Search
- Page Path
- HOME > Search
- Push-out bond strength and intratubular biomineralization of a hydraulic root-end filling material premixed with dimethyl sulfoxide as a vehicle
- Ju-Ha Park, Hee-Jin Kim, Kwang-Won Lee, Mi-Kyung Yu, Kyung-San Min
- Restor Dent Endod 2023;48(1):e8. Published online January 20, 2023
- DOI: https://doi.org/10.5395/rde.2023.48.e8
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
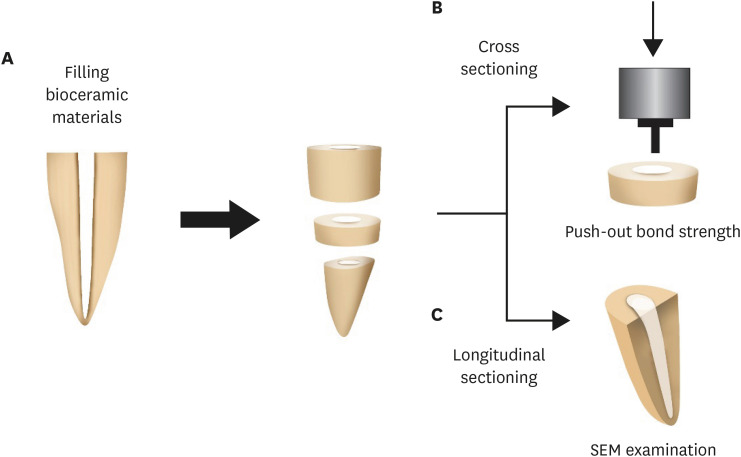
ePub Objectives This study was designed to evaluate the parameters of bonding performance to root dentin, including push-out bond strength and dentinal tubular biomineralization, of a hydraulic bioceramic root-end filling material premixed with dimethyl sulfoxide (Endocem MTA Premixed) in comparison to a conventional powder-liquid–type cement (ProRoot MTA).
Materials and Methods The root canal of a single-rooted premolar was filled with either ProRoot MTA or Endocem MTA Premixed (
n = 15). A slice of dentin was obtained from each root. Using the sliced specimen, the push-out bond strength was measured, and the failure pattern was observed under a stereomicroscope. The apical segment was divided into halves; the split surface was observed under a scanning electron microscope, and intratubular biomineralization was examined by observing the precipitates formed in the dentinal tubule. Then, the chemical characteristics of the precipitates were evaluated with energy-dispersive X-ray spectroscopic (EDS) analysis. The data were analyzed using the Student’st -test followed by the Mann-WhitneyU test (p < 0.05).Results No significant difference was found between the 2 tested groups in push-out bond strength, and cohesive failure was the predominant failure type. In both groups, flake-shaped precipitates were observed along dentinal tubules. The EDS analysis indicated that the mass percentage of calcium and phosphorus in the precipitate was similar to that found in hydroxyapatite.
Conclusions Regarding bonding to root dentin, Endocem MTA Premixed may have potential for use as an acceptable root-end filling material.
-
Citations
Citations to this article as recorded by- Comparison of intratubular biomineralization between in vivo and in vitro conditions
Sieun Nam, Yeon-Jee Yoo, Mi-Kyung Yu, Kyung-San Min
Journal of Oral Science.2026; 68(1): 30. CrossRef - Effectiveness of Sectioning Method and Filling Materials on Roughness and Cell Attachments in Root Resection Procedure
Tarek Ashi, Naji Kharouf, Olivier Etienne, Bérangère Cournault, Pierre Klienkoff, Varvara Gribova, Youssef Haikel
European Journal of Dentistry.2025; 19(01): 240. CrossRef - Bond Strength and Adhesive Interface Quality of New Pre‐Mixed Bioceramic Root Canal Sealer
Gustavo Creazzo, Bruna Monteiro de Barros Ciribelli Alves, Helena Cristina de Assis, Karen Gisselle Garay Villamayor, Manoel Damião de Sousa‐Neto, Jardel Francisco Mazzi‐Chaves, Fabiane Carneiro Lopes‐Olhê
Microscopy Research and Technique.2025; 88(7): 1989. CrossRef - Evaluation of clinical and radiographic outcome of premixed injectable mineral trioxide aggregate and conventional mineral trioxide aggregate as pulpotomy medicaments in primary molars – A split-mouth randomized control trial
U. S. Aiswarya, Sharan S. Sargod, Sundeep K. Hegde, H. T. Ajay Rao, Nanditha Hegde
Journal of Indian Society of Pedodontics and Preventive Dentistry.2025; 43(4): 559. CrossRef - Evaluation of the root dentin bond strength and intratubular biomineralization of a premixed calcium aluminate-based hydraulic bioceramic endodontic sealer
Yu-Na Lee, Min-Kyeong Kim, Hee-Jin Kim, Mi-Kyung Yu, Kwang-Won Lee, Kyung-San Min
Journal of Oral Science.2024; 66(2): 96. CrossRef - Removal efficiency of a fast setting pozzalan-based bioactive cement: a micro CT study
Feyza Çetinkaya, Ahter Şanal Çıkman, Ali Keleş, Banu Arıcıoğlu
BMC Oral Health.2024;[Epub] CrossRef - Antibacterial Activity and Sustained Effectiveness of Calcium Silicate-Based Cement as a Root-End Filling Material against Enterococcus faecalis
Seong-Hee Moon, Seong-Jin Shin, Seunghan Oh, Ji-Myung Bae
Materials.2023; 16(18): 6124. CrossRef
- Comparison of intratubular biomineralization between in vivo and in vitro conditions
- 3,371 View
- 94 Download
- 6 Web of Science
- 7 Crossref

- Biomineralization of three calcium silicate-based cements after implantation in rat subcutaneous tissue
- Ranjdar Mahmood Talabani, Balkees Taha Garib, Reza Masaeli, Kavosh Zandsalimi, Farinaz Ketabat
- Restor Dent Endod 2021;46(1):e1. Published online December 2, 2020
- DOI: https://doi.org/10.5395/rde.2021.46.e1
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
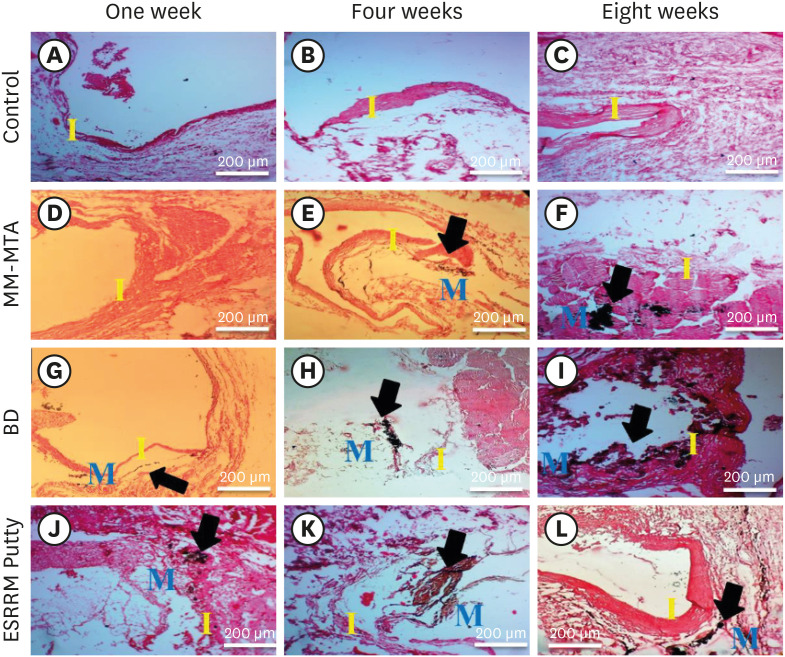
ePub Objectives The aim of this study was to evaluate the dystrophic mineralization deposits from 3 calcium silicate-based cements (Micro-Mega mineral trioxide aggregate [MM-MTA], Biodentine [BD], and EndoSequence Root Repair Material [ESRRM] putty) over time after subcutaneous implantation into rats.
Materials and Methods Forty-five silicon tubes containing the tested materials and 15 empty tubes (serving as a control group) were subcutaneously implanted into the backs of 15 Wistar rats. At 1, 4, and 8 weeks after implantation, the animals were euthanized (
n = 5 animals/group), and the silicon tubes were removed with the surrounding tissues. Histopathological tissue sections were stained with von Kossa stain to assess mineralization. Scanning electron microscopy and energy-dispersive X-ray spectroscopy (SEM/EDX) were also used to assess the chemical components of the surface precipitates deposited on the implant and the pattern of calcium and phosphorus distribution at the material-tissue interface. The calcium-to-phosphorus ratios were compared using the non-parametric Kruskal-Wallis test at a significance level of 5%.Results The von Kossa staining showed that both BD and ESRRM putty induced mineralization starting at week 1; this mineralization increased further until the end of the study. In contrast, MM-MTA induced dystrophic calcification later, from 4 weeks onward. SEM/EDX showed no statistically significant differences in the calcium- and phosphorus-rich areas among the 3 materials at any time point (
p > 0.05).Conclusions After subcutaneous implantation, biomineralization of the 3-calcium silicate-based cements started early and increased over time, and all 3 tested cements generated calcium- and phosphorus-containing surface precipitates.
-
Citations
Citations to this article as recorded by- Evaluating Retrieval-Augmented Large Language Models on External Cervical Resorption: A Comparative Study of Gemini and NotebookLM
Marc Garcia-Font, Nicolás Dufey-Portilla, Fernando Durán-Sindreu, José Antonio González Sánchez, Gustavo Rodríguez Millán, Venkateshbabu Nagendrababu, Paul M.H. Dummer, Francesc Abella Sans
Journal of Endodontics.2025;[Epub] CrossRef - Antibacterial, biocompatible, and mineralization‐inducing properties of calcium silicate‐based cements
Taimy Cruz Hondares, Xiaoxiao Hao, Yanfang Zhao, Yuyin Lin, Dobrawa Napierala, Janice G. Jackson, Ping Zhang
International Journal of Paediatric Dentistry.2024; 34(6): 843. CrossRef - Bioactive potential of Bio‐C Pulpo is evidenced by presence of birefringent calcite and osteocalcin immunoexpression in the rat subcutaneous tissue
Marcela Borsatto Queiroz, Rafaela Nanami Handa Inada, Camila Soares Lopes, Juliane Maria Guerreiro‐Tanomaru, Estela Sasso‐Cerri, Mário Tanomaru‐Filho, Paulo Sérgio Cerri
Journal of Biomedical Materials Research Part B: Applied Biomaterials.2022; 110(10): 2369. CrossRef
- Evaluating Retrieval-Augmented Large Language Models on External Cervical Resorption: A Comparative Study of Gemini and NotebookLM
- 2,499 View
- 21 Download
- 4 Web of Science
- 3 Crossref


 KACD
KACD

 First
First Prev
Prev


