Search
- Page Path
- HOME > Search
- Evaluation of platelet concentrates in regenerative endodontics: a systematic review and meta-analysis
- Anna Tsiolaki, Dimitrios Theocharis, Nikolaos Tsitsipas, Anastasia Fardi, Konstantinos Kodonas
- Restor Dent Endod 2025;50(4):e38. Published online November 28, 2025
- DOI: https://doi.org/10.5395/rde.2025.50.e38
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - Objectives
The aim of this systematic review is to compare the effectiveness of advanced platelet concentrates as regenerative endodontic therapeutic alternatives to blood clot (BC) revascularization in immature permanent necrotic teeth.
Methods
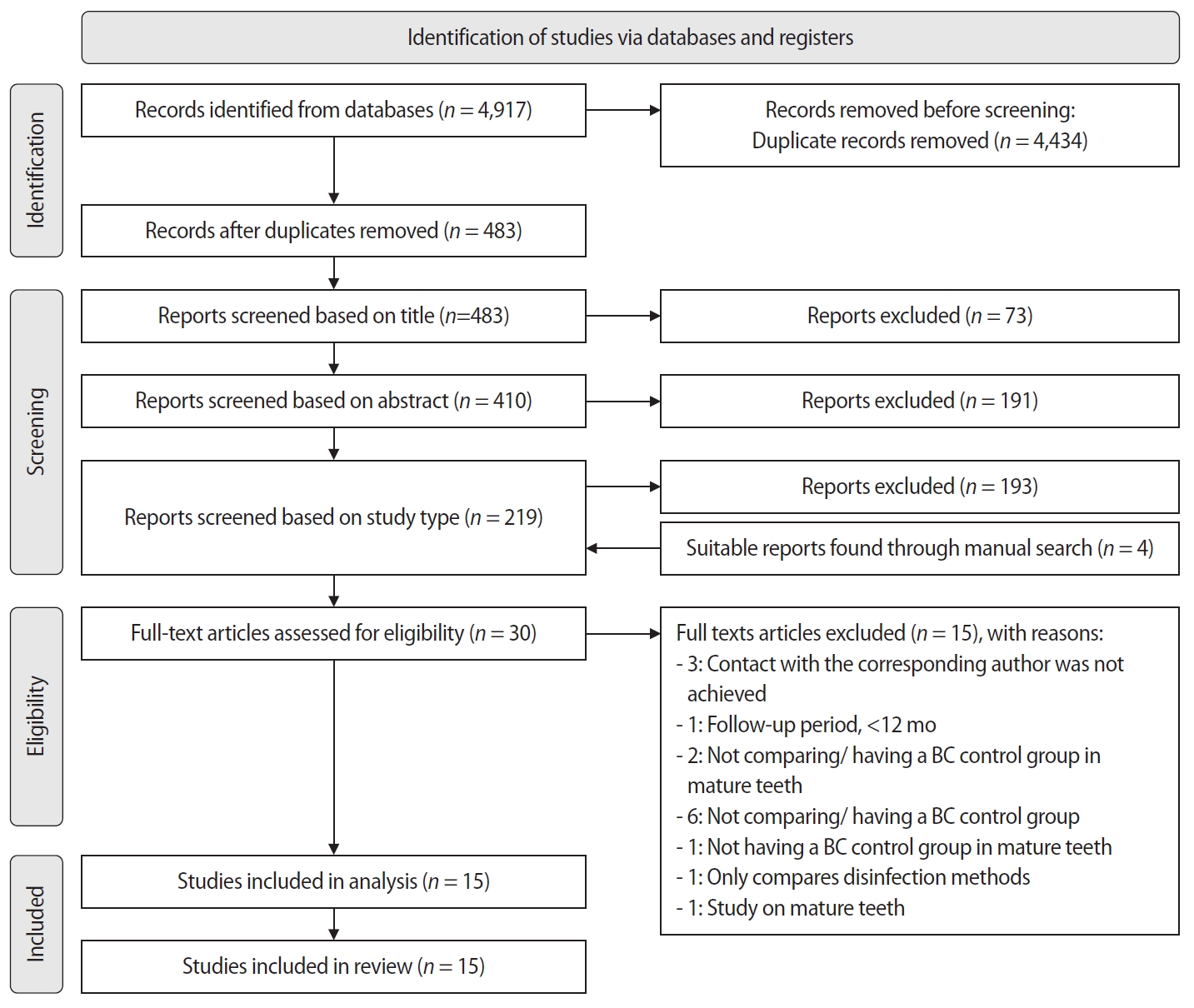
Randomized controlled trials (RCTs) comparing regenerative endodontic therapies using platelet-rich plasma (PRP), platelet-rich fibrin (PRF), or platelet pellet (PP) with the BC revascularization approach in immature permanent necrotic teeth were systematically searched in PubMed, Scopus, Cochrane Library, and Web of Science until May 2025. Data was extracted and analyzed both qualitatively and quantitatively. Study quality was assessed using the Cochrane Risk of Bias tool. A meta-analysis was conducted using IBM SPSS software (version 29.0), with success rates expressed as risk ratios and 95% confidence intervals (CIs).
Results
The initial search yielded 4,917 studies. After removing duplicates and applying eligibility criteria, 15 RCTs were included. Meta-analysis indicated no significant difference in the risk ratio (RR), as the BC method has similar success rates with PRP (10 studies; RR = 1.01; 95% CI, 0.94–1.09; p = 0.76) and PRF (8 studies; RR = 0.98; 95% CI, 0.89–1.08; p = 0.65) at 12 months. The primary outcomes evaluated were based on clinical and radiographic success.
Conclusions
Current evidence suggests PRP, PRF, and BC are all effective in treating immature permanent necrotic teeth with similar success rates. However, further research is needed to assess long-term outcomes.
- 1,413 View
- 85 Download

- Push-out bond strength and marginal adaptation of apical plugs with bioactive endodontic cements in simulated immature teeth
- Maria Aparecida Barbosa de Sá, Eduardo Nunes, Alberto Nogueira da Gama Antunes, Manoel Brito Júnior, Martinho Campolina Rebello Horta, Rodrigo Rodrigues Amaral, Stephen Cohen, Frank Ferreira Silveira
- Restor Dent Endod 2021;46(4):e53. Published online October 20, 2021
- DOI: https://doi.org/10.5395/rde.2021.46.e53
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
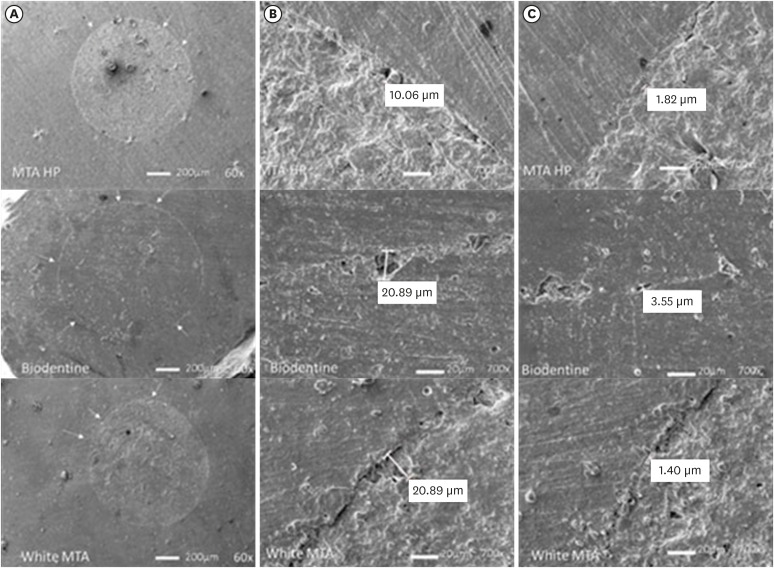
ePub Objectives This study evaluates the bond strength and marginal adaptation of mineral trioxide aggregate (MTA) Repair HP and Biodentine used as apical plugs; MTA was used as reference material for comparison.
Materials and Methods A total of 30 single-rooted teeth with standardized, artificially created open apices were randomly divided into 3 groups (
n = 10 per group), according to the material used to form 6-mm-thick apical plugs: group 1 (MTA Repair HP); group 2 (Biodentine); and group 3 (white MTA). Subsequently, the specimens were transversely sectioned to obtain 2 (cervical and apical) 2.5-mm-thick slices per root. Epoxy resin replicas were observed under a scanning electron microscope to measure the gap size at the material/dentin interface (the largest and smaller gaps were recorded for each replica). The bond strength of the investigated materials to dentin was determined using the push-out test. The variable bond strengths and gap sizes were evaluated independently at the apical and cervical root dentin slices. Data were analyzed using descriptive and analytic statistics.Results The comparison between the groups regarding the variables' bond strengths and gap sizes showed no statistical difference (
p > 0.05) except for a single difference in the smallest gap at the cervical root dentin slice, which was higher in group 3 than in group 1 (p < 0.05).Conclusions The bond strength and marginal adaptation to root canal walls of MTA HP and Biodentine cement were comparable to white MTA.
-
Citations
Citations to this article as recorded by- Evaluation of marginal adaptation and bond strength of apical root canal plugs using different bioceramic cements
Michel Sena Fernandes Faria Lima, Alberto Nogueira da Gama Antunes, Kênia Maria Pereira Soares de Toubes, Fábio Fernandes Borém Bruzinga, Camila de Sousa Caneschi, Luís Fernando dos Santos Alves Morgan, Frank Ferreira Silveira
BMC Oral Health.2026;[Epub] CrossRef - Application of Biodentine for Apexification of Immature Teeth of Children: A Scoping Review
Liz M Gerard, Sumit Gaur
International Journal of Clinical Pediatric Dentistry.2025; 18(5): 573. CrossRef - Evaluation of the root dentin bond strength and intratubular biomineralization of a premixed calcium aluminate-based hydraulic bioceramic endodontic sealer
Yu-Na Lee, Min-Kyeong Kim, Hee-Jin Kim, Mi-Kyung Yu, Kwang-Won Lee, Kyung-San Min
Journal of Oral Science.2024; 66(2): 96. CrossRef - Managing Cracked Teeth with Root Extension: A Prospective Preliminary Study Using Biodentine™ Material
Kênia Maria Soares de Toubes, Isabella Sousa Corrêa, Regina Célia Lopes Valadares, Stephanie Quadros Tonelli, Fábio Fernandes Borém Bruzinga, Frank Ferreira Silveira, Dr Karthikeyan Ramalingam
International Journal of Dentistry.2024;[Epub] CrossRef - Marginal adaptation of customized gutta percha cone with calcium silicate based sealer versus MTA and biodentine apical plugs in simulated immature permanent teeth (an in vitro study)
Mary M. Mina, Sybel M. Moussa, Mahmoud R. Aboelseoud
BMC Oral Health.2024;[Epub] CrossRef - Comparative Evaluation of Push-Out Bond Strength of Conventional Mineral Trioxide Aggregate, Biodentine, a Modified Mineral Trioxide Aggregate, and Two Novel Antibacterial-Enhanced Mineral Trioxide Aggregates
Arokia Rajkumar Shancy Merlin, Vignesh Ravindran, Ganesh Jeevanandan, Rajalakshmanan Eswaramoorthy, Abirami Arthanari
Cureus.2024;[Epub] CrossRef - Push out bond strength of hydraulic cements used at different thicknesses
C. Ruiz Durán, Dra L. Gancedo-Caravia, V. Vera González, C. González Losada
BMC Oral Health.2023;[Epub] CrossRef - Effects of different calcium-silicate based materials on fracture resistance of immature permanent teeth with replacement root resorption and osteoclastogenesis
Gabriela Leite de Souza, Gabrielle Alves Nunes Freitas, Maria Tereza Hordones Ribeiro, Nelly Xiomara Alvarado Lemus, Carlos José Soares, Camilla Christian Gomes Moura
Restorative Dentistry & Endodontics.2023;[Epub] CrossRef
- Evaluation of marginal adaptation and bond strength of apical root canal plugs using different bioceramic cements
- 2,526 View
- 31 Download
- 9 Web of Science
- 8 Crossref

- Observation of an extracted premolar 2.5 years after mineral trioxide aggregate apexification using micro-computed tomography
- Gayeon Lee, Chooryung Chung, Sunil Kim, Su-Jung Shin
- Restor Dent Endod 2020;45(2):e4. Published online November 22, 2019
- DOI: https://doi.org/10.5395/rde.2020.45.e4
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
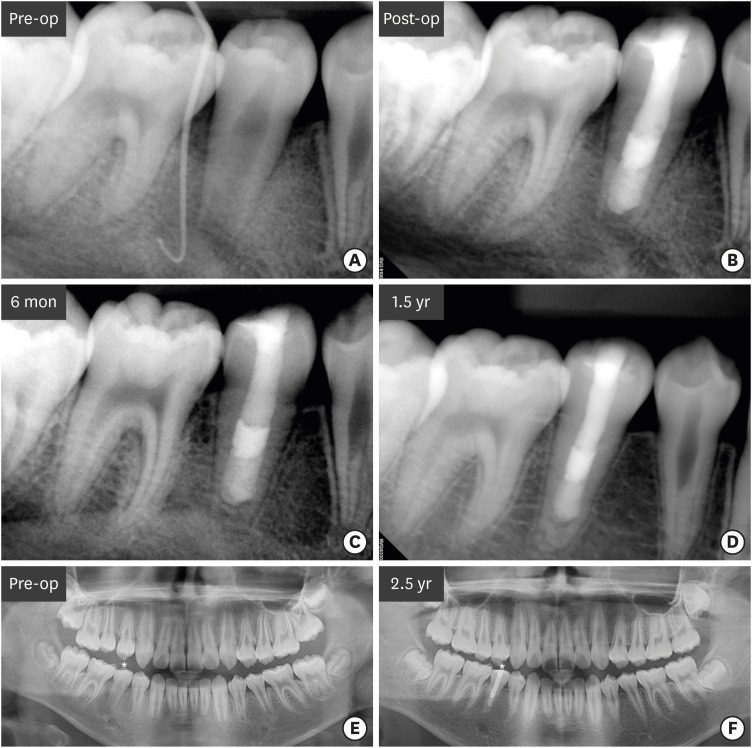
ePub Although numerous studies have been conducted on apexification using mineral trioxide aggregate (MTA), direct observation of extracted human teeth after the procedure has been rarely reported. This case report describes a mandibular premolar treated 2.5 years ago and extracted recently for orthodontic treatment. The tubercle of the right mandibular premolar of a 12-year-old boy with dens evaginatus was fractured and the pulp was exposed. The tooth was diagnosed with pulp necrosis and asymptomatic periapical abscess. During the first visit, copious irrigation was performed with 2.5% sodium hypochlorite. Calcium hydroxide paste was placed as an intracanal medicament. The sinus tract had disappeared at the second visit after 3 weeks. MTA was applied on to the bleeding point as a 4-mm-thick layer, followed by a 3-mm-thick gutta-percha filling and resin core build-up. After 2.5 years, the tooth and three other premolars were extracted for orthodontic treatment. The right and left mandibular premolars were scanned with micro-computed tomography to determine the root shape and canal anatomy. Irregular root growth was observed and the root outline of the right mandibular premolar differed from that of the contralateral tooth. Apexification with MTA leads to the formation of roots with irregular morphology, without any pulpal space.
-
Citations
Citations to this article as recorded by- Incorporation of amoxicillin-loaded microspheres in mineral trioxide aggregate cement: an in vitro study
Fábio Rocha Bohns, Vicente Castelo Branco Leitune, Isadora Martini Garcia, Bruna Genari, Nélio Bairros Dornelles, Silvia Stanisçuaski Guterres, Fabrício Aulo Ogliari, Mary Anne Sampaio de Melo, Fabrício Mezzomo Collares
Restorative Dentistry & Endodontics.2020;[Epub] CrossRef
- Incorporation of amoxicillin-loaded microspheres in mineral trioxide aggregate cement: an in vitro study
- 1,324 View
- 11 Download
- 1 Crossref

- Triple antibiotic paste: momentous roles and applications in endodontics: a review
- Ardavan Parhizkar, Hanieh Nojehdehian, Saeed Asgary
- Restor Dent Endod 2018;43(3):e28. Published online June 20, 2018
- DOI: https://doi.org/10.5395/rde.2018.43.e28
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub This study investigated the latest findings and notions regarding ‘triple antibiotic paste’ (TAP) and its applications in dentistry, particularly endodontics. TAP is a combination of 3 antibiotics, ciprofloxacin, metronidazole, and minocycline. Despite the problems and pitfalls research pertaining to this paste has unveiled, it has been vastly used in endodontic treatments. The paste's applications vary, from vital pulp therapy to the recently introduced regeneration and revascularisation protocol. Studies have shown that the paste can eliminate the root canal microorganisms and prepare an appropriate matrix for further treatments. This combination is able to remove diverse groups of obligate and facultative gram-positive and gram-negative bacteria, providing an environment for healing. In regeneration protocol cases, this allows the development, disinfection, and possible sterilization of the root canal system, so that new tissue can infiltrate and grow into the radicular area. Moreover, TAP is capable of creating a discipline in which other wanted and needed treatments can be successfully performed. In conclusion, TAP, as an antibacterial intracanal medication, has diverse uses. Nevertheless, despite its positive effects, the paste has shown drawbacks. Further research concerning the combined paste and other intracanal medications to control microbiota is a must.
-
Citations
Citations to this article as recorded by- Endodontic Intracanal Medicaments and Agents
Anu Priya Guruswamy Pandian, Depti Bellani, Ritya Mary Jibu, Varsha Agnihotri
Dental Clinics of North America.2026; 70(1): 45. CrossRef - Regenerative Endodontic Treatment in Permanent Incisors: Two Case Reports with 6 Years of Follow-Up
María Biedma-Perea, Marcela Arenas-González, María José Barra-Soto, Carolina Caleza-Jiménez, David Ribas-Pérez
Children.2026; 13(2): 246. CrossRef - Evaluation of antimicrobial efficacy of an herbal preparation vs triple antibiotic paste against E. faecalis: an in vitro study
Chandni Dhyani, Kalpna Chaudhry, Nitin Khanduri, Leina R. Pradhan, Yoshita Gupta
International Journal of Contemporary Pediatrics.2026; 13(3): 449. CrossRef - Evaluation of Effect of Laser in Root Canal Disinfection in Pulp Regenerative Therapy: A Systematic Review
Kiran Kumar N, Abhishek M, Savitha B. Naik, Biji Brigit, Swetha Geervani V, M Manimozhi
Photobiomodulation, Photomedicine, and Laser Surgery.2025; 43(2): 53. CrossRef - Assessing Cell Viability: Comparative Analysis of Calcium Hydroxide, Triple Antibiotic Paste, and Their Synergistic Impact on human Dental Pulp Stem Cells
Dini Asrianti Bagio, Ibramanto Warganegara, Ike Dwi Maharti, Anggraini Margono, Citra Kusumasari, Sylva Dinie Alinda, Valeria Widita Wairooy
European Journal of General Dentistry.2025; 14(01): 073. CrossRef - Cytotoxic and Antibiofilm Properties of Antibiotic-Loaded Thermoresponsive Hydrogels for Root Canal Therapy
Cristiane Duque, Gabriela Pacheco de Almeida Braga, Juliana Machado de Carvalho, Karina Sampaio Caiaffa, Gabriel Pereira Nunes, Rafaela Laruzo Rabelo, Vanessa Rodrigues dos Santos, Geórgia Rondó Peres, Lucas da Silva Ribeiro, Emerson Rodrigues de Camargo
Processes.2025; 13(3): 661. CrossRef - Antibiofilm properties, cytotoxicity, and effect on protease activity of antibiotics and EGCG-based medications for endodontic purposes
Daniela Alvim Chrisostomo, Jesse Augusto Pereira, Polliana Mendes Candia Scaffa, Zach Gouveia, Gabriel Flores Abuna, Sergey V. Plotnikov, Anuradha Prakki, Cristiane Duque
Journal of Dentistry.2025; 156: 105660. CrossRef - The use of three-dimensional-printed guides, static navigation, and bioactive materials to treat bilateral and double dens invaginatus
Parth Patel, Nidhi Bharti, Ankit Arora, C. Nimisha Shah
Saudi Endodontic Journal.2025; 15(2): 207. CrossRef - To Assess the Cell Viability of Triple Antibiotic Paste under Confocal Microscope: An In Vitro Study
Elanthendral Saravanan, Mahesh Ramakrishnan
Journal of South Asian Association of Pediatric Dentistry.2025; 8(2): 81. CrossRef - Eficacia de la pasta triantibiótica en endodoncia: actividad antibacteriana frente a cepas resistentes de Enterococcus faecalis. Una revisión exhaustiva
Elena Patricia Cevallos Fernández, Katherine de los Ángeles Cuenca León
Anatomía Digital.2025; 8(3.1): 88. CrossRef - Efectividad de diferentes antimicóticos, junto con la pasta triantibiotica, para el tratamiento de Candida albicans en conductos radiculares
Carlos Andrés Rodríguez Tapia, Jessica María Sarmiento Ordoñez
Anatomía Digital.2025; 8(3.2): 45. CrossRef - Comparative Evaluation of Calcium Hydroxide, Triple Antibiotic Paste, and Calcium Hydroxide with 2% Chlorhexidine as Intracanal Medicaments in Reducing Interappointment Pain during Endodontic Treatment: An In Vivo Study
Rachit Mathur, Shaista Gazal, Itika Jain, Shyam Agrawal, Akshada Mungee, Babra Khan
International Journal of Clinical Pediatric Dentistry.2025; 18(6): 628. CrossRef - In Vitro Effectiveness of Endodontic Triple Antibiotic Paste Associated With Daptomycin
Sabrina S Azevedo, Gabriela C Chianca, Bruna A Thurler, Raiane C Chamon, Helvécio C Corrêa Póvoa, Leonardo S Antunes, Natalia L Pontes Póvoa Iorio
Cureus.2025;[Epub] CrossRef - Effect of Chitosan and bioactive glass nanomaterials as intracanal medicaments on TGF-β1 release from intraradicular dentin
Sarah Salah Hashem, Mohammed M. Khalefa, Mahmoud Hassan Mohamed, Hemat M. ELSheikh, Fatma Abd El-Rahman Taher
BMC Oral Health.2025;[Epub] CrossRef - Clinical and radiographic success of lesion sterilization and tissue repair in primary teeth: a systematic review and meta-analysis
Khlood Baghlaf, Rana A. Alamoudi
The Saudi Dental Journal.2025;[Epub] CrossRef - Antibacterial Effect of Cannabinoids on Bacteria Associated with Persistent Endodontic Infections
Cassandra Wieczerza, Haoyan Zhai, Mazin Askar, Zheng Zhou, Susan Paurazas
International Journal of Molecular Sciences.2025; 26(24): 11936. CrossRef - A Comparative Evaluation of Herbal Extracts and Triple Antibiotic Paste as Intracanal Medicament against Enterococcus faecalis: A Microbiological Study
Divya Singh, Rashi Singh, Nidhi Gupta, Natasha Gambhir, Saritha Golla
International Journal of Clinical Pediatric Dentistry.2024; 17(3): 285. CrossRef - Comparative Evaluation of Push-Out Bond Strength of Conventional Mineral Trioxide Aggregate, Biodentine, a Modified Mineral Trioxide Aggregate, and Two Novel Antibacterial-Enhanced Mineral Trioxide Aggregates
Arokia Rajkumar Shancy Merlin, Vignesh Ravindran, Ganesh Jeevanandan, Rajalakshmanan Eswaramoorthy, Abirami Arthanari
Cureus.2024;[Epub] CrossRef - In Vitro Evaluation of the Effect of Oleanolic Acid as a Potential Root Canal Medicament on Viability and Proliferation of Dental Pulp Stem Cells
Khalifah A. Alhaila, Manal Farouk Badawi, Mohamed G. Elbeltagy, Amany E. Badr
European Journal of General Dentistry.2024; 13(01): 051. CrossRef - Regenerative Endodontic Treatment in Dentinogenesis Imperfecta‐Induced Apical Periodontitis
Ying Liao, Ting Pan, Xianghui Xing, Sivakumar Nuvvula
Case Reports in Dentistry.2024;[Epub] CrossRef - Efecto antimicrobiano como medicación intraconducto de la pasta triantibiótica.
Paúl Sebastián Ulloa Amores, Diana Álvarez Álvarez, María Elizabeth Moscoso Abad, Magda Zulay Bastidas Calva
Revista de la Asociación Dental Mexicana.2024; 81(4): 211. CrossRef - Synthesis and Characterization of Nanosilica-Coated Antibiotics, TAP: A Comprehensive Study Utilizing XRD, EDS, FTIR, SEM, and TEM – Invitro Study
Mahaboob S. Hameed, S. Delphine P. Antony, Rajeshkumar Shanmugam, Sandhya Raghu
Journal of International Oral Health.2024; 16(5): 386. CrossRef - Association between host defence peptide IDR‐1002 and ciprofloxacin: Effects on human dental pulp cells
Danilo César Mota Martins, Maurício Gonçalves da Costa Sousa, Poliana Amanda Oliveira Silva, Lana Ribeiro Aguiar, Rosângela Vieira de Andrade, Amandda Évellin Silva‐Carvalho, Felipe Saldanha‐Araújo, Octávio Luiz Franco, Taia Maria Berto Rezende
Australian Endodontic Journal.2024; 50(3): 547. CrossRef - Comparative evaluation of antimicrobial efficacy of triple antibiotic paste and amoxicillin clavulanate paste as an intracanal medicament against Enterococcus faecalis: An in vitro study
Dhandayuthapani Sasikala, Parisa Norouzi Baghkomeh, Jamaluddin Mohammed Farzan
Dental Research Journal.2024;[Epub] CrossRef - Triple Antibiotic Paste: A Game Changer in Endodontics
Kalagi G. Panchal, Karima Virani, Vraj Patel, Aquib Ali Khan, Anam Pettiwala, Srikala S. Puranik, Srushti Joshi
Journal of Pharmacy and Bioallied Sciences.2024; 16(Suppl 3): S1913. CrossRef - Non-surgical Management of a Large Periapical Lesion: A Case Study of the Successful Application of a Modified Triple Antibacterial Paste
Srushti Awghad, Joyeeta Mahapatra, Amit Reche, Ankita Burse, Aradhana Kibe
Cureus.2024;[Epub] CrossRef - Enhancing Antimicrobial Efficacy and Synergistic Effects of Nano-Silica-Based Combinations With Doxycycline, Metronidazole, and Ciprofloxacin Against Enterococcus faecalis Biofilms
Shahul Hameed, Delphine P Antony, Rajeshkumar Shanmugam, Sandhya Raghu, Hima Sandeep Adimulapu
Cureus.2024;[Epub] CrossRef - Healing of periapical lesion by non-surgical endodontic therapy: A case series
Athira Ramesh, Rajesh Pillai, Afzal A, Anakha Santhosh, Arunima G.S, Sandeep K. V
IP Indian Journal of Conservative and Endodontics.2024; 9(2): 99. CrossRef - Effect of Calcium Hydroxide Versus Double Antibiotic Paste on Endodontic Treatment Outcomes in Teeth With Large Periapical Lesions: A Triple‐Blind Randomized Clinical Trial
Afsaneh Rahmati, Farshad Seyedein, Omid Dianat, Sara Saedi, Golriz Rostami, Alireza Akbarzadeh Baghban, Shima Sabertahan, Majid Kazem, Kee Y. Kum
International Journal of Dentistry.2024;[Epub] CrossRef - Can antimicrobial photodynamic therapy serve as an effective adjunct protocol for disinfecting the necrotic root canal system? A randomized controlled study
Remy Barazy, Hisham Alafif, Hassan Achour, Ahmad Al-Aloul, Yasser Alsayed Tolibah
BDJ Open.2024;[Epub] CrossRef - Drain and Treat: A Rubber Dam Technique for Acute Periapical Abscess
S. Grover, K. Mala, J. D’Souza
Acta Medica Bulgarica.2024; 51(s2): 143. CrossRef - Microbial Dynamics in Endodontic Pathology—From Bacterial Infection to Therapeutic Interventions—A Narrative Review
Klara Wieczorkiewicz, Anna Jarząbek, Estera Bakinowska, Kajetan Kiełbowski, Andrzej Pawlik
Pathogens.2024; 14(1): 12. CrossRef - An in vitro comparative evaluation of the effect of three intracanal medicaments – chlorhexidine gel, triple antibiotic paste, and calcium hydroxide paste on the push-out bond strength of MTA Plus, Biodentine, and calcium-enriched mixture
Gouthami Datta, Ramya Raghu, Ashish Shetty, Gautham P Manjunath, Dishant Patel, Subhashini Rajasekhara
Endodontology.2023; 35(1): 60. CrossRef - The cytotoxic effect of cysteamine and its combinations with various endodontic intracanal medications on fibroblast cells: in vitro study
Esraa Adel Mohamed Abd Elhameed ElGammal, Abeer Hashem Mahran, Salma Hassan El Ashry, Sara Hossam Fahmy
Bulletin of the National Research Centre.2023;[Epub] CrossRef - Healing of large endodontic lesions using a new combination of triple antibiotics: A case report
Saeed Asgary, Ardavan Parhizkar
Clinical Case Reports.2023;[Epub] CrossRef - Effects of Intracanal Medicaments on the Measurement Accuracy of Four Apex Locators: An In Vitro Study
Hamza Cudal, Tuğrul Aslan, Bertan Kesim
Meandros Medical and Dental Journal.2023; 24(3): 215. CrossRef - Comparative evaluation of the antibacterial efficacy of herbal agents as intracanal medicaments individually or in combination with chitosan: An in vitro RTPCR study
Gaurav Patri, Kotni Sheetal, PrasantiKumar Pradhan, Pratik Agrawal, S Lata
Journal of International Oral Health.2023; 15(1): 89. CrossRef - Recent progress in carbon dots for anti-pathogen applications in oral cavity
Yuying Jiang, Chuqiang Yin, Jianning Mo, Xiaoyu Wang, Ting Wang, Guotai Li, Qihui Zhou
Frontiers in Cellular and Infection Microbiology.2023;[Epub] CrossRef - A Comprehensive Review of Lesion Sterilization and Tissue Repair: An Alternative for Pulpectomy in Deciduous Teeth
Aparna Achanta, Amit Reche, Rishika Dakhale, Rudra R Bharate
Cureus.2023;[Epub] CrossRef - Healing of Large Endodontic Lesions Using Long‐Term Application of a New Combination of Triple Antibiotics: A Series of Cases
Saeed Asgary, Ardavan Parhizkar, Maria Beatriz Duarte Gavião
Case Reports in Dentistry.2023;[Epub] CrossRef - Non-cytotoxic Root Canal Dressing with Improved Antimicrobial Efficacy
Farzad Koosha, Jerome Cymerman, Thomas Manders, Marcia Simon, Stephen Walker, Miriam Rafailovich
Journal of Endodontics.2023; 49(2): 205. CrossRef - Triple antibiotics: A synergistic approach to combating infection
Hemant Sawhney, Anukriti Kumari, Ritik Kashwani, Geetanjali Gupta, SJ Das
IP Indian Journal of Conservative and Endodontics.2023; 8(4): 189. CrossRef - A 1-year Clinical and Radiographic Assessment of Regenerative Endodontic Therapy for Necrotic Primary Molars: A Randomized controlled Trial
Dina D Abdelmoneim, Amr M Abdelaziz, Gehan G Allam, Amira S Badran
International Journal of Clinical Pediatric Dentistry.2023; 16(2): 295. CrossRef - “BIODENTINE” THE DENTINE IN A CAPSULE AS AN APICAL BARRIER IN TRAUMATIZED MAXILLARY CENTRAL INCISOR WITH TWO YEARS FOLLOW UP.
Savita Thakur, Udai Bhanu, Gurkirat Singh Grewal
INTERNATIONAL JOURNAL OF SCIENTIFIC RESEARCH.2022; : 64. CrossRef - Long-term treatment of dentine with triple antibiotic paste promotes stem cell viability and attachment
Samiya Riaz, Ahmad Azlina, Zuliani Mahmood, Aung T. Htun
Journal of Taibah University Medical Sciences.2022; 17(4): 630. CrossRef - Non surgical management of trauma induced root resorption and large periapical
lesion using bioactive material- A case report
Tejasvini Prajapati, Sonali Kapoor, Purnil Shah, Ankit Arora, Hardik Rana
Clinical Dentistry.2022;[Epub] CrossRef - Antibacterial efficacy of antibiotic pastes versus calcium hydroxide intracanal dressing: A systematic review and meta-analysis of ex vivo studies
Mohammadreza Vatankhah, Kamyar Khosravi, Nazanin Zargar, Armin Shirvani, MohammadHossein Nekoofar, Omid Dianat
Journal of Conservative Dentistry.2022; 25(5): 463. CrossRef - Triple Antibiotic Paste: A Suitable Medicament for Intracanal Disinfection
Krutika Malu, Monika Khubchandani
Cureus.2022;[Epub] CrossRef - Present status and future directions of intracanal medicaments
Ronald Ordinola‐Zapata, W. Craig Noblett, Alejandro Perez‐Ron, Zhou Ye, Jorge Vera
International Endodontic Journal.2022; 55(S3): 613. CrossRef - The effect of four different intracanal medicaments on the push-out bond strength of root canal sealers
Shalu Maan, Vijaya Dhar Bhatt, Rohit Singh, Sayak Gupta, Syed Alay Noorain, Aashna Gill, Pradeep Kumar, Sushil Yadav, Preeti Sharma
Journal of Medicine and Life.2022; 15(4): 448. CrossRef - A Comparative Evaluation of Microhardness and Chemical Structure of Radicular Dentin with Two Combinations of TAP and MTAP: An In Vitro Study
P Niharika, Saigeeta Kondamadugu, Nagireddy Venugopal Reddy, Muthumula Daneswari, Annie P Chris, Nikhila V Reddy
International Journal of Clinical Pediatric Dentistry.2022; 15(S2): S151. CrossRef - Comparative Evaluation of Two Antibiotic Pastes for Root Canal Disinfection
Sadhna Sharma, Urvashi Bhushan, Mridula Goswami, CP Baveja
International Journal of Clinical Pediatric Dentistry.2022; 15(S1): S12. CrossRef - Management of External Inflammatory Root Resorption following Tooth Autotransplantation Using a Modified Combination of Triple Antibiotics
Saeed Asgary, Ardavan Parhizkar, Paulo J. Palma
Case Reports in Dentistry.2022;[Epub] CrossRef - Effect of triple antibiotic paste on the bond strength of epoxy and methacrylate resin-based sealers to root canal dentin
Fereshte Sobhnamayan, Alireza Adl, Mahdi Sedigh-Shams, Hossein Mirkhaghani
Journal of Conservative Dentistry.2022; 25(4): 426. CrossRef - Progress of Research on the Application of Triple Antibiotic Paste and Hydrogel Scaffold Materials in Endodontic Revascularization: A Systematic Review
Jia Zhao, Tian Jiao Wang
Evidence-Based Complementary and Alternative Medicine.2022; 2022: 1. CrossRef - The effect of different intracanal medicaments on the dislodgement resistance of mineral trioxide aggregate
Farzaneh Afkhami, Shahrzad Razavi, Sholeh Ghabraei
BMC Oral Health.2022;[Epub] CrossRef - Efficacy of Ciprofloxacin, Metronidazole and Minocycline in Ordered Mesoporous Silica against Enterococcus faecalis for Dental Pulp Revascularization: An In-Vitro Study
Cintia Micaela Chamorro-Petronacci, Beatriz Santos Torres, Rocío Guerrero-Nieves, Mario Pérez-Sayáns, Marcia Carvalho-de Abreu Fantini, Luis Carlos Cides-da-Silva, Beatriz Magariños, Berta Rivas-Mundiña
Materials.2022; 15(6): 2266. CrossRef - Antibiotic Mixtures in Noninstrumental Endodontic Treatment of Primary Teeth with Necrotic Pulps: A Systematic Review
Farah Chouchene, Fatma Masmoudi, Ahlem Baaziz, Fethi Maatouk, Hichem Ghedira, Sivakumar Nuvvula
International Journal of Dentistry.2021; 2021: 1. CrossRef - Potential apply of hydrogel-carried chlorhexidine and metronidazole in root canal disinfection
Yanhong YAN, Peng ZHOU, Haibing LU, Yun GUAN, Ming MA, Juan WANG, Guangwei SHANG, Beizhan JIANG
Dental Materials Journal.2021; 40(4): 986. CrossRef - Evaluation of the Effect of Nitrofurantoin Paste as an Intracanal Medicament on the Chemical Structure of Radicular Dentine
Mewan Abdulrahman, Bestoon Faraj, Kawa Dizaye
Sulaimani Dental Journal.2021; 8(2): 8. CrossRef - Local Drug Delivery Systems for Vital Pulp Therapy: A New Hope
Ardavan Parhizkar, Saeed Asgary, Carlo Galli
International Journal of Biomaterials.2021; 2021: 1. CrossRef - Antibiofilm and cytotoxic effect of 3,3′-dihydroxycurcumin (DHC) as photosensitizer agent in antimicrobial photodynamic therapy for endodontic purposes
Jesse Augusto Pereira, Carlos Roberto Polaquini, VanessaRodrigues dos Santos, Karina Sampaio Caiaffa, Rafaela Laruzo Rabelo, Reinaldo dos Santos Theodoro, Letícia Helena Theodoro, Luis Octavio Regasini, Cristiane Duque
Photodiagnosis and Photodynamic Therapy.2021; 36: 102534. CrossRef - An in-vitro Comparative Evaluation of Quantitative Release of Transforming Growth Factor β-1 from Dentin upon the Action of Endodontic Irrigants, Medicaments, Ultrasonic Activation, and Low-Level Laser Irradiation
Anilkumar Akhila, V. P. Prabath Singh, Kerala R. Varma, Senthil V. Vasudevan, V. Sukhithasri, Salu Sasikumar
Amrita Journal of Medicine.2021; 17(2): 34. CrossRef - Effect of triple antibiotic paste and calcium hydroxide on the rate of healing of periapical lesions: A systematic review
NKiran Kumar, Biji Brigit, BS Annapoorna, SavithaB Naik, Seema Merwade, K Rashmi
Journal of Conservative Dentistry.2021; 24(4): 307. CrossRef - Comparison of the efficacy of CanalBrush, EndoActivator, and Passive Ultrasonic Irrigation on the removal of triple antibiotic paste from root canal walls: An in vitro study
Santosh Kumar, Kavisha Desai, Aparna Palekar, Baswaraj Biradar, Ananjan Chatterjee, Khushboo Kumari
Journal of International Society of Preventive and Community Dentistry.2020; 10(4): 424. CrossRef - Apexification with Calcium Hydroxide vs. Revascularization
H. Boufdil, M. Mtalsi, S. El Arabi, B. Bousfiha, Jose López-López
Case Reports in Dentistry.2020;[Epub] CrossRef - Effect of Intracanal Medicaments and Irrigants on the Release of Transforming Growth Factor Beta 1 and Vascular Endothelial Growth Factor from Cervical Root Dentin
Lívia Nazareth Ferreira, Regina Maria Puppin-Rontani, Fernanda Miori Pascon
Journal of Endodontics.2020; 46(11): 1616. CrossRef - Incorporation of amoxicillin-loaded microspheres in mineral trioxide aggregate cement: an in vitro study
Fábio Rocha Bohns, Vicente Castelo Branco Leitune, Isadora Martini Garcia, Bruna Genari, Nélio Bairros Dornelles, Silvia Stanisçuaski Guterres, Fabrício Aulo Ogliari, Mary Anne Sampaio de Melo, Fabrício Mezzomo Collares
Restorative Dentistry & Endodontics.2020;[Epub] CrossRef - Assessment of Nitrofurantoin as an Experimental Intracanal Medicament in Endodontics
Mewan Salahalddin A. Alrahman, Bestoon Muhammed Faraj, Kawa F. Dizaye, Abdelwahab Omri
BioMed Research International.2020;[Epub] CrossRef - An in vitro assessment of effect on microhardness of dentin using vicker's hardness method
Manoj Chandak, Richa Modi, Rakesh Gogiya, Rakhi Chandak, Anuja Ikhar, Nikhil Mankar
Journal of Datta Meghe Institute of Medical Sciences University.2020; 15(2): 251. CrossRef - Inspection of the Microbiota in Endodontic Lesions
Mario Dioguardi, Giovanni Di Gioia, Gaetano Illuzzi, Claudia Arena, Vito Carlo Alberto Caponio, Giorgia Apollonia Caloro, Khrystyna Zhurakivska, Iolanda Adipietro, Giuseppe Troiano, Lorenzo Lo Muzio
Dentistry Journal.2019; 7(2): 47. CrossRef - Materials for pulpotomy in immature permanent teeth: a systematic review and meta-analysis
Yuan Chen, Xinlei Chen, Yali Zhang, Fangjie Zhou, Jiaxin Deng, Jing Zou, Yan Wang
BMC Oral Health.2019;[Epub] CrossRef - Adjunctive antimicrobial photodynamic therapy to conventional chemo-mechanical debridement of infected root canal systems: A systematic review and meta-analysis
Maryam Pourhajibagher, Abbas bahador
Photodiagnosis and Photodynamic Therapy.2019; 26: 19. CrossRef - Comparison of Antibacterial Effects of Photodynamic Therapy, Modified Triple Antibiotic Paste and Calcium Hydroxide on Root Canals Infected With Enterococcus faecalis: An In Vitro Study
Mohammad Asnaashari, Mohammad Jafar Eghbal, Amirali Sahba Yaghmayi, Mehdi Shokri, Saranaz Azari-Marhabi
Journal of Lasers in Medical Sciences.2019; 10(5): S23. CrossRef
- Endodontic Intracanal Medicaments and Agents
- 16,175 View
- 180 Download
- 74 Crossref

- Treatment of non-vital immature teeth with amoxicillin-containing triple antibiotic paste resulting in apexification
- Hyon-Beom Park, Bin-Na Lee, Yun-Chan Hwang, In-Nam Hwang, Won-Mann Oh, Hoon-Sang Chang
- Restor Dent Endod 2015;40(4):322-327. Published online August 28, 2015
- DOI: https://doi.org/10.5395/rde.2015.40.4.322
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub A recent treatment option for non-vital immature teeth in young patients is revascularization with triple antibiotic paste (TAP). However, tooth discoloration was reported with the use of conventional minocycline-containing TAP. In this case report, amoxicillin-containing TAP was used for revascularization of non-vital immature teeth to prevent tooth discoloration. At the 1 yr follow up, the teeth were asymptomatic on clinical examination and showed slight discoloration of the crown due to mineral trioxide aggregate (MTA) filling rather than amoxicillin-containing TAP. Radiographic examination revealed complete resolution of the periapical radiolucency, and closed apex with obvious periodontal ligament space. However, the root growth was limited, and the treatment outcome was more like apexification rather than revascularization. These results may be due to unstable blood clot formation which could not resist the condensation force of MTA filling, whether or not a collagen matrix was in place. These cases showed that although revascularization was not successful, apexification could be expected, resulting in the resolution of the periapical radiolucency and the closure of the apex. Therefore, it is worthwhile attempting revascularization of non-vital immature teeth in young patients.
-
Citations
Citations to this article as recorded by- Comparative evaluation of effect of modified triple antibiotic paste and calcium hydroxide as intracanal medicament on microhardness of root dentin: An in vitro study
Aparna Palekar, Piyush Mantri, Minal Awinashe, Basawaraj Biradar, Mukund Singh
Endodontology.2024;[Epub] CrossRef - Healing of Large Endodontic Lesions Using Long‐Term Application of a New Combination of Triple Antibiotics: A Series of Cases
Saeed Asgary, Ardavan Parhizkar, Maria Beatriz Duarte Gavião
Case Reports in Dentistry.2023;[Epub] CrossRef - Comparative Evaluation of Two Antibiotic Pastes for Root Canal Disinfection
Sadhna Sharma, Urvashi Bhushan, Mridula Goswami, CP Baveja
International Journal of Clinical Pediatric Dentistry.2022; 15(S1): S12. CrossRef - Regenerative Endodontics as the Future Treatment of Immature Permanent Teeth
Justyna Zbańska, Katarzyna Herman, Piotr Kuropka, Maciej Dobrzyński
Applied Sciences.2021; 11(13): 6211. CrossRef - Antimicrobial efficacy of triple antibiotic paste in teeth with primary endodontic infection: A systematic review
Rhythm Bains, Aseem P. Tikku, Promila Verma, Pragya Pandey
Asian Journal of Oral Health and Allied Sciences.2021; 11: 2. CrossRef - Effectiveness of MTA apical plug in dens evaginatus with open apices
Khoa Van Pham, Thu Anh Tran
BMC Oral Health.2021;[Epub] CrossRef - Lesion Sterilization and Tissue Repair: A Literature Review
Ankit Rawat, Jyoti Nagpal, Shreeya Mehta, Divya Vyas, Abhishek Kumar, Fathima Amal
Journal of Research and Advancement in Dentistry.2021; 12(3): 6. CrossRef - Spectrophotometric assessment of Tooth discoloration induced by various Antibiotic pastes
Ravi Gupta, Radhika Kewalramani, Dishant Patel
Research Journal of Pharmacy and Technology.2021; : 1979. CrossRef - Comparative evaluation of calcium release of the apical plugs formed by mineral trioxide aggregate, Biodentine, and EndoSequence root repair material with and without 2% triple antibiotic powder: An in vitro study
PoojaNitin Mapara, ND Shashikiran, Sachin Gugawad, Namrata Gaonkar, Savita Hadakar, Swapnil Taur, Dhanshri Khade
Journal of Indian Society of Pedodontics and Preventive Dentistry.2020; 38(2): 132. CrossRef - Effect of triple antibiotic loaded apatitic nanocarriers on Enterococcus faecalis biofilm – An In vitro study
S. Nagarathinam, V. Sujatha, K. Madhumathi, S. Mahalaxmi, P.Pranav Vanajassun, T.S.Sampath Kumar
Journal of Drug Delivery Science and Technology.2019; 51: 499. CrossRef - Coronal tooth discoloration induced by regenerative endodontic treatment using different scaffolds and intracanal coronal barriers: a 6-month ex vivo study
Noushin Shokouhinejad, Hassan Razmi, Maryam Farbod, Marzieh Alikhasi, Josette Camilleri
Restorative Dentistry & Endodontics.2019;[Epub] CrossRef - Triple antibiotic paste: momentous roles and applications in endodontics: a review
Ardavan Parhizkar, Hanieh Nojehdehian, Saeed Asgary
Restorative Dentistry & Endodontics.2018;[Epub] CrossRef - Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview – part II: other clinical applications and complications
M. Torabinejad, M. Parirokh, P. M. H. Dummer
International Endodontic Journal.2018; 51(3): 284. CrossRef - Alternative to Avoid Tooth Discoloration after Regenerative Endodontic Procedure: A Systematic Review
Luciane Geanini Pena dos Santos, Luiz Alexandre Chisini, Camila Guerner Springmann, Beatriz Dulcineia Mendes de Souza, Fernanda Geraldo Pappen, Flávio Fernando Demarco, Mara Cristina Santos Felippe, Wilson Tadeu Felippe
Brazilian Dental Journal.2018; 29(5): 409. CrossRef - Regenerative Endodontic Treatment or Mineral Trioxide Aggregate Apical Plug in Teeth with Necrotic Pulps and Open Apices: A Systematic Review and Meta-analysis
Mahmoud Torabinejad, Ali Nosrat, Prashant Verma, Oyoyo Udochukwu
Journal of Endodontics.2017; 43(11): 1806. CrossRef - Revascularization in Immature Permanent Teeth with Necrotic Pulp and Apical Pathology: Case Series
López Carmen, Mendoza Asunción, Solano Beatriz, Yáñez-Vico Rosa, Jiiang H. Jeng
Case Reports in Dentistry.2017;[Epub] CrossRef
- Comparative evaluation of effect of modified triple antibiotic paste and calcium hydroxide as intracanal medicament on microhardness of root dentin: An in vitro study
- 2,137 View
- 9 Download
- 16 Crossref

- A review of the regenerative endodontic treatment procedure
- Bin-Na Lee, Jong-Wook Moon, Hoon-Sang Chang, In-Nam Hwang, Won-Mann Oh, Yun-Chan Hwang
- Restor Dent Endod 2015;40(3):179-187. Published online March 16, 2015
- DOI: https://doi.org/10.5395/rde.2015.40.3.179
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Traditionally, apexification has been used to treat immature permanent teeth that have lost pulp vitality. This technique promotes the formation of an apical barrier to close the open apex so that the filling materials can be confined to the root canal. Because tissue regeneration cannot be achieved with apexification, a new technique called regenerative endodontic treatment was presented recently to treat immature permanent teeth. Regenerative endodontic treatment is a treatment procedure designed to replace damaged pulp tissue with viable tissue which restores the normal function of the pulp-dentin structure. After regenerative endodontic treatment, continued root development and hard tissue deposition on the dentinal wall can occur under ideal circumstances. However, it is difficult to predict the result of regenerative endodontic treatment. Therefore, the purpose of this study was to summarize multiple factors effects on the result of regenerative endodontic treatment in order to achieve more predictable results. In this study, we investigated the features of regenerative endodontic treatment in comparison with those of other pulp treatment procedures and analyzed the factors that have an effect on regenerative endodontic treatment.
-
Citations
Citations to this article as recorded by- Evaluation of the Clinical Outcomes of Regenerative Endodontic Procedures Using Autologous Platelet Concentrate: A Systematic Review and Meta-Analysis
Elnaz Mousavi, Navid Nasrabadi, Samira Jamali, Arian Haddadi
Pesquisa Brasileira em Odontopediatria e Clínica Integrada.2025;[Epub] CrossRef - Antimicrobial 3D printed gelatin scaffolds for root canal disinfection in regenerative endodontics procedures
Mateo Dallos Ortega, Jenny Aveyard, Raghda Magdy Abdelgawad, Reem El-Gendy, Alexander Ciupa, David Whetnall, Julia Behnsen, Robert J. Poole, Raechelle A. D'Sa
Biomaterials Science.2025; 13(14): 3795. CrossRef - Regenerative Endodontic Therapies: Harnessing Stem Cells, Scaffolds, and Growth Factors
Rosana Farjaminejad, Samira Farjaminejad, Franklin Garcia-Godoy
Polymers.2025; 17(11): 1475. CrossRef - Effects of combining hyaluronic acid hydrogel with injectable platelet rich fibrin on apical papilla stem cells proliferation and differentiation
Azal H. Al-Masoody, Nasrin Asadi, Hadiseh Mohammadpour, Mahshid Hodjat, Tahereh Sadat Jafarzadeh Kashi
BMC Oral Health.2025;[Epub] CrossRef - Experts consensus on management of tooth luxation and avulsion
Ruijie Huang, Chenchen Zhou, Ling Zhan, Yuan Liu, Xian Liu, Qin Du, Jun Wang, Wei Zhao, Guangtai Song, Li-an Wu, Beizhan Jiang, Yanhong Li, Hongmei Zhang, Jing Zou
International Journal of Oral Science.2024;[Epub] CrossRef - A review of tissue engineering in regenerative endodontic treatment
Eric Priyo Prasetyo, Dian Agustin Wahjuningrum, Galih Sampoerno, Wilson Sukandar, Shafy Shariz Bin Sharizal, Nurfahira Paidal, Menza Fadiyan Amriel, Nathania Elita Gunawan, Ketut Suardita, Evelyn Tjendronegoro
Conservative Dentistry Journal.2024; 14(1): 1. CrossRef - Innovative Paradigms and Established Strategies in Tooth Revitalization: A Review
Ahmad Shah Khan, Zahid Mehmood Khan, Palwasha Ishaque, Muhammad Zubair, Syeda Fatima Tu Zahra, Sana Ashfaq
Dental Update.2024; 51(8): 570. CrossRef - Explore the most recent developments and upcoming outlooks in the field of dental nanomaterials
Ali Alsuraifi, Zainab M. Sulaiman, Noor Alhuda R. Mohammed, Jassim Mohammed, Sarah Kareem Ali, Yousef Husam Abdualihamaid, Fatimah Husam, Abdullah Ayad
Beni-Suef University Journal of Basic and Applied Sciences.2024;[Epub] CrossRef - Recent Advances in Regenerative Endodontics: A Review of Current Techniques and Future Directions
Firas A Alothman, Lamia S Hakami, Ali Alnasser, Faris M AlGhamdi, Abdullah A Alamri, Basel M Almutairii
Cureus.2024;[Epub] CrossRef - Regenerative Potential of Dental Pulp Stem Cells in Response to a Bioceramic Dental Sealer and Photobiomodulation: An In Vitro Study
Hamed A Alshawkani, Mohamed Mansy, Mahmoud Al Ankily, Mohamed Shamel
The Journal of Contemporary Dental Practice.2024; 25(4): 313. CrossRef - Marginal adaptation of customized gutta percha cone with calcium silicate based sealer versus MTA and biodentine apical plugs in simulated immature permanent teeth (an in vitro study)
Mary M. Mina, Sybel M. Moussa, Mahmoud R. Aboelseoud
BMC Oral Health.2024;[Epub] CrossRef - GelMA‐based hydrogel biomaterial scaffold: A versatile platform for regenerative endodontics
Lei Huang, Xuan Chen, XiaoXia Yang, Yinchun Zhang, Xiaoling Qiu
Journal of Biomedical Materials Research Part B: Applied Biomaterials.2024;[Epub] CrossRef - Regenerative Endodontic Treatment in Dentinogenesis Imperfecta‐Induced Apical Periodontitis
Ying Liao, Ting Pan, Xianghui Xing, Sivakumar Nuvvula
Case Reports in Dentistry.2024;[Epub] CrossRef - In vitro and in vivo evaluation of iRoot BP Plus as a coronal sealing material for regenerative endodontic procedures
Ning Yang, Wenxiao Yang, Rou Shen, Shengcai Zhang, Tianchi Ma, Yao Liu
Clinical Oral Investigations.2024;[Epub] CrossRef - Comparative evaluation of pH and Ca+ ion release from MTA on interaction with platelet-rich fibrin and blood clot: an in vitro study
Sonia Khatri, Sylvia Mathew, Shruthi Nagaraja, Swaroop Hegde, Soumyadeep Ghosh, Kavimalar Ravichandran
F1000Research.2023; 12: 364. CrossRef - Photobiomodulation Therapy and Pulp-Regenerative Endodontics: A Narrative Review
Jiawen Yong, Sabine Gröger, Zuping Wu, Sabine Ruf, Yuer Ye, Xiaoyan Chen
Bioengineering.2023; 10(3): 371. CrossRef - Efficacy of disinfection procedures performed prior to regenerative endodontic therapy: An integrative review
Ketillyn da Silva Magalhães, Ana Clara Kuerten Gil, Taynara Santos Goulart, Daniela Peressoni Vieira Schuldt, Beatriz Serrato Coelho, Daniela de Rossi Figueiredo, Lucas da Fonseca Roberti Garcia, Josiane de Almeida
Australian Endodontic Journal.2023; 49(2): 418. CrossRef - Newer Prospects of Regenerative Endodontics: A Comprehensive and Updated Review of Literature
Mohammad Kamran Khan, Mahendra Kumar Jindal
Journal of the Scientific Society.2023; 50(3): 299. CrossRef - Comparative evaluation of pH and Ca+ ion release from MTA on interaction with platelet-rich fibrin and blood clot: an in vitro study
Sonia Khatri, Sylvia Mathew, Shruthi Nagaraja, Swaroop Hegde, Soumyadeep Ghosh, Kavimalar Ravichandran
F1000Research.2023; 12: 364. CrossRef - Effects of CEM cement and emdogain on proliferation and differentiation of human stem cells from the apical papilla: a comparative in vitro study
Elham Khoshbin, Leila Ghasemi, Rezvan Najafi, Hamed Karkehabadi
Biotechnology Letters.2023; 45(1): 69. CrossRef - Comparative Evaluation of the Regenerative Potential of Blood Clot and Platelet-rich Fibrin in Young Permanent Teeth Based on the Revised American Academy of Endodontics Clinical Considerations for Regenerative Procedure: 2016
Saraswathi V Naik, Prabhakar Attiguppe, Aarathi J Prakash
International Journal of Clinical Pediatric Dentistry.2023; 16(S2): S149. CrossRef - Biomechanical characterization of a fibrinogen–blood hydrogel for human dental pulp regeneration
Sofia Silvia Piglionico, Bela Varga, Orsolya Pall, Olivier Romieu, Csilla Gergely, Frédéric Cuisinier, Bernard Levallois, Ivan Vladislavov Panayotov
Biomaterials Science.2023; 11(20): 6919. CrossRef - Intracellular bacterial eradication using a novel peptide in vitro
Wing Nok Isaac Ng, Shanthini Kalimuthu, Carmen Oi Kwan Law, Angeline Hui Cheng Lee, Terrence Chi Kong Lau, Yiu Yan Leung, Gary Shun Pan Cheung, Prasanna Neelakantan
International Endodontic Journal.2023; 56(11): 1360. CrossRef - Regenerative Endodontic Treatment of Previously Treated Mature Permanent Tooth: A Case Report with 3-year Follow Up
Myung-Jin Lee
The Korean Journal of Oral and Maxillofacial Pathology.2023; 47(6): 133. CrossRef - Clinical Outcome and Comparison of Regenerative and Apexification Intervention in Young Immature Necrotic Teeth—A Systematic Review and Meta-Analysis
Pratima Panda, Lora Mishra, Shashirekha Govind, Saurav Panda, Barbara Lapinska
Journal of Clinical Medicine.2022; 11(13): 3909. CrossRef - Evaluation of Attitude and Knowledge of Endodontic, Pedodontic and SBARD Residents in Saudi Arabia toward Regenerative Endodontics—A National Survey
Ali A. Assiry, Mohmed Isaqali Karobari, Niher Tabassum Snigdha, Roshan Noor Mohamed, Syed Nahid Basheer, Mohammed Zameer
Medicina.2022; 58(4): 545. CrossRef - Effects of Intracanal Antimicrobials on Viability and Differentiation of Stem Cells From the Apical Papilla: An In Vitro Study
Gavin Raddall, Isabel Mello, Brendan M. Leung
Journal of Endodontics.2022; 48(7): 880. CrossRef - Awareness and Acceptance of Vital Pulp Therapy and Regenerative Endodontic Procedures among Dental Professionals in India: A Web-based Survey
Saloni Rathi, Priya Chauhan, Suparna Ganguly Saha, Rolly Agarwal, Simar Kaur Manocha, Mrinali Chaddha
Journal of Research and Advancement in Dentistry.2022; 14(1): 10. CrossRef - Exosomes as Biochemistry Tools for Stem Cell Differentiation: A Novel Cell-Based Treatment for Diseases
Saeed Azandeh, Darioush Bijan Nejad, Samaneh Karimi, Fereshtesadat Fakhredini
Jentashapir Journal of Cellular and Molecular Biology.2022;[Epub] CrossRef - Effect of biodentine coated with emdogain on proliferation and differentiation of human stem cells from the apical papilla
Hamed Karkehabadi, Erfan Ahmadyani, Rezvan Najafi, Elham Khoshbin
Molecular Biology Reports.2022; 49(5): 3685. CrossRef - Evaluation of the Effectiveness of Laser‐Assisted Bleaching of the Teeth Discolored due to Regenerative Endodontic Treatment
Noushin Shokouhinejad, Mehrfam Khoshkhounejad, Fatemeh Hamidzadeh, Murilo Baena Lopes
International Journal of Dentistry.2022;[Epub] CrossRef - Triple Antibiotic Paste: A Suitable Medicament for Intracanal Disinfection
Krutika Malu, Monika Khubchandani
Cureus.2022;[Epub] CrossRef - A Comparative Evaluation of Microhardness and Chemical Structure of Radicular Dentin with Two Combinations of TAP and MTAP: An In Vitro Study
P Niharika, Saigeeta Kondamadugu, Nagireddy Venugopal Reddy, Muthumula Daneswari, Annie P Chris, Nikhila V Reddy
International Journal of Clinical Pediatric Dentistry.2022; 15(S2): S151. CrossRef - Comparing Antibiotic Pastes with Electrospun Nanofibers as Modern Drug Delivery Systems for Regenerative Endodontics
Nura Brimo, Dilek Çökeliler Serdaroğlu, Busra Uysal
Current Drug Delivery.2022; 19(9): 904. CrossRef - The Advances of Blood Clots Used as Biomaterials in Regenerative Medicine
Eliza VanZweden, Rachael Tolsma, Victor Hung, Peter Awad, Robert Sawyer, Yong Li
Regenerative Medicine.2022; 17(12): 957. CrossRef - Microstructure and color stability of calcium silicate-based dental materials exposed to blood or platelet-rich fibrin
Noushin Shokouhinejad, Ibrahim Abu Tahun, Shima Saber Tahan, Fatemeh Mohandes, Mohammad H. Nekoofar, Paul M. H. Dummer
Clinical Oral Investigations.2022; 27(3): 1193. CrossRef - Results of “proroot mta” application in treatment of chronic periodontitis in teeth with incomplete root formation
N.M. Korneeva, E.A. Novikova, D.S. Popova, K.S. Rabadanova, L.Ya Rzaeva
Stomatology for All / International Dental review.2022; (2(99)): 10. CrossRef - Antimicrobial Effect of Calcium Hydroxide Combined with Electrolyzed Superoxidized Solution at Neutral pH on Enterococcus faecalis Growth
Héctor Armando Jimenez-Gonzalez, María Argelia Akemi Nakagoshi-Cepeda, Sergio Eduardo Nakagoshi-Cepeda, Víctor Hugo Urrutia-Baca, Myriam Angélica De La Garza-Ramos, Juan Manuel Solis-Soto, Ricardo Gomez-Flores, Patricia Tamez-Guerra, Yeliz Guven
BioMed Research International.2021;[Epub] CrossRef - Unpredictable Outcomes of a Regenerative Endodontic Treatment
Zahra Mohammadi, Hadi Assadian, Behnam Bolhari, Mohammadreza Sharifian, Mehrfam Khoshkhounejad, Nazanin Chitsaz, Andrea Scribante
Case Reports in Dentistry.2021;[Epub] CrossRef - Revascularization of nonvital immature incisor with asymptomatic apical periodontitis
Ema Mulyawati, Pribadi Santosa, Tunjung Nugraheni
Scientific Dental Journal.2020; 4(3): 134. CrossRef - Comparative analysis of calcium hydroxide apexification and regenerative endodontic procedure for root dentine growth stimulation in immature incisors with pulp necrosis
M.S. Rakhmanova, M.V. Korolenkova
Stomatologiya.2020; 99(6): 55. CrossRef - Antimicrobial Efficacy of a Novel Antibiotic‐Eluting Injectable Platelet‐Rich Fibrin Scaffold against a Dual‐Species Biofilm in an Infected Immature Root Canal Model
Azade Rafiee, Mahtab Memarpour, Yasaman Najibi, Bahman Khalvati, Sedigheh Kianpour, Mohammad Hossein Morowvat, Sung-Hwan Choi
BioMed Research International.2020;[Epub] CrossRef - Exosomes Derived from Stem Cells from the Apical Papilla Promote Dentine-Pulp Complex Regeneration by Inducing Specific Dentinogenesis
Xueying Zhuang, Lingli Ji, Huan Jiang, Yao Liu, Xuemei Liu, Jing Bi, Weidong Zhao, Zhenjiang Ding, Xu Chen
Stem Cells International.2020; 2020: 1. CrossRef - Injectable Biomaterials for Dental Tissue Regeneration
Håvard Jostein Haugen, Poulami Basu, Mousumi Sukul, João F Mano, Janne Elin Reseland
International Journal of Molecular Sciences.2020; 21(10): 3442. CrossRef - Viability and Stimulation of Human Stem Cells from the Apical Papilla (hSCAPs) Induced by Silicate-Based Materials for Their Potential Use in Regenerative Endodontics: A Systematic Review
José Luis Sanz, Leopoldo Forner, Alicia Almudéver, Julia Guerrero-Gironés, Carmen Llena
Materials.2020; 13(4): 974. CrossRef - An Innovative Drug Delivery System Loaded with a Modified Combination of Triple Antibiotics for Use in Endodontic Applications
Ardavan Parhizkar, Hanieh Nojehdehian, Fahimeh Tabatabaei, Saeed Asgary
International Journal of Dentistry.2020; 2020: 1. CrossRef - Defining Endodontic Residents' Clinical Experiences: A National Survey
Jonathan D. Blacher, Kamran E. Safavi, Robert H. Aseltine, Blythe M. Kaufman
Journal of Dental Education.2019; 83(5): 504. CrossRef - Coronal tooth discoloration induced by regenerative endodontic treatment using different scaffolds and intracanal coronal barriers: a 6-month ex vivo study
Noushin Shokouhinejad, Hassan Razmi, Maryam Farbod, Marzieh Alikhasi, Josette Camilleri
Restorative Dentistry & Endodontics.2019;[Epub] CrossRef - Comparative Study between Revitalization of Necrotic Immature Permanent Anterior Teeth with and without Platelet Rich Fibrin: A Randomized Controlled Trial
Rasha Adel Ragab, Amr Ezzat Abd El Lattif, Norhan Abd El Wahab El Dokky
Journal of Clinical Pediatric Dentistry.2019; 43(2): 78. CrossRef - Biomaterials and Scaffold Design Strategies for Regenerative Endodontic Therapy
Gavin Raddall, Isabel Mello, Brendan M. Leung
Frontiers in Bioengineering and Biotechnology.2019;[Epub] CrossRef - Iloprost Induces Dental Pulp Angiogenesis in a Growth Factor–free 3-Dimensional Organ Culture System
Sonntana Seang, Prasit Pavasant, Chalida N. Limjeerajarus
Journal of Endodontics.2018; 44(5): 759. CrossRef - Ratio and Rate of Induced Root Growth in Necrotic Immature Teeth
Eun Jung Sang, Ji-Soo Song, Teo Jeon Shin, Young-Jae Kim, Jung-Wook Kim, Ki-Taeg Jang, Sang-Hoon Lee, Hong-Keun Hyun
THE JOURNAL OF THE KOREAN ACADEMY OF PEDTATRIC DENTISTRY.2018; 45(2): 225. CrossRef - Triple antibiotic paste: momentous roles and applications in endodontics: a review
Ardavan Parhizkar, Hanieh Nojehdehian, Saeed Asgary
Restorative Dentistry & Endodontics.2018;[Epub] CrossRef - Traumatic avulsion and delayed replantation of maxillary incisors in an eleven-year-old child
Gokcen Deniz Bayrak
Edorium Journal of Dentistry.2018; 5(1): 1. CrossRef - Influence of Apical Diameter on the Outcome of Regenerative Endodontic Treatment in Teeth with Pulp Necrosis: A Review
Yanjun Fang, Xinhuan Wang, Jingjing Zhu, Chaonan Su, Ying Yang, Liuyan Meng
Journal of Endodontics.2018; 44(3): 414. CrossRef - Assessment of Regaining Pulp Sensibility in Mature Necrotic Teeth Using a Modified Revascularization Technique with Platelet-rich Fibrin: A Clinical Study
Mohamed Nageh, Geraldine M. Ahmed, Alaa A. El-Baz
Journal of Endodontics.2018; 44(10): 1526. CrossRef - Local drug delivery in endodontics: A literature review
Shin Hye Chung, Young-Seok Park
Journal of Drug Delivery Science and Technology.2017; 39: 334. CrossRef - Regenerative Endodontics
Kristina Feigin, Bonnie Shope
Journal of Veterinary Dentistry.2017; 34(3): 161. CrossRef - Intentional Replantation of an Avulsed Immature Permanent Incisor: A Case Report
Claudio Maniglia-Ferreira, Fabio de Almeida Gomes, Marcelo de Morais Vitoriano
Journal of Endodontics.2017; 43(8): 1383. CrossRef - Effect of acidic solutions on the microhardness of dentin and set OrthoMTA and their cytotoxicity on murine macrophage
Soram Oh, Hiran Perinpanayagam, Yoon Lee, Jae-Won Kum, Yeon-Jee Yoo, Sang-Min Lim, Seok Woo Chang, Won-Jun Shon, Woocheol Lee, Seung-Ho Baek, Kee-Yeon Kum
Restorative Dentistry & Endodontics.2016; 41(1): 12. CrossRef - Questioning the spot light on Hi-tech endodontics
Jojo Kottoor, Denzil Albuquerque
Restorative Dentistry & Endodontics.2016; 41(1): 80. CrossRef - Effects of a Bioactive Scaffold Containing a Sustained Transforming Growth Factor-β1–releasing Nanoparticle System on the Migration and Differentiation of Stem Cells from the Apical Papilla
Craig Bellamy, Suja Shrestha, Calvin Torneck, Anil Kishen
Journal of Endodontics.2016; 42(9): 1385. CrossRef - Effects of Novel 3-dimensional Antibiotic-containing Electrospun Scaffolds on Dentin Discoloration
Margaret Louise A. Porter, Eliseu A. Münchow, Maria T.P. Albuquerque, Kenneth J. Spolnik, Anderson T. Hara, Marco C. Bottino
Journal of Endodontics.2016; 42(1): 106. CrossRef
- Evaluation of the Clinical Outcomes of Regenerative Endodontic Procedures Using Autologous Platelet Concentrate: A Systematic Review and Meta-Analysis
- 7,085 View
- 116 Download
- 63 Crossref

- Biodentine-a novel dentinal substitute for single visit apexification
- Gurudutt Nayak, Mohammad Faiz Hasan
- Restor Dent Endod 2014;39(2):120-125. Published online March 21, 2014
- DOI: https://doi.org/10.5395/rde.2014.39.2.120
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Use of an apical plug in management of cases with open apices has gained popularity in recent years. Biodentine, a new calcium silicate-based material has recently been introduced as a dentine substitute, whenever original dentine is damaged. This case report describes single visit apexification in a maxillary central incisor with necrotic pulp and open apex using Biodentine as an apical barrier, and a synthetic collagen material as an internal matrix. Following canal cleaning and shaping, calcium hydroxide was placed as an intracanal medicament for 1 mon. This was followed by placement of small piece of absorbable collagen membrane beyond the root apex to serve as matrix. An apical plug of Biodentine of 5 mm thickness was placed against the matrix using pre-fitted hand pluggers. The remainder of canal was back-filled with thermoplasticized gutta-percha and access cavity was restored with composite resin followed by all-ceramic crown. One year follow-up revealed restored aesthetics and function, absence of clinical signs and symptoms, resolution of periapical rarefaction, and a thin layer of calcific tissue formed apical to the Biodentine barrier. The positive clinical outcome in this case is encouraging for the use of Biodentine as an apical plug in single visit apexification procedures.
-
Citations
Citations to this article as recorded by- Cone-Beam Computed Tomography (CBCT)-Guided Non-surgical Management of Type II Dens Invaginatus in Maxillary Lateral Incisors Using Calcium Silicate-Based Materials: A Case Series
Prerna Priya
Cureus.2026;[Epub] CrossRef - A Prospective Randomised Clinical Trial Evaluating Pulpotomy in Primary Molars With Three Bioceramic Calcium Silicate Cements: 24 Month Follow‐Up
Abhinav L. Talekar, Prasad K. Musale, Gayatri S. Chaudhari, Tayaba M. H. Silotry, William F. Waggoner
International Journal of Paediatric Dentistry.2025; 35(4): 763. CrossRef - Comparative evaluation of sealing potential of mineral trioxide aggregate, biodentine, and bio-C repair in furcation perforations: A glucose penetration study
Ashwija Shetty, Hajira Anjum Sultana, A. Srirekha, C. Champa, Suditi Pal, V. Sahithi
Journal of Conservative Dentistry and Endodontics.2025; 28(2): 144. CrossRef - Effect of Vital Pulp Therapy Biomaterials on Tooth Discolouration: A Review of the Literature
Maedeh Gilvari Sarshari, Kiana Shakeri, Ardavan Parhizkar, Naresh Kasoju
International Journal of Biomaterials.2025;[Epub] CrossRef - Evaluation of interface gaps and internal voids in MTA-based biomaterials used for apexification with micro-CT
Huda Melike Bayram
Journal of the Australian Ceramic Society.2025;[Epub] CrossRef - Management of Immature Permanent Mandibular First Molar Using NeoPutty: A Case Report
Maryam Khorasanchi, Maryam Gharechahi, Zahra Azizi
Clinical Case Reports.2025;[Epub] CrossRef - Treating apical fenestration in a previously endodontically treated tooth
K. S Rajesh, Riza Farooq, F Abdul Rajak, Pradeep Kumar
Journal of Conservative Dentistry and Endodontics.2024; 27(11): 1193. CrossRef - Influence of Bioceramic Cements on the Quality of Obturation of the Immature Tooth: An In Vitro Microscopic and Tomographic Study
Raya Al-Rayesse, Ossama Al-Jabban, Ammar Eid, Alaa Kabtoleh, Frédéric Addiego, Davide Mancino, Youssef Haikel, Naji Kharouf
Bioengineering.2024; 11(3): 213. CrossRef - Fracture Susceptibility in Non-Vital Apex Teeth Following Various Modified Apexification Procedure – An In Vitro Study
NJ Nagaraj, Peyush Pratap Singh Sikarwar, Debkant Jena, Rini Gangwal, Ipsita Mohanty, Adnan Haider Rizvi
Journal of Pharmacy and Bioallied Sciences.2024; 16(Suppl 4): S3966. CrossRef - Bioceramics in Endodontics: Updates and Future Perspectives
Xu Dong, Xin Xu
Bioengineering.2023; 10(3): 354. CrossRef - Effects of Apical Barriers and Root Filling Materials on Stress Distribution in Immature Teeth: Finite Element Analysis Study
Minna Chun, Tory Silvestrin, Roberto Savignano, Gina Delia Roque-Torres
Journal of Endodontics.2023; 49(5): 575. CrossRef - Current Bio-based Cements and Radioactive Opacifiers in Endodontic Approaches: A Review of the Materials Used in Clinical Practice
A.Najah Saud, Erkan Koç , Olcay Özdemir
European Journal of Therapeutics.2023; 29(4): 930. CrossRef - Clinical Management of External Apical Root Resorption Using Amnion Membrane Matrix and Bio Dentine
Jeong-Kui Ku, In-Woong Um, Mi-Kyoung Jun, Il-hyung Kim
Journal of Current Research in Oral Surgery.2023; 3(1): 1. CrossRef - Comparative Evaluation of Mineral Trioxide Aggregate and Biodentine Apical Plug Thickness on Fracture Resistance of Immature Teeth
Pramod Mohite, Ankita Dadarao Ramteke, Ruchika Gupta, Suvarna Patil, Divya Gupta
Annals of African Medicine.2022; 21(3): 198. CrossRef - Comparison of sealing ability of mineral trioxide aggregate, biodentine with and without bioactive glass as furcation repair materials
Shaik Afreen Kamal, Roopadevi Garlapati, Nagesh Bolla, Sayesh Vemuri, Bandaru Pydiahnaidu, Yandra Lakshmi Suvarna
Endodontology.2022; 34(1): 45. CrossRef - “BIODENTINE” THE DENTINE IN A CAPSULE AS AN APICAL BARRIER IN TRAUMATIZED MAXILLARY CENTRAL INCISOR WITH TWO YEARS FOLLOW UP.
Savita Thakur, Udai Bhanu, Gurkirat Singh Grewal
INTERNATIONAL JOURNAL OF SCIENTIFIC RESEARCH.2022; : 64. CrossRef - Comparative Efficacy of Bioceramics Apexification in Periradicular Healing and Root-end Calcific Tissue Repair in Immature Traumatized Permanent Anterior Teeth
Shalini Garg, Sumit Singla, Satyavan Gangaram Damle, Abhishek Dhindsa, Ashish Loomba, Pragati Poddar
World Journal of Dentistry.2022; 13(S2): S194. CrossRef - Amnion Membrane Matrix And Bio Dentine In The Management Of An External Apical Root Resorption
Gyanendra Pratap Singh, Shruthi H Attavar, Sivaji Kavuri
Annals of Dental Specialty.2022; 10(2): 11. CrossRef - Morphological and Chemical Analysis of Different Types of Calcium Silicate‐Based Cements
Okba Mahmoud, Nashwan Abdullah Al-Afifi, Mohideen Salihu Farook, Maysara Adnan Ibrahim, Saaid Al Shehadat, Mohammed Amjed Alsaegh, Sandrine Bittencourt Berger
International Journal of Dentistry.2022;[Epub] CrossRef - Evaluation of a Novel Tool for Apical Plug Formation during Apexification of Immature Teeth
Yasser Alsayed Tolibah, Line Droubi, Saleh Alkurdi, Mohammad Tamer Abbara, Nada Bshara, Thuraya Lazkani, Chaza Kouchaji, Ibrahim Ali Ahmad, Ziad D. Baghdadi
International Journal of Environmental Research and Public Health.2022; 19(9): 5304. CrossRef - Fracture resistance of simulated immature roots using Biodentine and fiber post compared with different canal-filling materials under aging conditions
Amr Elnaghy, Shaymaa Elsaka
Clinical Oral Investigations.2020; 24(3): 1333. CrossRef - Modified Apexification Procedure for Immature Permanent Teeth with a Necrotic Pulp/Apical Periodontitis: A Case Series
Kamolthip Songtrakul, Talayeh Azarpajouh, Matthew Malek, Asgeir Sigurdsson, Bill Kahler, Louis M. Lin
Journal of Endodontics.2020; 46(1): 116. CrossRef - Efficacy of cavity liners with/without atmospheric cold helium plasma jet for dentin remineralization
Hamid Kermanshah, Reza Saeedi, Elham Ahmadi, Ladan Ranjbar Omrani
Biomaterial Investigations in Dentistry.2020; 7(1): 120. CrossRef - APICAL MICROLEAKAGE OF VARIOUS BIOMATERIALS IN SIMULATED IMMATURE APICES
Fatih TULUMBACI, Volkan ARIKAN, Aylin AKBAY OBA, İşıl SÖNMEZ ŞAROĞLU
Selcuk Dental Journal.2019; 6(3): 247. CrossRef - Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview – part II: other clinical applications and complications
M. Torabinejad, M. Parirokh, P. M. H. Dummer
International Endodontic Journal.2018; 51(3): 284. CrossRef - Recent Trends in Tricalcium Silicates for Vital Pulp Therapy
Imad About
Current Oral Health Reports.2018; 5(3): 178. CrossRef - Biodentine™ material characteristics and clinical applications: a 3 year literature review and update
S. Rajasekharan, L. C. Martens, R. G. E. C. Cauwels, R. P. Anthonappa
European Archives of Paediatric Dentistry.2018; 19(1): 1. CrossRef - Will Bioceramics be the Future Root Canal Filling Materials?
Josette Camilleri
Current Oral Health Reports.2017; 4(3): 228. CrossRef - Clinical and Molecular Perspectives of Reparative Dentin Formation
Minju Song, Bo Yu, Sol Kim, Marc Hayashi, Colby Smith, Suhjin Sohn, Euiseong Kim, James Lim, Richard G. Stevenson, Reuben H. Kim
Dental Clinics of North America.2017; 61(1): 93. CrossRef - Management of Dens Invaginatus Type II Associated with Immature Apex and Large Periradicular Lesion Using Platelet-rich Fibrin and Biodentine
Shruti Goel, Ruchika Roongta Nawal, Sangeeta Talwar
Journal of Endodontics.2017; 43(10): 1750. CrossRef - Biodentine: from biochemical and bioactive properties to clinical applications
Imad About
Giornale Italiano di Endodonzia.2016; 30(2): 81. CrossRef - Apical Closure in Apexification: A Review and Case Report of Apexification Treatment of an Immature Permanent Tooth with Biodentine
Karla Vidal, Gabriela Martin, Oscar Lozano, Marco Salas, Jaime Trigueros, Gabriel Aguilar
Journal of Endodontics.2016; 42(5): 730. CrossRef - Influence of Biodentine® - A Dentine Substitute - On Collagen Type I Synthesis in Pulp Fibroblasts In Vitro
Frangis Nikfarjam, Kim Beyer, Anke König, Matthias Hofmann, Manuel Butting, Eva Valesky, Stefan Kippenberger, Roland Kaufmann, Detlef Heidemann, August Bernd, Nadja Nicole Zöller, Dimitrios Karamichos
PLOS ONE.2016; 11(12): e0167633. CrossRef
- Cone-Beam Computed Tomography (CBCT)-Guided Non-surgical Management of Type II Dens Invaginatus in Maxillary Lateral Incisors Using Calcium Silicate-Based Materials: A Case Series
- 2,496 View
- 31 Download
- 33 Crossref


 KACD
KACD

 First
First Prev
Prev


