Articles
- Page Path
- HOME > Restor Dent Endod > Volume 48(1); 2023 > Article
- Research Article Push-out bond strength and intratubular biomineralization of a hydraulic root-end filling material premixed with dimethyl sulfoxide as a vehicle
-
Ju-Ha Park1
 , Hee-Jin Kim2
, Hee-Jin Kim2 , Kwang-Won Lee1,3,4
, Kwang-Won Lee1,3,4 , Mi-Kyung Yu1,3,4
, Mi-Kyung Yu1,3,4 , Kyung-San Min1,3,4
, Kyung-San Min1,3,4
-
Restor Dent Endod 2023;48(1):e8.
DOI: https://doi.org/10.5395/rde.2023.48.e8
Published online: January 20, 2023
1Department of Conservative Dentistry, School of Dentistry, Jeonbuk National University, Jeonju, Korea.
2Department of Dentistry, College of Medicine, Kosin University, Busan, Korea.
3Research Institute of Clinical Medicine of Jeonbuk National University, Jeonju, Korea.
4Biomedical Research Institute of Jeonbuk National University Hospital, Jeonju, Korea.
- Correspondence to Mi-Kyung Yu, DDS, PhD. Department of Conservative Dentistry, School of Dentistry, Jeonbuk National University, 567 Baekje-daero, Deokjin-gu, Jeonju 54896, Korea. mkyou102@jbnu.ac.kr
- Correspondence to Kyung-San Min, DDS, PhD. Department of Conservative Dentistry, School of Dentistry, Jeonbuk National University, 567 Baekje-daero, Deokjin-gu, Jeonju 54896, Korea. endomin@gmail.com
Copyright © 2023. The Korean Academy of Conservative Dentistry
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Objectives This study was designed to evaluate the parameters of bonding performance to root dentin, including push-out bond strength and dentinal tubular biomineralization, of a hydraulic bioceramic root-end filling material premixed with dimethyl sulfoxide (Endocem MTA Premixed) in comparison to a conventional powder-liquid–type cement (ProRoot MTA).
-
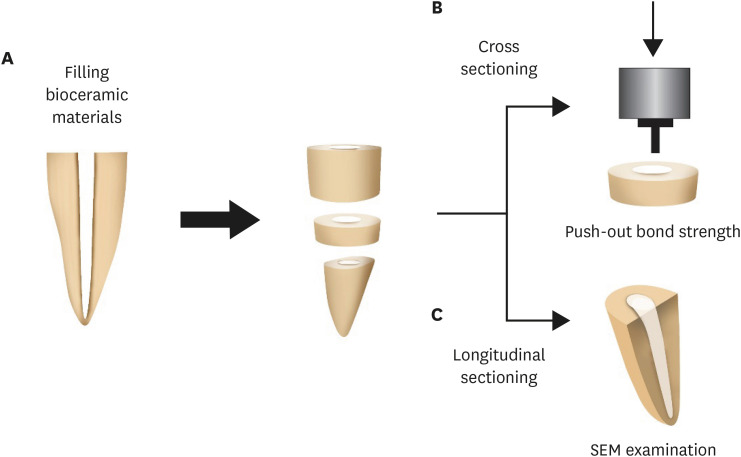
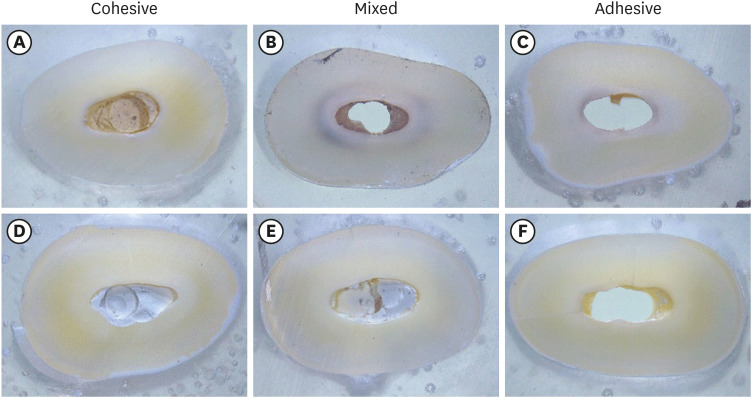
Materials and Methods The root canal of a single-rooted premolar was filled with either ProRoot MTA or Endocem MTA Premixed (n = 15). A slice of dentin was obtained from each root. Using the sliced specimen, the push-out bond strength was measured, and the failure pattern was observed under a stereomicroscope. The apical segment was divided into halves; the split surface was observed under a scanning electron microscope, and intratubular biomineralization was examined by observing the precipitates formed in the dentinal tubule. Then, the chemical characteristics of the precipitates were evaluated with energy-dispersive X-ray spectroscopic (EDS) analysis. The data were analyzed using the Student’s t-test followed by the Mann-Whitney U test (p < 0.05).
-
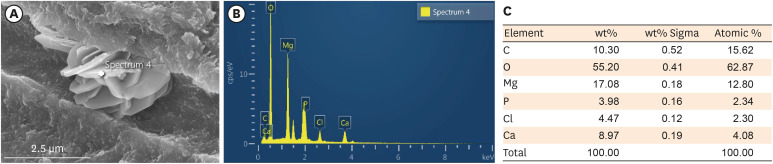
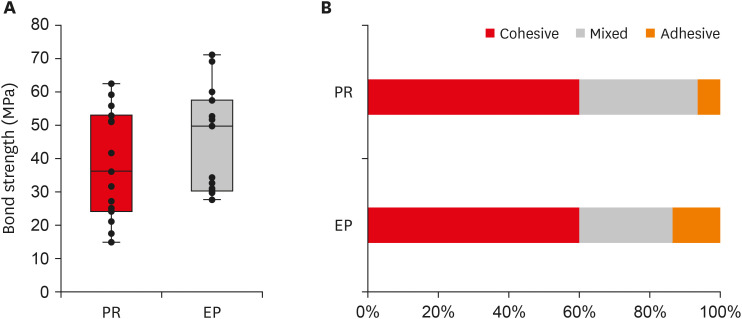
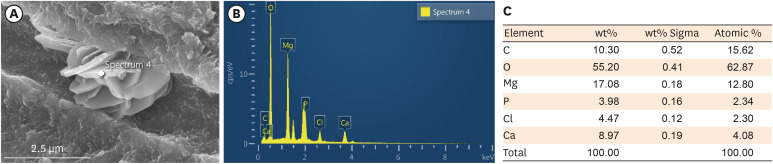
Results No significant difference was found between the 2 tested groups in push-out bond strength, and cohesive failure was the predominant failure type. In both groups, flake-shaped precipitates were observed along dentinal tubules. The EDS analysis indicated that the mass percentage of calcium and phosphorus in the precipitate was similar to that found in hydroxyapatite.
-
Conclusions Regarding bonding to root dentin, Endocem MTA Premixed may have potential for use as an acceptable root-end filling material.
INTRODUCTION
MATERIALS AND METHODS
(1)
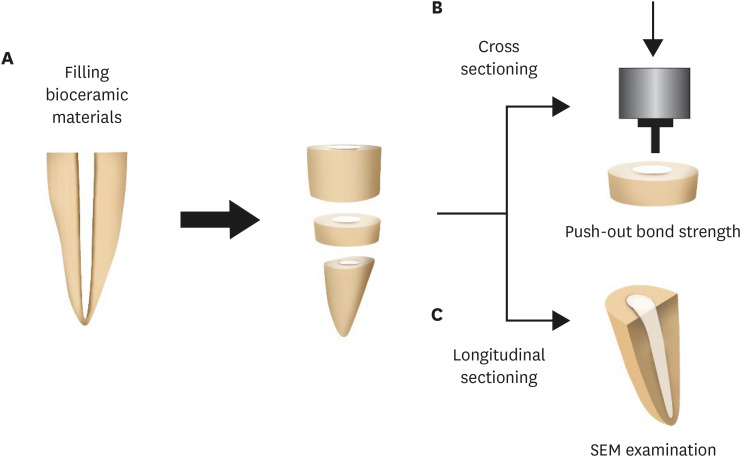
Push-out Bond Strength (MPa) = Maximum Load (N)/Adhesion Area of Root Filling (A) (mm2) ----------Illustration of the experimental procedure. (A) The tooth filled with the tested materials was sectioned horizontally to obtain a sliced specimen and an apical segment. (B) Push-out bond strength was measured with the sliced specimen using a universal testing machine. (C) The apical segment was sectioned longitudinally, and the intratubular biomineralization was observed under scanning electron microscopy.
RESULTS
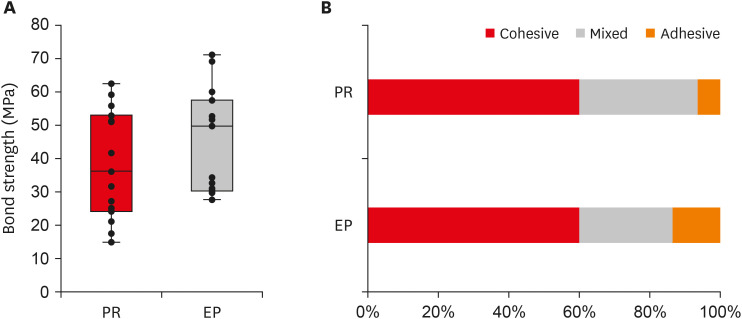
Push-out bond strength and the failure patterns of the tested materials. (A) Bar chart showing the mean bond strength of the 2 tested material groups. (B) Failure mode distribution according to filling material.
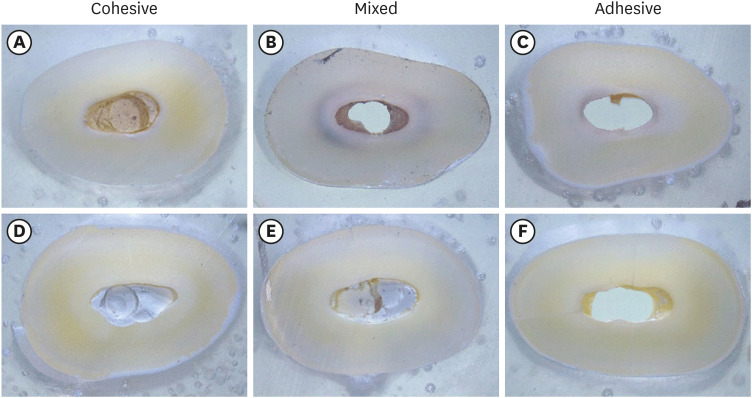
Failure mode analysis using a stereomicroscope at ×30 magnification. (A-C) Representative images of the ProRoot MTA group. (D-F) Representative images of the Endocem MTA Premixed group.
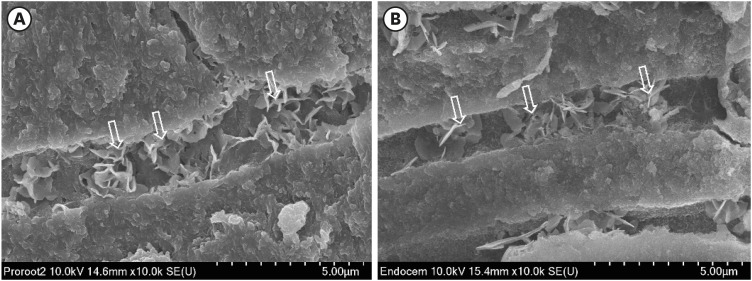
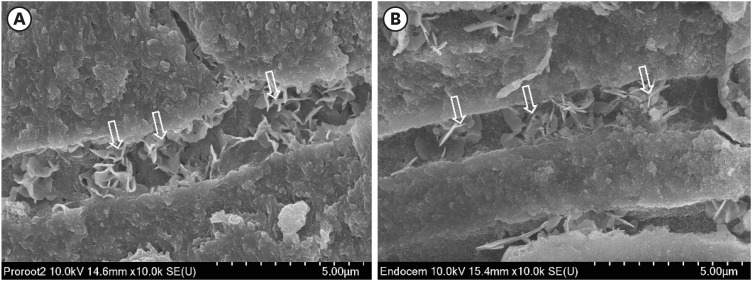
Representative scanning electron microscopy images of intratubular biomineralization. (A) ProRoot MTA-filled root canal. (B) Endocem MTA Premixed-filled root canal. Arrows indicate the flake-shaped intratubular precipitates.
EDS analysis of the chemical characteristics of intratubular precipitate. (A) A scanning electron microscope image showing the precipitate (white cross). (B) Representative graph of EDS analysis of the precipitate. (C) Semiquantitative chemical composition showing the calcium/phosphorus ratio of the crystalline area denoted with a white cross.
DISCUSSION
CONCLUSIONS
-
Funding: This research was supported by a grant of the Korea Medical Device Development Fund grant funded by the Korea government (the Ministry of Science and ICT, the Ministry of Trade, Industry and Energy, the Ministry of Health & Welfare, Republic of Korea, the Ministry of Food and Drug Safety) (Project Number: RS-2020-KD000045).
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Park JH, Yu MK, Min KS.
Data curation: Park JH, Yu MK.
Formal analysis: Min KS.
Funding acquisition: Min KS.
Investigation: Park JH, Kim HJ.
Methodology: Park JH, Yu MK, Min KS.
Project administration: Yu MK, Min KS.
Resources: Yu MK, Min KS.
Software: Min KS.
Supervision: Lee KW.
Validation: Lee KW, Min KS.
Visualization: Park JH, Min KS.
Writing - original draft: Park JH, Min KS.
Writing - review & editing: Kim HJ, Lee KW, Yu MK.
- 1. Saxena P, Gupta SK, Newaskar V. Biocompatibility of root-end filling materials: recent update. Restor Dent Endod 2013;38:119-127.ArticlePubMedPMC
- 2. Bernabé PF, Gomes-Filho JE, Bernabé DG, Nery MJ, Otoboni-Filho JA, Dezan E Jr, Cintra LT. Sealing ability of MTA used as a root end filling material: effect of the sonic and ultrasonic condensation. Braz Dent J 2013;24:107-110.ArticlePubMed
- 3. Torabinejad M, Hong CU, McDonald F, Pitt Ford TR. Physical and chemical properties of a new root-end filling material. J Endod 1995;21:349-353.ArticlePubMed
- 4. Alsubait SA, Hashem Q, AlHargan N, AlMohimeed K, Alkahtani A. Comparative evaluation of push-out bond strength of ProRoot MTA, bioaggregate and Biodentine. J Contemp Dent Pract 2014;15:336-340.ArticlePubMed
- 5. Nagas E, Cehreli ZC, Uyanik MO, Vallittu PK, Lassila LV. Effect of several intracanal medicaments on the push-out bond strength of ProRoot MTA and Biodentine. Int Endod J 2016;49:184-188.PubMed
- 6. Buldur B, Oznurhan F, Kaptan A. The effect of different chelating agents on the push-out bond strength of ProRoot MTA and EndoSequence root repair material. Eur Oral Res 2019;53:88-93.ArticlePubMedPMC
- 7. Saghiri MA, Shokouhinejad N, Lotfi M, Aminsobhani M, Saghiri AM. Push-out bond strength of mineral trioxide aggregate in the presence of alkaline pH. J Endod 2010;36:1856-1859.ArticlePubMed
- 8. Vivan RR, Guerreiro-Tanomaru JM, Bosso-Martelo R, Costa BC, Duarte MA, Tanomaru-Filho M. Push-out bond strength of root-end filling materials. Braz Dent J 2016;27:332-335.ArticlePubMed
- 9. Shokouhinejad N, Razmi H, Fekrazad R, Asgary S, Neshati A, Assadian H, Kheirieh S. Push-out bond strength of two root-end filling materials in root-end cavities prepared by Er,Cr:YSGG laser or ultrasonic technique. Aust Endod J 2012;38:113-117.ArticlePubMed
- 10. Ashofteh Yazdi K, Bolhari B, Sabetmoghaddam T, Meraji N, Kharazifard MJ. Effect of blood exposure on push-out bond strength of four calcium silicate based cements. Iran Endod J 2017;12:196-200.PubMedPMC
- 11. Tuncel B, Nagas E, Cehreli Z, Uyanik O, Vallittu P, Lassila L. Effect of endodontic chelating solutions on the bond strength of endodontic sealers. Braz Oral Res 2015;29:S1806-83242015000100256.ArticlePubMed
- 12. Araújo CC, Brito-Júnior M, Faria-E-Silva AL, Pereira RD, Silva-Sousa YT, Cruz-Filho AM, Sousa-Neto MD. Root filling bond strength using reciprocating file-matched single-cones with different sealers. Braz Oral Res 2016;30:S1806-83242016000100251.PubMed
- 13. Prado MC, Martiniano K, Pereira AC, Cortellazzi KL, Marciano MA, Abuna G, de-Jesus-Soares A. Do intracanal medications used in regenerative endodontics affect the bond strength of powder-to-liquid and ready-to-use cervical sealing materials? J Conserv Dent 2021;24:464-469.ArticlePubMed
- 14. Al-Hiyasat AS, Yousef WA. Push-out bond strength of calcium silicate-based cements in the presence or absence of a smear layer. Int J Dent 2022;2022:7724384.ArticlePubMedPMCPDF
- 15. Salem Milani A, Froughreyhani M, Charchi Aghdam S, Pournaghiazar F, Asghari Jafarabadi M. Mixing with propylene glycol enhances the bond strength of mineral trioxide aggregate to dentin. J Endod 2013;39:1452-1455.ArticlePubMed
- 16. Retana-Lobo C, Tanomaru-Filho M, Guerreiro-Tanomaru JM, Benavides-García M, Hernández-Meza E, Reyes-Carmona J. Push-out bond strength, characterization, and ion release of premixed and powder-liquid bioceramic sealers with or without gutta-percha. Scanning 2021;2021:6617930.ArticlePubMedPMCPDF
- 17. Salim Al-Ani AA, Mutluay M, Stape THS, Tjäderhane L, Tezvergil-Mutluay A. Effect of various dimethyl sulfoxide concentrations on the durability of dentin bonding and hybrid layer quality. Dent Mater J 2018;37:501-505.ArticlePubMed
- 18. Tjäderhane L, Mehtälä P, Scaffa P, Vidal C, Pääkkönen V, Breschi L, Hebling J, Tay FR, Nascimento FD, Pashley DH, Carrilho MR. The effect of dimethyl sulfoxide (DMSO) on dentin bonding and nanoleakage of etch-and-rinse adhesives. Dent Mater 2013;29:1055-1062.ArticlePubMed
- 19. Lindblad RM, Lassila LVJ, Vallittu PK, Tjäderhane L. The effect of chlorhexidine and dimethyl sulfoxide on long-term sealing ability of two calcium silicate cements in root canal. Dent Mater 2021;37:328-335.ArticlePubMed
- 20. Reyes-Carmona JF, Felippe MS, Felippe WT. Biomineralization ability and interaction of mineral trioxide aggregate and white Portland cement with dentin in a phosphate-containing fluid. J Endod 2009;35:731-736.ArticlePubMed
- 21. Yoo YJ, Lee YS, Yoo JS, Perinpanayagam H, Yoo CS, Kang HS, Oh S, Chang SW, Kum KY. Intratubular biomineralization in a root canal filled with calcium-enriched material over 8 years. Materials (Basel) 2017;10:1388.ArticlePubMedPMC
- 22. Reyes-Carmona JF, Felippe MS, Felippe WT. A phosphate-buffered saline intracanal dressing improves the biomineralization ability of mineral trioxide aggregate apical plugs. J Endod 2010;36:1648-1652.ArticlePubMed
- 23. Yoo YJ, Baek SH, Kum KY, Shon WJ, Woo KM, Lee W. Dynamic intratubular biomineralization following root canal obturation with pozzolan-based mineral trioxide aggregate sealer cement. Scanning 2016;38:50-56.ArticlePubMedPDF
- 24. Reyes-Carmona JF, Felippe MS, Felippe WT. The biomineralization ability of mineral trioxide aggregate and Portland cement on dentin enhances the push-out strength. J Endod 2010;36:286-291.ArticlePubMed
REFERENCES
Tables & Figures
REFERENCES
Citations

- Comparison of intratubular biomineralization between in vivo and in vitro conditions
Sieun Nam, Yeon-Jee Yoo, Mi-Kyung Yu, Kyung-San Min
Journal of Oral Science.2026; 68(1): 30. CrossRef - Effectiveness of Sectioning Method and Filling Materials on Roughness and Cell Attachments in Root Resection Procedure
Tarek Ashi, Naji Kharouf, Olivier Etienne, Bérangère Cournault, Pierre Klienkoff, Varvara Gribova, Youssef Haikel
European Journal of Dentistry.2025; 19(01): 240. CrossRef - Bond Strength and Adhesive Interface Quality of New Pre‐Mixed Bioceramic Root Canal Sealer
Gustavo Creazzo, Bruna Monteiro de Barros Ciribelli Alves, Helena Cristina de Assis, Karen Gisselle Garay Villamayor, Manoel Damião de Sousa‐Neto, Jardel Francisco Mazzi‐Chaves, Fabiane Carneiro Lopes‐Olhê
Microscopy Research and Technique.2025; 88(7): 1989. CrossRef - Evaluation of clinical and radiographic outcome of premixed injectable mineral trioxide aggregate and conventional mineral trioxide aggregate as pulpotomy medicaments in primary molars – A split-mouth randomized control trial
U. S. Aiswarya, Sharan S. Sargod, Sundeep K. Hegde, H. T. Ajay Rao, Nanditha Hegde
Journal of Indian Society of Pedodontics and Preventive Dentistry.2025; 43(4): 559. CrossRef - Evaluation of the root dentin bond strength and intratubular biomineralization of a premixed calcium aluminate-based hydraulic bioceramic endodontic sealer
Yu-Na Lee, Min-Kyeong Kim, Hee-Jin Kim, Mi-Kyung Yu, Kwang-Won Lee, Kyung-San Min
Journal of Oral Science.2024; 66(2): 96. CrossRef - Removal efficiency of a fast setting pozzalan-based bioactive cement: a micro CT study
Feyza Çetinkaya, Ahter Şanal Çıkman, Ali Keleş, Banu Arıcıoğlu
BMC Oral Health.2024;[Epub] CrossRef - Antibacterial Activity and Sustained Effectiveness of Calcium Silicate-Based Cement as a Root-End Filling Material against Enterococcus faecalis
Seong-Hee Moon, Seong-Jin Shin, Seunghan Oh, Ji-Myung Bae
Materials.2023; 16(18): 6124. CrossRef

 KACD
KACD
 ePub Link
ePub Link Cite
Cite

