Search
- Page Path
- HOME > Search
- Evaluation of platelet concentrates in regenerative endodontics: a systematic review and meta-analysis
- Anna Tsiolaki, Dimitrios Theocharis, Nikolaos Tsitsipas, Anastasia Fardi, Konstantinos Kodonas
- Restor Dent Endod 2025;50(4):e38. Published online November 28, 2025
- DOI: https://doi.org/10.5395/rde.2025.50.e38
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - Objectives
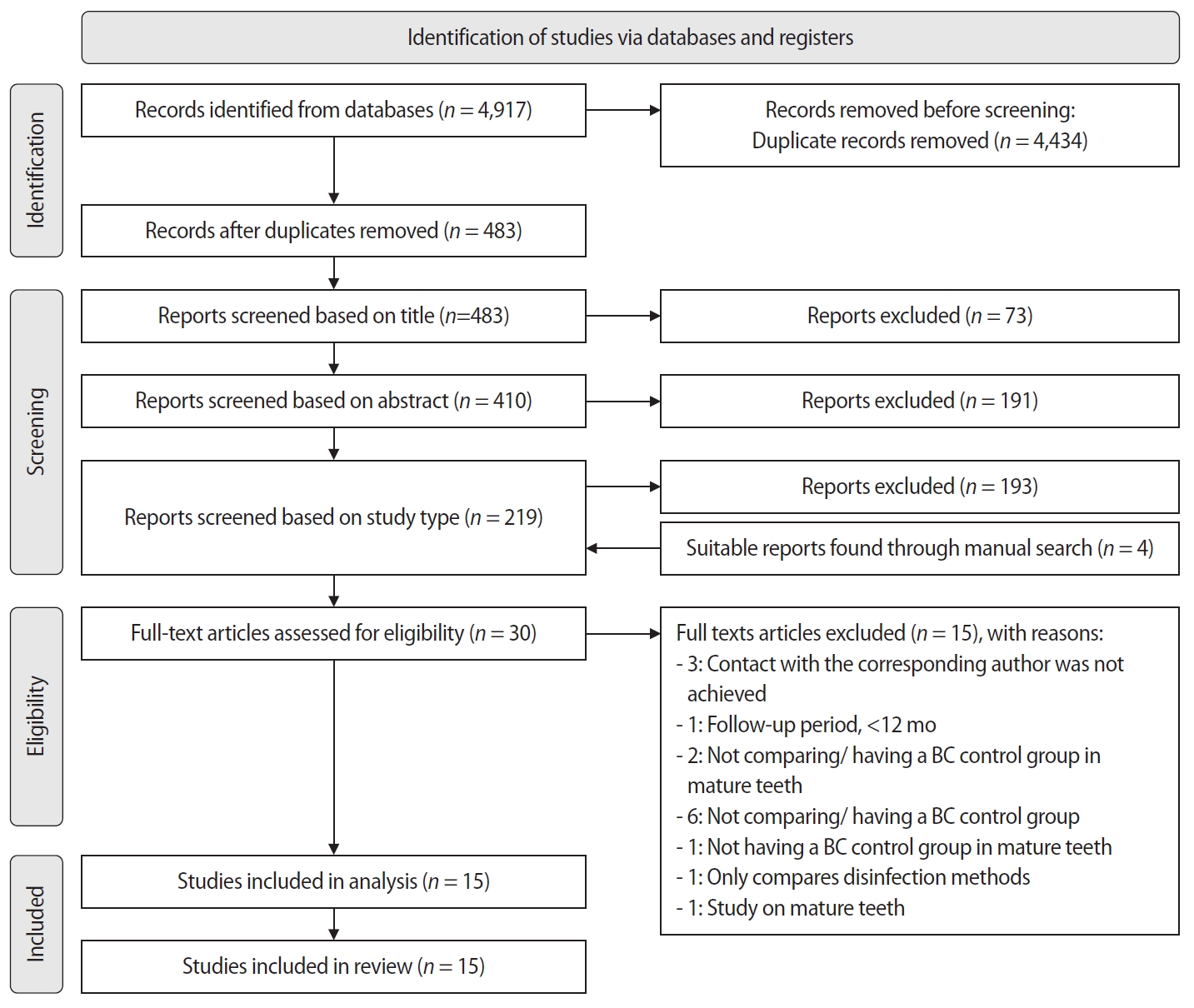
The aim of this systematic review is to compare the effectiveness of advanced platelet concentrates as regenerative endodontic therapeutic alternatives to blood clot (BC) revascularization in immature permanent necrotic teeth.
Methods
Randomized controlled trials (RCTs) comparing regenerative endodontic therapies using platelet-rich plasma (PRP), platelet-rich fibrin (PRF), or platelet pellet (PP) with the BC revascularization approach in immature permanent necrotic teeth were systematically searched in PubMed, Scopus, Cochrane Library, and Web of Science until May 2025. Data was extracted and analyzed both qualitatively and quantitatively. Study quality was assessed using the Cochrane Risk of Bias tool. A meta-analysis was conducted using IBM SPSS software (version 29.0), with success rates expressed as risk ratios and 95% confidence intervals (CIs).
Results
The initial search yielded 4,917 studies. After removing duplicates and applying eligibility criteria, 15 RCTs were included. Meta-analysis indicated no significant difference in the risk ratio (RR), as the BC method has similar success rates with PRP (10 studies; RR = 1.01; 95% CI, 0.94–1.09; p = 0.76) and PRF (8 studies; RR = 0.98; 95% CI, 0.89–1.08; p = 0.65) at 12 months. The primary outcomes evaluated were based on clinical and radiographic success.
Conclusions
Current evidence suggests PRP, PRF, and BC are all effective in treating immature permanent necrotic teeth with similar success rates. However, further research is needed to assess long-term outcomes.
- 878 View
- 50 Download

-
The influence of sodium hypochlorite concentration on the fibrin structure of human blood clots and transforming growth factor-beta 1 release: an
ex vivo study - Anisha Mishra, Velmurugan Natanasabapathy, Nandini Suresh
- Restor Dent Endod 2022;47(4):e42. Published online October 31, 2022
- DOI: https://doi.org/10.5395/rde.2022.47.e42
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
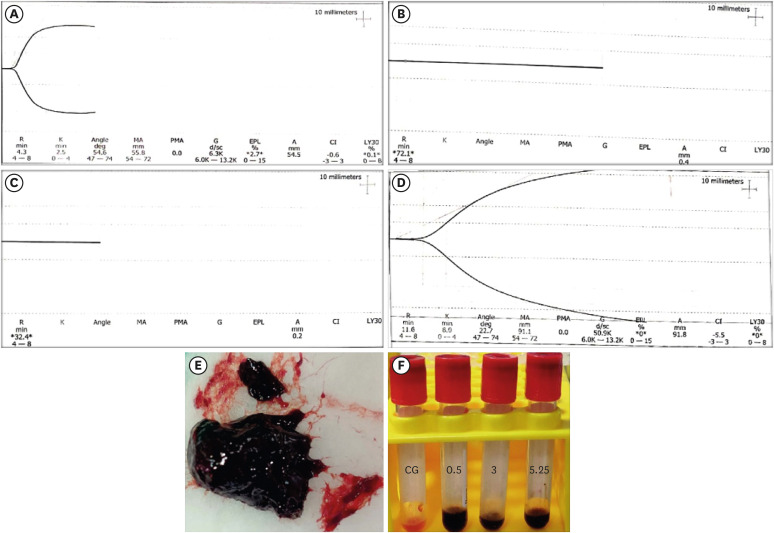
ePub Objective This study investigated the effects of various concentrations of sodium hypochlorite (NaOCl) on human whole-blood clotting kinetics, the structure of the blood clots formed, and transforming growth factor (TGF)-β1 release.
Materials and Methods Human whole blood was collected from 5 healthy volunteers and divided into 4 groups: CG (control, 0.5 mL of blood), BN0.5 (0.5 mL of blood with 0.5 mL of 0.5% NaOCl), BN3 (0.5 mL of blood with 0.5 mL of 3% NaOCl), and BN5.25 (0.5 mL of blood with 0.5 mL of 5.25% NaOCl). The effects of NaOCl on clotting kinetics, structure of fibrin and cells, and release of TGF-β1 were assessed using thromboelastography (TEG), scanning electron microscopy (SEM), and enzyme-linked immunosobent assay, respectively. Statistical analysis was conducted using the Kruskal Wallis and Mann-Whitney
U tests, followed by thepost hoc Dunn test. Ap value < 0.05 indicated statistical significance.Results The blood samples in BN0.5 and BN3 did not clot, whereas the TEG of BN5.25 showed altered clot formation. Samples from the CG and BN3 groups could only be processed with SEM, which showed that the latter lacked fibrin formation and branching of fibers, as well as clumping of red blood cells with surface roughening and distortion. TGF-β1 release was significantly highest in BN3 when all groups were compared to CG (
p < 0.05).Conclusions Each concentration of NaOCl affected the release of TGF-β1 from blood clots and altered the clotting mechanism of blood by affecting clotting kinetics and cell structure.
-
Citations
Citations to this article as recorded by- Cytotoxic Effects of Synthetic and Herbal Endodontic Irrigants on Human Red Blood Cells: An In Vitro Study
Panna Mangat, Bhaviya Chandel, Mampi Biswas, Sara Trivedy, Akshata Gupta, Nayan Shree, Seema Gupta
Cureus.2025;[Epub] CrossRef
- Cytotoxic Effects of Synthetic and Herbal Endodontic Irrigants on Human Red Blood Cells: An In Vitro Study
- 1,759 View
- 30 Download
- 1 Crossref

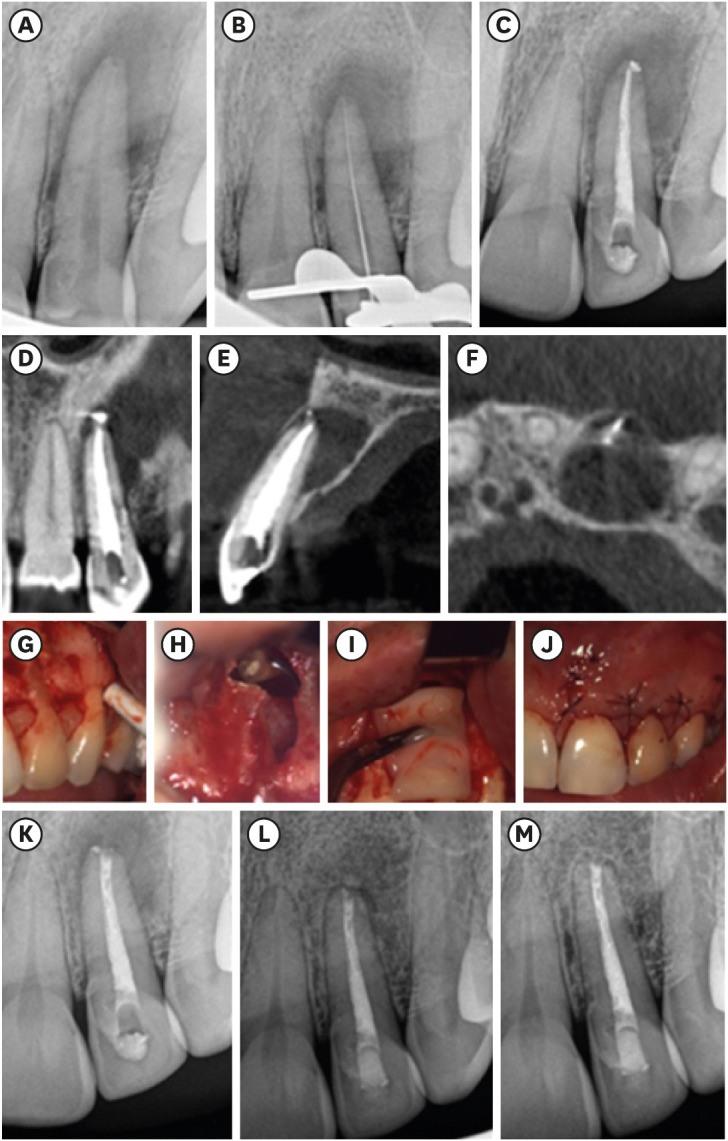
- Evaluation of blood clot, platelet-rich plasma, and platelet-rich fibrin–mediated regenerative endodontic procedures in teeth with periapical pathology: a CBCT study
- Swati Markandey, Haridas Das Adhikari
- Restor Dent Endod 2022;47(4):e41. Published online October 21, 2022
- DOI: https://doi.org/10.5395/rde.2022.47.e41
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
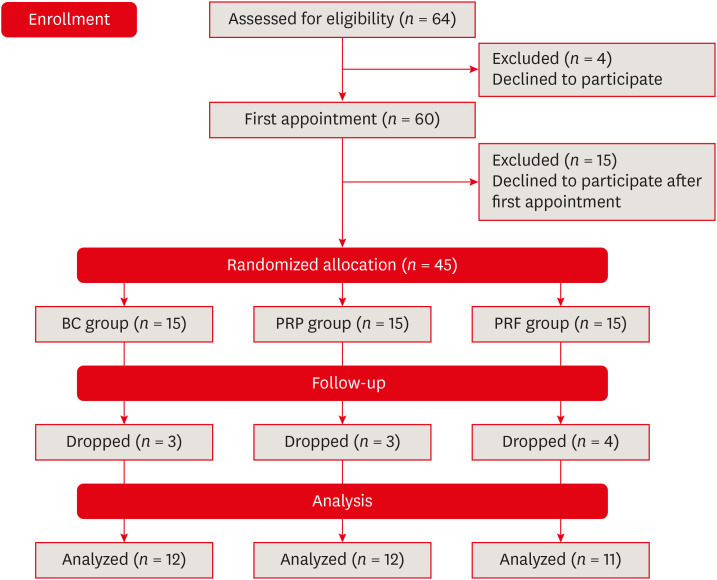
ePub Objectives This study compared the clinical and radiological outcomes of regenerative endodontic procedures (REPs) using blood clots (BCs), platelet-rich plasma (PRP), and platelet-rich fibrin (PRF) through intraoral periapical radiography (IOPAR) and cone-beam computed tomography (CBCT).
Materials and Methods Forty-five single-rooted necrotic teeth with periapical pathology were randomly allocated to receive BC, PRP, or PRF as an individual scaffold. Outcomes were evaluated in 35 teeth in 23 patients with a follow-up period of 12–24 months through qualitative IOPAR scoring and quantitative CBCT measurements. Healing of periapical lesions and in immature teeth, changes in the apical foramen diameter (AFD), root wall thickness (RWT), and root length (RL) were assessed. A
p value less than 0.05 was considered to indicate statistical significance.Results All teeth were asymptomatic except 1 in the PRP group. Periapical lesion healing was seen in all except 2 teeth in the BC group and 3 in the PRP group. Both IOPAR and CBCT revealed no significant differences in bone healing or changes in AFD, RWT, and RL among the 3 groups. A positive pulp sensibility response to the cold test was seen in 2 teeth in the BC group, but none to the electric pulp test. Intracanal calcification (ICC) was evident in more teeth in the BC group than in the PRP and PRF groups, and was also significantly higher in immature teeth.
Conclusions Our results revealed that BC, PRP, and PRF have similar potential as scaffolds in REPs, and ICC may be a concern for long-term outcomes.
-
Citations
Citations to this article as recorded by- Regenerative potential of concentrated growth factor compared to platelet-rich fibrin in treatment of necrotic mature teeth: a randomized clinical trial
Taghreed Salah, Wael Hussein, Heba Abdelkafy
BDJ Open.2025;[Epub] CrossRef - Clinical and radiographic outcomes of non-surgical retreatment of mature maxillary incisors using two regenerative endodontic techniques in adolescents: a 24-month randomized clinical trial
Ahmad Abdel Hamid Elheeny, Sherif Shafik EL Bahnasy, Yassmin Mohamed ElMakawi, Mohammed Turky, Eman Farouk Ahmed, Norhan Khaled Omar Wahba
BDJ Open.2025;[Epub] CrossRef - Clinical and Radiographic Outcomes of Autologous Platelet-Rich Products in Regenerative Endodontics: A Systematic Review and Meta-Analysis
Raewyn Huang, Wei Chen, Matthew Fang, Ove A. Peters, Sepanta Hosseinpour
Dentistry Journal.2025; 13(6): 236. CrossRef - Regenerative Endodontics in the Treatment of Periapical Lesions of Endodontic Origin: A Systematic Review of Randomized Controlled Trials
BelHaj Salah Kawthar, Berrima Fatma, Boukhris Hanen, Gnaba Imen, Ben Youssef Souha
The Journal of Contemporary Dental Practice.2025; 26(6): 623. CrossRef - Advanced Platelet-Rich Fibrin Plus Sealed Exclusively with Glass Ionomer Cement: Setting a New Standard for Healing, Aesthetics and Predictive Modelling in Regenerative Endodontics
Dubravka Turjanski, Dragutin Lisjak, Petra Bučević Sojčić, Jelena Valpotić, Tea Borojević Renić, Kristina Goršeta, Domagoj Glavina
Materials.2025; 18(18): 4421. CrossRef - Evaluation of different scaffolds and intracanal medications in revascularization of nonvital immature permanent teeth
Mona M. A. Sameia, Abeer M. Darrag, Neveen A. Shaheen, Dina A. Attia
Tanta Dental Journal.2025; 22(4): 693. CrossRef - Biomimetic pulp scaffolds prepared from extracellular matrix derived from stem cells from human exfoliated deciduous teeth promote pulp–dentine complex regeneration
Ning Yang, Rou Shen, Wenxiao Yang, Shengcai Zhang, Tianxing Gong, Yao Liu
International Endodontic Journal.2024; 57(9): 1279. CrossRef - Arrest and Repair of Inflammatory Root Resorption After an Endodontic Regeneration Procedure – A Hypothesis and Case Report
Arieh Y. Kaufman, Bill Kahler
Journal of Endodontics.2024; 50(12): 1743. CrossRef - Effect of Platelet Rich Plasma in Regenerative Endodontic Treatment: A Review of Clinical Trials
Hojat Rezazadeh, Mehrnaz Okhovatfard
Research Journal of Pharmacy and Technology.2023; : 5562. CrossRef
- Regenerative potential of concentrated growth factor compared to platelet-rich fibrin in treatment of necrotic mature teeth: a randomized clinical trial
- 4,357 View
- 108 Download
- 6 Web of Science
- 9 Crossref

- Endodontic micro-resurgery and guided tissue regeneration of a periapical cyst associated to recurrent root perforation: a case report
- Fernando Córdova-Malca, Hernán Coaguila-Llerena, Lucía Garré-Arnillas, Jorge Rayo-Iparraguirre, Gisele Faria
- Restor Dent Endod 2022;47(4):e35. Published online September 3, 2022
- DOI: https://doi.org/10.5395/rde.2022.47.e35
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
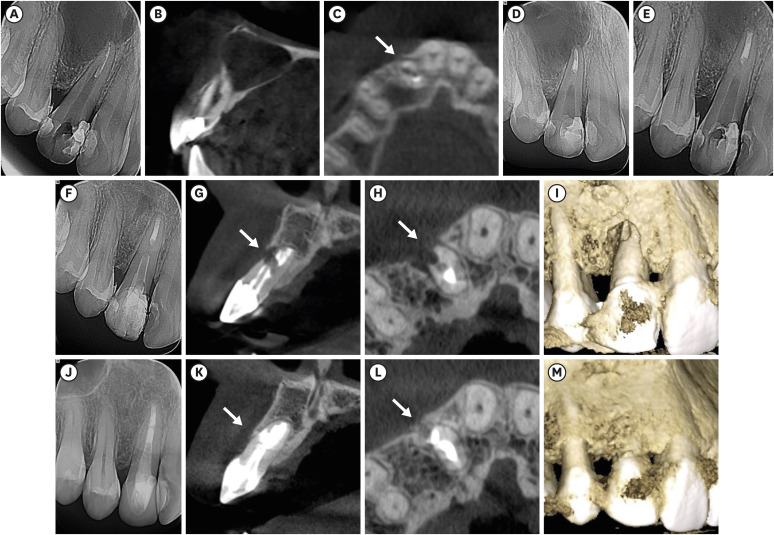
ePub Although the success rates of microsurgery and micro-resurgery are very high, the influence of a recurrent perforation combined with radicular cyst remains unclear. A 21-year-old white female patient had a history of root perforation in a previously treated right maxillary lateral incisor. Analysis using cone-beam computed tomography (CBCT) revealed an extensive and well-defined periapical radiolucency, involving the buccal and palatal bone plate. The perforation was sealed with bioceramic material (Biodentine) in the pre-surgical phase. In the surgical phase, guided tissue regeneration (GTR) was performed by combining xenograft (lyophilized bovine bone) and autologous platelet-rich fibrin applied to the bone defect. The root-end preparation was done using an ultrasonic tip. The retrograde filling was performed using a bioceramic material (Biodentine). Histopathological analysis confirmed a radicular cyst. The patient returned to her referring practitioner to continue the restorative procedures. CBCT analysis after 1-year recall revealed another perforation in the same place as the first intervention, ultimately treated by micro-resurgery using the same protocol with GTR, and a bioceramic material (MTA Angelus). The 2-year recall showed healing and bone neoformation. In conclusion, endodontic micro-resurgery with GTR showed long-term favorable results when a radicular cyst and a recurrent perforation compromised the success.
-
Citations
Citations to this article as recorded by- Outcome of endodontic micro-resurgery: A systematic review
Faisal Alnassar, Riyadh Alroomy, Qamar Hashem, Abdullah Alqedairi, Nabeel Almotairy
Saudi Endodontic Journal.2025; 15(2): 112. CrossRef - Platelet-Rich Plasma and Platelet-Rich Fibrin in Endodontics: A Scoping Review
Simão Rebimbas Guerreiro, Carlos Miguel Marto, Anabela Paula, Joana Rita de Azevedo Pereira, Eunice Carrilho, Manuel Marques-Ferreira, Siri Vicente Paulo
International Journal of Molecular Sciences.2025; 26(12): 5479. CrossRef - Non-surgical Approach to a Maxillary Cyst-Like Lesion: Orthograde Endodontic Treatment With Neodymium-Doped Yttrium Aluminum Garnet (Nd:YAG) Decontamination of the Canal System
Beatrice Spaggiari, Paolo Vescovi, Silvia Pizzi, Roberta Iaria, Ilaria Giovannacci
Cureus.2025;[Epub] CrossRef - Persistent Periradicular Lesion Associated With Concurrent Root Fracture and Odontogenic Keratocyst: A Case Report
Mehdi Vatanpour, Fatemeh Rezaei
Clinical Case Reports.2025;[Epub] CrossRef - Management of Apico-marginal Defects With Endodontic Microsurgery and Guided Tissue Regeneration: A Report of Thirteen Cases
Abayomi O. Baruwa, Jorge N.R. Martins, Mariana D. Pires, Beatriz Pereira, Pedro May Cruz, António Ginjeira
Journal of Endodontics.2023; 49(9): 1207. CrossRef
- Outcome of endodontic micro-resurgery: A systematic review
- 2,701 View
- 53 Download
- 4 Web of Science
- 5 Crossref

- Leukocyte platelet-rich fibrin in endodontic microsurgery: a report of 2 cases
- Mariana Domingos Pires, Jorge N. R. Martins, Abayomi Omokeji Baruwa, Beatriz Pereira, António Ginjeira
- Restor Dent Endod 2022;47(2):e17. Published online March 4, 2022
- DOI: https://doi.org/10.5395/rde.2022.47.e17
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Endodontic microsurgery is a predictable treatment option when orthograde treatment or retreatment is unsuccessful or unfeasible. However, when there is a gross compromise of periapical bone, achievement of bone regeneration after the surgical procedure may be hampered. In such cases, the application of guided tissue regeneration principles, with adjunctive use of leukocyte platelet-rich fibrin to fill the bone defect as a bone substitute and as a membrane to cover the site, provides a cost-effective solution with the benefits of accelerated physiological healing and reduced post-surgical pain and discomfort. This case report presents 2 cases of endodontic microsurgery of the upper lateral incisors with loss of buccal cortical plate, where platelet-rich fibrin was successfully applied.
-
Citations
Citations to this article as recorded by- Focuses and Trends of Research on Platelet-Rich Fibrin: A Bibliometric and Visual Analysis
Ying Zhao, Chen Dong, Liumeizi Fan, Ting Lei, Xin Ge, Zhou Yu, Sheng Hu
Indian Journal of Plastic Surgery.2024; 57(05): 356. CrossRef
- Focuses and Trends of Research on Platelet-Rich Fibrin: A Bibliometric and Visual Analysis
- 1,559 View
- 30 Download
- 1 Web of Science
- 1 Crossref

- Clinical effectiveness of combining platelet rich fibrin with alloplastic bone substitute for the management of combined endodontic periodontal lesion
- Lata Goyal
- Restor Dent Endod 2014;39(1):51-55. Published online January 20, 2014
- DOI: https://doi.org/10.5395/rde.2014.39.1.51
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub The term "endo-perio" lesion has been proposed to describe the destructive lesion resulting from inflammatory products found in varying degrees in both the periodontium and the pulpal tissues. In most of the cases, clinical symptoms disappear following successful endodontic therapy. However failure after conventional root canal treatment calls for surgical intervention. A 35 year old male patient with endo-perio lesion in right maxillary lateral incisor was treated with platelet rich fibrin (PRF) and alloplastic bone substitute after conventional endodontic therapy. At the end of 6 months there was gain in clinical attachment, increased radiographic bone fill and reduction in probing depth which was maintained till 18 month follow-up. Present case report aims to evaluate the efficacy of PRF and alloplastic bone substitute in the management of intrabony defect associated with endo-perio lesion in maxillary lateral incisor because the healing potential of PRF and bone graft has not been widely studied in endodontics. The use of PRF allows the clinician to optimize tissue remodelling, wound healing and angiogenesis by the local delivery of growth factors and proteins. The novel technique described here enables the clinician to be benefited from the full regenerative capacity of this autologous biologic material.
-
Citations
Citations to this article as recorded by- To Analyze the Efficacy of Platelet-rich Plasma in Contrast to Platelet-rich Fibrin along with Synthetic Nanocrystalline Hydroxyapatite and β-tricalcium Phosphate Bone Graft in Regeneration of Bony Defects in Children
Anshul Sharma, Sonali Saha, Amit Rai, Kavita Dhinsa, Nonie Marianne Koksi Sangma Shadap, Gunjan Yadav
International Journal of Clinical Pediatric Dentistry.2024; 16(6): 842. CrossRef - Regenerative Endodontic Management of an Immature Necrotic Premolar Using Advanced Platelet‐Rich Fibrin
Sepideh Hosseini, Nazanin Chitsaz, Mohammad Hassan Hamrah, Donya Maleki, Emad Taghizadeh, Hamdi Cem Gungor
Case Reports in Dentistry.2023;[Epub] CrossRef - Effect of biodentine coated with emdogain on proliferation and differentiation of human stem cells from the apical papilla
Hamed Karkehabadi, Erfan Ahmadyani, Rezvan Najafi, Elham Khoshbin
Molecular Biology Reports.2022; 49(5): 3685. CrossRef - Healing Assessment of Osseous Defects after Surgical Removal of Periapical Lesions in the Presence of Hydroxyapatite, Nanohydroxyapatite, and a Combination of Nanohydroxyapatite and Platelet-rich Fibrin: A Clinical Study
Amira Elkholly, Maged Negm, Reham Hassan, Nada Omar
Open Access Macedonian Journal of Medical Sciences.2022; 10(D): 406. CrossRef - Case report on combining PRF with alloplastic bone substitute in Endo-Perio lesion
Mansi Bansal, Manish Khatri, Komal Puri
Restorative Dentistry & Endodontics.2021;[Epub] CrossRef Treatment of an Endo-Perio Lesion with Ozone Gas in a Patient with Aggressive Periodontitis: A Clinical Case Report and Literature Review
Maria K Makeeva, Fatima Yu Daurova, Svetlana F Byakova, Anna Yu Turkina
Clinical, Cosmetic and Investigational Dentistry.2020; Volume 12: 447. CrossRef- Revisit to endo-perio lesion a review
Roopali Sharma, Akshita Gupta, K K. Gupta, Sarah Jameel, Rashmika Kapoor
IP International Journal of Periodontology and Implantology.2020; 5(2): 48. CrossRef - Autologous platelet-rich derivatives along with alloplastic bone substitute in the management of complex perio-endo cases
Lata Goyal, Namita Gupta, NarinderDev Gupta
Journal of Indian Society of Periodontology.2020; 24(2): 182. CrossRef - Platelet-Rich Fibrin as a Bone Graft Material in Oral and Maxillofacial Bone Regeneration: Classification and Summary for Better Application
Yiping Liu, Xiaolin Sun, Jize Yu, Jia Wang, Peisong Zhai, Siyu Chen, Manxuan Liu, Yanmin Zhou
BioMed Research International.2019; 2019: 1. CrossRef - Acute periodontal lesions (periodontal abscesses and necrotizing periodontal diseases) and endo‐periodontal lesions
David Herrera, Belén Retamal‐Valdes, Bettina Alonso, Magda Feres
Journal of Clinical Periodontology.2018;[Epub] CrossRef - Acute periodontal lesions (periodontal abscesses and necrotizing periodontal diseases) and endo‐periodontal lesions
David Herrera, Belén Retamal‐Valdes, Bettina Alonso, Magda Feres
Journal of Periodontology.2018;[Epub] CrossRef - Regenerative in endodontics: how, when and where
AL Ahmar Rima, Bassam Sanaa, Salloum Sarah, El Husseini Hassan, AL Ahmar Rima
Journal of Dental Health, Oral Disorders & Therapy.2018; 9(6): 531. CrossRef - Effect of Choukroun Platelet-Rich Fibrin Combined With Autologous Micro-Morselized Bone on the Repair of Mandibular Defects in Rabbits
Tian Zhou, Hua-Wei Yang, Zhuo-Wei Tian, Yang Wang, Xiao-Shan Tang, Jing-Zhou Hu
Journal of Oral and Maxillofacial Surgery.2018; 76(1): 221. CrossRef - Preliminary Results of Bone Regeneration in Oromaxillomandibular Surgery Using Synthetic Granular Graft
Noemi Mazzone, E. Mici, A. Calvo, M. Runci, S. Crimi, F. Lauritano, E. Belli
BioMed Research International.2018; 2018: 1. CrossRef - Treatment of endo-periodontal lesion using leukocyte- platelet- rich fibrin. A case report
Pablo Betancourt, Ricardo Elgueta, Ramon Fuentes
Colombia Medica.2017; 48(4): 204. CrossRef - The impact of autologous platelet concentrates on endodontic healing: a systematic review
Nastaran Meschi, Ana B. Castro, Katleen Vandamme, Marc Quirynen, Paul Lambrechts
Platelets.2016; 27(7): 613. CrossRef - A review of the regenerative endodontic treatment procedure
Bin-Na Lee, Jong-Wook Moon, Hoon-Sang Chang, In-Nam Hwang, Won-Mann Oh, Yun-Chan Hwang
Restorative Dentistry & Endodontics.2015; 40(3): 179. CrossRef - Platelet preparations in dentistry: How? Why? Where? When?
Luigi Fabrizio Rodella
World Journal of Stomatology.2015; 4(2): 39. CrossRef
- To Analyze the Efficacy of Platelet-rich Plasma in Contrast to Platelet-rich Fibrin along with Synthetic Nanocrystalline Hydroxyapatite and β-tricalcium Phosphate Bone Graft in Regeneration of Bony Defects in Children
- 1,541 View
- 4 Download
- 18 Crossref

- Platelet rich fibrin - a novel acumen into regenerative endodontic therapy
- Kavita Hotwani, Krishna Sharma
- Restor Dent Endod 2014;39(1):1-6. Published online January 20, 2014
- DOI: https://doi.org/10.5395/rde.2014.39.1.1
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Research into regenerative dentistry has added impetus onto the field of molecular biology. It can be documented as a prototype shift in the therapeutic armamentarium for dental disease. Regenerative endodontic procedures are widely being added to the current armamentarium of pulp therapy procedures. The regenerative potential of platelets has been deliberated. A new family of platelet concentrates called the platelet rich fibrin (PRF) has been recently used by several investigators and has shown application in diverse disciplines of dentistry. This paper is intended to add light on the various prospects of PRF and clinical insights to regenerative endodontic therapy.
-
Citations
Citations to this article as recorded by- Biomaterials to biofabrication: advanced scaffold technologies for regenerative endodontics
Arun Mayya, Akshatha Chatra, Vinita Dsouza, Raviraja N Seetharam, Shashi Rashmi Acharya, Kirthanashri S Vasanthan
Biomedical Physics & Engineering Express.2026; 12(1): 012001. CrossRef - Apicoectomy versus apical curettage in combination with or without L-PRF application: a randomized clinical trial
Serap Gulsever, Seyda Ersahan, Yelda Erdem Hepsenoglu, Alperen Tekin
Scientific Reports.2025;[Epub] CrossRef - Platelet-Rich Plasma and Platelet-Rich Fibrin in Endodontics: A Scoping Review
Simão Rebimbas Guerreiro, Carlos Miguel Marto, Anabela Paula, Joana Rita de Azevedo Pereira, Eunice Carrilho, Manuel Marques-Ferreira, Siri Vicente Paulo
International Journal of Molecular Sciences.2025; 26(12): 5479. CrossRef - Pulp regeneration treatment using different bioactive materials in permanent teeth of pediatric subjects
Dina Abdellatif, Alfredo Iandolo, Giuseppina De Benedetto, Francesco Giordano, Davide Mancino, Edouard Euvrard, Massimo Pisano
Journal of Conservative Dentistry and Endodontics.2024; 27(5): 458. CrossRef - Analysis of Pulp Tissue Viability and Cytotoxicity of Pulp Capping Agents
Pratima Panda, Shashirekha Govind, Sanjit Kumar Sahoo, Satabdi Pattanaik, Rachappa M. Mallikarjuna, Triveni Nalawade, Sanjay Saraf, Naseer Al Khaldi, Salma Al Jahdhami, Vinay Shivagange, Amit Jena
Journal of Clinical Medicine.2023; 12(2): 539. CrossRef - Implantation Effect of a Fibrin Matrix Associated with Mesenchymal Wharton’s Jelly Stromal Cells on the Course of an Experimental Spinal Cord Injury
V. V. Medvediev, N. P. Oleksenko, L. D. Pichkur, S. A. Verbovska, S. I. Savosko, N. G. Draguntsova, Yu. A. Lontkovskyi, V. V. Vaslovych, V. I. Tsymbalyuk
Cytology and Genetics.2023; 57(1): 19. CrossRef - Advanced Platelet-rich Fibrin-mediated Regeneration of Necrotic Immature Permanent Teeth: A Clinico-radiographic Observational Study
Ashi Chug, Sagrika Shukla, Tulika Wakhloo, Mridul Dhar
International Journal of Clinical Pediatric Dentistry.2022; 15(4): 402. CrossRef - Effect of Implantation of a Fibrin Matrix Associated with Neonatal Brain Cells on the Course of an Experimental Spinal Cord Injury
V. V. Medvediev, N. P. Oleksenko, L. D. Pichkur, S. A. Verbovska, S. I. Savosko, N. G. Draguntsova, Yu. A. Lontkovskiy, V. V. Vaslovych, V. I. Tsymbalyuk
Cytology and Genetics.2022; 56(2): 125. CrossRef - Comparison of Autologous Platelet-Rich Fibrin Matrix and Transplantation of Autologous Noncultured Epidermal Cell Suspension in the Treatment of Chronic Non Healing Ulcer
Satyendra K. Singh, Sri Rupa
Indian Journal of Dermatology.2022; 67(4): 334. CrossRef - Effect of amniotic membrane and platelet‐rich fibrin membrane on bone healing post endodontic surgery: An ultrasonographic, randomized controlled study
Saumya Johri, Promila Verma, Aseem Prakash Tikku, Rhythm Bains, Neera Kohli
Journal of Tissue Engineering and Regenerative Medicine.2022; 16(12): 1208. CrossRef - Effect of biodentine coated with emdogain on proliferation and differentiation of human stem cells from the apical papilla
Hamed Karkehabadi, Erfan Ahmadyani, Rezvan Najafi, Elham Khoshbin
Molecular Biology Reports.2022; 49(5): 3685. CrossRef - SINGLE VISIT- APEXIFICATION USING MTA AND AUTOLOGOUS PRF AS AN INTERNAL MATRIX. A CASE SERIES.
Deepika Deepika, Abhishek Sharma, Ajay Kumar Nagpal, Muhammad Mutiur Rahman
INTERNATIONAL JOURNAL OF SCIENTIFIC RESEARCH.2022; : 61. CrossRef - COMPARATIVE CLINICAL, RADIOGRAPHICAL AND HISTOLOGICAL EVALUATION OF CORONAL PULPOTOMY TECHNIQUE WITH PRF AND A NOVEL CROSSLINKED PRF AS AN ALTERNATIVE TO PULPECTOMY FOR PRESERVING THE TOOTH VITALITY IN CONTEXT OF TISSUE ENGINEERING.
Suman Kar, R. R. Paul, H. D. Adhikari, Swagata Gayen, Sandip Sinha
INTERNATIONAL JOURNAL OF SCIENTIFIC RESEARCH.2022; : 84. CrossRef - Clinical Application of Platelet-Rich Fibrin in Pediatric Dentistry
Sowndarya Gunasekaran, Soundarya Sakthivel, Shanthala B. M., George Babu, Vidhya Vijayan
Journal of Health and Allied Sciences NU.2022; 12(02): 186. CrossRef - Platelet-Rich Fibrin Used as a Scaffold in Pulp Regeneration: Case Series
Ceren ÇİMEN, Selin ŞEN, Elif ŞENAY, Tuğba BEZGİN
Cumhuriyet Dental Journal.2021; 24(1): 113. CrossRef - Treatment of Miller I Mandibular Gingival Recessions Using PRF vs. Connective Graft
Hernan S. Garzon, Camilo Alfonso, Francisco J. Vega, Andrea García, Ana Muñoz, Gustavo Jaimes, Katherine Isaza, Katherine Rivera, Gaetano Isola
International Journal of Dentistry.2021; 2021: 1. CrossRef - Human Umbilical Cord Mesenchymal Stem Cells Over Platelet Rich Fibrin Scaffold for Mandibular Cartilage Defects Regenerative Medicine
Ni Putu Mira Sumarta, David Buntoro Kamadjaja, Nike Hendrijantini, Coen Pramono Danudiningrat, Fedik Abdul Rantam
Pesquisa Brasileira em Odontopediatria e Clínica Integrada.2021;[Epub] CrossRef - Platelet-Rich Fibrin Enhances Surgical Wound Healing in Total Laryngectomy
Mirta H. Reksodiputro, Syahrial M. Hutauruk, Dini W. Widodo, Fauziah Fardizza, Dita Mutia
Facial Plastic Surgery.2021; 37(03): 325. CrossRef - Role of Platelet-Rich Fibrin (PRF) and Platelet-Rich Plasma (PRP) in Oro-Facial Tissue Regeneration: A Narrative Review
Modhi Al Deeb
Journal of Advanced Oral Research.2020; 11(1): 5. CrossRef - Efficacy of Autologous Platelet Concentrates in Regenerative Endodontic Treatment: A Systematic Review of Human Studies
Joanna Metlerska, Irini Fagogeni, Alicja Nowicka
Journal of Endodontics.2019; 45(1): 20. CrossRef - Autologous platelet-rich-fibrin-induced revascularization sequelae: Two case reports
Ahmed M Eltawila, Rania El Backly
World Journal of Stomatology.2019; 7(3): 28. CrossRef - Revascularization of a Nonvital, Immature Permanent Tooth Using Amniotic Membrane: A Novel Approach
Meghna Bajaj, Ashu J Soni
International Journal of Clinical Pediatric Dentistry.2019; 12(2): 150. CrossRef - Biomimetics in Endodontics: A Review of the Changing Trends in Endodontics
Jalak Patel, Tejal Sheth, Dhwanit Thakore, Dharmesh Dhamat
Journal of Advanced Oral Research.2018; 9(1-2): 11. CrossRef - Regenerative in endodontics: how, when and where
AL Ahmar Rima, Bassam Sanaa, Salloum Sarah, El Husseini Hassan, AL Ahmar Rima
Journal of Dental Health, Oral Disorders & Therapy.2018; 9(6): 531. CrossRef - Effects of the nitric oxide releasing biomimetic nanomatrix gel on pulp-dentin regeneration: Pilot study
Chan-Yang Moon, Ok Hyung Nam, Misun Kim, Hyo-Seol Lee, Sagar N. Kaushik, David A. Cruz Walma, Ho-Wook Jun, Kyounga Cheon, Sung Chul Choi, Jinkee Hong
PLOS ONE.2018; 13(10): e0205534. CrossRef - Growth Factors and Cell Homing in Dental Tissue Regeneration
Henry F. Duncan, Yoshifumi Kobayashi, Emi Shimizu
Current Oral Health Reports.2018; 5(4): 276. CrossRef - Use of Leukocyte Platelet (L-PRF) Rich Fibrin in Diabetic Foot Ulcer with Osteomyelitis (Three Clinical Cases Report)
Alessandro Crisci, Giuseppe Marotta, Anna Licito, Edda Serra, Giulio Benincasa, Michela Crisci
Diseases.2018; 6(2): 30. CrossRef - Pulp Regeneration Concepts for Nonvital Teeth: From Tissue Engineering to Clinical Approaches
Valérie Orti, Pierre-Yves Collart-Dutilleul, Sofía Piglionico, Orsolya Pall, Frédéric Cuisinier, Ivan Panayotov
Tissue Engineering Part B: Reviews.2018; 24(6): 419. CrossRef - Long-term cytokine and growth factor release from equine platelet-rich fibrin clots obtained with two different centrifugation protocols
Román F. Jiménez-Aristizabal, Catalina López, María E. Álvarez, Carlos Giraldo, Marta Prades, Jorge U. Carmona
Cytokine.2017; 97: 149. CrossRef - Rejeneratif Pulpa Tedavilerine Genel Bir Bakış
Elif Sungurtekin Ekçi
Cumhuriyet Dental Journal.2017; 19(3): 238. CrossRef - Three-dimensional structure and cytokine distribution of platelet-rich fibrin
Meng-Yi Bai, Ching-Wei Wang, Jyun-Yi Wang, Ming-Fang Lin, Wing P Chan
Clinics.2017; 72(2): 116. CrossRef - The impact of autologous platelet concentrates on endodontic healing: a systematic review
Nastaran Meschi, Ana B. Castro, Katleen Vandamme, Marc Quirynen, Paul Lambrechts
Platelets.2016; 27(7): 613. CrossRef - Platelet concentrates for revitalization of immature necrotic teeth: a systematic review of the clinical studies
Alessandra Lolato, Cristina Bucchi, Silvio Taschieri, Ahmed El Kabbaney, Massimo Del Fabbro
Platelets.2016; 27(5): 383. CrossRef - Endodontie in der unreifen bleibenden Dentition — Maßnahmen zur Vitalerhaltung, Apexifikation und Regeneration der Pulpa
Martin Jung
Oralprophylaxe & Kinderzahnheilkunde.2016; 38(1): 29. CrossRef - A review of the regenerative endodontic treatment procedure
Bin-Na Lee, Jong-Wook Moon, Hoon-Sang Chang, In-Nam Hwang, Won-Mann Oh, Yun-Chan Hwang
Restorative Dentistry & Endodontics.2015; 40(3): 179. CrossRef - Platelet preparations in dentistry: How? Why? Where? When?
Luigi Fabrizio Rodella
World Journal of Stomatology.2015; 4(2): 39. CrossRef - The use of platelet rich plasma in the treatment of immature tooth with periapical lesion: a case report
Günseli Güven Polat, Ceren Yıldırım, Özlem Martı Akgün, Ceyhan Altun, Didem Dinçer, Cansel Köse Özkan
Restorative Dentistry & Endodontics.2014; 39(3): 230. CrossRef
- Biomaterials to biofabrication: advanced scaffold technologies for regenerative endodontics
- 2,367 View
- 19 Download
- 37 Crossref


 KACD
KACD

 First
First Prev
Prev


