-shaped canals in maxillary molars in a Chinese population using CBCT
Yuyan Qian, Yamei Li, Jukun Song, Ping Zhang, Zhu Chen
BMC Medical Imaging.2022;[Epub] CrossRef - Comprehensive evaluation of root and root canal morphology of mandibular second molars in a Saudi subpopulation evaluated by cone-beam computed tomography
Moazzy I. Almansour, Saad M. Al‑Zubaidi, Abdulmjeed S. Enizy, Ahmed A. Madfa
BMC Oral Health.2022;[Epub] CrossRef - Evaluation of C-shaped canal configuration in maxillary molars: A retrospective cone-beam computed tomography study
Emre KÖSE, Rüya AK
Clinical and Experimental Health Sciences.2021; 11(3): 444. CrossRef - Maxillary First Molars with Two Palatal Root Canals
Kun-Hwa Sung, Ho-Keel Hwang, Hyoung-Hoon Jo, Konstantinos Michalakis
Case Reports in Dentistry.2021;[Epub] CrossRef - Preferred Reporting Items for Epidemiologic Cross-sectional Studies on Root and Root Canal Anatomy Using Cone-beam Computed Tomographic Technology: A Systematized Assessment
Jorge N.R. Martins, Anil Kishen, Duarte Marques, Emmanuel João Nogueira Leal Silva, João Caramês, António Mata, Marco A. Versiani
Journal of Endodontics.2020; 46(7): 915. CrossRef - Evaluation of root and root canal morphology of elderly Korean patients maxillary molars using cone-beam computed tomography
Tae-Yong Lee, Mi-Yeon Kim, Sun-Ho Kim, Jeong-Hee Kim
The Journal of Korean Academy of Prosthodontics.2020; 58(2): 95. CrossRef - Second mesiobuccal root canal in maxillary molars—A systematic review and meta-analysis of prevalence studies using cone beam computed tomography
Jorge N.R. Martins, Duarte Marques, Emmanuel João Nogueira Leal Silva, João Caramês, António Mata, Marco A. Versiani
Archives of Oral Biology.2020; 113: 104589. CrossRef - Prevalência estimada de canais “C- Shaped”: Uma revisão sistemática e meta-análise
Natália Pereira da Silva Falcão, Sandro Junio de Oliveira Tavares, Ludmila Silva Guimarães, Katherine Azevedo Batistela Rodrigues Thuller, Leonardo dos Santos Antunes, Estefano Borgo Sarmento, Fellipe Navarro Azevedo de Azevedo, Cinthya Cristina Gomes, Ca
Revista Científica Multidisciplinar Núcleo do Conhecimento.2020; : 91. CrossRef - Evaluation of the internal anatomy of paramolar tubercles using cone-beam computed tomography
G. Colakoglu, I. Kaya Buyukbayram, M. A. Elcin, M. Kazak, H. Sezer
Surgical and Radiologic Anatomy.2020; 42(1): 15. CrossRef - Analysis of Prevalence of Pyramidal Molars in Adolescent
Woojin Kwon, Hyung-Jun Choi, Jaeho Lee, Je Seon Song
THE JOURNAL OF THE KOREAN ACADEMY OF PEDTATRIC DENTISTRY.2020; 47(4): 389. CrossRef - Prevalence Studies on Root Canal Anatomy Using Cone-beam Computed Tomographic Imaging: A Systematic Review
Jorge N.R. Martins, Duarte Marques, Emmanuel João Nogueira Leal Silva, João Caramês, Marco A. Versiani
Journal of Endodontics.2019; 45(4): 372. CrossRef - Fused roots of maxillary molars: characterization and prevalence in a Latin American sub-population: a cone beam computed tomography study
Maytté Marcano-Caldera, Jose Luis Mejia-Cardona, María del Pilar Blanco-Uribe, Elena Carolina Chaverra-Mesa, Didier Rodríguez-Lezama, Jose Hernán Parra-Sánchez
Restorative Dentistry & Endodontics.2019;[Epub] CrossRef - An original micro‐CT study and meta‐analysis of the internal and external anatomy of maxillary molars—implications for endodontic treatment
Iwona M. Tomaszewska, Anna Jarzębska, Bendik Skinningsrud, Przemysław A. Pękala, Sebastian Wroński, Joe Iwanaga
Clinical Anatomy.2018; 31(6): 838. CrossRef - A Cone-beam Computed Tomographic Study of Root and Canal Morphology of Maxillary First and Second Permanent Molars in a Thai Population
Roserin Ratanajirasut, Anchana Panichuttra, Soontra Panmekiate
Journal of Endodontics.2018; 44(1): 56. CrossRef - Retrospective Assessment of Healing Outcome of Endodontic Treatment for Mandibular Molars with C-shaped Root Canal
Kishore Kumar Majety, Basanta Kumar Choudhury, Anika Bansal, Achla Sethi, Jaina Panjabi
The Journal of Contemporary Dental Practice.2017; 18(7): 591. CrossRef - The morphology of maxillary first and second molars analyzed by cone-beam computed tomography in a polish population
Katarzyna Olczak, Halina Pawlicka
BMC Medical Imaging.2017;[Epub] CrossRef
-
1,715
View
-
10
Download
-
25
Crossref
-
Apical foramen morphology according to the length of merged canal at the apex
-
Hee-Ho Kim, Jeong-Bum Min, Ho-Keel Hwang
-
Restor Dent Endod 2013;38(1):26-30. Published online February 26, 2013
-
DOI: https://doi.org/10.5395/rde.2013.38.1.26
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Objectives
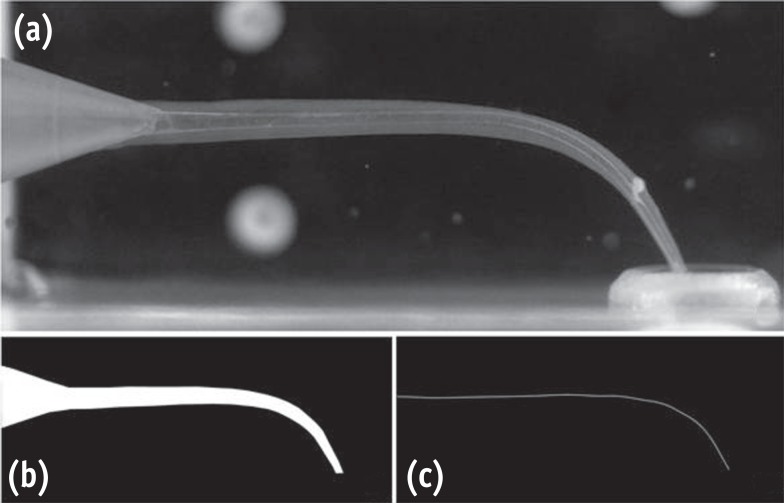
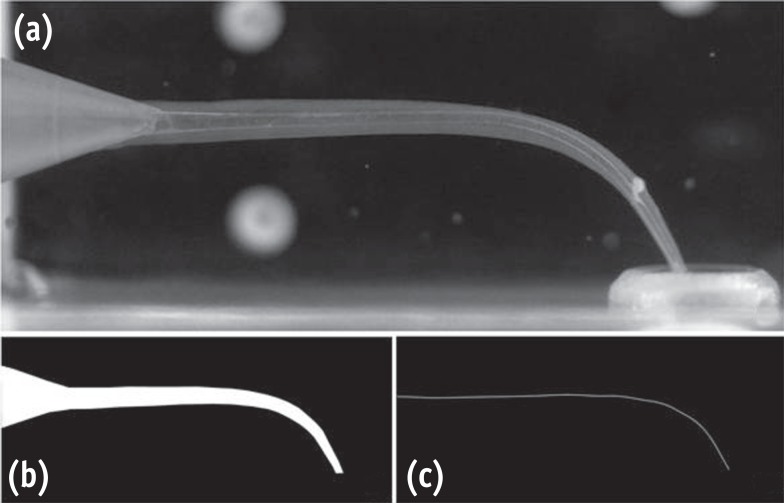
The aim of this study was to investigate the relationship between the apical foramen morphology and the length of merged canal at the apex in type II root canal system. Materials and MethodsThis study included intact extracted maxillary and mandibular human premolars (n = 20) with fully formed roots without any visible signs of external resorption. The root segments were obtained by removing the crown 1 mm beneath the cementum-enamel junction (CEJ) using a rotary diamond disk. The distance between the file tip and merged point of joining two canals was defined as Lj. The roots were carefully sectioned at 1 mm from the apex by a slow-speed water-cooled diamond saw. All cross sections were examined under the microscope at ×50 magnification and photographed to estimate the shape of the apical foramen. The longest and the shortest diameter of apical foramen was measured using ImageJ program (1.44p, National Institutes of Health). Correlation coefficient was calculated to identify the link between Lj and the apical foramen shape by Pearson's correlation. ResultsThe average value of Lj was 3.74 mm. The average of proportion (P), estimated by dividing the longest diameter into the shortest diameter of the apical foramen, was 3.64. This study showed a significant negative correlation between P and Lj (p < 0.05). ConclusionsAs Lj gets longer, the apical foramen becomes more ovally shaped. Likewise, as it gets shorter, the apical foramen becomes more flat shaped.
-
Citations
Citations to this article as recorded by  - Mandibular first premolar apical morphology: A stereomicroscopic study
Lama Awawdeh, Mousa Abu Fadaleh, Aladdin Al‐Qudah
Australian Endodontic Journal.2019; 45(2): 233. CrossRef - Surgical endodontic management of infected lateral canals of maxillary incisors
Ji-Hyun Jang, Jung-Min Lee, Jin-Kyu Yi, Sung-Baik Choi, Sang-Hyuk Park
Restorative Dentistry & Endodontics.2015; 40(1): 79. CrossRef
-
1,611
View
-
8
Download
-
2
Crossref
-
Power density of various light curing units through resin inlays with modified layer thickness
-
Sung-Ok Hong, Yonghui Oh, Jeong-Bum Min, Jin-Woo Kim, Bin-Na Lee, Yun-Chan Hwang, In-Nam Hwang, Won-Mann Oh, Hoon-Sang Chang
-
Restor Dent Endod 2012;37(3):130-135. Published online August 29, 2012
-
DOI: https://doi.org/10.5395/rde.2012.37.3.130
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Objectives
The purpose of this study was to enhance curing light penetration through resin inlays by modifying the thicknesses of the dentin, enamel, and translucent layers. Materials and MethodsTo investigate the layer dominantly affecting the power density of light curing units, resin wafers of each layer with 0.5 mm thickness were prepared and power density through resin wafers was measured with a dental radiometer (Cure Rite, Kerr). The dentin layer, which had the dominant effect on power density reduction, was decreased in thickness from 0.5 to 0.1 mm while thickness of the enamel layer was kept unchanged at 0.5 mm and thickness of the translucent layer was increased from 0.5 to 0.9 mm and vice versa, in order to maintain the total thickness of 1.5 mm of the resin inlay. Power density of various light curing units through resin inlays was measured. ResultsPower density measured through 0.5 mm resin wafers decreased more significantly with the dentin layer than with the enamel and translucent layers (p < 0.05). Power density through 1.5 mm resin inlays increased when the dentin layer thickness was reduced and the enamel or translucent layer thickness was increased. The highest power density was recorded with dentin layer thickness of 0.1 mm and increased translucent layer thickness in all light curing units. ConclusionsTo enhance the power density through resin inlays, reducing the dentin layer thickness and increasing the translucent layer thickness would be recommendable when fabricating resin inlays.
-
Citations
Citations to this article as recorded by  - Effects of layering technique on the shade of resin overlays and the microhardness of dual cure resin cement
Hoon-Sang Chang, Sung-Ok Hong
Brazilian Oral Research.2014;[Epub] CrossRef - Early Hardness and Shear Bond Strength of Dual-cure Resin Cement Light Cured Through Resin Overlays With Different Dentin-layer Thicknesses
H-S Chang, J-W Kim
Operative Dentistry.2014; 39(4): 398. CrossRef - Light curing of dual cure resin cement
Hoon-Sang Chang
Restorative Dentistry & Endodontics.2013; 38(4): 266. CrossRef
-
1,200
View
-
1
Download
-
3
Crossref
-
Evaluation of polymerization shrinkage stress in silorane-based composites
-
Seung-Ji Ryu, Ji-Hoon Cheon, Jeong-Bum Min
-
J Korean Acad Conserv Dent 2011;36(3):188-195. Published online May 31, 2011
-
DOI: https://doi.org/10.5395/JKACD.2011.36.3.188
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
-
Objectives
The purpose of this study was to evaluate the polymerization shrinkage stress among conventional methacrylate-based composite resins and a silorane-based composite resin.
Materials and Methods
The strain gauge method was used for the determination of polymerization shrinkage strain. Specimens were divided by 3 groups according to various composite materials. Filtek Z-250 (3M ESPE) and Filtek P-60 (3M ESPE) were used as a conventional methacrylate-based composites and Filtek P-90 (3M ESPE) was used as a silorane-based composites. Measurements were recorded at each 1 second for the total of 800 seconds including the periods of light application. The results of polymerization shrinkage stress were statistically analyzed using One way ANOVA and Tukey test (p = 0.05).
Results
The polymerization shrinkage stress of a silorane-based composite resin was lower than those of conventional methacrylate-based composite resins (p < 0.05). The shrinkage stress between methacrylate-based composite resin groups did not show significant difference (p > 0.05).
Conclusions
Within the limitation of this study, silorane-based composites showed lower polymerization shrinkage stress than methacrylate-based composites. We need to investigate more into polymerization shrinkage stress with regard to elastic modulus of silorane-based composites for the precise result.
-
Citations
Citations to this article as recorded by  - Polymerization shrinkage and stress analysis during dental restoration observed by digital image correlation method
Jung-Hoon Park, Nak-Sam Choi
Journal of Mechanical Science and Technology.2021; 35(12): 5435. CrossRef - Evaluation of the color stability of light cured composite resins according to the resin matrices
Da-Hye Yu, Hyun-Jin Jung, Sung-Hyeon Choi, In-Nam Hwang
Korean Journal of Dental Materials.2019; 46(2): 109. CrossRef - Behavior of Polymerization Shrinkage Stress of Methacrylate-based Composite and Silorane-based Composite during Dental Restoration
Jung-Hoon Park, Nak-Sam Choi
Composites Research.2015; 28(1): 6. CrossRef - Microtensile bond strength of silorane-based composite specific adhesive system using different bonding strategies
Laura Alves Bastos, Ana Beatriz Silva Sousa, Brahim Drubi-Filho, Fernanda de Carvalho Panzeri Pires-de-Souza, Lucas da Fonseca Roberti Garcia
Restorative Dentistry & Endodontics.2015; 40(1): 23. CrossRef
-
1,652
View
-
8
Download
-
4
Crossref
-
Surface roughness of composite resin according to finishing methods
-
Jeong-Bum Min, Kong-Chul Cho, Young-Gon Cho
-
J Korean Acad Conserv Dent 2007;32(2):138-150. Published online March 31, 2007
-
DOI: https://doi.org/10.5395/JKACD.2007.32.2.138
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
The purpose of this study was to evaluate the difference of surface roughness of composite resin according to composite resin type, polishing methods, and use of resin sealant.
Two hundred rectangular specimens, sized 8 × 3 × 2 mm, were made of Micro-new (Bisco, Inc., Schaumburg, IL, U.S.A) and Filtek Supreme (3M ESPE Dental Products, St. Paul, MN, U.S.A.), and divided into two groups; Micronew-M group, Filtek Supreme-S group. Specimens for each composite group were subdivided into five groups by finishing and polishing instruments used; M1 & S1 (polyester strip), M2 & S2 (Sof-Lex disc), M3 & S3 (Enhance disc and polishing paste), M4 & S4 (Astropol), and M5 & S5 (finishing bur). Polished groups were added letter B after the application of resin surface sealant (Biscover), eg, M1B and S1B.
After specimens were stored with distilled water for 24 hr, average surface roughness (Ra) was taken using a surface roughness tester. Representative specimens of each group were examined by FE-SEM (S-4700: Hitachi High Technologies Co., Tokyo, Japan). The data were analysed using paired t-test, ANOVA and Duncan's tests at the 0.05 probability level. The results of this study were as follows;
The lowest Ra was achieved in all groups using polyester strip and the highest Ra was achieved in M5, S5 and M5B groups using finishing bur. On FE-SEM, M1 and S1 groups provided the smoothest surfaces, M5 and S5 groups were presented the roughest surfaces and voids by debonding of filler on the polished specimens.
There was no significant difference in Ra between Micronew and Filtek Supreme before the application of resin sealant, but Micronew was smoother than Filek Supreme after the application of resin sealant.
There was significant corelation between Ra of type of composite resin and polishing methods before the application of resin sealant (p = 0.000), but no significant interaction between them after the application of resin sealant. On FE-SEM, most of composite resin surfaces were smooth after the application of resin sealant on the polished specimens.
Compared with before and after the application of resin sealant in group treated in the same composite and polishing methods, Ra of M4B and M5B was statistically lower than that of M4 and M5, and S5B was lower than that of S5, respectively (p < 0.05).
In conclusion, surface roughness by polishing instruments was different according to type of composite resin. Overall, polyester strip produced the smoothest surface, but finishing bur produced the roughest surface. Application of resin sealant provided the smooth surfaces in specimens polished with Enhance, Astropol and finishing bur, but not provided them in specimens polished with Sof-Lex disc.
|