Articles
- Page Path
- HOME > Restor Dent Endod > Volume 45(4); 2020 > Article
- Research Article Physicochemical properties, cytotoxicity and penetration into dentinal tubules of sodium hypochlorite with and without surfactants
-
Hernán Coaguila-Llerena1
 , Isadora Barbieri1
, Isadora Barbieri1 , Mário Tanomaru-Filho1
, Mário Tanomaru-Filho1 , Renato de Toledo Leonardo1
, Renato de Toledo Leonardo1 , Ana Paula Ramos2
, Ana Paula Ramos2 , Gisele Faria1
, Gisele Faria1
-
Restor Dent Endod 2020;45(4):e47.
DOI: https://doi.org/10.5395/rde.2020.45.e47
Published online: September 10, 2020
1Department of Restorative Dentistry, São Paulo State University (UNESP), Araraquara School of Dentistry, Araraquara, SP, Brazil.
2Department of Chemistry, São Paulo University (USP), Ribeirão Preto College of Philosophy Sciences and Letters, Ribeirão Preto, SP, Brazil.
- Correspondence to Gisele Faria, PhD. Professor, Department of Restorative Dentistry, São Paulo State University (UNESP), Araraquara School of Dentistry, 1680 Humaitá Street, Araraquara, SP 14801-903, Brazil. gisele.faria@unesp.br
Copyright © 2020. The Korean Academy of Conservative Dentistry
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 2,469 Views
- 32 Download
- 11 Crossref
Abstract
-
Objectives The aim of this study was to assess the physicochemical properties, cytotoxicity and penetration into dentinal tubules of ChlorCid™ Surf (3% sodium hypochlorite [NaOCl] with surfactant) in comparison to ChlorCid™ (3% NaOCl without surfactant).
-
Materials and Methods The physicochemical properties evaluated were pH, surface tension, free available chlorine (FAC) and contact angle. Cytotoxicity was evaluated in L929 fibroblasts exposed to the solutions by 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide and neutral red assays. Assessment of penetration into dentinal tubules was performed by staining single-rooted permanent human teeth with crystal violet (n = 9), which were irrigated with the solutions and analyzed in cervical, middle and apical segments. Data were analyzed by one-way analysis of variance (ANOVA) and Tukey's post-test, 2-way ANOVA and Bonferroni's post-test or t-test (α = 0.05).
-
Results ChlorCid™ Surf and ChlorCid™ FAC values were close to those indicated by the manufacturer. ChlorCid™ Surf showed lower surface tension and contact angle on dentin, and higher pH than ChlorCid™ (p < 0.05). The penetration of ChlorCid™ Surf was higher in cervical and middle segments, compared with ChlorCid™ (p < 0.05). There was no difference in irrigant cytotoxicity (p > 0.05).
-
Conclusions ChlorCid™ Surf showed lower surface tension, lower contact angle on root canal dentin, higher penetration into dentinal tubules and more alkaline pH, compared with ChlorCid™. However, both solutions showed similar cytotoxicity and FAC content.
INTRODUCTION
MATERIALS AND METHODS
1. pH
2. FAC content
3. Surface tension
4. Contact angle
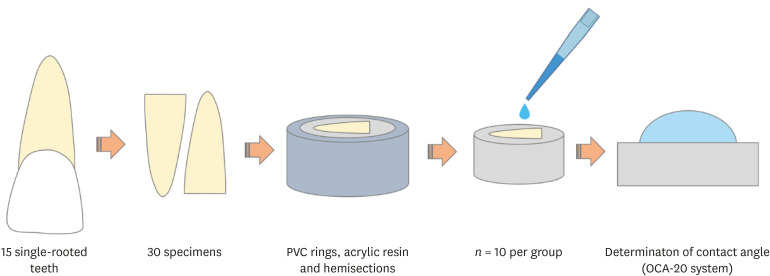
Schematic representation of the contact angle evaluation of ChlorCid™ and ChlorCid™ Surf on root canal dentin. First, each tooth hemisection was mounted on PVC rings with acrylic resin. After resin curing, the rings were removed and the specimen was polished to avoid surface irregularities. Thereafter, 5 µL-drops of each solution were placed on the specimens to measure the contact angle using the OCA-20 system.
RESULTS
Mean and standard deviation of pH and free available chlorine in percentage (%) of weight/mass (w/w) of ChlorCid™ and ChlorCid™ Surf
| Solution | pH | Free available chlorine (% [m/m]) |
|---|---|---|
| ChlorCid™ | 12.27 ± 0.05* | 2.788 ± 0.047 |
| ChlorCid™ Surf | 13.08 ± 0.02 | 2.854 ± 0.044 |
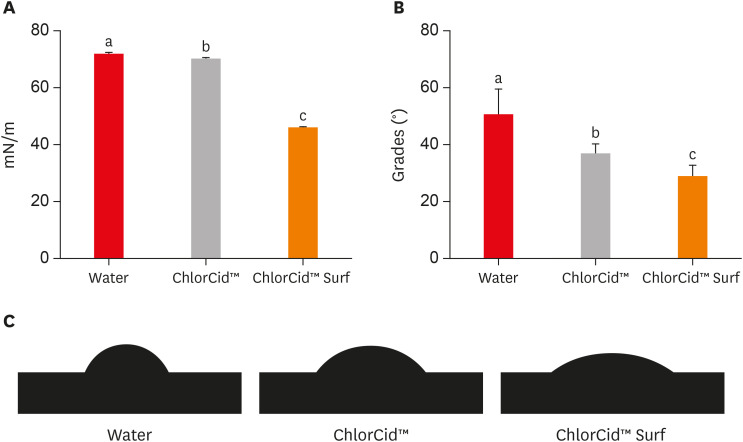
Mean and standard deviation of (A) surface tension in millinewton/meter (mN/m) and (B) contact angle (Ө) of ChlorCid™, ChlorCid™ Surf and deionized water (control). Different letters in columns indicate a significant difference between solutions. (C) Representative images of the contact angle on the dentin surface.
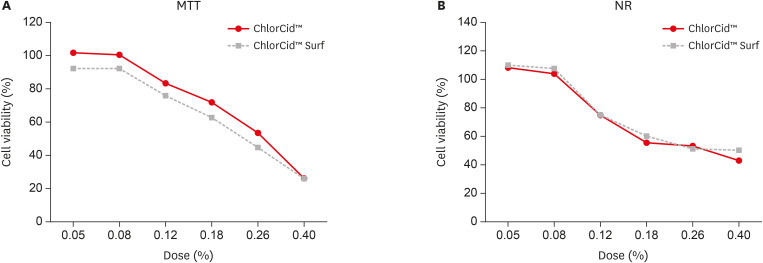
Viability of L929 fibroblasts after exposure to ChlorCid™ and ChlorCid™ Surf solutions at different doses by (A) MTT and (B) NR assays. No significant differences were founded between the solutions (p > 0.05).
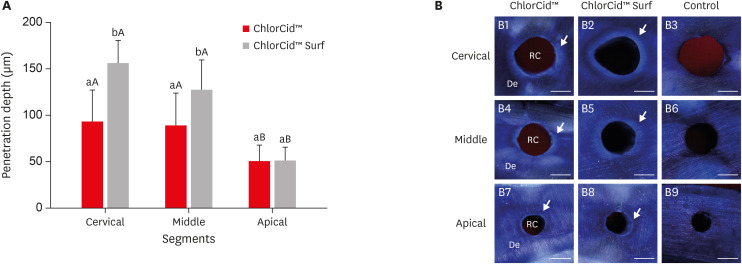
Penetration depth of ChlorCid™ and ChlorCid™ Surf solutions into dentinal tubules. (A) Mean and standard deviation in micrometers (µm) of penetration depth. Different lowercase letters in columns of each segment indicate a significant difference between the solutions. Different capital letters in columns indicate a significant difference between segments of each solution. (B) Representative images of penetration depth of ChlorCid™, ChlorCid™ Surf and water in cervical (B1-B3), middle (B4-B6) and apical (B7-B9) segments, respectively. The bleached crystal violet represents the penetration depth of irrigants into the dentin (arrow) (bar = 500 µm).
DISCUSSION
CONCLUSIONS
-
Funding: This work was supported by Fundação de Amparo à Pesquisa do Estado de São Paulo - FAPESP under Grant 2018/24662-6; and Conselho Nacional de Desenvolvimento Científico e Tecnológico - CNPq under Grant 51759.
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Coaguila-Llerena H, Faria G, Ramos AP.
Data curation: Coaguila-Llerena H, Barbieri I, Faria G.
Formal analysis: Tanomaru-Filho M, Leonardo RDT, Ramos AP, Faria G.
Funding acquisition: Coaguila-Llerena H, Barbieri I, Faria G.
Investigation: Coaguila-Llerena H, Ramos AP, Faria G.
Methodology: Coaguila-Llerena H, Barbieri I, Ramos AP, Faria G.
Project administration: Faria G, Ramos AP.
Resources: Coaguila-Llerena H, Tanomaru-Filho M, Leonardo RDT, Ramos AP, Faria G.
Software: Coaguila-Llerena H, Faria G, Ramos AP.
Supervision: Faria G, Ramos AP.
Validation: Coaguila-Llerena H, Barbieri I, Tanomaru-Filho M, Leonardo RDT, Ramos AP, Faria G.
Visualization: Coaguila-Llerena H, Barbieri I, Tanomaru-Filho M, Leonardo RDT, Ramos AP, Faria G.
Writing - original draft: Coaguila-Llerena H, Barbieri I, Tanomaru-Filho M, Leonardo RDT, Ramos AP, Faria G.
Writing - review & editing: Coaguila-Llerena H, Barbieri I, Tanomaru-Filho M, Leonardo RDT, Ramos AP, Faria G.
- 1. Nair PN, Henry S, Cano V, Vera J. Microbial status of apical root canal system of human mandibular first molars with primary apical periodontitis after “one-visit” endodontic treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005;99:231-252.ArticlePubMed
- 2. Ricucci D, Siqueira JF Jr. Biofilms and apical periodontitis: study of prevalence and association with clinical and histopathologic findings. J Endod 2010;36:1277-1288.ArticlePubMed
- 3. Palazzi F, Blasi A, Mohammadi Z, Del Fabbro M, Estrela C. Penetration of sodium hypochlorite modified with surfactants into root canal dentin. Braz Dent J 2016;27:208-216.ArticlePubMed
- 4. Zou L, Shen Y, Li W, Haapasalo M. Penetration of sodium hypochlorite into dentin. J Endod 2010;36:793-796.ArticlePubMed
- 5. Faria G, Viola KS, Coaguila-Llerena H, Oliveira LRA, Leonardo RT, Aranda-García AJ, Guerreiro-Tanomaru JM. Penetration of sodium hypochlorite into root canal dentine: effect of surfactants, gel form and passive ultrasonic irrigation. Int Endod J 2019;52:385-392.ArticlePubMedPDF
- 6. Pécora JD, Guimarães LF, Savioli RN. Surface tension of several drugs used in endodontics. Braz Dent J 1992;2:123-127.PubMed
- 7. Kontakiotis EG, Tzanetakis GN, Loizides AL. A comparative study of contact angles of four different root canal sealers. J Endod 2007;33:299-302.ArticlePubMed
- 8. Abou-Rass M, Patonai FJ Jr. The effects of decreasing surface tension on the flow of irrigating solutions in narrow root canals. Oral Surg Oral Med Oral Pathol 1982;53:524-526.ArticlePubMed
- 9. Giardino L, Ambu E, Becce C, Rimondini L, Morra M. Surface tension comparison of four common root canal irrigants and two new irrigants containing antibiotic. J Endod 2006;32:1091-1093.ArticlePubMed
- 10. Bukiet F, Couderc G, Camps J, Tassery H, Cuisinier F, About I, Charrier A, Candoni N. Wetting properties and critical micellar concentration of benzalkonium chloride mixed in sodium hypochlorite. J Endod 2012;38:1525-1529.ArticlePubMed
- 11. Palazzi F, Morra M, Mohammadi Z, Grandini S, Giardino L. Comparison of the surface tension of 5.25% sodium hypochlorite solution with three new sodium hypochlorite-based endodontic irrigants. Int Endod J 2012;45:129-135.ArticlePubMed
- 12. Guastalli AR, Clarkson RM, Rossi-Fedele G. The effect of surfactants on the stability of sodium hypochlorite preparations. J Endod 2015;41:1344-1348.ArticlePubMed
- 13. Stojicic S, Zivkovic S, Qian W, Zhang H, Haapasalo M. Tissue dissolution by sodium hypochlorite: effect of concentration, temperature, agitation, and surfactant. J Endod 2010;36:1558-1562.ArticlePubMed
- 14. Iglesias JE, Pinheiro LS, Weibel DE, Montagner F, Grecca FS. Influence of surfactants addition on the properties of calcium hypochlorite solutions. J Appl Oral Sci 2019;27:e20180157.ArticlePubMedPMC
- 15. Giardino L, Cavani F, Generali L. Sodium hypochlorite solution penetration into human dentine: a histochemical evaluation. Int Endod J 2017;50:492-498.ArticlePubMedPDF
- 16. Clarkson RM, Kidd B, Evans GE, Moule AJ. The effect of surfactant on the dissolution of porcine pulpal tissue by sodium hypochlorite solutions. J Endod 2012;38:1257-1260.ArticlePubMed
- 17. Wong DT, Cheung GS. Extension of bactericidal effect of sodium hypochlorite into dentinal tubules. J Endod 2014;40:825-829.ArticlePubMed
- 18. del Carpio-Perochena A, Bramante CM, de Andrade FB, Maliza AG, Cavenago BC, Marciano MA, Amoroso-Silva P, Duarte MH. Antibacterial and dissolution ability of sodium hypochlorite in different pHs on multi-species biofilms. Clin Oral Investig 2015;19:2067-2073.ArticlePubMedPDF
- 19. Yasuda Y, Tatematsu Y, Fujii S, Maeda H, Akamine A, Torabinejad M, Saito T. Effect of MTAD on the differentiation of osteoblast-like cells. J Endod 2010;36:260-263.ArticlePubMed
- 20. Ultradent Products. ChlorCid® Surf [Internet]. South Jordan, UT: Ultradent Products; 2018. cited 2020 Sep 3]. Available from: https://assets.ctfassets.net/wfptrcrbtkd0/4TD20QySslMLYQ7krTGsHX/fcc08568844faa1a5ac6b149a927537f/ChlorCid-Surf-Sales-Sheet-1005815AR03.pdf.
- 21. European Directorate for the Quality of Medicines & HealthCare. European pharmacopoeia. Strasbourg Cedex: European Directorate for the Quality of Medicines & HealthCare; 2014. p. 24-25.
- 22. Baird R, Eaton A, Rice E. Standard methods for the examination of water and wastewater. Washington, D.C.: American Public Health Association; American Water Works Association; Water Environment Federation; 2017. p. 11-12.
- 23. Andrade MA, Favarin B, Derradi R, Bolean M, Simão AM, Millán JL, Ciancaglini P, Ramos AP. Pendant-drop method coupled to ultraviolet-visible spectroscopy: a useful tool to investigate interfacial phenomena. Colloids Surf A Physicochem Eng Asp 2016;504:305-311.ArticlePubMedPMC
- 24. Tartari T, Wichnieski C, Bachmann L, Jafelicci M Jr, Silva RM, Letra A, van der Hoeven R, Duarte MA, Bramante CM. Effect of the combination of several irrigants on dentine surface properties, adsorption of chlorhexidine and adhesion of microorganisms to dentine. Int Endod J 2018;51:1420-1433.ArticlePubMedPDF
- 25. Viola KS, Rodrigues EM, Tanomaru-Filho M, Carlos IZ, Ramos SG, Guerreiro-Tanomaru JM, Faria G. Cytotoxicity of peracetic acid: evaluation of effects on metabolism, structure and cell death. Int Endod J 2018;51(Suppl 4):e264-e277.ArticlePubMedPDF
- 26. Yilmaz Z, Basbag B, Buzoglu HD, Gümüsderelioglu M. Effect of low-surface-tension EDTA solutions on the wettability of root canal dentin. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2011;111:109-114.ArticlePubMed
- 27. Guneser MB, Arslan D, Dincer AN, Er G. Effect of sodium hypochlorite irrigation with or without surfactants on the bond strength of an epoxy-based sealer to dentin. Clin Oral Investig 2017;21:1259-1265.ArticlePubMedPDF
- 28. Dragan O, Tomuta I, Casoni D, Sarbu C, Campian R, Frentiu T. Influence of mixed additives on the physicochemical properties of a 5.25% sodium hypochlorite solution: an unsupervised multivariate statistical approach. J Endod 2018;44:280-285.e3.ArticlePubMed
- 29. Ballal NV, Ferrer-Luque CM, Sona M, Prabhu KN, Arias-Moliz T, Baca P. Evaluation of final irrigation regimens with maleic acid for smear layer removal and wettability of root canal sealer. Acta Odontol Scand 2018;76:199-203.ArticlePubMed
- 30. Milosevic A. The influence of surface finish and in-vitro pellicle on contact-angle measurement and surface morphology of three commercially available composite restoratives. J Oral Rehabil 1992;19:85-97.ArticlePubMed
- 31. Rossi-Fedele G, Guastalli AR, Doğramacı EJ, Steier L, De Figueiredo JA. Influence of pH changes on chlorine-containing endodontic irrigating solutions. Int Endod J 2011;44:792-799.ArticlePubMed
- 32. Vogel A. A textbook of quantitative inorganic analysis. London: Longmans; 1962.
- 33. Coaguila-Llerena H, Rodrigues EM, Tanomaru-Filho M, Guerreiro-Tanomaru JM, Faria G. Effects of calcium hypochlorite and octenidine hydrochloride on L929 and human periodontal ligament cells. Braz Dent J 2019;30:213-219.ArticlePubMed
- 34. Zhang W, Torabinejad M, Li Y. Evaluation of cytotoxicity of MTAD using the MTT-tetrazolium method. J Endod 2003;29:654-657.ArticlePubMed
- 35. Peters OA. Research that matters - biocompatibility and cytotoxicity screening. Int Endod J 2013;46:195-197.ArticlePubMed
- 36. Fotakis G, Timbrell JA. In vitro cytotoxicity assays: comparison of LDH, neutral red, MTT and protein assay in hepatoma cell lines following exposure to cadmium chloride. Toxicol Lett 2006;160:171-177.ArticlePubMed
- 37. Mosmann T. Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays. J Immunol Methods 1983;65:55-63.ArticlePubMed
- 38. Repetto G, del Peso A, Zurita JL. Neutral red uptake assay for the estimation of cell viability/cytotoxicity. Nat Protoc 2008;3:1125-1131.ArticlePubMedPDF
REFERENCES
Tables & Figures
REFERENCES
Citations

- Effects of penetration enhancers on the performance of irrigants for root canal disinfection
Yi Luo, Runze Liu, Pei Liu, Mengting Duan, Wei Fan, Bing Fan
Clinical Oral Investigations.2025;[Epub] CrossRef - Physicochemical and Biological Properties of the “All-In-One” Endodontic Irrigant Triton
Jesus Aranda, Elda Olivia Nobre de Souza, Arturo Javier Aranda Garcia, Renato de Toledo Leonardo, Ana Paula Ramos, Giampiero Rossi-Fedele, Gisele Faria
Journal of Endodontics.2025;[Epub] CrossRef - Influence of post space disinfection protocols on the push-out bond strength of fiber posts luted with self-adhesive cement
Satheesh B. Haralur, Salem Ali Alqahtani, Khalid Salem Alqahtani, Mohammed A. Al-Qarni, Saeed M. AlQahtani
AIP Advances.2025;[Epub] CrossRef - Research methods assessing sodium hypochlorite cytotoxicity: A scoping review
Hernán Coaguila-Llerena, Luana Raphael da Silva, Gisele Faria
Heliyon.2024; 10(1): e23060. CrossRef - Amelioration in the sodium hypochlorite as root canal irrigant – A review
Preety Sehrawat
International Dental Journal of Student's Research.2024; 12(2): 65. CrossRef - Sonic-assisted antibacterial photodynamic therapy: a strategy for enhancing lateral canal disinfection
Yanhuang Wang, Lishan Lei, Jing Huang, Zhiyu Cai, Xiaojing Huang
BMC Oral Health.2024;[Epub] CrossRef - A Comparative Evaluation of Contact Angle and Depth of Penetration of Sodium Hypochlorite With Various Surfactants: An In Vitro Study
Shubhashini N, Krithika D, Akhilesh Gowda , Shruthi Nagaraja , Rhea S Mathew, Nivaskumar G A, Vinaychandra R
Cureus.2024;[Epub] CrossRef - Antibacterial efficacy of silver nanoparticles, sodium hypochlorite, chlorhexidine, and hypochlorous acid on dentinal surfaces infected with Enterococcus faecalis
Aysenur Oncu, Berkan Celikten, Betül Aydın, Gulin Amasya, Erkan Tuncay, Gamze Guney Eskiler, Leyla Açık, Fatma Semra Sevimay
Microscopy Research and Technique.2024; 87(9): 2094. CrossRef - Advances in the Role of Sodium Hypochlorite Irrigant in Chemical Preparation of Root Canal Treatment
Chen Cai, Xuan Chen, Yang Li, Qianzhou Jiang, Yeliz Guven
BioMed Research International.2023;[Epub] CrossRef - Effect of sodium hypochlorite-based formulations on the adhesion interface after fiber post cementation
Joatan Lucas de Sousa Gomes COSTA, Tatiane Miranda MANZOLI, João Felipe BESEGATO, Joissi Ferrari ZANIBONI, Eliane Cristina Gulin DE OLIVEIRA, Lucas David GALVANI, Andréa Abi Rached DANTAS, Luis Geraldo VAZ, Milton Carlos KUGA
Dental Materials Journal.2023; 42(6): 878. CrossRef - Physicochemical properties and penetration into dentinal tubules of calcium hypochlorite with surfactants
Hernán Coaguila-Llerena, Julia da Silva Toledo, Ana Paula Ramos, Gisele Faria
Brazilian Dental Journal.2022; 33(2): 1. CrossRef
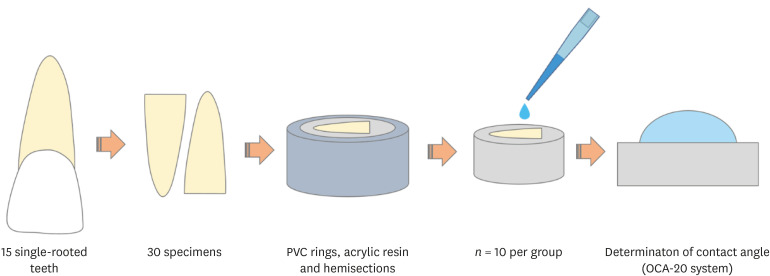
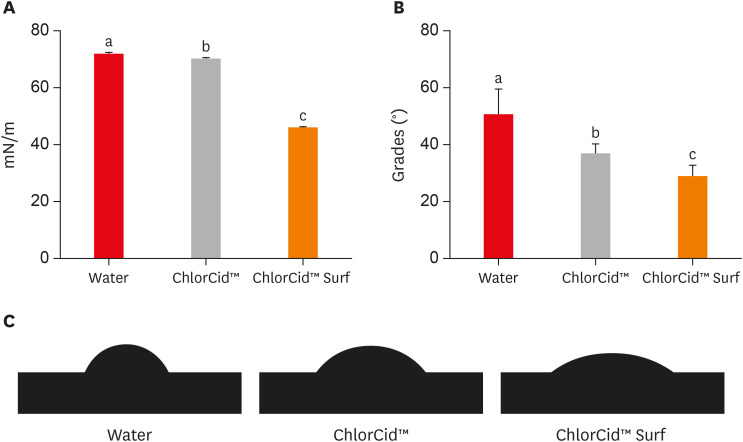
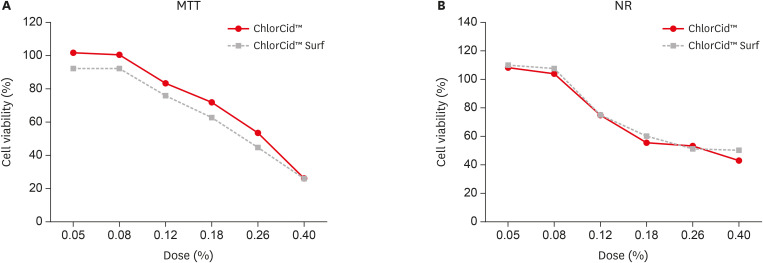
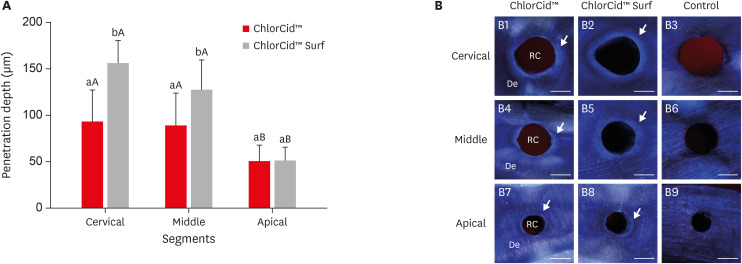
Figure 1
Figure 2
Figure 3
Figure 4
Mean and standard deviation of pH and free available chlorine in percentage (%) of weight/mass (w/w) of ChlorCid™ and ChlorCid™ Surf
| Solution | pH | Free available chlorine (% [m/m]) |
|---|---|---|
| ChlorCid™ | 12.27 ± 0.05* | 2.788 ± 0.047 |
| ChlorCid™ Surf | 13.08 ± 0.02 | 2.854 ± 0.044 |
*p < 0.0001.
*

 KACD
KACD
 ePub Link
ePub Link Cite
Cite

