Articles
- Page Path
- HOME > Restor Dent Endod > Volume 44(1); 2019 > Article
- Research Article The push-out bond strength of BIOfactor mineral trioxide aggregate, a novel root repair material
-
Makbule Bilge Akbulut
 , Durmus Alperen Bozkurt
, Durmus Alperen Bozkurt , Arslan Terlemez
, Arslan Terlemez , Melek Akman
, Melek Akman
-
Restor Dent Endod 2019;44(1):e5.
DOI: https://doi.org/10.5395/rde.2019.44.e5
Published online: January 28, 2019
Department of Endodontics, Faculty of Dentistry, Necmettin Erbakan University, Konya, Turkey.
- Correspondence to Makbule Bilge Akbulut, DDS, PhD. Assistant Professor, Department of Endodontics, Faculty of Dentistry, Necmettin Erbakan University, Ankara Street, Karatay, Konya 42050, Turkey. dt.bilge@yahoo.com
Copyright © 2019. The Korean Academy of Conservative Dentistry
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 2,060 Views
- 12 Download
- 25 Crossref
Abstract
-
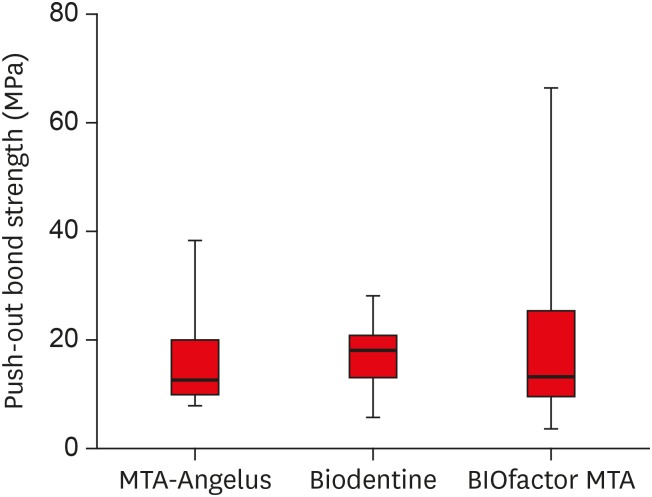
Objectives The aim of this in vitro study was to evaluate the push-out bond strength of a novel calcium silicate-based root repair material-BIOfactor MTA to root canal dentin in comparison with white MTA-Angelus (Angelus) and Biodentine (Septodont).
-
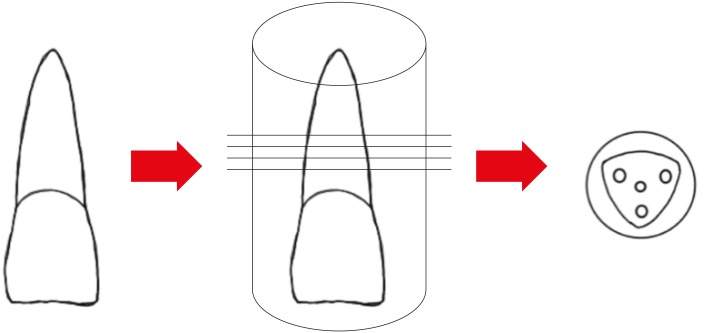
Materials and Methods The coronal parts of 12 central incisors were removed and the roots were embedded in acrylic resin blocks. Midroot dentin of each sample was horizontally sectioned into 1.1 mm slices and 3 slices were obtained from each root. Three canal-like standardized holes having 1 mm in diameter were created parallel to the root canal on each dentin slice with a diamond bur. The holes were filled with MTA-Angelus, Biodentine, or BIOfactor MTA. Wet gauze was placed over the specimens and samples were stored in an incubator at 37°C for 7 days to allow complete setting. Then samples were subjected to the push-out test method using a universal test machine with the loading speed of 1 mm/min. Data was statistically analyzed using Friedman test and post hoc Wilcoxon signed rank test with Bonferroni correction.
-
Results There were no significant differences among the push-out bond strength values of MTA-Angelus, Biodentine, and BIOfactor MTA (p > 0.017). Most of the specimens exhibited cohesive failure in all groups, with the highest rate found in Biodentine group.
-
Conclusions Based on the results of this study, MTA-Angelus, Biodentine, and BIOfactor MTA showed similar resistances to the push-out testing.
INTRODUCTION
MATERIALS AND METHODS
Compositions of tested root repair materials and instructions for use according to manufacturer
RESULTS
Failure mode distribution after the push-out test for root repair materials
| Failure type | MTA-Angelus | Biodentine | BIOfactor MTA |
|---|---|---|---|
| Adhesive | 1 (3.3) | 0 (0) | 0 (0) |
| Cohesive | 27 (90.0) | 29 (96.6) | 24 (80.0) |
| Mixed | 2 (6.6) | 1 (3.3) | 6 (20.0) |
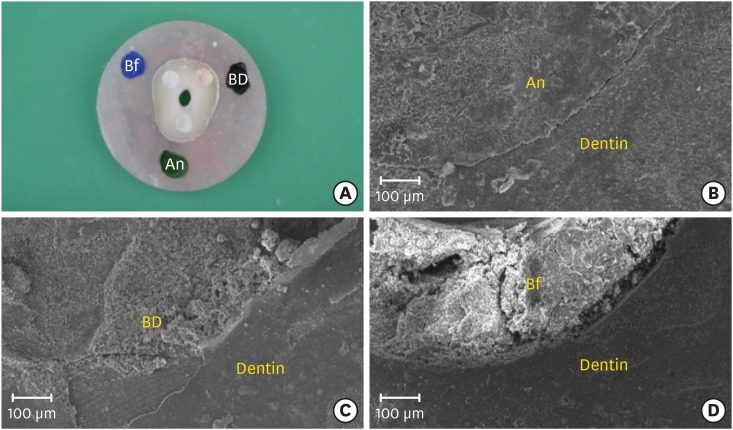
(A) Cohesive failure modes in randomly selected dentin disc (original magnification, ×25) and (B-D) representative scanning electron micrographs of root repair material-dentin interface after push-out testing; (B) MTA-Angelus (An), (C) Biodentine (BD), and (D) BIOfactor MTA (Bf) (original magnification, ×50).
DISCUSSION
CONCLUSIONS
ACKNOWLEDGEMENTS
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Akbulut MB, Terlemez A.
Data curation: Akbulut MB, Bozkurt DA, Terlemez A.
Formal analysis: Bozkurt DA, Terlemez A.
Funding acquisition: Akman M.
Investigation: Akbulut MB, Bozkurt DA, Terlemez A, Akman M.
Methodology: Akbulut MB, Bozkurt DA, Terlemez A, Akman M.
Project administration: Akbulut MB.
Resources: Akbulut MB.
Software: Akman M.
Supervision: Akbulut MB, Akman M.
Validation: Bozkurt DA, Terlemez A, Akman M.
Visualization: Akbulut MB.
Writing - original draft: Akbulut MB.
Writing - review & editing: Akbulut MB, Bozkurt DA, Terlemez A, Akman M.
- 1. Siew K, Lee AH, Cheung GS. Treatment outcome of repaired root perforation: a systematic review and meta-analysis. J Endod 2015;41:1795-1804.ArticlePubMed
- 2. Fuss Z, Trope M. Root perforations: classification and treatment choices based on prognostic factors. Endod Dent Traumatol 1996;12:255-264.ArticlePubMed
- 3. Clauder T, Shin SJ. Repair of perforations with MTA: clinical applications and mechanisms of action. Endod Topics 2006;15:32-55.Article
- 4. Parirokh M, Torabinejad M. Mineral trioxide aggregate: a comprehensive literature review--Part I: chemical, physical, and antibacterial properties. J Endod 2010;36:16-27.ArticlePubMed
- 5. Srinivasan V, Waterhouse P, Whitworth J. Mineral trioxide aggregate in paediatric dentistry. Int J Paediatr Dent 2009;19:34-47.ArticlePubMed
- 6. Butt N, Talwar S, Chaudhry S, Nawal RR, Yadav S, Bali A. Comparison of physical and mechanical properties of mineral trioxide aggregate and Biodentine. Indian J Dent Res 2014;25:692-697.ArticlePubMed
- 7. Marciano MA, Costa RM, Camilleri J, Mondelli RF, Guimarães BM, Duarte MA. Assessment of color stability of white mineral trioxide aggregate angelus and bismuth oxide in contact with tooth structure. J Endod 2014;40:1235-1240.ArticlePubMed
- 8. Camilleri J. Investigation of Biodentine as dentine replacement material. J Dent 2013;41:600-610.ArticlePubMed
- 9. Reyes-Carmona JF, Felippe MS, Felippe WT. The biomineralization ability of mineral trioxide aggregate and Portland cement on dentin enhances the push-out strength. J Endod 2010;36:286-291.ArticlePubMed
- 10. Scelza MZ, da Silva D, Scelza P, de Noronha F, Barbosa IB, Souza E, De Deus G. Influence of a new push-out test method on the bond strength of three resin-based sealers. Int Endod J 2015;48:801-806.ArticlePubMed
- 11. Skidmore LJ, Berzins DW, Bahcall JK. An in vitro comparison of the intraradicular dentin bond strength of Resilon and gutta-percha. J Endod 2006;32:963-966.ArticlePubMed
- 12. Kim HY. Statistical notes for clinical researchers: nonparametric statistical methods: 2. Nonparametric methods for comparing three or more groups and repeated measures. Restor Dent Endod 2014;39:329-332.ArticlePubMedPMC
- 13. Goracci C, Tavares AU, Fabianelli A, Monticelli F, Raffaelli O, Cardoso PC, Tay F, Ferrari M. The adhesion between fiber posts and root canal walls: comparison between microtensile and push-out bond strength measurements. Eur J Oral Sci 2004;112:353-361.ArticlePubMed
- 14. Drummond JL, Sakaguchi RL, Racean DC, Wozny J, Steinberg AD. Testing mode and surface treatment effects on dentin bonding. J Biomed Mater Res 1996;32:533-541.ArticlePubMed
- 15. Sousa-Neto MD, Silva Coelho FI, Marchesan MA, Alfredo E, Silva-Sousa YT. Ex vivo study of the adhesion of an epoxy-based sealer to human dentine submitted to irradiation with Er : YAG and Nd : YAG lasers. Int Endod J 2005;38:866-870.ArticlePubMed
- 16. Perdigão J. Dentin bonding-variables related to the clinical situation and the substrate treatment. Dent Mater 2010;26:e24-e37.ArticlePubMed
- 17. Carvalho NK, Prado MC, Senna PM, Neves AA, Souza EM, Fidel SR, Sassone LM, Silva EJ. Do smear-layer removal agents affect the push-out bond strength of calcium silicate-based endodontic sealers? Int Endod J 2017;50:612-619.ArticlePubMedPDF
- 18. Silva EJ, Carvalho NK, Prado MC, Zanon M, Senna PM, Souza EM, De-Deus G. Push-out bond strength of injectable pozzolan-based root canal sealer. J Endod 2016;42:1656-1659.ArticlePubMed
- 19. Silva EJ, Carvalho NK, Guberman MR, Prado M, Senna PM, Souza EM, De-Deus G. Push-out bond strength of fast-setting mineral trioxide aggregate and pozzolan-based cements: ENDOCEM MTA and ENDOCEM Zr. J Endod 2017;43:801-804.ArticlePubMed
- 20. Silva EJ, Carvalho NK, Zanon M, Senna PM, DE-Deus G, Zuolo ML, Zaia AA. Push-out bond strength of MTA HP, a new high-plasticity calcium silicate-based cement. Braz Oral Res 2016;30:e84.Article
- 21. Brichko J, Burrow MF, Parashos P. Design variability of the push-out bond test in endodontic research: a systematic review. J Endod 2018;44:1237-1245.ArticlePubMed
- 22. Nagas E, Uyanik O, Durmaz V, Cehreli ZC. Effect of plunger diameter on the push-out bond values of different root filling materials. Int Endod J 2011;44:950-955.ArticlePubMed
- 23. Pane ES, Palamara JE, Messer HH. Critical evaluation of the push-out test for root canal filling materials. J Endod 2013;39:669-673.ArticlePubMed
- 24. Stefaneli Marques JH, Silva-Sousa YT, Rached-Júnior FJ, Macedo LM, Mazzi-Chaves JF, Camilleri J, Sousa-Neto MD. Push-out bond strength of different tricalcium silicate-based filling materials to root dentin. Braz Oral Res 2018;32:e18.PubMed
- 25. Han L, Okiji T. Uptake of calcium and silicon released from calcium silicate-based endodontic materials into root canal dentine. Int Endod J 2011;44:1081-1087.ArticlePubMed
- 26. Duarte MA, Demarchi AC, Yamashita JC, Kuga MC, Fraga SC. pH and calcium ion release of 2 root-end filling materials. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003;95:345-347.ArticlePubMed
- 27. Atmeh AR, Chong EZ, Richard G, Festy F, Watson TF. Dentin-cement interfacial interaction: calcium silicates and polyalkenoates. J Dent Res 2012;91:454-459.ArticlePubMedPMCPDF
- 28. Antonijevic D, Medigovic I, Zrilic M, Jokic B, Vukovic Z, Todorovic L. The influence of different radiopacifying agents on the radiopacity, compressive strength, setting time, and porosity of Portland cement. Clin Oral Investig 2014;18:1597-1604.ArticlePubMedPDF
- 29. Bye GC. Portland cement: composition, production and properties. 2nd ed. London: Thomas Telford; 1999.
- 30. Alsubait SA. Effect of sodium hypochlorite on push-out bond strength of four calcium silicate-based endodontic materials when used for repairing perforations on human dentin: an in vitro evaluation. J Contemp Dent Pract 2017;18:289-294.ArticlePubMed
- 31. Dawood AE, Manton DJ, Parashos P, Wong RH, Palamara JE, Reynolds EC. Push-out bond strength of CPP-ACP-modified calcium silicate-based cements. Dent Mater J 2015;34:490-494.ArticlePubMed
- 32. Guneser MB, Akbulut MB, Eldeniz AU. Effect of various endodontic irrigants on the push-out bond strength of Biodentine and conventional root perforation repair materials. J Endod 2013;39:380-384.ArticlePubMed
- 33. Kadić S, Baraba A, Miletić I, Ionescu A, Brambilla E, Ivanišević Malčić A, Gabrić D. Push-out bond strength of three different calcium silicate-based root-end filling materials after ultrasonic retrograde cavity preparation. Clin Oral Investig 2018;22:1559-1565.ArticlePubMedPDF
- 34. Saghiri MA, Garcia-Godoy F, Gutmann JL, Lotfi M, Asatourian A, Ahmadi H. Push-out bond strength of a nano-modified mineral trioxide aggregate. Dent Traumatol 2013;29:323-327.ArticlePubMed
REFERENCES
Tables & Figures
REFERENCES
Citations

- Evaluation of marginal adaptation and bond strength of apical root canal plugs using different bioceramic cements
Michel Sena Fernandes Faria Lima, Alberto Nogueira da Gama Antunes, Kênia Maria Pereira Soares de Toubes, Fábio Fernandes Borém Bruzinga, Camila de Sousa Caneschi, Luís Fernando dos Santos Alves Morgan, Frank Ferreira Silveira
BMC Oral Health.2026;[Epub] CrossRef - Examination of the Bond Strength of Retrograde Filling in Teeth with Failed Apical Resection After Retreatment
Sevda Tok, Leyla Benan Ayranci
Applied Sciences.2025; 15(7): 3441. CrossRef - Comparative Analysis of Physicocomechanical Properties of MTA and Biodentine with Addition of Graphene Oxide to MTA and Biodentine: An In-vitro Study
Tanvi Arvind Jagtap, Budhabhushan A. Sonvane, Guruprasad Handal, Jayashri Nimba Bhangare, Kedar Vilas Saraf, Abhishek Mulay
Journal of Pharmacy and Bioallied Sciences.2025; 17(Suppl 1): S608. CrossRef - Influence of Incubation Duration on Bond Strength and Microhardness of Calcium Silicate‐Based Materials
Emine Şimşek, Makbule Bilge Akbulut
Australian Endodontic Journal.2025; 51(2): 438. CrossRef - Comparative evaluation of push-out bond strength after root perforation repair using recently introduced bioceramic and calcium silicate-based materials – An in vitro study
Gurinder Kaur, Deepak Kurup, Deepyanti Dubey, Ajit Hindlekar, Ganesh Ranganath Jadhav, Priya Mittal, Siddharth Shinde
Endodontology.2025; 37(2): 194. CrossRef - Comparative Evaluation of Push-out Bond Strength of Conventional Mineral Trioxide Aggregate, Biodentine, and Two Novel Antibacterial-enhanced Mineral Trioxide Aggregates
Sanjeev Khanagar, Suman Panda, Prabhadevi C Maganur, Ganesh Jeevanandan, Satish Vishwanathaiah, Ather A Syed, Sara Kalagi, Arokia RS Merlin, Vignesh Ravindran, Aram AlShehri
The Journal of Contemporary Dental Practice.2024; 25(2): 168. CrossRef - Influence of Phase Composition and Morphology on the Calcium Ion Release of Several Classical and Hybrid Endodontic Cements
Ivanka Dimitrova, Galia Gentscheva, Ivanka Spassova, Daniela Kovacheva
Materials.2024; 17(22): 5568. CrossRef - The Effect of Two Different MTA (Mineral Trioxide Aggregate) On Thermal Insulation
Gizem Akkus, Ecem Salmaz, Didem Oner Ozdas
The Open Dentistry Journal.2024;[Epub] CrossRef - Comparison of push‐out bond strength and apical microleakage of different calcium silicate‐based cements after using EDTA, chitosan and phytic acid irrigations
Tutku Koçak Şahin, Murat Ünal
Microscopy Research and Technique.2024; 87(9): 2072. CrossRef - In vitro evaluation of the physical characteristics and push-out bond strength of new experimental nano-MTA
Nada Omar, Yousra Aly, Haidy N. Salem
Bulletin of the National Research Centre.2024;[Epub] CrossRef - Interfacial characteristics of BIOfactor MTA and Biodentine with dentin
Makbule Bilge Akbulut, Şeref Nur Mutlu, Mehmet Ali Soylu, Emine Şimşek
Microscopy Research and Technique.2023; 86(2): 258. CrossRef - Systemic effect of calcium silicate-based cements with different radiopacifiers-histopathological analysis in rats
Osman Ataş, Kubra Bılge, Semsettin Yıldız, Serkan Dundar, Ilknur Calik, Asime Gezer Ataş, Alihan Bozoglan
PeerJ.2023; 11: e15376. CrossRef - The push-out bond strength of three root canal materials used in primary teeth: in vitro study
Hazal Özer, Merve Abaklı İnci, Sevcihan Açar Tuzluca
Frontiers in Dental Medicine.2023;[Epub] CrossRef - Effects of different irrigation protocols on push-out bond strength of pre-mixed calcium silicate-based cements
Sabiha Ceren İlisulu, Aliye Tugce Gürcan, Soner Sismanoglu
Journal of the Australian Ceramic Society.2023; 59(5): 1381. CrossRef - Micro-Computed Tomographic Evaluation of the Sealing Quality and Bond Strength of Different MTA Apical Plugs
Taibe Tokgöz Kaplan, Murat Selim Botsalı
European Journal of Therapeutics.2023; 30(1): 29. CrossRef - Kan kontaminasyonunun farklı kök ucu dolgu materyallerinin dentine bağlanma dayanımına etkisi
Şeyma Nur GERÇEKCİOĞLU, Melike BAYRAM, Emre BAYRAM
Acta Odontologica Turcica.2023; 40(1): 9. CrossRef - Tooth Discoloration Effect of BIOfactor Mineral Trioxide Aggregate: A 6-Month In Vitro Study
Şeref Nur Mutlu, Makbule Bilge Akbulut
Applied Sciences.2023; 13(15): 8914. CrossRef - Comparative Evaluation of the Push-Out Bond Strength of Root-End Filling Materials by Using Different Condensation Methods
Pelin Tüfenkçi, Sevinç Sevgi, Ayşenur Öncü, Fatma Semra Sevimay, Berkan Çelikten
Cyprus Journal of Medical Sciences.2022; 7(7): 115. CrossRef - Effect of Different Adhesive Strategies on the Microshear Bond Strength of Calcium-Silicate-Based Materials
Aliye Tuğçe Gürcan, Soner Şişmanoğlu, Görkem Sengez
Journal of Advanced Oral Research.2022; 13(2): 191. CrossRef - BIOfactor MTA’nın Radyoopasitesinin Dijital Radyografi ile Değerlendirilmesi
Şeref Nur MUTLU, Makbule Bilge AKBULUT
Selcuk Dental Journal.2022; 9(2): 520. CrossRef - Morphological and Chemical Analysis of Different Types of Calcium Silicate‐Based Cements
Okba Mahmoud, Nashwan Abdullah Al-Afifi, Mohideen Salihu Farook, Maysara Adnan Ibrahim, Saaid Al Shehadat, Mohammed Amjed Alsaegh, Sandrine Bittencourt Berger
International Journal of Dentistry.2022;[Epub] CrossRef - Influence of Blood Contamination on Push-Out Bond Strength of Three Calcium Silicate-Based Materials to Root Dentin
Cristina Rodrigues Paulo, Joana A. Marques, Diana B. Sequeira, Patrícia Diogo, Rui Paiva, Paulo J. Palma, João Miguel Santos
Applied Sciences.2021; 11(15): 6849. CrossRef - An In vitro comparative evaluation of effect of novel irrigant Qmix and 17% ethylenediaminetetraacetic acid on the push-out bond strength of biodentine and endosequence bioceramic root repair material
VandanaJ Gade, Aparajita Gangrade, JaykumarR Gade, Neelam Rahul
Journal of the International Clinical Dental Research Organization.2021; 13(2): 124. CrossRef - A micro-computed tomographic study using a novel test model to assess the filling ability and volumetric changes of bioceramic root repair materials
Fernanda Ferrari Esteves Torres, Jader Camilo Pinto, Gabriella Oliveira Figueira, Juliane Maria Guerreiro-Tanomaru, Mario Tanomaru-Filho
Restorative Dentistry & Endodontics.2021;[Epub] CrossRef - Micro-computed tomographic evaluation of the flow and filling ability of endodontic materials using different test models
Fernanda Ferrari Esteves Torres, Juliane Maria Guerreiro-Tanomaru, Gisselle Moraima Chavez-Andrade, Jader Camilo Pinto, Fábio Luiz Camargo Villela Berbert, Mario Tanomaru-Filho
Restorative Dentistry & Endodontics.2020;[Epub] CrossRef
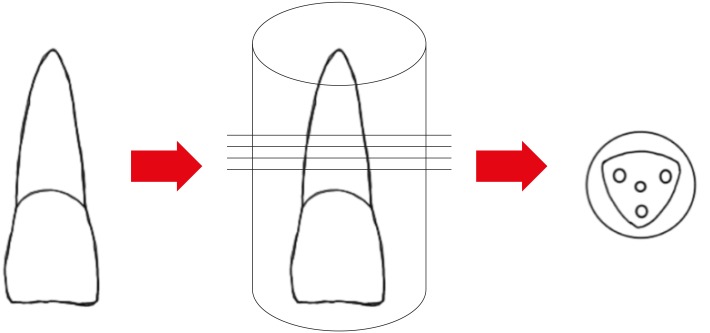

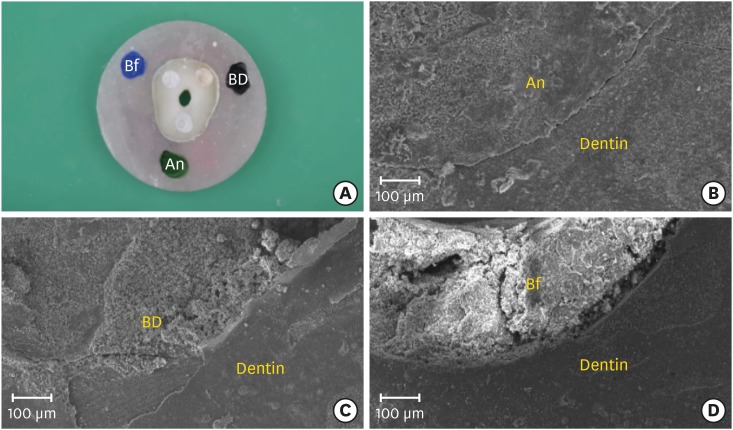
Figure 1
Figure 2
Figure 3
Compositions of tested root repair materials and instructions for use according to manufacturer
| Product and manufacturer | Composition | Instructions for use |
|---|---|---|
| MTA-Angelus (Angelus Industria de Produtos Odontologicos, Londrina, Brazil) | Powder: tricalcium silicate, dicalcium silicate, tricalcium aluminate, calcium oxide, bismuth oxide | Mix 1 scoop of powder with 1 drop of distilled water for 30 seconds |
| Liquid: distilled water | ||
| Biodentine (Septodont, St-Maur-des-fosses, France) | Powder: tricalcium silicate, dicalcium silicate, calcium carbonate, calcium oxide, zirconium oxide as a radiopacifier | Mix 1 capsule of powder with 5 drops of liquid for 30 seconds using amalgam mixing machine |
| Liquid: water, calcium chloride, hydrosoluble polymer (plasticizing agent) | ||
| BIOfactor MTA (Imicryl Dental, Konya, Turkey) | Powder: tricalcium silicate, dicalcium silicate, tricalcium aluminate, ytterbium oxide as a radiopacifier | Mix 3 scoops of powder with 1 drop of liquid until having a homogeneous consistency |
| Liquid: 0.5%–3% hydrosoluble carboxylated polymer, demineralized water |
Failure mode distribution after the push-out test for root repair materials
| Failure type | MTA-Angelus | Biodentine | BIOfactor MTA |
|---|---|---|---|
| Adhesive | 1 (3.3) | 0 (0) | 0 (0) |
| Cohesive | 27 (90.0) | 29 (96.6) | 24 (80.0) |
| Mixed | 2 (6.6) | 1 (3.3) | 6 (20.0) |
Values are presented as number (%).
Values are presented as number (%).

 KACD
KACD
 ePub Link
ePub Link Cite
Cite

