Articles
- Page Path
- HOME > Restor Dent Endod > Volume 42(3); 2017 > Article
- Research Article Comparing the effect of a desensitizing material and a self-etch adhesive on dentin sensitivity after periodontal surgery: a randomized clinical trial
-
Hila Hajizadeh1,2, Atefeh Nemati-Karimooy2
 , Sara Majidinia1,2, Amir Moeintaghavi3, Marjaneh Ghavamnasiri1
, Sara Majidinia1,2, Amir Moeintaghavi3, Marjaneh Ghavamnasiri1 -
2017;42(3):-175.
DOI: https://doi.org/10.5395/rde.2017.42.3.168
Published online: July 21, 2017
1Dental Research Center, Mashhad University of Medical Sciences, Mashhad, Iran.
2Department of Restorative and Cosmetic Dentistry, School of Dentistry, Mashhad University of Medical Sciences, Mashhad, Iran.
3Department of Periodontics, School of Dentistry, Mashhad University of Medical Sciences, Mashhad, Iran.
- Correspondence to Atefeh Nemati-Karimooy, DDS, MS. Assistant Professor, Department of Restorative and Cosmetic Dentistry, Mashhad University of Medical Sciences School of Dentistry, Vakil-Abad Blvd., Mashhad 91735, Iran. Tel: +98-9151098060, Fax: +98-51-38832300, Nematika@mums.ac.ir
Copyright © 2017. The Korean Academy of Conservative Dentistry
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 2,199 Views
- 10 Download
- 10 Crossref
Abstract
-
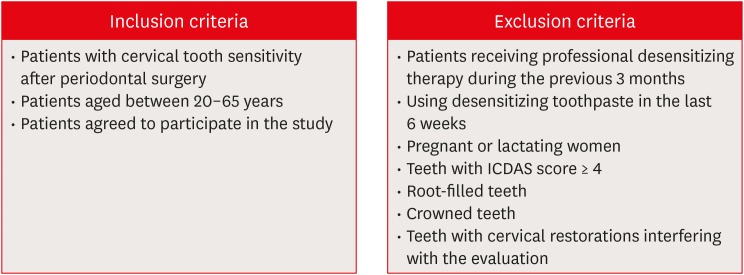
Objectives This double-blind randomized placebo-controlled clinical trial evaluated the ability of a desensitizing agent and a self-etch adhesive on cervical dentin sensitivity (CDS) after periodontal surgery.
-
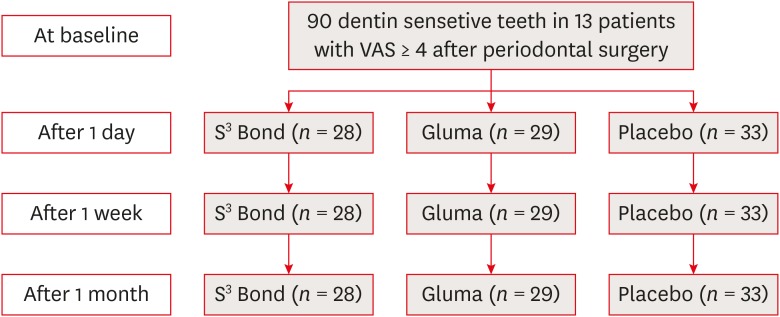
Materials and Methods Ninety hypersensitive teeth of 13 subjects were included in the study. After periodontal surgery, the teeth of each posterior sextant treated with one of the following materials: G1: Clearfil S3 Bond (Kuraray Dental), G2: Gluma Desensitizer (Heraeus Kulzer), and G3: placebo (water). The sensitivity was assessed using evaporative stimuli before treatment (baseline, T0), 1 day after treatment (T1), after 1 week (T2), and after 1 month (T3) according to visual analog scale (VAS).
-
Results Following the treatment, all the 3 groups showed significant reduction of CDS in T1 compared to T0. Reduction of CDS between T1 and T2 was observed only in G1 but there was no significant difference between T2 and T3 in this group. Although we observed a significant difference in T3 compared to T1 and T2 in G2 and G3, comparison of treatment groups in each assessment time showed a significant difference only in T3. According to paired comparison, this was due to the difference between G2 and G3.
-
Conclusions Dentin sensitivity following periodontal surgery will decrease spontaneously over time, but treating the sensitive teeth with Gluma Desensitizer and Clearfil S3 Bond can have some benefits.
INTRODUCTION
MATERIALS AND METHODS
RESULTS
Mean visual analog scale (VAS) scores for each treatment group within each assessment time
DISCUSSION
CONCLUSIONS
ACKNOWLEDGEMENT
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Ghavamnasiri M.
Data curation: Hajizadeh H.
Formal analysis: Moeintaghavi A.
Funding acquisition: Hajizadeh H.
Investigation: Nemati-Karimooy A.
Methodology: Moeintaghavi A.
Project administration: Hajizadeh H.
Software: Hajizadeh H.
Supervision: Ghavamnasiri M.
Validation: Majidinia S.
Visualization: Ghavamnasiri M.
Writing - original draft: Nemati-Karimooy A, Hajizadeh H.
Writing - review & editing: Nemati-Karimooy A, Majidinia S, Ghavamnasiri M.
- 1. Davari A, Ataei E, Assarzadeh H. Dentin hypersensitivity: etiology, diagnosis and treatment; a literature review. J Dent (Shiraz) 2013;14:136-145.PubMedPMC
- 2. Canadian Advisory Board on Dentin Hypersensitivity. Consensus-based recommendations for the diagnosis and management of dentin hypersensitivity. J Can Dent Assoc 2003;69:221-226.PubMed
- 3. Splieth CH, Tachou A. Epidemiology of dentin hypersensitivity. Clin Oral Investig 2013;17(Supplement 1):S3-S8.ArticlePubMedPDF
- 4. Walters PA. Dentinal hypersensitivity: a review. J Contemp Dent Pract 2005;6:107-117.Article
- 5. Brännström M, Åström A. A study on the mechanism of pain elicited from the dentin. J Dent Res 1964;43:619-625.ArticlePubMedPDF
- 6. Yoshiyama M, Suge T, Kawasaki A, Ebisu S. Morphological characterization of tube-like structures in hypersensitive human radicular dentine. J Dent 1996;24:57-63.PubMed
- 7. Ling TY, Gillam DG. The effectiveness of desensitizing agents for the treatment of cervical dentine sensitivity (CDS)--a review. J West Soc Periodontol Periodontal Abstr 1996;44:5-12.PubMed
- 8. Lin PY, Cheng YW, Chu CY, Chien KL, Lin CP, Tu YK. In-office treatment for dentin hypersensitivity: a systematic review and network meta-analysis. J Clin Periodontol 2013;40:53-64.ArticlePubMedPDF
- 9. Fu B, Shen Y, Wang H, Hannig M. Sealing ability of dentin adhesives/desensitizer. Oper Dent 2007;32:496-503.ArticlePubMedPDF
- 10. Grégoire G, Joniot S, Guignes P, Millas A. Dentin permeability: self-etching and one-bottle dentin bonding systems. J Prosthet Dent 2003;90:42-49.ArticlePubMed
- 11. Tsuchiya S, Nikaido T, Sonoda H, Foxton RM, Tagami J. Ultrastructure of the dentin-adhesive interface after acid-base challenge. J Adhes Dent 2004;6:183-190.PubMed
- 12. Yu X, Liang B, Jin X, Fu B, Hannig M. Comparative in vivo study on the desensitizing efficacy of dentin desensitizers and one-bottle self-etching adhesives. Oper Dent 2010;35:279-286.ArticlePubMedPDF
- 13. Al-Sabbagh M, Beneduce C, Andreana S, Ciancio SG. Incidence and time course of dentinal hypersensitivity after periodontal surgery. Gen Dent 2010;58:e14-e19.PubMed
- 14. Nishida M, Murayama Y, Nomura Y, Asano K, Ujimoto F, Shinoda S, Sakan J, Uchida A, Katamsi D, Yokomizo I. Hypersensitivity of the exposed root surface after the surgical periodontal treatment. Nippon Shishubyo Gakkai Kaishi 1976;18:502-510.
- 15. Lin YH, Gillam DG. The prevalence of root sensitivity following periodontal therapy: a systematic review. Int J Dent 2012;2012:407023.ArticlePubMedPMCPDF
- 16. Absi EG, Addy M, Adams D. Dentine hypersensitivity. A study of the patency of dentinal tubules in sensitive and non-sensitive cervical dentine. J Clin Periodontol 1987;14:280-284.PubMed
- 17. Duran I, Sengun A. The long-term effectiveness of five current desensitizing products on cervical dentine sensitivity. J Oral Rehabil 2004;31:351-356.ArticlePubMed
- 18. Gillam DG, Coventry JF, Manning RH, Newman HN, Bulman JS. Comparison of two desensitizing agents for the treatment of cervical dentine sensitivity. Endod Dent Traumatol 1997;13:36-39.ArticlePubMed
- 19. Ide M, Morel AD, Wilson RF, Ashley FP. The role of a dentine-bonding agent in reducing cervical dentine sensitivity. J Clin Periodontol 1998;25:286-290.PubMed
- 20. Prati C, Cervellati F, Sanasi V, Montebugnoli L. Treatment of cervical dentin hypersensitivity with resin adhesives: 4-week evaluation. Am J Dent 2001;14:378-382.PubMed
- 21. Swift EJ Jr, May KN Jr, Mitchell S. Clinical evaluation of Prime & Bond 2.1 for treating cervical dentin hypersensitivity. Am J Dent 2001;14:13-16.PubMed
- 22. Kakaboura A, Rahiotis C, Thomaidis S, Doukoudakis S. Clinical effectiveness of two agents on the treatment of tooth cervical hypersensitivity. Am J Dent 2005;18:291-295.PubMed
- 23. Inoue G, Tsuchiya S, Nikaido T, Foxton RM, Tagami J. Morphological and mechanical characterization of the acid-base resistant zone at the adhesive-dentin interface of intact and caries-affected dentin. Oper Dent 2006;31:466-472.ArticlePubMedPDF
- 24. Nikaido T, Inoue G, Takagaki T, Waidyasekera K, Iida Y, Shinohara MS, Sadr A, Tagami J. New strategy to create “Super Dentin” using adhesive technology: reinforcement of adhesive–dentin interface and protection of tooth structures. Jpn Dent Sci Rev 2011;47:31-42.Article
- 25. Polderman RN, Frencken JE. Comparison between effectiveness of a low-viscosity glass ionomer and a resin-based glutaraldehyde containing primer in treating dentine hypersensitivity--a 25.2-month evaluation. J Dent 2007;35:144-149.ArticlePubMed
- 26. Aranha AC, Pimenta LA, Marchi GM. Clinical evaluation of desensitizing treatments for cervical dentin hypersensitivity. Braz Oral Res 2009;23:333-339.PubMed
- 27. Qin C, Xu J, Zhang Y. Spectroscopic investigation of the function of aqueous 2-hydroxyethylmethacrylate/glutaraldehyde solution as a dentin desensitizer. Eur J Oral Sci 2006;114:354-359.ArticlePubMed
- 28. Kawasaki A, Ishikawa K, Suge T, Shimizu H, Suzuki K, Matsuo T, Ebisu S. Effects of plaque control on the patency and occlusion of dentine tubules in situ . J Oral Rehabil 2001;28:439-449.ArticlePubMed
- 29. Pashley DH. Dentin permeability, dentin sensitivity, and treatment through tubule occlusion. J Endod 1986;12:465-474.ArticlePubMed
- 30. Pashley DH, Nelson R, Kepler EE. The effects of plasma and salivary constituents on dentin permeability. J Dent Res 1982;61:978-981.ArticlePubMedPDF
REFERENCES
Tables & Figures
REFERENCES
Citations

- Biomineralization reaction from nanosized calcium silicate: A new method for reducing dentin hypersensitivity
Mi-Jeong Jeon, Yu-Sung Choi, Jeong-Kil Park, Jin-Soo Ahn, Yu-Chih Chiang, Deog-Gyu Seo
Journal of Dental Sciences.2025; 20(1): 428. CrossRef - Effectiveness of Self-etching Adhesive Only Versus in Combination with Gluma Desensitizer for Preventing Post-composite Sensitivity - A Prospective Study
Hemamalini Rath, Shilpa Mahapatra, Sri Priya Narayanan
Indian Journal of Dental Research.2025; 36(1): 32. CrossRef - Efficacy of seventh generation bonding agents as desensitizers in patients with dentin hypersensitivity: a randomized clinical trial
Sumaiya Shabbir, Shahbaz Ahmed, Syed Jaffar Abbas Zaidi, Sania Riaz, Huma Sarwar, Muhammad Taqi, Zia ur Rahman Khan
BMC Oral Health.2024;[Epub] CrossRef - Investigation of the crystal formation from calcium silicate in human dentinal tubules and the effect of phosphate buffer saline concentration
Mi-Jeong Jeon, Jin-Soo Ahn, Jeong-Kil Park, Deog-Gyu Seo
Journal of Dental Sciences.2024; 19(4): 2278. CrossRef - The effect of fluoride iontophoresis on seal ability of self-etch adhesive in human dentin in vitro
Kanittha Kijsamanmith, Parintorn Wallanon, Chanya Pitchayasatit, Poonnapha Kittiratanaviwat
BMC Oral Health.2022;[Epub] CrossRef - The study of toothpaste desensitizing properties
S. B. Ulitovskiy, O. V. Kalinina, A. A. Leontev, O. V. Khabarova, L. I. Pankrateva, E. S. Soloveva, N. K. Fok
Parodontologiya.2022; 27(1): 81. CrossRef - Effectiveness and cytotoxicity of two desensitizing agents: a dentin permeability measurement and dentin barrier testing in vitro study
Ruodan Jiang, Yongxiang Xu, Feilong Wang, Hong Lin
BMC Oral Health.2022;[Epub] CrossRef - A randomized clinical trial of dentin hypersensitivity reduction over one month after a single topical application of comparable materials
Samar Hatem Abuzinadah, Abdulrahman Jafar Alhaddad
Scientific Reports.2021;[Epub] CrossRef - Comparison between effectiveness of dentine desensitizer and one bottle self-etch adhesive on dentine hypersensitivity
Muhammad Zohaib Younus, Muhammad Adeel Ahmed, Azeem Ul Yaqin Syed, Jiand Malik Baloch, Muhammad Ali, Abubakar Sheikh
Technology and Health Care.2021; 29(6): 1153. CrossRef - A long-term evaluation of experimental potassium oxalate concentrations on dentin hypersensitivity reduction: A triple-blind randomized clinical trial
Alexia da Mata Galvão, Livia Fávaro Zeola, Guilherme Faria Moura, Daniela Navarro Ribeiro Teixeira, Ramon Corrêa de Queiroz Gonzaga, Gisele Rodrigues da Silva, Paulo Vinícius Soares
Journal of Dentistry.2019; 89: 103180. CrossRef
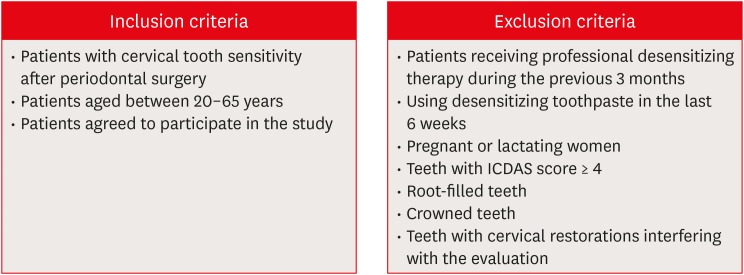
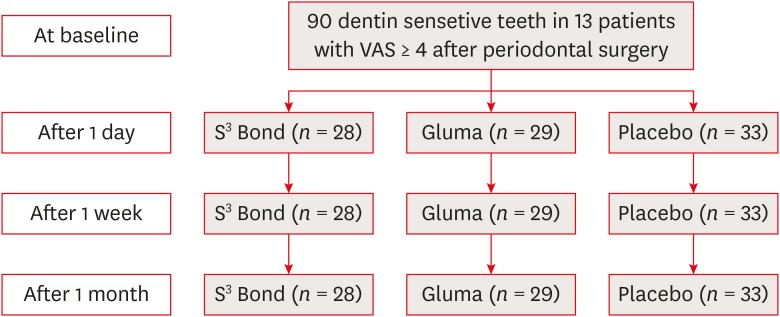
Figure 1
Figure 2
Mean visual analog scale (VAS) scores for each treatment group within each assessment time
| Material | Baseline (T0) | One day (T1) | One week (T2) | One month (T3) |
|---|---|---|---|---|
| S3 Bond (G1) | 5.38 ± 1.62Aa | 3.70 ± 1.97Ab | 3.10 ± 1.67Ac | 2.46 ± 1.10ABc |
| Gluma Desensitizer (G2) | 5.15 ± 1.39Aa | 2.92 ± 1.37Ab | 2.42 ± 1.46Ab | 1.57 ± 0.84Ac |
| Placebo (G3) | 5.06 ± 1.19Aa | 4.24 ± 1.63Ab | 3.65 ± 1.74Ab | 2.78 ± 1.40Bc |
The data were presented as mean ± standard deviation.
Same superscript letter indicates no significant differences between groups as per the results of pairwise multiple comparisons (p < 0.05). Lowercase superscripts denote differences in each row (horizontal). Uppercase superscripts denote differences in each column (vertical).
The data were presented as mean ± standard deviation.
Same superscript letter indicates no significant differences between groups as per the results of pairwise multiple comparisons (

 KACD
KACD
 ePub Link
ePub Link Cite
Cite

