Abstract
The replacement of missing teeth, especially in the anterior region, is an essential part of dental practice. Fiber-reinforced composite resin bridges are a conservative alternative to conventional fixed dental prostheses or implants. It is a minimally invasive, reversible technique that can be completed in a single visit. The two cases presented herein exemplify the treatment of root-fractured anterior teeth with a natural pontic immediately after extraction.
-
Keywords: Bridges; Fiber-reinforced composite; Immediate restoration; Root fracture
INTRODUCTION
After trauma occurs, a root-fractured tooth can be healed through a proper diagnosis and emergency treatment. However, sometimes such a tooth cannot be treated appropriately and must be extracted. Implant-supported crowns or fixed dental prostheses (FDPs) are the most common treatment options. However, FDPs require preparation of the adjacent intact teeth [
1,
2]. Additionally, implant-supported prostheses may not be the best solution due to bone resorption, an inadequate volume of bone, or the unwillingness of the patient to undergo implant surgery because of its inconvenience and/or cost [
3].
Fiber-reinforced composite resin (FRC) bridges are a conservative alternative method for the replacement of missing teeth. The abutment teeth can be conserved with a minimally invasive preparation, thereby ensuring that the technique is reversible, and FRC bridge treatment can be performed in a single visit [
4]. The following 2 cases, in which a single mandibular anterior tooth had a fractured root, exemplify treatment with a FRC bridge using a natural pontic immediately after extraction.
CASE REPORT
Case 1
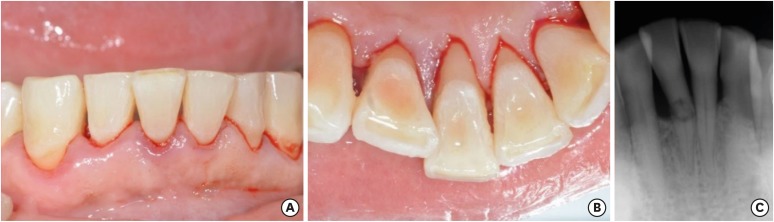
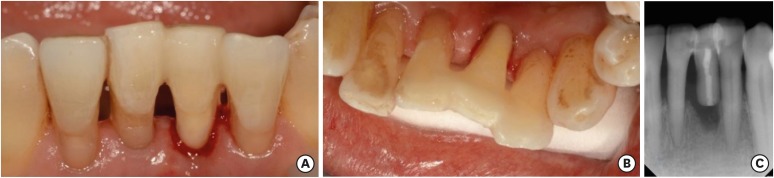
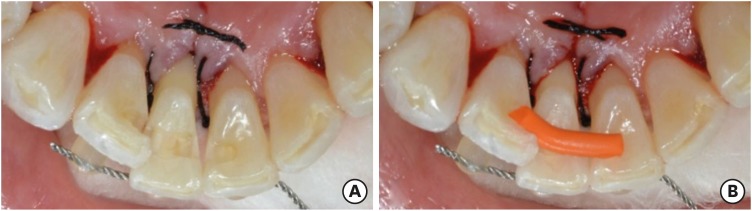
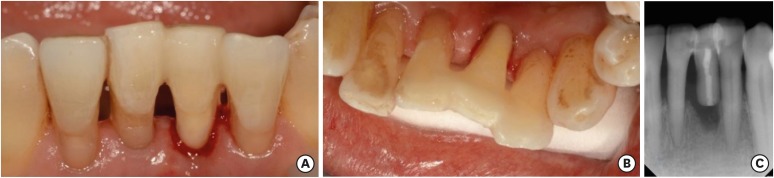
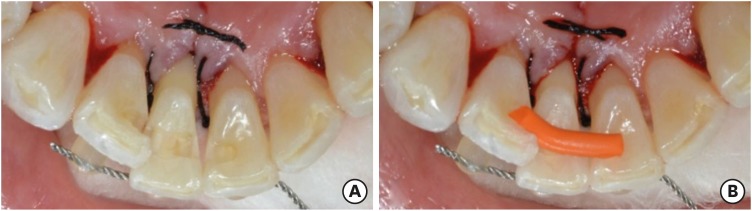
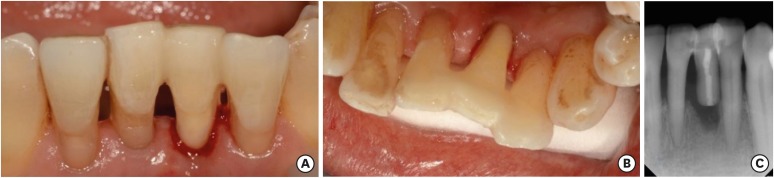
A 52-year-old man visited the Department of Conservative Dentistry because of mobility of the right mandibular central incisor (tooth #41) after it was smashed on a door 6 months previously. The tooth showed degree 3 mobility and slight tenderness on percussion. Clinical and radiographic examinations revealed that the tooth was root-fractured at the cervical third (
Figure 1).
Figure 1Preoperative view. (A) Intraoral photograph (labial view); (B) intraoral photograph (lingual view); (C) periapical view.
The tooth needed extraction, and an FDP or implant would have been the conventional treatment options. However, the patient did not want a surgical procedure for an implant or excessive preparation of the intact adjacent teeth for an FDP. Therefore, a direct FRC bridge was chosen with consent of the patient.
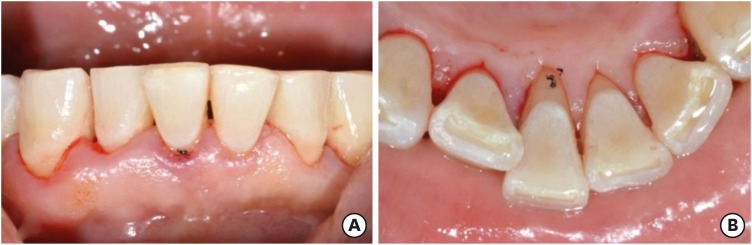
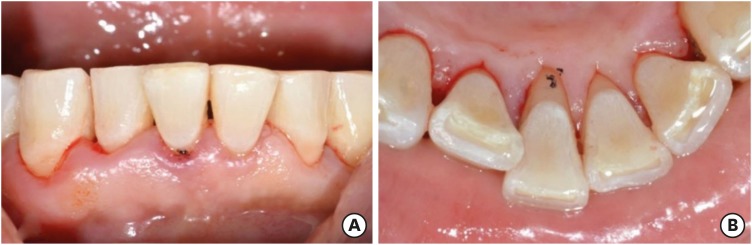
First of all, to mark the gingiva level, a black dot was made on the labial and lingual surfaces of the tooth (
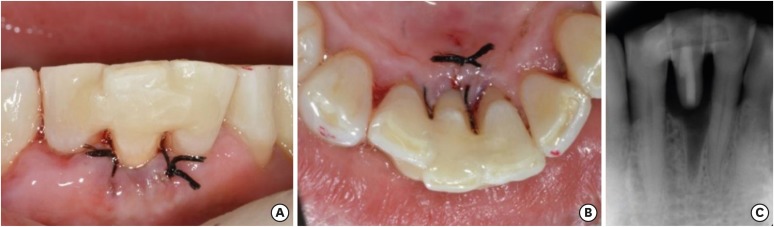
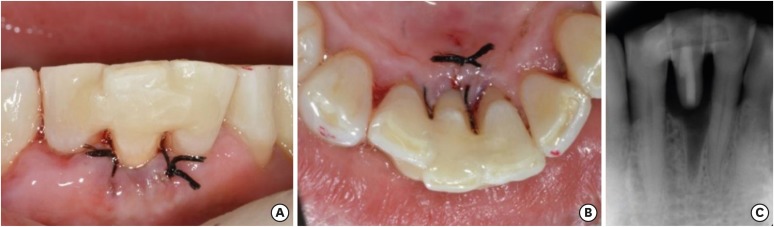
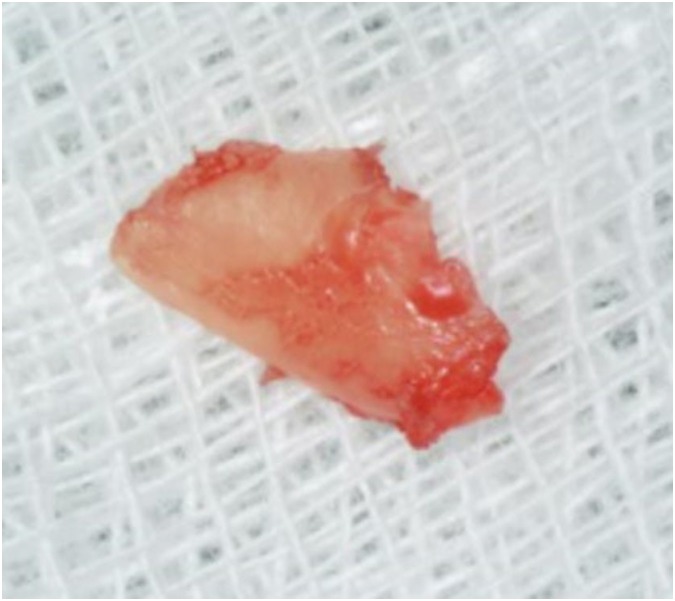
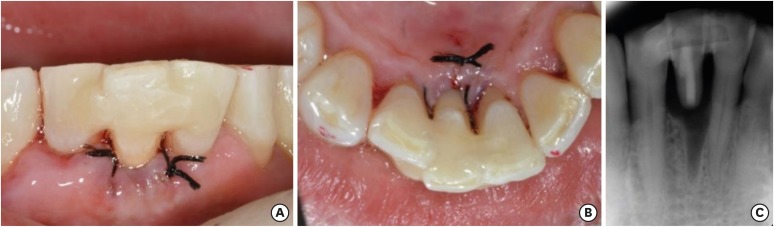
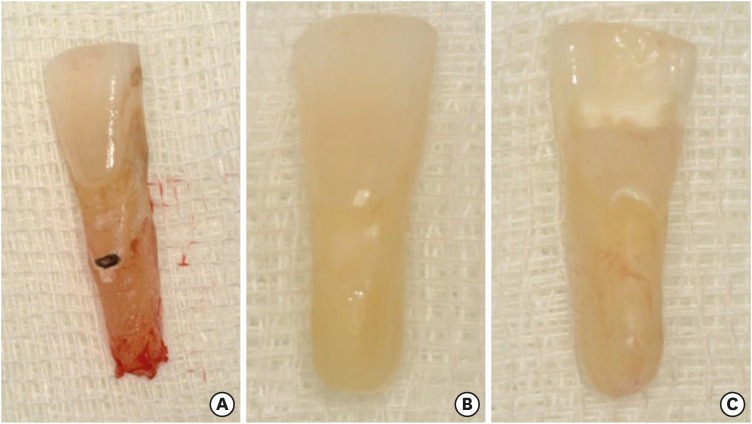
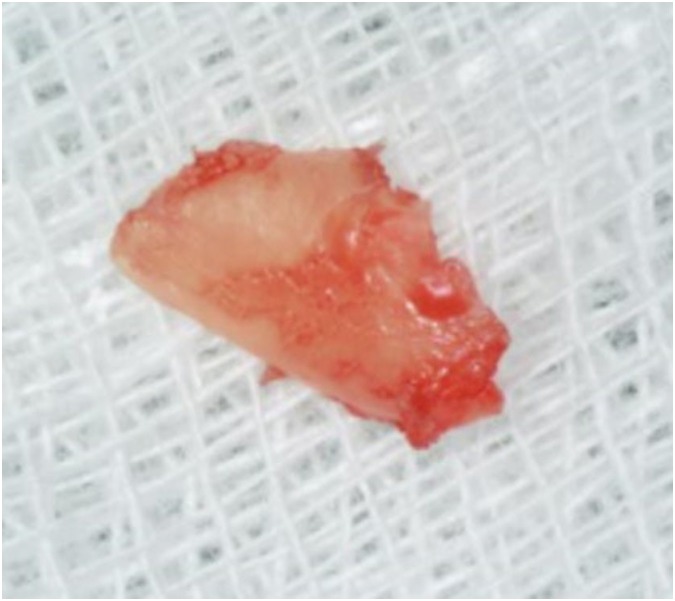
Figure 2). Then, the coronal fragment and fractured root were extracted under local anesthesia (
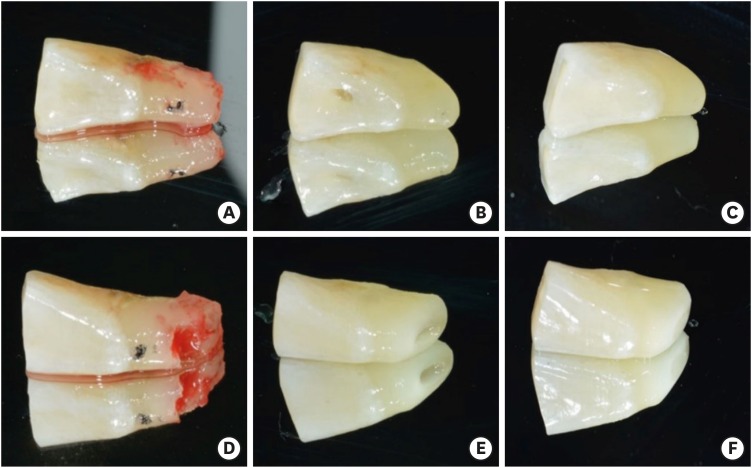
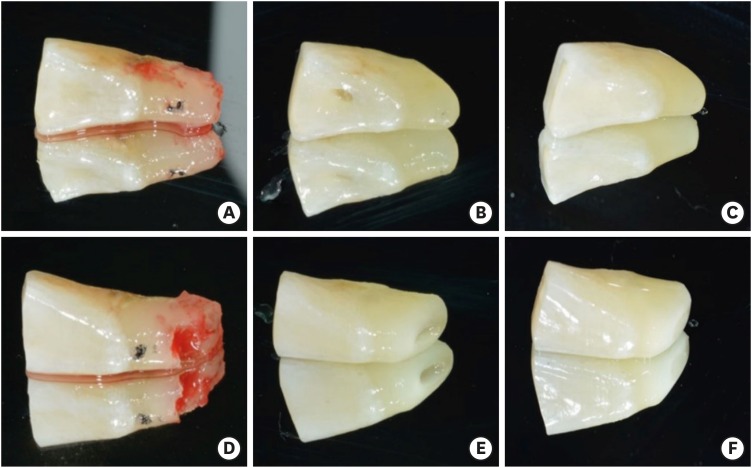
Figure 3). An access cavity for the coronal fragment was formed on the lingual surface of the tooth using a high-speed #330 bur (H7.314.008, Komet, Lemgo, Germany). The root canal was enlarged using a Gates-Glidden drill (MANI, Tochigi, Japan). Next, the coronal fragment was soaked in 5% sodium hypochlorite for 5 minutes. The root canal was filled with a resin-modified glass ionomer (Fuji II LC, GC, Tokyo, Japan) and polished using a white stone (Dura-White Stones, Shofu, Kyoto, Japan) and One-gloss (Midi, Shofu) (
Figure 4). The coronal fragment was reinserted in the extraction socket and fixed temporarily using G-fix (GC) and a twisted wire (0.0215″ stainless steel wire, American Orthodontics, Sheboygan, WI, USA). The torn gingiva during root fragment removal was ligated with 4-0 black silk (AILEE, Busan, Korea) (
Figure 5). Space for a reinforcing fiber was made using a high-speed tapered diamond bur (SF-12, MANI) on the middle of the lingual side from the mesial aspect of tooth #42 to the distal aspect of tooth #31, across tooth #41. The depth of the preparation was approximately 1.0 mm to make adequate space for the fiber and composite resin. The length of the cavity was measured using a Wedjet (Coltene/Whaledent, Alstatten, Switzerland) and Everstick C&B fiber (GC) was cut to that length (
Figure 6). A 37% phosphoric acid gel (DenFil Etchant-37, Vericom, Anyang, Korea) was applied to the enamel for 20 seconds, rinsed off, and then gently dried. Singlebond Universal (3M ESPE, St. Paul, MN, USA) was applied to the enamel and dentin, dried gently for 5 seconds, then light-cured for 10 seconds using a LED curing light (G-Light, GC) A thin layer of flowable composite was placed on the preparation site and the fiber was inserted using hand instruments and then light-cured. Composite resin (Filtek Z-350 XT, 3M ESPE) was packed on the fiber and interproximal surface. Because of crowding of tooth #41, resin was packed on the buccal side of the pontic and adjacent teeth to reinforce the connector area. Areas of premature contact or lateral excursion contact on the pontic site were removed during occlusal adjustment. After occlusal adjustment using a diamond finishing bur, the surfaces were polished with One-gloss and an Astro-brush (Ivoclar Vivadent, Schaan, Liechtenstein) (
Figure 7). The stiches were removed after 1 week.
Figure 2A black dot was made to mark the gingiva level. (A) Intraoral photograph (labial view); (B) intraoral photograph (lingual view).
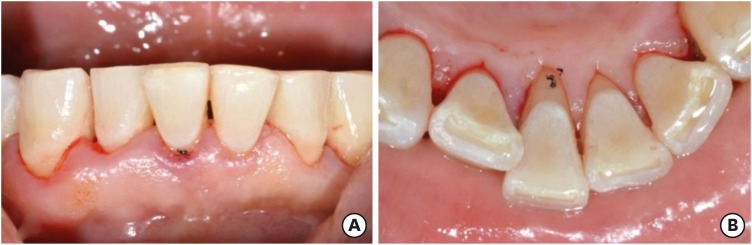
Figure 3Extracted retained root.
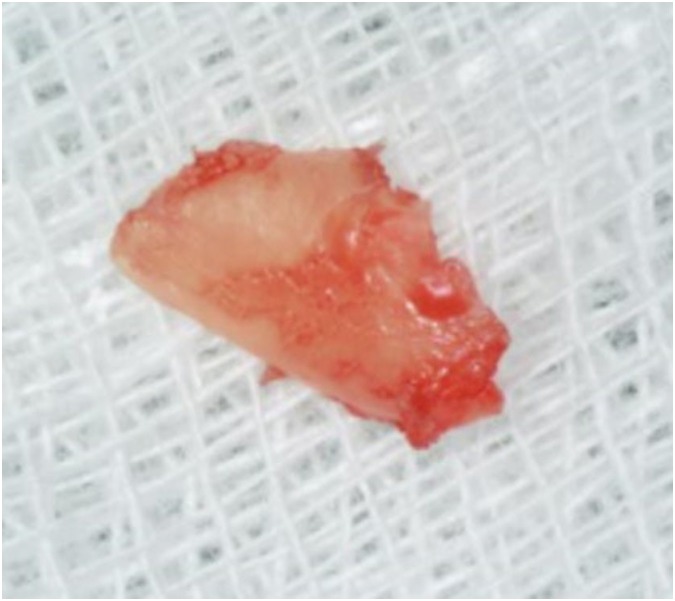
Figure 4Coronal fragment of tooth #41 as a natural tooth pontic. (A, D) Extracted coronal fragment; (B, E) prepared coronal fragment; (C, F) polished coronal fragment; (A-C) lingual view; (D-F) labial view.
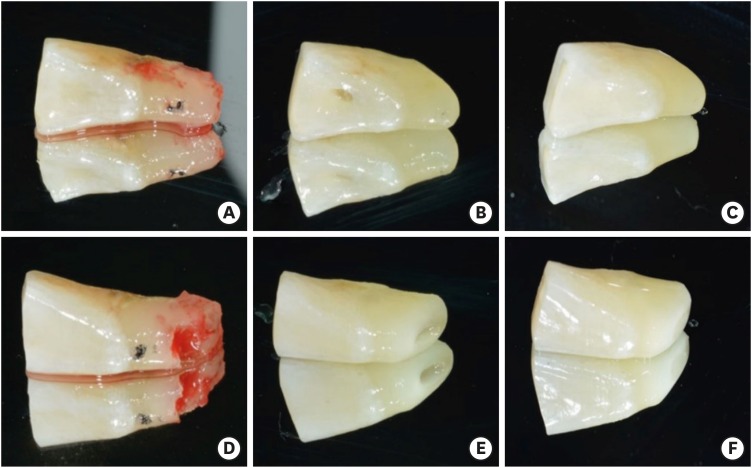
Figure 5Labial view after temporary fixation.

Figure 6Lingual view of tooth preparation. (A) Preparation of space for fiber extending from the mesial aspect of tooth #42 to the distal aspect of tooth #31 across tooth #41; (B) measurement of the span using a Wedjet.
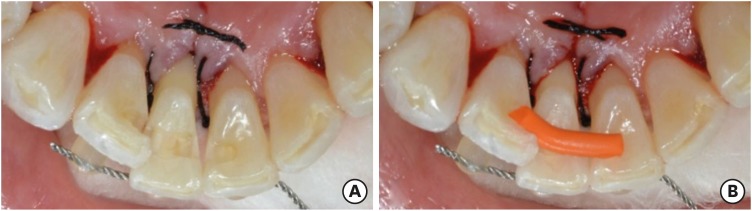
Figure 7Postoperative view. (A) Intraoral photograph (labial view); (B) intraoral photograph (lingual view); (C) periapical view.
At a 10-month recall examination, the pontic and abutment teeth were in sound condition. No specific discomfort was reported, and the patient was satisfied with having saved his natural tooth. Periapical radiography was taken and it showed bony healing of the extraction socket (
Figure 8).
Figure 8At a 10-month recall check. (A) Intraoral photograph (labial view); (B) intraoral photograph (lingual view); (C) periapical view.

Case 2
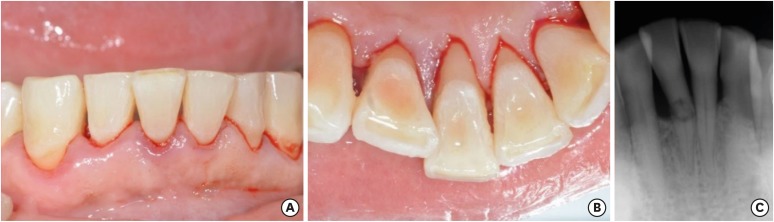
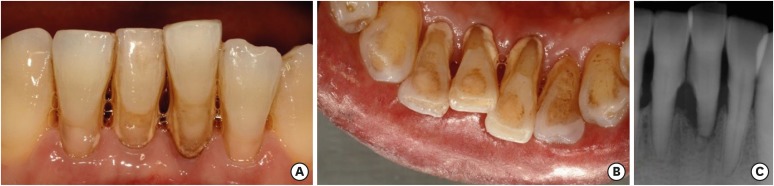
A 66-year-old man visited our department because of severe mobility of the left mandibular central incisor (tooth #31). The tooth showed degree 3 mobility and slight tenderness on percussion. Clinical and radiographic examinations revealed that the tooth was root-fractured at the apical third. The tooth was diagnosed with apical root fracture and chronic periodontitis (
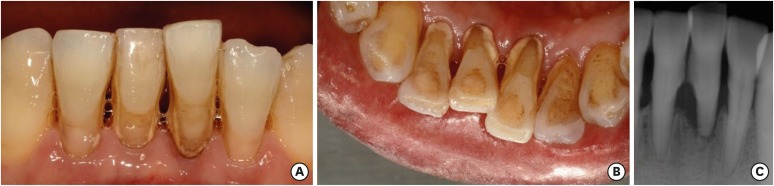
Figure 9). The tooth needed extraction, but patient was concerned about the high costs of an implant or fixed partial denture. Therefore, a direct FRC bridge was chosen as a treatment and patient consent was obtained.
Figure 9Preoperative view. (A) Intraoral photograph (labial view); (B) intraoral photograph (lingual view); (C) periapical view.
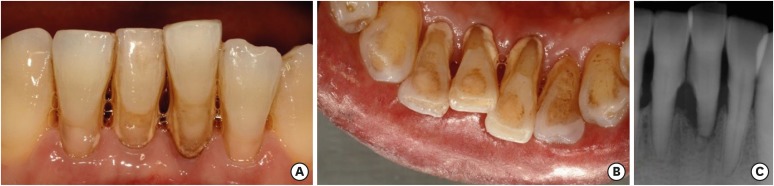
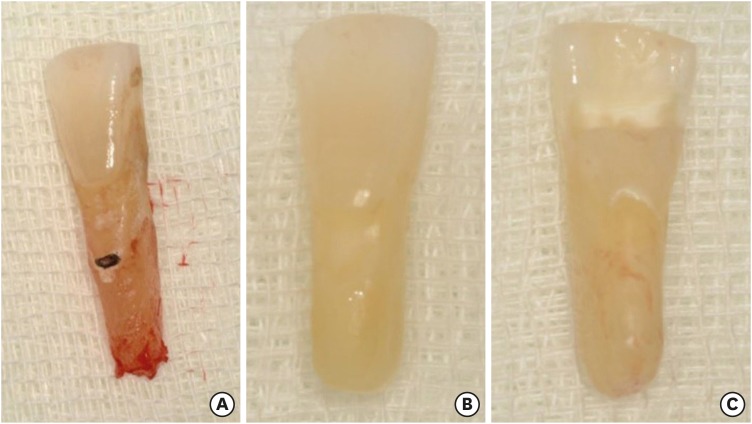
First, heavy calculus of the mandibular anterior teeth was removed before the procedure. After removal of the tooth, a direct FRC bridge was made in the same way as described above for case 1 (
Figures 10,
11,
12).
Figure 10#31 Coronal fragment as a natural tooth pontic. (A) Extracted coronal fragment; (B) polished coronal fragment (labial view); (C) polished coronal fragment (lingual view).
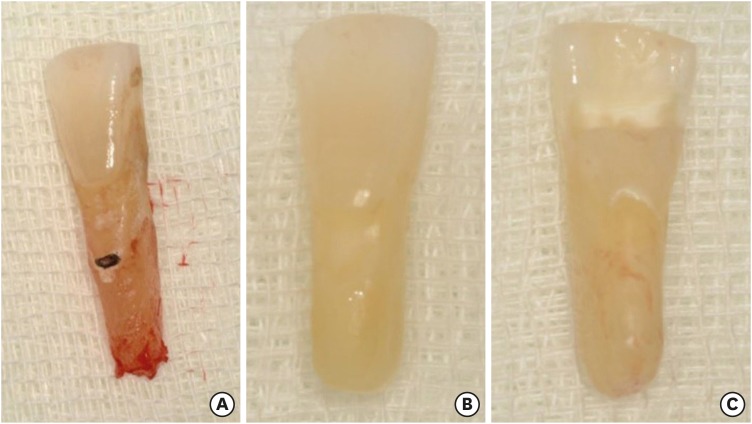
Figure 11Lingual view after the abutment preparation was done.

Figure 12Postoperative view. (A) Intraoral photograph (labial view); (B) intraoral photograph (lingual view); (C) periapical view.
The pontic and abutment teeth were in good condition at an 8-month recall examination. No specific discomfort was reported, although some calculus was present on the mandibular anterior tooth. Periapical radiography was taken and it showed bony healing of the extraction socket (
Figure 13).
Figure 13At an 8-month recall check.

DISCUSSION
Two perspectives exist regarding the benefits of an FRC bridge: that of the dentist and that of the patient. For the dentist, minimal invasiveness is the main advantage of an FRC bridge. Initially using the least invasive treatment preserves the maximum possible amount of tooth substance, which helps to conserve dental hard tissues for any further possible treatments. Furthermore, by using an extracted natural tooth, favorable esthetics and a natural feeling can be achieved, resulting in high patient satisfaction. For the patient, the possibility of receiving a single-visit treatment and avoiding removable devices is satisfactory, as removable dental prostheses usually lead to lower satisfaction than FDPs. Furthermore, an FRC bridge is a less expensive, painless treatment option, unlike an implant or FDP [
5].
Regarding the survival rate of FRC bridges, Frese
et al. [
6] reported that FRC bridges showed a promising survival rate and good quality after a median follow-up period of 4.5 years, thereby indicating that FRC bridges are a reliable treatment option for the restoration of single missing teeth in the anterior area. Recently, a systematic review investigating the longevity of FRC bridges was published. That study included 9 studies, involving the placement of 592 FRC bridges in 463 patients. The follow-up periods ranged between 2 months and 8 years, and overall survival rate was 94.4% at 4.8 years [
7]. The majority of failures were due to debonding and delamination of veneering composites [
8]. In most cases, these failures could be repaired and the repairability of FRC bridges could lengthen the longevity of the restoration.
The extraction of a tooth results in bone loss in the horizontal and vertical dimension, mainly on the buccal aspect. Dimensional changes in alveolar bone after extraction have been reported to involve a mean loss of about 4.0 mm in ridge width and 1.5 mm in height during first the 3 months of healing [
9]. This phenomenon makes it challenging to restore the anterior tooth esthetically and naturally. It is necessary to strive to preserve the periodontal tissue. By inserting an ovate pontic into the extraction socket immediately after extraction, a gingival embrasure forms and the papilla can be maintained [
10]. Furthermore, a highly polished ovate pontic stabilizes the fibrin clot, acts as a chamber matrix for the formation of stratified squamous epithelium, and mechanically supports the soft tissue [
11]. In these 2 cases, immediate insertion of an ovate pontic made it possible not only to preserve the soft tissue, but also to promote the healing of hard tissue.
In these cases, the cavity was lingually prepared to provide space for the fiber and composite resin. If the abutment teeth are intact (no caries or restorations), controversy exists regarding the necessity of a preparation. Perea-Lowery and Vallittu [
12] stated that it is important to ensure a macro-mechanical interlocking of a natural tooth pontic to the FRC framework to diminish the magnitude of tensile stresses at the bonding interface. Macro-mechanical interlocking is ensured by grinding a groove into the pontic tooth to resist dislodgement forces. In addition, according to the manufacturer's manual, the fiber must always be covered entirely with composite resin. For the surface-retained type of FRC bridge, a considerable amount of resin should be filled to ensure sufficient retention of the restoration and to fully cover the fiber. This can cause over-contouring on the lingual side of the abutment and pontic tooth, which can result in poor oral hygiene. Furthermore, the patient may feel discomfort or irritation due to an over-contoured restoration. As a result, the intra-coronal restoration type was selected to ensure proper fracture resistance and better maintenance of the restoration.
Xie
et al. [
13] stated that adding one more fiber bundle, perpendicular to the main framework, provided support to the cusps of the pontic most effectively, as it increased the load-bearing capacity of the framework. Additional fibers in the cervico-incisal direction could maximize the retention of the pontic, which is wholly made from composite resin. Doing so could also arrest crack development and propagation within the composite resin under loading conditions [
12]. However, in these cases, a natural tooth pontic was used after an extraction. Therefore, an additional preparation for fibers in the cervico-incisal direction would not be needed.
Malmstrom
et al. [
14] reported high levels of patient satisfaction when assessed by a visual analogue scale, with a mean score of more than 80 mm, in regards to prosthesis appearance, color, chewing ability, and overall satisfaction at a 2-year follow-up visit. Even if a limitation of that study is the lack of a comparison between FRC bridges and FDPs or implants, the FRC bridges led to considerable patient satisfaction. The benefits of utilizing the natural tooth, minimal invasiveness, and lower cost could explain these results.
Some risk factors may decrease the longevity of an FRC bridge. Occlusion and limited vertical space seem to represent major risk factors for damage to FRC bridges [
5]. By increasing the occlusal thickness of the pontic, the load-bearing capacity of the FRC bridge may be increased [
15]. In both of the cases described herein, the inlay-retained type of FRC bridge was used to obtain adequate space for the fiber and composite resin. However, Aktas
et al. [
16] suggested that different preparation designs (inlay-retained and surface-retained) had no significant effect on the fracture strength of FRC bridges in the anterior region. Controversy remains regarding which type of framework design is better. Increased mobility of the abutment teeth appears to increase the risk for debonding of intra-coronal retainers and periodontal splints. Therefore, the abutment teeth must be carefully examined and proper patient selection is mandatory. It should be mentioned that the patients strictly observed the oral hygiene instructions. Periodic recall checks and supportive periodontal therapy are also needed. The oral environment and oral hygiene could affect the treatment outcome of any dental treatment in patients with an elevated risk for dental caries and periodontal disease.
CONCLUSIONS
The loss of anterior teeth can be psychologically and socially damaging. FRC bridges are a minimally invasive, esthetically favorable, and cost-effective method for the replacement of missing teeth. Furthermore, using the extracted natural tooth as a pontic offers the benefits of it being the right size, shape, and color, producing good esthetic and functional results. Consequently, FRC bridges can be a good alternative method for rehabilitating root-fractured teeth that need extraction.
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Cho KM.
Data curation: Heo G.
Formal analysis: Kim JW, Cho KM, Park SH.
Funding acquisition: Cho KM.
Investigation: Heo G.
Methodology: Cho KM.
Project administration: Park SH.
Resources: Heo G.
Software: Lee EH.
Supervision: Cho KM.
Validation: Park SH.
Visualization: Lee EH.
Writing - original draft: Heo G.
Writing - review & editing: Kim JW, Cho KM, Park SH.
REFERENCES
- 1. Kim H, Song MJ, Shin SJ, Lee Y, Park JW. Esthetic rehabilitation of single anterior edentulous space using fiber-reinforced composite. Restor Dent Endod 2014;39:220-225.ArticlePubMedPMC
- 2. Kumar KP, Nujella SK, Gopal SS, Roy KK. Immediate esthetic rehabilitation of periodontally compromised anterior tooth using natural tooth as pontic. Case Rep Dent 2016;2016:8130352.ArticlePubMedPMCPDF
- 3. Kermanshah H, Motevasselian F. Immediate tooth replacement using fiber-reinforced composite and natural tooth pontic. Oper Dent 2010;35:238-245.ArticlePubMedPDF
- 4. Khetarpal A, Talwar S, Verma M. Creating a single-visit, fibre-reinforced, composite resin bridge by using a natural tooth pontic: a viable alternative to a PFM bridge. J Clin Diagn Res 2013;7:772-775.ArticlePubMedPMC
- 5. Vallittu PK, Shinya A, Baraba A, Kerr I, Keulemans F, Kreulen C, Lassila L, Malmstrom H, Novotny R, Peumans M, Van Rensburg J, Wolff D, Özcan M. Fiber-reinforced composites in fixed prosthodontics-Quo vadis? Dent Mater 2017;33:877-879.ArticlePubMed
- 6. Frese C, Schiller P, Staehle HJ, Wolff D. Fiber-reinforced composite fixed dental prostheses in the anterior area: a 4.5-year follow-up. J Prosthet Dent 2014;112:143-149.ArticlePubMed
- 7. Ahmed KE, Li KY, Murray CA. Longevity of fiber-reinforced composite fixed partial dentures (FRC FPD)-systematic review. J Dent 2017;61:1-11.ArticlePubMed
- 8. Kumbuloglu O, Özcan M. Clinical survival of indirect, anterior 3-unit surface-retained fibre-reinforced composite fixed dental prosthesis: up to 7.5-years follow-up. J Dent 2015;43:656-663.ArticlePubMed
- 9. Van der Weijden F, Dell'Acqua F, Slot DE. Alveolar bone dimensional changes of post-extraction sockets in humans: a systematic review. J Clin Periodontol 2009;36:1048-1058.ArticlePubMed
- 10. Spear FM, Cooney JP. Restorative interrelationships. In: Newman M, Takei H, Klokkevold P, Carranza F, editors. Carranza's clinical periodontology. 12th ed. St. Louis, MO: Saunders Elsevier; 2014. p. Chapter 67.
- 11. Steigmann M, Cooke J, Wang HL. Use of the natural tooth for soft tissue development: a case series. Int J Periodontics Restorative Dent 2007;27:603-608.PubMed
- 12. Perea-Lowery L, Vallittu PK. Framework design and pontics of fiber-reinforced composite fixed dental prostheses - an overview. J Prosthodont Res 2018;62:281-286.ArticlePubMed
- 13. Xie Q, Lassila LV, Vallittu PK. Comparison of load-bearing capacity of direct resin-bonded fiber-reinforced composite FPDs with four framework designs. J Dent 2007;35:578-582.ArticlePubMed
- 14. Malmstrom H, Dellanzo-Savu A, Xiao J, Feng C, Jabeen A, Romero M, Huang J, Ren Y, Yunker MA. Success, clinical performance and patient satisfaction of direct fibre-reinforced composite fixed partial dentures - a two-year clinical study. J Oral Rehabil 2015;42:906-913.ArticlePubMedPDF
- 15. Perea L, Matinlinna JP, Tolvanen M, Lassila LV, Vallittu PK. Fiber-reinforced composite fixed dental prostheses with various pontics. J Adhes Dent 2014;16:161-168.PubMed
- 16. Aktas G, Basara EG, Sahin E, Uctasli S, Vallittu PK, Lassila LV. Effects of different cavity designs on fracture load of fiber-reinforced adhesive fixed dental prostheses in the anterior region. J Adhes Dent 2013;15:131-135.PubMed
 , Eun-Hye Lee2
, Eun-Hye Lee2 , Jin-Woo Kim1
, Jin-Woo Kim1 , Kyung-Mo Cho1
, Kyung-Mo Cho1 , Se-Hee Park1
, Se-Hee Park1








 KACD
KACD



 ePub Link
ePub Link Cite
Cite

