Search
- Page Path
- HOME > Search
- Effects of CTHRC1 on odontogenic differentiation and angiogenesis in human dental pulp stem cells
- Jong-soon Kim, Bin-Na Lee, Hoon-Sang Chang, In-Nam Hwang, Won-Mann Oh, Yun-Chan Hwang
- Restor Dent Endod 2023;48(2):e18. Published online April 28, 2023
- DOI: https://doi.org/10.5395/rde.2023.48.e18
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives This study aimed to determine whether collagen triple helix repeat containing-1 (CTHRC1), which is involved in vascular remodeling and bone formation, can stimulate odontogenic differentiation and angiogenesis when administered to human dental pulp stem cells (hDPSCs).
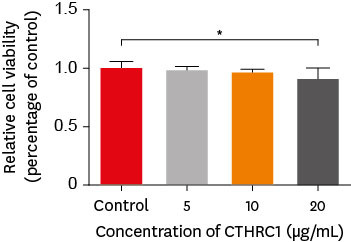
Materials and Methods The viability of hDPSCs upon exposure to CTHRC1 was assessed with the WST-1 assay. CTHRC1 doses of 5, 10, and 20 µg/mL were administered to hDPSCs. Reverse-transcription polymerase reaction was used to detect dentin sialophosphoprotein, dentin matrix protein 1, vascular endothelial growth factor, and fibroblast growth factor 2. The formation of mineralization nodules was evaluated using Alizarin red. A scratch wound assay was conducted to evaluate the effect of CTHRC1 on cell migration. Data were analyzed using 1-way analysis of variance followed by the Tukey
post hoc test. The threshold for statistical significance was set atp < 0.05.Results CTHRC1 doses of 5, 10, and 20 µg/mL had no significant effect on the viability of hDPSCs. Mineralized nodules were formed and odontogenic markers were upregulated, indicating that CTHRC1 promoted odontogenic differentiation. Scratch wound assays demonstrated that CTHRC1 significantly enhanced the migration of hDPSCs.
Conclusions CTHRC1 promoted odontogenic differentiation and mineralization in hDPSCs.
- 1,593 View
- 34 Download

- Diagnostic challenges of nonodontogenic toothache
- Hyung-Ok Park, Jung-Hong Ha, Myoung-Uk Jin, Young-Kyung Kim, Sung-Kyo Kim
- Restor Dent Endod 2012;37(3):170-174. Published online August 29, 2012
- DOI: https://doi.org/10.5395/rde.2012.37.3.170
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub The objective of this article was to present two nonodontogenic conditions that may mimic odontogenic toothache: trigeminal neuralgia and burning mouth syndrome. Two cases are presented in which one is related to the upper left second premolar and the other is related to the upper left first molar. Both showed pain when chewing. These two cases highlight the complexities involved in diagnosing nonodontogenic toothache. This article demonstrates the importance of having a thorough knowledge of both odontogenic and nonodontogenic toothache, as well as the need for careful evaluation of the nature of the pain and history, clinical and radiographic examinations.
-
Citations
Citations to this article as recorded by- Analysis of Final Diagnosis of Patients with Suspected Nonodontogenic Toothache: A Retrospective Study
Jeong Yeop Chun, Young Joo Shim
Journal of Oral Medicine and Pain.2024; 49(3): 57. CrossRef - Interactions of Acetyl-11-Keto-Beta-Boswellic Acid on Catechol-O-Methyltransferase in the Management of Masticatory Myofascial Pain Syndrome
Ramya Suresh, Pradeep Kumar Yadalam, Ramya Ramadoss, Karthikeyan Ramalingam, Arvind Muthukrishnan
Cureus.2024;[Epub] CrossRef - Assessment of Concordance between Chairside Ultrasonography and Digital Palpation in Detecting Myofascial Trigger Points in Masticatory Myofascial Pain Syndrome
Mohamed Elbarbary, Michael Goldberg, Howard C. Tenenbaum, David K. Lam, Bruce V. Freeman, David J. Pustaka, David Mock, Joseph Beyene, Amir Azarpazhooh
Journal of Endodontics.2023; 49(2): 129. CrossRef - Masticatory Myofascial Pain Syndrome: Implications for Endodontists
Mohamed Elbarbary, Ariel Oren, Michael Goldberg, Bruce V. Freeman, David Mock, Howard C. Tenenbaum, Amir Azarpazhooh
Journal of Endodontics.2022; 48(1): 55. CrossRef - PRICE 2020 guidelines for reporting case reports in Endodontics: explanation and elaboration
V. Nagendrababu, B. S. Chong, P. McCabe, P. K. Shah, E. Priya, J. Jayaraman, S. J. Pulikkotil, P. M. H. Dummer
International Endodontic Journal.2020; 53(7): 922. CrossRef - Clinical Outline of Oral Diseases
Arvind Babu Rajendra Santosh, Doryck Boyd, Kumaraswamy Kikeri Laxminarayana
Dental Clinics of North America.2020; 64(1): 1. CrossRef - Nonodontogenic Sources of Dental Pain
Scott E. Schames, Michael Jordan, Hila Robbins, Lenard Katz, Kaitlyn Tarbert
Journal of the California Dental Association.2016; 44(8): 507. CrossRef - Nonodontogenic toothaches
Edward F. Wright
The Journal of the American Dental Association.2015; 146(6): 406. CrossRef - Síndrome de boca ardiente: claves diagnósticas y terapéuticas
Eduardo Chimenos-Küstner, Cristina Arcos-Guerra, Maria Sueli Marques-Soares
Medicina Clínica.2014; 142(8): 370. CrossRef
- Analysis of Final Diagnosis of Patients with Suspected Nonodontogenic Toothache: A Retrospective Study
- 2,047 View
- 27 Download
- 9 Crossref

- Clinical diagnosis of herpes zoster presenting as odontogenic pain
- Seong-Hak Yang, Dong-Ho Jung, Hae-Doo Lee, Yoon Lee, Hoon-Sang Chang, Kyung-San Min
- J Korean Acad Conserv Dent 2008;33(5):452-456. Published online September 30, 2008
- DOI: https://doi.org/10.5395/JKACD.2008.33.5.452
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Herpes zoster, an acute viral infection produced by the varicella zoster virus, may affect any of the trigeminal branches. This case report presents a patient with symptoms mimicking odontogenic pain. No obvious cause of the symptoms could be found based on clinical and radiographic examinations. After a dermatologist made a diagnosis of herpes zoster involving the third trigeminal branch, the patient was given antiviral therapy. Two months later, the facial lesions and pain had almost disappeared, and residual pigmented scars were present. During the diagnostic process, clinicians should keep in mind the possibility that orofacial pain might be related to herpes zoster.
-
Citations
Citations to this article as recorded by- Herpes Zoster Accompanying Odontogenic Inflammation: A Case Report with Literature Review
Soyeon Lee, Minsik Kim, Jong-Ki Huh, Jae-Young Kim
Journal of Oral Medicine and Pain.2021; 46(1): 9. CrossRef - Recurrent Herpetic Stomatitis Mimicking Post-Root Resection Complication
Sung-Ok Hong, Jae-Kwan Lee, Hoon-Sang Chang
Journal of Dental Rehabilitation and Applied Science.2013; 29(4): 418. CrossRef - Diagnostic challenges of nonodontogenic toothache
Hyung-Ok Park, Jung-Hong Ha, Myoung-Uk Jin, Young-Kyung Kim, Sung-Kyo Kim
Restorative Dentistry & Endodontics.2012; 37(3): 170. CrossRef
- Herpes Zoster Accompanying Odontogenic Inflammation: A Case Report with Literature Review
- 2,739 View
- 12 Download
- 3 Crossref


 KACD
KACD

 First
First Prev
Prev


