Articles
- Page Path
- HOME > Restor Dent Endod > Volume 40(4); 2015 > Article
- Research Article Clinical and radiographical evaluation of mineral trioxide aggregate, biodentine and propolis as pulpotomy medicaments in primary teeth
- Bharti Kusum1, Kumar Rakesh2, Khanna Richa2
-
2015;40(4):-285.
DOI: https://doi.org/10.5395/rde.2015.40.4.276
Published online: September 9, 2015
1Department of Pedodontics and Preventive Dentistry, Maulana Azad Institute of Dental Sciences, MAMC complex, BSZ Marg, New Delhi, India.
2Department of Pediatric and Preventive Dentistry, Faculty of Dental Sciences, King George Medical University, Lucknow, India.
- Correspondence to Bharti Kusum, MDS. Senior Resident, Department of Pedodontics and Preventive Dentistry, Maulana Azad Institute of Dental Sciences, MAMC complex, BSZ Marg, New Delhi, 110002, India. TEL, +91-094-50361835; FAX, +91-011-23217081; kusumbharti1984@gmail.com
©Copyrights 2015. The Korean Academy of Conservative Dentistry.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 2,494 Views
- 23 Download
- 50 Crossref
Abstract
-
Objectives The purpose of this study was to evaluate the efficacy of mineral trioxide aggregate (MTA), Biodentine and Propolis as pulpotomy medicaments in primary dentition, both clinically and radiographically.
-
Materials and Methods A total of 75 healthy 3 to 10 yr old children each having at least one carious primary molar tooth were selected. Random assignment of the pulpotomy medicaments was done as follows: Group I, MTA; Group II, Biodentine; Group III, Propolis. All the pulpotomized teeth were evaluated at 3, 6, and 9 mon clinically and radiographically, based on the scoring criteria system.
-
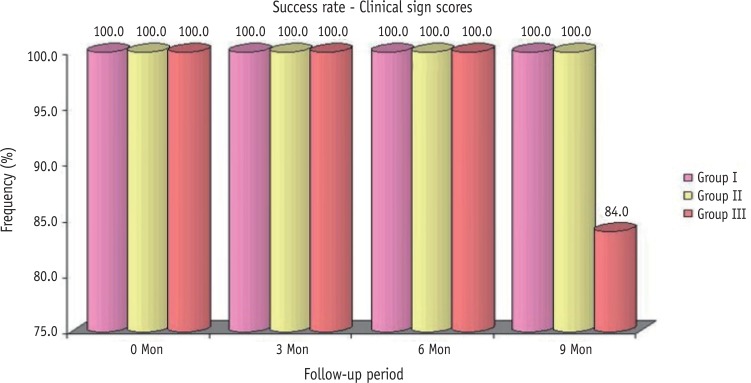
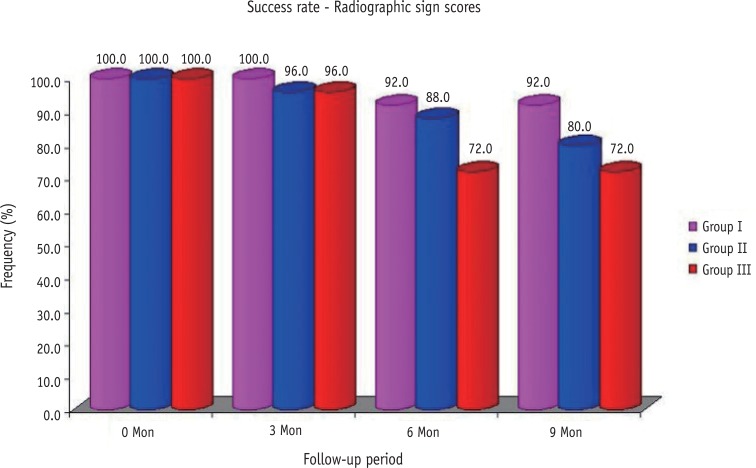
Results The clinical success rates were found to be similar among the three groups at 3 and 6 mon where as a significant decrease in success rate was observed in Group III (84%) compared to both Group I (100%) and Group II (100%) at 9 mon. Radiographic success rates over a period of 9 mon in Groups I, II, and III were 92, 80, and 72%, respectively.
-
Conclusions Teeth treated with MTA and Biodentine showed more favorable clinical and radiographic success as compared to Propolis at 9 mon follow-up.
Introduction
Materials and Methods
Results
Discussion
Conclusions
- 1. Caicedo R, Abbott PV, Alongi DJ, Alarcon MY. Clinical, radiographic and histological analysis of the effects of mineral trioxide aggregate used in direct pulp capping and pulpotomies of primary teeth. Aust Dent J 2006;51:297-305.ArticlePubMed
- 2. Magnusson B. Attempts to predict prognosis of pulpotomy in primary molars. Scand J Dent Res 1970;78:232-240.PubMed
- 3. Ranly DM. Pulpotomy therapy in primary teeth: new modalities for old rationales. Pediatr Dent 1994;16:403-409.PubMed
- 4. Eidelman E, Holan G, Fuks AB. Mineral trioxide aggregate vs. formocresol in pulpotomized primary molars: a preliminary report. Pediatr Dent 2001;23:15-18.PubMed
- 5. Myers DR, Shoaf HK, Dirksen TR, Pashley DH, Whitford GM, Reynolds KE. Distribution of 14C-formaldehyde after pulpotomy with formocresol. J Am Dent Assoc 1978;96:805-813.ArticlePubMed
- 6. Primosch RE, Glomb TA, Jerrell RG. Primary tooth pulp therapy as taught in Predoctoral pediatric dental programs in the United States. Pediatr Dent 1997;19:118-122.PubMed
- 7. Torabinejad M, Chivian N. Clinical applications of mineral trioxide aggregate. J Endod 1999;25:197-205.ArticlePubMed
- 8. Holan G, Eidelman E, Fuks AB. Long-term evaluation of pulpotomy in primary molars using mineral trioxide aggregate or formocresol. Pediatr Dent 2005;27:129-136.PubMed
- 9. Oguntebi BR, Heaven T, Clark AE, Pink FE. Quantitative assessment of dentin bridge formation following pulpcapping in miniature swine. J Endod 1995;21:79-82.ArticlePubMed
- 10. Ford TR, Torabinejad M, Abedi HR, Bakland LK, Kariyawasam SP. Using mineral trioxide aggregate as a pulp-capping material. J Am Dent Assoc 1996;127:1491-1494.ArticlePubMed
- 11. Damamaschke T, Gerth HU, Züchner H, Schäfer E. Chemical and physical surface and bulk material characterization of white ProRoot MTA and two Portland cements. Dent Mater 2005;21:731-738.ArticlePubMed
- 12. Parirokh M, Torabinejad M. Mineral trioxide aggregate: a comprehensive literature review-part I: chemical, physical, and antibacterial properties. J Endod 2010;36:16-27.ArticlePubMed
- 13. Laurent P, Camps J, About I. Biodentine induces TGF-β1 release from human pulp cells and early dental pulp mineralization. Int Endod J 2012;45:439-448.PubMed
- 14. Peng W, Liu W, Zhai W, Jiang L, Li L, Chang J, Zhu Y. Effect of tricalcium silicate on the proliferation and odontogenic differentiation of human dental pulp cells. J Endod 2011;37:1240-1246.ArticlePubMed
- 15. Tran XV, Gorin C, Willing C, Baroukh B, Pellat B, Decup F, Opsahl Vital S, Chaussain C, Boukpessi T. Effect of a calicum-silicate-based restorative cement on pulp repair. J Dent Res 2012;91:1166-1171.ArticlePubMedPDF
- 16. Zanini M, Sautier JM, Berdal A, Simon S. Biodentine induces immortalized murine pulp cell differentiation into odontoblast-like cells and stimulates biomineralization. J Endod 2012;38:1220-1226.ArticlePubMed
- 17. Banskota AH, Tezuka Y, Kadota S. Recent progress in pharmacological research of propolis. Phytother Res 2001;15:561-571.ArticlePubMed
- 18. Burdock GA. Review of the biological properties and toxicity of bee propolis (propolis). Food Chem Toxicol 1998;36:347-363.ArticlePubMed
- 19. Marcucci MC. Propolis: chemical composition, biological properties and therapeutic activity. Apidologie 1995;26:83-99.Article
- 20. Al-Haj Ali SN. In vitro toxicity of propolis in comparison with other primary teeth pulpotomy agents on human fibroblasts. J Investig Clin Dent 2015 4 27 [Epub ahead of print].
- 21. Ozório JE, Carvalho LF, de Oliveira DA, de Sousa-Neto MD, Perez DE. Standardized propolis extract and calcium hydroxide as pulpotomy agents in primary pig teeth. J Dent Child (Chic) 2012;79:53-58.PubMed
- 22. Parolia A, Kundabala M, Rao NN, Acharya SR, Agrawal P, Mohan M, Thomas M. A comparative histological analysis of human pulp following direct pulp capping with Propolis, mineral trioxide aggregate and Dycal. Aust Dent J 2010;55:59-64.ArticlePubMed
- 23. Zurn D, Seale NS. Light-cured calcium hydroxide vs formocresol in human primary molar pulpotomies: a randomized controlled trial. Pediatr Dent 2008;30:34-41.
- 24. Sushynski JM, Zealand CM, Botero TM, Boynton JR, Majewski RF, Shelburne CE, Hu JC. Comparison of gray mineral trioxide aggregate and diluted formocresol in pulpotomized primary molars: a 6- to 24-month observation. Pediatr Dent 2012;34:120-128.PubMedPMC
- 25. Scheller S, Ilewicz L, Luciak M, Skrobidurska D, Stojko A, Matuga W. Biological properties and chemical application of propolis. IX. Experimental observation on the influence of ethanol extract of propolis (EEP) on dental pulp regeneration. Arzneimittelforschung 1978;28:289-291.PubMed
- 26. Nowicka A, Lipski M, Parafiniuk M, Sporniak-Tutak K, Lichota D, Kosierkiewicz A, Kaczmarek W, Buczkowska-Radlińska J. Response of human dental pulp capped with biodentine and mineral trioxide aggregate. J Endod 2013;39:743-747.ArticlePubMed
- 27. Park YK, Alencar SM, Aguiar CL. Botanical origin and chemical composition of Brazilian propolis. J Agric Food Chem 2002;50:2502-2506.ArticlePubMed
- 28. Croll TP, Killian CM. Zinc oxide-eugenol pulpotomy and stainless steel crown restoration of a primary molar. Quintessence Int 1992;23:383-388.PubMed
- 29. Gruythuysen RJ, Weerheijm KL. Calcium hydroxide pulpotomy with a light-cured cavity-sealing material after two years. ASDC J Dent Child 1997;64:251-253.PubMed
- 30. Zealand CM, Briskie DM, Botero TM, Boynton JR, Hu JC. Comparing gray mineral trioxide aggregate and diluted formocresol in pulpotomized human primary molars. Pediatr Dent 2010;32:393-399.PubMedPMC
- 31. Erdem AP, Guven Y, Balli B, Ilhan B, Sepet E, Ulukapi I, Aktoren O. Success rates of mineral trioxide aggregate, ferric sulfate, and formocresol pulpotomies: a 24-month study. Pediatr Dent 2011;33:165-170.PubMed
- 32. Willard RM. Radiographic changes following formocresol pulpotomy in primary molars. ASDC J Dent Child 1976;43:414-415.PubMed
- 33. Fuks AB, Holan G, Davis JM, Eidelman E. Ferric sulfate versus dilute formocresol in pulpotomized primary molars: long-term follow up. Pediatr Dent 1997;19:327-330.PubMed
- 34. Koo H, Gomes BP, Rosalen PL, Ambrosano GM, Park YK, Cury JA. In vitro antimicrobial activity of propolis and arnica montana against oral pathogens. Arch Oral Biol 2000;45:141-148.ArticlePubMed
- 35. Silva FB, Almeida JM, Sousa SM. Natural medicaments in endodontics - a comparative study of the antiinflammatory action. Braz Oral Res 2004;18:174-179.ArticlePubMed
- 36. Tan-No K, Nakajima T, Shoji T, Nakagawasai O, Niijima F, Ishikawa M, Endo Y, Sato T, Satoh S, Tadano T. Antiinflammatory effect of propolis through inhibition of nitric oxide production on carrageenin-induced mouse paw edema. Biol Pharm Bull 2006;29:96-99.ArticlePubMed
- 37. Jabbarifar SE, Khademi AA, Ghasemi D. Success rate of formocresol pulpotomy versus mineral trioxide aggregate in human primary molar tooth. J Res Med Sci 2004;9:304-307.
- 38. Sonmez D, Sari S, Cetinbaş T. A Comparison of four pulpotomy techniques in primary molars: a long-term follow-up. J Endod 2008;34:950-955.ArticlePubMed
- 39. del Carmen González Rodríguez W, Carpio MHC, Ramos MRM, Milanés MG, Antúnez LN. Pulpotomies of dead pulps in temporal molars using 10% propolis tinction. Rev Cubana Estomatol [online] 2007;44(3):Available from: http://scielo.sld.cu/scielo.php?script=sci_abstract&pid=S0034-75072007000300006&lng=en&nrm=iso&tlng=en (updated 2015 Sep 3).
- 40. Waterhouse PJ, Nunn JH, Whitworth JM. Primary molar vital pulp theory. Br Dent J 2000;188:417.
REFERENCES
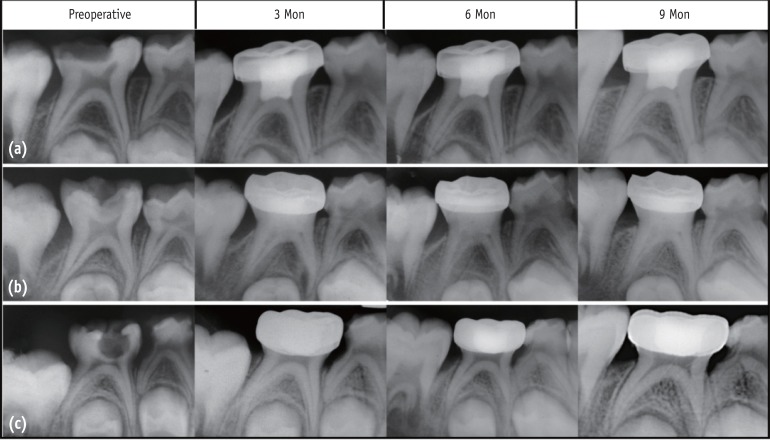
Representative radiographic observations in all the three groups over different follow-up periods. (a) MTA; (b) Biodentine; (c) Propolis pulpotomies in primary molars.
Comparison of clinical success rates in all the three groups over different follow-up periods.
Comparison of radiographic success rates in all the three groups over different follow-up periods.
Clinical and radiographic scoring criteria
Clinical sign scores of three groups over the periods
Radiographic sign scores of three groups over the periods
Tables & Figures
REFERENCES
Citations

- The Clinical Effectiveness of Propolis on the Endodontic Treatment of Permanent Teeth: A Systematic Review of Randomized Clinical Trials and Updates
Amirah Y Aldosari, Amira M Aljared, Hanin S Alqurshy, Abdullah M Alfarran, Mohanad G Alnahdi, Sarah S Alharbi, Wed S Alharbi, Faisal T Alghamdi
Cureus.2025;[Epub] CrossRef - Natural nanoparticles versus the gold standard in direct pulp capping: a randomized clinical trial
Dalia M. Elasser, Sabah M. Sobhy, Rania Rashad Omar Taha, Nevin A. Gad, Dina M. Abdel-Ghany
The Saudi Dental Journal.2025;[Epub] CrossRef - Systematic review and meta analysis of first and second generation bioceramic materials in primary dentition pulpotomies
João Albernaz Neves, Luísa Bandeira Lopes, Marta Alves Duarte, José João Mendes, Tiago Pimentel
Scientific Reports.2025;[Epub] CrossRef - EFFICACY OF BIODENTINE VERSUS MINERAL TRIOXIDE AGGREGATE IN PULPOTOMY FOR PRIMARY TEETH: A SYSTEMATIC REVIEW AND META-ANALYSIS OF RANDOMIZED CONTROLLED TRIALS
KORINA YUN-FAN LU, JENNIFER L. GIBBS, CHENG-YU WU, MARKUS B. BLATZ, XUEHAO MA, MIN-WEN FU, KEVIN SHENG-KAI MA
Journal of Evidence-Based Dental Practice.2025; 25(4): 102191. CrossRef - Calcium Silicate-Based Cements in Restorative Dentistry: Vital Pulp Therapy Clinical, Radiographic, and Histological Outcomes on Deciduous and Permanent Dentition—A Systematic Review and Meta-Analysis
Maria Teresa Xavier, Ana Luísa Costa, João Carlos Ramos, João Caramês, Duarte Marques, Jorge N. R. Martins
Materials.2024; 17(17): 4264. CrossRef - Outcome assessment methods of bioactive and biodegradable materials as pulpotomy agents in primary and permanent teeth: a scoping review
Yasmine Elhamouly, May M. Adham, Karin M L Dowidar, Rania M. El Backly
BMC Oral Health.2024;[Epub] CrossRef - Comparative Evaluation of the Efficacy of Theracal Lc, Mineral Trioxide Aggregate, and Biodentine As Direct Pulp Capping Materials in Patients With Pulpal Exposure in Posterior Teeth: A Triple Blinded Randomized Parallel Group Clinical Trial
Joyeeta Mahapatra, Pradnya P Nikhade, Aditya Patel, Nikhil Mankar, Prachi Taori
Cureus.2024;[Epub] CrossRef - Efficacy of different endodontic irrigants in the lesion sterilization and tissue repair technique in primary molars: A randomized controlled clinical trial
Anukriti Dimri, Nikhil Srivastava, Vivek Rana, Noopur Kaushik
Journal of Indian Society of Pedodontics and Preventive Dentistry.2024; 42(4): 294. CrossRef - Clinical and Radiographic Success Rates of Pulpotomies in Primary Molars Treated with Formocresol, BiodentineTM, and Endo Repair: A Randomized Clinical Trial
Elham Farokh Gisour, Farzaneh Jalali, Fatemeh Jahanimoghadam, Tania Dehesh
Pesquisa Brasileira em Odontopediatria e Clínica Integrada.2023;[Epub] CrossRef - Evaluation and comparison of mineral trioxide aggregate and cold ceramic in primary tooth pulpotomy: Clinical and radiographic study
Bita Rasteh, Leila Basir, Shirin Taravati, Masoumeh Khataminia
Journal of Family Medicine and Primary Care.2023; 12(12): 3068. CrossRef - Comparison between the Radiographic and Clinical Rates of Success for TheraCal and MTA in Primary Tooth Pulpotomy within a 12‐Month Follow‐Up: A Split‐Mouth Clinical Trial
Sedigheh Hassanpour, Naser Asl Aminabadi, Mahdi Rahbar, Leila Erfanparast, Iole Vozza
BioMed Research International.2023;[Epub] CrossRef - Biodentine™ Pulpotomy in Stage I Primary Molars: A 12-month Follow-up
Balsam Noueiri, Hitaf Nasrallah
International Journal of Clinical Pediatric Dentistry.2023; 15(6): 660. CrossRef - Omega 3 based formulations as new possible pulpotomy agents for primary teeth
Nancy M. Metwally, Amina M. El Hosary, Gamal M. El Maghraby, Maha A. El Demellawy, Mohamed Nabil, Elsayed M. Deraz
Tanta Dental Journal.2022; 19(4): 287. CrossRef - Clinical efficacy of Er:YAG laser application in pulpotomy of primary molars: a 2-year follow-up study
Junhui Wang, Yujiang Chen, Baize Zhang, Xin Ge, Xiaojing Wang
Lasers in Medical Science.2022; 37(9): 3705. CrossRef - Comparative efficacy of medicaments or techniques for pulpotomy of primary molars: a network meta-analysis
Jiehua Guo, Na Zhang, Yuzhao Cheng
Clinical Oral Investigations.2022; 27(1): 91. CrossRef - Comparative evaluation of zinc oxide-eugenol and zinc oxide with Neem oil in root canal treatment of primary teeth
Dhvani Gordhanbhai Patel, Shoba Fernandes, Yash Bafna, Krunal Choksi, Shaila Chaudhary, Priya Mishra
AYU (An International Quarterly Journal of Research in Ayurveda).2022; 43(1): 8. CrossRef - Treatment Outcomes of Pulpotomy with Propolis in Comparison with MTA in Human Primary Molars: A 24-month Follow-up Randomized Controlled Trial
Rayala Chandrasekhar, C Vinay, KS Uloopi, Kakarla Sri RojaRamya
International Journal of Clinical Pediatric Dentistry.2022; 15(S1): S3. CrossRef - Comparison of Clinical and Radiographic Success between MTA and Biodentine in Pulpotomy of Primary Mandibular Second Molars with Irreversible Pulpitis: A Randomized Double‐Blind Clinical Trial
Alireza Eshghi, Maryam Hajiahmadi, Mohammad Hossein Nikbakht, Mona Esmaeili, Murilo Baena Lopes
International Journal of Dentistry.2022;[Epub] CrossRef - Does the use of natural products for endodontic therapy in primary teeth have sufficient evidence for clinical practice? A scoping review
Filipe Colombo Vitali, Ana Cristina Andrada, Helhen Cristina da Luz Cardoso, Gesner Francisco Xavier-Junior, Cleonice da Silveira Teixeira, Loise Pedrosa Salles, Erica Negrini Lia, Carla Massignan
Clinical Oral Investigations.2022; 26(10): 6043. CrossRef - Prevalence of pain following single-visit pulpectomy with stainless steel crown done by postgraduate students in a university sitting
Ashwin Shravan Kumar, Mahesh Ramakrishnan
Journal of Advanced Pharmaceutical Technology & Research.2022; 13(Suppl 1): S177. CrossRef - Clinical and histological response of human pulp tissue to direct pulp capping with mineral trioxide aggregate, Biodentine and propolis
Zahra Nasri, MaryamZare Jahromi, Atousa Aminzadeh
Dental Research Journal.2022; 19(1): 40. CrossRef - Long-term evaluation of primary teeth molar pulpotomies with Biodentine and MTA: a CONSORT randomized clinical trial
S. Vilella-Pastor, S. Sáez, A. Veloso, F. Guinot-Jimeno, M. Mercadé
European Archives of Paediatric Dentistry.2021; 22(4): 685. CrossRef - Tailored 70S30C Bioactive glass induces severe inflammation as pulpotomy agent in primary teeth: an interim analysis of a randomised controlled trial
Yasmine Elhamouly, Rania M. El Backly, Dalia M. Talaat, Samia S. Omar, Maha El Tantawi, Karin M. L. Dowidar
Clinical Oral Investigations.2021; 25(6): 3775. CrossRef - Efficacy of laser photobiomodulation pulpotomy in human primary teeth
Chandrashekar Murugesh Yavagal, Akshaya Lal, Viplavi Vijaysinh Chavan Patil, Puja C. Yavagal, Kiran Kumar Neelakantappa, Madhu Hariharan
Journal of Indian Society of Pedodontics and Preventive Dentistry.2021; 39(4): 436. CrossRef - SÜT DİŞİ AMPUTASYON TEDAVİSİNDE GÜNCEL YAKLAŞIMLAR
Necibe Damla ŞAHİN, Volkan ARIKAN
Atatürk Üniversitesi Diş Hekimliği Fakültesi Dergisi.2021; : 1. CrossRef - The use of propolis in dentistry, oral health, and medicine: A review
Felix Zulhendri, Rafael Felitti, James Fearnley, Munir Ravalia
Journal of Oral Biosciences.2021; 63(1): 23. CrossRef - Clinical and radiographic evaluation of pulpotomy using MTA, Biodentine and Er,Cr:YSGG laser in primary teeth. A clinical study
Pandiyan Ramanandvignesh, Kumar Gyanendra, Dhillon Jatinder Kaur Goswami Mridula
Laser Therapy.2020; 29(1): 29. CrossRef - Comparative Evaluation of Success of Biodentine and Mineral Trioxide Aggregate with Formocresol as Pulpotomy Medicaments in Primary Molars: An In Vivo Study
Ritika Malhotra, Shilpa Ahuja, Dipanshu Kumar, Kapil Gandhi, Rishabh Kapoor, Kumari Surabhi
International Journal of Clinical Pediatric Dentistry.2020; 13(2): 167. CrossRef - Comparison of Partial Pulpotomy in Permanent Molars Using Different Pulp Capping Agents and Restoration Materials
Jimi Lee, Nanyoung Lee, Sangho Lee, Myeongkwan Jih
THE JOURNAL OF THE KOREAN ACADEMY OF PEDTATRIC DENTISTRY.2020; 47(2): 148. CrossRef - A Comparative Evaluation between Propolis and Mineral Trioxide Aggregate as Pulpotomy Medicaments in Primary Molars
Kavita Madan, Sudhindra Baliga, Pranjali Deulkar, Nilima Thosar, Nilesh Rathi, Meghana Deshpande, Sphurti Bane
Journal of Evolution of Medical and Dental Sciences.2020; 9(15): 1256. CrossRef - Efficacy of Biodentine and Mineral Trioxide Aggregate in Primary Molar Pulpotomies—A Systematic Review and Meta-Analysis With Trial Sequential Analysis of Randomized Clinical Trials
Venkateshbabu Nagendrababu, Shaju Jacob Pulikkotil, Sajesh K. Veettil, Peerawat Jinatongthai, James L. Gutmann
Journal of Evidence Based Dental Practice.2019; 19(1): 17. CrossRef - Efficacy of Alternative Medicaments for Pulp Treatment in Primary Teeth in the Short Term: A Meta-analysis
Joon Soo Park, Bosky Jasani, Jilen Patel, Robert P. Anthonappa, Nigel M. King
Journal of Evidence Based Dental Practice.2019; 19(4): 101309. CrossRef - The evaluation of MTA and Biodentine as a pulpotomy materials for carious exposures in primary teeth
Burcu Nihan Çelik, Merve Safa Mutluay, Volkan Arıkan, Şaziye Sarı
Clinical Oral Investigations.2019; 23(2): 661. CrossRef - Effects of MTA and Brazilian propolis on the biological properties of dental pulp cells
Bingqing Shi, Yuming Zhao, Xiaojing Yuan
Brazilian Oral Research.2019;[Epub] CrossRef - MTA and biodentine for primary teeth pulpotomy: a systematic review and meta-analysis of clinical trials
Emyr Stringhini Junior, Manuela Gouvêa Campêlo dos Santos, Luciana Butini Oliveira, Montse Mercadé
Clinical Oral Investigations.2019; 23(4): 1967. CrossRef - Comparison of the success rate of a bioactive dentin substitute with those of other root restoration materials in pulpotomy of primary teeth
Hooman Shafaee, Mehrnoosh Alirezaie, Abdolrasoul Rangrazi, Erfan Bardideh
The Journal of the American Dental Association.2019; 150(8): 676. CrossRef - BiodentineTM versus formocresol pulpotomy technique in primary molars: a 12–month randomized controlled clinical trial
Omar Abd El Sadek El Meligy, Najlaa Mohamed Alamoudi, Sulaiman Mohamed Allazzam, Azza Abdel Mohsen El-Housseiny
BMC Oral Health.2019;[Epub] CrossRef - Randomized Controlled Trial of Pulpotomy in Primary Molars using MTA and Formocresol Compared to 3Mixtatin: A Novel Biomaterial
Zahra Jamali, Vajiheh Alavi, Ebrahim Najafpour, Naser Asl Aminabadi, Sajjad Shirazi
Journal of Clinical Pediatric Dentistry.2018; 42(5): 361. CrossRef - Recent Trends in Tricalcium Silicates for Vital Pulp Therapy
Imad About
Current Oral Health Reports.2018; 5(3): 178. CrossRef - Clinical and Radiographic Evaluations of Biodentine™ Pulpotomies in Mature Primary Molars (Stage 2)
Fouad Ayoub, Hitaf Nasrallah, Balsam El Noueiri, Charles Pilipili
International Journal of Clinical Pediatric Dentistry.2018; 11(6): 496. CrossRef - Clinical and radiographic evaluation of biodentine versus calcium hydroxide in primary teeth pulpotomies: a retrospective study
Silvia Caruso, Teresa Dinoi, Giuseppe Marzo, Vincenzo Campanella, Maria Rita Giuca, Roberto Gatto, Marco Pasini
BMC Oral Health.2018;[Epub] CrossRef - How does the pulpal response to Biodentine and ProRoot mineral trioxide aggregate compare in the laboratory and clinic?
R. Careddu, H. F. Duncan
British Dental Journal.2018; 225(8): 743. CrossRef - Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview – part I: vital pulp therapy
M. Parirokh, M. Torabinejad, P. M. H. Dummer
International Endodontic Journal.2018; 51(2): 177. CrossRef - Pulp treatment for extensive decay in primary teeth
Violaine Smaïl-Faugeron, Anne-Marie Glenny, Frédéric Courson, Pierre Durieux, Michele Muller-Bolla, Helene Fron Chabouis
Cochrane Database of Systematic Reviews.2018;[Epub] CrossRef - Biodentine™ material characteristics and clinical applications: a 3 year literature review and update
S. Rajasekharan, L. C. Martens, R. G. E. C. Cauwels, R. P. Anthonappa
European Archives of Paediatric Dentistry.2018; 19(1): 1. CrossRef - Microleakage and Shear Bond Strength of Biodentine at Different Setting Time
Yong Ho Song, Nanyoung Lee, Sangho Lee, Myeongkwan Jih
THE JOURNAL OF THE KOREAN ACADEMY OF PEDTATRIC DENTISTRY.2018; 45(3): 344. CrossRef - Evaluation of Biodentine Pulpotomies in Deciduous Molars with Physiological Root Resorption (Stage 3)
Fouad Ayoub, Hitaf Nasrallah, Balsam El Noueiri, Charles Pilipili
International Journal of Clinical Pediatric Dentistry.2018; 11(5): 393. CrossRef - Clinical and radiographic comparison of biodentine, mineral trioxide aggregate and formocresol as pulpotomy agents in primary molars
P. Juneja, S. Kulkarni
European Archives of Paediatric Dentistry.2017; 18(4): 271. CrossRef - Success Rates of Pulpotomies in Primary Molars Using Calcium Silicate-Based Materials: A Randomized Control Trial
Yeliz Guven, Sermin Dicle Aksakal, Nilufer Avcu, Gulcan Unsal, Elif Bahar Tuna, Oya Aktoren
BioMed Research International.2017; 2017: 1. CrossRef - Biodentine: from biochemical and bioactive properties to clinical applications
Imad About
Giornale Italiano di Endodonzia.2016; 30(2): 81. CrossRef
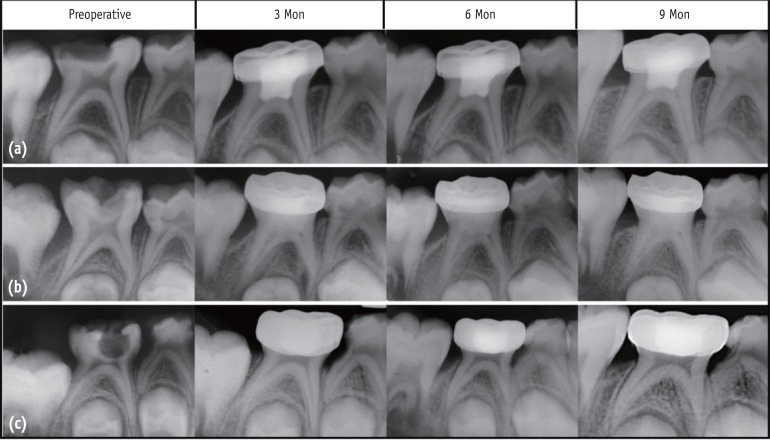
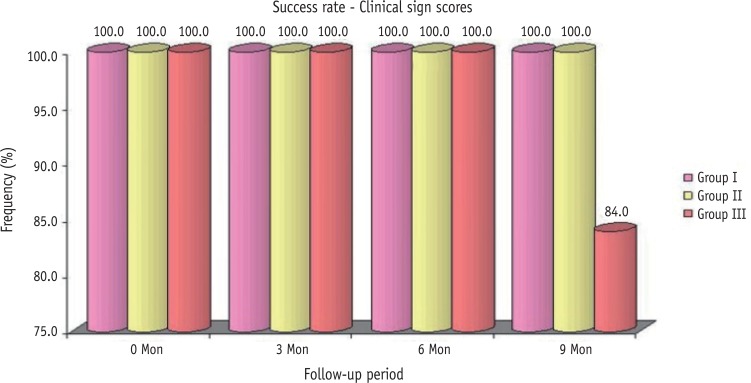
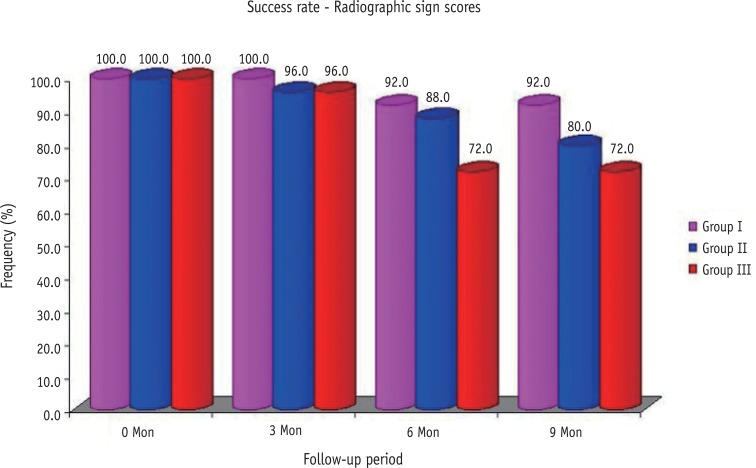
Figure 1
Figure 2
Figure 3
Clinical and radiographic scoring criteria
| Criteria for clinical and radiographic scoring | ||
|---|---|---|
| Clinical score | Clinical symptom | Definition |
| 1 | asymptomatic | •Pathology: absent |
| •Normal functioning | ||
| •Mobility (physiological) ≤ 1 mm | ||
| 2 | slight discomfort, short-lived | •Pathology: questionable |
| •Percussion sensitivity | ||
| •Gingival inflammation (due to poor oral hygiene) | ||
| •Mobility (physiological) > 1 mm, but < 2 mm | ||
| 3 | minor discomfort, short-lived | •Pathology: initial changes present |
| •Gingival swelling (not due to poor oral hygiene) | ||
| •Mobility > 2 mm, but < 3 mm | ||
| 4 | major discomfort, long-lived Extract immediately | •Pathology: late changes present |
| •Spontaneous pain | ||
| •Gingival swelling (not due to poor oral hygiene) | ||
| •Periodontal pocket formation (exudate) | ||
| •Sinus tract present | ||
| •Mobility ≥ 3 mm | ||
| •Premature tooth loss, due to pathology | ||
| Radiographic score | Radiographic finding | Definition |
|---|---|---|
| 1 | no changes present at 6 mon follow-up* | •Internal root canal form tapering from chamber to the apex |
| •Periodontal ligament (PDL)/periapical regions; normal width and trabeculation | ||
| 2 | pathological changes of questionable clinical significance at 3 mon follow-up* | •External changes are not allowed (widened PDL) widening, abnormal inter-radicular trabeculation or variation in radiodensity |
| •Internal resorption acceptable (not perforated) | ||
| •Calcific metamorphosis is acceptable and defined as: uniformly thin root canal; shape (non-tapering); variation in radiodensity from canal to canal (one cloudier than the other) | ||
| 3 | pathological changes present at 1 mon follow-up* | •External changes are present, but not large |
| •Mildly widened PDL | ||
| •Minor inter-radicular radiolucency with trabeculation still present | ||
| •Minor external root resorption; internal resorption changes are acceptable, but not if external change is also present (perforated form) | ||
| 4 | pathological changes present Extract immediately | •Frank osseous radiolucency present |
*time period from the beginning of the treatment to the assigned follow-up
Clinical sign scores of three groups over the periods
| Time period | Clinical sign score | Group I | Group II | Group III | χ2 value | p value |
|---|---|---|---|---|---|---|
| baseline/0 mon | 1 | 25 (100.0) | 25 (100.0) | 25 (100.0) | NA | - |
| 2 | 0 (0.0) | 0 (0.0) | 0 (0.0) | |||
| 3 | 0 (0.0) | 0 (0.0) | 0 (0.0) | |||
| 4 | 0 (0.0) | 0 (0.0) | 0 (0.0) | |||
| 3 mon | 1 | 25 (100.0) | 25 (100.0) | 24 (96.0) | 2.03 | 0.363 |
| 2 | 0 (0.0) | 0 (0.0) | 1 (4.0) | |||
| 3 | 0 (0.0) | 0 (0.0) | 0 (0.0) | |||
| 4 | 0 (0.0) | 0 (0.0) | 0 (0.0) | |||
| 6 mon | 1 | 25 (100.0) | 25 (100.0) | 20 (80.0) | 10.71 | 0.030 |
| 2 | 0 (0.0) | 0 (0.0) | 4 (16.0) | |||
| 3 | 0 (0.0) | 0 (0.0) | 1 (4.0) | |||
| 4 | 0 (0.0) | 0 (0.0) | 0 (0.0) | |||
| 9 mon | 1 | 25 (100.0) | 25 (100.0) | 20 (80.0) | 10.71 | 0.030 |
| 2 | 0 (0.0) | 0 (0.0) | 1 (4.0) | |||
| 3 | 0 (0.0) | 0 (0.0) | 0 (0.0) | |||
| 4 | 0 (0.0) | 0 (0.0) | 4 (16.0) |
The numbers in the parentheses were the percentages of the cases rated as the score.
NA, not applicable.
Radiographic sign scores of three groups over the periods
| Time period | Radiographic sign score | Group I | Group II | Group III | χ2 value | p value |
|---|---|---|---|---|---|---|
| 0 mon | 1 | 25 (100.0) | 25 (100.0) | 25 (100.0) | NA | - |
| 2 | 0 (0.0) | 0 (0.0) | 0 (0.0) | |||
| 3 | 0 (0.0) | 0 (0.0) | 0 (0.0) | |||
| 4 | 0 (0.0) | 0 (0.0) | 0 (0.0) | |||
| 3 mon | 1 | 25 (100.0) | 23 (92.0) | 24 (96.0) | 3.08 | 0.544 |
| 2 | 0 (0.0) | 1 (4.0) | 0 (0.0) | |||
| 3 | 0 (0.0) | 1 (4.0) | 1 (4.0) | |||
| 4 | 0 (0.0) | 0 (0.0) | 0 (0.0) | |||
| 6 mon | 1 | 20 (80.0) | 16 (64.0) | 18 (72.0) | 13.11 | 0.041 |
| 2 | 3 (12.0) | 6 (24.0) | 0 (0.0) | |||
| 3 | 2 (8.0) | 3 (12.0) | 4 (16.0%) | |||
| 4 | 0 (0.0) | 0 (0.0) | 3 (12.0) | |||
| 9 mon | 1 | 17 (68.0) | 14 (56.0) | 18 (72.0) | 21.78 | 0.001 |
| 2 | 6 (24.0) | 6 (24.0) | 0 (0.0) | |||
| 3 | 2 (8.0) | 5 (20.0) | 1 (4.0) | |||
| 4 | 0 (0.0) | 0 (0.0) | 6 (24.0) |
The numbers in the parentheses were the percentages of the cases rated as the score.
NA, not applicable.
*time period from the beginning of the treatment to the assigned follow-up
The numbers in the parentheses were the percentages of the cases rated as the score. NA, not applicable.
The numbers in the parentheses were the percentages of the cases rated as the score. NA, not applicable.

 KACD
KACD
 ePub Link
ePub Link Cite
Cite

