Articles
- Page Path
- HOME > Restor Dent Endod > Volume 45(1); 2020 > Article
-
Research Article
Isthmuses, accessory canals, and the direction of root curvature in permanent mandibular first molars: an
in vivo computed tomography study -
Aria Chuppani Dastgerdi1
 , Manizheh Navabi2
, Manizheh Navabi2 , Vahid Rakhshan1
, Vahid Rakhshan1
-
Restor Dent Endod 2019;45(1):e7.
DOI: https://doi.org/10.5395/rde.2020.45.e7
Published online: December 12, 2019
1Department of Dental Morphology, Dental Branch, Islamic Azad University, Tehran, Iran.
2Department of Removable Prosthodontics, Dental Faculty, Tehran Medical Sciences, Islamic Azad University, Tehran, Iran.
- Correspondence to Manizheh Navabi, DDS. Academic Faculty Member, Department of Removable Prosthodontics, Dental Faculty, Tehran Medical Sciences, Islamic Azad University, Pasdaran Ave., No. 9, Tehran 1946853314, Iran. dr.ma.navabi@gmail.com
Copyright © 2020. The Korean Academy of Conservative Dentistry
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 2,569 Views
- 27 Download
- 6 Crossref
Abstract
-
Objectives This study was performed to assess the anatomy of mandibular first molars.
-
Materials and Methods In this in vivo study, cone-beam computed tomography (CBCT) volumes of 312 bilateral intact first mandibular molars from 156 patients (79 men and 77 women; average age, 35.6 ± 11.2 years) were investigated in terms of the direction of each canal's curvature in the buccolingual and mesiodistal dimensions (direction of the position of the apex in relation to the longitudinal axis of the root), the presence of an isthmus (a narrow, ribbon-shaped communication between 2 root canals) in 3 segments (0–2, 2–4, and 4–6 mm) from the apex), and the presence and number of accessory canals (smaller canals besides the main root canals, connecting the pulp to the periodontium). Data were analyzed statistically (α = 0.05).
-
Results Mesiolingual canals were mostly buccally and distally inclined, while mesiobuccal and distolingual canals were mostly distally curved. Isthmuses were more common in younger patients (χ2 test, p < 0.05). The average numbers of accessory canals in the apical, middle, and coronal segments were 9.9 ± 4.2, 6.9 ± 2.9, and 9.3 ± 3.0 canals per segment, respectively (analysis of variance, p < 0.001). Age and sex were not associated with the number of accessory canals (p > 0.05).
-
Conclusions The complex anatomy of these teeth deserves attention during non-surgical or surgical endodontic treatment. Around the apex, isthmuses might be more prevalent in younger and female individuals.
INTRODUCTION
MATERIALS AND METHODS
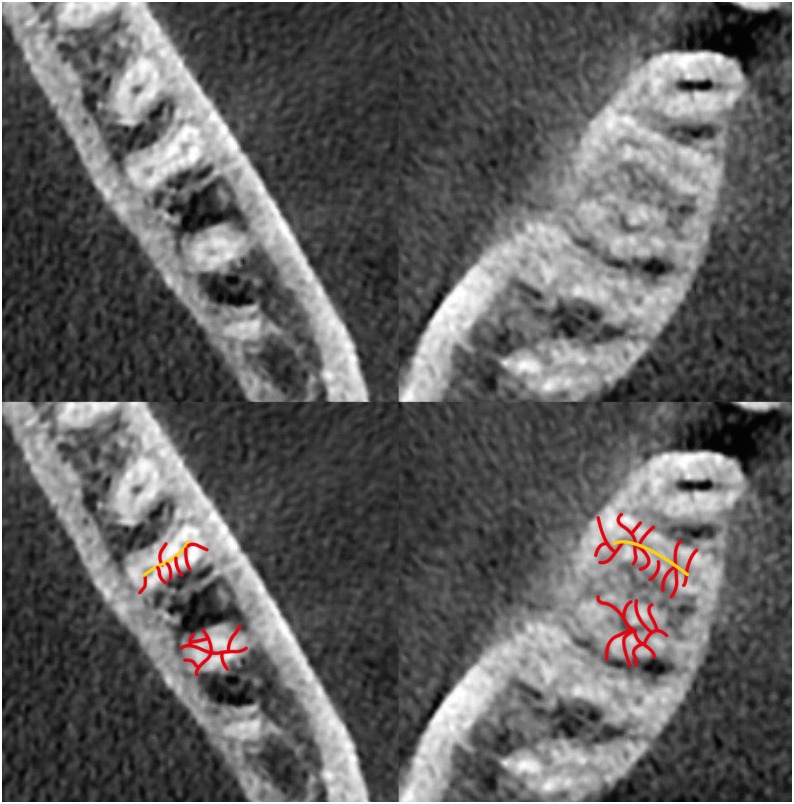
An example of accessory canals. In the bottom image, the main (yellow) and accessory (red) canals are marked.
RESULTS
Distribution of apical foramen locations in mesiobuccal, mesiolingual, distobuccal, and distolingual canals
Distribution of isthmuses in each root segment
Number of accessory canals per root segment
DISCUSSION
Summary of reports on root and canal curvature
| Author | Year | Country | Ref. | Method | Sample size | Root/canal curvature |
|---|---|---|---|---|---|---|
| Rocha et al. | 1996 | Brazil | [19] | In vitro (clearing technique) assessment of root curvature | 232 | Mesial root: 73% distal, 17% straight |
| Distal root: 8% distal, 12% mesial, 78% straight | ||||||
| Estrela et al. | 2015 | Brazil | [17] | CBCT (in vivo) assessment of canal curvature | 200 | 92.7% curvature in the apical third, 73.2% curvature in the cervical third |
| Schäfer et al. | 2002 | Germany | [18] | CBCT (in vitro) assessment of canal curvature | 50 | 58% to 76% of curved canals with 33° to 48° angles |
Summary of reports on isthmus prevalence and locations (all reported values are percentages)
| Author | Year | Country | Ref. | Method | Sample size | Mesial root | Most common location | Distal root | Most common location |
|---|---|---|---|---|---|---|---|---|---|
| de Pablo et al. | 2010 | Spain | [20] | Review of literature of 41 articles | 18,781 | 54.8% (range 23%–77%) | Middle third | 20.2% (range, 8%–55%) | |
| Demirbuga et al. | 2013 | Turkey | [27] | Micro-CT (in vitro) | 1,748 | 30% | - | 12% | - |
| Chourasia et al. | 2012 | India | [29] | In vitro (clearing technique) | 150 | 30% | - | 10% | - |
| Al-Qudah and Awawdeh | 2009 | Jordan | [7] | In vitro (clearing technique) | 330 | 37.3% | Middle and apical thirds | 13% | Middle third |
| Ahmed et al. | 2007 | Sudan | [8] | In vitro (clearing technique) | 100 | 62% | - | 8% | - |
| Villas-Bôas et al. | 2011 | Brazil | [25] | In vitro (micro-CT) | 60 first/second molars | 61% | 3–4 mm from apex | - | - |
| Gulabivala et al. | 2001 | Myanmar | [9] | In vitro (clearing technique) | 139 | 69.2% | - | 9.2% | - |
| Mohammadzadeh Akhlaghi et al. | 2017 | Iran | [2] | In vitro (clearing technique) | 150 | 44.6% | 22.5% (2 mm from apex), 41.7% (4 mm), 35.8% (6 mm) | 27.3% | 34.3% (2 mm), 36.5% (4 mm), 29.3% (6 mm) |
| Faraz et al. | 2015 | - | [28] | In vitro (clearing technique) | 123 | 10% | - | 5% | - |
| Peiris et al. | 2008 | Japan | [10] | In vitro (clearing technique) | 177 first/second molars | 77.4% | Middle third | 11.3% | Middle third |
| Mehrvarzfar et al. | 2012 | Iran | [4] | In vitro (clearing technique) | 60 | 83% | 92%, 88%, and 70% respectively in ranges 6, 4, and 2 mm from apex | - | - |
| Gu et al. | 2009 | China | [24] | Micro-CT (in vivo) | 120 | 81% | At 6 mm from apex of mesial root: 20–40 years old (80%), 40–60 (67%), and over 60% (30%) | ||
| von Arx et al. | 2005 | - | [6] | Endoscope (in vivo) | 56 | 88.5% | 3–4 mm from apex | - | - |
| Fan et al. | 2010 | - | [26] | Micro-CT (in vivo) | 126 | 85% | 5 mm from apex | - | - |
Summary of reports on the prevalence and location of accessory canals (all reported values are percentages)
| Author | Year | Country | Ref. | Method | Sample size | No. of accessory canals | |
|---|---|---|---|---|---|---|---|
| Mesial root | Distal root | ||||||
| Al-Qudah and Awawdeh | 2009 | Jordan | [7] | In vitro (clearing technique) | 330 | 1% (0.6% in the middle third, 0.3% in the apical third) | 3% (all in the apical third) |
| Ahmed et al. | 2007 | Sudan | [8] | In vitro (clearing technique) | 100 | 52% | - |
| Gulabivala et al. | 2001 | Myanmar | [9] | In vitro (clearing technique) | 139 | 11% in the apical third (highest percentage) | - |
| Peiris et al. | 2008 | Japan | [10] | In vitro (clearing technique) | 177 first/second molars | 45.2% in the apical third | 29.4% in the apical third |
CONCLUSIONS
ACKNOWLEDGEMENTS
-
Conflict of Interest: The authors declare that they do not have any conflict of interest.
-
Author Contributions:
Conceptualization: Chuppani Dastgerdi A.
Data curation: Chuppani Dastgerdi A.
Formal analysis: Rakhshan V.
Funding acquisition: Navabi M.
Investigation: Chuppani Dastgerdi A, Navabi M, Rakhshan V.
Methodology: Chuppani Dastgerdi A, Navabi M.
Project administration: Chuppani Dastgerdi A, Navabi M, Rakhshan V.
Resources: Chuppani Dastgerdi A.
Software: Chuppani Dastgerdi A, Rakhshan V.
Supervision: Navabi M.
Validation: Chuppani Dastgerdi A, Navabi M, Rakhshan V.
Visualization: Chuppani Dastgerdi A, Rakhshan V.
Writing - original draft: Chuppani Dastgerdi A, Navabi M, Rakhshan V.
Writing - review & editing: Chuppani Dastgerdi A, Navabi M, Rakhshan V.
- 1. Akhlaghi NM, Abbas FM, Mohammadi M, Shamloo MR, Radmehr O, Kaviani R, Rakhshan V. Radicular anatomy of permanent mandibular second molars in an Iranian population: a preliminary study. Dent Res J (Isfahan) 2016;13:362-366.ArticlePubMedPMC
- 2. Mohammadzadeh Akhlaghi N, Khalilak Z, Vatanpour M, Mohammadi S, Pirmoradi S, Fazlyab M, Safavi K. Root canal anatomy and morphology of mandibular first molars in a selected Iranian population: an in vitro study. Iran Endod J 2017;12:87-91.PubMedPMC
- 3. Madani ZS, Mehraban N, Moudi E, Bijani A. Root and canal morphology of mandibular molars in a selected Iranian population using cone-beam computed tomography. Iran Endod J 2017;12:143-148.PubMedPMC
- 4. Mehrvarzfar P, Akhlagi NM, Khodaei F, Shojaee G, Shirazi S. Evaluation of isthmus prevalence, location, and types in mesial roots of mandibular molars in the Iranian population. Dent Res J (Isfahan) 2014;11:251-256.PubMedPMC
- 5. Weller RN, Niemczyk SP, Kim S. Incidence and position of the canal isthmus. Part 1. Mesiobuccal root of the maxillary first molar. J Endod 1995;21:380-383.ArticlePubMed
- 6. von Arx T. Frequency and type of canal isthmuses in first molars detected by endoscopic inspection during periradicular surgery. Int Endod J 2005;38:160-168.ArticlePubMed
- 7. Al-Qudah AA, Awawdeh LA. Root and canal morphology of mandibular first and second molar teeth in a Jordanian population. Int Endod J 2009;42:775-784.ArticlePubMed
- 8. Ahmed HA, Abu-bakr NH, Yahia NA, Ibrahim YE. Root and canal morphology of permanent mandibular molars in a Sudanese population. Int Endod J 2007;40:766-771.ArticlePubMed
- 9. Gulabivala K, Aung TH, Alavi A, Ng YL. Root and canal morphology of Burmese mandibular molars. Int Endod J 2001;34:359-370.ArticlePubMedPDF
- 10. Peiris HR, Pitakotuwage TN, Takahashi M, Sasaki K, Kanazawa E. Root canal morphology of mandibular permanent molars at different ages. Int Endod J 2008;41:828-835.ArticlePubMed
- 11. Razmi H, Shokouhinejad N, Hooshyar M. An in vitro study of the number of distal roots and canals in mandibular first molars in Iranian population. Iran Endod J 2008;2:126-130.PubMedPMC
- 12. Choupani Dastgerdi A, Navabi M, Hafezi L, Khalilak Z, Rakhshan V. Anatomy of permanent mandibular first molars in a selected Iranian population using cone-beam computed tomography. Iran Endod J 2018;13:251-256.PubMedPMC
- 13. Lee KW, Kim Y, Perinpanayagam H, Lee JK, Yoo YJ, Lim SM, Chang SW, Ha BH, Zhu Q, Kum KY. Comparison of alternative image reformatting techniques in micro-computed tomography and tooth clearing for detailed canal morphology. J Endod 2014;40:417-422.ArticlePubMed
- 14. Dalili Kajan Z, Taramsari M, Khosravi Fard N, Kanani M. Accuracy of cone-beam computed tomography in comparison with standard method in evaluating root canal morphology: an in vitro study. Iran Endod J 2018;13:181-187.PubMedPMC
- 15. Faramarzi F, Vossoghi M, Shokri A, Shams B, Vossoghi M, Khoshbin E. Cone beam computed tomography study of root and canal morphology of maxillary first molar in an Iranian population. Avicenna J Dent Res 2015;7:e24038.ArticlePDF
- 16. Hsu YY, Kim S. The resected root surface. The issue of canal isthmuses. Dent Clin North Am 1997;41:529-540.PubMed
- 17. Estrela C, Bueno MR, Barletta FB, Guedes OA, Porto OC, Estrela CR, Pécora JD. Identification of apical and cervical curvature radius of human molars. Braz Dent J 2015;26:351-356.ArticlePubMed
- 18. Schäfer E, Diez C, Hoppe W, Tepel J. Roentgenographic investigation of frequency and degree of canal curvatures in human permanent teeth. J Endod 2002;28:211-216.ArticlePubMed
- 19. Rocha LF, Sousa Neto MD, Fidel SR, da Costa WF, Pécora JD. External and internal anatomy of mandibular molars. Braz Dent J 1996;7:33-40.PubMed
- 20. de Pablo ÓV, Estevez R, Péix Sánchez M, Heilborn C, Cohenca N. Root anatomy and canal configuration of the permanent mandibular first molar: a systematic review. J Endod 2010;36:1919-1931.ArticlePubMed
- 21. Zafar M, Alrahabi M. Cone beam computed tomography for exploring morphology of mandibular first molar. Br J Med Med Res 2015;6:514-521.Article
- 22. Arjmand N, Kolahdouzan A, Rouhi N. Evaluation of root and canal morphology of first and second mandibular molars according to Vertucci and Weine classification by using cone-beam computed tomography archive in Partow Radiology Center in Qazvin in 1391 [dissertation]. Qazvin: Qazvin University of Medical Sciences; 2014.
- 23. Masoudi SM, Rouhi N. Evaluation of root canal number and anatomy of first and second mandibular molars with available CBCT in Qazvin in 2013 [dissertation]. Qazvin: Qazvin University of Medical Sciences; 2014.
- 24. Gu L, Wei X, Ling J, Huang X. A microcomputed tomographic study of canal isthmuses in the mesial root of mandibular first molars in a Chinese population. J Endod 2009;35:353-356.ArticlePubMed
- 25. Villas-Bôas MH, Bernardineli N, Cavenago BC, Marciano M, Del Carpio-Perochena A, de Moraes IG, Duarte MH, Bramante CM, Ordinola-Zapata R. Micro-computed tomography study of the internal anatomy of mesial root canals of mandibular molars. J Endod 2011;37:1682-1686.ArticlePubMed
- 26. Fan B, Pan Y, Gao Y, Fang F, Wu Q, Gutmann JL. Three-dimensional morphologic analysis of isthmuses in the mesial roots of mandibular molars. J Endod 2010;36:1866-1869.ArticlePubMed
- 27. Demirbuga S, Sekerci AE, Dinçer AN, Cayabatmaz M, Zorba YO. Use of cone-beam computed tomography to evaluate root and canal morphology of mandibular first and second molars in Turkish individuals. Med Oral Patol Oral Cir Bucal 2013;18:e737-e744.ArticlePubMedPMC
- 28. Faraz SA, Tariq A, Jameel A. Root canal morphology of mandibular first permanent molars-Karachi sample. Pak Oral Dent J 2015;35:294-298.
- 29. Chourasia HR, Meshram GK, Warhadpande M, Dakshindas D. Root canal morphology of mandibular first permanent molars in an Indian population. Int J Dent 2012;2012:745152.ArticlePubMedPMCPDF
- 30. Wu DM, Wu YN, Guo W, Sameer S. Accuracy of direct digital radiography in the study of the root canal type. Dentomaxillofac Radiol 2006;35:263-265.ArticlePubMed
- 31. Neelakantan P, Subbarao C, Subbarao CV. Comparative evaluation of modified canal staining and clearing technique, cone-beam computed tomography, peripheral quantitative computed tomography, spiral computed tomography, and plain and contrast medium-enhanced digital radiography in studying root canal morphology. J Endod 2010;36:1547-1551.ArticlePubMed
REFERENCES
Tables & Figures
REFERENCES
Citations

- Micro-CT and histological examination of accessory canals in 34 equine cheek teeth
Szabolcs A. Korsós, Carsten Staszyk, Matthieu Boone, Iván Josipovic, Jörg Vogelsberg, Lieven Vlaminck
Frontiers in Veterinary Science.2024;[Epub] CrossRef - Diagnostic value of cone beam computed tomography for root canal morphology assessment – a micro-CT based comparison
Mariana Pires, Jorge N.R. Martins, Mário Rito Pereira, Isabel Vasconcelos, Rui Pereira da Costa, Isabel Duarte, António Ginjeira
Clinical Oral Investigations.2024;[Epub] CrossRef - Exploring age and gender variations in root canal morphology of maxillary premolars in Saudi sub population: a cross-sectional CBCT study
Mohmed Isaqali Karobari, Azhar Iqbal, Rumesa Batul, Abdul Habeeb Adil, Jamaluddin Syed, Hmoud Ali Algarni, Meshal Aber Alonazi, Tahir Yusuf Noorani
BMC Oral Health.2024;[Epub] CrossRef - Comprehensive analysis of root canal morphology in maxillary premolars among the Pakistani subpopulation: a CBCT-based study
Hmoud Ali Algarni, Meshal Aber Alonazi, Hamza Arshad, Fatima Zahra, Fahad Umer, Irfan Maqbool, Azhar Iqbal, Mohmed Isaqali Karobari
European Journal of Medical Research.2024;[Epub] CrossRef - The efficacy of a novel SWEEPS laser-activated irrigation compared to ultrasonic activation in the removal of pulp tissue from an isthmus area in the apical third of the root canal
Ivona Bago, Adriana Đurin, Debora Kanižaj, Lovorka Batelja Vuletić, Ivana Vidović Zdrilić, Ivica Anić
Lasers in Medical Science.2023;[Epub] CrossRef - Effect of passive ultrasonic irrigation on hard tissue debris removal: a systematic review and meta-analysis
Ana Flávia Almeida Barbosa, Carolina Oliveira de Lima, Luciana Moura Sassone, Raissa Dias Fares, Tatiana Kelly da Silva Fidalgo, Emmanuel João Nogueira Leal Silva
Brazilian Oral Research.2021;[Epub] CrossRef
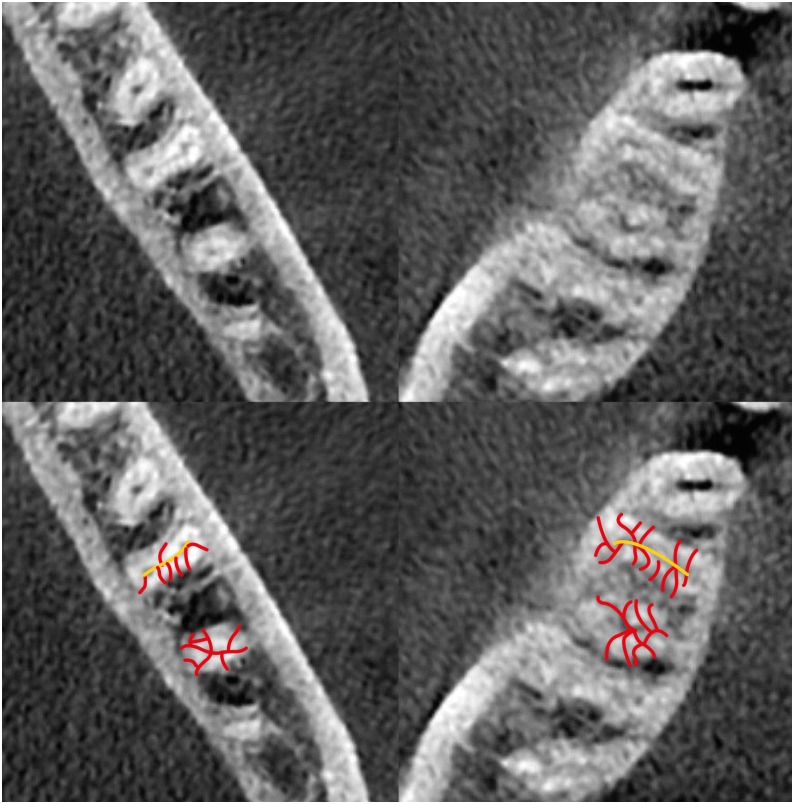
Figure 1
Distribution of apical foramen locations in mesiobuccal, mesiolingual, distobuccal, and distolingual canals
| Canal | Buccolingual dimension | Mesiodistal dimension | ||||
|---|---|---|---|---|---|---|
| Straight | Buccal | Lingual | Straight | Mesial | Distal | |
| Mesiobuccal | 218 (69.8) | 38 (12.2) | 56 (17.9) | 27 (8.6) | 3 (0.9) | 282 (90.4) |
| Mesiolingual | 83 (26.6) | 226 (72.4) | 3 (0.9) | 20 (6.4) | 7 (2.2) | 285 (91.3) |
| Distobuccal | 249 (79.8) | 49 (15.7) | 14 (4.5) | 8 (2.6) | 0 (0) | 304 (97.4) |
| Distolingual | 137 (77.8) | 29 (16.5) | 10 (5.7) | 0 (0) | 0 (0) | 176 (100) |
Values are presented as number (%).
Distribution of isthmuses in each root segment
| Age (yr) | Root | Root segment (mm) | ||
|---|---|---|---|---|
| 0–2 | 2–4 | 4–6 | ||
| 20–39 | Mesial | 53 (17.0) | 100 (32.0) | 116 (37.1) |
| Distal | 34 (10.9) | 64 (20.5) | 71 (22.7) | |
| 40–60 | Mesial | 41 (13.1) | 59 (18.9) | 78 (25) |
| Distal | 26 (8.3) | 28 (8.9) | 45 (14.4) | |
Values are presented as number (%).
Number of accessory canals per root segment
| Age (yr) | Root | Root segment | ||
|---|---|---|---|---|
| Cervical | Middle | Apical | ||
| 20–39 | Mesial | 4.98 ± 1.70 | 3.72 ± 1.71 | 5.30 ± 2.49 |
| Distal | 4.25 ± 1.55 | 3.05 ± 1.92 | 4.41 ± 2.22 | |
| 40–60 | Mesial | 4.92 ± 1.93 | 3.92 ± 1.92 | 5.41 ± 2.41 |
| Distal | 4.48 ± 1.60 | 3.11 ± 1.70 | 4.68 ± 2.26 | |
Data are presented as mean ± standard deviation.
Summary of reports on root and canal curvature
| Author | Year | Country | Ref. | Method | Sample size | Root/canal curvature |
|---|---|---|---|---|---|---|
| Rocha et al. | 1996 | Brazil | [ | In vitro (clearing technique) assessment of root curvature | 232 | Mesial root: 73% distal, 17% straight |
| Distal root: 8% distal, 12% mesial, 78% straight | ||||||
| Estrela et al. | 2015 | Brazil | [ | CBCT (in vivo) assessment of canal curvature | 200 | 92.7% curvature in the apical third, 73.2% curvature in the cervical third |
| Schäfer et al. | 2002 | Germany | [ | CBCT (in vitro) assessment of canal curvature | 50 | 58% to 76% of curved canals with 33° to 48° angles |
CBCT, cone-beam computed tomography.
Summary of reports on isthmus prevalence and locations (all reported values are percentages)
| Author | Year | Country | Ref. | Method | Sample size | Mesial root | Most common location | Distal root | Most common location |
|---|---|---|---|---|---|---|---|---|---|
| de Pablo et al. | 2010 | Spain | [ | Review of literature of 41 articles | 18,781 | 54.8% (range 23%–77%) | Middle third | 20.2% (range, 8%–55%) | |
| Demirbuga et al. | 2013 | Turkey | [ | Micro-CT (in vitro) | 1,748 | 30% | - | 12% | - |
| Chourasia et al. | 2012 | India | [ | In vitro (clearing technique) | 150 | 30% | - | 10% | - |
| Al-Qudah and Awawdeh | 2009 | Jordan | [ | In vitro (clearing technique) | 330 | 37.3% | Middle and apical thirds | 13% | Middle third |
| Ahmed et al. | 2007 | Sudan | [ | In vitro (clearing technique) | 100 | 62% | - | 8% | - |
| Villas-Bôas et al. | 2011 | Brazil | [ | In vitro (micro-CT) | 60 first/second molars | 61% | 3–4 mm from apex | - | - |
| Gulabivala et al. | 2001 | Myanmar | [ | In vitro (clearing technique) | 139 | 69.2% | - | 9.2% | - |
| Mohammadzadeh Akhlaghi et al. | 2017 | Iran | [ | In vitro (clearing technique) | 150 | 44.6% | 22.5% (2 mm from apex), 41.7% (4 mm), 35.8% (6 mm) | 27.3% | 34.3% (2 mm), 36.5% (4 mm), 29.3% (6 mm) |
| Faraz et al. | 2015 | - | [ | In vitro (clearing technique) | 123 | 10% | - | 5% | - |
| Peiris et al. | 2008 | Japan | [ | In vitro (clearing technique) | 177 first/second molars | 77.4% | Middle third | 11.3% | Middle third |
| Mehrvarzfar et al. | 2012 | Iran | [ | In vitro (clearing technique) | 60 | 83% | 92%, 88%, and 70% respectively in ranges 6, 4, and 2 mm from apex | - | - |
| Gu et al. | 2009 | China | [ | Micro-CT (in vivo) | 120 | 81% | At 6 mm from apex of mesial root: 20–40 years old (80%), 40–60 (67%), and over 60% (30%) | ||
| von Arx et al. | 2005 | - | [ | Endoscope (in vivo) | 56 | 88.5% | 3–4 mm from apex | - | - |
| Fan et al. | 2010 | - | [ | Micro-CT (in vivo) | 126 | 85% | 5 mm from apex | - | - |
CT, computed tomography.
| Author | Year | Country | Ref. | Method | Sample size | No. of accessory canals | |
|---|---|---|---|---|---|---|---|
| Mesial root | Distal root | ||||||
| Al-Qudah and Awawdeh | 2009 | Jordan | [ | In vitro (clearing technique) | 330 | 1% (0.6% in the middle third, 0.3% in the apical third) | 3% (all in the apical third) |
| Ahmed et al. | 2007 | Sudan | [ | In vitro (clearing technique) | 100 | 52% | - |
| Gulabivala et al. | 2001 | Myanmar | [ | In vitro (clearing technique) | 139 | 11% in the apical third (highest percentage) | - |
| Peiris et al. | 2008 | Japan | [ | In vitro (clearing technique) | 177 first/second molars | 45.2% in the apical third | 29.4% in the apical third |
Values are presented as number (%).
Values are presented as number (%).
Data are presented as mean ± standard deviation.
CBCT, cone-beam computed tomography.
CT, computed tomography.

 KACD
KACD
 ePub Link
ePub Link Cite
Cite

