Abstract
Chronic osteomyelitis with proliferative periostitis, known as Garre’s osteomyelitis, is a type of osteomyelitis characterized by a distinctive gross thickening of the periosteum of bones. Peripheral reactive bone formation can be caused by mild irritation or infection. Garre’s osteomyelitis is usually diagnosed in children and young adults, and the mandible is more affected than the maxilla. The following is a case report of a 12-year-old female patient with Garre’s osteomyelitis of the mandible due to an infection of a root canal-treated tooth. Without surgical intervention, the patient’s symptoms were relieved through nonsurgical root canal re-treatment with long-term calcium hydroxide placement. A cone-beam computed tomography image obtained 6 months after treatment completion displayed complete healing of the periapical lesion and resolution of the peripheral reactive buccal bone. Due to the clinical features of Garre's osteomyelitis, which is characterized by thickening of the periosteum, it can be mistaken for other diseases such as fibrous dysplasia. It is important to correctly diagnose Garre's osteomyelitis based on its distinctive clinical features to avoid unnecessary surgical intervention, and it can lead to minimally invasive treatment options.
-
Keywords: Calcium hydroxide; Garre’s osteomyelitis; Proliferative periostitis
INTRODUCTION
In 1893, Garré [
1] first reported chronic non-suppurative sclerotic bone inflammation characterized by distinctive gross thickening of the periosteum by the formation of new subperiosteal bone on the cortical bone and named the condition Garre's osteomyelitis. Moreover, Garre's osteomyelitis is also referred to as periostitis ossificans, non-suppurative ossifying periostitis, osteomyelitis sicca, osteomyelitis with proliferative periostitis, and other similar terms [
2]. This is a rare chronic inflammatory osteomyelitis characterized by localized thickening of the periosteum of the cortical bone due to minor irritation or infection and is more common in children and adolescents [
3,
4].
Clinically, Garre's osteomyelitis can present with mandibular enlargement leading to facial asymmetry. The affected bone appears to be hard and immobile without fluctuation. The affected mandibular bone appears to expand during intraoral examinations, but the oral mucosa typically maintains a normal color and appearance [
5]. Lesions at the root apex can be identified on radiographic images. New periosteal proliferation forms successive layers parallel to the cortical bone. As a result, cone beam computed tomography (CBCT) image displays a layered proliferative cortical appearance called an “onion peel” appearance [
6]. As previously mentioned, Garre's osteomyelitis has unique proliferative clinical features, which can be confused with other diseases like fibrous dysplasia. It is essential to diagnose Garre's osteomyelitis accurately based on its distinctive clinical features to avoid unnecessary extraction or surgery, which can manage the patient with a minimally invasive and conservative approach.
This case report describes the case of a 12-year-old girl with Garre’s osteomyelitis of the mandible caused by a root canal-treated tooth infection.
CASE REPORT
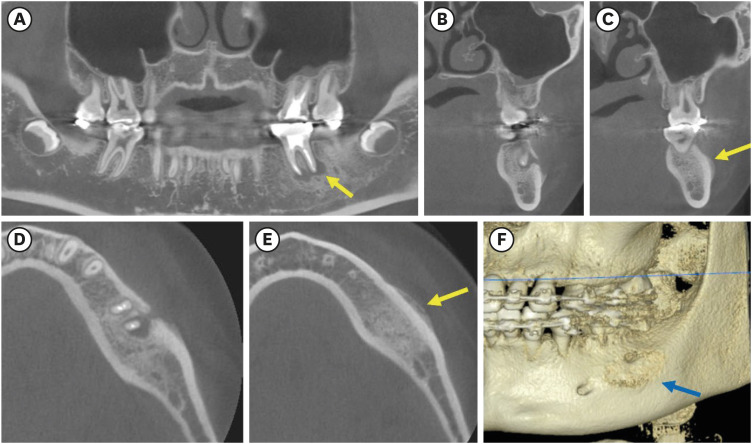
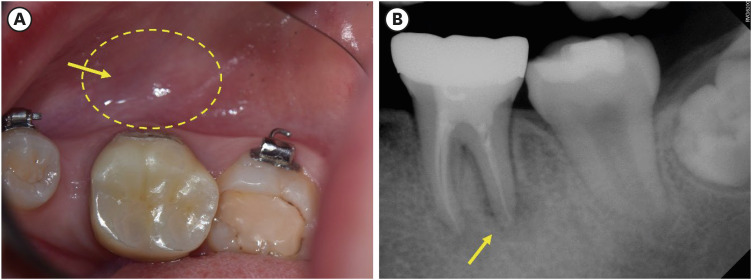
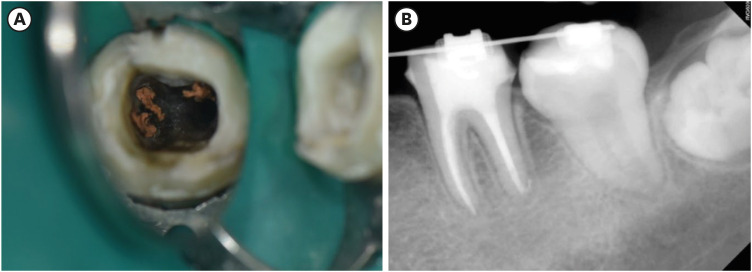
A 12-year-old female patient presented with a swelling of the left mandible. The patient had no relevant medical history. She experienced slight pain approximately 1 year before presentation, and the pain did not increase. An extraoral examination did not reveal any facial asymmetry. The patient had a dental history of endodontic treatment and zirconia crown restoration on tooth #36, which was also included in her ongoing orthodontic treatment. The medical history of the patient was non-contributory. Intraoral examination revealed a small, fixed, indurated swelling on the buccal vestibule of tooth #36 and slight pain reported by the patient upon palpation of the swelling. She reported that the intraoral indurated swelling was formed a year ago. No sinus tract was observed and the oral mucosa exhibited a normal pink coral color (
Figure 1A). The periapical radiograph revealed apical periodontitis associated with tooth #36 (
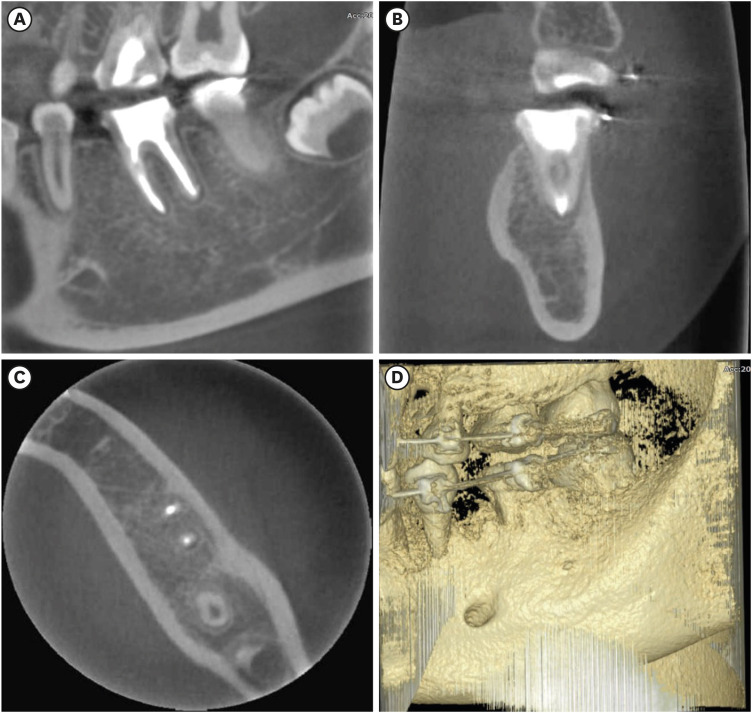
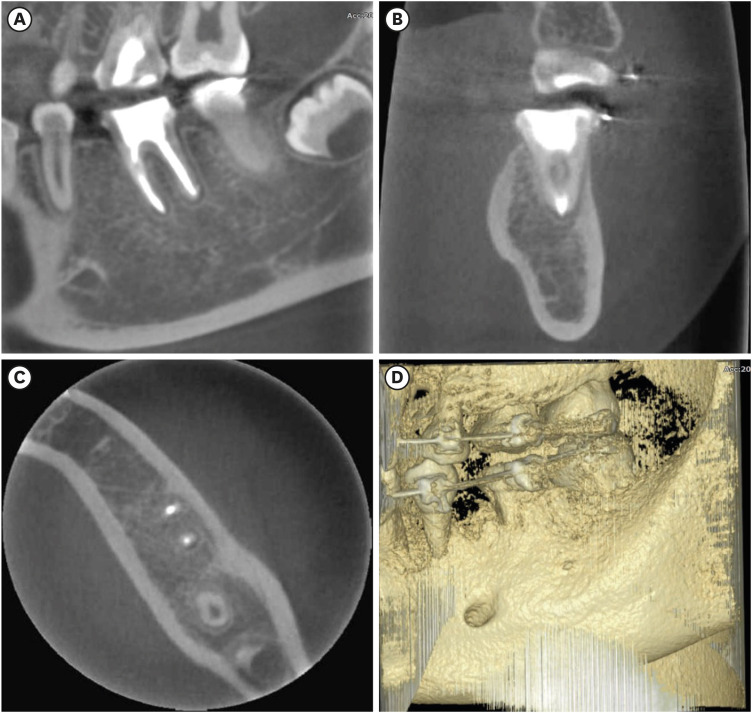
Figure 1B). A CBCT image was obtained (Alphad Vega, Asahi Roentgen Inc., Kyoto, Japan) to examine the hard nodule in the intraoral buccal vestibular area with the following parameters: 8mA, 80 kVp, and 51 × 51 mm field of view. A radiological examination via CBCT revealed the presence of a tunnel-like defect in the cortical bone of the vestibular surface. The defect was located at the apical region of tooth #36. The aforementioned defect is characterized by a periapical radiolucency (
Figure 2A-
2C). In addition to the periapical radiolucency, a new bone formation over buccal cortical bone with an “onion peel” appearance was also observed (
Figure 2D-
2F), which led to the intraoral indurated swollen mass. Tooth #36 was diagnosed as a previously treated tooth with symptomatic apical periodontitis and Garre's osteomyelitis. The treatment plan was thoroughly discussed with the patient and her parents, and nonsurgical root canal re-treatment was planned to eliminate infection from tooth #36. The patient and her parents were informed regarding the diagnosis, treatment plan, and treatment methods and signed a consent form and further publication of the case. Whole dental treatment was performed by one operator (H.K.), who was a resident majoring in endodontics of conservative dentistry, and assisted by an endodontist with experience of more than 15 years (J.H.J.).
Figure 1 Preoperative examination. (A) A clinical photograph displaying the normal coral-pink color of the buccal vestibule of tooth #36 and the absence of a sinus tract. (B) A periapical radiograph displaying apical radiolucency associated with #36.
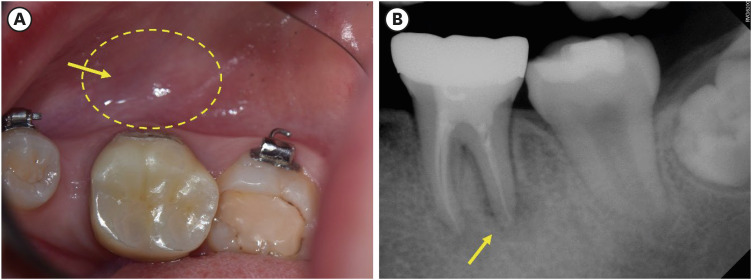
Figure 2 Cone beam computed tomography images of tooth #36. (A) A sagittal image displaying periapical radiolucency of tooth #36. (B, C) The coronal view exhibits unique proliferative buccal cortical bone formation (arrow). (D, E) The axial view displays a typical “onion skin-like appearance over the cortical bone (arrow). (F) Three-dimensional reconstruction image presenting buccal bone changes which indicate the neo-hard tissue formation (arrow).

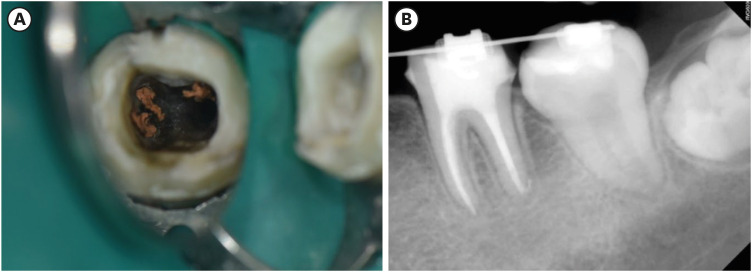
Local anesthesia was obtained with 1.8 mL 2% lidocaine hydrochloride solution containing 1:100,000 epinephrine (Huons, Seongnam, Korea) by buccal infiltration technique. After the removal of the #36 zirconia crown, the access cavity was prepared under rubber dam isolation. The contaminated gutta-percha (
Figure 3A) and core material were removed under a dental operating microscope (Extaro 300, Zeiss, Oberkochen, Germany) with D1 and D2 ProTaper universal retreatment files (size 30/09 taper and size 25/08 taper, respectively). The root canals were copiously irrigated with 2.5% sodium hypochlorite using a side-vented syringe, followed by passive ultrasonic irrigation using UC-One (EP dent, Gimpo, Korea) for 10 seconds ×5 cycles. Moreover, the canals were dried, and calcium hydroxide was placed with a lentulo spiral in the root canal and sealed with a temporary coronal sealing material (Caviton, GC, Tokyo, Japan), followed by temporary crown restoration, which was fabricated and cemented with Protemp 4 (3M ESPE, Seefeld, Germany) and TempBond NE (Kerr, Hamm, Germany), respectively. At 1-month intervals, root canal irrigation and calcium hydroxide replacement were performed.
Figure 3 Intraoperative photograph and follow-up periapical radiograph. (A) After removal of composite resin core, contaminated gutta-percha cones were observed. (B) Six-month follow-up after nonsurgical root canal retreatment revealed the resolution of periapical radiolucency. Tooth #36 is asymptomatic and functional.
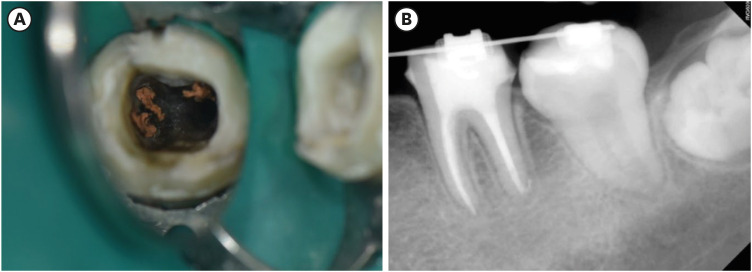
The patient exhibited no signs or symptoms 3 months after the first appointment. No discomfort on percussion or palpation was observed, and the small hard nodule disappeared. The root canals were obturated with gutta-percha cones and a calcium silicate-based sealer (Ceraseal, Meta Biomed, Cheongju, Korea) (
Figure 3B), followed by restoration with a dual-cure resin core (LuxaCore Z, DMG, Hamburg, Germany) and provisional hybrid crown restoration. The periapical radiograph displayed increased radiopacity around tooth #36, indicating the resolution of the periapical lesion.
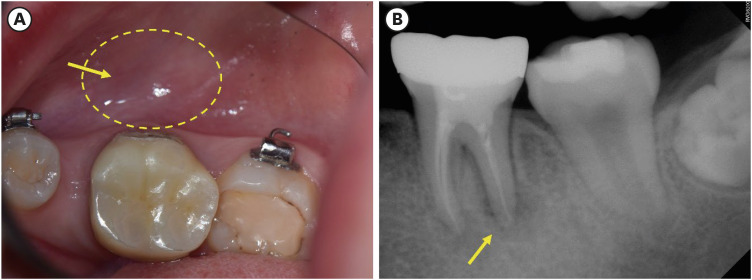
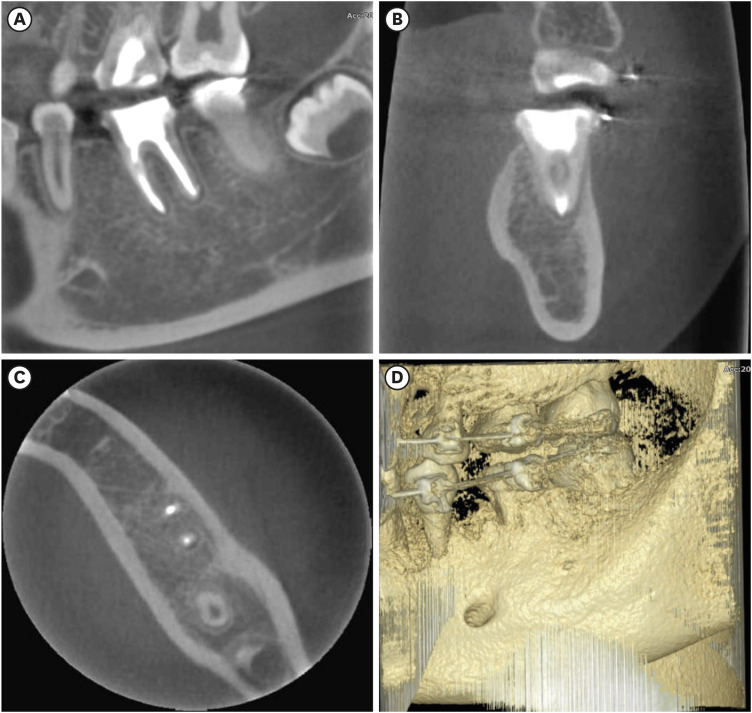
When the patient was evaluated 6 months after her last endodontic treatment, the patient had no symptoms or discomfort, and tooth #36 was functional, although the tooth was undergoing orthodontic treatment. A periapical radiograph and CBCT image were obtained to track the development of the newly formed hard proliferative tissue on the buccal surface. Complete healing of the apical area of #36 and the disappearance of new bone formation were observed (
Figure 4).
Figure 4 Cone beam computed tomography images of tooth #36 after 6-month follow-up. (A) A sagittal image displaying the complete resolution of periapical radiolucency of tooth #36. (B, C) Coronal and axial views display the absence of buccal cortical bone formation. (D) Three-dimensional reconstruction image presents normal buccal bone anatomy of the mandible.
DISCUSSION
In this case report, we diagnosed Garre’s osteomyelitis, a unique subtype of chronic osteomyelitis with distinctive gross thickening of the periosteum of the bones that rarely occurs in young patients.
Osteomyelitis is a condition characterized by a bone infection usually caused by microorganisms, such as bacteria, entering the bone through a wound or the bloodstream. This infection can result in vascular thrombosis and bone collapse, eventually affecting the cortical bone, disrupting blood supply, and leading to ischemia and sequestrum formation [
7]. To effectively treat osteomyelitis, most cases require extensive surgical resection and debridement of both the infected bone and the adjacent teeth with antimicrobial therapy [
8].
Garre's osteomyelitis is a distinct type of chronic osteomyelitis usually associated with persistent low-grade infections, often as a result of dental infections or periodontal disease. One of the distinct features of Garre's osteomyelitis is the periosteal reaction. In response to chronic inflammation, the periosteum thickens and creates new bone layers, resulting in the development of sclerotic or dense bone [
9]. Over time, persistent inflammation and the formation of new bone layers cause the affected bone to become thick and dense. Sclerosis can be identified in imaging studies, such as radiographs or computed tomography scans, as an identifiable pattern of increased bone density. In this case, the patient did not exhibit any facial asymmetry; however, a firm mass was palpable in the vestibule of tooth #36, located unilaterally, and not easily identified on the periapical radiograph. Initially, a provisional diagnosis of chronic apical periodontitis was made based on the periapical radiographs. However, upon observing the characteristic “onion peel” appearance on the CBCT image, a provisional diagnosis of Garre's osteomyelitis was established. Furthermore, CBCT is a valuable diagnostic tool in cases of Garre's osteomyelitis. Additionally, occlusal radiographs, considering radiation exposure, could also assist in the diagnosis [
6,
9].
Several cases have reported successful outcomes of Garre’s osteomyelitis treatment using endodontic therapy [
9,
10,
11,
12]. Calcium hydroxide is used as an intermediate medication. Zand
et al. [
11] supported the use of calcium hydroxide as an intracanal medication for the treatment of osteomyelitis. Calcium hydroxide is considered the first choice of root canal dressing materials, which has a wide range of antimicrobial effects against common endodontic pathogens. The antimicrobial effect is related to the hydroxyl ions, which lead to the highly alkaline environment released in an aqueous environment, which affects cell membranes, proteins, and the DNA of microorganisms [
13,
14]. Despite the conventional and extensive preference of dental clinicians to deal with persistent chronic endodontic lesions, there has been a controversial issue with the use of calcium hydroxide as an intracanal medicament due to its effectiveness and difficulties in removal from the root canals [
15]. In this case, elimination of the periapical infection was successfully achieved by nonsurgical root canal re-treatment with 1-month intracanal calcium hydroxide medicaments, and complete bone healing was observed on periapical radiograph and CBCT radiography after 6 months of follow-up. The healing follow-up, which confirmed the visual resolution of the proliferative bone formation using the 3-dimensional CBCT image, has been rarely demonstrated in the management of Garre`s osteomyelitis to the best of our knowledge.
During the whole treatment period, systemic antibiotics were not administered without the use of systemic antibiotics as the patient did not present with severe symptoms, and no sign of fever or systematic infection. In this case, the source of infection was easy to identify (tooth 36). However, in cases where the source of infection is not easily distinguished, a biopsy for histological examination and the administration of systemic antibiotics could be considered.
The differential diagnosis between Garre's osteomyelitis and other diseases is also important. Fibrous dysplasia presents with clinical symptoms and radiological findings similar to those of Garre's osteomyelitis and is characterized by enlargement of the affected jaw with sclerotic bone. In cases of Garre's osteomyelitis, the main feature is subperiosteal new bone formation, while fibrous dysplasia involves secondary bone deposition outside the endosteum. Fibrous dysplasia can cause expansion of adjacent bone however, it is characterized to maintain an intact thinned cortical boundary [
16]. Therefore, an accurate differential diagnosis requires the consideration of clinical symptoms, radiological findings, and histopathological examination.
CONCLUSIONS
In this case, Garre’s osteomyelitis of the left mandible with an infected root-filled tooth was successfully managed with nonsurgical root canal re-treatment accompanied by long-term calcium hydroxide intracanal medication. At the 6-month follow-up with periapical radiography and CBCT, the periapical lesion had resolved along with the disappearance of the newly formed periosteal hard tissue.
Due to the clinical features of Garre's osteomyelitis, which is characterized by thickening of the periosteum, it can be mistaken for other diseases such as fibrous dysplasia. It is important to correctly diagnose Garre's osteomyelitis based on its distinctive clinical features to avoid unnecessary surgical intervention, and it can lead to minimally invasive treatment options.
-
Funding: This research was supported by the Bio & Medical Technology Development Program of the National Research Foundation (NRF) and funded by the Korean government (MSIP and MSIP&MOHW) (No. 22022R1C1C100785112).
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Jang JH.
Data curation: Kim H.
Formal analysis: Kim H, Jang JH.
Funding acquisition: Jang JH.
Investigation: Kim H.
Methodology: Kim H, Oh S, Jang JH.
Project administration: Kim DS, Jang JH.
Visualization: Kim H, Kwon J.
Writing - original draft: Kim H.
Writing - review & editing: Kim H, Jang JH.
REFERENCES
- 1. Garré C. Über besondere formen und folgezustande der akuten infekfionsen osteomyelitis. Beitr Z Klin Chir 1893;10:241-298.
- 2. Lichty G, Langlais RP, Aufdemorte T. Garré’s osteomyelitis. Literature review and case report. Oral Surg Oral Med Oral Pathol 1980;50:309-313.PubMed
- 3. Seok H, Kim SG, Song JY. Proliferative periostitis of the mandibular ramus and condyle: a case report. J Korean Assoc Oral Maxillofac Surg 2015;41:198-202.ArticlePubMedPMC
- 4. Suma R, Vinay C, Shashikanth MC, Subba Reddy VV. Garre’s sclerosing osteomyelitis. J Indian Soc Pedod Prev Dent 2007;25(Supplment):S30-S33.PubMed
- 5. Eisenbud L, Miller J, Roberts IL. Garré’s proliferative periostitis occurring simultaneously in four quadrants of the jaws. Oral Surg Oral Med Oral Pathol 1981;51:172-178.ArticlePubMed
- 6. Batcheldor GD Jr, Giansanti JS, Hibbard ED, Waldron CA. Garré’s osteomyelitis of the jaws: a review and report of two cases. J Am Dent Assoc 1973;87:892-897.ArticlePubMed
- 7. Kannan SK, Sandhya G, Selvarani R. Periostitis ossificans (Garrè’s osteomyelitis) radiographic study of two cases. Int J Paediatr Dent 2006;16:59-64.ArticlePubMed
- 8. Dym H, Zeidan J. Microbiology of acute and chronic osteomyelitis and antibiotic treatment. Dent Clin North Am 2017;61:271-282.ArticlePubMed
- 9. Jalali P, Riccobono J, Augsburger RA, Tahmasbi-Arashlow M. Radiographic patterns of periosteal bone reactions associated with endodontic lesions. Restor Dent Endod 2023;48:e23.ArticlePubMedPMCPDF
- 10. McWalter GM, Schaberg SJ. Garre’s osteomyelitis of the mandible resolved by endodontic treatment. J Am Dent Assoc 1984;108:193-195.ArticlePubMed
- 11. Zand V, Lotfi M, Vosoughhosseini S. Proliferative periostitis: a case report. J Endod 2008;34:481-483.ArticlePubMed
- 12. Aeran H, Tuli A, Pokhiriyal A, Chaudhary A. Management of Garré’s sclerosing osteomyelitis by endodontic therapy: a case report. Int J Oral Health Dent 2018;4:55-57.Article
- 13. Kim D, Kim E. Antimicrobial effect of calcium hydroxide as an intracanal medicament in root canal treatment: a literature review - part I. In vitro studies. Restor Dent Endod 2014;39:241-252.ArticlePubMedPMC
- 14. Kim D, Kim E. Antimicrobial effect of calcium hydroxide as an intracanal medicament in root canal treatment: a literature review - part II. In vivo studies. Restor Dent Endod 2015;40:97-103.ArticlePubMedPMC
- 15. Ibrahim AM, Zakhary SY, Amin SA. Calcium hydroxide intracanal medication effects on pain and flare-up: a systematic review and meta-analysis. Restor Dent Endod 2020;45:e26.ArticlePubMedPMCPDF
- 16. Petrikowski CG, Pharoah MJ, Lee L, Grace MG. Radiographic differentiation of osteogenic sarcoma, osteomyelitis, and fibrous dysplasia of the jaws. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995;80:744-750.ArticlePubMed
 , Jiyoung Kwon
, Jiyoung Kwon , Hyun-Jung Kim
, Hyun-Jung Kim , Soram Oh
, Soram Oh , Duck-Su Kim
, Duck-Su Kim , Ji-Hyun Jang
, Ji-Hyun Jang



 KACD
KACD

 ePub Link
ePub Link Cite
Cite

