Search
- Page Path
- HOME > Search
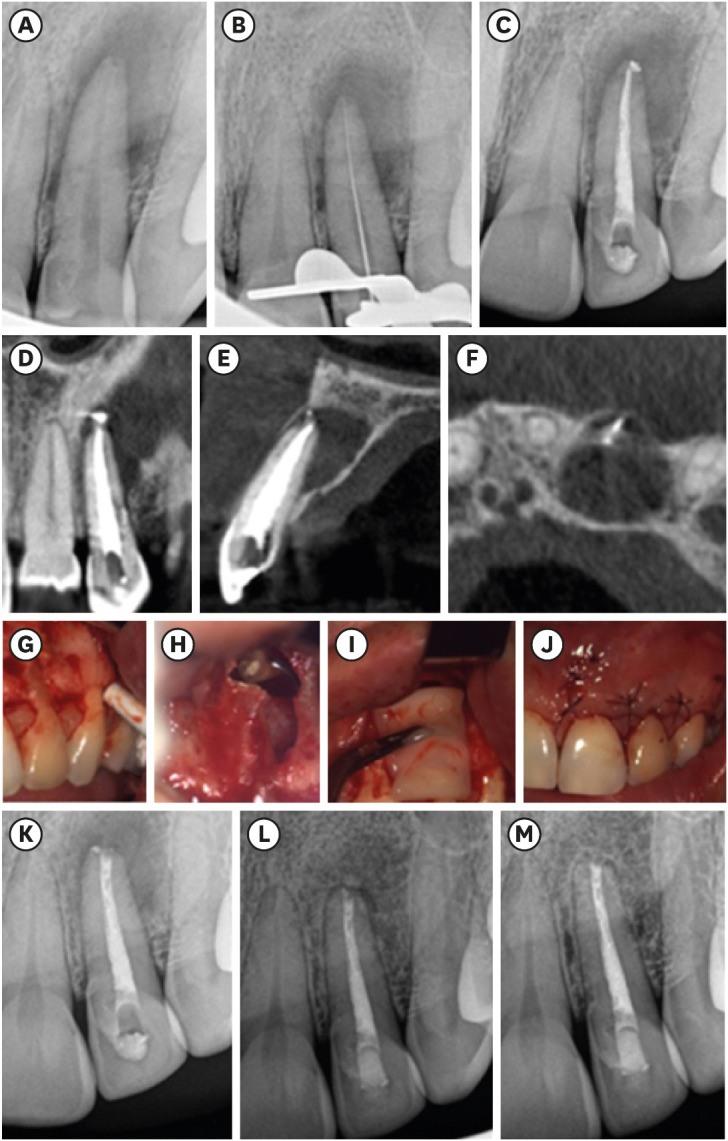
- Endodontic micro-resurgery and guided tissue regeneration of a periapical cyst associated to recurrent root perforation: a case report
- Fernando Córdova-Malca, Hernán Coaguila-Llerena, Lucía Garré-Arnillas, Jorge Rayo-Iparraguirre, Gisele Faria
- Restor Dent Endod 2022;47(4):e35. Published online September 3, 2022
- DOI: https://doi.org/10.5395/rde.2022.47.e35
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Although the success rates of microsurgery and micro-resurgery are very high, the influence of a recurrent perforation combined with radicular cyst remains unclear. A 21-year-old white female patient had a history of root perforation in a previously treated right maxillary lateral incisor. Analysis using cone-beam computed tomography (CBCT) revealed an extensive and well-defined periapical radiolucency, involving the buccal and palatal bone plate. The perforation was sealed with bioceramic material (Biodentine) in the pre-surgical phase. In the surgical phase, guided tissue regeneration (GTR) was performed by combining xenograft (lyophilized bovine bone) and autologous platelet-rich fibrin applied to the bone defect. The root-end preparation was done using an ultrasonic tip. The retrograde filling was performed using a bioceramic material (Biodentine). Histopathological analysis confirmed a radicular cyst. The patient returned to her referring practitioner to continue the restorative procedures. CBCT analysis after 1-year recall revealed another perforation in the same place as the first intervention, ultimately treated by micro-resurgery using the same protocol with GTR, and a bioceramic material (MTA Angelus). The 2-year recall showed healing and bone neoformation. In conclusion, endodontic micro-resurgery with GTR showed long-term favorable results when a radicular cyst and a recurrent perforation compromised the success.
- 22 View
- 1 Download
- 1 Web of Science

- Leukocyte platelet-rich fibrin in endodontic microsurgery: a report of 2 cases
- Mariana Domingos Pires, Jorge N. R. Martins, Abayomi Omokeji Baruwa, Beatriz Pereira, António Ginjeira
- Restor Dent Endod 2022;47(2):e17. Published online March 4, 2022
- DOI: https://doi.org/10.5395/rde.2022.47.e17
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Endodontic microsurgery is a predictable treatment option when orthograde treatment or retreatment is unsuccessful or unfeasible. However, when there is a gross compromise of periapical bone, achievement of bone regeneration after the surgical procedure may be hampered. In such cases, the application of guided tissue regeneration principles, with adjunctive use of leukocyte platelet-rich fibrin to fill the bone defect as a bone substitute and as a membrane to cover the site, provides a cost-effective solution with the benefits of accelerated physiological healing and reduced post-surgical pain and discomfort. This case report presents 2 cases of endodontic microsurgery of the upper lateral incisors with loss of buccal cortical plate, where platelet-rich fibrin was successfully applied.
- 22 View
- 1 Download
- 1 Web of Science

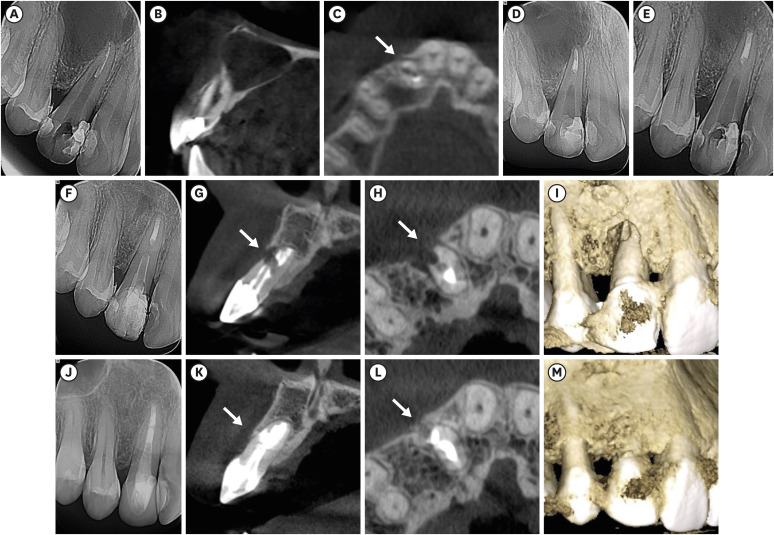
- Management of apicomarginal defect in esthetic region associated with a tooth with anomalies
- Vinayak Venkoosa Meharwade, Dipali Yogesh Shah, Pradyna Prabhakar Mali, Vidya Vinayak Meharwade
- Restor Dent Endod 2015;40(4):314-321. Published online June 24, 2015
- DOI: https://doi.org/10.5395/rde.2015.40.4.314
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Tooth related factors such as palatoradicular groove can be one of the causes for localized periodontal destruction. Such pathological process may result in apicomarginal defect along with inflammation of pulp. This creates challenging situation which clinician must be capable of performing advanced periodontal regenerative procedures for the successful management. This case report discusses clinical management of apicomarginal defect associated with extensive periradicular destruction in a maxillary lateral incisor, along with histopathologic aspect of the lesion.
- 20 View
- 0 Download

- Pulp tissue regeneration and root formation of permanent teeth with pulpal/periapical deseases
- Yeon-Jee Yoo, Seung-Ho Baek, Ho-Hyun Son
- J Korean Acad Conserv Dent 2010;35(4):238-245. Published online July 31, 2010
- DOI: https://doi.org/10.5395/JKACD.2010.35.4.238
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Numerous cases about additional growth of roots or pulp tissue regeneration by using various intracanal medicaments in immature permanent teeth with periapical or pulpal disease have been reported. The underlying mechanism has not been clearly delineated, but it has been widely accepted that undifferentiated mesenchymal cells and stem cells are involved. Moreover, the growth and deposition of osteoid or cementoid tissues have been observed in regenerated pulp and roots. This new and non-invasive treatment has brightened the future of endodontics, and enlarged the vision of regenerative root canal treatment with multi-potent stem cells and various tissue engineering techniques.
- 23 View
- 0 Download

- Tissue engineering of dental pulp on type I collagen
- Gwang-Hee Lee, Sung-Yoon Huh, Sang-Hyuk Park
- J Korean Acad Conserv Dent 2004;29(4):370-377. Published online July 31, 2004
- DOI: https://doi.org/10.5395/JKACD.2004.29.4.370
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub The purpose of this study was to regenerate human dental pulp tissues similar to native pulp tissues. Using the mixture of type I collagen solution, primary cells collected from the different tissues (pulp, gingiva, and skin) and NIH 3T3 (1 × 105 cells/ml/well) were cultured at 12-well plate at 37℃ for 14 days. Standardized photographs were taken with digital camera during 14 days and the diameter of the contracted collagen gel matrix was measured and statistically analyzed with student t-test. As one of the pulp tissue engineering, normal human dental pulp tissue and collagen gel matrix cultured with dental pulp cells for 14 days were fixed and stained with Hematoxyline & Eosin.
According to this study, the results were as follows:
1. The contraction of collagen gel matrix cultured with pulp cells for 14 days was significantly higher than other fibroblasts (gingiva, skin) (p < 0.05).
2. The diameter of collagen gel matrix cultured with pulp cells was reduced to 70.4% after 7 days, and 57.1% after 14 days.
3. The collagen gel without any cells did not contract, whereas the collagen gel cultured with gingiva and skin showed mild contraction after 14 days (88.1% and 87.6% respectively).
4. The contraction of the collagen gel cultured with NIH 3T3 cells after 14 days was higher than those cultured with gingival and skin fibroblasts, but it was not statistically significant (72.1%, p > 0.05).
5. The collagen gel matrix cultured with pulp cells for 14 days showed similar shape with native pulp tissue without blood vessels.
This approach may provide a means of engineering a variety of other oral tissue as well and these cell behaviors may provide information needed to establish pulp tissue engineering protocols.
- 24 View
- 0 Download


 KACD
KACD
 First
First Prev
Prev


