Articles
- Page Path
- HOME > Restor Dent Endod > Volume 46(3); 2021 > Article
- Research Article Postoperative pain after endodontic treatment of necrotic teeth with large intentional foraminal enlargement
-
Ricardo Machado1
 , Daniel Comparin2
, Daniel Comparin2 , Sérgio Aparecido Ignácio3
, Sérgio Aparecido Ignácio3 , Ulisses Xavier da Silva Neto3
, Ulisses Xavier da Silva Neto3
-
Restor Dent Endod 2021;46(3):e31.
DOI: https://doi.org/10.5395/rde.2021.46.e31
Published online: May 31, 2021
1Department of Endodontics, School of Health and Bioscience, Pontifical Catholic University of Paraná – PUC/PR, Curitiba, Paraná, Brazil.
2Department of Endodontics, School of Dentistry, Paranaense University – UNIPAR, Francisco Beltrão, Paraná, Brazil.
3Department of Statistics, School of Health and Bioscience, Pontifical Catholic University of Paraná – PUC/PR, Curitiba, Paraná, Brazil.
- Correspondence to Ricardo Machado, DDS, MSc, PhD. Post-Doctorate Student, Department of Endodontics, School of Health and Bioscience, Pontifical Catholic University of Paraná, – PUC/PR, Rua Imaculada Conceição, 1155, Prado Velho, 80.215-901, Curitiba, Paraná, Brazil. ricardo.machado.endo@gmail.com
Copyright © 2021. The Korean Academy of Conservative Dentistry
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Objectives To evaluate postoperative pain after endodontic treatment of necrotic teeth using large intentional foraminal enlargement (LIFE).
-
Materials and Methods The sample included 60 asymptomatic necrotic teeth (with or without chronic apical periodontitis), and a periodontal probing depth of 3 mm, previously accessed and referred to perform endodontic treatment. After previous procedures, the position and approximate size of the apical foramen (AF) were determined by using an apex locator and K flexo-files, respectively. The chemomechanical preparation was performed with Profile 04 files 2 mm beyond the AF to achieve the LIFE, using 2.5 mL of 2.5% NaOCl at each file change. The filling was performed by Tagger's hybrid technique and EndoFill sealer. Phone calls were made to all the patients at 24, 48 and 72 hours after treatment, to classify postoperative pain. Statistical analysis was performed by different tests with a significance level of 5%.
-
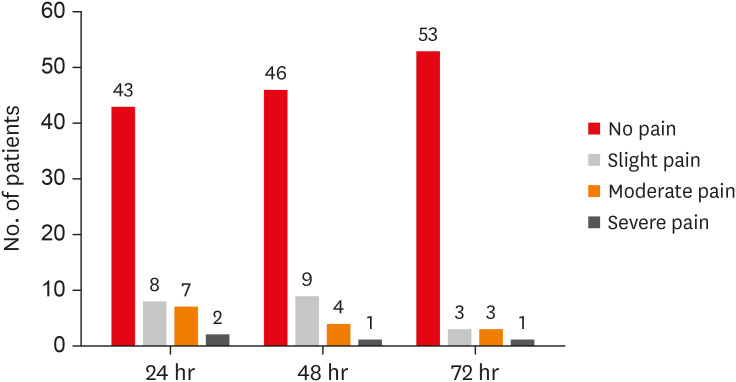
Results Age, gender, periradicular status and tooth type did not influence postoperative pain (p > 0.05). Only 1 patient (1.66%) reported severe pain after 72 hours. Moderate pain was reported by 7, 4 and 3 patients after 24, 48 and 72 hours, respectively (p = 0.0001). However, paired analyses showed a statistically significant difference only between 24 and 72 hours (p = 0.04). Sealer extrusion did not influence the postoperative pain (p > 0.05).
-
Conclusions Acute or moderate postoperative pain was uncommon after endodontic treatment of necrotic teeth with LIFE.
-
Trial Registration The Brazilian Clinical Trials Registry Identifier: RBR-3r967t
INTRODUCTION
MATERIALS AND METHODS
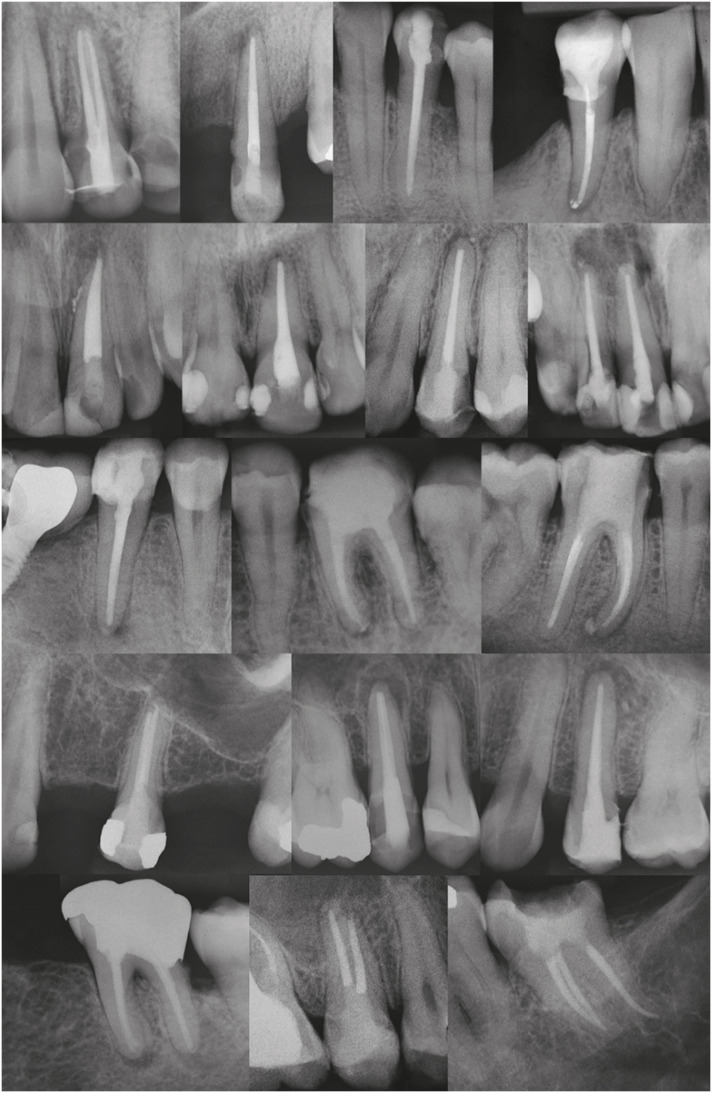
Instrumentation planning for similar large intentional foraminal enlargement (LIFE) to treat different teeth
Scores and features of the pain
RESULTS
Demographic data
Postoperative pain considering time and age, gender, periradicular status, and tooth type
Postoperative pain considering time frame
Postoperative pain considering sealer extrusion
DISCUSSION
CONCLUSIONS
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Machado R.
Data curation: Machado R, Comparin D.
Formal analysis: Ignácio SA.
Funding acquisition: Machado R.
Investigation: Machado R.
Methodology: Machado R.
Project administration: Silva Neto UX.
Resources: Machado R.
Software: Machado R, Ignácio SA.
Supervision: Silva Neto UX.
Validation: Ignácio SA.
Visualization: Machado R.
Writing - original draft: Machado R, Comparin D.
Writing - review & editing: Silva Neto UX.
- 1. Schilder H. Filling root canals in three dimensions. Dent Clin North Am 1967;723-744.ArticlePubMed
- 2. Schilder H. Cleaning and shaping the root canal. Dent Clin North Am 1974;18:269-296.ArticlePubMed
- 3. Üreyen Kaya B, Erik CE, Sesli Çetin E, Köle M, Maden M. Mechanical reduction in intracanal Enterococcus faecalis when using three different single-file systems: an ex vivo comparative study. Int Endod J 2019;52:77-85.ArticlePubMedPDF
- 4. Martinho FC, Gomes CC, Nascimento GG, Gomes AP, Leite FR. Clinical comparison of the effectiveness of 7- and 14-day intracanal medications in root canal disinfection and inflammatory cytokines. Clin Oral Investig 2018;22:523-530.ArticlePubMedPDF
- 5. Chavez de Paz LE. Redefining the persistent infection in root canals: possible role of biofilm communities. J Endod 2007;33:652-662.ArticlePubMed
- 6. Wang J, Chen W, Jiang Y, Liang J. Imaging of extraradicular biofilm using combined scanning electron microscopy and stereomicroscopy. Microsc Res Tech 2013;76:979-983.ArticlePubMed
- 7. Wang J, Jiang Y, Chen W, Zhu C, Liang J. Bacterial flora and extraradicular biofilm associated with the apical segment of teeth with post-treatment apical periodontitis. J Endod 2012;38:954-959.ArticlePubMed
- 8. Brandão PM, de Figueiredo JA, Morgental RD, Scarparo RK, Hartmann RC, Waltrick SB, Souza RA. Influence of foraminal enlargement on the healing of periapical lesions in rat molars. Clin Oral Investig 2019;23:1985-1991.ArticlePubMedPDF
- 9. Borlina SC, de Souza V, Holland R, Murata SS, Gomes-Filho JE, Dezan Junior E, Marion JJ, Neto DA. Influence of apical foramen widening and sealer on the healing of chronic periapical lesions induced in dogs' teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010;109:932-940.ArticlePubMed
- 10. de Souza Filho FJ, Benatti O, de Almeida OP. Influence of the enlargement of the apical foramen in periapical repair of contaminated teeth of dog. Oral Surg Oral Med Oral Pathol 1987;64:480-484.ArticlePubMed
- 11. Tinaz AC, Alacam T, Uzun O, Maden M, Kayaoglu G. The effect of disruption of apical constriction on periapical extrusion. J Endod 2005;31:533-535.ArticlePubMed
- 12. Mostafa MEHAA, El-Shrief YAI, Anous WIO, Hassan MW, Salamah FTA, El Boghdadi RM, El-Bayoumi MAA, Seyam RM, Abd-El-Kader KG, Amin SAW. Postoperative pain following endodontic irrigation using 1.3% versus 5.25% sodium hypochlorite in mandibular molars with necrotic pulps: a randomized double-blind clinical trial. Int Endod J 2020;53:154-166.ArticlePubMedPDF
- 13. Nagendrababu V, Gutmann JL. Factors associated with postobturation pain following single-visit nonsurgical root canal treatment: a systematic review. Quintessence Int 2017;48:193-208.PubMed
- 14. Yaylali IE, Teke A, Tunca YM. The effect of foraminal enlargement of necrotic teeth with a continuous rotary system on postoperative pain: a randomized controlled trial. J Endod 2017;43:359-363.ArticlePubMed
- 15. Cruz Junior JA, Coelho MS, Kato AS, Vivacqua-Gomes N, Fontana CE, Rocha DG, da Silveira Bueno CE. The effect of foraminal enlargement of necrotic teeth with the reciproc system on postoperative pain: a prospective and randomized clinical trial. J Endod 2016;42:8-11.ArticlePubMed
- 16. Silva EJ, Menaged K, Ajuz N, Monteiro MR, Coutinho-Filho TS. Postoperative pain after foraminal enlargement in anterior teeth with necrosis and apical periodontitis: a prospective and randomized clinical trial. J Endod 2013;39:173-176.ArticlePubMed
- 17. Kuttler Y. Microscopic investigation of root apexes. J Am Dent Assoc 1955;50:544-552.ArticlePubMed
- 18. Ponce EH, Vilar Fernández JA. The cemento-dentino-canal junction, the apical foramen, and the apical constriction: evaluation by optical microscopy. J Endod 2003;29:214-219.ArticlePubMed
- 19. Dummer PM, McGinn JH, Rees DG. The position and topography of the apical canal constriction and apical foramen. Int Endod J 1984;17:192-198.ArticlePubMed
- 20. Aminoshariae A, Kulild JC. Master apical file size - smaller or larger: a systematic review of healing outcomes. Int Endod J 2015;48:639-647.ArticlePubMed
- 21. Pasqualini D, Mollo L, Scotti N, Cantatore G, Castellucci A, Migliaretti G, Berutti E. Postoperative pain after manual and mechanical glide path: a randomized clinical trial. J Endod 2012;38:32-36.ArticlePubMed
- 22. Cailleteau JG, Mullaney TP. Prevalence of teaching apical patency and various instrumentation and obturation techniques in United States dental schools. J Endod 1997;23:394-396.ArticlePubMed
- 23. Kherlakian D, Cunha RS, Ehrhardt IC, Zuolo ML, Kishen A, da Silveira Bueno CE. Comparison of the incidence of postoperative pain after using 2 reciprocating systems and a continuous rotary system: a prospective randomized clinical trial. J Endod 2016;42:171-176.ArticlePubMed
- 24. Arias A, de la Macorra JC, Azabal M, Hidalgo JJ, Peters OA. Prospective case controlled clinical study of post-endodontic pain after rotary root canal preparation performed by a single operator. J Dent 2015;43:389-395.ArticlePubMed
- 25. Arias A, de la Macorra JC, Hidalgo JJ, Azabal M. Predictive models of pain following root canal treatment: a prospective clinical study. Int Endod J 2013;46:784-793.ArticlePubMed
- 26. Sun C, Sun J, Tan M, Hu B, Gao X, Song J. Pain after root canal treatment with different instruments: a systematic review and meta-analysis. Oral Dis 2018;24:908-919.ArticlePubMedPDF
- 27. Alí A, Olivieri JG, Duran-Sindreu F, Abella F, Roig M, García-Font M. Influence of preoperative pain intensity on postoperative pain after root canal treatment: A prospective clinical study. J Dent 2016;45:39-42.ArticlePubMed
- 28. Sadaf D, Ahmad MZ. Factors associated with postoperative pain in endodontic therapy. Int J Biomed Sci 2014;10:243-247.ArticlePubMedPMC
- 29. Patil AA, Joshi SB, Bhagwat SV, Patil SA. Incidence of postoperative pain after single visit and two visit root canal therapy: a randomized controlled trial. J Clin Diagn Res 2016;10:ZC09-ZC12.Article
- 30. El Mubarak AH, Abu-bakr NH, Ibrahim YE. Postoperative pain in multiple-visit and single-visit root canal treatment. J Endod 2010;36:36-39.ArticlePubMed
- 31. Paredes-Vieyra J, Enriquez FJ. Success rate of single- versus two-visit root canal treatment of teeth with apical periodontitis: a randomized controlled trial. J Endod 2012;38:1164-1169.ArticlePubMed
- 32. García-Font M, Duran-Sindreu F, Calvo C, Basilio J, Abella F, Ali A, Roig M, Olivieri JG. Comparison of postoperative pain after root canal treatment using reciprocating instruments based on operator's experience: a prospective clinical study. J Clin Exp Dent 2017;9:e869-e874.PubMedPMC
- 33. Graunaite I, Skucaite N, Lodiene G, Agentiene I, Machiulskiene V. Effect of resin-based and bioceramic root canal sealers on postoperative pain: a split-mouth randomized controlled trial. J Endod 2018;44:689-693.ArticlePubMed
- 34. Al-Negrish AR, Habahbeh R. Flare up rate related to root canal treatment of asymptomatic pulpally necrotic central incisor teeth in patients attending a military hospital. J Dent 2006;34:635-640.ArticlePubMed
- 35. Relvas JB, Bastos MM, Marques AA, Garrido AD, Sponchiado EC Jr. Assessment of postoperative pain after reciprocating or rotary NiTi instrumentation of root canals: a randomized, controlled clinical trial. Clin Oral Investig 2016;20:1987-1993.ArticlePubMedPDF
- 36. Çiçek E, Koçak MM, Koçak S, Sağlam BC, Türker SA. Postoperative pain intensity after using different instrumentation techniques: a randomized clinical study. J Appl Oral Sci 2017;25:20-26.ArticlePubMedPMC
- 37. Farzaneh S, Parirokh M, Nakhaee N, Abbott PV. Effect of two different concentrations of sodium hypochlorite on postoperative pain following single-visit root canal treatment: a triple-blind randomized clinical trial. Int Endod J 2018;51(Suppl 1):e2-e11.ArticlePubMedPDF
- 38. Attar S, Bowles WR, Baisden MK, Hodges JS, McClanahan SB. Evaluation of pretreatment analgesia and endodontic treatment for postoperative endodontic pain. J Endod 2008;34:652-655.ArticlePubMed
- 39. Arias A, Azabal M, Hidalgo JJ, de la Macorra JC. Relationship between postendodontic pain, tooth diagnostic factors, and apical patency. J Endod 2009;35:189-192.ArticlePubMed
- 40. Ali SG, Mulay S, Palekar A, Sejpal D, Joshi A, Gufran H. Prevalence of and factors affecting post-obturation pain following single visit root canal treatment in Indian population: a prospective, randomized clinical trial. Contemp Clin Dent 2012;3:459-463.ArticlePubMedPMC
- 41. Ng YL, Glennon JP, Setchell DJ, Gulabivala K. Prevalence of and factors affecting post-obturation pain in patients undergoing root canal treatment. Int Endod J 2004;37:381-391.ArticlePubMed
- 42. Polycarpou N, Ng YL, Canavan D, Moles DR, Gulabivala K. Prevalence of persistent pain after endodontic treatment and factors affecting its occurrence in cases with complete radiographic healing. Int Endod J 2005;38:169-178.ArticlePubMed
- 43. Unruh AM. Gender variations in clinical pain experience. Pain 1996;65:123-167.ArticlePubMed
- 44. Fillingim RB, Maixner W. Gender differences in the responses to noxious stimuli. Pain Forum 1995;4:209-221.Article
- 45. Vier FV, Figueiredo JA. Prevalence of different periapical lesions associated with human teeth and their correlation with the presence and extension of apical external root resorption. Int Endod J 2002;35:710-719.PubMed
- 46. Marshall JG, Liesinger AW. Factors associated with endodontic posttreatment pain. J Endod 1993;19:573-575.ArticlePubMed
- 47. Genet JM, Hart AA, Wesselink PR, Thoden van Velzen SK. Preoperative and operative factors associated with pain after the first endodontic visit. Int Endod J 1987;20:53-64.ArticlePubMed
- 48. Estrela C, Bueno MR, Leles CR, Azevedo B, Azevedo JR. Accuracy of cone beam computed tomography and panoramic and periapical radiography for detection of apical periodontitis. J Endod 2008;34:273-279.ArticlePubMed
- 49. Bender IB, Seltzer S. Roentgenographic and direct observation of experimental lesions in bone: II. 1961. J Endod 2003;29:707-712.PubMed
- 50. Bender IB, Seltzer S. Roentgenographic and direct observation of experimental lesions in bone: I. 1961. J Endod 2003;29:702-706.PubMed
- 51. Halse A, Molven O, Fristad I. Diagnosing periapical lesions--disagreement and borderline cases. Int Endod J 2002;35:703-709.ArticlePubMed
- 52. Yesilsoy C, Koren LZ, Morse DR, Rankow H, Bolanos OR, Furst ML. Post-endodontic obturation pain: a comparative evaluation. Quintessence Int 1988;19:431-438.PubMed
- 53. Liddell A, Locker D. Gender and age differences in attitudes to dental pain and dental control. Community Dent Oral Epidemiol 1997;25:314-318.ArticlePubMed
- 54. Shokraneh A, Ajami M, Farhadi N, Hosseini M, Rohani B. Postoperative endodontic pain of three different instrumentation techniques in asymptomatic necrotic mandibular molars with periapical lesion: a prospective, randomized, double-blind clinical trial. Clin Oral Investig 2017;21:413-418.ArticlePubMedPDF
- 55. Pak JG, White SN. Pain prevalence and severity before, during, and after root canal treatment: a systematic review. J Endod 2011;37:429-438.ArticlePubMed
- 56. Hackel D, Pflücke D, Neumann A, Viebahn J, Mousa S, Wischmeyer E, Roewer N, Brack A, Rittner HL. The connection of monocytes and reactive oxygen species in pain. PLoS One 2013;8:e63564.ArticlePubMedPMC
- 57. Vengerfeldt V, Mändar R, Saag M, Piir A, Kullisaar T. Oxidative stress in patients with endodontic pathologies. J Pain Res 2017;10:2031-2040.PubMedPMC
- 58. Camargo CH, Camargo SE, Valera MC, Hiller KA, Schmalz G, Schweikl H. The induction of cytotoxicity, oxidative stress, and genotoxicity by root canal sealers in mammalian cells. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;108:952-960.ArticlePubMed
- 59. Cintra LT, Benetti F, de Azevedo Queiroz IO, Ferreira LL, Massunari L, Bueno CR, de Oliveira SH, Gomes-Filho JE. Evaluation of the cytotoxicity and biocompatibility of new resin epoxy-based endodontic sealer containing calcium hydroxide. J Endod 2017;43:2088-2092.ArticlePubMed
- 60. Morgental RD, Vier-Pelisser FV, Oliveira SD, Antunes FC, Cogo DM, Kopper PM. Antibacterial activity of two MTA-based root canal sealers. Int Endod J 2011;44:1128-1133.ArticlePubMed
REFERENCES
Tables & Figures
REFERENCES
Citations

- Assessment of apical extrusion in regenerative endodontics: a comparative study of different irrigation methods using three-dimensional immature tooth models
Vahide Hazal Abat, Gökçen Deniz Bayrak, Mustafa Gündoğar
Odontology.2025; 113(1): 213. CrossRef - Clinical Advances in Calcium Phosphate for Maxillomandibular Bone Regeneration: From Bench to Bedside
Seyed Ali Mostafavi Moghaddam, Hamid Mojtahedi, Amirhossein Bahador, Lotfollah Kamali Hakim, Hamid Tebyaniyan
Ceramics.2025; 8(4): 129. CrossRef - Postoperative pain after single-visit root canal treatments in necrotic teeth comparing instruments’ kinematics and apical instrumentation limits – a prospective randomized multicenter clinical trial
Ricardo Machado, Guilherme Moreira, Daniel Comparin, Arthur Pimentel Barroso, Jaqueline Nascimento, Caio Cézar Randi Ferraz, Sérgio Aparecido Ignácio, Lucas da Fonseca Roberti Garcia, Rodrigo Rodrigues Amaral, David Shadid, Ulisses Xavier da Silva Neto
BMC Oral Health.2024;[Epub] CrossRef - Assessment of mechanical allodynia in healthy teeth adjacent and contralateral to endodontically diseased teeth: a clinical study
Vaishnavi Ratnakar Patankar, Ashish K Jain, Rahul D Rao, Prajakta R Rao
Restorative Dentistry & Endodontics.2024;[Epub] CrossRef - A systematic review and meta-analysis on the effects of phototherapy on postoperative pain in conventional endodontic reintervention
Larissa Pereira Nunes, Gabriel Pereira Nunes, Túlio Morandin Ferrisse, Henrico Badaoui Strazzi-Sahyon, Eloi Dezan-Júnior, Luciano Tavares Angelo Cintra, Gustavo Sivieri-Araujo
Clinical Oral Investigations.2024;[Epub] CrossRef - The effect of intracanal cryotherapy with and without foraminal enlargement on pain prevention after endodontic treatment: a randomized clinical trial
Marcos Felipe Iparraguirre Nuñovero, Marco Antonio Hungaro Duarte, André Vinícius Kaled Segato, Ulisses Xavier da Silva Neto, Vania Portela Ditzel Westphalen, Everdan Carneiro
Scientific Reports.2024;[Epub] CrossRef - Clinical determination of anatomical diameter in different dental groups correlating them with gender, age, tooth/canal and pulpoperiradicular diagnosis: an observational clinical study
Ricardo Machado, Gabriel Filipe Pamplona, Claudemir de Souza Júnior, Jaqueline Nascimento, Eduardo Donato Eing Elgelke Back, Daniel Comparin, Sérgio Aparecido Ignácio, Stella Maria Glaci Reinke, Ana Cristina Kovalik, Ulisses Xavier da Silva Neto
Scientific Reports.2023;[Epub] CrossRef - How much to enlarge? A letter to the editor
Krishnamachari Janani, Kavalipurapu Venkata Teja, Kumar Chandan Srivatsava
Saudi Endodontic Journal.2023; 13(3): 288. CrossRef - Efficiency of diode laser in control of post-endodontic pain: a randomized controlled trial
Hend H. Ismail, Maram Obeid, Ehab Hassanien
Clinical Oral Investigations.2023; 27(6): 2797. CrossRef - Periapical Healing following Root Canal Treatment Using Different Endodontic Sealers: A Systematic Review
Akshay Khandelwal, Krishnamachari Janani, KavalipurapuVenkata Teja, Jerry Jose, Gopi Battineni, Francesco Riccitiello, Alessandra Valletta, Ajitha Palanivelu, Gianrico Spagnuolo, Vincenzo Grassia
BioMed Research International.2022;[Epub] CrossRef
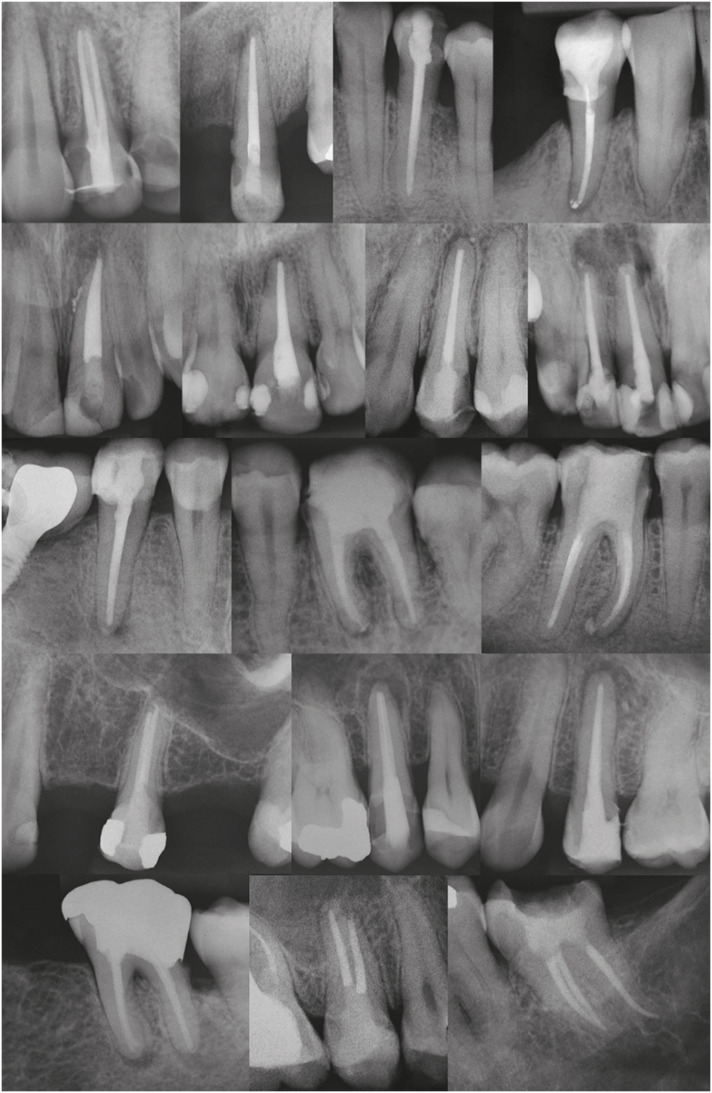
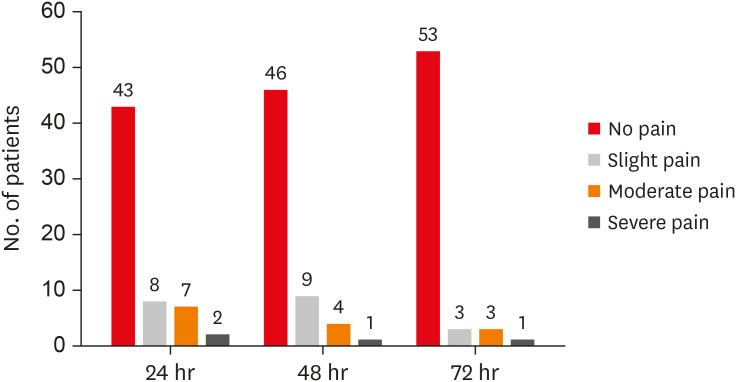
Figure 1
Figure 2
Instrumentation planning for similar large intentional foraminal enlargement (LIFE) to treat different teeth
| Approximate size of AF before instrumentation (corresponding to the manual Flexo-File number) | Final file used 2mm beyond the AF (tip/taper) | Approximate size of AF after instrumentation (corresponding to D2 of the final file used) |
|---|---|---|
| 10 | 30.04 | 38 |
| 15 | 35.04 | 43 |
| 20 | 40.04 | 48 |
| 25 | 45.04 | 53 |
| 30 | 60.04 | 68 |
AF, apical foramen.
Scores and features of the pain
| Score | Pain | Features |
|---|---|---|
| 0 | No pain | The patient felt well. |
| 1 | Slight pain | The patient could be distracted from feeling pain, and no analgesic was required. |
| 2 | Moderate pain | The patient felt moderate pain even while concentrating on some other activity, and an analgesic was required. |
| 3 | Severe pain | The patient was no longer able to perform any type of activity, and needed to lie down and rest (analgesics had little or no effect on relieving the pain). |
Demographic data
| Characteristics | Men | Women | Total | |
|---|---|---|---|---|
| No. of patients | 28 | 32 | 60 | |
| Age (mean ± standard deviation) | 37.86 ± 18.55 | 38.38 ± 15.29 | - | |
| Periradicular status | Without lesion: 3 | Without lesion: 9 | 12 | |
| With lesion: 25 | With lesion: 23 | 48 | ||
| Tooth | ||||
| Maxillary canine | 1 | 2 | 3 | |
| Mandibular central incisor | 4 | 0 | 4 | |
| Maxillary central incisor | 3 | 4 | 7 | |
| Mandibular lateral incisor | 1 | 0 | 1 | |
| Maxillary lateral incisor | 0 | 1 | 1 | |
| First mandibular molar | 3 | 5 | 8 | |
| First maxillary molar | 2 | 3 | 5 | |
| First mandibular premolar | 1 | 1 | 2 | |
| First maxillary premolar | 3 | 3 | 6 | |
| Second mandibular molar | 0 | 1 | 1 | |
| Second maxillary molar | 4 | 0 | 4 | |
| Second mandibular premolar | 2 | 5 | 7 | |
| Second maxillary premolar | 4 | 7 | 11 | |
Postoperative pain considering time and age, gender, periradicular status, and tooth type
| Characteristics | Time (after; hr) | Subdivision | Number | Mean pain score | Standard deviation | p value |
|---|---|---|---|---|---|---|
| Age | 24 | < 30 years old | 21 | 0.52 | 0.873 | 0.10* |
| ≥ 30 and ≤ 50 years old | 21 | 0.71 | 1.007 | |||
| > 50 years old | 18 | 0.11 | 0.323 | |||
| 48 | < 30 years old | 21 | 0.43 | 0.811 | 0.30* | |
| ≥ 30 and ≤ 50 years old | 21 | 0.43 | 0.746 | |||
| > 50 years old | 18 | 0.11 | 0.323 | |||
| 72 | < 30 years old | 21 | 0.29 | 0.784 | 0.17* | |
| ≥ 30 and ≤ 50 years old | 21 | 0.29 | 0.644 | |||
| > 50 years old | 18 | 0.00 | 0.000 | |||
| Gender | 24 | Men | 28 | 0.32 | 0.612 | 0.40† |
| Women | 32 | 0.59 | 0.979 | |||
| 48 | Men | 28 | 0.25 | 0.518 | 0.62† | |
| Women | 32 | 0.41 | 0.798 | |||
| 72 | Men | 28 | 0.07 | 0.378 | 0.07† | |
| Women | 32 | 0.31 | 0.738 | |||
| Periradicular status | 24 | Without lesion | 12 | 0.50 | 0.790 | 0.72† |
| With lesion | 48 | 0.46 | 0.840 | |||
| 48 | Without lesion | 12 | 0.50 | 0.790 | 0.32† | |
| With lesion | 48 | 0.29 | 0.650 | |||
| 72 | Without lesion | 12 | 0.33 | 0.770 | 0.50† | |
| With lesion | 48 | 0.17 | 0.550 | |||
| Tooth type‡ | 24 | Maxillary canine | 3 | 0.00 | 0.000 | 0.87* |
| Mandibular central incisor | 4 | 0.50 | 1.000 | |||
| Maxillary central incisor | 7 | 0.71 | 0.951 | |||
| First mandibular molar | 8 | 0.50 | 1.069 | |||
| First maxillary molar | 5 | 0.60 | 0.894 | |||
| First maxillary premolar | 6 | 0.17 | 0.408 | |||
| Second maxillary molar | 4 | 0.50 | 0.577 | |||
| Second mandibular premolar | 7 | 0.71 | 1.254 | |||
| Second maxillary premolar | 11 | 0.27 | 0.647 | |||
| 48 | Maxillary canine | 3 | 0.00 | 0.000 | 0.81* | |
| Mandibular central incisor | 4 | 0.25 | 0.500 | |||
| Maxillary central incisor | 7 | 0.57 | 0.787 | |||
| First mandibular molar | 8 | 0.50 | 1.069 | |||
| First maxillary molar | 5 | 0.00 | 0.000 | |||
| First maxillary premolar | 6 | 0.17 | 0.408 | |||
| Second maxillary molar | 4 | 0.25 | 0.500 | |||
| Second mandibular premolar | 7 | 0.43 | 0.787 | |||
| Second maxillary premolar | 11 | 0.27 | 0.647 | |||
| 72 | Maxillary canine | 3 | 0.00 | 0.000 | 0.56* | |
| Mandibular central incisor | 4 | 0.00 | 0.000 | |||
| Maxillary central incisor | 7 | 0.43 | 0.787 | |||
| First mandibular molar | 8 | 0.38 | 1.061 | |||
| First maxillary molar | 5 | 0.00 | 0.000 | |||
| First maxillary premolar | 6 | 0.00 | 0.000 | |||
| Second maxillary molar | 4 | 0.00 | 0.000 | |||
| Second mandibular premolar | 7 | 0.43 | 0.787 | |||
| Second maxillary premolar | 11 | 0.18 | 0.603 |
*Value obtained from Kruskal-Wallis test; †Value obtained from Mann-Whitney U test; ‡Only tooth types with n. greater than 2 were used to analyze this variable.
Postoperative pain considering time frame
| Characteristics | Comparative analysis (hr) | Mean pain difference | Standard error | Test statistics | p value* |
|---|---|---|---|---|---|
| Time frame | 24 vs. 48 | 0.13 | 0.18 | 0.73 | 0.46 |
| 48 vs. 72 | 0.18 | 0.18 | 1.00 | 0.31 | |
| 24 vs. 72 | 0.37 | 0.18 | 2.02 | 0.04 |
*Value obtained by Friedman's multiple 2 to 2 comparisons test.
Postoperative pain considering sealer extrusion
| Characteristics | Time (after; hr) | Occurrence of the event | Number | Mean pain score | Standard deviation | p value* |
|---|---|---|---|---|---|---|
| Sealer extrusion | 24 | No | 36 | 0.25 | 0.50 | 0.07 |
| Yes | 24 | 0.79 | 1.10 | |||
| 48 | No | 36 | 0.19 | 0.46 | 0.10 | |
| Yes | 24 | 0.54 | 0.88 | |||
| 72 | No | 36 | 0.08 | 0.36 | 0.07 | |
| Yes | 24 | 0.38 | 0.82 |
*Value obtained from Mann-Whitney U test.
AF, apical foramen.
*Value obtained from Kruskal-Wallis test; †Value obtained from Mann-Whitney
*Value obtained by Friedman's multiple 2 to 2 comparisons test.
*Value obtained from Mann-Whitney

 KACD
KACD
 ePub Link
ePub Link Cite
Cite

