Articles
- Page Path
- HOME > Restor Dent Endod > Volume 43(3); 2018 > Article
- Research Article CBCT study of mandibular first molars with a distolingual root in Koreans
-
Hee-Ho Kim
 , Hyoung-Hoon Jo
, Hyoung-Hoon Jo , Jeong-Bum Min
, Jeong-Bum Min , Ho-Keel Hwang
, Ho-Keel Hwang
-
Restor Dent Endod 2018;43(3):e33.
DOI: https://doi.org/10.5395/rde.2018.43.e33
Published online: July 30, 2018
Department of Conservative Dentistry, Chosun University School of Dentistry, Gwangju, Korea.
- Correspondence to Ho-Keel Hwang, DDS, PhD. Professor, Department of Conservative Dentistry, Chosun University School of Dentistry, 309 Pilmun-daero, Dong-gu, Gwangju 61452, Korea. rootcanal@hanmail.net
Copyright © 2018. The Korean Academy of Conservative Dentistry
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 1,688 Views
- 10 Download
- 10 Crossref
Abstract
-
Objectives This study aimed to investigate the prevalence of a separate distolingual root and to measure the thickness of the buccal cortical bone in mandibular first molars in Koreans using cone-beam computed tomography (CBCT) images.
-
Materials and Methods High-quality CBCT data from 432 patients were analyzed in this study. The prevalence of a separate distolingual root of the mandibular first molar was investigated. The distance from the distobuccal and distolingual root apices to the outer surface of the buccal cortical bone was measured. We also evaluated the thickness of the buccal cortical bone.
-
Results The prevalence of a separate distolingual root (2 separate distal roots with 1 canal in each root; 2R2C) was 23.26%. In mandibular first molars with 2R2C, the distance from the distobuccal root apex to the outer surface of the buccal cortical bone was 5.51 mm. Furthermore, the distance from the distolingual root apex to the outer surface of the buccal cortical bone was 12.09 mm. In mandibular first molars with 2R2C morphology, the thickness of the buccal cortical bone at the distobuccal root apex of the mandibular first molar was 3.30 mm. The buccal cortical bone at the distobuccal root apex was significantly thicker in the right side (3.38 mm) than the left side (3.09 mm) (p < 0.05).
-
Conclusions A separate distolingual root is not rare in mandibular first molars in the Korean population. Anatomic and morphologic knowledge of the mandibular first molar can be useful in treatment planning, including surgical endodontic treatment.
INTRODUCTION
MATERIALS AND METHODS
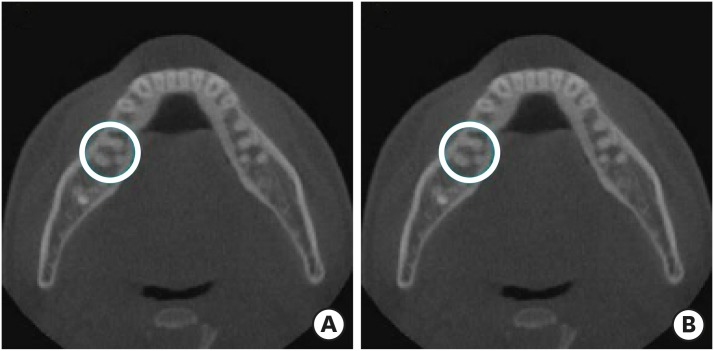
Representative cone-beam computed tomography images. (A) Mandibular first molar with the morphology of 2 separate distal roots with 1 canal in each root (blue circle); (B) Mandibular first molar with the morphology of 1 distal root with 2 separate canals (blue circle).
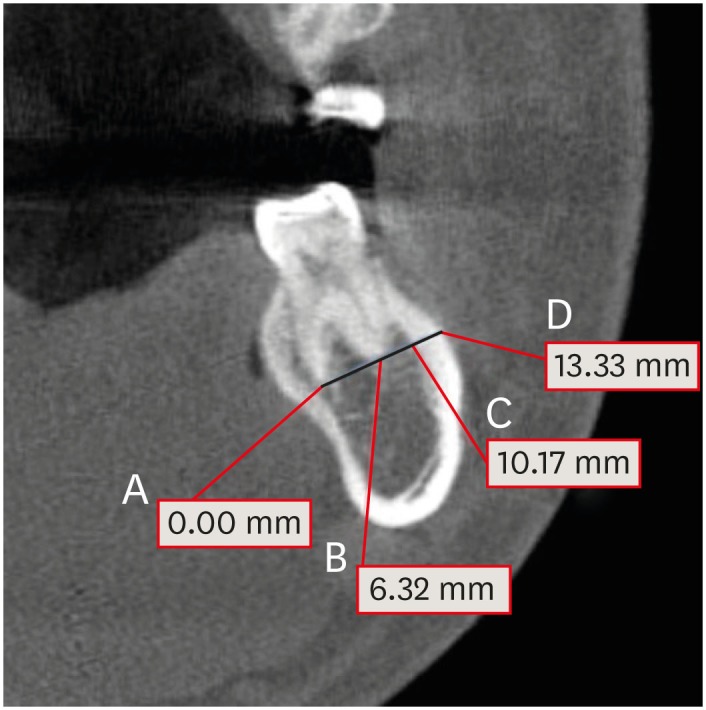
Representative measurements on the coronal plane of a cone-beam computed tomography image. Four points that intersected with the horizontal line crossing the apex of DB and DL root in a mandibular first molar with the morphology of 2 separate distal roots with 1 canal in each root were set up, as follows: (A) DL root apex; (B) DB root apex; (C) inner surface of the buccal cortical bone; (D) outer surface of the buccal cortical bone. The measurements at 4 points are the distances from point A.
RESULTS
Prevalence (%) of 2R2C and 1R2C morphology in the distal root of mandibular first molars
Unilateral and bilateral 2R2C morphology in mandibular first molars among Korean patients
| Unilateral left | Unilateral right | Bilateral | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Female | Male | Total | Female | Male | Total | Female | Male | Total | |
| 2R2C | 5 | 0 | 5 | 14 | 20 | 34 | 32 | 49 | 81 (18.75) |
The distance (mm) from the DB and DL root apices to the outer surface of the buccal cortical bone in mandibular first molars with 2R2C morphology
| DB root to buccal bone | DL root to buccal bone | |||||
|---|---|---|---|---|---|---|
| Left | Right | Total | Left | Right | Total | |
| 2R2C | 5.27 ± 1.73a | 5.70 ± 2.01a | 5.51 ± 1.90B | 11.57 ± 2.07b | 12.48 ± 2.38a | 12.09 ± 2.29A |
Thickness (mm) of the buccal cortical bone in mandibular first molars with 2R2C morphology
| Buccal cortical bone thickness | |||
|---|---|---|---|
| Left | Right | Total | |
| 2R2C | 3.09 ± 1.08b | 3.38 ± 1.09a | 3.30 ± 1.09 |
DISCUSSION
CONCLUSIONS
-
Funding: This study was supported by a research fund from Chosun University Dental Hospital in 2018.
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Kim HH, Hwang HK.
Data curation: Kim HH, Hwang HK.
Formal analysis: Kim HH, Jo HH, Min JB, Hwang HK.
Funding acquisition: Jo HH, Min JB, Hwang HK.
Investigation: Kim HH, Jo HH, Min JB, Hwang HK.
Methodology: Kim HH, Jo HH, Min JB, Hwang HK.
Project administration: Kim HH, Hwang HK.
Resources: Kim HH, Jo HH, Min JB.
Software: Kim HH, Jo HH, Min JB.
Supervision: Jo HH, Min JB, Hwang HK.
Validation: Kim HH, Jo HH, Min JB, Hwang HK.
Visualization: Kim HH, Min JB.
Writing - original draft: Kim HH.
Writing - review & editing: Kim HH, Jo HH, Min JB, Hwang HK.
- 1. Song JS, Choi HJ, Jung IY, Jung HS, Kim SO. The prevalence and morphologic classification of distolingual roots in the mandibular molars in a Korean population. J Endod 2010;36:653-657.ArticlePubMed
- 2. Wang Y, Zheng QH, Zhou XD, Tang L, Wang Q, Zheng GN, Huang DM. Evaluation of the root and canal morphology of mandibular first permanent molars in a western Chinese population by cone-beam computed tomography. J Endod 2010;36:1786-1789.ArticlePubMed
- 3. Tu MG, Tsai CC, Jou MJ, Chen WL, Chang YF, Chen SY, Cheng HW. Prevalence of three-rooted mandibular first molars among Taiwanese individuals. J Endod 2007;33:1163-1166.ArticlePubMed
- 4. Chen YC, Lee YY, Pai SF, Yang SF. The morphologic characteristics of the distolingual roots of mandibular first molars in a Taiwanese population. J Endod 2009;35:643-645.ArticlePubMed
- 5. De Moor RJ, Deroose CA, Calberson FL. The radix entomolaris in mandibular first molars: an endodontic challenge. Int Endod J 2004;37:789-799.ArticlePubMed
- 6. Stephen C, Hargreaves KM. Pathways of the pulp. 9th ed. St. Louis, MO: Mosby Elsevier; 2005. Chapter 7, 20.
- 7. Lin L, Skribner J, Shovlin F, Langeland K. Periapical surgery of mandibular posterior teeth: anatomical and surgical considerations. J Endod 1983;9:496-501.ArticlePubMed
- 8. Cotton TP, Geisler TM, Holden DT, Schwartz SA, Schindler WG. Endodontic applications of cone-beam volumetric tomography. J Endod 2007;33:1121-1132.ArticlePubMed
- 9. Tu MG, Huang HL, Hsue SS, Hsu JT, Chen SY, Jou MJ, Tsai CC. Detection of permanent three-rooted mandibular first molars by cone-beam computed tomography imaging in Taiwanese individuals. J Endod 2009;35:503-507.ArticlePubMed
- 10. Patel S, Dawood A, Ford TP, Whaites E. The potential applications of cone beam computed tomography in the management of endodontic problems. Int Endod J 2007;40:818-830.ArticlePubMed
- 11. Nair MK, Nair UP. Digital and advanced imaging in endodontics: a review. J Endod 2007;33:1-6.ArticlePubMed
- 12. Choi MR, Moon YM, Seo MS. Prevalence and features of distolingual roots in mandibular molars analyzed by cone-beam computed tomography. Imaging Sci Dent 2015;45:221-226.ArticlePubMedPMC
- 13. Gulabivala K, Opasanon A, Ng YL, Alavi A. Root and canal morphology of Thai mandibular molars. Int Endod J 2002;35:56-62.ArticlePubMed
- 14. Song JS, Kim SO, Choi BJ, Choi HJ, Son HK, Lee JH. Incidence and relationship of an additional root in the mandibular first permanent molar and primary molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;107:e56-e60.ArticlePubMed
- 15. Walker RT, Quackenbush LE. Three-rooted lower first permanent molars in Hong Kong Chinese. Br Dent J 1985;159:298-299.ArticlePubMedPDF
- 16. Loh HS. Incidence and features of three-rooted permanent mandibular molars. Aust Dent J 1990;35:434-437.ArticlePubMed
- 17. Curzon ME. Three-rooted mandibular permanent molars in English Caucasians. J Dent Res 1973;52:181.ArticlePubMedPDF
- 18. Huang RY, Cheng WC, Chen CJ, Lin CD, Lai TM, Shen EC, Chiang CY, Chiu HC, Fu E. Three-dimensional analysis of the root morphology of mandibular first molars with distolingual roots. Int Endod J 2010;43:478-484.ArticlePubMed
- 19. Kim SY, Yang SE. Cone-beam computed tomography study of incidence of distolingual root and distance from distolingual canal to buccal cortical bone of mandibular first molars in a Korean population. J Endod 2012;38:301-304.ArticlePubMed
- 20. Gutmann JL, Harrison JW. Posterior endodontic surgery: anatomical considerations and clinical techniques. Int Endod J 1985;18:8-34.ArticlePubMed
- 21. Matthews LS, Hirsch C. Temperatures measured in human cortical bone when drilling. J Bone Joint Surg Am 1972;54:297-308.ArticlePubMed
- 22. Eriksson RA, Albrektsson T, Magnusson B. Assessment of bone viability after heat trauma. A histological, histochemical and vital microscopic study in the rabbit. Scand J Plast Reconstr Surg 1984;18:261-268.ArticlePubMed
REFERENCES
Tables & Figures
REFERENCES
Citations

- The association between complex root canal morphology of mandibular anteriors and distolingual roots in mandibular first molars in a Turkish population
Özge Kurt, Elif Solakoğlu
BMC Oral Health.2025;[Epub] CrossRef - Radix molaris is a hidden truth of mandibular first permanent molars: A descriptive- analytic study using cone beam computed tomography
Mohammed A. Alobaid, Saurabh Chaturvedi, Ebtihal Mobarak S. Alshahrani, Ebtsam M. Alshehri, Amal S. Shaiban, Mohamed Khaled Addas, Giuseppe Minervini
Technology and Health Care.2023; 31(5): 1957. CrossRef - Prevalence of radix entomolaris in India and its comparison with the rest of the world
Sumit MOHAN, Jyoti THAKUR
Minerva Dental and Oral Science.2022;[Epub] CrossRef - A critical analysis of laboratory and clinical research methods to study root and canal anatomy
Hany Mohamed Aly Ahmed
International Endodontic Journal.2022; 55(S2): 229. CrossRef - Three‐Rooted Permanent Mandibular First Molars: A Meta‐Analysis of Prevalence
Nyan M. Aung, Kyaw K. Myint, Luca Testarelli
International Journal of Dentistry.2022;[Epub] CrossRef - Reproducibilidad en el diagnóstico imagenológico de periodontitis apical a partir de CBCT
Sandra Milena Buitrago Rojas, Yeny Zulay Castellanos Dominguez, Jhonny Alexander Contreras Vargas, Yosdi Tomás Solano Diaz, Eder Fabián Gutierrez Argote
Acta Odontológica Colombiana.2020;[Epub] CrossRef - Assessment of Root and Root Canal Morphology of Human Primary Molars using CBCT
Yoomin Choi, Seonmi Kim, Namki Choi
THE JOURNAL OF THE KOREAN ACADEMY OF PEDTATRIC DENTISTRY.2020; 47(1): 25. CrossRef - The prevalence of radix molaris in the mandibular first molars of a Saudi subpopulation based on cone-beam computed tomography
Hassan AL-Alawi, Saad Al-Nazhan, Nassr Al-Maflehi, Mazen A. Aldosimani, Mohammed Nabil Zahid, Ghadeer N. Shihabi
Restorative Dentistry & Endodontics.2020;[Epub] CrossRef - Preferred Reporting Items for Epidemiologic Cross-sectional Studies on Root and Root Canal Anatomy Using Cone-beam Computed Tomographic Technology: A Systematized Assessment
Jorge N.R. Martins, Anil Kishen, Duarte Marques, Emmanuel João Nogueira Leal Silva, João Caramês, António Mata, Marco A. Versiani
Journal of Endodontics.2020; 46(7): 915. CrossRef - Evaluation of roots and canal systems of mandibular first molars in a vietnamese subpopulation using cone-beam computed tomography
KhoaVan Pham, AnhHoang Lan Le
Journal of International Society of Preventive and Community Dentistry.2019; 9(4): 356. CrossRef
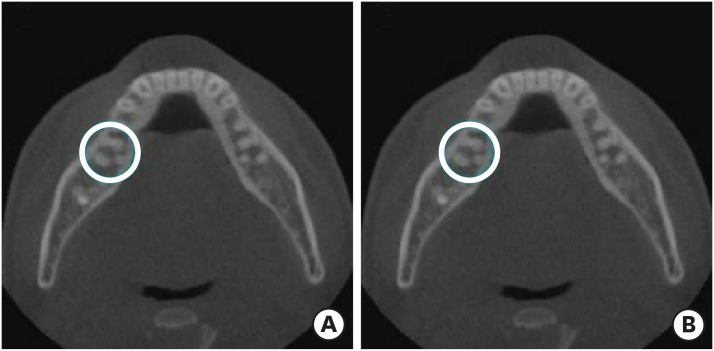
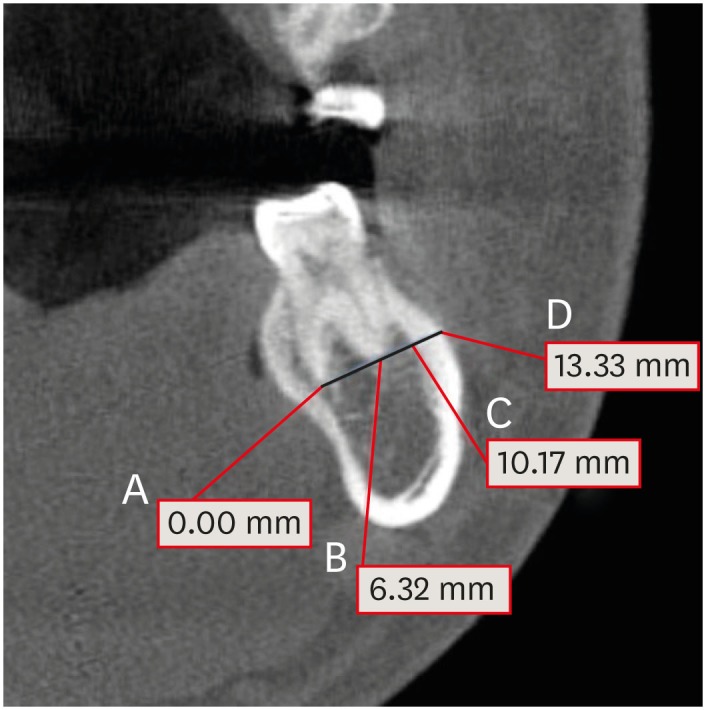
Figure 1
Figure 2
Prevalence (%) of 2R2C and 1R2C morphology in the distal root of mandibular first molars
| Left | Right | Overall | |||||
|---|---|---|---|---|---|---|---|
| Female | Male | Total | Female | Male | Total | ||
| 2R2C | 37 | 49 | 86 (19.91) | 55 | 60 | 115 (26.62) | 201 (23.26) |
| 1R2C | 51 | 65 | 116 (26.85) | 49 | 57 | 106 (24.54) | 222 (25.69) |
| 1R1C | 121 | 109 | 230 (53.24) | 105 | 106 | 211 (48.84) | 441 (51.04) |
| Total | 209 | 223 | 432 (100) | 209 | 223 | 432 (100) | 864 (100) |
Values are presented as number of patients or number of teeth; Values in the parentheses were prevalence in percentage (%).
2R2C, 2 separate distal roots with 1 canal in each root; 1R2C, 1 distal root with 2 separate canals.
Unilateral and bilateral 2R2C morphology in mandibular first molars among Korean patients
| Unilateral left | Unilateral right | Bilateral | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Female | Male | Total | Female | Male | Total | Female | Male | Total | |
| 2R2C | 5 | 0 | 5 | 14 | 20 | 34 | 32 | 49 | 81 (18.75) |
Values are presented as number of patients or number of teeth; Values in the parenthesis was prevalence in percentage (%).
2R2C, 2 separate distal roots with 1 canal in each root.
The distance (mm) from the DB and DL root apices to the outer surface of the buccal cortical bone in mandibular first molars with 2R2C morphology
| DB root to buccal bone | DL root to buccal bone | |||||
|---|---|---|---|---|---|---|
| Left | Right | Total | Left | Right | Total | |
| 2R2C | 5.27 ± 1.73a | 5.70 ± 2.01a | 5.51 ± 1.90B | 11.57 ± 2.07b | 12.48 ± 2.38a | 12.09 ± 2.29A |
Different lowercase superscript letters indicate significant differences between the left and right sides (p < 0.05). Different uppercase superscript letters indicate significant differences between DB and DL roots (p < 0.05).
DB, distobuccal; DL, distolingual; 2R2C, 2 separate distal roots with 1 canal in each root.
Thickness (mm) of the buccal cortical bone in mandibular first molars with 2R2C morphology
| Buccal cortical bone thickness | |||
|---|---|---|---|
| Left | Right | Total | |
| 2R2C | 3.09 ± 1.08b | 3.38 ± 1.09a | 3.30 ± 1.09 |
Different superscript letters indicate a significant difference between the groups (p < 0.05).
2R2C, 2 separate distal roots with 1 canal in each root.
Values are presented as number of patients or number of teeth; Values in the parentheses were prevalence in percentage (%).
2R2C, 2 separate distal roots with 1 canal in each root; 1R2C, 1 distal root with 2 separate canals.
Values are presented as number of patients or number of teeth; Values in the parenthesis was prevalence in percentage (%).
2R2C, 2 separate distal roots with 1 canal in each root.
Different lowercase superscript letters indicate significant differences between the left and right sides (
DB, distobuccal; DL, distolingual; 2R2C, 2 separate distal roots with 1 canal in each root.
Different superscript letters indicate a significant difference between the groups (
2R2C, 2 separate distal roots with 1 canal in each root.

 KACD
KACD
 ePub Link
ePub Link Cite
Cite

