Articles
- Page Path
- HOME > Restor Dent Endod > Volume 44(4); 2019 > Article
-
Research Article
The effect of individualization of fiberglass posts using bulk-fill resin-based composites on cementation: an
in vitro study -
Rodrigo Barros Esteves Lins1
 , Jairo Matozinho Cordeiro2
, Jairo Matozinho Cordeiro2 , Carolina Perez Rangel1
, Carolina Perez Rangel1 , Thiago Bessa Marconato Antunes1
, Thiago Bessa Marconato Antunes1 , Luís Roberto Marcondes Martins1
, Luís Roberto Marcondes Martins1
-
Restor Dent Endod 2019;44(4):e37.
DOI: https://doi.org/10.5395/rde.2019.44.e37
Published online: October 18, 2019
1Department of Restorative Dentistry, Piracicaba Dental School, State University of Campinas, Piracicaba, SP, Brazil.
2Department of Prosthodontics and Periodontology, Piracicaba Dental School, University of Campinas, Piracicaba, SP, Brazil.
- Correspondence to Rodrigo Barros Esteves Lins, DDS, MSc. PhD Student, Department of Restorative Dentistry, Piracicaba Dental School, State University of Campinas, Av. Limeira, 901 Areião, Piracicaba, SP 13414-903, Brazil. rodrigowlins@hotmail.com
Copyright © 2019. The Korean Academy of Conservative Dentistry
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 1,459 Views
- 11 Download
- 6 Crossref
Abstract
-
Objectives This study evaluated the bond strength of various fiberglass post cementation techniques using different resin-based composites.
-
Materials and Methods The roots from a total of 100 bovine incisors were randomly assigned to 5 treatment groups: G1, post + Scotchbond Multi-Purpose (SBMP) + RelyX ARC luting agent; G2, relined post (Filtek Z250) + SBMP + RelyX ARC; G3, individualized post (Filtek Z250) + SBMP; G4, individualized post (Filtek Bulk-Fill) + SBMP; G5, individualized post (Filtek Bulk-Fill Flow) + SBMP. The samples were subjected to the push-out (n = 10) and pull-out (n = 10) bond strength tests. Data from the push-out bond strength test were analyzed using 2-way analysis of variance (ANOVA) with the Bonferroni post hoc test, and data from the pull-out bond strength test were analyzed using 1-way ANOVA.
-
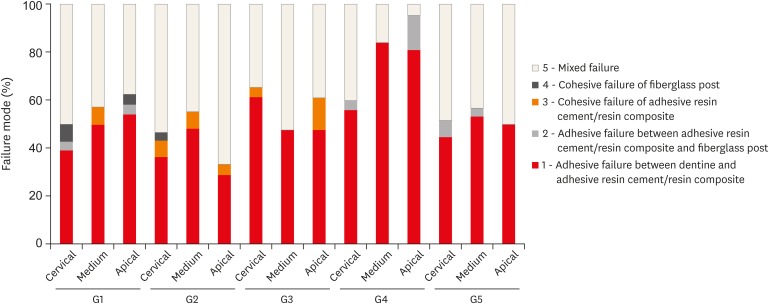
Results The data for push-out bond strength presented higher values for G2 and G5, mainly in the cervical and middle thirds, and the data from the apical third showed a lower mean push-out bond strength in all groups. No significant difference was noted for pull-out bond strength among all groups. The most frequent failure modes observed were adhesive failure between dentine and resin and mixed failure.
-
Conclusions Fiberglass post cementation using restorative and flowable bulk-fill composites with the individualization technique may be a promising alternative to existing methods of post cementation.
INTRODUCTION
MATERIALS AND METHODS
Material information evaluated in this study
Cementation protocol of each treatment group
RESULTS
Bond strength values obtained by push-out and pull-out bond strength tests
Distribution of failure modes (frequency, %) in 5 different cementation protocols and at 3 locations (the apical, middle, and cervical thirds) of the root canal dentin. The fracture modes were classified into 5 types.
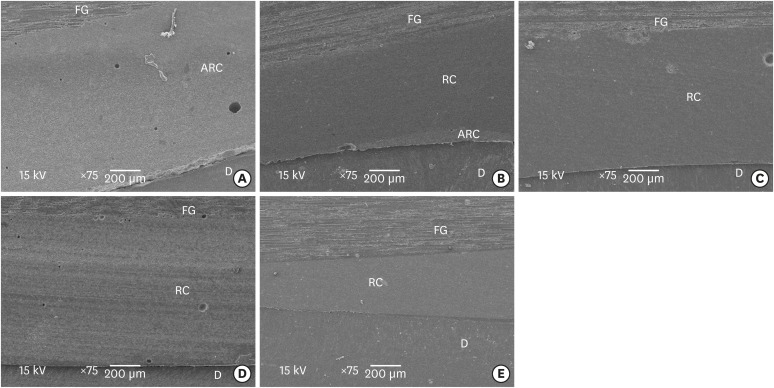
Scanning electron microscopic images of the adhesive interface present in each of the 5 groups (A, G1; B, G2; C, G3; D, G4; E, G5).
DISCUSSION
CONCLUSIONS
-
Funding: The authors acknowledge the financial support of FAPESP (#2016/17701-0).
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Lins RBE, Martins LRM.
Data curation: Rangel CP, Antunes TBM.
Formal analysis: Cordeiro JM.
Funding acquisition: Martins LRM.
Investigation: Lins RBE.
Methodology: Rangel C, Antunes TBM.
Project administration: Lins RBE.
Resources: Martins LRM.
Supervision: Lins RBE, Martins LRM.
Writing - original draft: Lins RBE.
Writing - review & editing: Cordeiro JM, Martins LRM.
- 1. Keul C, Köhler P, Hampe R, Roos M, Stawarczyk B. Glass fiber post/composite core systems bonded to human dentin: analysis of tensile load vs calculated tensile strength of various systems using pull-out tests. J Adhes Dent 2016;18:247-256.PubMed
- 2. Rezende EC, Gomes GM, Szesz AL, da Silveira Bueno CE, Reis A, Loguercio AD. Effects of dentin moisture on cementation of fiber posts to root canals. J Adhes Dent 2016;18:29-34.PubMed
- 3. Goracci C, Ferrari M. Current perspectives on post systems: a literature review. Aust Dent J 2011;56(Supplement 1):77-83.ArticlePubMed
- 4. Santos-Filho PC, Veríssimo C, Soares PV, Saltarelo RC, Soares CJ, Marcondes Martins LR. Influence of ferrule, post system, and length on biomechanical behavior of endodontically treated anterior teeth. J Endod 2014;40:119-123.ArticlePubMed
- 5. de Souza NC, Marcondes ML, da Silva D, Borges GA, Júnior LB, Spohr AM. Relined fiberglass post: effect of luting length, resin cement, and cyclic loading on the bond to weakened root dentin. Oper Dent 2016;41:e174-e182.ArticlePubMedPDF
- 6. Gruber YL, Bakaus TE, Gomes OM, Reis A, Gomes GM. Effect of dentin moisture and application mode of universal adhesives on the adhesion of glass fiber posts to root canal. J Adhes Dent 2017;19:385-393.PubMed
- 7. Zarpellon DC, Szesz AL, Loguercio AD, Arrais CA. Effect of sonic application of universal adhesive systems on bond strength of fiber posts to root canal. J Adhes Dent 2016;18:493-499.PubMed
- 8. Anchieta RB, Rocha EP, Almeida EO, Freitas AC Jr, Martin M Jr, Martini AP, Archangelo CM, Ko CC. Influence of customized composite resin fibreglass posts on the mechanics of restored treated teeth. Int Endod J 2012;45:146-155.ArticlePubMed
- 9. Conde DM, Rodrigues VP, Carvalho Souza SF, Bauer JR, Bramante FS, Linares Lima SN, Filho EM, Bandeca MC, de Mendonça AA, Lima DM. Influence of relining post on the bond strength of resin cements. J Contemp Dent Pract 2015;16:559-564.ArticlePubMed
- 10. Santana FR, Soares CJ, Silva JA, Alencar AH, Renovato SR, Lopes LG, Estrela C. Effect of instrumentation techniques, irrigant solutions and artificial accelerated aging on fiberglass post bond strength to intraradicular dentin. J Contemp Dent Pract 2015;16:523-530.ArticlePubMed
- 11. Grandini S, Goracci C, Monticelli F, Borracchini A, Ferrari M. SEM evaluation of the cement layer thickness after luting two different posts. J Adhes Dent 2005;7:235-240.PubMed
- 12. Fernandes AS, Shetty S, Coutinho I. Factors determining post selection: a literature review. J Prosthet Dent 2003;90:556-562.ArticlePubMed
- 13. Rosatto CM, Bicalho AA, Veríssimo C, Bragança GF, Rodrigues MP, Tantbirojn D, Versluis A, Soares CJ. Mechanical properties, shrinkage stress, cuspal strain and fracture resistance of molars restored with bulk-fill composites and incremental filling technique. J Dent 2015;43:1519-1528.ArticlePubMed
- 14. Marques EF, Bueno CE, Veloso HH, Almeida G, Pinheiro SL. Influence of instrumentation techniques and irrigating solutions on bond strength of glass fiber posts to root dentin. Gen Dent 2014;62:50-53.
- 15. Goracci C, Grandini S, Bossù M, Bertelli E, Ferrari M. Laboratory assessment of the retentive potential of adhesive posts: a review. J Dent 2007;35:827-835.ArticlePubMed
- 16. Shafiei F, Mohammadparast P, Jowkar Z. Adhesion performance of a universal adhesive in the root canal: effect of etch-and-rinse vs. self-etch mode. PLoS One 2018;13:e0195367.ArticlePubMedPMC
- 17. de Souza Batista VE, Vechiato-Filho AJ, Cesar PF, Coelho Goiato M, Cipriano Rangel E, Piza Pellizzer E, Ramos Verri F, Barão VA, Dos Santos DM. Surface characterization of a glass fiber post after nonthermal plasma treatment with hexamethyldisiloxane. J Adhes Dent 2017;19:525-533.
- 18. Mobarak E, Seyam R. Interfacial nanoleakage and bonding of self-adhesive systems cured with a modified-layering technique to dentin of weakened roots. Oper Dent 2013;38:E154-E165.ArticlePubMedPDF
- 19. Sarkis-Onofre R, Jacinto RC, Boscato N, Cenci MS, Pereira-Cenci T. Cast metal vs. glass fibre posts: a randomized controlled trial with up to 3 years of follow up. J Dent 2014;42:582-587.ArticlePubMed
- 20. Barcelos LM, Bicalho AA, Veríssimo C, Rodrigues MP, Soares CJ. Stress distribution, tooth remaining strain, and fracture resistance of endodontically treated molars restored without or with one or two fiberglass posts and direct composite resin. Oper Dent 2017;42:646-657.ArticlePubMedPDF
- 21. Macedo VC, Faria e Silva AL, Martins LR. Effect of cement type, relining procedure, and length of cementation on pull-out bond strength of fiber posts. J Endod 2010;36:1543-1546.ArticlePubMed
- 22. Gomes GM, Gomes OM, Reis A, Gomes JC, Loguercio AD, Calixto AL. Effect of operator experience on the outcome of fiber post cementation with different resin cements. Oper Dent 2013;38:555-564.ArticlePubMedPDF
- 23. Caixeta RV, Guiraldo RD, Kaneshima EN, Barbosa AS, Picolotto CP, Lima AE, Gonini Júnior A, Berger SB. Push-out bond strength of restorations with bulk-fill, flow, and conventional resin composites. Sci World J 2015;2015:452976.ArticlePubMedPMCPDF
- 24. Lins RB, Aristilde S, Osório JH, Cordeiro CM, Yanikian CR, Bicalho AA, Stape TH, Soares CJ, Martins LR. Biomechanical behaviour of bulk-fill resin composites in class II restorations. J Mech Behav Biomed Mater 2019;98:255-261.ArticlePubMed
- 25. Leprince JG, Palin WM, Vanacker J, Sabbagh J, Devaux J, Leloup G. Physico-mechanical characteristics of commercially available bulk-fill composites. J Dent 2014;42:993-1000.ArticlePubMed
- 26. Francis AV, Braxton AD, Ahmad W, Tantbirojn D, Simon JF, Versluis A. Cuspal flexure and extent of cure of a bulk-fill flowable base composite. Oper Dent 2015;40:515-523.ArticlePubMedPDF
- 27. Marovic D, Tauböck TT, Attin T, Panduric V, Tarle Z. Monomer conversion and shrinkage force kinetics of low-viscosity bulk-fill resin composites. Acta Odontol Scand 2015;73:474-480.ArticlePubMed
- 28. Castellan CS, Santos-Filho PC, Soares PV, Soares CJ, Cardoso PE. Measuring bond strength between fiber post and root dentin: a comparison of different tests. J Adhes Dent 2010;12:477-485.PubMed
- 29. Ferrari M, Mannocci F, Vichi A, Cagidiaco MC, Mjör IA. Bonding to root canal: structural characteristics of the substrate. Am J Dent 2000;13:255-260.PubMed
- 30. Park JS, Lee JS, Park JW, Chung WG, Choi EH, Lee Y. Comparison of push-out bond strength of fiber-reinforced composite resin posts according to cement thickness. J Prosthet Dent 2017;118:372-378.ArticlePubMed
- 31. Santos-Filho PC, Castro CG, Silva GR, Campos RE, Soares CJ. Effects of post system and length on the strain and fracture resistance of root filled bovine teeth. Int Endod J 2008;41:493-501.ArticlePubMed
- 32. de Assis FS, Lima SN, Tonetto MR, Bhandi SH, Pinto SC, Malaquias P, Loguercio AD, Bandéca MC. Evaluation of bond strength, marginal integrity, and fracture strength of bulk- vs incrementally-filled restorations. J Adhes Dent 2016;18:317-323.PubMed
- 33. Machado FW, Bossardi M, Ramos TS, Valente LL, Münchow EA, Piva E. Application of resin adhesive on the surface of a silanized glass fiber-reinforced post and its effect on the retention to root dentin. J Endod 2015;41:106-110.ArticlePubMed
- 34. Nova V, Karygianni L, Altenburger MJ, Wolkewitz M, Kielbassa AM, Wrbas KT. Pull-out bond strength of a fibre-reinforced composite post system luted with self-adhesive resin cements. J Dent 2013;41:1020-1026.ArticlePubMed
REFERENCES
Tables & Figures
REFERENCES
Citations

- EVALUATION OF PUSH-OUT BOND STRENGTH OF GLASS FIBER POSTS USING DIFFERENT LUTING CEMENTS
Jannah Mohammed, Maha Agha
BULLETIN OF STOMATOLOGY AND MAXILLOFACIAL SURGERY.2025; : 274. CrossRef - Effects of a relined fiberglass post with conventional and self-adhesive resin cement
Wilton Lima dos Santos Junior, Marina Rodrigues Santi, Rodrigo Barros Esteves Lins, Luís Roberto Marcondes Martins
Restorative Dentistry & Endodontics.2024;[Epub] CrossRef - Fracture resistance of weakened roots restored with relined or milled CAD-CAM glass fiber posts
Belizane das Graças Oliveira MAIA, Thais da Silva Alves SANTOS, Cláudio Antonio Talge CARVALHO, Francielle Silvestre VERNER, Rafael Binato JUNQUEIRA
Dental Materials Journal.2023; 42(1): 92. CrossRef - Evaluation of pretreatments on intra‐radicular dentin bond strength of self‐adhesive resin cements
Marina Rodrigues Santi, Rodrigo Barros Esteves Lins, Beatriz Ometto Sahadi, Luís Roberto Marcondes Martins, Jorge Rodrigo Soto‐Montero
Journal of Esthetic and Restorative Dentistry.2022; 34(7): 1051. CrossRef - Comparison of the Mechanical Properties and Push-out Bond Strength of Self-adhesive and Conventional Resin Cements on Fiber Post Cementation
MR Santi, RBE Lins, BO Sahadi, JR Soto-Montero, LRM Martins
Operative Dentistry.2022; 47(3): 346. CrossRef - Glass fiber posts
Renata Pereira, Rodrigo Barros Esteves Lins, Victória Castelan Rodrigues, Débora Alves Nunes Leite Lima, Luís Roberto Marcondes Martins, Flávio Henrique Baggio Aguiar
Brazilian Journal of Oral Sciences.2020; 19: e207508. CrossRef
- Figure
- Related articles
-
- The influence of bioactive glass (BGS-7) on enamel remineralization: an in vitro study
- Cleaning protocols to enhance bond strength of fiberglass posts on root canals filled with bioceramic sealer: an in vitro comparative study
- The effect of limonene extract on the adhesion of different endodontic cements to root dentin: an in vitro experimental study
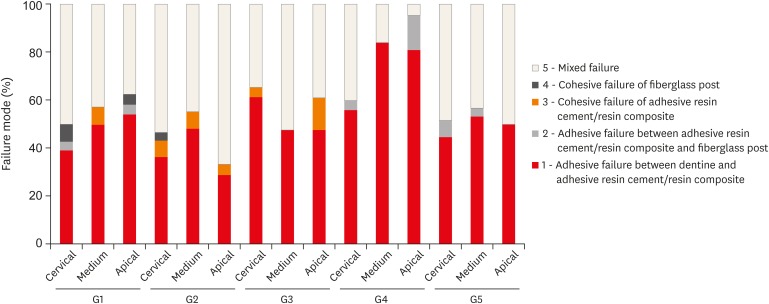
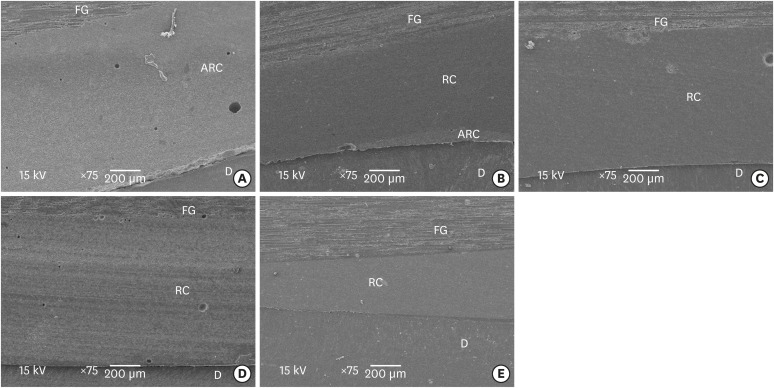
Figure 1
Figure 2
Material information evaluated in this study
| Material | Description | Composition | Shade | Manufacturer |
|---|---|---|---|---|
| Filtek Z250 | Universal restorative resin composite | Bis-EMA, UDMA, Bis-GMA, TEGDMA, silane-treated ceramic, aluminum oxide (#81465) | A2 | 3M ESPE, St. Paul, MN, USA |
| Filtek Bulk Fill | Restorative bulk-fill resin composite | Aromatic urethane dimethacrylate, YbF3, UDMA, silane-treated ceramic, silica and zirconia, DDDMA, water, EDMAB, benzotriazole, titanium dioxide (#N685666) | A2 | |
| Filtek Bulk Fill Flow | Restorative flowable bulk-fill resin composite | UDMA, Bis-EMA, YbF3, Bis-GMA, TEGDMA, silane-treated ceramic, substituted dimethacrylate, benzotriazole, ethyl 4-(dimethylamino) benzoate (#N706754) | A2 | |
| Ceramic Primer | Silane agent | Ethyl alcohol, water, methacryloxypropyltrimethoxysilane (#N699035) | - | |
| Scotchbond Multi–Purpose | Activator | Ethyl alcohol (#N708060) | - | |
| Primer | Water, HEMA, copolymer of acrylic and itaconic acids (#1801700484) | - | ||
| Catalyst | Bis-GMA, HEMA, triphenylantimony, triphenylphosphine, hydroquinone (#N562953) | - | ||
| Adhesive | Bis-GMA, HEMA, triphenylantimony (#N808224) | - | ||
| RelyX ARC (ARC) | Adhesive resin cement | Paste A: Bis-GMA, TEGDMA, silane-treated ceramic and silica, reacted polycaprolactone polymer, 2-benzotriazolyl-4-methylphenol, EDMAB, 4-(dimethylamino)-benzeneethanol | A1 | |
| Paste B: Bis-GMA, TEGDMA, silane-treated ceramic and silica, reacted polycaprolactone polymer, 2-benzotriazolyl-4-methylphenol, benzoyl peroxide (#N696957) |
ARC, adhesive resin cement; Bis-EMA, ethoxylated bisphenol A dimethacrylate; UDMA, urethane dimethacrylate; Bis-GMA, bisphenol A diglycidyl ether dimethacrylate; TEGDMA, triethyleneglycol dimethacrylate; YbF3, ytterbium fluoride; DDDMA, 1,12-dodecane dimethacrylate; EDMAB, ethyl 4-(dimethylamino)benzoate; HEMA, 2-hydroxyethyl methacrylate; EDMAB, ethyl 4-(dimethylamino)benzoate; #, lot number.
Cementation protocol of each treatment group
| Group | Technique | Cementation protocol |
|---|---|---|
| G1 | Fiberglass post + SBMP + ARC | 1. Apply 35% phosphoric acid to the fiberglass post; |
| 2. Rinse with water, then dry; | ||
| 3. Apply Ceramic Primer, followed by a 5-minute wait; | ||
| 4. Apply bond with a disposable brush; perform strong volatilization and photoactivation for 20 seconds; | ||
| 5. Acid etch the canal with 35% phosphoric acid for 15 seconds; | ||
| 6. Rinse for 15 seconds with water; | ||
| 7. Dry with a paper point; | ||
| 8. Apply SBMP with a disposable brush for each material (activator, primer, and catalyst), followed by removable of any excess with a paper point; | ||
| 9. Manipulate and apply RelyX ARC into the canal with a Centrix syringe; | ||
| 10. Position the Fiberglass post into the canal with digital pressure; | ||
| 11. Wait for 5 minutes, then light-cure the resin (VALO, Ultradent, South Jordan, UT, USA) for 40 seconds for each side. | ||
| G2 | Relined fiberglass post (Filtek Z250 resin composite) + SBMP + ARC | 1. Apply 35% phosphoric acid to the fiberglass post; |
| 2. Rinse with water, then dry; | ||
| 3. Apply Ceramic Primer, followed by a 5-minute wait; | ||
| 4. Apply bond with a disposable brush; perform strong volatilization and photoactivation for 20 seconds; | ||
| 5. Apply water-soluble lubricant to the canal; | ||
| 6. Manipulate the resin composite onto the fiberglass post and position it into the canal; | ||
| 7. Perform photoactivation for 3 seconds, then remove from the canal for 40 seconds to complete the light-curing process; | ||
| 8. Rinse and dry the canal; | ||
| Repeat steps 5–11 from the G1 cementation protocol. | ||
| G3 | Individualized fiberglass post (Filtek Z250 resin composite) + SBMP | 1. Apply 35% phosphoric acid to the fiberglass post; |
| 2. Rinse with water, then dry; | ||
| 3. Apply Ceramic Primer, followed by a 5-minute wait; | ||
| 4. Apply bond with a disposable brush; perform strong volatilization and photoactivation for 20 seconds; | ||
| 5. Acid etch the canal with 35% phosphoric acid for 15 seconds; | ||
| 6. Rinse for 15 seconds with water; | ||
| 7. Dry with a paper point; | ||
| 8. Apply primer and adhesive with a disposable brush; perform volatilization and photoactivation for 20 seconds; | ||
| 9. Position the Fiberglass post into the canal and insert the conventional resin composite with a resin spatula using the incremental technique (with a thickness of 2 mm); | ||
| 10. Perform occlusal photoactivation of each layer for 40 seconds. | ||
| G4 | Individualized fiberglass post (Filtek Bulk Fill resin composite) + SBMP | Repeat the G3 cementation protocol (above), with the exception of: |
| 9. Position the Fiberglass post into the canal and insert the bulk-fill resin composite with a resin spatula using the bulk-fill technique (with a thickness of 4 mm); | ||
| 10. Perform occlusal photoactivation for 20 seconds from the occlusal end. | ||
| G5 | Individualized fiberglass post (Filtek Bulk Fill Flow resin composite) + SBMP | Repeat the G3 cementation protocol (above), with the exception of: |
| 9. Position the Fiberglass post into the canal and insert the bulk-fill flow resin composite using the bulk technique (with a thickness of 4 mm); | ||
| 10. Perform occlusal photoactivation for 20 seconds from the occlusal end. |
SBMP, Scotchbond Multi–Purpose; ARC, Adhesive resin cement.
Bond strength values obtained by push-out and pull-out bond strength tests
| Group | Push-out by canal root region | Pull-out | ||
|---|---|---|---|---|
| Cervical | Medium | Apical | ||
| 1 | 4.38 ± 1.13Ac | 4.62 ± 1.47Ab | 4.67 ± 2.08Aa | 4.77 ± 1.04a |
| 2 | 7.89 ± 2.68Aa | 7.06 ± 1.95Aa | 4.90 ± 1.80Ba | 4.94 ± 0.69a |
| 3 | 4.58 ± 2.34Ac | 3.01 ± 1.76Bc | 2.76 ± 1.38Bb | 4.94 ± 1.00a |
| 4 | 4.48 ± 1.41Ac | 4.53 ± 2.12Ab | 3.82 ± 2.25Aab | 5.59 ± 1.01a |
| 5 | 6.18 ± 2.61Ab | 6.26 ± 2.49Aa | 4.53 ± 2.98Ba | 4.83 ± 1.41a |
Data are presented as mean ± standard deviation (unit: MPa). Different uppercase letters indicate significant differences between root regions in the same row. Different lowercase letters indicate significant differences between groups in the same column (p < 0.05).
ARC, adhesive resin cement; Bis-EMA, ethoxylated bisphenol A dimethacrylate; UDMA, urethane dimethacrylate; Bis-GMA, bisphenol A diglycidyl ether dimethacrylate; TEGDMA, triethyleneglycol dimethacrylate; YbF3, ytterbium fluoride; DDDMA, 1,12-dodecane dimethacrylate; EDMAB, ethyl 4-(dimethylamino)benzoate; HEMA, 2-hydroxyethyl methacrylate; EDMAB, ethyl 4-(dimethylamino)benzoate; #, lot number.
SBMP, Scotchbond Multi–Purpose; ARC, Adhesive resin cement.
Data are presented as mean ± standard deviation (unit: MPa). Different uppercase letters indicate significant differences between root regions in the same row. Different lowercase letters indicate significant differences between groups in the same column (

 KACD
KACD
 ePub Link
ePub Link Cite
Cite

