Articles
- Page Path
- HOME > Restor Dent Endod > Volume 47(3); 2022 > Article
- Research Article Chitosan-induced biomodification on demineralized dentin to improve the adhesive interface
-
Isabella Rodrigues Ziotti
 , Vitória Leite Paschoini
, Vitória Leite Paschoini , Silmara Aparecida Milori Corona
, Silmara Aparecida Milori Corona , Aline Evangelista Souza-Gabriel
, Aline Evangelista Souza-Gabriel
-
Restor Dent Endod 2022;47(3):e28.
DOI: https://doi.org/10.5395/rde.2022.47.e28
Published online: June 15, 2022
Department of Restorative Dentistry, School of Dentistry of Ribeirão Preto, University of São Paulo, Ribeirão Preto, SP, Brazil.
- Correspondence to Vitória Leite Paschoini, DDS, MSc. Graduate Student, Department of Restorative Dentistry, School of Dentistry of Ribeirão Preto, University of São Paulo, Av. Café s/n, Monte Alegre, Ribeirão Preto, SP 14040-904, Brazil. vitoria.paschoini@usp.br
Copyright © 2022. The Korean Academy of Conservative Dentistry
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Objectives Metalloproteinase-inhibiting agents, such as chitosan, can prevent collagen degradation in demineralized dental substrates, thereby improving the adhesive interface. This study evaluated the bond strength (BS) and chemical and morphological characterization of the adhesive interface after applying chitosan solution to demineralized dentin.
-
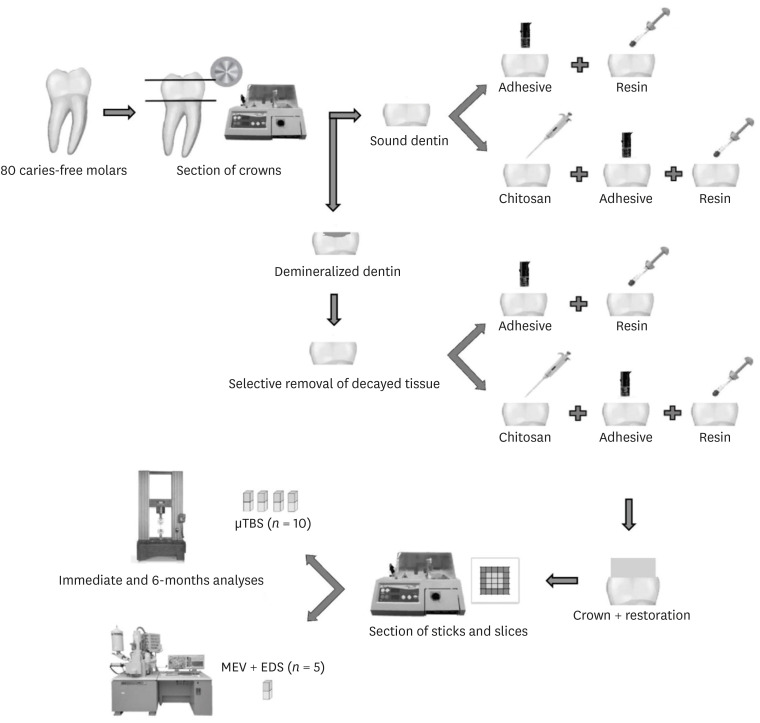
Materials and Methods The 80 third molars were selected. Forty teeth underwent caries induction using the pH cycling method. The teeth were divided according to the treatment: distilled water (control) and 2.5% chitosan solution. The surfaces were restored using adhesive and composite resins. Half of the specimens in each group were aged, and the other half underwent immediate analyses. The teeth were sectioned and underwent the microtensile bond strength test (µTBS), and chemical and morphological analyses using energy-dispersive spectroscopy and scanning electron microscopy, respectively. Data analysis was performed using 3-way analysis of variance.
-
Results For µTBS, sound dentin was superior to demineralized dentin (p < 0.001), chitosan-treated specimens had higher bond strength than the untreated ones (p < 0.001), and those that underwent immediate analysis had higher values than the aged specimens (p = 0.019). No significant differences were observed in the chemical or morphological compositions.
-
Conclusions Chitosan treatment improved bond strength both immediately and after aging, even in demineralized dentin.
INTRODUCTION
MATERIALS AND METHODS
Material’s particulars used in this study
RESULTS
Microtensile bond strength mean values and standard deviations of dentin with water (control) and chitosan solution
3-way analysis of variance interaction regarding the substrate, dentin treatment, and aging
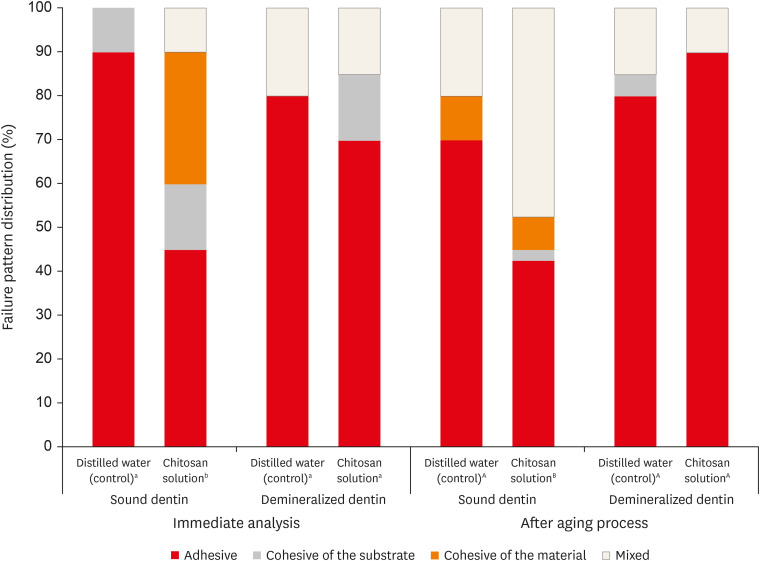
Frequency distribution of the failure patterns (%) after microtensile bond strength (µTBS) test. Different letters indicate significant difference among groups. Capital letters correspond to immediate analysis and lowercase letters to after aging process (χ2 test, p < 0.05).
Mean and standard deviations of the atomic percentage (wt%) of chemical elements in the specimens
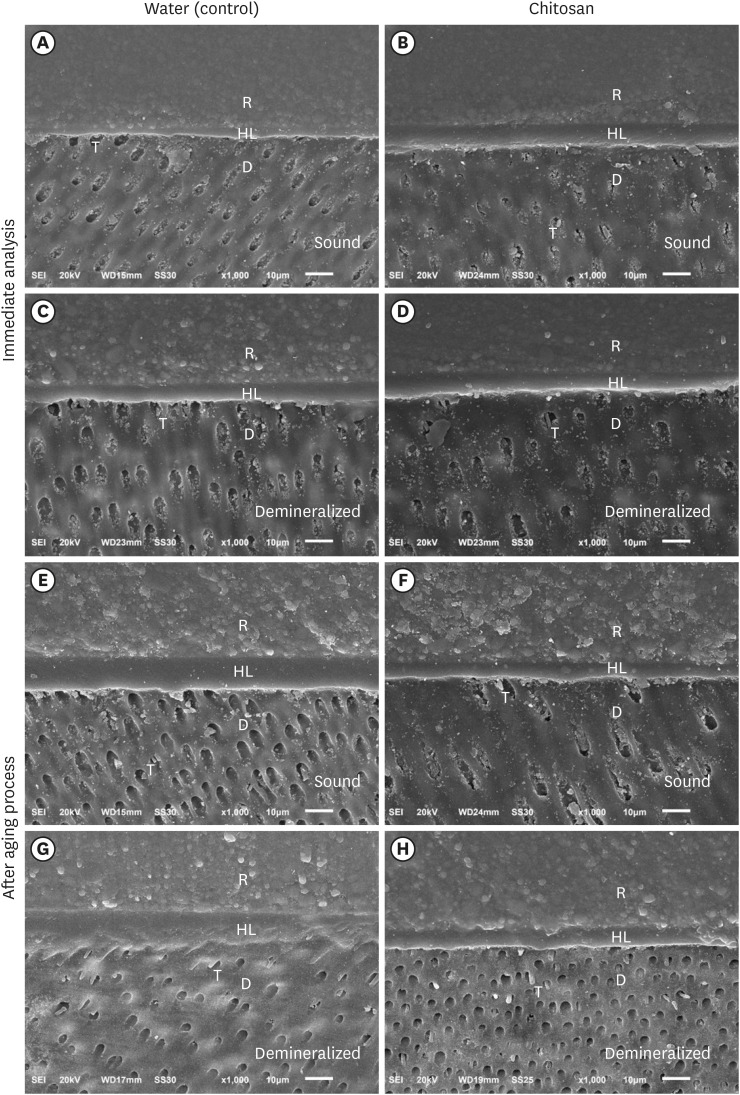
Photomicrographs (×1,000) of the adhesive interface - Immediately after the adhesive procedure: (A) Sound dentin with water (control); (B) Sound dentin with chitosan; (C) Demineralized dentin with water and (D) Demineralized dentin with chitosan. After aging of the adhesive interface: (E) Sound dentin with water (control); F) Sound dentin with chitosan; (G) Demineralized dentin with water; and (H) Demineralized dentin with chitosan. R, resin; HL, hybrid layer; D, dentin; T, resin tags.
DISCUSSION
CONCLUSIONS
ACKNOWLEDGEMENTS
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Ziotti IR.
Souza-Gabriel AE. Data curation: Ziotti IR.
Souza-Gabriel AE. Formal analysis: Souza-Gabriel AE. Funding acquisition.
Souza-Gabriel AE. Investigation: Ziotti IR. Methodology.
Ziotti IR. Project administration and Supervision: Souza-Gabriel AE. Resources.
Souza-Gabriel AE. Software: Ziotti IR.
Souza-Gabriel AE. Writing - original draft: Ziotti IR.
Souza-Gabriel AE. Writing - review & editing: Paschoini VL.
- 1. Brostek AM, Walsh LJ. Minimal intervention dentistry in general practice. Oral Health Dent Manag 2014;13:285-294.PubMed
- 2. Comert S, Oz AA. Clinical effect of a fluoride-releasing and rechargeable primer in reducing white spot lesions during orthodontic treatment. Am J Orthod Dentofacial Orthop 2020;157:67-72.ArticlePubMed
- 3. Perdigão J. Dentin bonding-variables related to the clinical situation and the substrate treatment. Dent Mater 2010;26:e24-e37.ArticlePubMed
- 4. Chaussain-Miller C, Fioretti F, Goldberg M, Menashi S. The role of matrix metalloproteinases (MMPs) in human caries. J Dent Res 2006;85:22-32.ArticlePubMedPDF
- 5. Kato MT, Leite AL, Hannas AR, Calabria MP, Magalhães AC, Pereira JC, Buzalaf MA. Impact of protease inhibitors on dentin matrix degradation by collagenase. J Dent Res 2012;91:1119-1123.ArticlePubMedPDF
- 6. Park KM, Lee HJ, Koo KT, Ben Amara H, Leesungbok R, Noh K, Lee SC, Lee SW. Oral soft tissue regeneration using nano controlled system inducing sequential release of trichloroacetic acid and epidermal growth factor. Tissue Eng Regen Med 2020;17:91-103.ArticlePubMedPMCPDF
- 7. Mazzi-Chaves JF, Martins CV, Souza-Gabriel AE, Brito-Jùnior M, Cruz-Filho AM, Steier L, Sousa-Neto MD. Effect of a chitosan final rinse on the bond strength of root canal fillings. Gen Dent 2019;67:54-57.PubMed
- 8. Machado AH, Garcia IM, Motta AS, Leitune VC, Collares FM. Triclosan-loaded chitosan as antibacterial agent for adhesive resin. J Dent 2019;83:33-39.ArticlePubMed
- 9. Rodrigues MR. Synthesis and investigation of chitosan derivatives formed by reaction with acyl chlorides. J Carbohydr Chem 2005;24:41-54.Article
- 10. Kong M, Chen XG, Xing K, Park HJ. Antimicrobial properties of chitosan and mode of action: a state of the art review. Int J Food Microbiol 2010;144:51-63.ArticlePubMed
- 11. Chronopoulou L, Nocca G, Castagnola M, Paludetti G, Ortaggi G, Sciubba F, Bevilacqua M, Lupi A, Gambarini G, Palocci C. Chitosan based nanoparticles functionalized with peptidomimetic derivatives for oral drug delivery. N Biotechnol 2016;33:23-31.ArticlePubMed
- 12. Curylofo-Zotti FA, Tanta GS, Zucoloto ML, Souza-Gabriel AE, Corona SA. Selective removal of carious lesion with Er:YAG laser followed by dentin biomodification with chitosan. Lasers Med Sci 2017;32:1595-1603.ArticlePubMedPDF
- 13. Baena E, Cunha SR, Maravić T, Comba A, Paganelli F, Alessandri-Bonetti G, Ceballos L, Tay FR, Breschi L, Mazzoni A. Effect of chitosan as a cross-linker on matrix metalloproteinase activity and bond stability with different adhesive systems. Mar Drugs 2020;18:18.Article
- 14. Persadmehr A, Torneck CD, Cvitkovitch DG, Pinto V, Talior I, Kazembe M, Shrestha S, McCulloch CA, Kishen A. Bioactive chitosan nanoparticles and photodynamic therapy inhibit collagen degradation in vitro . J Endod 2014;40:703-709.PubMed
- 15. Anjana J, Mohandas A, Seethalakshmy S, Suresh MK, Menon R, Biswas R, Jayakumar R. Bi-layered nanocomposite bandages for controlling microbial infections and overproduction of matrix metalloproteinase activity. Int J Biol Macromol 2018;110:124-132.ArticlePubMed
- 16. Curylofo-Zotti FA, Scheffel DL, Macedo AP, Souza-Gabriel AE, Hebling J, Corona SA. Effect of Er:YAG laser irradiation and chitosan biomodification on the stability of resin/demineralized bovine dentin bond. J Mech Behav Biomed Mater 2019;91:220-228.ArticlePubMed
- 17. Pini NI, Lima DA, Luka B, Ganss C, Schlueter N. Viscosity of chitosan impacts the efficacy of F/Sn containing toothpastes against erosive/abrasive wear in enamel. J Dent 2020;92:103247.ArticlePubMed
- 18. Fawzy AS, Nitisusanta LI, Iqbal K, Daood U, Beng LT, Neo J. Chitosan/Riboflavin-modified demineralized dentin as a potential substrate for bonding. J Mech Behav Biomed Mater 2013;17:278-289.ArticlePubMed
- 19. Hashimoto M, Tay FR, Svizero NR, de Gee AJ, Feilzer AJ, Sano H, Kaga M, Pashley DH. The effects of common errors on sealing ability of total-etch adhesives. Dent Mater 2006;22:560-568.ArticlePubMed
- 20. Marquezan PK, Alves LS, Dalla Nora A, Maltz M, do Amaral Zenkner JE. Radiographic pattern of underlying dentin lesions (ICDAS 4) in permanent teeth. Clin Oral Investig 2019;23:3879-3883.ArticlePubMedPDF
- 21. Daood U, Iqbal K, Nitisusanta LI, Fawzy AS. Effect of chitosan/riboflavin modification on resin/dentin interface: spectroscopic and microscopic investigations. J Biomed Mater Res A 2013;101:1846-1856.ArticlePubMedPDF
- 22. Profeta AC, Mannocci F, Foxton RM, Thompson I, Watson TF, Sauro S. Bioactive effects of a calcium/sodium phosphosilicate on the resin-dentine interface: a microtensile bond strength, scanning electron microscopy, and confocal microscopy study. Eur J Oral Sci 2012;120:353-362.ArticlePubMed
- 23. Borsatto MC, Martinelli MG, Contente MM, Mellara TS, Pécora JD, Galo R. Bond durability of Er:YAG laser-prepared primary tooth enamel. Braz Dent J 2013;24:330-334.ArticlePubMed
- 24. Ganss C, Klimek J, Brune V, Schürmann A. Effects of two fluoridation measures on erosion progression in human enamel and dentine in situ . Caries Res 2004;38:561-566.ArticlePubMedPDF
- 25. Castellan CS, Bedran-Russo AK, Antunes A, Pereira PN. Effect of dentin biomodification using naturally derived collagen cross-linkers: one-year bond strength study. Int J Dent 2013;2013:918010.ArticlePubMedPMCPDF
- 26. Ururahy MS, Curylofo-Zotti FA, Galo R, Nogueira LF, Ramos AP, Corona SA. Wettability and surface morphology of eroded dentin treated with chitosan. Arch Oral Biol 2017;75:68-73.ArticlePubMed
- 27. Gu LS, Cai X, Guo JM, Pashley DH, Breschi L, Xu HH, Wang XY, Tay FR, Niu LN. Chitosan-based extrafibrillar demineralization for dentin bonding. J Dent Res 2019;98:186-193.ArticlePubMedPDF
- 28. Costa AR, Garcia-Godoy F, Correr-Sobrinho L, Naves LZ, Raposo LH, Carvalho FG, Sinhoreti MA, Puppin-Rontani RM. Influence of different dentin substrate (caries-affected, caries-infected, sound) on long-term μTBS. Braz Dent J 2017;28:16-23.ArticlePubMed
- 29. Yoshiyama M, Tay FR, Torii Y, Nishitani Y, Doi J, Itou K, Ciucchi B, Pashley DH. Resin adhesion to carious dentin. Am J Dent 2003;16:47-52.PubMed
- 30. Stenhagen IS, Rukke HV, Dragland IS, Kopperud HM. Effect of methacrylated chitosan incorporated in experimental composite and adhesive on mechanical properties and biofilm formation. Eur J Oral Sci 2019;127:81-88.ArticlePubMedPDF
- 31. Diolosà M, Donati I, Turco G, Cadenaro M, Di Lenarda R, Breschi L, Paoletti S. Use of methacrylate-modified chitosan to increase the durability of dentine bonding systems. Biomacromolecules 2014;15:4606-4613.ArticlePubMed
- 32. Perdigão J. New developments in dental adhesion. Dent Clin North Am 2007;51:333-357.ArticlePubMed
- 33. Rohanizadeh R, LeGeros RZ, Fan D, Jean A, Daculsi G. Ultrastructural properties of laser-irradiated and heat-treated dentin. J Dent Res 1999;78:1829-1835.ArticlePubMedPDF
- 34. Beltrame APCA, Suchyta D, Abd Alraheam I, Mohammed A, Schoenfisch M, Walter R, Almeida IC, Souza LC, Miguez PA. Effect of phosphorylated chitosan on dentin erosion: an in vitro study. Caries Res 2018;52:378-386.ArticlePubMedPDF
REFERENCES
Tables & Figures
REFERENCES
Citations

- Recent advances in medical applications of chitosan-based biomaterials
Dinesh Kumar Sharma
International Journal of Polymeric Materials and Polymeric Biomaterials.2025; 74(11): 1027. CrossRef - Push-Out Bond Strength of Different Luting Cements Following Post Space Irrigation with 2% Chitosan: An In Vitro Study
Shimaa Rifaat, Ahmed Rahoma, Hind Muneer Alharbi, Sawsan Jamal Kazim, Shrouq Ali Aljuaid, Basmah Omar Alakloby, Faraz A. Farooqi, Noha Taymour
Prosthesis.2025; 7(1): 18. CrossRef - Bioinspired Dentin Biomodification: Current Evidence and Emerging Approaches
Priyanka S R, Sharath Pare
International Journal of Innovative Science and Research Technology.2025; : 219. CrossRef - A synergistic approach to tooth remineralization using nano-chitosan, fluoride, and pulsed magnetic field
Alaa M. Khalil, Samar A. Abbassy, Mona Mohy ElDin, Sherif Kandil, Ahmed M. El-Khatib
Scientific Reports.2025;[Epub] CrossRef - Chitosan-based Nano/Biomaterials in Bone Tissue Engineering and Regenerative Medicine: Recent Progress and Advances
Taha Jafari, Seyed Morteza Naghib, M. R. Mozafari
Current Organic Synthesis.2025; 22(4): 457. CrossRef - Influence of Non-Staining Chitosan-Based Nano-Silver Fluoride on Shear Bond Strengths of Dental Restorations
Bennett T. Amaechi, Sima Abdollahi, Tejal Gohil, Amos C. Obiefuna, Temitayo Omoniyi, Temitope O. Omosebi, Thais S. Phillips, Noha Elhabashi
Journal of Composites Science.2025; 9(10): 518. CrossRef - Does dentin pretreatment with chitosan improve the bond strength of restorative material? A systematic review and meta-analysis of in vitro studies
Luísa Valente Gotardo Lara Alves, Nathália Mancioppi Cerqueira, Amanda Pelegrin Candemil, André Luis Faria-e-Silva, Manoel Damião Sousa-Neto, Aline Evangelista Souza-Gabriel
International Journal of Adhesion and Adhesives.2024; 128: 103553. CrossRef - Comparative Evaluation of Apical Leakage in Root Canal Obturation Using AH Plus Sealer, Bioceramic Sealer, and Bioceramic Sealer Incorporated With Chitosan Nanoparticles: An In Vitro Study
Sushmita Rane, Varsha Pandit, Sanpreet S Sachdev, Shivani Chauhan, Rishabh Mistry, Barun Kumar
Cureus.2024;[Epub] CrossRef - Aesthetic impact of resin infiltration and its mechanical effect on ceramic bonding for white spot lesions
Jiaen Shu, Yijia Huang, Xueying Ma, Zhonghua Duan, Pei Wu, Sijing Chu, Yuqiong Wu, Yuhua Wang
BMC Oral Health.2024;[Epub] CrossRef - Effect of Incorporating Chitosan to Resin Modified Glass Ionomer Cement on Shear Bond Strength to Dentin (An In vitro Comparative Study)
Aya Tahseen Khudhair, Muna Saleem Khalaf
Journal of International Society of Preventive and Community Dentistry.2024; 14(3): 225. CrossRef - Biomodification of eroded and abraded dentin with epigallocatechin-3-gallate (EGCG)
Bruna Dantas Abreu, Renata Siqueira Scatolin, Silmara Aparecida Milori Corona, Fabiana Almeida Curylofo Zotti
Journal of the Mechanical Behavior of Biomedical Materials.2023; 147: 106158. CrossRef - Chitosan-Based Biomaterials for Tissue Regeneration
Yevgeniy Kim, Zharylkasyn Zharkinbekov, Kamila Raziyeva, Laura Tabyldiyeva, Kamila Berikova, Dias Zhumagul, Kamila Temirkhanova, Arman Saparov
Pharmaceutics.2023; 15(3): 807. CrossRef - Er:YAG laser in selective caries removal and dentin treatment with chitosan: a randomized clinical trial in primary molars
Rai Matheus Carvalho Santos, Renata Siqueira Scatolin, Sérgio Luiz de Souza Salvador, Aline Evangelista Souza-Gabriel, Silmara Aparecida Milori Corona
Lasers in Medical Science.2023;[Epub] CrossRef - Effect of Dentin Surface Pretreatment With Chitosan Nanoparticles on Immediate and Prolonged Shear Bond Strength of Resin Composite: An in Vitro Study
Shaymaa Ali Abdul-Razzaq, Muna Saleem Khalaf
Dental Hypotheses.2023; 14(3): 84. CrossRef - MODERN TRENDS AND PERSPECTIVES OF THE DEVELOPMENT OF ADHESIVE DENTISTRY. INNOVATIVE TECHNIQUES FOR THE APPLICATION OF ADHESIVE SYSTEMS
Oleksandr O. Pompii, Viktor A. Tkachenko, Tetiana M. Kerimova, Elina S. Pompii
Wiadomości Lekarskie.2023; 76(12): 2721. CrossRef
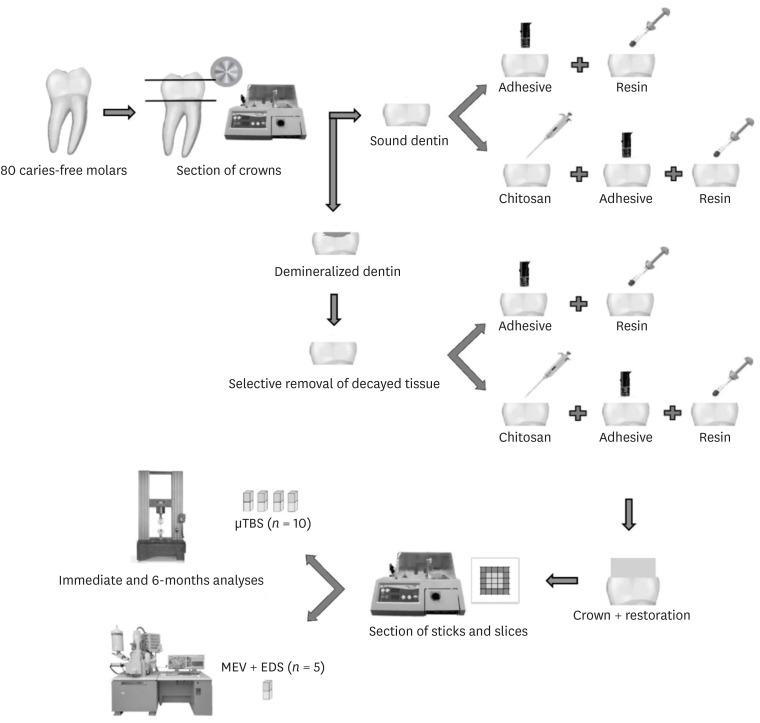
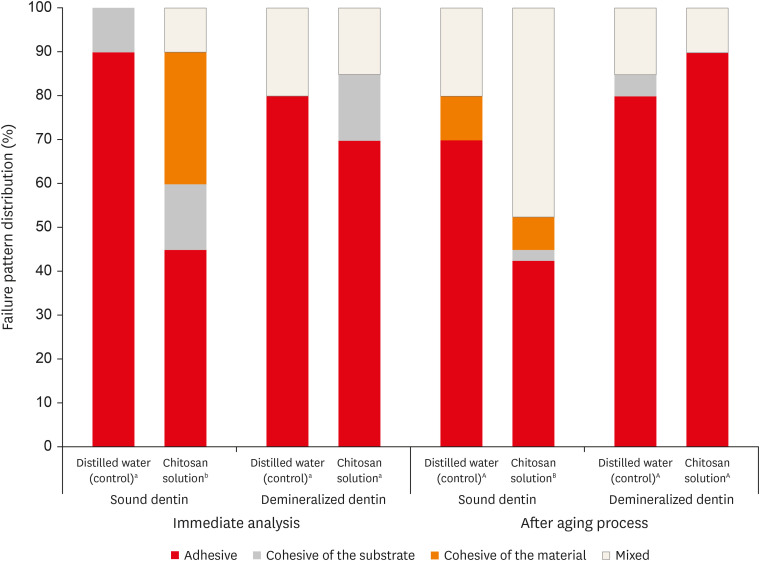
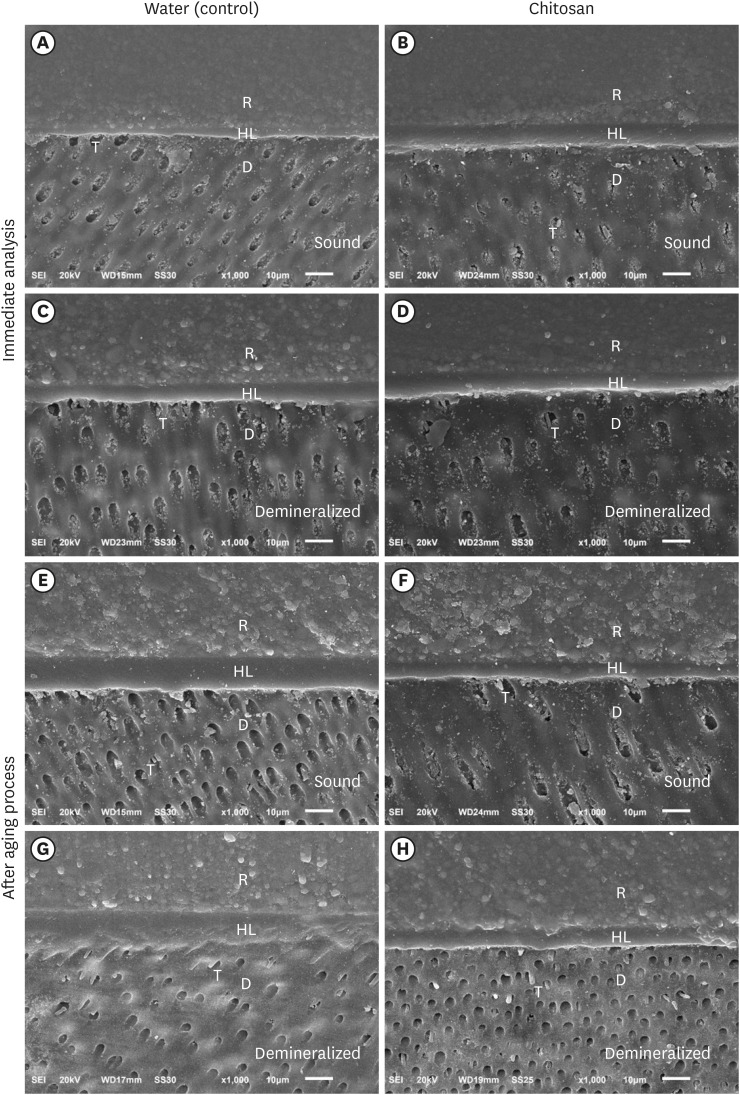
Figure 1
Figure 2
Figure 3
Material’s particulars used in this study
| Material | Composition | Manufacturer |
|---|---|---|
| Chitosan solution | Low molecular weight chitosan, acetic acid, sodium hydroxide | Sigma-Aldrich, Saint Louis, MO, USA |
| Adhesive System – Single Bond Universal | MDP phosphate monomer, dimethacrylate resins, HEMA, Vitrebond Copolymer, filler, ethanol, water, initiators, silane | 3M ESPE, St. Paul, MN, USA |
| Composite resin – Filtek Z250 | Bis-GMA, UDMA, Bis-EMA, camphorquinone, zirconia/silica | 3M ESPE, St. Paul, MN, USA |
MDP, methacryloyloxydecyl dihydrogen phosphate; HEMA, 2-hydroxyethyl methacrylate; Bis-GMA, bisphenol A-glycidyl methacrylate; UDMA, urethane dimethacrylate; Bis-EMA, bisphenol-A glycidyl dimethacrylate.
Microtensile bond strength mean values and standard deviations of dentin with water (control) and chitosan solution
| Dental substrate | Distilled water (control) | Chitosan solution | ||
|---|---|---|---|---|
| Immediate | Aged* | Immediate | Aged* | |
| Sound dentin | 27.34 ± 4.33Ab | 32.20 ± 5.85Ab | 38.47 ± 8.21Aa | 33.39 ± 9.92Aa |
| Demineralized dentin | 13.54 ± 4.28Bb | 9.74 ± 4.90Bb | 24.65 ± 9.54Ba | 13.93 ± 5.34Ba |
*Six months of water storage + 12,000 thermal cycles + enzymatic degradation.
Same capital letters denote groups that are not statistically different in the comparison within columns (
3-way analysis of variance interaction regarding the substrate, dentin treatment, and aging
| Source | Type III sum of squares | DF | Mean square | F | Sig. |
|---|---|---|---|---|---|
| Corrected model | 8,037.606a | 9 | 1,148.229 | 25.927 | 0.000 |
| Intercept | 46,884.118 | 1 | 46,884.118 | 1,058.659 | 0.000 |
| V1 – Substrate | 6,115.204 | 1 | 6,115.204 | 138.083 | 0.000 |
| V2 – Dentin treatment | 1,139.899 | 1 | 1,139.899 | 25.739 | 0.000 |
| V3 – Aging | 257.260 | 1 | 257.260 | 5.809 | 0.019 |
| V1 * V2 | 0.194 | 1 | 0.194 | 0.004 | 0.947 |
| V1 * V3 | 270.039 | 1 | 270.039 | 6.098 | 0.016 |
| V2 * V3 | 254.755 | 1 | 254.755 | 5.752 | 0.019 |
| V1 * V2 * V3 | 0.255 | 1 | 0.255 | 0.006 | 0.940 |
| Error | 3,188.614 | 72 | 44.286 | ||
| Total | 58,110.338 | 80 | |||
| Corrected total | 11,226.221 | 79 |
DF, degrees of freedom.
aR squared = 0.716 (adjusted R squared = 0.688).
Mean and standard deviations of the atomic percentage (wt%) of chemical elements in the specimens
| Chemical element | Sound dentin | Demineralized dentin | ||||||
|---|---|---|---|---|---|---|---|---|
| Distilled water (control) | Chitosan solution | Distilled water (control) | Chitosan solution | |||||
| 24 hours | 6 months | 24 hours | 6 months | 24 hours | 6 months | 24 hours | 6 months | |
| C | 37.93 ± 0.82 | 39.97 ± 2.86 | 37.97 ± 2.79 | 39.73 ± 3.47 | 38.28 ± 0.28 | 39.65 ± 0.74 | 37.00 ± 2.36 | 38.60 ± 2.00 |
| O | 33.40 ± 0.50 | 42.17 ± 2.73 | 42.98 ± 10.20 | 37.52 ± 3.04 | 42.43 ± 7.00 | 41.55 ± 4.18 | 43.21 ± 1.29 | 40.62 ± 6.68 |
| P | 4.89 ± 0.66 | 5.09 ± 0.00 | 5.73 ± 1.94 | 6.80 ± 0.30 | 5.94 ± 2.10 | 5.80 ± 1.12 | 5.98 ± 0.38 | 6.33 ± 1.41 |
| Ca | 10.87 ± 0.97 | 11.36 ± 0.12 | 12.85 ± 5.45 | 15.65 ± 0.02 | 13.07 ± 4.45 | 12.57 ± 2.51 | 13.43 ± 0.48 | 13.92 ± 3.31 |
C, carbon; O, oxygen; P, phosphorus; Ca, calcium.
MDP, methacryloyloxydecyl dihydrogen phosphate; HEMA, 2-hydroxyethyl methacrylate; Bis-GMA, bisphenol A-glycidyl methacrylate; UDMA, urethane dimethacrylate; Bis-EMA, bisphenol-A glycidyl dimethacrylate.
*Six months of water storage + 12,000 thermal cycles + enzymatic degradation.
Same capital letters denote groups that are not statistically different in the comparison within columns (
DF, degrees of freedom.
aR squared = 0.716 (adjusted R squared = 0.688).
C, carbon; O, oxygen; P, phosphorus; Ca, calcium.

 KACD
KACD
 ePub Link
ePub Link Cite
Cite

