Articles
- Page Path
- HOME > Restor Dent Endod > Volume 44(3); 2019 > Article
-
Research Article
Coronal tooth discoloration induced by regenerative endodontic treatment using different scaffolds and intracanal coronal barriers: a 6-month
ex vivo study -
Noushin Shokouhinejad1,2
 , Hassan Razmi1
, Hassan Razmi1 , Maryam Farbod1
, Maryam Farbod1 , Marzieh Alikhasi2,3,4
, Marzieh Alikhasi2,3,4 , Josette Camilleri5
, Josette Camilleri5
-
Restor Dent Endod 2019;44(3):e25.
DOI: https://doi.org/10.5395/rde.2019.44.e25
Published online: July 16, 2019
1Department of Endodontics, School of Dentistry, Tehran University of Medical Sciences, Tehran, Iran.
2Dental Research Center, Dentistry Research Institute, Tehran University of Medical Sciences, Tehran, Iran.
3Dental Implant Research Center, Dentistry Research Institute, Tehran University of Medical Sciences, Tehran, Iran.
4Department of Prosthodontics, School of Dentistry, Tehran University of Medical Sciences, Tehran, Iran.
5School of Dentistry, Institute of Clinical Sciences, College of Medical and Dental Sciences, University of Birmingham, Edgbaston, Birmingham, UK.
- Correspondence to Josette Camilleri. School of Dentistry, Institute of Clinical Sciences, College of Medical and Dental Sciences, University of Birmingham, 5 Mill Pool Way, Edgbaston, Birmingham B5 7EG, UK. J.Camilleri@bham.ac.uk
Copyright © 2019. The Korean Academy of Conservative Dentistry
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 1,982 Views
- 22 Download
- 15 Crossref
Abstract
-
Objective The aim of this study was to evaluate discoloration of teeth undergoing regenerative endodontic procedures (REPs) using blood clot or platelet-rich fibrin (PRF) as the scaffolds and different calcium silicate-based materials as the intracanal coronal barriers in an ex vivo model.
-
Materials and Methods Forty-eight bovine incisors were prepared and disinfected using 1 mg/mL double antibiotic paste (DAP). The specimens were then randomly divided into 2 groups (n = 24) according to the scaffolds (blood or PRF). After placement of scaffolds each group was divided into 2 subgroups (n = 12) according to the intracanal coronal barriers (ProRoot MTA or Biodentine). The pulp chamber walls were sealed with dentin bonding agent before placement of DAP and before placement of scaffolds. The color changes (∆E) were measured at different steps. The data were analyzed using 2-way analysis of variance.
-
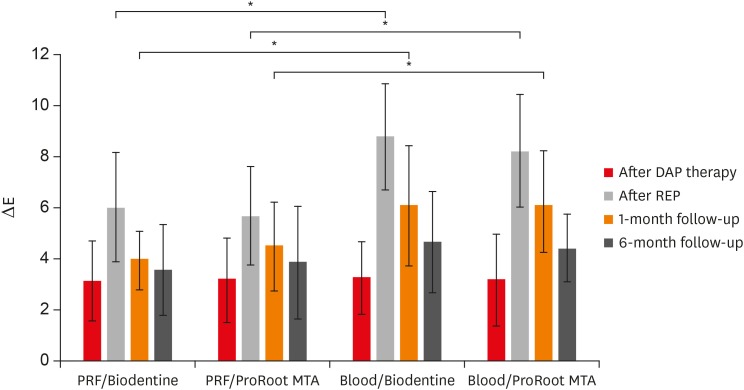
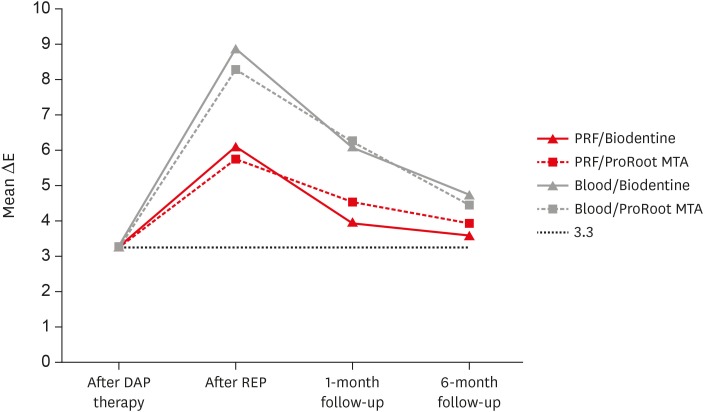
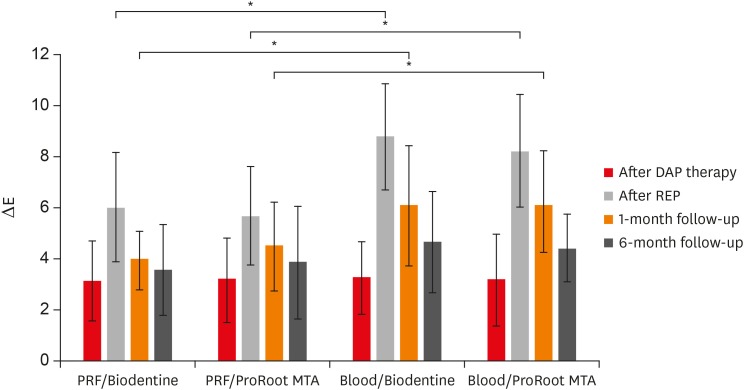
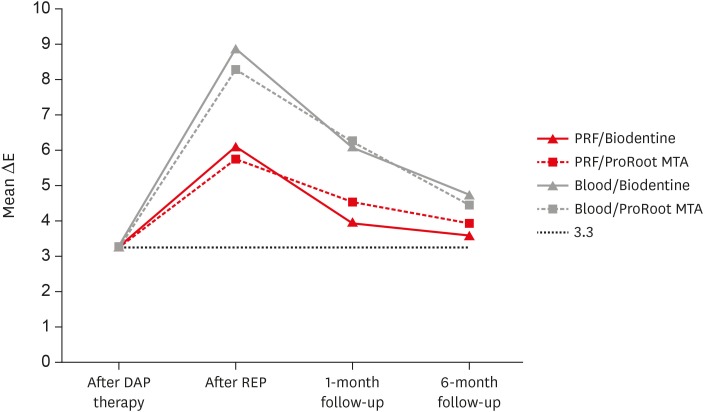
Results Coronal discoloration induced by DAP was not clinically perceptible (ΔE ≤ 3.3). Regarding the type of the scaffold, coronal discoloration was significantly higher in blood groups compared with PRF groups at the end of REP and after 1 month (p < 0.05). However, no significant difference was found between PRF and blood clot after 6 months (p > 0.05). Considering the type of intracanal coronal barrier, no significant difference existed between ProRoot MTA and Biodentine (p > 0.05).
-
Conclusions With sealing the dentinal tubules of pulp chamber with a dentin bonding agent and application of DAP as an intracanal medicament, coronal color change of the teeth following the use of PRF and blood sealed with either ProRoot MTA or Biodentine was not different at 6-month follow-up.
INTRODUCTION
MATERIALS AND METHODS
Group 1: the root canals were filled with human blood using a syringe up to 4 mm below the facial CEJ and it was allowed to form a blood clot for 15 minutes.
Group 2: the root canals were filled with PRF as a scaffold up to 4 mm below the facial CEJ. For the PRF preparation, human blood was collected in sterile tubes from the cubital vein. The tubes were centrifuged for 8 minutes with a speed of 1,300 rpm (DUO Quattro Centrifuge, Nice, France). Three layers were formed inside each test tube: a base layer containing erythrocytes, an intermediate layer of PRF, and a surface layer of platelet poor plasma. The PRF was separated from the other layers.
1. Initial: prior to application of antibiotic mixture as the baseline color
2. After DAP therapy: 4 weeks after placement of antibiotic mixture
3. After REP: after placement of scaffolds, intracanal coronal barriers and coronal restoration
4. At 1-month follow-up
5. At 6-month follow-up
RESULTS
ΔE values (mean and standard deviation) of the experimental groups at the different steps. Significant difference between scaffolds (blood and platelet-rich fibrin [PRF]) was shown at the end of regenerative endodontic procedure (REP) and 1-month follow-up.
The color changes at each treatment step. The dotted line represents clinically perceptible discoloration of ΔE ≥ 3.3.
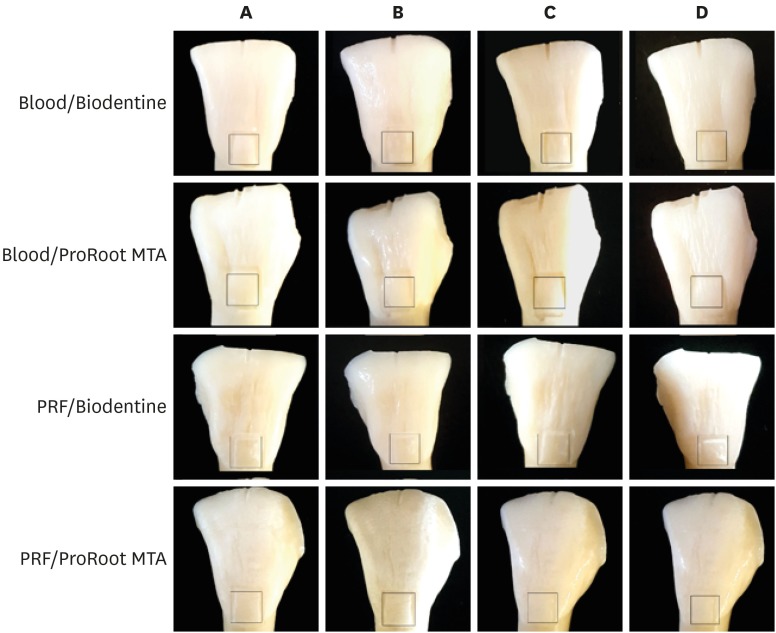
Photographs of teeth in each group. (A) At the end of 4-week antibiotic therapy. (B) At the end of endodontic regenerative procedure. (C) At 1-month follow-up. (D) At 6-month follow-up. The color changes were measured within the defined area.

DISCUSSION
CONCLUSIONS
ACKNOWLEDGEMENTS
-
Funding: This study was funded by Tehran University of Medical Sciences (grant No. 35610).
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Shokouhinejad N, Razmi H, Alikhasi M, Farbod M, Camilleri J.
Data curation: Shokouhinejad N, Farbod M.
Formal analysis: Alikhasi M.
Investigation: Shokouhinejad N, Farbod M, Alikhasi M.
Methodology: Shokouhinejad N, Razmi H, Alikhasi M.
Supervision: Shokouhinejad N, Razmi H, Camilleri J.
Writing - original draft: Farbod M, Alikhasi M.
Writing - review & editing: Shokouhinejad N, Camilleri J.
- 1. Nosrat A, Homayounfar N, Oloomi K. Drawbacks and unfavorable outcomes of regenerative endodontic treatments of necrotic immature teeth: a literature review and report of a case. J Endod 2012;38:1428-1434.ArticlePubMed
- 2. Hargreaves KM, Diogenes A, Teixeira FB. Treatment options: biological basis of regenerative endodontic procedures. J Endod 2013;39:S30-S43.ArticlePubMedPMC
- 3. Hargreaves KM, Giesler T, Henry M, Wang Y. Regeneration potential of the young permanent tooth: what does the future hold? J Endod 2008;34:S51-S56.ArticlePubMed
- 4. Kim JH, Kim Y, Shin SJ, Park JW, Jung IY. Tooth discoloration of immature permanent incisor associated with triple antibiotic therapy: a case report. J Endod 2010;36:1086-1091.ArticlePubMed
- 5. Park HB, Lee BN, Hwang YC, Hwang IN, Oh WM, Chang HS. Treatment of non-vital immature teeth with amoxicillin-containing triple antibiotic paste resulting in apexification. Restor Dent Endod 2015;40:322-327.ArticlePubMedPMC
- 6. American Association of Endodontists. AAE clinical considerations for a regenerative procedure. Revised 6-8-16 [Internet]. Chicago (IL): American Association of Endodontists; 2017. cited 2017 Jul 30]. Available from: https://www.aae.org/specialty/wp-content/uploads/sites/2/2017/06/currentregenerativeendodonticconsiderations.pdf.
- 7. Galler KM, Krastl G, Simon S, Van Gorp G, Meschi N, Vahedi B, Lambrechts P. European Society of Endodontology position statement: revitalization procedures. Int Endod J 2016;49:717-723.ArticlePubMed
- 8. Lee BN, Moon JW, Chang HS, Hwang IN, Oh WM, Hwang YC. A review of the regenerative endodontic treatment procedure. Restor Dent Endod 2015;40:179-187.ArticlePubMedPMC
- 9. Kontakiotis EG, Filippatos CG, Tzanetakis GN, Agrafioti A. Regenerative endodontic therapy: a data analysis of clinical protocols. J Endod 2015;41:146-154.ArticlePubMed
- 10. Akcay M, Arslan H, Yasa B, Kavrık F, Yasa E. Spectrophotometric analysis of crown discoloration induced by various antibiotic pastes used in revascularization. J Endod 2014;40:845-848.ArticlePubMed
- 11. Reynolds K, Johnson JD, Cohenca N. Pulp revascularization of necrotic bilateral bicuspids using a modified novel technique to eliminate potential coronal discolouration: a case report. Int Endod J 2009;42:84-92.ArticlePubMed
- 12. Shokouhinejad N, Khoshkhounejad M, Alikhasi M, Bagheri P, Camilleri J. Prevention of coronal discoloration induced by regenerative endodontic treatment in an ex vivo model. Clin Oral Investig 2018;22:1725-1731.ArticlePubMedPDF
- 13. Porter ML, Münchow EA, Albuquerque MT, Spolnik KJ, Hara AT, Bottino MC. Effects of novel 3-dimensional antibiotic-containing electrospun scaffolds on dentin discoloration. J Endod 2016;42:106-112.ArticlePubMed
- 14. Kahler B, Mistry S, Moule A, Ringsmuth AK, Case P, Thomson A, Holcombe T. Revascularization outcomes: a prospective analysis of 16 consecutive cases. J Endod 2014;40:333-338.ArticlePubMed
- 15. Torabinejad M, Faras H. A clinical and histological report of a tooth with an open apex treated with regenerative endodontics using platelet-rich plasma. J Endod 2012;38:864-868.ArticlePubMed
- 16. Güven Polat G, Yıldırım C, Akgün OM, Altun C, Dinçer D, Ozkan CK. The use of platelet rich plasma in the treatment of immature tooth with periapical lesion: a case report. Restor Dent Endod 2014;39:230-234.ArticlePubMedPMC
- 17. Shivashankar VY, Johns DA, Maroli RK, Sekar M, Chandrasekaran R, Karthikeyan S, Renganathan SK. Comparison of the effect of PRP, PRF and induced bleeding in the revascularization of teeth with necrotic pulp and open apex: a triple blind randomized clinical trial. J Clin Diagn Res 2017;11:ZC34-ZC39.ArticlePubMedPMC
- 18. Huang FM, Yang SF, Zhao JH, Chang YC. Platelet-rich fibrin increases proliferation and differentiation of human dental pulp cells. J Endod 2010;36:1628-1632.ArticlePubMed
- 19. Shokouhinejad N, Nekoofar MH, Pirmoazen S, Shamshiri AR, Dummer PM. Evaluation and comparison of occurrence of tooth discoloration after the application of various calcium silicate-based cements: an ex vivo study. J Endod 2016;42:140-144.ArticlePubMed
- 20. Felman D, Parashos P. Coronal tooth discoloration and white mineral trioxide aggregate. J Endod 2013;39:484-487.ArticlePubMed
- 21. Schilke R, Lisson JA, Bauss O, Geurtsen W. Comparison of the number and diameter of dentinal tubules in human and bovine dentine by scanning electron microscopic investigation. Arch Oral Biol 2000;45:355-361.ArticlePubMed
- 22. Kato MT, Hannas AR, Leite AL, Bolanho A, Zarella BL, Santos J, Carrilho M, Tjäderhane L, Buzalaf MA. Activity of matrix metalloproteinases in bovine versus human dentine. Caries Res 2011;45:429-434.ArticlePubMedPDF
- 23. Camargo MA, Marques MM, de Cara AA. Morphological analysis of human and bovine dentine by scanning electron microscope investigation. Arch Oral Biol 2008;53:105-108.ArticlePubMed
- 24. Fahmy SH, Hassanien EE, Nagy MM, El Batouty KM, Mekhemar M, Fawzy El Sayed K, Hassanein EH, Wiltfang J, Dörfer C. Investigation of the regenerative potential of necrotic mature teeth following different revascularisation protocols. Aust Endod J 2017;43:73-82.ArticlePubMedPDF
- 25. Iwaya SI, Ikawa M, Kubota M. Revascularization of an immature permanent tooth with apical periodontitis and sinus tract. Dent Traumatol 2001;17:185-187.ArticlePubMedPDF
- 26. Sabrah AH, Yassen GH, Spolnik KJ, Hara AT, Platt JA, Gregory RL. Evaluation of residual antibacterial effect of human radicular dentin treated with triple and double antibiotic pastes. J Endod 2015;41:1081-1084.ArticlePubMed
- 27. Ruparel NB, Teixeira FB, Ferraz CC, Diogenes A. Direct effect of intracanal medicaments on survival of stem cells of the apical papilla. J Endod 2012;38:1372-1375.ArticlePubMed
- 28. Marconyak LJ Jr, Kirkpatrick TC, Roberts HW, Roberts MD, Aparicio A, Himel VT, Sabey KA. A comparison of coronal tooth discoloration elicited by various endodontic reparative materials. J Endod 2016;42:470-473.ArticlePubMed
- 29. Lenherr P, Allgayer N, Weiger R, Filippi A, Attin T, Krastl G. Tooth discoloration induced by endodontic materials: a laboratory study. Int Endod J 2012;45:942-949.ArticlePubMed
- 30. Marin PD, Heithersay GS, Bridges TE. A quantitative comparison of traditional and non-peroxide bleaching agents. Endod Dent Traumatol 1998;14:64-67.ArticlePubMed
- 31. Guimarães BM, Tartari T, Marciano MA, Vivan RR, Mondeli RF, Camilleri J, Duarte MA. Color stability, radiopacity, and chemical characteristics of white mineral trioxide aggregate associated with 2 different vehicles in contact with blood. J Endod 2015;41:947-952.ArticlePubMed
- 32. Możyńska J, Metlerski M, Lipski M, Nowicka A. Tooth discoloration induced by different calcium silicate-based cements: a systematic review of in vitro studies. J Endod 2017;43:1593-1601.ArticlePubMed
- 33. Vallés M, Roig M, Duran-Sindreu F, Martínez S, Mercadé M. Color stability of teeth restored with biodentine: a 6-month in vitro study. J Endod 2015;41:1157-1160.ArticlePubMed
- 34. Marciano MA, Costa RM, Camilleri J, Mondelli RF, Guimarães BM, Duarte MA. Assessment of color stability of white mineral trioxide aggregate angelus and bismuth oxide in contact with tooth structure. J Endod 2014;40:1235-1240.ArticlePubMed
- 35. Marciano MA, Duarte MA, Camilleri J. Dental discoloration caused by bismuth oxide in MTA in the presence of sodium hypochlorite. Clin Oral Investig 2015;19:2201-2209.ArticlePubMedPDF
REFERENCES
Tables & Figures
REFERENCES
Citations

- Impact of Biodentine Placement on Fracture Resistance and its Influence on Discoloration with Different Scaffolds
Evren Sarıyılmaz, Öznur Sarıyılmaz, Burak Çarıkçıoğlu, Gülşah Uslu, Raif Alan
Journal of Endodontics.2025; 51(9): 1199. CrossRef - Effect of pH on the solubility and volumetric change of ready-to-use Bio-C Repair bioceramic material
Luana Raphael da SILVA, Jader Camilo PINTO, Juliane Maria GUERREIRO-TANOMARU, Mário TANOMARU-FILHO
Brazilian Oral Research.2024;[Epub] CrossRef - Efficacy of Potassium Iodide and Glutathione for Correlation of Dentin Discoloration Caused by Silver Diamine Fluoride
Mahsa Samani, Hamid Majzoub, Faramarz Zakavi, Ayyub Mojaddami
Cureus.2024;[Epub] CrossRef - Intracanal medicaments and coronal sealing materials influence on root fracture resistance and coronal discoloration: An in vitro study
Rasoul Sahebalam, Marzie Boskabady, Maryam Naghavi, Samira Dehghanitafti
Saudi Endodontic Journal.2024; 14(2): 199. CrossRef - Potential Crown Discoloration Induced by the Combination of Various Intracanal Medicaments and Scaffolds Applied in Regenerative Endodontic Therapy
NB Altun, A Turkyilmaz
Nigerian Journal of Clinical Practice.2024; 27(7): 897. CrossRef - Evaluation of the effectiveness of different treatment approaches in preventing coronal discoloration caused by regenerative endodontic treatment
Melis Oya Ateş, Zeliha Uğur Aydın
Clinical Oral Investigations.2023; 27(8): 4595. CrossRef - Evaluation of the Effectiveness of Laser‐Assisted Bleaching of the Teeth Discolored due to Regenerative Endodontic Treatment
Noushin Shokouhinejad, Mehrfam Khoshkhounejad, Fatemeh Hamidzadeh, Murilo Baena Lopes
International Journal of Dentistry.2022;[Epub] CrossRef - Effectiveness of Teeth Whitening after Regenerative Endodontics Procedures: An In Vitro Study
Irini Fagogeni, Joanna Metlerska, Tomasz Falgowski, Maciej Górski, Mariusz Lipski, Alicja Nowicka
Journal of Clinical Medicine.2022; 11(23): 7016. CrossRef - Microstructure and color stability of calcium silicate-based dental materials exposed to blood or platelet-rich fibrin
Noushin Shokouhinejad, Ibrahim Abu Tahun, Shima Saber Tahan, Fatemeh Mohandes, Mohammad H. Nekoofar, Paul M. H. Dummer
Clinical Oral Investigations.2022; 27(3): 1193. CrossRef - Spectrophotometric analysis of internal bleaching of traumatized teeth with coronal discoloration following regenerative endodontic procedures
Jaqueline Lazzari, Walbert Vieira, Vanessa Pecorari, Brenda Paula Figueiredo de Almeida Gomes, José Flávio Affonso de Almeida, Adriana De-Jesus-Soares
Brazilian Journal of Oral Sciences.2021;[Epub] CrossRef - Biological parameters, discolouration and radiopacity of calcium silicate‐based materials in a simulated model of partial pulpotomy
Lilian Vieira Oliveira, Gabriela Leite de Souza, Gisele Rodrigues da Silva, Thamara Eduarda Alves Magalhães, Gabrielle Alves Nunes Freitas, Ana Paula Turrioni, Gabriella Lopes de Rezende Barbosa, Camilla Christian Gomes Moura
International Endodontic Journal.2021; 54(11): 2133. CrossRef - Effect of hydrogel-based antibiotic intracanal medicaments on crown discoloration
Rayan B. Yaghmoor, Jeffrey A. Platt, Kenneth J. Spolnik, Tien Min Gabriel Chu, Ghaeth H. Yassen
Restorative Dentistry & Endodontics.2021;[Epub] CrossRef - The effect of different calcium silicate-based pulp capping materials on tooth discoloration: an in vitro study
Ahmad S. Al-Hiyasat, Dana M. Ahmad, Yousef S. Khader
BMC Oral Health.2021;[Epub] CrossRef - Knowledge, attitudes, and practices of undergraduate students concerning Regenerative Endodontics
Ligia B. da Silva, Mariana Gabriel, Márcia M. Marques, Fernanda C. Carrer, Flávia Gonçalves, Giovanna Sarra, Giovanna L. Carvalho, Ana Armas-Vega, Maria S. Moreira
Minerva Stomatologica.2020;[Epub] CrossRef - Coronal Discoloration Related to Bioceramic and Mineral Trioxide Aggregate Coronal Barrier in Non-vital Mature Teeth Undergoing Regenerative Endodontic Procedures
Mazen Doumani, Mohammad Yaman Seirawan, Kinda Layous, Mohammad Kinan Seirawan
World Journal of Dentistry.2020; 11(1): 52. CrossRef

 KACD
KACD
 ePub Link
ePub Link Cite
Cite

