Articles
- Page Path
- HOME > Restor Dent Endod > Volume 42(3); 2017 > Article
- Review Article Survival rates against fracture of endodontically treated posterior teeth restored with full-coverage crowns or resin composite restorations: a systematic review
-
Warattama Suksaphar1, Danuchit Banomyong1
 , Titalee Jirathanyanatt1, Yaowaluk Ngoenwiwatkul2
, Titalee Jirathanyanatt1, Yaowaluk Ngoenwiwatkul2 -
2017;42(3):-167.
DOI: https://doi.org/10.5395/rde.2017.42.3.157
Published online: July 31, 2017
1Department of Operative Dentistry and Endodontics, Mahidol University Faculty of Dentistry, Bangkok, Thailand.
2Department of Community Dentistry, Mahidol University Faculty of Dentistry, Bangkok, Thailand.
- Correspondence to Danuchit Banomyong, DDS, PhD. Assistant Professor, Department of Operative Dentistry and Endodontics, Mahidol University Faculty of Dentistry, 6, Yothi Road, Ratchathewi, Bangkok 10400, Thailand. Tel: +66-2-200-7825, Fax: +66-2-200-7824, danuchit.ban@mahidol.ac.th
Copyright © 2017. The Korean Academy of Conservative Dentistry
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 5,417 Views
- 64 Download
- 26 Crossref
Abstract
- This systematic review aims to summarize the current clinical studies that investigated survival rates against fracture of endodontically treated posterior teeth restored with crowns or resin composite restorations. Literature search were performed using keywords. Publications from 1980 to 2016 were searched in PubMed, ScienceDirect, Web of Science, MEDLINE, and SCOPUS. Included studies were selected based on inclusion and exclusion criteria. Three clinical studies were included: 1 randomized controlled trial and 1 prospective and 1 retrospective cohort studies. Pooled survival rates ranged from 94%–100% and 91.9%–100% for crowns and resin composite, respectively. The majority of teeth had no more than 3 surface loss of tooth structure. The studies included were heterogeneous, and were not appropriate for further meta-analysis. Current evidence suggested that the survival rates against the fracture of endodontically treated posterior teeth restored with crowns or resin composites were not significantly different in the teeth with minimum to moderate loss of tooth structure.
INTRODUCTION
MATERIALS AND METHODS
P (population): endodontically treated posterior permanent teeth (with mature root formation).
I (intervention): post-endodontic restoration with non-cuspal coverage, direct resin composite.
C (comparison): post-endodontic restoration with full-coverage crown.
O (outcome): survival rate against fracture.
Clinical study on posterior ETTs with indirect full-coverage crowns or direct non-cuspal coverage resin composite restorations, presenting comparison of survival rates.
The clinical study could be randomized or non-randomized controlled trials, or retrospective or prospective cohort studies.
No evaluation of survival rate against fracture.
No detail on the types of post-endodontic restoration.
Tooth types were combined between anterior and posterior teeth.
Levels of evidence and definitions based on the Oxford Centre for Evidence Based Medicine (OCEBM) Levels of Evidence [15]
RESULTS
Six excluded studies after full paper reviewing and reasons for exclusion
| Study | LOE | Study designs | Reasons for exclusion |
|---|---|---|---|
| Pratt et al. [18] | 3 | R | · Could not identify definite number and survival rate of resin composite restorations (combined numbers of amalgam and resin composite in direct restorations). |
| Skupien et al. [19] | 2 | RCT | · Could not identify definite number and survival rate of posterior teeth (combined numbers of anterior and posterior teeth). |
| Fransson et al. [20] | 3 | R | · Could not identify definite number and survival rate of posterior teeth (combined numbers of anterior and posterior teeth). |
| · Could not identify definite number and survival rate of full-crown or resin composite (including full-crown, inlay and onlay in indirect restorations; combining all types of direct restorations). | |||
| · Could not identify reasons for tooth extraction. | |||
| Skupien et al. [21] | 3 | R | · Could not identify definite number and survival rate of posterior teeth (combined numbers of anterior and posterior teeth). |
| Aquilino et al. [9] | 3 | R | · Could not identify definite number and survival rate of posterior teeth (combined numbers of anterior and posterior teeth). |
| · Could not identify definite number of resin composite restorations (combined numbers of amalgam and resin composite in direct restorations). | |||
| Sorensen et al. [11] | 3 | R | · Could not identify definite number and survival rate of posterior teeth restored with full-coverage crown or resin composite restoration (combining numbers of crown and onlay in cuspal-coverage indirect restoration; combining numbers of amalgam and resin composite in non-cuspal coverage direct restorations). |
Characteristics and survival rates of 3 included studies
| Studies | LOE | Study design | No. of teeth | Type of teeth | Restoration | Type of post | Criterion of survival from fracture | Statistical method | Survival rate against fracture | F/U period (mon) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Crown | Composite | ||||||||||
| Dammaschke et al. [17] | 3 | R | 401 | Premolar/molar | Crown/bridge (364) | Without post, prefabricated, or cast metal post | Fracture of tooth and/or restorations | LR | 94% | 91.90% | 60–192 (Mean 116.4) |
| Resin composite (37) | Without post | Mean survival times (mon) | |||||||||
| 152.4–168.0 | 160.8 | ||||||||||
| Cagidiaco et al. [16] | 3 | P | 105 | Premolar/molar | Crown (86) | Prefabricated fiber post | Post fracture, vertical, or horizontal root fracture | χ2 | 100% | 100% | 24 |
| Resin composite (19) | Prefabricated fiber post | ||||||||||
| Mannocci et al. [13] | 2 | RCT | 117 | Premolar | Crown (57) | Prefabricated fiber post | Root fracture, post fracture | 1-way ANOVA | 100% | 100% | 12, 24, 36 |
| Resin composite (60) | Prefabricated fiber post | ||||||||||
Number of teeth restored with resin composite restorations according to the number of tooth structure loss (surfaces) from the 3 included studies
| Clinical studies | No. | 1–3 surfaces loss | 4–5 surfaces loss | ||
|---|---|---|---|---|---|
| No. | % | No. | % | ||
| Dammaschke et al. [17] | 37 | 31 | 83.8 | 6 | 16.2 |
| Cagidiaco et al. [16] | 19 | 19 | 100.0 | 0 | 0 |
| Mannocci et al. [13] | 60 | 60 | 100.0 | 0 | 0 |
| Total | 116 | 110 | 94.8 | 6 | 5.2 |
DISCUSSION
Conclusions
Acknowledgement
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Banomyong D, Jirathanyanatt T.
Data curation: Suksaphar W, Ngoenwiwatkul Y.
Formal analysis: Suksaphar W, Ngoenwiwatkul Y.
Funding acquisition: Banomyong D, Jirathanyanatt T.
Investigation: Suksaphar W, Banomyong D.
Methodology: Suksaphar W, Banomyong D, Jirathanyanatt T, Ngoenwiwatkul Y.
Project administration: Suksaphar W.
Resources: Banomyong D, Jirathanyanatt T.
Software: Suksaphar W, Ngoenwiwatkul Y.
Supervision: Banomyong D, Jirathanyanatt T, Ngoenwiwatkul Y.
Validation: Banomyong D, Ngoenwiwatkul Y.
Visualization: Banomyong D, Ngoenwiwatkul Y.
Writing - original draft: Suksaphar W, Banomyong D.
Writing - review & editing: Suksaphar W, Banomyong D.
- 1. Panitvisai P, Messer HH. Cuspal deflection in molars in relation to endodontic and restorative procedures. J Endod 1995;21:57-61.ArticlePubMed
- 2. Reeh ES, Douglas WH, Messer HH. Stiffness of endodontically-treated teeth related to restoration technique. J Dent Res 1989;68:1540-1544.ArticlePubMedPDF
- 3. Sedgley CM, Messer HH. Are endodontically treated teeth more brittle? J Endod 1992;18:332-335.ArticlePubMed
- 4. Saunders WP, Saunders EM. Coronal leakage as a cause of failure in root-canal therapy: a review. Endod Dent Traumatol 1994;10:105-108.ArticlePubMed
- 5. Safavi KE, Dowden WE, Langeland K. Influence of delayed coronal permanent restoration on endodontic prognosis. Endod Dent Traumatol 1987;3:187-191.ArticlePubMed
- 6. Uranga A, Blum JY, Esber S, Parahy E, Prado C. A comparative study of four coronal obturation materials in endodontic treatment. J Endod 1999;25:178-180.ArticlePubMed
- 7. Chan CP, Lin CP, Tseng SC, Jeng JH. Vertical root fracture in endodontically versus nonendodontically treated teeth: a survey of 315 cases in Chinese patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999;87:504-507.ArticlePubMed
- 8. Kumagai H, Suzuki T, Hamada T, Sondang P, Fujitani M, Nikawa H. Occlusal force distribution on the dental arch during various levels of clenching. J Oral Rehabil 1999;26:932-935.ArticlePubMed
- 9. Aquilino SA, Caplan DJ. Relationship between crown placement and the survival of endodontically treated teeth. J Prosthet Dent 2002;87:256-263.ArticlePubMed
- 10. Ng YL, Mann V, Gulabivala K. A prospective study of the factors affecting outcomes of non-surgical root canal treatment: part 2: tooth survival. Int Endod J 2011;44:610-625.ArticlePubMed
- 11. Sorensen JA, Martinoff JT. Intracoronal reinforcement and coronal coverage: a study of endodontically treated teeth. J Prosthet Dent 1984;51:780-784.ArticlePubMed
- 12. Schwartz RS, Jordan R. Restoration of endodontically treated teeth: the endodontist's perspective, part 1. updated 2017 Jun 7]. Available from: http://www.aae.org/publications-and-research/endodontics-colleagues-for-excellence-newsletter/restoration-of-endodontically-treated-teeth,-the-endodontist-s-perspective-part-1.aspx.
- 13. Mannocci F, Bertelli E, Sherriff M, Watson TF, Ford TR. Three-year clinical comparison of survival of endodontically treated teeth restored with either full cast coverage or with direct composite restoration. J Prosthet Dent 2002;88:297-301.ArticlePubMed
- 14. Sequeira-Byron P, Fedorowicz Z, Carter B, Nasser M, Alrowaili EF. Single crowns versus conventional fillings for the restoration of root-filled teeth. Cochrane Database Syst Rev 2015;CD009109.ArticlePubMedPMC
- 15. Centre for Evidence-Based Medicine (GB). Oxford Centre for Evidence-Based Medicine: levels of evidence (March 2009). updated 2009]. Available from: http://www.cebm.net/oxford-centre-evidence-based-medicine-levels-evidence-march-2009.
- 16. Cagidiaco MC, Radovic I, Simonetti M, Tay F, Ferrari M. Clinical performance of fiber post restorations in endodontically treated teeth: 2-year results. Int J Prosthodont 2007;20:293-298.PubMed
- 17. Dammaschke T, Nykiel K, Sagheri D, SchaferSchäfer E. Influence of coronal restorations on the fracture resistance of root canal-treated premolar and molar teeth: a retrospective study. Aust Endod J 2013;39:48-56.ArticlePubMed
- 18. Pratt I, Aminoshariae A, Montagnese TA, Williams KA, Khalighinejad N, Mickel A. Eight-year retrospective study of the critical time lapse between root canal completion and crown placement: its influence on the survival of endodontically treated teeth. J Endod 2016;42:1598-1603.ArticlePubMed
- 19. Skupien JA, Cenci MS, Opdam NJ, Kreulen CM, Huysmans MC, Pereira-Cenci T. Crown vs. composite for post-retained restorations: Aa randomized clinical trial. J Dent 2016;48:34-39.PubMed
- 20. Fransson H, Dawson VS, Frisk F, Bjørndal L, Kvist T, Bjørndal L, Dawson VS, Fransson H, Frisk F, Jonasson P, Kvist T, Markvart M, Petersson K, Pigg M, Reit C, Wolf E. EndoReCo. Survival of root-filled teeth in the Swedish adult population. J Endod 2016;42:216-220.ArticlePubMed
- 21. Skupien JA, Opdam N, Winnen R, Bronkhorst E, Kreulen C, Pereira-Cenci T, Huysmans MC. A Practicepractice-based Studystudy on the Survivalsurvival of Restored Endodontically Treated Teeth.restored endodontically treated teeth. J Endod 2013;39:1335-1340.PubMed
- 22. Nagasiri R, Chitmongkolsuk S. Long-term survival of endodontically treated molars without crown coverage: a retrospective cohort study. J Prosthet Dent 2005;93:164-170.ArticlePubMed
- 23. Ferrari M, Vichi A, Fadda GM, Cagidiaco MC, Tay FR, Breschi L, Polimeni A, Goracci C. A randomized controlled trial of endodontically treated and restored premolars. J Dent Res 2012;91:72S-78S.ArticlePubMedPDF
- 24. Salameh Z, Sorrentino R, Papacchini F, Ounsi HF, Tashkandi E, Goracci C, Ferrari M. Fracture resistance and failure patterns of endodontically treated mandibular molars restored using resin composite with or without translucent glass fiber posts. J Endod 2006;32:752-755.ArticlePubMed
- 25. Tan L, Chen NN, Poon CY, Wong HB. Survival of root filled cracked teeth in a tertiary institution. Int Endod J 2006;39:886-889.ArticlePubMed
- 26. Hiatt WH. Incomplete crown-root fracture in pulpal-periodontal disease. J Periodontol 1973;44:369-379.ArticlePubMed
- 27. Lynch CD, McConnell RJ. The cracked tooth syndrome. J Can Dent Assoc 2002;68:470-475.PubMed
- 28. Cavel WT, Kelsey WP, Blankenau RJ. An in vivo study of cuspal fracture. J Prosthet Dent 1985;53:38-42.ArticlePubMed
- 29. Nam SH, Chang HS, Min KS, Lee Y, Cho HW, Bae JM. Effect of the number of residual walls on fracture resistances, failure patterns, and photoelasticity of simulated premolars restored with or without fiber-reinforced composite posts. J Endod 2010;36:297-301.ArticlePubMed
- 30. Dietschi D, Bouillaguet S, Sadan A. Restoration of the endodontically treated tooth. In: Hargreaves KM, Cohen S, editors. Cohen's pathways of the pulp. 10th ed. St. Louis (MO): Mosby Elsevier; 2011. p. 777-807.
- 31. Mincik J, Urban D, Timkova S, Urban R. Fracture resistance of endodontically treated maxillary premolars restored by various direct filling materials: an in vitro study. Int J Biomater 2016;2016:9138945.ArticlePubMedPMCPDF
- 32. Ausiello P, De Gee AJ, Rengo S, Davidson CL. Fracture resistance of endodontically-treated premolars adhesively restored. Am J Dent 1997;10:237-241.PubMed
- 33. Hansen EK. In vivo cusp fracture of endodontically treated premolars restored with MOD amalgam or MOD resin fillings. Dent Mater 1988;4:169-173.ArticlePubMed
- 34. Mannocci F, Qualtrough AJ, Worthington HV, Watson TF, Pitt Ford TR. Randomized clinical comparison of endodontically treated teeth restored with amalgam or with fiber posts and resin composite: five-year results. Oper Dent 2005;30:9-15.PubMed
- 35. Hashimoto M, Fujita S, Endo K, Ohno H. In vitro degradation of resin-dentin bonds with one-bottle self-etching adhesives. Eur J Oral Sci 2009;117:611-617.ArticlePubMed
- 36. Opdam NJ, van de Sande FH, Bronkhorst E, Cenci MS, Bottenberg P, Pallesen U, Gaengler P, Lindberg A, Huysmans MC, van Dijken JW. Longevity of posterior composite restorations: a systematic review and meta-analysis. J Dent Res 2014;93:943-949.ArticlePubMedPMCPDF
REFERENCES
Tables & Figures
REFERENCES
Citations

- Effect of using different materials and restorative techniques on cuspal deflection and microleakage in endodontically treated teeth
Ceyda Sari, Oya Bala, Sinem Akgul, Cemile Kedici Alp
BMC Oral Health.2025;[Epub] CrossRef - Direct restorations versus full crowns in endodontically treated molar teeth: A three-year randomized clinical trial
Motasum Abu-Awwad, Ruba Halasa, Laila Haikal, Ahmad El-Ma'aita, Mohammad Hammad, Haralampos Petridis
Journal of Dentistry.2025; 156: 105699. CrossRef - Is the use of an intraradicular post essential for reducing failures in restoring endodontically treated teeth? A systematic review and meta-analysis
Jacqueline Salomão Jardim, Vinicius de Menezes Félix Ferreira, Hiskell Francine Fernandes e Oliveira, Daniele Sorgatto Faé, Cleidiel Aparecido Araujo Lemos
Journal of Dentistry.2025; 159: 105739. CrossRef - Systematic Reviews Comparing Direct and Indirect Restorations: An Umbrella Review That Examines Restoration Type and Confidence in Results
Mona Kimmel, Clovis Mariano Faggion
Clinical and Experimental Dental Research.2025;[Epub] CrossRef - Knowledge, Awareness, and Perceptions on Root Canal Treatment among Patients Reporting with Dental Pain to Conservative Dentistry and Endodontics Department: An Institution-based Survey
Abdu Semeer Palottil, Moopil Midhun Mohanan, N. T. Nishad, S. Jayasree
Journal of Primary Care Dentistry and Oral Health.2025; 6(2): 99. CrossRef - One-year clinical performance of restorations with and without a bulk-fill flowable base in endodontically treated premolars: a pilot randomized controlled trial
Brenda Leyton, Jullyana Dezanetti, Rodrigo Rached, Sérgio Ignácio, Evelise Souza
BMC Oral Health.2025;[Epub] CrossRef - One-piece endodontic crown fixed partial denture: Is it possible?
João Paulo M. Tribst, Amanda Maria de O. Dal Piva, Joris Muris, Cornelis J. Kleverlaan, Albert J. Feilzer
The Journal of Prosthetic Dentistry.2024; 131(6): 1118. CrossRef - Survival Rate Against Fracture of Endodontically Treated Premolars Restored with Crowns and Resin Composites: A Retrospective Study
Enas Khamakhim, Farida Alsayeh
AlQalam Journal of Medical and Applied Sciences.2024; : 398. CrossRef - Knowledge and Awareness of Root Canal Treatment among Patients in Tripoli: A Survey-Based Study
Sumaya Aghila
AlQalam Journal of Medical and Applied Sciences.2024; : 532. CrossRef - Clinical performance of polyethylenefiber reinforced resin composite restorations in endodontically treated teeth: (a randomized controlled clinical trial)
Ahmed Abdelsattar Metwaly, Amira Farid Elzoghby, Rawda Hesham Abd ElAziz
BMC Oral Health.2024;[Epub] CrossRef - Direct Versus Indirect Treatment Options of Endodontically Treated Posterior Teeth: A Narrative Review
Mai M Alhamdan, Rodina F Aljamaan, Munira M Abuthnain, Shahd A Alsumikhi, Ghada S Alqahtani, Reem A Alkharaiyef
Cureus.2024;[Epub] CrossRef - Single crown vs. composite for glass fiber post-retained restorations: An 8-year randomized clinical trial
Victório Poletto-Neto, Luiz Alexandre Chisini, Wietske Fokkinga, Cees Kreulen, Bas Loomans, Maximiliano Sérgio Cenci, Tatiana Pereira-Cenci
Journal of Dentistry.2024; 142: 104837. CrossRef - Factors influencing the clinical performance of the restoration of endodontically treated teeth: An assessment of systematic reviews of clinical studies
Lara Dotto, Luiza Paloma S. Girotto, Yara Teresinha Correa Silva Sousa, Gabriel Kalil Rocha Pereira, Ataís Bacchi, Rafael Sarkis-Onofre
The Journal of Prosthetic Dentistry.2024; 131(6): 1043. CrossRef - Influence of technical quality and coronal restoration on periapical health of root canal treatment performed by Malaysian undergraduate students
Norazlina Mohammad, Faizah Abdul Fatah, Azlan Jaafar, Siti Hajar Omar, Aimi Amalina Ahmad, Abdul Azim Asy Abdul Aziz, Aws Hashim Ali Al-Kadhim
Saudi Endodontic Journal.2023; 13(1): 63. CrossRef - The success rate of indirect adhesive restorations in the distal dentition fabricated with chairside CAD/CAM system
Marek Šupler, Andrej Jenča, Michal Straka, Juraj Deglovič, Janka Jenčová
Stomatológ.2023; 33(2): 10. CrossRef - A Comparative Study of the Marginal Fit of Endocrowns Fabricated From Three Different Computer-Aided Design/Computer-Aided Manufacturing (CAD/CAM) Ceramic Materials: An In Vitro Study
Esraa Attar, Shatha Alshali, Tariq Abuhaimed
Cureus.2023;[Epub] CrossRef - Evaluation of titanium mesh and fibers in reinforcing endodontically treated molars: An in vitro study
Hemalatha Hiremath, Devansh Verma, Sheetal Khandelwal, AishwaryaSingh Solanki, Sonam Patidar
Journal of Conservative Dentistry.2022; 25(2): 189. CrossRef - Effect of surface treatment, ferrule height, and luting agent type on pull-out bond strength of monolithic zirconia endocrowns
Emine B. Buyukerkmen, Durmuş A. Bozkurt, Arslan Terlemez
Journal of Oral Science.2022; 64(4): 279. CrossRef - An Umbrella Review of Systematic Reviews and Meta‐Analyses Evaluating the Success Rate of Prosthetic Restorations on Endodontically Treated Teeth
Amirhossein Fathi, Behnaz Ebadian, Sara Nasrollahi Dezaki, Nahal Mardasi, Ramin Mosharraf, Sabire Isler, Shiva Sadat Tabatabaei, Stefano Pagano
International Journal of Dentistry.2022;[Epub] CrossRef - Survival and success of endocrowns: A systematic review and meta-analysis
Raghad A. Al-Dabbagh
The Journal of Prosthetic Dentistry.2021; 125(3): 415.e1. CrossRef - Fracture strength of non-invasively reinforced MOD cavities on endodontically treated teeth
René Daher, Stefano Ardu, Enrico Di Bella, Giovanni T. Rocca, Albert J. Feilzer, Ivo Krejci
Odontology.2021; 109(2): 368. CrossRef - Retrospective study of fracture survival in endodontically treated molars: the effect of single-unit crowns versus direct-resin composite restorations
Kanet Chotvorrarak, Warattama Suksaphar, Danuchit Banomyong
Restorative Dentistry & Endodontics.2021;[Epub] CrossRef - An insight into patient's perceptions regarding root canal treatment: A questionnaire-based survey
Ramta Bansal, Aditya Jain
Journal of Family Medicine and Primary Care.2020; 9(2): 1020. CrossRef - Endodontically treated posterior teeth restored with or without crown restorations: A 5‐year retrospective study of survival rates from fracture
Titalee Jirathanyanatt, Warattama Suksaphar, Danuchit Banomyong, Yaowaluk Ngoenwiwatkul
Journal of Investigative and Clinical Dentistry.2019;[Epub] CrossRef - Fracture resistance, gap and void formation in root‐filled mandibular molars restored with bulk‐fill resin composites and glass‐ionomer cement base
Nathamon Thongbai‐on, Kanet Chotvorrarak, Danuchit Banomyong, Michael F. Burrow, Sittichoke Osiri, Nattha Pattaravisitsate
Journal of Investigative and Clinical Dentistry.2019;[Epub] CrossRef - Current options concerning the endodontically-treated teeth restoration with the adhesive approach
Marco Aurélio de Carvalho, Priscilla Cardoso Lazari, Marco Gresnigt, Altair Antoninha Del Bel Cury, Pascal Magne
Brazilian Oral Research.2018;[Epub] CrossRef
- Figure
- Related articles
-
- Fracture resistance and failure modes of endodontically-treated permanent teeth restored with Ribbond posts vs other post systems: a systematic review and meta-analysis of in vitro studies
- The prevalence of apical periodontitis in patients prior to hematopoietic cell transplantation: a systematic review
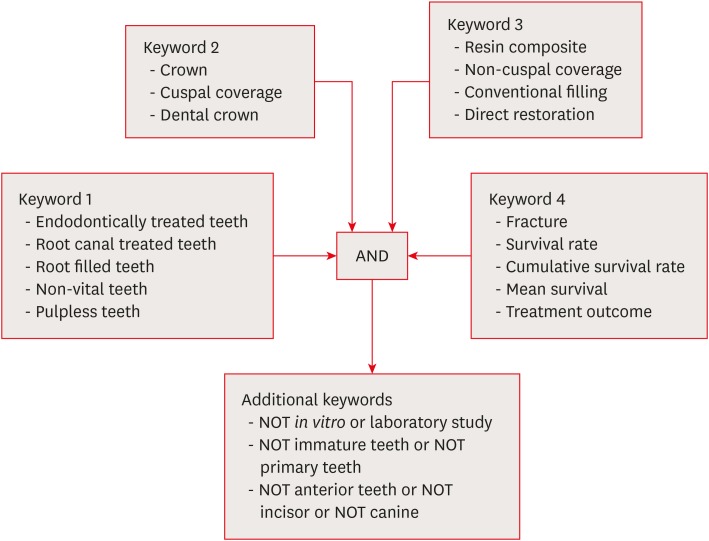
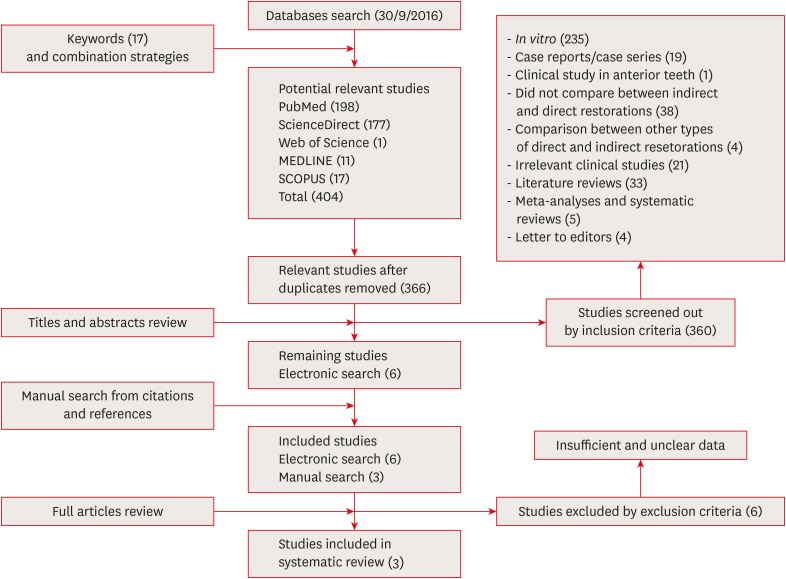
Figure 1
Figure 2
Levels of evidence and definitions based on the Oxford Centre for Evidence Based Medicine (OCEBM) Levels of Evidence [15]
| Levels | Definitions |
|---|---|
| 1 | Systematic review of randomized trials or n-of-1 trials |
| 2 | Randomized trial or observational study with dramatic effect |
| 3 | Non-randomized controlled cohort/follow-up study |
| 4 | Case-series, case-control studies, or historically controlled studies |
| 5 | Mechanism-based reasoning |
Six excluded studies after full paper reviewing and reasons for exclusion
| Study | LOE | Study designs | Reasons for exclusion |
|---|---|---|---|
| Pratt et al. [ | 3 | R | · Could not identify definite number and survival rate of resin composite restorations (combined numbers of amalgam and resin composite in direct restorations). |
| Skupien et al. [ | 2 | RCT | · Could not identify definite number and survival rate of posterior teeth (combined numbers of anterior and posterior teeth). |
| Fransson et al. [ | 3 | R | · Could not identify definite number and survival rate of posterior teeth (combined numbers of anterior and posterior teeth). |
| · Could not identify definite number and survival rate of full-crown or resin composite (including full-crown, inlay and onlay in indirect restorations; combining all types of direct restorations). | |||
| · Could not identify reasons for tooth extraction. | |||
| Skupien et al. [ | 3 | R | · Could not identify definite number and survival rate of posterior teeth (combined numbers of anterior and posterior teeth). |
| Aquilino et al. [ | 3 | R | · Could not identify definite number and survival rate of posterior teeth (combined numbers of anterior and posterior teeth). |
| · Could not identify definite number of resin composite restorations (combined numbers of amalgam and resin composite in direct restorations). | |||
| Sorensen et al. [ | 3 | R | · Could not identify definite number and survival rate of posterior teeth restored with full-coverage crown or resin composite restoration (combining numbers of crown and onlay in cuspal-coverage indirect restoration; combining numbers of amalgam and resin composite in non-cuspal coverage direct restorations). |
LOE, level of evidence; R, retrospective cohort study; RCT, randomized control trial study.
Characteristics and survival rates of 3 included studies
| Studies | LOE | Study design | No. of teeth | Type of teeth | Restoration | Type of post | Criterion of survival from fracture | Statistical method | Survival rate against fracture | F/U period (mon) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Crown | Composite | ||||||||||
| Dammaschke et al. [ | 3 | R | 401 | Premolar/molar | Crown/bridge (364) | Without post, prefabricated, or cast metal post | Fracture of tooth and/or restorations | LR | 94% | 91.90% | 60–192 (Mean 116.4) |
| Resin composite (37) | Without post | Mean survival times (mon) | |||||||||
| 152.4–168.0 | 160.8 | ||||||||||
| Cagidiaco et al. [ | 3 | P | 105 | Premolar/molar | Crown (86) | Prefabricated fiber post | Post fracture, vertical, or horizontal root fracture | χ2 | 100% | 100% | 24 |
| Resin composite (19) | Prefabricated fiber post | ||||||||||
| Mannocci et al. [ | 2 | RCT | 117 | Premolar | Crown (57) | Prefabricated fiber post | Root fracture, post fracture | 1-way ANOVA | 100% | 100% | 12, 24, 36 |
| Resin composite (60) | Prefabricated fiber post | ||||||||||
LOE, level of evidence; F/U, follow-up; R, retrospective cohort study; LR, log-rank test; P, prospective cohort study; RCT, randomized control trial study; ANOVA, analysis of variance.
Number of teeth restored with resin composite restorations according to the number of tooth structure loss (surfaces) from the 3 included studies
| Clinical studies | No. | 1–3 surfaces loss | 4–5 surfaces loss | ||
|---|---|---|---|---|---|
| No. | % | No. | % | ||
| Dammaschke et al. [ | 37 | 31 | 83.8 | 6 | 16.2 |
| Cagidiaco et al. [ | 19 | 19 | 100.0 | 0 | 0 |
| Mannocci et al. [ | 60 | 60 | 100.0 | 0 | 0 |
| Total | 116 | 110 | 94.8 | 6 | 5.2 |
LOE, level of evidence; R, retrospective cohort study; RCT, randomized control trial study.
LOE, level of evidence; F/U, follow-up; R, retrospective cohort study; LR, log-rank test; P, prospective cohort study; RCT, randomized control trial study; ANOVA, analysis of variance.

 KACD
KACD
 ePub Link
ePub Link Cite
Cite

