Search
- Page Path
- HOME > Search
- An unusual case of dens invaginatus on a mandibular second molar: a case report
- Davide Mancino, Dina Abdellatif, Alfredo Iandolo, Fabien Bornert, Youssef Haïkel
- Restor Dent Endod 2025;50(1):e2. Published online January 8, 2025
- DOI: https://doi.org/10.5395/rde.2025.50.e2

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
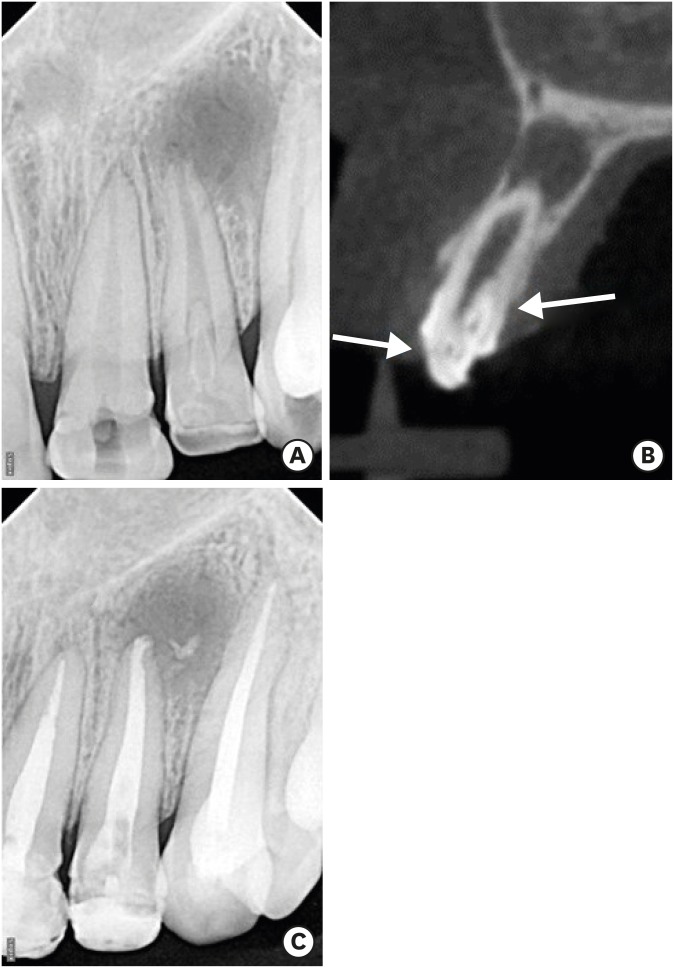
ePub - The present case report describes the endodontic treatment of a type III B dens invaginatus (DI) in a three-rooted mandibular second molar since the invagination invades the root and extends apically. Clinical and cone-beam computed tomography examination of the mandibular second molar showed a broadened coronal morphology, DI, a third root, periapical radiolucency, and compression of a distal root canal by the invagination, which developed an atypical semilunar shape. The tooth was diagnosed with pulpal necrosis, symptomatic apical, and peri-invagination periodontitis. Consequently, three-dimensional virtual reconstruction was conducted to improve anatomical interpretation and case planning and accelerate the intraoperative phase by reducing operator stress and minimizing intraoperative variables. The present case report aims to raise awareness of the existence of DI on the mandibular second molar.
-
Citations
Citations to this article as recorded by- Dens Invaginatus—Mandibular Second Molar—Case Report
Krystyna Pietrzycka, Natalia Lutomska, Cornelis H. Pameijer, Monika Lukomska-Szymanska
Dentistry Journal.2026; 14(1): 27. CrossRef - Type IIIb dens invaginatus in a maxillary second molar and its microscopic anatomical features: a case report
Mingming Li, Zhiwu Wu, Shaoying Duan, Yuling Zuo
BMC Oral Health.2025;[Epub] CrossRef
- Dens Invaginatus—Mandibular Second Molar—Case Report
- 2,941 View
- 213 Download
- 2 Crossref

- Successful nonsurgical treatment of type II dens invaginatus with 5 root canals using a self-adjusting file: a case report
- George Táccio de Miranda Candeiro, Antônio Sérgio Teixeira de Menezes, Ana Carolina Saldanha de Oliveira, Flávio Rodrigues Ferreira Alves
- Restor Dent Endod 2023;48(2):e17. Published online April 27, 2023
- DOI: https://doi.org/10.5395/rde.2023.48.e17

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub The present report describes the endodontic treatment of an Oehlers type II dens invaginatus in a maxillary lateral incisor with 5 root canals, an extremely rare condition. Apical periodontitis and related symptoms were noted. Cone-beam computed tomography was used to aid the diagnosis, reveal tooth morphology, and assist in canal location. The pulp chamber was carefully accessed, and the root canals were explored under magnification. All root canals were prepared with an R25 Reciproc Blue system and sodium hypochlorite (NaOCl) irrigation. After initial preparation, a self-adjusting file (SAF) with NaOCl and ethylenediaminetetraacetic acid was used to complement the disinfection. Additionally, calcium hydroxide medication was applied. Vertical compaction was used to fill the canals with a calcium silicate-based endodontic sealer and gutta-percha. After 12 months, the patient exhibited healing of the periapical region, absence of symptoms, and normal dental function. In conclusion, this nonsurgical treatment protocol was successful in promoting the cure of apical periodontitis. Both complementary disinfection with an SAF and use of calcium hydroxide medication should be considered when choosing the best treatment approach for dens invaginatus with very complex anatomy.
-
Citations
Citations to this article as recorded by- Non-surgical endodontic management of dens invaginatus type II in an immature maxillary lateral incisor using a bioceramic apical plug: A 3-year follow-up case report
Yahya Raja Alharbi, Qayed Saad Alharbi, Shaul Hameed Kolarkodi
Saudi Endodontic Journal.2026; 16(1): 115. CrossRef
- Non-surgical endodontic management of dens invaginatus type II in an immature maxillary lateral incisor using a bioceramic apical plug: A 3-year follow-up case report
- 1,872 View
- 67 Download
- 1 Crossref

- A case report of multiple bilateral dens invaginatus in maxillary anteriors
- Shin Hye Chung, You-Jeong Hwang, Sung-Yeop You, Young-Hye Hwang, Soram Oh
- Restor Dent Endod 2019;44(4):e39. Published online October 21, 2019
- DOI: https://doi.org/10.5395/rde.2019.44.e39

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub The present report presents a case of dens invaginatus (DI) in a patient with 4 maxillary incisors. A 24-year-old female complained of swelling of the maxillary left anterior region and discoloration of the maxillary left anterior tooth. The maxillary left lateral incisor (tooth #22) showed pulp necrosis and a chronic apical abscess, and a periapical X-ray demonstrated DI on bilateral maxillary central and lateral incisors. All teeth responded to a vitality test, except tooth #22. The anatomic form of tooth #22 was similar to that of tooth #12, and both teeth had lingual pits. In addition, panoramic and periapical X-rays demonstrated root canal calcification, such as pulp stones, in the maxillary canines, first and second premolars, and the mandibular incisors, canines, and first premolars bilaterally. The patient underwent root canal treatment of tooth #22 and non-vital tooth bleaching. After a temporary filling material was removed, the invaginated mass was removed using ultrasonic tips under an operating microscope. The working length was established, and the root canal was enlarged up to #50 apical size and obturated with gutta-percha and AH 26 sealer using the continuous wave of condensation technique. Finally, non-vital bleaching was performed, and the access cavity was filled with composite resin.
-
Citations
Citations to this article as recorded by- The use of three-dimensional-printed guides, static navigation, and bioactive materials to treat bilateral and double dens invaginatus
Parth Patel, Nidhi Bharti, Ankit Arora, C. Nimisha Shah
Saudi Endodontic Journal.2025; 15(2): 207. CrossRef - Endodontic Management of Dens in Dente – A Systematic Review of Case Reports and Case Series
Sanket Dilip Aras, Anamika Chetan Borkar, Sonal Kale, Sayali Maral, Prakriti Jaggi, Shailendra Sonawane
Journal of the International Clinical Dental Research Organization.2024; 16(1): 17. CrossRef - Dens invaginatus of fourteen teeth in a pediatric patient
Momoko Usuda, Tatsuya Akitomo, Mariko Kametani, Satoru Kusaka, Chieko Mitsuhata, Ryota Nomura
Pediatric Dental Journal.2023; 33(3): 240. CrossRef - The Impact of the Preferred Reporting Items for Case Reports in Endodontics (PRICE) 2020 Guidelines on the Reporting of Endodontic Case Reports
Sofian Youssef, Phillip Tomson, Amir Reza Akbari, Natalie Archer, Fayjel Shah, Jasmeet Heran, Sunmeet Kandhari, Sandeep Pai, Shivakar Mehrotra, Joanna M Batt
Cureus.2023;[Epub] CrossRef - Root Maturation of an Immature Dens Invaginatus Despite Unsuccessful Revitalization Procedure: A Case Report and Recommendations for Educational Purposes
Julia Ludwig, Marcel Reymus, Alexander Winkler, Sebastian Soliman, Ralf Krug, Gabriel Krastl
Dentistry Journal.2023; 11(2): 47. CrossRef - Conservative Management of Infraorbital Space Infection Secondary to Type III B Dens Invaginatus: A Case Report
Ashima Goyal, Aditi Kapur, Manoj A Jaiswal, Gauba Krishan, Raja Raghu, Sanjeev K Singh
Journal of Postgraduate Medicine, Education and Research.2022; 56(4): 192. CrossRef
- The use of three-dimensional-printed guides, static navigation, and bioactive materials to treat bilateral and double dens invaginatus
- 2,417 View
- 28 Download
- 6 Crossref

- Guided endodontics: a case report of maxillary lateral incisors with multiple dens invaginatus
- Afzal Ali, Hakan Arslan
- Restor Dent Endod 2019;44(4):e38. Published online October 21, 2019
- DOI: https://doi.org/10.5395/rde.2019.44.e38
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Navigation of the main root canal and dealing with a dens invaginatus (DI) is a challenging task in clinical practice. Recently, the guided endodontics technique has become an alternative method for accessing root canals, surgical cavities, and calcified root canals without causing iatrogenic damage to tissue. In this case report, the use of the guided endodontics technique for two maxillary lateral incisors with multiple DIs is described. A 16-year-old female patient was referred with the chief complaint of pain and discoloured upper front teeth. Based on clinical and radiographic findings, a diagnosis of pulp necrosis and chronic periapical abscess associated with double DI (Oehler's type II) was established for the upper left lateral maxillary incisor (tooth #22). Root canal treatment and the sealing of double DI with mineral trioxide aggregate was planned for tooth #22. For tooth #12 (Oehler's type II), preventive sealing of the DI was planned. Minimally invasive access to the double DI and the main root canal of tooth #22, and to the DI of tooth #12, was achieved using the guided endodontics technique. This technique can be a valuable tool because it reduces chair-time and, more importantly, the risk of iatrogenic damage to the tooth structure.
-
Citations
Citations to this article as recorded by- Guided endodontics in the application of personalized mini-invasive treatment in clinical cases: a literature review
Shuangshuang Ren, Wanping Wang, Mingyue Cheng, Wenyue Tang, Yue Zhao, Leiying Miao
The Saudi Dental Journal.2025;[Epub] CrossRef - Navigating Calcified Challenges: Guided Endodontic Treatment of a Maxillary Central Incisor
Saide Nabavi, Sara Navabi, Iman Shiezadeh, SeyedehZahra JamaliMotlagh
Clinical Case Reports.2025;[Epub] CrossRef - Successful nonsurgical management of Oehler’s type III dens invaginatus in maxillary lateral incisor: A case report as per CARE guidelines
Anshul Sachdeva, Gurdeep Singh Gill, Adel Al Obied, Suraj Arora, Ali Y. Alsaeed, Waled Abdulmalek Alanesi, Gotam Das
Medicine.2025; 104(31): e42725. CrossRef - Guided Endodontics in Managing Root Canal Treatment for Anomalous Teeth—A Narrative Review
Pouya Sabanik, Mohammad Samiei, Shiva Tavakkoli Avval, Bruno Cavalcanti
Australian Endodontic Journal.2025;[Epub] CrossRef - Efficacy of Computer-aided Static Navigation on Accuracy of Guided Endodontic Root Canal Treatment: A Systematic Review and Meta-analysis
Ashish Jain, Rahul D Rao, Meenakshi R Verma, Rishabhkumar N Jain, Shreya Sivasailam, Anandita Sinha
World Journal of Dentistry.2024; 14(11): 1004. CrossRef - Application of personalized templates in minimally invasive management of coronal dens invaginatus: a report of two cases
Mingming Li, Guosong Wang, Fangzhi Zhu, Han Jiang, Yingming Yang, Ran Cheng, Tao Hu, Ru Zhang
BMC Oral Health.2024;[Epub] CrossRef - Endodontic management of severely calcified mandibular anterior teeth using guided endodontics: A report of a case and a review of the literature
Mina Davaji, Sahar Karimpour
Saudi Endodontic Journal.2024; 14(2): 245. CrossRef - Application of an Endodontic Static Guide in Fiber Post Removal from a Compromised Tooth
Mehran Farajollahi, Omid Dianat, Samaneh Gholami, Shima Saber Tahan, Sivakumar Nuvvula
Case Reports in Dentistry.2023;[Epub] CrossRef - The Impact of the Preferred Reporting Items for Case Reports in Endodontics (PRICE) 2020 Guidelines on the Reporting of Endodontic Case Reports
Sofian Youssef, Phillip Tomson, Amir Reza Akbari, Natalie Archer, Fayjel Shah, Jasmeet Heran, Sunmeet Kandhari, Sandeep Pai, Shivakar Mehrotra, Joanna M Batt
Cureus.2023;[Epub] CrossRef - Effectiveness of guided endodontics in locating calcified root canals: a systematic review
F. Peña-Bengoa, M. Valenzuela, M. J. Flores, N. Dufey, K. P. Pinto, E. J. N. L. Silva
Clinical Oral Investigations.2023; 27(5): 2359. CrossRef - Expert consensus on digital guided therapy for endodontic diseases
Xi Wei, Yu Du, Xuedong Zhou, Lin Yue, Qing Yu, Benxiang Hou, Zhi Chen, Jingping Liang, Wenxia Chen, Lihong Qiu, Xiangya Huang, Liuyan Meng, Dingming Huang, Xiaoyan Wang, Yu Tian, Zisheng Tang, Qi Zhang, Leiying Miao, Jin Zhao, Deqin Yang, Jian Yang, Junqi
International Journal of Oral Science.2023;[Epub] CrossRef - Prevalence and morphological analysis of dens invaginatus in anterior teeth using cone beam computed tomography: A systematic review and meta-analysis
Guilherme Nilson Alves dos Santos, Manoel Damião Sousa-Neto, Helena Cristina Assis, Fabiane Carneiro Lopes-Olhê, André L. Faria-e-Silva, Matheus L. Oliveira, Jardel Francisco Mazzi-Chaves, Amanda Pelegrin Candemil
Archives of Oral Biology.2023; 151: 105715. CrossRef - Root Maturation of an Immature Dens Invaginatus Despite Unsuccessful Revitalization Procedure: A Case Report and Recommendations for Educational Purposes
Julia Ludwig, Marcel Reymus, Alexander Winkler, Sebastian Soliman, Ralf Krug, Gabriel Krastl
Dentistry Journal.2023; 11(2): 47. CrossRef - Guided Endodontics as a Personalized Tool for Complicated Clinical Cases
Wojciech Dąbrowski, Wiesława Puchalska, Adam Ziemlewski, Iwona Ordyniec-Kwaśnica
International Journal of Environmental Research and Public Health.2022; 19(16): 9958. CrossRef - Present status and future directions – Guided endodontics
Thomas Connert, Roland Weiger, Gabriel Krastl
International Endodontic Journal.2022; 55(S4): 995. CrossRef - Treatment options for dens in dente: state-of-art literature review
Volodymyr Fedak
Ukrainian Dental Journal.2022; 1(1): 37. CrossRef - Dens Invaginatus: Clinical Implications and Antimicrobial Endodontic Treatment Considerations
José F. Siqueira, Isabela N. Rôças, Sandra R. Hernández, Karen Brisson-Suárez, Alessandra C. Baasch, Alejandro R. Pérez, Flávio R.F. Alves
Journal of Endodontics.2022; 48(2): 161. CrossRef - Guided Endodontics: Static vs. Dynamic Computer-Aided Techniques—A Literature Review
Diana Ribeiro, Eva Reis, Joana A. Marques, Rui I. Falacho, Paulo J. Palma
Journal of Personalized Medicine.2022; 12(9): 1516. CrossRef - Application of CBCT Data and Three-Dimensional Printing for Endodontic Diagnosis and Treatment
Srinidhi Vishnu Ballulaya, Neha Taufin, Nenavath Deepthi, Venu Babu Devella
Nigerian Journal of Experimental and Clinical Biosciences.2021; 9(3): 206. CrossRef - When to consider the use of CBCT in endodontic treatment planning in adults
Nisha Patel, Andrew Gemmell, David Edwards
Dental Update.2021; 48(11): 932. CrossRef
- Guided endodontics in the application of personalized mini-invasive treatment in clinical cases: a literature review
- 2,816 View
- 93 Download
- 20 Crossref

- Endodontic management of a maxillary lateral incisor with dens invaginatus and external root irregularity using cone-beam computed tomography
- Young-Jun Lim, Sook-Hyun Nam, Sung-Ho Jung, Dong-Ryul Shin, Su-Jung Shin, Kyung-San Min
- Restor Dent Endod 2012;37(1):50-53. Published online March 2, 2012
- DOI: https://doi.org/10.5395/rde.2012.37.1.50
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Cone-beam computed tomography (CBCT) is a useful diagnostic tool for identification of both internal and external root configurations. This case report describes the endodontic management of a lateral incisor with both dens invaginatus and external root irregularity by using CBCT. Nonsurgical endodontic retreatment was performed on the lateral incisor with dens invaginatus. A perforation through the dens invaginatus and external concavity was repaired using mineral trioxide aggregate. After 18 mon of follow-up, there were no clinical symptoms. Recall radiographs appeared normal and showed healing of the periapical pathosis. The understanding of both internal root canal configuration and external root irregularity using CBCT can ensure predictable and successful results.
-
Citations
Citations to this article as recorded by- Cone-beam computed tomography for assessment of dens invaginatus in the Polish population
T. Katarzyna Różyło, Ingrid Różyło-Kalinowska, Magdalena Piskórz
Oral Radiology.2018; 34(2): 136. CrossRef - Nonsurgical Endodontic Management of a Molar-Incisor Malformation-affected Mandibular First Molar: A Case Report
Wonyoung Yue, Euiseong Kim
Journal of Endodontics.2016; 42(4): 664. CrossRef - Three-year follow-up: Healing of a large periapical lesion related to a maxillary central incisor and two canalled lateral incisor after a single visit root canal treatment
Abu Mostafa Ammar
Journal of Dentistry and Oral Hygiene.2015; 7(4): 40. CrossRef - Dilemmas pertaining to three canals in the mesiobuccal root of a maxillary second molar: a case report
Ankit Arora, Shashi Rashmi Acharya, Muliya Vidya Saraswathi, Padmaja Sharma, Amber Ather
Restorative Dentistry & Endodontics.2013; 38(3): 172. CrossRef - Management of root canal perforation by using cone-beam computed tomography
Kyung-San Min
Restorative Dentistry & Endodontics.2013; 38(1): 55. CrossRef - Endodontic treatment of maxillary lateral incisors with anatomical variations
Moon-Hwan Lee, Jung-Hong Ha, Myoung-Uk Jin, Young-Kyung Kim, Sung-Kyo Kim
Restorative Dentistry & Endodontics.2013; 38(4): 253. CrossRef
- Cone-beam computed tomography for assessment of dens invaginatus in the Polish population
- 1,385 View
- 10 Download
- 6 Crossref


 KACD
KACD

 First
First Prev
Prev


