Articles
- Page Path
- HOME > Restor Dent Endod > Volume 47(4); 2022 > Article
- Case Report Endodontic micro-resurgery and guided tissue regeneration of a periapical cyst associated to recurrent root perforation: a case report
-
Fernando Córdova-Malca1
 , Hernán Coaguila-Llerena2
, Hernán Coaguila-Llerena2 , Lucía Garré-Arnillas3
, Lucía Garré-Arnillas3 , Jorge Rayo-Iparraguirre3
, Jorge Rayo-Iparraguirre3 , Gisele Faria2
, Gisele Faria2
-
Restor Dent Endod 2022;47(4):e35.
DOI: https://doi.org/10.5395/rde.2022.47.e35
Published online: September 3, 2022
1Department of Endodontics, Cayetano Heredia Peruvian University (UPCH), Lima, Peru.
2Department of Restorative Dentistry, Araraquara School of Dentistry, São Paulo State University (UNESP), Araraquara, SP, Brazil.
3Academic Department of Stomatological Clinic, Cayetano Heredia Peruvian University (UPCH), Lima, Peru.
- Correspondence to Hernán Coaguila-Llerena, DDS, MSc. PhD Student, Department of Restorative Dentistry, Araraquara School of Dentistry, São Paulo State University (UNESP), Rua Humaitá 1680, Araraquara, SP 14801-903, Brazil. ehernanco@gmail.com
Copyright © 2022. The Korean Academy of Conservative Dentistry
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
- Although the success rates of microsurgery and micro-resurgery are very high, the influence of a recurrent perforation combined with radicular cyst remains unclear. A 21-year-old white female patient had a history of root perforation in a previously treated right maxillary lateral incisor. Analysis using cone-beam computed tomography (CBCT) revealed an extensive and well-defined periapical radiolucency, involving the buccal and palatal bone plate. The perforation was sealed with bioceramic material (Biodentine) in the pre-surgical phase. In the surgical phase, guided tissue regeneration (GTR) was performed by combining xenograft (lyophilized bovine bone) and autologous platelet-rich fibrin applied to the bone defect. The root-end preparation was done using an ultrasonic tip. The retrograde filling was performed using a bioceramic material (Biodentine). Histopathological analysis confirmed a radicular cyst. The patient returned to her referring practitioner to continue the restorative procedures. CBCT analysis after 1-year recall revealed another perforation in the same place as the first intervention, ultimately treated by micro-resurgery using the same protocol with GTR, and a bioceramic material (MTA Angelus). The 2-year recall showed healing and bone neoformation. In conclusion, endodontic micro-resurgery with GTR showed long-term favorable results when a radicular cyst and a recurrent perforation compromised the success.
INTRODUCTION
CASE REPORT
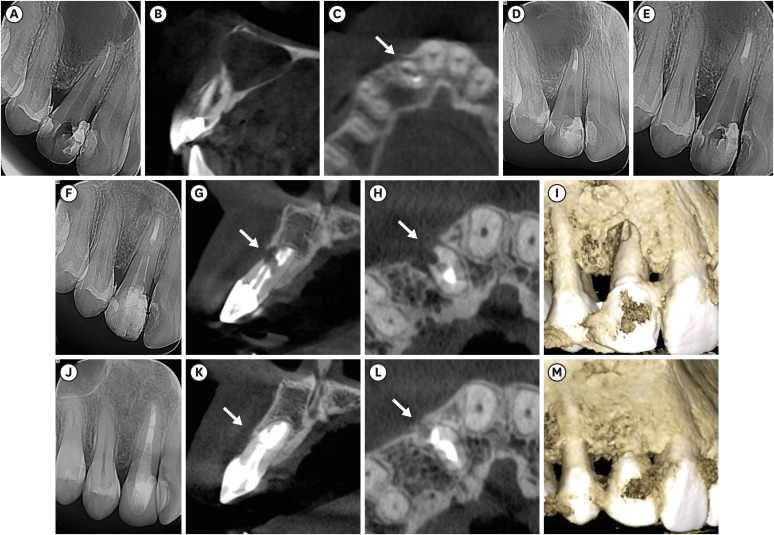
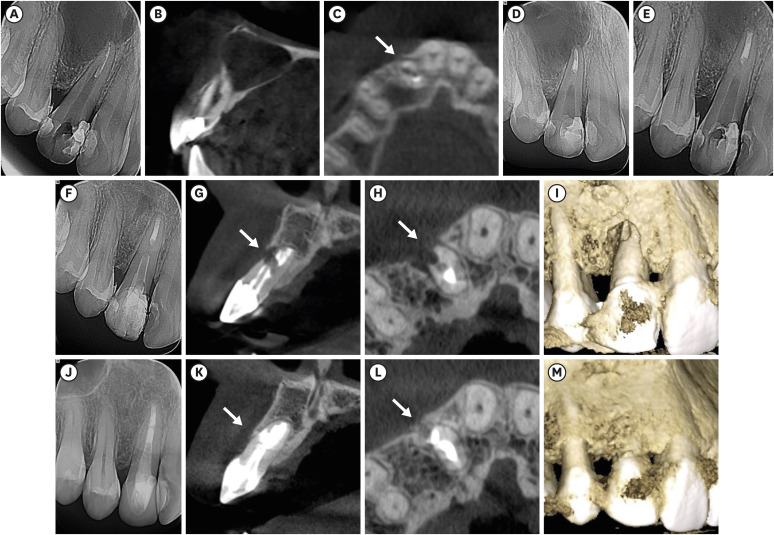
Chronological radiographs and CBCT images of the case management. Preoperative radiograph (A). Sagittal plane of a CBCT image, confirming that the cyst compromised buccal and palatal bone plates (B). Axial plane of a CBCT image, confirming the first perforation. The white arrow indicates the perforation (C). Immediate post-surgical radiograph (D). Periapical radiographs after 1 month and 1 year, respectively. As can be observed, the cyst is apparently decreasing in size (E, F). Sagittal and axial planes of CBCT images, confirming the second perforation, respectively. The white arrows indicate the perforation (G, H). Three-dimensional CBCT reconstruction. The buccal bone plate is clearly affected (I). Periapical radiograph 2 years after micro-resurgery (J). Sagittal and axial planes of CBCT images 2 years after micro-resurgery, confirming new bone formation—white arrows (K, L). Three-dimensional CBCT reconstruction 2 years after micro-resurgery (M).
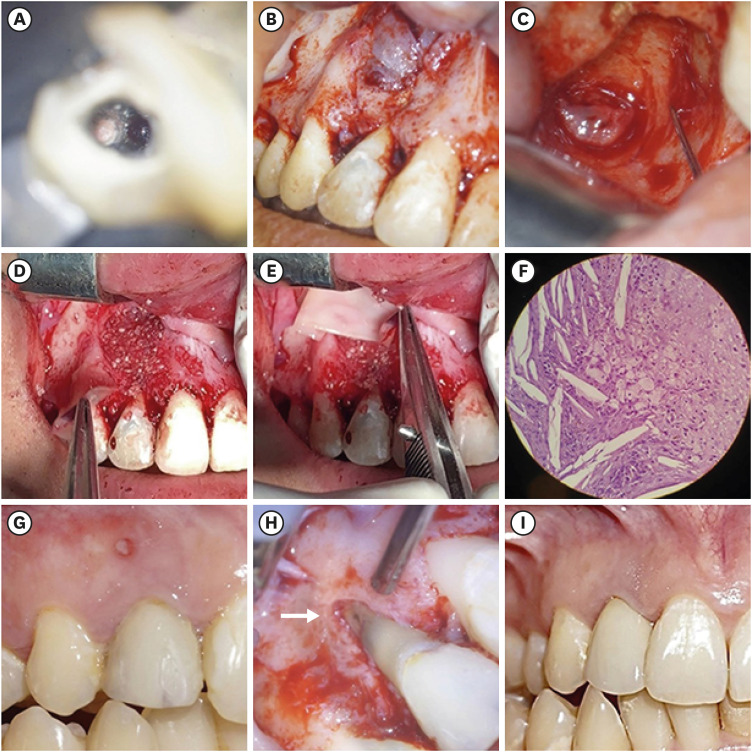
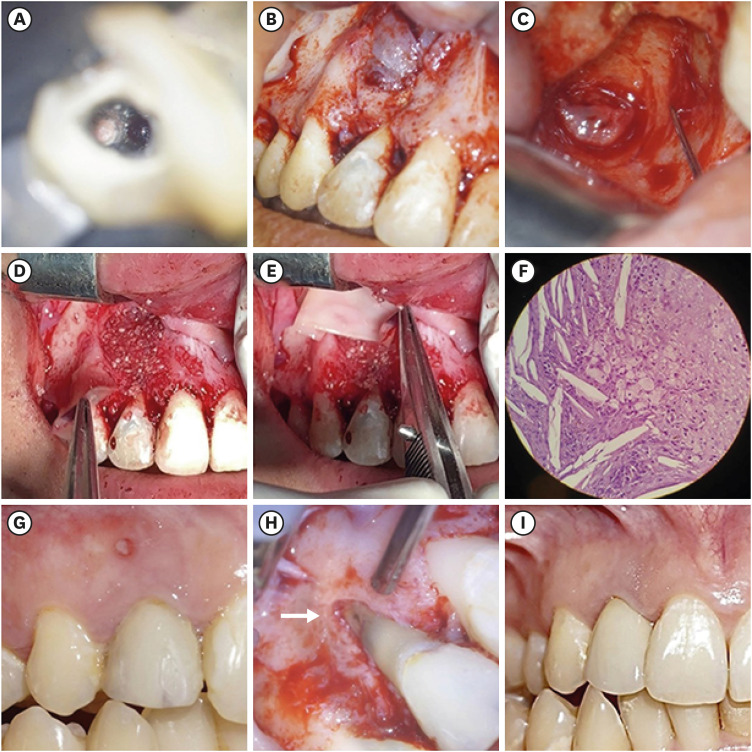
Chronological, illustrative images of the case management. A root canal perforation can be observed in the buccal root surface of the right maxillary lateral incisor, 13× OP magnification (A). The cyst involving the buccal bone plate can be observed during the surgical phase, 5× OP magnification (B). Clinical appearance after cyst removal, where it can be observed that both buccal and palatal bone plates were compromised, 13× OP magnification (C). Application of lyophilized bovine bone and autologous platelet-rich fibrin into the bone defect, 5× OP magnification (D, E). Histopathological image (original magnification ×400) of the removed tissue showing cholesterol crystals, confirming the presence of a radicular cyst (F). Intraoral photograph 1 year after first microsurgery; a sinus tract appeared and was associated with the treated tooth (G). Clinical appearance of the second perforation in the buccal root surface of the affected tooth—white arrow, 8× OP magnification (H). Intraoral photograph 2 years after micro-resurgery. The tooth was restored with a crown (I).
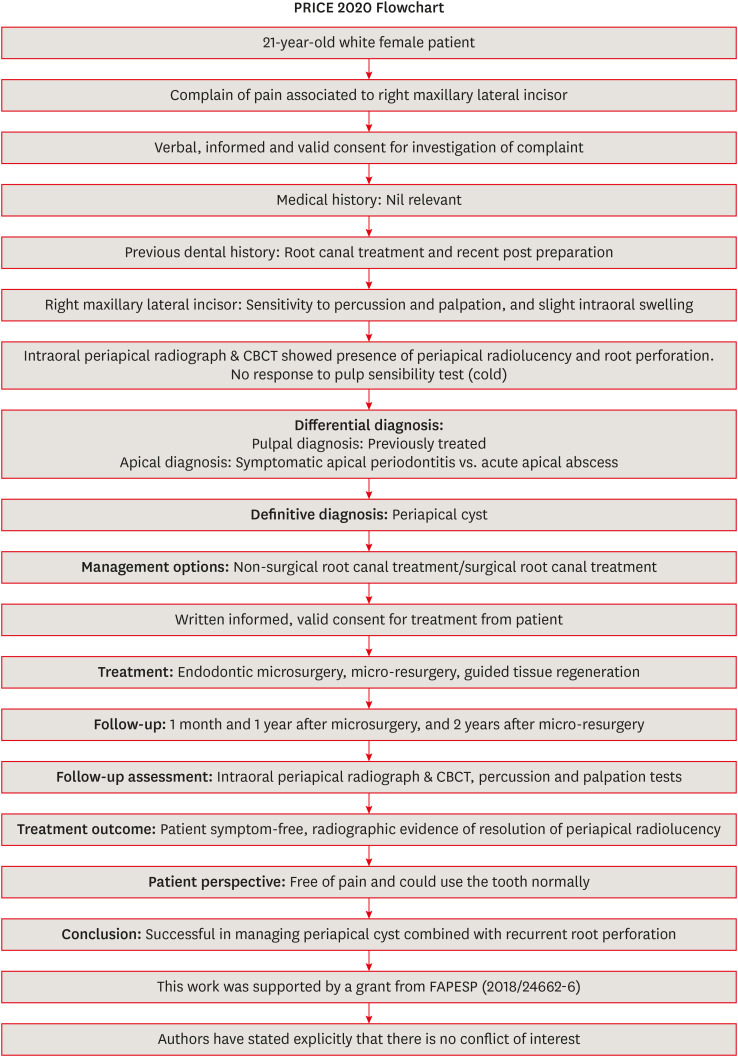
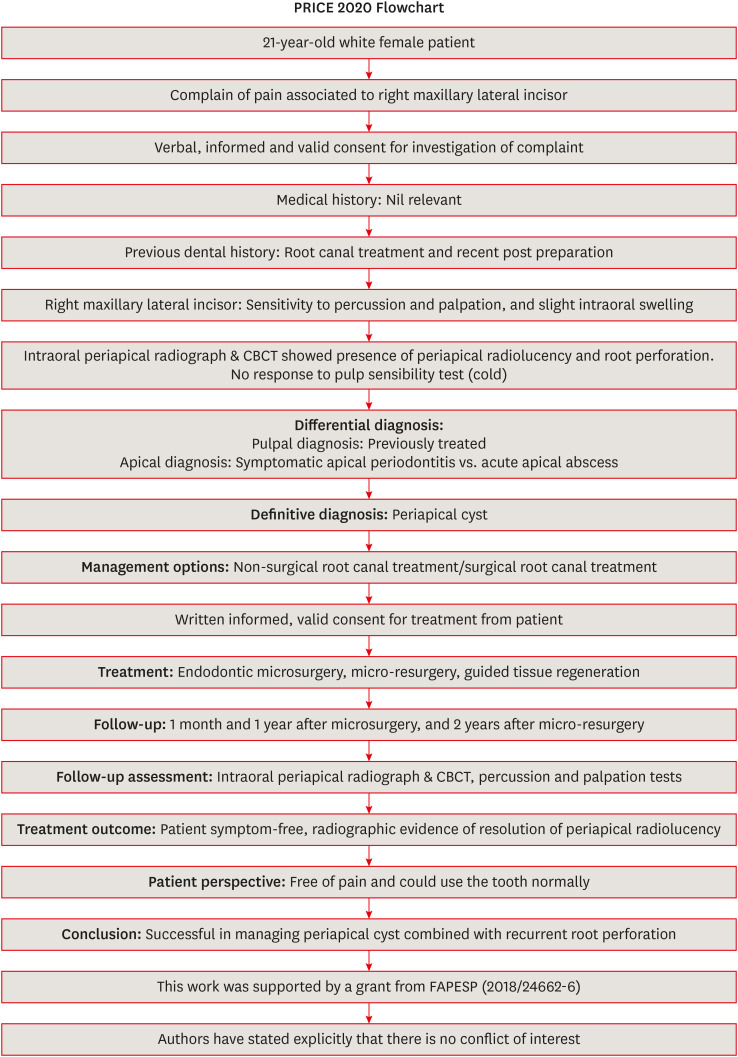
This flow chart was adopted from PRICE 2020 guidelines for reporting case reports in endodontics [16]. For further details visit: http://pride-endodonticguidelines.org/price/.
DISCUSSION
CONCLUSIONS
-
Funding: This research was supported by Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP) (grant number 18/24662-6).
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Córdova-Malca F, Coaguila-Llerena H.
Funding acquisition: Coaguila-Llerena H.
Methodology: Córdova-Malca F, Coaguila-Llerena H, Garré-Arnillas L, Rayo-Iparraguire J.
Resources: Córdova-Malca F, Garré-Arnillas L.
Supervision: Faria G.
Visualization: Córdova-Malca F, Coaguila-Llerena H, Garré-Arnillas L, Rayo-Iparraguire J, Faria G.
Writing - original draft: Córdova-Malca F, Coaguila-Llerena H, Garré-Arnillas L, Rayo-Iparraguire J, Faria G.
Writing - review & editing: Córdova-Malca F, Coaguila-Llerena H, Garré-Arnillas L, Rayo-Iparraguire J, Faria G.
- 1. Ricucci D, Siqueira JF Jr, Lopes WS, Vieira AR, Rôças IN. Extraradicular infection as the cause of persistent symptoms: a case series. J Endod 2015;41:265-273.ArticlePubMed
- 2. Nair PN. New perspectives on radicular cysts: Do they heal? Int Endod J 1998;31:155-160.ArticlePubMed
- 3. Floratos S, Kim S. Modern endodontic microsurgery concepts: a clinical update. Dent Clin North Am 2017;61:81-91.PubMed
- 4. Niemczyk SP. Essentials of endodontic microsurgery. Dent Clin North Am 2010;54:375-399.ArticlePubMed
- 5. Setzer FC, Kohli MR, Shah SB, Karabucak B, Kim S. Outcome of endodontic surgery: a meta-analysis of the literature--Part 2: comparison of endodontic microsurgical techniques with and without the use of higher magnification. J Endod 2012;38:1-10.ArticlePubMed
- 6. Kim D, Kim S, Song M, Kang DR, Kohli MR, Kim E. Outcome of endodontic micro-resurgery: retrospective study based on propensity score–matched survival analysis. J Endod 2018;44:1632-1640.PubMed
- 7. Song M, Shin SJ, Kim E. Outcomes of endodontic micro-resurgery: a prospective clinical study. J Endod 2011;37:316-320.ArticlePubMed
- 8. Yoshikawa G, Murashima Y, Wadachi R, Sawada N, Suda H. Guided bone regeneration (GBR) using membranes and calcium sulphate after apicectomy: a comparative histomorphometrical study. Int Endod J 2002;35:255-263.ArticlePubMed
- 9. Lin L, Chen MY, Ricucci D, Rosenberg PA. Guided tissue regeneration in periapical surgery. J Endod 2010;36:618-625.ArticlePubMed
- 10. Rankow HJ, Krasner PR. Endodontic applications of guided tissue regeneration in endodontic surgery. Oral Health 1996;86:33-35.Article
- 11. Tsesis I, Fuss Z. Diagnosis and treatment of accidental root perforations. Endod Topics 2006;13:95-107.Article
- 12. Estrela C, Decurcio DA, Rossi-Fedele G, Silva JA, Guedes OA, Borges ÁH. Root perforations: a review of diagnosis, prognosis and materials. Braz Oral Res 2018;32:e73.ArticlePubMed
- 13. Nakata TT, Bae KS, Baumgartner JC. Perforation repair comparing mineral trioxide aggregate and amalgam using an anaerobic bacterial leakage model. J Endod 1998;24:184-186.ArticlePubMed
- 14. Fuss Z, Trope M. Root perforations: classification and treatment choices based on prognostic factors. Endod Dent Traumatol 1996;12:255-264.ArticlePubMed
- 15. Silberman JJ, Moldauer BI, Torres J, Gallardo C, Sanabria-Liviac D. Palatal root surgery of a maxillary molar using a piezosurgery transantral approach with simultaneous sinus lift grafting: a case report. Int Endod J 2021;54:464-475.ArticlePubMedPDF
- 16. Nagendrababu V, Chong BS, McCabe P, Shah PK, Priya E, Jayaraman J, Pulikkotil SJ, Setzer FC, Sunde PT, Dummer PM. PRICE 2020 guidelines for reporting case reports in endodontics: a consensus-based development. Int Endod J 2020;53:619-626.ArticlePubMedPDF
- 17. Pallarés-Serrano A, Glera-Suarez P, Tarazona-Alvarez B, Peñarrocha-Diago M, Peñarrocha-Diago M, Peñarrocha-Oltra D. Prognostic factors after endodontic microsurgery: a retrospective study of 111 cases with 5 to 9 years of follow-up. J Endod 2021;47:397-403.ArticlePubMed
- 18. Çalışkan MK, Kaval ME, Tekin U, Ünal T. Radiographic and histological evaluation of persistent periapical lesions associated with endodontic failures after apical microsurgery. Int Endod J 2016;49:1011-1019.ArticlePubMed
- 19. Trasatti C, Spears R, Gutmann JL, Opperman LA. Increased Tgf-β1 production by rat osteoblasts in the presence of PepGen P-15 in vitro . J Endod 2004;30:213-217.PubMed
- 20. Bashutski JD, Wang HL. Periodontal and endodontic regeneration. J Endod 2009;35:321-328.ArticlePubMed
- 21. Taschieri S, Del Fabbro M, Testori T, Saita M, Weinstein R. Efficacy of guided tissue regeneration in the management of through-and-through lesions following surgical endodontics: a preliminary study. Int J Periodontics Restorative Dent 2008;28:265-271.PubMed
- 22. Taschieri S, Del Fabbro M, Testori T, Weinstein R. Efficacy of xenogeneic bone grafting with guided tissue regeneration in the management of bone defects after surgical endodontics. J Oral Maxillofac Surg 2007;65:1121-1127.ArticlePubMed
- 23. Dietrich T, Zunker P, Dietrich D, Bernimoulin JP. Periapical and periodontal healing after osseous grafting and guided tissue regeneration treatment of apicomarginal defects in periradicular surgery: results after 12 months. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003;95:474-482.ArticlePubMed
- 24. Dhiman M, Kumar S, Duhan J, Sangwan P, Tewari S. Effect of platelet-rich fibrin on healing of apicomarginal defects: a randomized controlled trial. J Endod 2015;41:985-991.ArticlePubMed
- 25. Karan NB, Aricioğlu B. Assessment of bone healing after mineral trioxide aggregate and platelet-rich fibrin application in periapical lesions using cone-beam computed tomographic imaging. Clin Oral Investig 2020;24:1065-1072.ArticlePubMedPDF
- 26. Christensen CE, McNeal SF, Eleazer P. Effect of lowering the pH of sodium hypochlorite on dissolving tissue in vitro . J Endod 2008;34:449-452.PubMed
- 27. Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Gogly B. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part III: leucocyte activation: a new feature for platelet concentrates? Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;101:e51-e55.ArticlePubMed
- 28. Soto-Peñaloza D, Peñarrocha-Diago M, Cervera-Ballester J, Peñarrocha-Diago M, Tarazona-Alvarez B, Peñarrocha-Oltra D. Pain and quality of life after endodontic surgery with or without advanced platelet-rich fibrin membrane application: a randomized clinical trial. Clin Oral Investig 2020;24:1727-1738.ArticlePubMedPDF
- 29. Makhlouf M, Zogheib C, Makhlouf AC, Kaloustian MK, El Hachem C, Habib M. Sealing ability of calcium silicate-based materials in the repair of furcal perforations: a laboratory comparative study. J Contemp Dent Pract 2020;21:1091-1097.ArticlePubMed
- 30. da Fonseca TS, Silva GF, Guerreiro-Tanomaru JM, Delfino MM, Sasso-Cerri E, Tanomaru-Filho M, Cerri PS. Biodentine and MTA modulate immunoinflammatory response favoring bone formation in sealing of furcation perforations in rat molars. Clin Oral Investig 2019;23:1237-1252.ArticlePubMedPDF
- 31. Coaguila-Llerena H, Ochoa-Rodriguez VM, Castro-Núñez GM, Faria G, Guerreiro-Tanomaru JM, Tanomaru-Filho M. Physicochemical properties of a bioceramic repair material - BioMTA. Braz Dent J 2020;31:511-515.ArticlePubMed
REFERENCES
Tables & Figures
REFERENCES
Citations

- Outcome of endodontic micro-resurgery: A systematic review
Faisal Alnassar, Riyadh Alroomy, Qamar Hashem, Abdullah Alqedairi, Nabeel Almotairy
Saudi Endodontic Journal.2025; 15(2): 112. CrossRef - Platelet-Rich Plasma and Platelet-Rich Fibrin in Endodontics: A Scoping Review
Simão Rebimbas Guerreiro, Carlos Miguel Marto, Anabela Paula, Joana Rita de Azevedo Pereira, Eunice Carrilho, Manuel Marques-Ferreira, Siri Vicente Paulo
International Journal of Molecular Sciences.2025; 26(12): 5479. CrossRef - Non-surgical Approach to a Maxillary Cyst-Like Lesion: Orthograde Endodontic Treatment With Neodymium-Doped Yttrium Aluminum Garnet (Nd:YAG) Decontamination of the Canal System
Beatrice Spaggiari, Paolo Vescovi, Silvia Pizzi, Roberta Iaria, Ilaria Giovannacci
Cureus.2025;[Epub] CrossRef - Persistent Periradicular Lesion Associated With Concurrent Root Fracture and Odontogenic Keratocyst: A Case Report
Mehdi Vatanpour, Fatemeh Rezaei
Clinical Case Reports.2025;[Epub] CrossRef - Management of Apico-marginal Defects With Endodontic Microsurgery and Guided Tissue Regeneration: A Report of Thirteen Cases
Abayomi O. Baruwa, Jorge N.R. Martins, Mariana D. Pires, Beatriz Pereira, Pedro May Cruz, António Ginjeira
Journal of Endodontics.2023; 49(9): 1207. CrossRef

 KACD
KACD
 ePub Link
ePub Link Cite
Cite

