Search
- Page Path
- HOME > Search
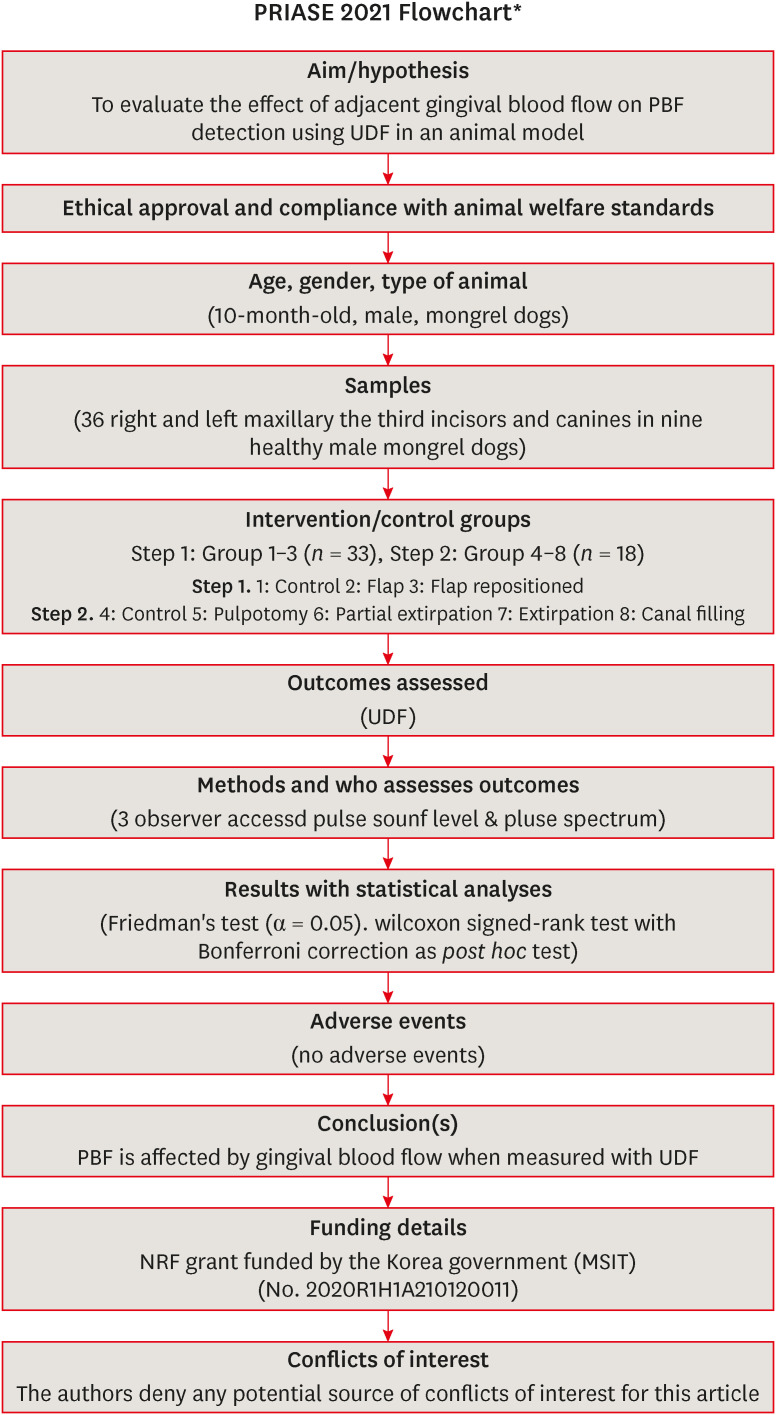
- The effects of gingival blood flow on pulpal blood flow detection using ultrasound Doppler flowmetry: animal study
- Dohyun Kim, Hyoung-Seok Ko, Soo-Yeon Park, Seung-Yeon Ryu, Sung-ho Park
- Restor Dent Endod 2023;48(1):e9. Published online January 30, 2023
- DOI: https://doi.org/10.5395/rde.2023.48.e9
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives This study evaluated the effect of adjacent gingival blood flow on detection of pulpal blood flow (PBF) using ultrasound Doppler flowmetry (UDF) through animal study.
Materials and Methods The study included 36 right and left maxillary the third incisors and canines in 9 experimental dogs. The study included 2 main steps: In the first step, the pulse sound level (PSL) was recorded on the cervical part of each tooth without flap elevation (Group 1), with flap elevation (Group 2), and after it was repositioned in place (Group 3). In the second step, the PSL was recorded on the cervical part of each tooth (Group 4), after pulpotomy (Group 5), after partial pulp extirpation (Group 6), after complete extirpation (Group 7), and after canal filling (Group 8). In Groups 5–8, the study was performed with and without flap elevation in the left and right teeth, respectively. The PSL was graded as follows: 0, inaudible; 1, heard faintly; and 2, heard well. The difference between each group was analyzed using Friedman’s test with Wilcoxon signed-rank tests (α = 0.05).
Results In step 1, the PSL results were Group 1 > 2 and 3. In step 2, there was no significant difference between the groups when the flap was not elevated, while PSL results were Group 4 > 5 ≥ 6 and 7 ≥ 8 when the flap was elevated.
Conclusions PBF is affected by gingival blood flow when measured with UDF. UDF measurements require isolation of gingiva from the tooth.
-
Citations
Citations to this article as recorded by- Modern aspects of the use of hardware methods for diagnosing pulp vitality (Part 2. Non-traditional diagnostic methods)
K. V. Shadrina, L. Yu. Orekhova, V. D. Goncharov, V. Yu. Vashneva, E. S. Silina, E. V. Kosova, A. A. Petrov
Endodontics Today.2025; 23(3): 423. CrossRef - Exploring approaches to pulp vitality assessment: A scoping review of nontraditional methods
Farzaneh Afkhami, Patricia Paule Wright, Philip Yuan‐Ho Chien, Chun Xu, Laurence James Walsh, Ove Andreas Peters
International Endodontic Journal.2024; 57(8): 1065. CrossRef
- Modern aspects of the use of hardware methods for diagnosing pulp vitality (Part 2. Non-traditional diagnostic methods)
- 2,223 View
- 39 Download
- 1 Web of Science
- 2 Crossref

- Involvement of TRPA1 in the cinnamaldehyde-induced pulpal blood flow change in the feline dental pulp
- Dokyung Kim, Moon-Hwan Lee, Sung Kyo Kim
- Restor Dent Endod 2016;41(3):202-209. Published online July 29, 2016
- DOI: https://doi.org/10.5395/rde.2016.41.3.202
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives The purpose of this study was to investigate the involvement of TRPA1 in the cinnamaldehyde-induced pulpal blood flow (PBF) change in the feline dental pulp.
Materials and Methods Mandibles of eight cats were immobilized and PBF was monitored with a laser Doppler flowmetry at the mandibular canine tooth. To evaluate the effect of cinnamaldehyde on PBF, cinnamaldehyde was injected into the pulp through the lingual artery at a constant rate for 60 seconds. As a control, a mixture of 70% ethanol and 30% dimethyl sulfoxide (DMSO, vehicle) was used. To evaluate the involvement of transient receptor potential ankyrin 1 (TRPA1) in PBF change, AP18, a specific TRPA1 antagonist, was applied into the pulp through the Class V dentinal cavity followed by cinnamaldehyde-administration 3 minutes later. The paired variables of experimental data were statistically analyzed using paired
t -test. Ap value of less than 0.05 was considered as statistically significant.Results Administration of cinnamaldehyde (0.5 mg/kg, intra-arterial [i.a.]) induced significant increases in PBF (
p < 0.05). While administration of a TRPA1 antagonist, AP18 (2.5 - 3.0 mM, into the dentinal cavity [i.c.]) caused insignificant change of PBF (p > 0.05), administration of cinnamaldehyde (0.5 mg/kg, i.a.) following the application of AP18 (2.5 - 3.0 mM, i.c.) resulted in an attenuation of PBF increase from the control level (p < 0.05). As a result, a TRPA1 antagonist, AP18 effectively inhibited the vasodilative effect of cinnamaldehyde (p < 0.05).Conclusions The result of the present study provided a functional evidence that TRPA1 is involved in the mechanism of cinnamaldehyde-induced vasodilation in the feline dental pulp.
-
Citations
Citations to this article as recorded by- A simple model for the assessment of the agonistic activity of dibenzazepine derivatives by molecular moieties
Mohammad Hossein Keshavarz, Hossein Fakhraian, Norollah Saedi
Medicinal Chemistry Research.2021; 30(1): 215. CrossRef
- A simple model for the assessment of the agonistic activity of dibenzazepine derivatives by molecular moieties
- 2,068 View
- 4 Download
- 1 Crossref

- Effect of local anesthesia on pulpal blood flow in mechanically stimulated teeth
- Wan-Sik Chu, Seung-Ho Park, Dong-Kuk Ahn, Sung Kyo Kim
- J Korean Acad Conserv Dent 2006;31(4):257-262. Published online January 14, 2006
- DOI: https://doi.org/10.5395/JKACD.2006.31.4.257
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Abstract The aims of the study were to evaluate the effect of epinephrine-containing local anesthetics on pulpal blood flow (PBF) and to investigate its effect on cavity preparation-induced PBF change. PBF was recorded using a laser Doppler flowmeter (Perimed Co., Sweden) from canines of nine cats under general anesthesia before and after injection of local anesthetics and after cavity preparation. 2% lidocaine hydrochloride with 1 : 100,000 epinephrine was administered by local infiltration given apical to the mandibular canine at the vestibular area and the same volume of isotonic saline was injected on the contralateral tooth as a control. A round carbide bur was operated at slow speed with isotonic saline flushing to grind spherical cavities with increasing depth through the enamel and into the dentin on both teeth. The obtained data was analyzed with paired
t -test.Cavity preparation caused significant increase of PBF (
n = 9,p < 0.05). Local infiltration of lidocaine with epinephrine resulted in decreases of PBF (n = 9,p < 0.05), whereas there was no significant change of PBF with the physiologic saline as a control. Cavity preparation on tooth anesthetized with lidocaine with epinephrine caused significantly less increase of PBF than in control tooth (p < 0.05).Therefore, the result of the present study demonstrates that local infiltration of 2% lidocaine with 1 : 100,000 epinephrine effectively reduces PBF increase caused by cavity preparation.
-
Citations
Citations to this article as recorded by- Effect of laser-induced pulpal anesthesia of single-rooted teeth with irreversible pulpitis treated by single-visit root canal therapy - A randomized clinical trial
Geeta Asthana, Dhwani Morakhia, Ravina Parmar, Rajashree Tamuli
Endodontology.2025; 37(3): 244. CrossRef - Systematic Injection Patterned-Technique of One-Per-Mil Tumescent Solution for Perforator-Based Skin Flap: Is it Better Than the Random Patterned-Technique?
Theddeus O. H. Prasetyono, Sweety Pribadi
International Surgery.2015; 100(9-10): 1308. CrossRef - Biologic response of local hemostatic agents used in endodontic microsurgery
Youngjune Jang, Hyeon Kim, Byoung-Duck Roh, Euiseong Kim
Restorative Dentistry & Endodontics.2014; 39(2): 79. CrossRef - Change in Pulpal Blood Flow of Heat-induced Neurogenic Inflammation in Feline Dental Plup
Min-Kyoung Park
Journal of the Korea Academia-Industrial cooperation Society.2013; 14(12): 6340. CrossRef - Cardiovascular effect of epinephrine in endodontic microsurgery: a review
Youngjune Jang, Euiseong Kim
Restorative Dentistry & Endodontics.2013; 38(4): 187. CrossRef
- Effect of laser-induced pulpal anesthesia of single-rooted teeth with irreversible pulpitis treated by single-visit root canal therapy - A randomized clinical trial
- 1,729 View
- 16 Download
- 5 Crossref

- REGULATION OF PULPAL MICROCIRCULATION BY CALCITONIN GENE-RELATED PEPTIDE
- Sung-Kyo Kim, Young-Kyung Kim, Myoung-Uk Jin
- J Korean Acad Conserv Dent 2005;30(6):470-476. Published online January 14, 2005
- DOI: https://doi.org/10.5395/JKACD.2005.30.6.470
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Abstract The purpose of this study was to investigate the function of calcitonin gene-related peptide (CGRP) in regulatory mechanism of pulpal microcirculation with the aim of elucidating neurogenic inflammation.
Experiments were performed on twelve cats under general anesthesia. CGRP was administered through the femoral vein to see the systemic influence and through the external carotid artery to see the local effect. Sympathetic nerve to the dental pulp was stimulated electrically and pulpal blood flow (PBF) was measured with a laser Doppler flowmeter on the canine teeth to the drug administration. The paired variables of control and experimental data were compared by paired
t -test and differences withp < 0.05 were considered statistically significant.Systemic administration of CGRP (0.3 μg/kg) exerted decreases in systemic blood pressure and caused changes in PBF with an initial increase followed by decrease and a more marked second increase and decrease.
Close intra-arterial (i.a.) injection of CGRP (0.03 μ/kg) resulted in slight PBF increase. The effect of CGRP resulted in no significant increase in PBF in the presence of CGRP8-37.
The electrical stimulation of the sympathetic nerve alone resulted in PBF decreases. The i.a. administration of CGRP following the electrical stimulation of the sympathetic nerve compensated the decreased PBF. Therefore, CGRP effectively blocked the sympathetic nerve stimulation-induced PBF decrease.
Results of the present study have provided evidences that even though the local vasodilatory function of CGRP are weak, CGRP is effectively involved in blocking the vasoconstriction caused by sympathetic nerve stimulation in the feline dental pulp.
- 747 View
- 0 Download

- Local application of NK1 receptor antagonists and pulpal blood flow in cat
- Young-Kyung Kim, Wan-Sik Chu, Ho-Jeong Lee, Dong-Kuk Ahn, Hyun-Mi Yoo, Sung-Kyo Kim
- J Korean Acad Conserv Dent 2004;29(3):239-248. Published online May 31, 2004
- DOI: https://doi.org/10.5395/JKACD.2004.29.3.239
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub The purpose of this study was to investigate the influence of NK1 receptor antagonists on the pulpal blood flow (PBF) when applied iontophoretically through the dentinal cavity of the teeth in order to understand whether iontophoretically applied NK1 receptor antagonists can control the pulpal inflammation.
Eleven cats were anesthetized with alpha-chloralose and urethane, and substance P (SP) was administered to the dental pulp through the catheterized lingual artery in doses that caused PBF change without the influence of systemic blood pressure. NK1 receptor antagonists were applied iontophoretically to the prepared dentinal cavity of ipsilateral canine teeth of the drug administration, and PBF was monitored. Data were analyzed statistically with paired t-test.
PBF increase after iontophoretic application of the NK1 receptor antagonists followed by the intra-arterial administration of SP was significantly less than PBF increase after iontophoretic application of the 0.9% saline followed by the intra-arterial administration of SP as a control (
p < 0.05).Iontophoretic application of the NK1 receptor antagonists (0.2~3.4 mM) following the intra-arterial administration of SP resulted in less increase of PBF than the iontophoretic application of the 0.9% saline following the intra-arterial administration of SP as a control (
p < 0.05).Therefore, the results of the present study provide evidences that the iontophoretic application is an effective method to deliver drugs to the dental pulp, and that iontophoretically applied NK1 receptor antagonists block SP-induced vasodilation effectively. The above results show the possibility that the iontophoretical application of NK1 receptor antagonists can control the neurogenic inflammation in the dental pulp.
- 829 View
- 1 Download

- The influence of epinephrine concentration in local anesthetics on pulpal and gingival blood flows
- Jae-Sang Lee, Sung-Kyo Kim
- J Korean Acad Conserv Dent 2003;28(6):475-484. Published online November 30, 2003
- DOI: https://doi.org/10.5395/JKACD.2003.28.6.475
-
 PDF
PDF PubReader
PubReader ePub
ePub -
Citations
Citations to this article as recorded by- Biologic response of local hemostatic agents used in endodontic microsurgery
Youngjune Jang, Hyeon Kim, Byoung-Duck Roh, Euiseong Kim
Restorative Dentistry & Endodontics.2014; 39(2): 79. CrossRef - Cardiovascular effect of epinephrine in endodontic microsurgery: a review
Youngjune Jang, Euiseong Kim
Restorative Dentistry & Endodontics.2013; 38(4): 187. CrossRef - Effect of local anesthesia on pulpal blood flow in mechanically stimulated teeth
Wan-Sik Chu, Seung-Ho Park, Dong-Kuk Ahn, Sung Kyo Kim
Journal of Korean Academy of Conservative Dentistry.2006; 31(4): 257. CrossRef
- Biologic response of local hemostatic agents used in endodontic microsurgery
- 1,949 View
- 9 Download
- 3 Crossref


 KACD
KACD

 First
First Prev
Prev


