Articles
- Page Path
- HOME > Restor Dent Endod > Volume 46(1); 2021 > Article
- Research Article A micro-computed tomographic study using a novel test model to assess the filling ability and volumetric changes of bioceramic root repair materials
-
Fernanda Ferrari Esteves Torres
 , Jader Camilo Pinto
, Jader Camilo Pinto , Gabriella Oliveira Figueira
, Gabriella Oliveira Figueira , Juliane Maria Guerreiro-Tanomaru
, Juliane Maria Guerreiro-Tanomaru , Mario Tanomaru-Filho
, Mario Tanomaru-Filho
-
Restor Dent Endod 2020;46(1):e2.
DOI: https://doi.org/10.5395/rde.2021.46.e2
Published online: December 8, 2020
Department of Restorative Dentistry, São Paulo State University (UNESP), School of Dentistry, Araraquara, SP, Brazil.
- Correspondence to Mario Tanomaru-Filho, DDS, PhD. Full Professor, Department of Restorative Dentistry, São Paulo State University (UNESP), School of Dentistry, Rua Humaitá, 1680 CEP Araraquara, SP 14801-903, Brazil. tanomaru@uol.com.br
Copyright © 2021. The Korean Academy of Conservative Dentistry
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Objectives New premixed bioceramic root repair materials require moisture for setting. Using micro-computed tomography (micro-CT), this study evaluated the filling ability and volumetric changes of calcium silicate-based repair materials (mineral trioxide aggregate repair high-plasticity [MTA HP] and Bio-C Repair, Angelus), in comparison with a zinc oxide and eugenol-based material (intermediate restorative material [IRM]; Dentsply DeTrey).
-
Materials and Methods Gypsum models with cavities 3 mm deep and 1 mm in diameter were manufactured and scanned using micro-CT (SkyScan 1272. Bruker). The cavities were filled with the cements and scanned again to evaluate their filling capacity. Another scan was performed after immersing the samples in distilled water for 7 days to assess the volumetric changes of the cements. The statistical significance of differences in the data was evaluated using analysis of variance and the Tukey test with a 5% significance level.
-
Results Bio-C Repair had a greater filling ability than MTA HP (p < 0.05). IRM was similar to Bio-C and MTA HP (p > 0.05). MTA HP presented the largest volumetric change (p < 0.05), showing more volume loss than Bio-C and IRM, which were similar (p > 0.05).
-
Conclusions Bio-C Repair is a new endodontic material with excellent filling capacity and low volumetric change. The gypsum model proposed for evaluating filling ability and volumetric changes by micro-CT had appropriate and reproducible results. This model may enhance the physicochemical evaluation of premixed bioceramic materials, which need moisture for setting.
INTRODUCTION
MATERIALS AND METHODS
The manufacturers, composition, and proportions of the endodontic materials used in this study
Schematic figure of the assessments of filling ability and volumetric changes. Gypsum–based models with cavities measuring 3 mm deep and 1 mm in diameter were manufactured and scanned using micro-computed tomography before and after filling. The samples were immersed in distilled water for 7 days, and another scan was performed.

RESULTS
Results for filling ability and volumetric changes of the endodontic materials
| Test/material | Bio-C Repair | MTA HP | IRM |
|---|---|---|---|
| Filling ability (%) | 97.30 ± 2.01a | 89.80 ± 4.94b | 92.30 ± 5.37a,b |
| Volumetric change (%) | −2.36 ± 0.75b | −3.67 ± 0.86a | −2.10 ± 0.83b |
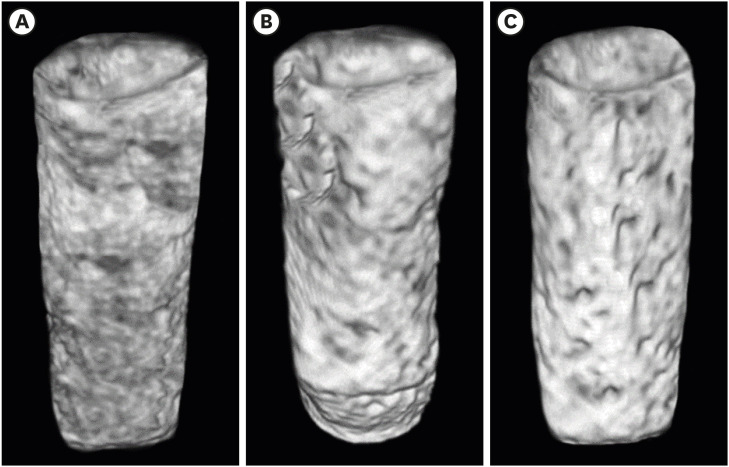
Three-dimensional models illustrating microtomographic images of the filling ability of Bio-C Repair (A), mineral trioxide aggregate repair high-plasticity (B), and intermediate restorative material (C) in CTVox software.
DISCUSSION
CONCLUSIONS
-
Funding: This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior, Brasil (CAPES) Finance Code 001, PIBIC/CNPq, and was fully supported by FAPESP (2016/00321-0, 2017/19049-0 and 2018/19665-6).
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Torres FFE, Tanomaru-Filho M, Pinto JC, Guerreiro-Tanomaru JM.
Data curation: Torres FFE, Pinto JC.
Formal analysis: Torres FFE, Tanomaru-Filho M.
Funding acquisition: Torres FFE, Pinto JC, Tanomaru-Filho M.
Investigation: Torres FFE, Tanomaru-Filho M, Pinto JC, Figueira GO.
Methodology: Torres FFE, Pinto JC, Figueira GO.
Project administration: Tanomaru-Filho M.
Resources: Tanomaru-Filho M, Guerreiro-Tanomaru JM.
Software: Torres FFE, Pinto JC, Figueira GO.
Supervision: Tanomaru-Filho M.
Validation: Torres FFE, Tanomaru-Filho M, Pinto JC.
Visualization: Torres FFE, Tanomaru-Filho M, Pinto JC.
Writing - original draft: Torres FFE, Pinto JC, Tanomaru-Filho M, Guerreiro-Tanomaru JM.
Writing - review & editing: Tanomaru-Filho M, Torres FFE.
- 1. Torabinejad M, Parirokh M, Dummer PMH. Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview - part II: other clinical applications and complications. Int Endod J 2018;51:284-317.ArticlePubMedPDF
- 2. Akbulut MB, Bozkurt DA, Terlemez A, Akman M. The push-out bond strength of BIOfactor mineral trioxide aggregate, a novel root repair material. Restor Dent Endod 2019;44:e5.ArticlePubMedPMCPDF
- 3. Prati C, Gandolfi MG. Calcium silicate bioactive cements: biological perspectives and clinical applications. Dent Mater 2015;31:351-370.ArticlePubMed
- 4. Ferreira CMA, Sassone LM, Gonçalves AS, de Carvalho JJ, Tomás-Catalá CJ, García-Bernal D, Oñate-Sánchez RE, Rodríguez-Lozano FJ, Silva EJ. Physicochemical, cytotoxicity and in vivo biocompatibility of a high-plasticity calcium-silicate based material. Sci Rep 2019;9:3933.ArticlePubMedPMCPDF
- 5. Jiménez-Sánchez MDC, Segura-Egea JJ, Díaz-Cuenca A. MTA HP Repair stimulates in vitro an homogeneous calcium phosphate phase coating deposition. J Clin Exp Dent 2019;11:e322-e326.PubMedPMC
- 6. Cintra LTA, Benetti F, de Azevedo Queiroz IO, de Araújo Lopes JM, Penha de Oliveira SH, Sivieri Araújo G, Gomes-Filho JE. Cytotoxicity, biocompatibility, and biomineralization of the new high-plasticity MTA material. J Endod 2017;43:774-778.ArticlePubMed
- 7. Tomás-Catalá CJ, Collado-González M, García-Bernal D, Oñate-Sánchez RE, Forner L, Llena C, Lozano A, Castelo-Baz P, Moraleda JM, Rodríguez-Lozano FJ. Comparative analysis of the biological effects of the endodontic bioactive cements MTA-Angelus, MTA Repair HP and NeoMTA Plus on human dental pulp stem cells. Int Endod J 2017;50(Supplement 2):e63-e72.PubMed
- 8. Benetti F, Queiroz ÍOA, Cosme-Silva L, Conti LC, Oliveira SHP, Cintra LTA. Cytotoxicity, biocompatibility and biomineralization of a new ready-for-use Bioceramic Repair material. Braz Dent J 2019;30:325-332.ArticlePubMed
- 9. López-García S, Lozano A, García-Bernal D, Forner L, Llena C, Guerrero-Gironés J, Moraleda JM, Murcia L, Rodríguez-Lozano FJ. Biological effects of new hydraulic materials on human periodontal ligament stem cells. J Clin Med 2019;8:1216.ArticlePubMedPMC
- 10. Biočanin V, Antonijević Đ, Poštić S, Ilić D, Vuković Z, Milić M, Fan Y, Li Z, Brković B, Đurić M. Marginal gaps between 2 calcium silicate and glass ionomer cements and apical root dentin. J Endod 2018;44:816-821.ArticlePubMed
- 11. Chang SW. Chemical characteristics of mineral trioxide aggregate and its hydration reaction. Restor Dent Endod 2012;37:188-193.ArticlePubMedPMC
- 12. Torres FFE, Guerreiro-Tanomaru JM, Chavez-Andrade GM, Pinto JC, Berbert FL, Tanomaru-Filho M. Micro-computed tomographic evaluation of the flow and filling ability of endodontic materials using different test models. Restor Dent Endod 2020;45:e11.ArticlePubMedPMCPDF
- 13. Torres FFE, Zordan-Bronzel CL, Guerreiro-Tanomaru JM, Chávez-Andrade GM, Pinto JC, Tanomaru-Filho M. Effect of immersion in distilled water or phosphate-buffered saline on the solubility, volumetric change and presence of voids within new calcium silicate-based root canal sealers. Int Endod J 2020;53:385-391.ArticlePubMedPDF
- 14. Zordan-Bronzel CL, Esteves Torres FF, Tanomaru-Filho M, Chávez-Andrade GM, Bosso-Martelo R, Guerreiro-Tanomaru JM. Evaluation of physicochemical properties of a new calcium silicate-based sealer, Bio-C sealer. J Endod 2019;45:1248-1252.ArticlePubMed
- 15. Darvell BW, Wu RC. “MTA”-an hydraulic silicate cement: review update and setting reaction. Dent Mater 2011;27:407-422.ArticlePubMed
- 16. Silva Almeida LH, Moraes RR, Morgental RD, Pappen FG. Are premixed calcium silicate-based endodontic sealers comparable to conventional materials? a systematic review of in vitro studies. J Endod 2017;43:527-535.ArticlePubMed
- 17. International Organization for Standardization. ISO 6876: dental root canal sealing materials. Geneva: International Organization for Standardization; 2012.
- 18. Torres FFE, Bosso-Martelo R, Espir CG, Cirelli JA, Guerreiro-Tanomaru JM, Tanomaru-Filho M. Evaluation of physicochemical properties of root-end filling materials using conventional and micro-CT tests. J Appl Oral Sci 2017;25:374-380.ArticlePubMedPMC
- 19. Guo YJ, Du TF, Li HB, Shen Y, Mobuchon C, Hieawy A, Wang ZJ, Yang Y, Ma J, Haapasalo M. Physical properties and hydration behavior of a fast-setting bioceramic endodontic material. BMC Oral Health 2016;16:23.ArticlePubMedPMC
- 20. Camilleri J, Grech L, Galea K, Keir D, Fenech M, Formosa L, Damidot D, Mallia B. Porosity and root dentine to material interface assessment of calcium silicate-based root-end filling materials. Clin Oral Investig 2014;18:1437-1446.ArticlePubMedPDF
- 21. Gandolfi MG, Siboni F, Botero T, Bossù M, Riccitiello F, Prati C. Calcium silicate and calcium hydroxide materials for pulp capping: biointeractivity, porosity, solubility and bioactivity of current formulations. J Appl Biomater Funct Mater 2015;13:43-60.ArticlePubMedPDF
- 22. Kim S, Kratchman S. Modern endodontic surgery concepts and practice: a review. J Endod 2006;32:601-623.ArticlePubMed
- 23. Torres FF, Jacobs R, EzEldeen M, Guerreiro-Tanomaru JM, Dos Santos BC, Lucas-Oliveira É, Bonagamba TJ, Tanomaru-Filho M. Micro-computed tomography high resolution evaluation of dimensional and morphological changes of 3 root-end filling materials in simulated physiological conditions. J Mater Sci Mater Med 2020;31:14.ArticlePubMedPDF
- 24. Hashem AA, Hassanien EE. ProRoot MTA, MTA-Angelus and IRM used to repair large furcation perforations: sealability study. J Endod 2008;34:59-61.PubMed
- 25. Övsay E, Kaptan RF, Şahin F. The repair of furcal perforations in different diameters with Biodentine, MTA, and IRM repair materials: a laboratory study using an E. Faecalis leakage model. BioMed Res Int 2018;2018:5478796.PubMedPMC
- 26. Lertmalapong P, Jantarat J, Srisatjaluk RL, Komoltri C. Bacterial leakage and marginal adaptation of various bioceramics as apical plug in open apex model. J Investig Clin Dent 2019;10:e12371.ArticlePubMedPDF
- 27. Tanomaru-Filho M, Torres FFE, Bosso-Martelo R, Chávez-Andrade GM, Bonetti-Filho I, Guerreiro-Tanomaru JM. A novel model for evaluating the flow of endodontic materials using micro-computed tomography. J Endod 2017;43:796-800.ArticlePubMed
- 28. Dorileo MC, Pedro FL, Bandeca MC, Guedes OA, Villa RD, Borges AH. Comparative analysis of physicochemical properties of root perforation sealer materials. Restor Dent Endod 2014;39:201-209.ArticlePubMedPMC
- 29. Elyassi Y, Moinzadeh AT, Kleverlaan CJ. Characterization of leachates from 6 root canal sealers. J Endod 2019;45:623-627.ArticlePubMed
- 30. Song YS, Choi Y, Lim MJ, Yu MK, Hong CU, Lee KW, Min KS. In vitro evaluation of a newly produced resin-based endodontic sealer. Restor Dent Endod 2016;41:189-195.ArticlePubMedPMCPDF
- 31. Guimarães BM, Prati C, Duarte MAH, Bramante CM, Gandolfi MG. Physicochemical properties of calcium silicate-based formulations MTA Repair HP and MTA Vitalcem. J Appl Oral Sci 2018;26:e2017115.PubMedPMC
- 32. Singh S, Podar R, Dadu S, Kulkarni G, Purba R. Solubility of a new calcium silicate-based root-end filling material. J Conserv Dent 2015;18:149-153.ArticlePubMedPMC
REFERENCES
Tables & Figures
REFERENCES
Citations

- Comparative evaluation of sealing potential of mineral trioxide aggregate, biodentine, and bio-C repair in furcation perforations: A glucose penetration study
Ashwija Shetty, Hajira Anjum Sultana, A. Srirekha, C. Champa, Suditi Pal, V. Sahithi
Journal of Conservative Dentistry and Endodontics.2025; 28(2): 144. CrossRef - Evaluation of volumetric and surface stability of calcium silicate-based repair cements at different pHs
Ana Cristina Padilha Janini, Débora Leticia Bittencourt Leite Alves, Victor Augusto Benedicto dos Santos, Brenda Fornazaro Moraes, Nilvan Alves da Silva, Matheus Barros-Costa, Luciano Augusto Cano Martins, Francisco Haiter Neto, Marina Angélica Marciano
Clinical Oral Investigations.2025;[Epub] CrossRef - Bioceramics in Endodontics: Limitations and Future Innovations—A Review
Peramune Arachchilage Amila Saman Prasad Kumara, Paul Roy Cooper, Peter Cathro, Maree Gould, George Dias, Jithendra Ratnayake
Dentistry Journal.2025; 13(4): 157. CrossRef - Physicochemical properties and periodontal ligament stem cell response to NeoMTA 2
Danilo Cassiano Ferraz, Jáder Camilo Pinto, Ariadne Letra, Renato Menezes Silva, Letícia Chaves de Souza, Juliane Maria Guerreiro-Tanomaru, Mario Tanomaru-Filho
Clinical Oral Investigations.2025;[Epub] CrossRef - Effect of Ultrasonic Condensation Time on Void Formation and Microhardness of Well-RootTM PT Apical Plugs in 3D-Printed Immature Teeth
Krasimir Hristov, Ralitsa Bogovska-Gigova
Materials.2025; 18(21): 4835. CrossRef - Effect of pH on the solubility and volumetric change of ready-to-use Bio-C Repair bioceramic material
Luana Raphael da SILVA, Jader Camilo PINTO, Juliane Maria GUERREIRO-TANOMARU, Mário TANOMARU-FILHO
Brazilian Oral Research.2024;[Epub] CrossRef - Effect of blood and artificial saliva contamination on marginal adaptation and sealing ability of different retrograde filling materials: A comparative analysis
Yantrapragada Lakshmi Sunanda, Krishna Prasad Parvathaneni, T. B. V. G. Raju, Abitha Seshadri, Gowtam Dev Dondapati
Journal of Conservative Dentistry and Endodontics.2024; 27(7): 743. CrossRef - Marginal Adaptation and Porosity of a Novel MTA Brand Applied as Root-End Filling Material: A Micro-CT Study
Yaneta Kouzmanova, Ivanka Dimitrova
Applied Sciences.2024; 14(7): 2758. CrossRef - Volumetric change of calcium silicate-based repair materials in a simulated inflammatory environment: A micro-computed tomography study
Giovanna da Cunha Mendonça, Karina Ines Medina Carita Tavares, Airton Oliveira Santos-Junior, Fernanda Ferrari Esteves Torres, Jáder Camilo Pinto, Juliane Maria Guerreiro-Tanomaru, Mário Tanomaru-Filho
Journal of Conservative Dentistry and Endodontics.2024; 27(8): 817. CrossRef - Biocompatibility, bioactivity, porosity, and sealer/dentin interface of bioceramic ready-to-use sealers using a dentin-tube model
Rafaela Nanami Handa Inada, Evelin Carine Alves Silva, Camila Soares Lopes, Marcela Borsatto Queiroz, Fernanda Ferrari Esteves Torres, Guilherme Ferreira da Silva, Paulo Sérgio Cerri, Juliane Maria Guerreiro–Tanomaru, Mário Tanomaru-Filho
Scientific Reports.2024;[Epub] CrossRef - Healing the Open Apex: A Case Report on Innovative Apexogenesis of a Maxillary Molar Using Bio-C Repair
Ashwija Shetty, Hajira A Sultana, Keerthan B V, Nithin S Reddy
Cureus.2024;[Epub] CrossRef - Evaluation the Marginal Adaptation for the Bio C Repair and Other Root end Filling Material by Using Scanning Electron Microscope (A Comparative In Vitro Study)
Fatimah HAMADHİ, Zainab M.
Cumhuriyet Dental Journal.2023; 26(3): 261. CrossRef - Biocompatibility, bioactive potential, porosity, and interface analysis calcium silicate repair cements in a dentin tube model
Rafaela Nanami Handa Inada, Marcela Borsatto Queiroz, Camila Soares Lopes, Evelin Carine Alves Silva, Fernanda Ferrari Esteves Torres, Guilherme Ferreira da Silva, Juliane Maria Guerreiro-Tanomaru, Paulo Sérgio Cerri, Mário Tanomaru-Filho
Clinical Oral Investigations.2023; 27(7): 3839. CrossRef - A new proposal for evaluating of the solubility of bioceramic materials in dentin tubes after immersion in PBS: a laboratory investigation
Giovanna da Cunha MENDONÇA, Karina Ines Medina Carita TAVARES, Airton Oliveira SANTOS-JUNIOR, Jáder Camilo PINTO, Juliane Maria GUERREIRO-TANOMARU, Mário TANOMARU-FILHO
Revista de Odontologia da UNESP.2023;[Epub] CrossRef

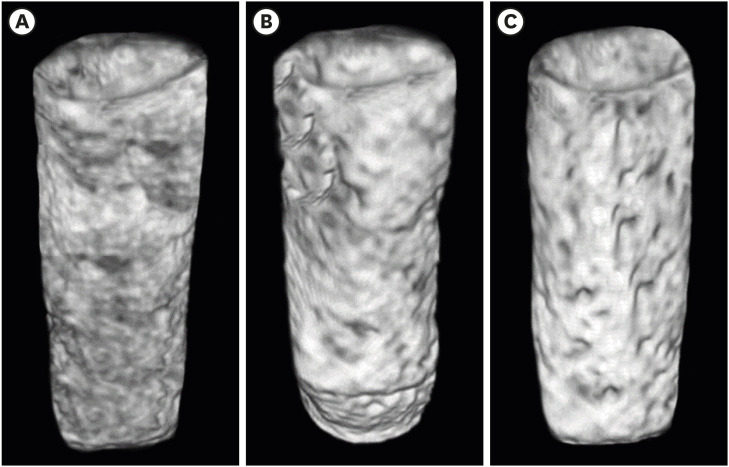
Figure 1
Figure 2
The manufacturers, composition, and proportions of the endodontic materials used in this study
| Material | Manufacturer | Composition | Proportion |
|---|---|---|---|
| Bio-C Repair | Angelus, Londrina, PR, Brazil | Calcium silicate, calcium aluminate, calcium oxide, zirconium oxide, iron oxide, silicon dioxide, dispersing agent | Ready to use |
| MTA HP | Angelus, Londrina, PR, Brazil | Powder: tricalcium silicate, dicalcium silicate, tricalcium aluminate, calcium oxide, calcium tungstate | 1 g powder: 300 µL liquid |
| Liquid: water and plasticizer | |||
| IRM | Dentsply DeTrey, Konstanz, Germany | Powder: zinc oxide, polymethyl methacrylate | 1 g powder: 200 µL liquid |
| Liquid: eugenol, acetic acid |
MTA HP, mineral trioxide aggregate repair high-plasticity; IRM, intermediate restorative material.
Results for filling ability and volumetric changes of the endodontic materials
| Test/material | Bio-C Repair | MTA HP | IRM |
|---|---|---|---|
| Filling ability (%) | 97.30 ± 2.01a | 89.80 ± 4.94b | 92.30 ± 5.37a,b |
| Volumetric change (%) | −2.36 ± 0.75b | −3.67 ± 0.86a | −2.10 ± 0.83b |
The values are mean ± standard deviation. Different lowercase letters on the same line indicate statistically significant differences between the different cements (p < 0.05) (1-way analysis of variance and Tukey test).
MTA HP, mineral trioxide aggregate repair high-plasticity; IRM, intermediate restorative material.
MTA HP, mineral trioxide aggregate repair high-plasticity; IRM, intermediate restorative material.
The values are mean ± standard deviation. Different lowercase letters on the same line indicate statistically significant differences between the different cements (
MTA HP, mineral trioxide aggregate repair high-plasticity; IRM, intermediate restorative material.

 KACD
KACD
 ePub Link
ePub Link Cite
Cite

