Articles
- Page Path
- HOME > Restor Dent Endod > Volume 43(4); 2018 > Article
- Review Article Unwanted effects due to interactions between dental materials and magnetic resonance imaging: a review of the literature
-
Sherin Jose Chockattu1
 , Deepak Byathnal Suryakant2
, Deepak Byathnal Suryakant2 , Sophia Thakur1
, Sophia Thakur1
-
Restor Dent Endod 2018;43(4):e39.
DOI: https://doi.org/10.5395/rde.2018.43.e39
Published online: August 30, 2018
1Department of Conservative Dentistry & Endodontics, Bapuji Dental College & Hospital, Davangere, KA, India.
2Department of Conservative Dentistry & Endodontics, Dental College, Regional Institute of Medical Sciences, Imphal, MN, India.
- Correspondence to Sherin Jose Chockattu, MDS. Senior Lecturer, Department of Conservative Dentistry & Endodontics, Bapuji Dental College & Hospital, MCC B-block, MCC, Davangere, KA 570004, India. sherinjose.com@gmail.com
Copyright © 2018. The Korean Academy of Conservative Dentistry
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 6,268 Views
- 55 Download
- 39 Crossref
Abstract
- Magnetic resonance imaging (MRI) is an advanced diagnostic tool used in both medicine and dentistry. Since it functions based on a strong uniform static magnetic field and radiofrequency pulses, it is advantageous over imaging techniques that rely on ionizing radiation. Unfortunately, the magnetic field and radiofrequency pulses generated within the magnetic resonance imager interact unfavorably with dental materials that have magnetic properties. This leads to unwanted effects such as artifact formation, heat generation, and mechanical displacement. These are a potential source of damage to the oral tissue surrounding the affected dental materials. This review aims to compile, based on the current available evidence, recommendations for dentists and radiologists regarding the safety and appropriate management of dental materials during MRI in patients with orthodontic appliances, maxillofacial prostheses, dental implants, direct and indirect restorative materials, and endodontic materials.
INTRODUCTION
REVIEW
Unwanted effects of magnetic resonance imaging (MRI)-dental material interaction
1. Artifact formation in MRI
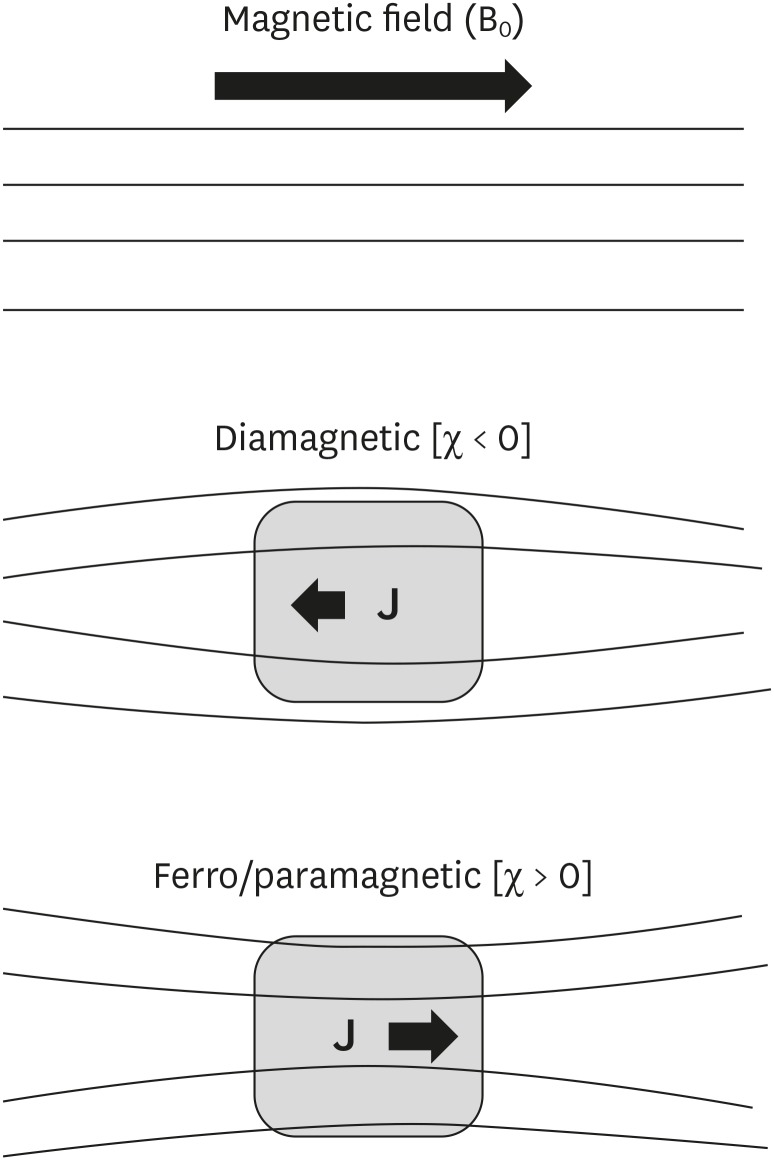
1) Distortion of the static magnetic field (B0) due to differences in the magnetic susceptibility of materials and body tissues
2) Eddy currents
2. Unwanted mechanical (magnetically-induced displacement) effects
3. Unwanted physical effects (radiofrequency heating)
1. Magnetic susceptibility and magnetic permeability
Classification of materials according to their interactions with magnetic fields
| Type of magnetic effect | Effect on applied magnetic field | Magnetic permeability/susceptibility | Significance | Example |
|---|---|---|---|---|
| Diamagnetism | Internal magnetization (polarization) opposes the externally applied field; | µ < 1 (or χ < 0); | Least likely to cause an artifact | All biological tissues; silver (dental amalgam alloy) |
| Magnetic field lines are ‘thinned’ or ‘dispersed’ | Slightly lower permeability than free space; | |||
| Negative susceptibility | ||||
| Paramagnetism | Internal magnetization (polarization) is in the same direction as the externally applied field; | µ > 1 (or χ > 0); | Far less likely to cause an artifact | Vascular stents [46]; dental amalgam |
| Magnetic field lines are ‘concentrated’ in the object | Slightly higher permeability than free space; | |||
| Positive susceptibility | ||||
| Ferromagnetism | Magnetic field lines are ‘concentrated’ in the object; | µ >> 1 (or χ >> 0); | High potential to cause MRI artifacts | Stainless steel |
| Strongly attracted by a magnetic field | High permeability; | |||
| Positive susceptibility |
Classification of materials according to their interactions with magnetic fields.
Classification of materials based on magnetic susceptibility
2. Electrical conductivity of the dental material
3. Mechanical history (tensile strength) of the dental material
4. Imaging sequence used for MRI
Relationship between artifacts and imaging sequence
| MRI sequence | Magnitude of artifact | Reason |
|---|---|---|
| Long echo time; GRE sequences | Most severe artifacts (loss of signal around the material) [8] | Intravoxel dephasing is the predominant cause of signal loss, resulting in a dark or black area around the metal on processed images [48,49]. |
| Shortened echo time and decreased voxel size; SE sequence [49,50] | Best sequence for reducing the severity of susceptibility artifacts (complex spear-shaped artifacts) [8] | Diminished phase shifts in voxel caused by local static magnetic field gradients [80]. |
Summary of unwanted effects due to interactions of dental materials with MRI, according to a literature search (1988–2018)
| No. | Author (year) | Dental material used | MRI specifications/area of interest | Results | Conclusion/recommendation |
|---|---|---|---|---|---|
| 1 | Beau et al. (2017) [51] | Orthodontic brackets (S.S., Ti, ceramic with metal slots); retainers | 1.5 T; 2 scans per patient with empty wax jig & with wax jig including the attachment. | S.S brackets always caused non-interpretability of all anatomic areas (100%). Ti (20%), ceramic brackets with metal slots (17%) and S.S. retainers (87%) caused artifacts in the oral cavity. | Ceramic brackets with metal slots & Ti brackets do not have to removed, based on the scan area; metal fixed retainers are to be removed only in oral cavity scans; S.S. brackets must always be removed before head & neck MRI. |
| [Article in French] | |||||
| 2 | Blankenstein et al. (2017) [52] | 11 test specimens of known permeability (1.003–1.431) | 1.5 T MRI; TSE & gradient-echo sequences of head & neck region. | Steel caused a wide range of artifact sizes (10–74 mm), depending on their permeability. Ti, Co-Cr & ceramic materials produced artifact radii up to 20 mm. | Permeability can be reliably assessed by conventional measurement devices & artifact size can be predicted. Radiologists can decide whether the orthodontic attachments should be removed. |
| 3 | Zhylich et al. (2017) [53] | Orthodontic brackets (S.S., ceramic, ceramic with metal slots); retainers | Head MR scans of 9 regions: sagittal T1-weighted, axial T2-weighted, axial gradient-recalled, axial diffusion-weighted, non-contrast axial MR angiography, & axial fluid-attenuated inversion recovery sequences. | MR images were affected by type of appliance, MR sequence, and location (head region). The maximum image distortion was found with S.S. brackets and molar tubes; minimal distortion occurred with ceramic brackets. | Type of appliance, region imaged, and MR sequence must be considered before imaging is done in patients with fixed orthodontic appliances. |
| 4 | Smeets et al. (2017) [54] | Dental implants of Zr, Ti, and Ti-Zr alloy embedded in gelatin | 3 T MRI; T2-weighted space sequence & T1-weighted volumetric interpolated brain examination technique. | Ti & Ti-Zr alloy induced an extensive signal void in MRI (strong susceptibility — MR signal attenuated up to 14.1 mm from implant); Zr implants were clearly definable with only minor distortion artifacts. | MRI allows excellent image contrast and limited artifacts for Zr implants. CT & CBCT examinations are less affected by artifacts from Ti & Ti-Zr alloy implants than MRI. |
| 5 | Hilgenfeld et al. (2016) [55] | 1 Zr & 4 Ti dental implants were provided with different single crown materials: PFM precious alloy, PFM non-precious alloy, porcelain-fused-to-Zr and monolithic Zr | 3 T MRI; applying SPACE and TSE (2 standard sequence types). | The fewest artifacts were found with the Zr implant combined with a monolithic Zr crown. The Ti implant combined with a single crown framework of non-precious alloys had an unfavorable artifact volume. Smaller artifact volumes were noted for Ti implants with remaining 3 crown materials (PFM precious alloy, porcelain-fused-to-Zr, and monolithic Zr). | Material composition of dental implants provided with single crowns had a profound impact on artifact volume. In comparison with crowns containing cobalt, chromium and tungsten, MRI artifacts are reduced in precious alloy- and Zr-based crowns. |
| 6 | Lan et al. (2016) [56] | Crowns of Co-Cr, Ni-Cr, Ti alloy & pure Ti | 3 T MRI with 6 sequences: T1weighted SE, T2 weighted-inversion recovery, T2 star GRE, T2 weighted-FSE, T1 weighted-fluid attenuate inversion recovery, and T2 weighted-imaging. | Artifacts in the T2 star GRE sequence were significantly wider than those in the other sequences. | The T2 star GRE exhibited the strongest influence on artifacts, whereas the other 5 sequences contributed equally to artifact generation. |
| [Chinese] | |||||
| 7 | Murakami et al. (2016) [24] | 7 metallic dental materials: Al, silver alloy (Ag), type IV gold alloy (Au), gold-palladium-silver alloy (Au-Pd-Ag), Ti, Ni-Cr & Co-Cr alloy | Sequences included GRE, FSE, GRASS, SPGR, FSPGR, FIESTA & EPI (axial/sagittal planes). | Artifact volumes: FSE-T1/FSE-T2 < FSPGR/SPGR < GRASS/GRE < FIESTA < EPI. For all scan sequences, artifact volumes for Au, Al, Ag & Au-Pd-Ag were significantly smaller than other materials (artifact volume size: Ti < Ni-Cr < Co-Cr. Artifact-specific shape (cubic sample) depended on scan plane (i.e., circular pattern for the axial plane & ‘clover-like’ for the sagittal plane). | Availability of standardized information on artifact size & configuration during MRI will enhance the diagnosis in patients with metallic compounds. |
| 8 | Xu et al. (2015) [57] | 3 metals and 2 ceramics, fabricated to same size and thickness of incisor crown | Different sequences of 3 MRI field strengths: 0.35, 1.5 & 3 T–T1WI & T2WI images. | No artifacts were found for Zr crowns; for casting ceramic, they were minimal. All dental precious metal alloys, Ni-Cr alloy dental porcelain, & Co-Cr ceramic alloy had varying degrees of artifacts. | Zr & casting ceramics presented almost no or faint artifacts. By contrast, precious metal alloys, Ni-Cr alloy dental porcelain and Co-Cr ceramic alloy displayed MRI artifacts. The artifact area increased with the strength of the magnetic field. |
| [Article in Chinese] | |||||
| 9 | Cortes et al. (2015) [58] | Ni-Cr metal-ceramic restorations (i.e., dental crowns & fixed bridges) and cylindrical reference specimens | 1.5 & 3 T MRI scanners; GRE, SE & UTE pulse sequences. | A significant correlation was found between TE and artifact area in GRE images. Higher receiver bandwidth significantly reduced artifact area in SE images. UTE images yielded smallest artifact area at 1.5 T. Significant differences were found in the mean artifact area between 1.5 & 3 T images and between images from GRE & SE pulse sequences. | A significant correlation found between TE and artifact area in GRE images. It is possible to compensate for the effect of higher field strength on MRI artifacts by setting optimized pulse sequences for scanning patients with metal-ceramic restorations. |
| 10 | Shalish et al. (2015) [59] | 2 commonly used fixed retainers: Twistflex & Ortho Flex Tech retainers. | 1.5 to 3 T; SE sequence; T1- & T2-weighted sequence. | Ortho Flex Tech retainers caused no distortion. Twistflex retainers caused distortion (46%) in areas close to the retainer (tongue, jaws). Maxillary fixed retainers & maxillary-mandibular fixed retainer combination further increased distortion. Greater distortion was seen with 3 T magnetic fields & T1-weighted SE sequences. | Removal of Ortho Flex Tech retainer is unnecessary before MRI. Removal of Twistflex should be considered if MRI scans are performed to diagnose areas close to fixed retainers, when 3 T magnetic fields and T1-weighted sequences are used, and when both maxillary & mandibular fixed retainers are present. |
| 11 | Zachriat et al. (2015) [60] | Ceramic brackets & S.S. brackets | 1.5 T MRI of head & neck region; different types of MR sequences (EPI, TSE and TSE-WARP, GRE). | In vitro: Artifact radii of 1.12 (ceramic brackets) and 7.4 cm (ferromagnetic steel brackets). WARP reduced artifacts by 32.7%. | In vitro measurements allow estimation of in vivo artifact size. Orthodontic appliances may often remain intraorally when performing MRI. WARP showed more significant effect in vitro than in vivo. |
| In vivo: EPI sequence for brain imaging was not analyzable. The TSE sequence of the brain had no artifacts except for the nasal cavity. The TSE sequence of the cervical spine had severe artifacts in the midface region. The GRE sequence was more susceptible to artifacts than TSE. | |||||
| 12 | Wylezinska et al. (2015) [61] | S.S. arch wire, brackets & molar bands; appliances/reinforcement with Ni/Ti alloys. | 0.5 T scanner using standard spin & GRE sequences. Craniofacial region, with special interest in soft palate and velopharyngeal wall (real-time speech imaging) & TMJ & pituitaries (anatomical imaging). | The most extensive effects were associated with S.S. arch wire, particularly if combined with S.S. brackets & S.S. molar bands (diagnostic quality severely degraded). All non-metallic, non-metallic with Ni/Cr reinforcement, or Ni/Ti alloys appliances were of little concern. | Appliances manufactured from S.S. cause extensive artifacts, which may render the image non-diagnostic. The presence and type of orthodontic appliances should be always included in patient's screening, so risks of artifacts can be assessed prior to imaging. Although risks to patients with fixed orthodontic appliances at 1.5 T are low, their secure attachment should be confirmed. |
| 13 | Blankenstein et al. (2015) [62] | 16 orthodontic small-device and wire specimens made of different steel and Ti or Co-Cr alloys | SE and GRE sequences at 1.5 & 3 T. | Artifact formation depends on material properties (specimen size, crystalline structure, processing) & MRI specifications (main field strength, sequence type). Artifact radii ranged from 14 mm (SE, 1.5 T) to 51 mm (GRE, 3 T). No artifacts at 1.5 T around Ti & Co-Cr specimens; the same observation was made with 1 of the steel grades. | Artifact size cannot be predicted merely from the designation ‘steel’ or from crystalline structure. Relevant is the magnetic permeability (or susceptibility) of the final products, which is not disclosed by manufacturers, and it cannot be measured in fixed intraoral appliances. Some steel devices can remain in situ without triggering adverse consequences. |
| 14 | Beau et al. (2015) [23] | 60 patients requiring head MRI scan for medical reasons were given one of 4 types of fixed attachments: S.S., Ti, ceramic brackets with metal slots, & S.S. retainers | Each patient had 2 scans at 1.5 T; the 4 areas under investigation were maxillary sinus, oral cavity, TMJ, & posterior cerebral fossa. | S.S. brackets always caused non-interpretability of all anatomic areas (100%). Ti brackets, ceramic brackets with metal slots, and S.S. retainers caused artifacts in the oral cavity only (for 20%, 16.65%, and 86.65% of subjects). | Ceramic brackets with metal slots & Ti brackets do not always have to be removed before head & neck MRI, depending on the investigation area. Metal fixed retainers are to be removed if the oral cavity itself is under investigation. S.S. brackets are to always be removed before head & neck MRI. |
| 15 | Duttenhoefer et al. (2015) [63] | Ti & Zr implants embedded in 10% (w/v) gelatin phantoms (MRI), or post-implantation (micro-CT) | 3 T MRI; T1-weighted TSE & T2-weighted TSE sequences. | Post-implantation, while Ti implants induced a strong B0-field distortion resulting in extensive signal voids, Zr implants were clearly depicted with only minor distortions. | Excellent contrast, limited artifacts, radiation-free and accurate implant assessment indicate that MRI is a valuable imaging alternative for Zr implants. |
| 16 | Fang et al. (2014) [64] | 6 casting alloy post & cores (Zr post & core – control). All 7 types of post & cores were of same the size & shape | T1-weighted SE imaging (SE-T1WI), T2-weighted turbo spin-echo imaging (TSE-T2WI), and DWI. | Co-Cr alloy post & core generated severe artifacts, whereas Au-Pd alloy post & core generated no obvious artifacts, & no difference was seen between the Zr & Au-Pd alloy post & cores. Pure Ti alloy post & core produced mild artifacts. Post & cores of Ti, Ni-Cd, & Au-Pt alloys generated moderate artifacts. | Different metal post & cores had different influences on MRI. With exception of that generated by Co-Cr alloy, the artifacts generated by single-alloy post & core did not influence normal head & neck imaging. |
| [Article in Chinese] | |||||
| 17 | Sinkiewicz et al. (2013) [7] | Orthodontic appliances | - | - | This review article gave recommendations for the removal or retention of orthodontic appliances during MR imaging. |
| 18 | Tymofiyeva et al. (2013) [12] | A series of standard dental materials was studied & their magnetic susceptibility was estimated | 1.5 T MRI system using SE and GRE pulse sequences. | Materials were classified as fully compatible (material can be present even in tooth of interest), compatible I, & non-compatible (material should not be present in patient's mouth for any dental MRI applications). | A material classification that complies with the standard grouping of materials according to their magnetic susceptibility can serve as a guideline in future dental MRI research. |
| 19 | Taniyama et al. (2010) [65] | Non-magnetic metal (type-4 gold alloy ring) that was intact or cut | 2 T MRI; excitation RF field was along the x-axis, with RF-receiver coil in the y-z plane. T1 (spin-lattice relaxation time)-weighted images. | For the intact gold ring, a portion around the ring disappeared. It was nearly restored with a cut ring. Artifacts appeared when the circumferential surface of the ring was placed perpendicular to the RF field of MRI. However, in other directions or with a cut ring, the artifact disappeared. | This demonstrated the characteristics and cause of artifacts by non-magnetic dental metals. An alternating magnetic field was shown to induce a surface current that interfered with the field on the continuous gold ring. |
| 20 | Costa et al. (2009) [27] | Retrospective study of 1,200 medical records of epileptics who underwent MRI. 70 MR images with artifacts were retrieved & reviewed | MRI acquisition parameters were: 1) sagittal T1 SE; 2) coronal images, T1-weighted inversion recovery; 3) axial images, T1-weighted GRE. | The artifact image plane was given a score of 0 or 1 (0 = distinguishable for diagnosis; 1 = not distinguishable). 78% of artifacts were caused by orthodontic appliances (the highest scores in all planes), followed by dental Ti implants (18%) & metallic crowns (4%). | It is difficult to avoid the effects of metallic artifacts in maxillofacial regions on brain scans. Removing the metallic parts of orthodontic appliance should ensure diagnostically useful scans. |
| Metallic objects were dental (Au) crowns, dental Ti implants, & metallic orthodontic appliances (bands, brackets, arch wires) | a) T1-weighted GRE; b) FLAIR. | ||||
| 21 | Hunt et al. (2009) [18] | - | - | - | In this letter to the editor, the authors contemplated the use of Essix trays to fit over bonded canine-to-canine retainers or other fixed attachments prior to MRI to prevent appliance dislodgement. They also suggested the use of TMA wire for fixed retainers. |
| 22 | Elison et al. (2008) [66] | 10 subjects received 5 consecutive cranial MR scans. A control scan was conducted with Essix trays fitted over the maxillary & mandibular teeth. 4 experimental head MR scans were done with plastic, ceramic, Ti, & S.S. brackets incorporated into Essix tray material | Each MR scan consisted of 4 sequences: sagittal T1-weighted SE (T1 sagittal), axial T2-weighted SE (T2 axial), GRE & DWI. | Statistically significant difference between the distortion scores of S.S. brackets & those of other experimental MR scans. | Plastic, ceramic & Ti brackets caused minimal distortion of cranial MR images. However, S.S. brackets caused significant distortion (cranial regions were non-diagnostic). The areas with the most distortion were the mandible body, hard palate, base of tongue, globes, nasopharynx & frontal lobes. The closer the S.S. appliance was to a specific anatomic region, the greater MR image distortion was found. |
| 23 | Hu et al. (2008) [17] | - | - | - | This review article concluded that FPDs produced artifacts in MRI, thus reducing image quality when patients with a metallic prosthesis in mouth undergo head & neck MRI. However, these FPDs cannot be removed arbitrarily. |
| [Article in Chinese] | |||||
| 24 | Destine et al. (2008) [28] | 1 pre-fabricated magnetic keeper and 4 clinical dental alloys (Au-Ag-Pa, casting Au alloy type 3, Co-Cr, Au porcelain alloy); in total, 2 metal crowns & 5 magnetic keepers were analyzed | 1.5 T MRI apparatus; in axial, coronal, & sagittal planes; T1-weighted SE sequence (TR/TE) & T2-weighted TSE sequence were used. | Co-Cr showed greater signal intensity, up to 40 mm in coronal T2WI images & 70 mm in axial T1WI images for the magnetic keeper. The signal intensities of Au-Ag-Pa & casting Au alloy type 3 were similar to the control. The signal intensity of Au-porcelain alloy was different from the control at 0 mm & 5 mm in coronal T1, T2WI & in sagittal T1WI at 0 mm. | The artifacts generated by the magnetic keeper and Co-Cr crown when they were used in a second molar could disturb MR images of the TMJ. |
| 25 | Starčuková et al. (2008) [34] | Magnetic susceptibility, electrical conductivity and artifacts were evaluated for 45 cylindrical standardized samples of dental alloys and amalgam. | Artifact sizes were measured in SE and GRE images at 1.5 T according to the standards of the American Society for Testing and Materials. | Short-echo-time GRE imaging is possible even at very close distances from dental devices made of amalgam, precious alloys & Ti alloys. Ni-Cr & Co-Cr artifacts were still acceptable, but large restorations of Al-bronzes preclude orofacial imaging. Influence of electrical conductivity on artifact size was negligible. | Dental materials differ considerably in their magnetic susceptibility, electrical conductivity and artifacts. For dental devices, magnetic susceptibility differences are of little clinical importance for diagnostic SE/GRE imaging of the neck and brain, but are significant for orofacial imaging. MRI is possible even close to dental devices if they are made of dental materials with low magnetic susceptibility. Not all materials in current use meet this requirement. |
| Magnetic susceptibility and electrical conductivity were determined. | |||||
| 26 | Blankenstein et al. (2006) [67] | 5 standard dental magnet attachments with volumes of 6.5–31.4 mm3: NdFeB magnet with open magnetic field, NdFeB magnet with closed magnetic field, SmCo magnet with open magnetic field, S.S. keeper (AUM-20) & PdCo piece | 1.5 T & 3 T MRI; gradient-echo and T1- & T2-weighted SE sequence. | In gradient-echo images, artifacts were substantially larger and symmetrically adjusted around the object. Areas with total signal loss were mushroom-like. In SE images, the signal loss areas were smaller, but not centered. Different ferromagnetic attachments had no clinically relevant influence on the signal loss in either 1.5 T or 3 T MRI. | Ferromagnetic materials used in dentistry are not intraorally standardized. To ensure that the area of interest is not affected by artifacts, the maximum extent of the signal loss area should be assumed: a radius of up to 7 cm in 1.5 & 3 T MRI by T1 & T2 sequences, and a radius of up to 10 cm in T2 sequences. To decide whether magnet attachments have to be removed before MRI, physicians should consider both the intact retention of keepers and safety distance between ferromagnetic objects and the area of interest. |
| [Article in German] | |||||
| 27 | Hubálková et al. (2006) [16] | - | - | - | This review article concluded that MRI causes movement or heating of metal objects (with positive magnetic properties) present in the body, which can lead to health risks. The safety & MRI compatibility of dental alloys must always be considered prior to MRI. |
| 28 | Harris et al. (2006) [68] | A patient undergoing orthodontic treatment who required repeated MRI scans on a regular basis | - | S.S. & other metallic orthodontic appliances created substantial artifacts & obliterated details in the facial area. Ceramic brackets & directly-bonded metal tubes did not affect MRI scan diagnostic quality. | The authors concluded that metallic orthodontic appliances in the head & neck region can distort MR images, thus reducing their value. Aesthetic brackets (no metal components and arch wires removed) do not distort MRI scans. |
| 29 | Shafiei et al. (2003) [32] | 11 dental casting or implant materials were imaged | 1.5 T MRI apparatus with 3 different sequences. | A variety of artifacts with different magnitudes was observed. Only 1 sample, composed mainly of Pa, In, & antimony (Sb), showed no artifacts in any imaging sequences. | Selecting specific dental casting alloys according to their elemental compositions can minimize metal artifacts in MRI; however, Ti alloys currently pose a problem with respect to causing MRI artifacts. |
| 30 | Okano et al. (2003) [69] | MR imaging was performed in 20 TMJs before and after insertion of 6 kinds of orthodontic appliances (ceramic/metal brackets; directly-bonded tube/band tube; +/− S.S. arch wires) | - | For disk position, diagnostic accuracy was 70%–80% (ceramic/metal brackets with no S.S. arch wires), & 60%–70% with S.S. arch wires. For condylar configurations, accuracy was 80% (ceramic brackets & directly-bonded tube), 55% (metal brackets & directly-bonded tube), 40% (metal brackets & band tube), reduced to 10%–40% in the presence of S.S. arch wires. No significant changes were found in the condylar head marrow signals. | MRI should preferably be performed in orthodontic patients by using ceramic brackets in the front teeth & direct bonding tubes in molars, while removing arch wires. |
| 31 | Hubálková et al. (2002) [70] | 15 dental alloys, 4 dental implants, 1 surgical splint & 2 wires for fixation of maxillofacial fractures | - | Artifacts were significant: for surgical splints, a spherical artifact of 55 mm in diameter; for wires, up to 22 mm; & for the dental blade implant, a 28 × 20 mm artifact. | Although the selected dental appliances are safe when present in patients undergoing MRI, artifacts can substantially influence MRI results. |
| 32 | Savane et al. (2001) [71] | Ti implants | 1.5 T MR unit, with 2 commonly used sequences (SE,GRE) | Minor artifacts, without distortions | In order to minimize ‘ghost images’, Ti and its alloys should be an alternative. |
| [Article in French] | |||||
| 33 | Abbaszadeh et al. (2000) [25] | Dental Au, amalgam, S.S., Ti, Ag-Pa, & vitallium | T1-weighted MR imaging. | All metallic objects produced artifacts. Artifacts were most pronounced in the central plane of the object. Au produced the greatest artifacts; amalgam produced the least. | Because metals commonly used in the maxillofacial region produce artifacts on MR images, avoidance measures should be used to minimize these artifacts. |
| 34 | Tetsumura et al. (1999) [72] | Minute metallic particles deposited during surgery may cause artifacts — 4 types of cutting instruments were used to cut an extracted tooth: a diamond bur attached to a rotor handpiece, a steel bur & bone bur attached to a micromotor handpiece & a bone file | 1.5 T; 6 MR sequences: SE, 2 TSE sequences, fast low angle short, turbo gradient SE, turbo inversion recovery sequences. | MR artifacts seen in tooth samples using the bone bur & bone file, but not the diamond & steel burs. | Artifacts seen on postoperative MRI were derived from minute metal particles from the bone bur or file used for condylar arthroplasty. Metal artifacts should be considered when interpreting postoperative MR images. |
| 35 | Borris et al. (1999) [73] | Large ferromagnetic MRI artifacts were seen in the area of a previous mandibular osteotomy | - | MRI revealed multiple non-uniform halo-appearing teardrop-shaped areas associated with the mandibular ramus in the osteotomy area, visible in axial & coronal views. Surgical exploration revealed several minute hard & soft tissue specimens (foreign bodies). | Even tiny particles distort MR images leading to halo artifacts. Surgeons must be aware of foreign bodies implanted during surgery, and recognize their appearance. Dental restorations usually do not cause artifacts. |
| 36 | Devge et al. (1997) [44] | Implants from the Brånemark System were tested | The ferromagnetic properties of implant materials are seldom described by the manufacturer. Important factors are alloy composition, size & shape of the metallic material, and its position in body. | Artifacts caused by implants were minor and did not jeopardize scan evaluation. However, magnet keepers attached to implants caused major artifacts. | Magnet keepers attached to implants must be removed before an implant patient is referred for MRI examination |
| 37 | Behr et al. (1996) [74] | Cylindrical samples of 13 alloys & 14 pure substances (in plaster & water-filled acrylic resin phantom-representing disc & TMJ condyle were investigated) | SE & GRE sequence. | Metallic artifacts appeared on SE technique as distortions, and on gradient-echo technique signal loss could be observed. Precious alloys were diamagnetic. Non-precious alloys investigated were paramagnetic. | Paramagnetic alloys produce clinically relevant artifacts. |
| 38 | Beuf et al. (1994) [26] | Cylindrical dental alloy samples incorporating gold, silver, and palladium (placed in a Pyrex beaker filled with distilled water) | 0.13 T using 2-dimensional Fourier transformation and projection reconstruction at 360° imaging methods. | Only palladium-based alloys were detected to be paramagnetic. One of the silver-based alloys did not induce detectable distortion because its susceptibility was very close to that of distilled water. | Use of this material may be recommended for applications involving MRI evaluation. |
| 39 | Iimuro (1994) [75] | Specimens of each material were prepared as spheres & cylinders. Sphere samples with diameters of 1, 2, and 3 mm and 4 mm cylinders of 0.2, 0.3, 0.4, 0.6, 0.8 diameter and 1 mm height were prepared | 0.2 T; 3 sequences: short SE (TR-300, TE-38), long SE (TR-500, TE-110) and GRE (TR-200, TE-23, flip angle 60) were used. Images were taken in the coronal, sagittal & transverse planes. | During MRI, artifacts were not caused by the magnet itself, but by the S.S. keeper (ferromagnetic). Short & long SE sequences resulted in the same artifact range (distortion; further from the specimen, distortion was attenuated); the gradient-echo sequence caused a larger image artifact (signal loss/blackout). The image around the most severely deformed area was quite distorted, but the structures could be distinguished. | The higher the magnetic permeability, the greater the artifact produced. The size and volume of the material directly influence the artifact produced. Artifact size can be attenuated by the sequence used to obtain images. In vitro and in vivo results suggest that even in patients with a magnetic attachment system, MRI is the diagnostic method of choice. Possible solutions to reduce the artifact range are to find alternative keeper materials with a lower magnetic permeability; or to design the keeper in such a manner that it can be removed easily. |
| 40 | Oikarinen et al. (1993) [76] | 4 samples of different sizes of fractured tooth crown, pieces of amalgam, glass, asphalt, composite, dry wood, and stone (embedded in soft tissue) | 1 T; T1 and T2 weighted and proton-density images. | MRI was the least suitable imaging method, as particles with a metallic content gave rise to artifacts. Foreign body particles in soft tissue were better defined in form & size with CT & ultrasonography than with MRI or plain radiography. | When plain radiographs, history, and clinical examination fail to reveal the presence of superficial foreign bodies, ultrasonography or CT can serve as an alternative method that is preferable to MRI. |
| 41 | Laurell et al. (1989) [77] | 8 types of prosthetic magnet keepers of the disc and bar type | 1.5 T, with partial saturation pulse sequence. | Image artifacts present in all 8 samples (160–280 mm diameter). Artifacts obliterated vital cranio-cervical areas. For bar keepers & Jackson disc keepers, artifacts partially/totally obliterated eye & brain images. Other disc keepers degraded eye images, but not brain or cervical spine images. | The ferromagnetic potential of magnetic keepers caused sufficient localized alterations of the magnetic field, leading to signal loss. Patients with magnetic keepers requiring comprehensive head & neck MRI must have them removed. |
| 42 | Sadowsky et al. (1988) [78] | 5 patients with fixed appliances in maxillary & mandibular arches undergoing MRI scans of brain & TMJ | T1-weighted scan; transverse multi-echo sequence of the brain. | Orthodontic appliances produced MR artifacts in the facial region (mouth & maxillary sinus). The frontal & temporal lobes of the brain were most affected, but the degree of the artifact varied from patient to patient. Artifacts were not severe enough to alter the diagnostic scan quality. On TMJ scans, no degradation was detected. | Phantom studies indicated that orthodontic arch wires increased distortion & artifacts. All banded & bonded attachments should be checked for firm attachment to the teeth or passively ligated with elastic chains for added safety. Eliminating all removable components of appliances (arch wires) ensures a diagnostic scan. Complete removal of metallic appliances is not needed unless the region of interest is close to the mouth. |
1. Orthodontic materials: the issue of artifacts
When firmly bonded and carefully ligated, fixed orthodontic appliances are safe for use in MRI scanners. Steel retainer bonds should be checked prior to the scan to ensure their attachment.
Leaving a non-ferromagnetic wire in place keeps the brackets together even if the enamel bond fails.
If the dento-alveolar region is to be studied, the plane of the scan should be altered to avoid the site of metal devices. If not feasible, the orthodontic brackets and wires should be removed [7,21].
Artifacts may not always interfere with the diagnosis, especially when they are present in areas that are not of interest (Table 6) [22].
Recommendations for the removal of orthodontic appliances based on the type of material
2. Orthodontic materials: issues regarding physical and mechanical effects
3. Maxillofacial prostheses
Radiofrequency-induced heating of magnetic dental attachments during 3 T MRI should not pose a risk to patients.
Since the magnetically-induced torque was within the acceptable limits, but the deflection forces exceeded those limits, ferromagnetic devices should ideally be removed from the oral area before MRI. Since this may not always be possible, for safety purposes, the fixation (cement degradation) of such devices should be inspected before and after MRI [22].
4. Dental implants
5. Direct restorative materials
1) Glass-ionomer cements (GIC)
2) Composite resin
3) Amalgam
6. Indirect restorative materials
1) Gold crowns
2) Ceramic and metal-ceramic crowns
7. Endodontic materials
CONCLUSIONS
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Deepak BS.
Data curation: Chockattu SJ.
Formal analysis: Chockattu SJ.
Investigation: Chockattu SJ.
Methodology: Chockattu SJ.
Project administration:
Resources: Chockattu SJ.
Software: Chockattu SJ.
Supervision: Thakur S.
Validation: Thakur S.
Writing - original draft: Chockattu SJ.
Writing - review & editing: Deepak BS.
- 1. White SC, Pharoah MJ. Oral Radiology: principles of Interpretation. 7th ed. St. Louis (MO): Elsevier; 2014. Chapter 14.
- 2. Tutton LM, Goddard PR. MRI of the teeth. Br J Radiol 2002;75:552-562.ArticlePubMed
- 3. Yilmaz S, Misirlioglu M. The effect of 3 T MRI on microleakage of amalgam restorations. Dentomaxillofac Radiol 2013;42:20130072.ArticlePubMedPMC
- 4. Gray CF, Redpath TW, Smith FW, Staff RT. Advanced imaging: magnetic resonance imaging in implant dentistry. Clin Oral Implants Res 2003;14:18-27.ArticlePubMedPDF
- 5. Czervionke LF, Daniels DL, Wehrli FW, Mark LP, Hendrix LE, Strandt JA, Williams AL, Haughton VM. Magnetic susceptibility artifacts in gradient-recalled echo MR imaging. AJNR Am J Neuroradiol 1988;9:1149-1155.PubMedPMC
- 6. Fache JS, Price C, Hawbolt EB, Li DK. MR imaging artifacts produced by dental materials. AJNR Am J Neuroradiol 1987;8:837-840.PubMedPMC
- 7. Sinkiewicz D. MRI scan hazard. Br Dent J 2013;214:376.ArticlePDF
- 8. Tymofiyeva O, Vaegler S, Rottner K, Boldt J, Hopfgartner AJ, Proff PC, Richter EJ, Jakob PM. Influence of dental materials on dental MRI. Dentomaxillofac Radiol 2013;42:20120271.ArticlePubMedPMC
- 9. Kress B, Buhl Y, Anders L, Stippich C, Palm F, Bähren W, Sartor K. Quantitative analysis of MRI signal intensity as a tool for evaluating tooth pulp vitality. Dentomaxillofac Radiol 2004;33:241-244.ArticlePubMed
- 10. Tymofiyeva O, Rottner K, Gareis D, Boldt J, Schmid F, Lopez MA, Richter EJ, Jakob PM. In vivo MRI-based dental impression using an intraoral RF receiver coil. Concepts Magn Reson Part B Magn Reson Eng 2008;33B:244-251.Article
- 11. Tymofiyeva O, Schmid F, von Kienlin M, Breuer FA, Rottner K, Boldt J, Richter EJ, Jakob PM. On precise localization of boundaries between extended uniform objects in MRI: tooth imaging as an example. MAGMA 2011;24:19-28.ArticlePubMedPDF
- 12. Tymofiyeva O, Rottner K, Jakob PM, Richter EJ, Proff P. Three-dimensional localization of impacted teeth using magnetic resonance imaging. Clin Oral Investig 2010;14:169-176.ArticlePubMedPDF
- 13. Tymofiyeva O, Boldt J, Rottner K, Schmid F, Richter EJ, Jakob PM. High-resolution 3D magnetic resonance imaging and quantification of carious lesions and dental pulp in vivo . MAGMA 2009;22:365-374.ArticlePubMedPDF
- 14. Idiyatullin D, Corum C, Moeller S, Prasad HS, Garwood M, Nixdorf DR. Dental magnetic resonance imaging: making the invisible visible. J Endod 2011;37:745-752.ArticlePubMedPMC
- 15. Bracher AK, Hofmann C, Bornstedt A, Boujraf S, Hell E, Ulrici J, Spahr A, Haller B, Rasche V. Feasibility of ultra-short echo time (UTE) magnetic resonance imaging for identification of carious lesions. Magn Reson Med 2011;66:538-545.ArticlePubMedPDF
- 16. Hubálková H, La Serna P, Linetskiy I, Dostálová T. Dental alloys and magnetic resonance imaging. Int Dent J 2006;56:135-141.ArticlePubMed
- 17. Hu YY, Wei B. Research progress of the MRI artifacts produced by fixed partial dentures. Shanghai Kou Qiang Yi Xue 2008;17:441-443.PubMed
- 18. Hunt HL. Orthodontic appliances and MRIs. Am J Orthod Dentofacial Orthop 2009;135:7.ArticlePubMed
- 19. Swash M, Glynn M. Hutchison's clinical methods. 21st ed. New York (NY): Saunders Elsevier; 2007. Chapter 22.
- 20. Görgülü S, Ayyildiz S, Kamburoglu K, Gökçe S, Ozen T. Effect of orthodontic brackets and different wires on radiofrequency heating and magnetic field interactions during 3-T MRI. Dentomaxillofac Radiol 2014;43:20130356.ArticlePubMedPMC
- 21. Cross B, Beckett H. Unwanted effects. Br Dent J 2006;201:325.ArticlePDF
- 22. Hasegawa M, Miyata K, Abe Y, Ishii T, Ishigami T, Ohtani K, Nagai E, Ohyama T, Umekawa Y, Nakabayashi S. 3-T MRI safety assessments of magnetic dental attachments and castable magnetic alloys. Dentomaxillofac Radiol 2015;44:20150011.ArticlePubMedPMC
- 23. Beau A, Bossard D, Gebeile-Chauty S. Magnetic resonance imaging artefacts and fixed orthodontic attachments. Eur J Orthod 2015;37:105-110.ArticlePubMed
- 24. Murakami S, Verdonschot RG, Kataoka M, Kakimoto N, Shimamoto H, Kreiborg S. A standardized evaluation of artefacts from metallic compounds during fast MR imaging. Dentomaxillofac Radiol 2016;45:20160094.ArticlePubMedPMC
- 25. Abbaszadeh K, Heffez LB, Mafee MF. Effect of interference of metallic objects on interpretation of T1-weighted magnetic resonance images in the maxillofacial region. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000;89:759-765.ArticlePubMed
- 26. Beuf O, Lissac M, Crémillieux Y, Briguet A. Correlation between magnetic resonance imaging disturbances and the magnetic susceptibility of dental materials. Dent Mater 1994;10:265-268.ArticlePubMed
- 27. Costa AL, Appenzeller S, Yasuda CL, Pereira FR, Zanardi VA, Cendes F. Artifacts in brain magnetic resonance imaging due to metallic dental objects. Med Oral Patol Oral Cir Bucal 2009;14:E278-E282.PubMed
- 28. Destine D, Mizutani H, Igarashi Y. Metallic artifacts in MRI caused by dental alloys and magnetic keeper. Nippon Hotetsu Shika Gakkai Zasshi 2008;52:205-210.ArticlePubMed
- 29. Eggers G, Rieker M, Kress B, Fiebach J, Dickhaus H, Hassfeld S. Artefacts in magnetic resonance imaging caused by dental material. MAGMA 2005;18:103-111.ArticlePubMedPDF
- 30. Lissac M, Metrop D, Brugirard J, Coudert JL, Pimmel P, Briguet A, Revel D, Amiel M. Dental materials and magnetic resonance imaging. Invest Radiol 1991;26:40-45.ArticlePubMed
- 31. Masumi S, Arita M, Morikawa M, Toyoda S. Effect of dental metals on magnetic resonance imaging (MRI). J Oral Rehabil 1993;20:97-106.ArticlePubMed
- 32. Shafiei F, Honda E, Takahashi H, Sasaki T. Artifacts from dental casting alloys in magnetic resonance imaging. J Dent Res 2003;82:602-606.ArticlePubMedPDF
- 33. Starcuk Z, Bartusek K, Hubalkova H, Bachorec T, Starcukova J, Krupa P. Evaluation of MRI artifacts caused by metallic dental implants and classification of the dental materials in use. Meas Sci Rev 2006;6:24-27.
- 34. Starčuková J, Starčuk Z Jr, Hubálková H, Linetskiy I. Magnetic susceptibility and electrical conductivity of metallic dental materials and their impact on MR imaging artifacts. Dent Mater 2008;24:715-723.ArticlePubMed
- 35. Camacho CR, Plewes DB, Henkelman RM. Nonsusceptibility artifacts due to metallic objects in MR imaging. J Magn Reson Imaging 1995;5:75-88.ArticlePubMed
- 36. Shellock FG, Woods TO, Crues JV 3rd. MR labeling information for implants and devices: explanation of terminology. Radiology 2009;253:26-30.ArticlePubMed
- 37. Shellock FG. Magnetic resonance safety update 2002: implants and devices. J Magn Reson Imaging 2002;16:485-496.ArticlePubMed
- 38. Huettel SA, Song AW, McCarthy G. Functional magnetic resonance imaging. 2nd ed. Sunderland (MA): Sinauer Associates; 2008.
- 39. New PF, Rosen BR, Brady TJ, Buonanno FS, Kistler JP, Burt CT, Hinshaw WS, Newhouse JH, Pohost GM, Taveras JM. Potential hazards and artifacts of ferromagnetic and nonferromagnetic surgical and dental materials and devices in nuclear magnetic resonance imaging. Radiology 1983;147:139-148.ArticlePubMed
- 40. American Society for Testing and Materials (ASTM). ASTM Standard F2182-09. Standard test method for measurement of radio frequency induced heating on or near passive implants during magnetic resonance imaging [Internet]. West Conshohocken (PA): ASTM International; 2009. updated year month day]. cited year month day]. Available from: http://www.astm.org/.
- 41. American Society for Testing and Materials (ASTM). ASTM Standard F2052. Standard test method for measurement of magnetically induced displaced force on medical devices in magnetic resonance environment [Internet]. West Conshohocken (PA): ASTM International; 2006. updated year month day]. cited year month day]. Available from: http://www.astm.org/.
- 42. Oyar O. The clinical use and indications of magnetic resonance imaging. Harran Univ Tıp Fak Derg 2008;5:31-40.
- 43. Shellock FG. MR imaging of metallic implants and materials: a compilation of the literature. AJR Am J Roentgenol 1988;151:811-814.ArticlePubMed
- 44. Devge C, Tjellström A, Nellström H. Magnetic resonance imaging in patients with dental implants: a clinical report. Int J Oral Maxillofac Implants 1997;12:354-359.PubMed
- 45. Schenck JF. The role of magnetic susceptibility in magnetic resonance imaging: MRI magnetic compatibility of the first and second kinds. Med Phys 1996;23:815-850.ArticlePubMedPDF
- 46. Klinke T, Daboul A, Maron J, Gredes T, Puls R, Jaghsi A, Biffar R. Artifacts in magnetic resonance imaging and computed tomography caused by dental materials. PLoS One 2012;7:e31766.ArticlePubMedPMC
- 47. Bartels LW, Smits HF, Bakker CJ, Viergever MA. MR imaging of vascular stents: effects of susceptibility, flow, and radiofrequency eddy currents. J Vasc Interv Radiol 2001;12:365-371.ArticlePubMed
- 48. Hosein I, Sherriff M, Ireland AJ. Enamel loss during bonding, debonding, and cleanup with use of a self-etching primer. Am J Orthod Dentofacial Orthop 2004;126:717-724.ArticlePubMed
- 49. Hinshaw DB Jr, Holshouser BA, Engstrom HI, Tjan AH, Christiansen EL, Catelli WF. Dental material artifacts on MR images. Radiology 1988;166:777-779.ArticlePubMed
- 50. Holton A, Walsh E, Anayiotos A, Pohost G, Venugopalan R. Comparative MRI compatibility of 316 L stainless steel alloy and nickel-titanium alloy stents. J Cardiovasc Magn Reson 2002;4:423-430.ArticlePubMed
- 51. Beau A, Bossard D, Gebeile-Chauty S. Magnetic resonance imaging artefacts and fixed orthodontic attachments. Orthod Fr 2017;88:131-138.ArticlePubMed
- 52. Blankenstein FH, Asbach P, Beuer F, Glienke J, Mayer S, Zachriat C. Magnetic permeability as a predictor of the artefact size caused by orthodontic appliances at 1.5 T magnetic resonance imaging. Clin Oral Investig 2017;21:281-289.ArticlePubMedPDF
- 53. Zhylich D, Krishnan P, Muthusami P, Rayner T, Shroff M, Doria A, Tompson B, Lou W, Suri S. Effects of orthodontic appliances on the diagnostic quality of magnetic resonance images of the head. Am J Orthod Dentofacial Orthop 2017;151:484-499.ArticlePubMed
- 54. Smeets R, Schöllchen M, Gauer T, Aarabi G, Assaf AT, Rendenbach C, Beck-Broichsitter B, Semmusch J, Sedlacik J, Heiland M, Fiehler J, Siemonsen S. Artefacts in multimodal imaging of titanium, zirconium and binary titanium-zirconium alloy dental implants: an in vitro study. Dentomaxillofac Radiol 2017;46:20160267.ArticlePubMedPMC
- 55. Hilgenfeld T, Prager M, Schwindling FS, Heil A, Kuchenbecker S, Rammelsberg P, Bendszus M, Heiland S. Artefacts of implant-supported single crowns - Impact of material composition on artefact volume on dental MRI. Eur J Oral Implantology 2016;9:301-308.PubMed
- 56. Lan G, Yunmin L, Pu W, Haili H. Contrastive analysis of artifacts produced by metal dental crowns in 3.0 T magnetic resonance imaging with six sequences. Hua Xi Kou Qiang Yi Xue Za Zhi 2016;34:277-280.PubMedPMC
- 57. Xu Y, Yu R. Comparison of magnetic resonance imaging artifacts of five common dental materials. Hua Xi Kou Qiang Yi Xue Za Zhi 2015;33:230-233.PubMedPMC
- 58. Cortes AR, Abdala-Junior R, Weber M, Arita ES, Ackerman JL. Influence of pulse sequence parameters at 1.5 T and 3.0 T on MRI artefacts produced by metal-ceramic restorations. Dentomaxillofac Radiol 2015;44:20150136.ArticlePubMedPMC
- 59. Shalish M, Dykstein N, Friedlander-Barenboim S, Ben-David E, Gomori JM, Chaushu S. Influence of common fixed retainers on the diagnostic quality of cranial magnetic resonance images. Am J Orthod Dentofacial Orthop 2015;147:604-609.ArticlePubMed
- 60. Zachriat C, Asbach P, Blankenstein KI, Peroz I, Blankenstein FH. MRI with intraoral orthodontic appliance-a comparative in vitro and in vivo study of image artefacts at 1.5 T. Dentomaxillofac Radiol 2015;44:20140416.ArticlePubMedPMC
- 61. Wylezinska M, Pinkstone M, Hay N, Scott AD, Birch MJ, Miquel ME. Impact of orthodontic appliances on the quality of craniofacial anatomical magnetic resonance imaging and real-time speech imaging. Eur J Orthod 2015;37:610-617.ArticlePubMed
- 62. Blankenstein F, Truong BT, Thomas A, Thieme N, Zachriat C. Predictability of magnetic susceptibility artifacts from metallic orthodontic appliances in magnetic resonance imaging. J Orofac Orthop 2015;76:14-29.ArticlePubMedPDF
- 63. Duttenhoefer F, Mertens ME, Vizkelety J, Gremse F, Stadelmann VA, Sauerbier S. Magnetic resonance imaging in zirconia-based dental implantology. Clin Oral Implants Res 2015;26:1195-1202.ArticlePubMedPDF
- 64. Fang Y, Xin L, Qingyun M, Lu W, Ye S. Effect of oral alloy post and core on magnetic resonance imaging. Hua Xi Kou Qiang Yi Xue Za Zhi 2014;32:588-591.PubMedPMC
- 65. Taniyama T, Sohmura T, Etoh T, Aoki M, Sugiyama E, Takahashi J. Metal artifacts in MRI from non-magnetic dental alloy and its FEM analysis. Dent Mater J 2010;29:297-302.ArticlePubMed
- 66. Elison JM, Leggitt VL, Thomson M, Oyoyo U, Wycliffe ND. Influence of common orthodontic appliances on the diagnostic quality of cranial magnetic resonance images. Am J Orthod Dentofacial Orthop 2008;134:563-572.ArticlePubMed
- 67. Blankenstein FH, Truong B, Thomas A, Schröder RJ, Naumann M. Signal loss in magnetic resonance imaging caused by intraoral anchored dental magnetic materials. RoFo Fortschr Geb Rontgenstr Nuklearmed 2006;178:787-793.PubMed
- 68. Harris TM, Faridrad MR, Dickson JA. The benefits of aesthetic orthodontic brackets in patients requiring multiple MRI scanning. J Orthod 2006;33:90-94.ArticlePubMed
- 69. Okano Y, Yamashiro M, Kaneda T, Kasai K. Magnetic resonance imaging diagnosis of the temporomandibular joint in patients with orthodontic appliances. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003;95:255-263.ArticlePubMed
- 70. Hubálková H, Hora K, Seidl Z, Krásenský J. Dental materials and magnetic resonance imaging. Eur J Prosthodont Restor Dent 2002;10:125-130.PubMed
- 71. Savane S, N’Dindin AC, N’Dindin GB, Kouame PA, Doyon D. Artifacts induced by dental reconstruction materials: the case of titanium. Odontostomatol Trop 2001;24:33-37.
- 72. Tetsumura A, Honda E, Sasaki T, Kino K. Metallic residues as a source of artifacts in magnetic resonance imaging of the temporomandibular joint. Dentomaxillofac Radiol 1999;28:186-190.ArticlePubMed
- 73. Borris TJ, Weber CR. Ferromagnetic MRI artifact secondary to a previous mandibular modified condylotomy. Br J Oral Maxillofac Surg 1999;37:104-105.ArticlePubMed
- 74. Behr M, Fellner C, Bayreuther G, Leibrock A, Held P, Fellner F, Handel G. MR-imaging of the TMJ: artefacts caused by dental alloys. Eur J Prosthodont Restor Dent 1996;4:111-115.PubMed
- 75. Iimuro FT. Magnetic resonance imaging artifacts and the magnetic attachment system. Dent Mater J 1994;13:76-88.ArticlePubMed
- 76. Oikarinen KS, Nieminen TM, Mäkäräinen H, Pyhtinen J. Visibility of foreign bodies in soft tissue in plain radiographs, computed tomography, magnetic resonance imaging, and ultrasound. An in vitro study. Int J Oral Maxillofac Surg 1993;22:119-124.PubMed
- 77. Laurell KA, Gegauff AG, Rosenstiel SF. Magnetic resonance image degradation from prosthetic magnet keepers. J Prosthet Dent 1989;62:344-348.ArticlePubMed
- 78. Sadowsky PL, Bernreuter W, Lakshminarayanan AV, Kenney P. Orthodontic appliances and magnetic resonance imaging of the brain and temporomandibular joint. Angle Orthod 1988;58:9-20.PubMed
- 79. Anusavice K, Shen C, Rawls RH. Phillips' science of dental materials. 12th ed. St. Louis (MO): Elsevier/Saunders; 2013. Chapter 15.
- 80. Shahidi SH, Bronoosh P, Alavi AA, Zamiri B, Sadeghi AR, Bagheri MH, Javadpour S. Effect of magnetic resonance imaging on microleakage of amalgam restorations: an in vitro study. Dentomaxillofac Radiol 2009;38:470-474.ArticlePubMed
- 81. Bates LF, Tai LC. The magnetic properties of amalgams. Proc Phys Soc 1936;48:795-809.Article
- 82. Bates LF, Ireland AW. The magnetic properties of silver amalgams. Proc Phys Soc 1937;49:642-645.Article
REFERENCES
Tables & Figures
REFERENCES
Citations

- Artifacts in magnetic resonance imaging of the head and neck: Unwanted effects caused by implant-supported restorations fabricated with different alloys
Lauren Bohner, Dieter Dirksen, Marcel Hanisch, Newton Sesma, Johannes Kleinheinz, Norbert Meier
The Journal of Prosthetic Dentistry.2025; 133(6): 1574. CrossRef - The influence of preformed metal crowns versus zirconia crowns on the diagnostic quality of magnetic resonance images
O. Dalzell, P. Haghighi, J. Ho, T. Rayner, L. Vidarsson, G. A. Garisto
European Archives of Paediatric Dentistry.2025; 26(1): 109. CrossRef - Interference of titanium and zirconia implants on dental-dedicated MR image quality: ex vivo and in vivo assessment
Katrine M Johannsen, Jennifer Christensen, Louise Hauge Matzen, Brian Hansen, Rubens Spin-Neto
Dentomaxillofacial Radiology.2025; 54(2): 132. CrossRef - Accuracy of Ionizing‐Radiation‐Based and Non‐Ionizing Imaging Assessments for the Diagnosis of Periodontitis: Systematic Review and Meta‐Analysis
Nicola Discepoli, Isabella De Rubertis, Cecile Wasielewski, Giuseppe Troiano, Maria Clotilde Carra
Journal of Clinical Periodontology.2025; 52(S29): 74. CrossRef - The Effect of MRI Exposure on the Shear Bond Strength and Adhesive Remnant Index of Different Bracket Types
Luka Šimunović, Jakov Stojanović, Katarina Tečić, Dijana Zadravec, Senka Meštrović
Dentistry Journal.2025; 13(3): 108. CrossRef - Impact of Artifacts Caused by Intraoral Dental Materials in Magnetic Resonance Imaging
Divya Josephraj, Ravindranath Vineetha, Priya Pattath Sankaran, Prakashini Koteshwara, Mathangi Kumar, Kalyana Chakravarthy Pentapati
Pesquisa Brasileira em Odontopediatria e Clínica Integrada.2025;[Epub] CrossRef - Orthodontic appliances and their diagnostic impact to brain MRI
Lisa Latzko, Anna Schmit, Bernhard Glodny, Astrid E. Grams, Christoph Birkl, Adriano G. Crismani
Clinical Oral Investigations.2025;[Epub] CrossRef - Impact of Intra-Oral Dental Materials on Magnetic Resonance Imaging: A Perspective Survey from Dental Professionals
Sejal Gupta, Mathangi Kumar, Kalyana C Pentapati, Ravindranath Vineetha, Vinu Thomas George, Nidambur Vasudev Ballal, Priya Pattath Sankaran
Journal of Pharmacy and Bioallied Sciences.2025; 17(Suppl 1): S551. CrossRef - Beyond radiation: Emerging applications of MRI in dental diagnostics and clinical practice
Gerta Halilaj, Nebi Cemeta
Journal of Dentistry and Multidisciplinary Sciences.2025; 1(1): 31. CrossRef - Nonionizing diagnostic imaging modalities for visualizing health and pathology of periodontal and peri‐implant tissues
Andy Wai Kan Yeung, Abeer AlHadidi, Rutvi Vyas, Michael M. Bornstein, Hiroshi Watanabe, Ray Tanaka
Periodontology 2000.2024; 95(1): 87. CrossRef - Cortical thickness and grey-matter volume anomaly detection in individual MRI scans: Comparison of two methods
David Romascano, Michael Rebsamen, Piotr Radojewski, Timo Blattner, Richard McKinley, Roland Wiest, Christian Rummel
NeuroImage: Clinical.2024; 43: 103624. CrossRef - Association between dental restorations and artefacts on head magnetic resonance images in paediatric patients
Pitchaya Tunlayadechanont, Padcha Tunlayadechanont, Nantana Sriudomporn, Ploy Wisetsathon, Duangporn Duangthip, Varangkanar Jirarattanasopha
International Journal of Paediatric Dentistry.2024; 34(5): 546. CrossRef - Commercially Pure Titanium Implants With Selenium and Hyaluronic Acid Coating for Dental Applications
Soorya Ganesh, Gheena S, Kalaiyarasan Madhu
Cureus.2024;[Epub] CrossRef - Multibraided Fixed Retainers with Different Diameters after Magnetic Resonance Imaging (MRI): In Vitro Study Investigating Temperature Changes and Bonding Efficacy
Maria Francesca Sfondrini, Maurizio Pascadopoli, Paola Gandini, Lorenzo Preda, Domenico Sfondrini, Karin Bertino, Cinzia Rizzi, Andrea Scribante
Dentistry Journal.2024; 12(8): 255. CrossRef - Chronic non-bacterial osteomyelitis of the mandible – orthodontic considerations and management: A case report
Saskia Andrea Schwabe, Sean Booth, Susi Caldwell
Journal of Orthodontics.2024; 51(4): 415. CrossRef - Magnetic resonance imaging in the diagnosis of periodontal and periapical disease
Katrine Mølgaard Johannsen, João Marcus de Carvalho E Silva Fuglsig, Louise Hauge Matzen, Jennifer Christensen, Rubens Spin-Neto
Dentomaxillofacial Radiology.2023;[Epub] CrossRef - Surveillance of head neck cancer: Case for personalized and standardized surveillance
Shrikant B. Mali
Oral Oncology.2023; 139: 106354. CrossRef - Effect of Magnetic Resonance Imaging at 1.5 T and 3 T on Temperature and Bond Strength of Orthodontic Bands with Welded Tubes: An In Vitro Study
Maria Francesca Sfondrini, Simone Gallo, Maurizio Pascadopoli, Cinzia Rizzi, Andrea Boldrini, Simone Santagostini, Luca Anemoni, Maria Sole Prevedoni Gorone, Lorenzo Preda, Paola Gandini, Andrea Scribante
Materials.2023; 16(2): 651. CrossRef - Magnetic resonance imaging artefacts caused by orthodontic appliances and/or implant-supported prosthesis: a systematic review
Katrine Mølgaard Johannsen, João Marcus de Carvalho E Silva Fuglsig, Brian Hansen, Ann Wenzel, Rubens Spin-Neto
Oral Radiology.2023; 39(2): 394. CrossRef - Magnetic resonance imaging investigations in patients with metallic dental prosthesis: “The associated dilemma for medical fraternity and the dentist's role”
Ritika Bhambhani, SantanuSen Roy, Shubha Joshi
The Journal of Indian Prosthodontic Society.2023; 23(2): 203. CrossRef - Recent advances in the application and biological mechanism of silicon nitride osteogenic properties: a review
Ziyi Liu, Ruijie Wang, Wenjing Liu, Yushan Liu, Xiaoli Feng, Fujian Zhao, Pei Chen, Longquan Shao, Mingdeng Rong
Biomaterials Science.2023; 11(21): 7003. CrossRef - Techniques, Tricks, and Stratagems of Oral Cavity Computed Tomography and Magnetic Resonance Imaging
Davide Maraghelli, Michele Pietragalla, Linda Calistri, Luigi Barbato, Luca Giovanni Locatello, Martina Orlandi, Nicholas Landini, Antonio Lo Casto, Cosimo Nardi
Applied Sciences.2022; 12(3): 1473. CrossRef - GEÇICI VE DAIMI SIMANLARIN DENTINE OLAN BAĞLANMA DAYANIMI ÜZERINE MANYETIK REZONANS GÖRÜNTÜLEME İŞLEMININ ETKISININ ARAŞTIRILMASI
Melih ÜLGEY, Oğuzhan GÖRLER, İsmail ŞALK, Derya ÖZDEMİR DOĞAN
Atatürk Üniversitesi Diş Hekimliği Fakültesi Dergisi.2022; : 1. CrossRef - Performance of PROPELLER FSE T2WI in reducing metal artifacts of material porcelain fused to metal crown: a clinical preliminary study
Wenjin Li, Jing Shi, Wenjin Bian, Jianting Li, Xiaoqing Chen, Juan Feng, Jiali Yu, Jun Wang, Jinliang Niu
Scientific Reports.2022;[Epub] CrossRef - Tracking the Molecular Fingerprint of Head and Neck Cancer for Recurrence Detection in Liquid Biopsies
Araceli Diez-Fraile, Joke De Ceulaer, Charlotte Derpoorter, Christophe Spaas, Tom De Backer, Philippe Lamoral, Johan Abeloos, Tim Lammens
International Journal of Molecular Sciences.2022; 23(5): 2403. CrossRef - Review on Biocompatibility and Prospect Biomedical Applications of Novel Functional Metallic Glasses
Michał Biały, Mariusz Hasiak, Amadeusz Łaszcz
Journal of Functional Biomaterials.2022; 13(4): 245. CrossRef - MRI compatibility of orthodontic brackets and wires: systematic review article
Adrienn Dobai, Fanni Dembrovszky, Tamás Vízkelety, Péter Barsi, Fanni Juhász, Csaba Dobó-Nagy
BMC Oral Health.2022;[Epub] CrossRef - The interaction and interference of preformed metal crowns on magnetic resonance imaging: a scoping review with a systematic methodology
O. Sumner, R. Goldsmith, N. Heath, G. D. Taylor
European Archives of Paediatric Dentistry.2021; 22(6): 1023. CrossRef - An Evidence-based Protocol for the Management of Orthodontic Patients Undergoing MRI Scans
Rachael Shivam, Sheelagh Rogers, Nicholas Drage
Orthodontic Update.2021; 14(1): 32. CrossRef - Reversal of Osseointegration as a Novel Perspective for the Removal of Failed Dental Implants: A Review of Five Patented Methods
Rolf G. Winnen, Kristian Kniha, Ali Modabber, Faruk Al-Sibai, Andreas Braun, Reinhold Kneer, Frank Hölzle
Materials.2021; 14(24): 7829. CrossRef - Magnetic resonance imaging as a diagnostic tool for periodontal disease: A prospective study with correlation to standard clinical findings—Is there added value?
Monika Probst, Egon Burian, Teresa Robl, Dominik Weidlich, Dimitrios Karampinos, Teresa Brunner, Claus Zimmer, Florian Andreas Probst, Matthias Folwaczny
Journal of Clinical Periodontology.2021; 48(7): 929. CrossRef - An Update of the Possible Applications of Magnetic Resonance Imaging (MRI) in Dentistry: A Literature Review
Rodolfo Reda, Alessio Zanza, Alessandro Mazzoni, Andrea Cicconetti, Luca Testarelli, Dario Di Nardo
Journal of Imaging.2021; 7(5): 75. CrossRef - Implant-supported overdentures: part 1
David Gray, Jaymit Patel
British Dental Journal.2021; 231(2): 94. CrossRef - Oral and dental considerations in pediatric cancers
Priyanshi Ritwik, Tammuella E. Chrisentery-Singleton
Cancer and Metastasis Reviews.2020; 39(1): 43. CrossRef - Recent advances in bioelectronics chemistry
Yin Fang, Lingyuan Meng, Aleksander Prominski, Erik N. Schaumann, Matthew Seebald, Bozhi Tian
Chemical Society Reviews.2020; 49(22): 7978. CrossRef - Imaging of root canal treatment using ultra high field 9.4T UTE-MRI – a preliminary study
Maximilian Timme, Max Masthoff, Nina Nagelmann, Malte Masthoff, Cornelius Faber, Sebastian Bürklein
Dentomaxillofacial Radiology.2020; 49(1): 20190183. CrossRef - Magnetic resonance imaging based computer‐guided dental implant surgery—A clinical pilot study
Florian Andreas Probst, Josef Schweiger, Maria Juliane Stumbaum, Dimitrios Karampinos, Egon Burian, Monika Probst
Clinical Implant Dentistry and Related Research.2020; 22(5): 612. CrossRef - Magnetic resonance imaging artifacts produced by dental implants with different geometries
Lauren Bohner, Norbert Meier, Felix Gremse, Pedro Tortamano, Johannes Kleinheinz, Marcel Hanisch
Dentomaxillofacial Radiology.2020; 49(8): 20200121. CrossRef - Implications and Considerations of Dental Materials in MRI: A Case Report and Literature Review
Brenton J. Wilson, Phoebe E. O’hare, John Zacariah, Wen Lin Chai
Case Reports in Dentistry.2020;[Epub] CrossRef
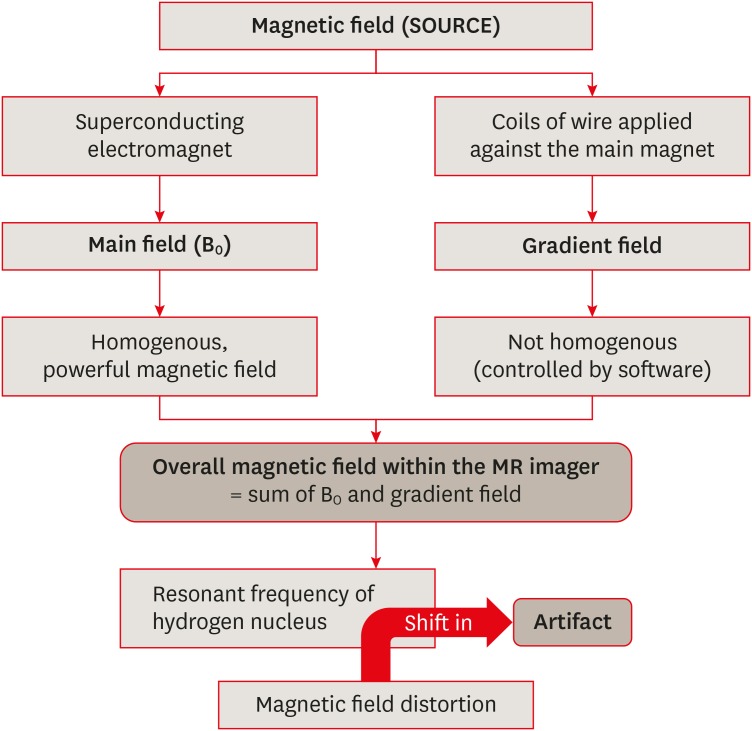
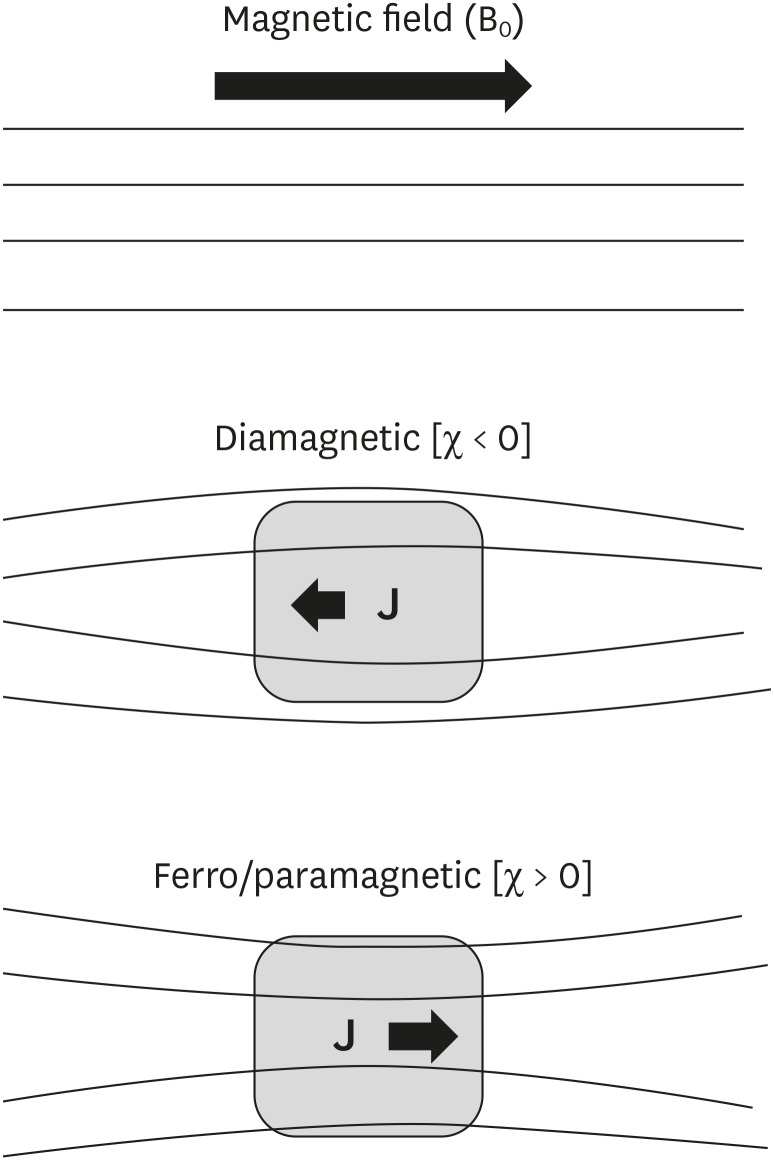
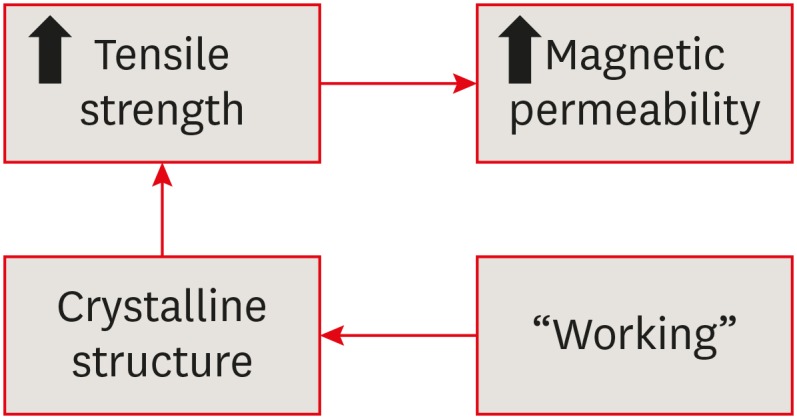
Figure 1
Figure 2
Figure 3
Unwanted effects of magnetic resonance imaging (MRI)-dental material interaction
| Type of unwanted effect | Description |
|---|---|
| Artifactual | The accuracy of the image is affected by the dental material. |
| Mechanical (magnetically-induced displacement) | The external strong magnetic field may dislodge or move a ferromagnetic material into a position parallel to the lines of that field. |
| Physical (radiofrequency heating) | The ferromagnetic material is heated by the high-frequency electromagnetic field. |
Classification of materials according to their interactions with magnetic fields
| Type of magnetic effect | Effect on applied magnetic field | Magnetic permeability/susceptibility | Significance | Example |
|---|---|---|---|---|
| Diamagnetism | Internal magnetization (polarization) opposes the externally applied field; | µ < 1 (or χ < 0); | Least likely to cause an artifact | All biological tissues; silver (dental amalgam alloy) |
| Magnetic field lines are ‘thinned’ or ‘dispersed’ | Slightly lower permeability than free space; | |||
| Negative susceptibility | ||||
| Paramagnetism | Internal magnetization (polarization) is in the same direction as the externally applied field; | µ > 1 (or χ > 0); | Far less likely to cause an artifact | Vascular stents [ |
| Magnetic field lines are ‘concentrated’ in the object | Slightly higher permeability than free space; | |||
| Positive susceptibility | ||||
| Ferromagnetism | Magnetic field lines are ‘concentrated’ in the object; | µ >> 1 (or χ >> 0); | High potential to cause MRI artifacts | Stainless steel |
| Strongly attracted by a magnetic field | High permeability; | |||
| Positive susceptibility |
MRI, magnetic resonance imaging; χ, magnetic susceptibility (synonym = magnetizability); µ, magnetic permeability, µ = 1 + χ.
Classification of materials based on magnetic susceptibility
| Classification | Description | Significance | Example |
|---|---|---|---|
| Compatible | Compatible: Δx < 3 ppm; | Fully compatible materials; | Resin-based sealer AH Plus, glass ionomer cement, gutta-percha, zirconium dioxide, and some composites. |
| Material produces no detectable distortions on either SE or GRE imaging. | Can be present even in the tooth of interest. | ||
| Compatible I | Compatible I: 3 < Δx < 200 ppm; | Limited distortions; | Some composites, amalgam, gold alloy, gold-ceramic crowns, titanium alloy, NiTi orthodontic wires |
| Material produces noticeable distortions, acceptability depends on application. | Image usability depends on area of interest. | ||
| Non-compatible | Non-compatible: Δx > 200 ppm; | Strongest distortions; | Stainless steel orthodontic appliances (wires, brackets), Co-Cr sample. |
| Material produces strong image distortions even located far from the imaging region. | Classified as non-compatible. |
χ, magnetic susceptibility (synonym = magnetizability); SE, spin-echo; GRE, gradient-echo; compatible I, 3 < Δx < 200 ppm; material produces noticeable distortions, acceptability depends on application.
Relationship between artifacts and imaging sequence
| MRI sequence | Magnitude of artifact | Reason |
|---|---|---|
| Long echo time; GRE sequences | Most severe artifacts (loss of signal around the material) [ | Intravoxel dephasing is the predominant cause of signal loss, resulting in a dark or black area around the metal on processed images [ |
| Shortened echo time and decreased voxel size; SE sequence [ | Best sequence for reducing the severity of susceptibility artifacts (complex spear-shaped artifacts) [ | Diminished phase shifts in voxel caused by local static magnetic field gradients [ |
MRI, magnetic resonance imaging; GRE, gradient echo; SE, spin-echo.
Summary of unwanted effects due to interactions of dental materials with MRI, according to a literature search (1988–2018)
| No. | Author (year) | Dental material used | MRI specifications/area of interest | Results | Conclusion/recommendation |
|---|---|---|---|---|---|
| 1 | Beau et al. (2017) [ | Orthodontic brackets (S.S., Ti, ceramic with metal slots); retainers | 1.5 T; 2 scans per patient with empty wax jig & with wax jig including the attachment. | S.S brackets always caused non-interpretability of all anatomic areas (100%). Ti (20%), ceramic brackets with metal slots (17%) and S.S. retainers (87%) caused artifacts in the oral cavity. | Ceramic brackets with metal slots & Ti brackets do not have to removed, based on the scan area; metal fixed retainers are to be removed only in oral cavity scans; S.S. brackets must always be removed before head & neck MRI. |
| [Article in French] | |||||
| 2 | Blankenstein et al. (2017) [ | 11 test specimens of known permeability (1.003–1.431) | 1.5 T MRI; TSE & gradient-echo sequences of head & neck region. | Steel caused a wide range of artifact sizes (10–74 mm), depending on their permeability. Ti, Co-Cr & ceramic materials produced artifact radii up to 20 mm. | Permeability can be reliably assessed by conventional measurement devices & artifact size can be predicted. Radiologists can decide whether the orthodontic attachments should be removed. |
| 3 | Zhylich et al. (2017) [ | Orthodontic brackets (S.S., ceramic, ceramic with metal slots); retainers | Head MR scans of 9 regions: sagittal T1-weighted, axial T2-weighted, axial gradient-recalled, axial diffusion-weighted, non-contrast axial MR angiography, & axial fluid-attenuated inversion recovery sequences. | MR images were affected by type of appliance, MR sequence, and location (head region). The maximum image distortion was found with S.S. brackets and molar tubes; minimal distortion occurred with ceramic brackets. | Type of appliance, region imaged, and MR sequence must be considered before imaging is done in patients with fixed orthodontic appliances. |
| 4 | Smeets et al. (2017) [ | Dental implants of Zr, Ti, and Ti-Zr alloy embedded in gelatin | 3 T MRI; T2-weighted space sequence & T1-weighted volumetric interpolated brain examination technique. | Ti & Ti-Zr alloy induced an extensive signal void in MRI (strong susceptibility — MR signal attenuated up to 14.1 mm from implant); Zr implants were clearly definable with only minor distortion artifacts. | MRI allows excellent image contrast and limited artifacts for Zr implants. CT & CBCT examinations are less affected by artifacts from Ti & Ti-Zr alloy implants than MRI. |
| 5 | Hilgenfeld et al. (2016) [ | 1 Zr & 4 Ti dental implants were provided with different single crown materials: PFM precious alloy, PFM non-precious alloy, porcelain-fused-to-Zr and monolithic Zr | 3 T MRI; applying SPACE and TSE (2 standard sequence types). | The fewest artifacts were found with the Zr implant combined with a monolithic Zr crown. The Ti implant combined with a single crown framework of non-precious alloys had an unfavorable artifact volume. Smaller artifact volumes were noted for Ti implants with remaining 3 crown materials (PFM precious alloy, porcelain-fused-to-Zr, and monolithic Zr). | Material composition of dental implants provided with single crowns had a profound impact on artifact volume. In comparison with crowns containing cobalt, chromium and tungsten, MRI artifacts are reduced in precious alloy- and Zr-based crowns. |
| 6 | Lan et al. (2016) [ | Crowns of Co-Cr, Ni-Cr, Ti alloy & pure Ti | 3 T MRI with 6 sequences: T1weighted SE, T2 weighted-inversion recovery, T2 star GRE, T2 weighted-FSE, T1 weighted-fluid attenuate inversion recovery, and T2 weighted-imaging. | Artifacts in the T2 star GRE sequence were significantly wider than those in the other sequences. | The T2 star GRE exhibited the strongest influence on artifacts, whereas the other 5 sequences contributed equally to artifact generation. |
| [Chinese] | |||||
| 7 | Murakami et al. (2016) [ | 7 metallic dental materials: Al, silver alloy (Ag), type IV gold alloy (Au), gold-palladium-silver alloy (Au-Pd-Ag), Ti, Ni-Cr & Co-Cr alloy | Sequences included GRE, FSE, GRASS, SPGR, FSPGR, FIESTA & EPI (axial/sagittal planes). | Artifact volumes: FSE-T1/FSE-T2 < FSPGR/SPGR < GRASS/GRE < FIESTA < EPI. For all scan sequences, artifact volumes for Au, Al, Ag & Au-Pd-Ag were significantly smaller than other materials (artifact volume size: Ti < Ni-Cr < Co-Cr. Artifact-specific shape (cubic sample) depended on scan plane (i.e., circular pattern for the axial plane & ‘clover-like’ for the sagittal plane). | Availability of standardized information on artifact size & configuration during MRI will enhance the diagnosis in patients with metallic compounds. |
| 8 | Xu et al. (2015) [ | 3 metals and 2 ceramics, fabricated to same size and thickness of incisor crown | Different sequences of 3 MRI field strengths: 0.35, 1.5 & 3 T–T1WI & T2WI images. | No artifacts were found for Zr crowns; for casting ceramic, they were minimal. All dental precious metal alloys, Ni-Cr alloy dental porcelain, & Co-Cr ceramic alloy had varying degrees of artifacts. | Zr & casting ceramics presented almost no or faint artifacts. By contrast, precious metal alloys, Ni-Cr alloy dental porcelain and Co-Cr ceramic alloy displayed MRI artifacts. The artifact area increased with the strength of the magnetic field. |
| [Article in Chinese] | |||||
| 9 | Cortes et al. (2015) [ | Ni-Cr metal-ceramic restorations (i.e., dental crowns & fixed bridges) and cylindrical reference specimens | 1.5 & 3 T MRI scanners; GRE, SE & UTE pulse sequences. | A significant correlation was found between TE and artifact area in GRE images. Higher receiver bandwidth significantly reduced artifact area in SE images. UTE images yielded smallest artifact area at 1.5 T. Significant differences were found in the mean artifact area between 1.5 & 3 T images and between images from GRE & SE pulse sequences. | A significant correlation found between TE and artifact area in GRE images. It is possible to compensate for the effect of higher field strength on MRI artifacts by setting optimized pulse sequences for scanning patients with metal-ceramic restorations. |
| 10 | Shalish et al. (2015) [ | 2 commonly used fixed retainers: Twistflex & Ortho Flex Tech retainers. | 1.5 to 3 T; SE sequence; T1- & T2-weighted sequence. | Ortho Flex Tech retainers caused no distortion. Twistflex retainers caused distortion (46%) in areas close to the retainer (tongue, jaws). Maxillary fixed retainers & maxillary-mandibular fixed retainer combination further increased distortion. Greater distortion was seen with 3 T magnetic fields & T1-weighted SE sequences. | Removal of Ortho Flex Tech retainer is unnecessary before MRI. Removal of Twistflex should be considered if MRI scans are performed to diagnose areas close to fixed retainers, when 3 T magnetic fields and T1-weighted sequences are used, and when both maxillary & mandibular fixed retainers are present. |
| 11 | Zachriat et al. (2015) [ | Ceramic brackets & S.S. brackets | 1.5 T MRI of head & neck region; different types of MR sequences (EPI, TSE and TSE-WARP, GRE). | In vitro: Artifact radii of 1.12 (ceramic brackets) and 7.4 cm (ferromagnetic steel brackets). WARP reduced artifacts by 32.7%. | In vitro measurements allow estimation of in vivo artifact size. Orthodontic appliances may often remain intraorally when performing MRI. WARP showed more significant effect in vitro than in vivo. |
| In vivo: EPI sequence for brain imaging was not analyzable. The TSE sequence of the brain had no artifacts except for the nasal cavity. The TSE sequence of the cervical spine had severe artifacts in the midface region. The GRE sequence was more susceptible to artifacts than TSE. | |||||
| 12 | Wylezinska et al. (2015) [ | S.S. arch wire, brackets & molar bands; appliances/reinforcement with Ni/Ti alloys. | 0.5 T scanner using standard spin & GRE sequences. Craniofacial region, with special interest in soft palate and velopharyngeal wall (real-time speech imaging) & TMJ & pituitaries (anatomical imaging). | The most extensive effects were associated with S.S. arch wire, particularly if combined with S.S. brackets & S.S. molar bands (diagnostic quality severely degraded). All non-metallic, non-metallic with Ni/Cr reinforcement, or Ni/Ti alloys appliances were of little concern. | Appliances manufactured from S.S. cause extensive artifacts, which may render the image non-diagnostic. The presence and type of orthodontic appliances should be always included in patient's screening, so risks of artifacts can be assessed prior to imaging. Although risks to patients with fixed orthodontic appliances at 1.5 T are low, their secure attachment should be confirmed. |
| 13 | Blankenstein et al. (2015) [ | 16 orthodontic small-device and wire specimens made of different steel and Ti or Co-Cr alloys | SE and GRE sequences at 1.5 & 3 T. | Artifact formation depends on material properties (specimen size, crystalline structure, processing) & MRI specifications (main field strength, sequence type). Artifact radii ranged from 14 mm (SE, 1.5 T) to 51 mm (GRE, 3 T). No artifacts at 1.5 T around Ti & Co-Cr specimens; the same observation was made with 1 of the steel grades. | Artifact size cannot be predicted merely from the designation ‘steel’ or from crystalline structure. Relevant is the magnetic permeability (or susceptibility) of the final products, which is not disclosed by manufacturers, and it cannot be measured in fixed intraoral appliances. Some steel devices can remain in situ without triggering adverse consequences. |
| 14 | Beau et al. (2015) [ | 60 patients requiring head MRI scan for medical reasons were given one of 4 types of fixed attachments: S.S., Ti, ceramic brackets with metal slots, & S.S. retainers | Each patient had 2 scans at 1.5 T; the 4 areas under investigation were maxillary sinus, oral cavity, TMJ, & posterior cerebral fossa. | S.S. brackets always caused non-interpretability of all anatomic areas (100%). Ti brackets, ceramic brackets with metal slots, and S.S. retainers caused artifacts in the oral cavity only (for 20%, 16.65%, and 86.65% of subjects). | Ceramic brackets with metal slots & Ti brackets do not always have to be removed before head & neck MRI, depending on the investigation area. Metal fixed retainers are to be removed if the oral cavity itself is under investigation. S.S. brackets are to always be removed before head & neck MRI. |
| 15 | Duttenhoefer et al. (2015) [ | Ti & Zr implants embedded in 10% (w/v) gelatin phantoms (MRI), or post-implantation (micro-CT) | 3 T MRI; T1-weighted TSE & T2-weighted TSE sequences. | Post-implantation, while Ti implants induced a strong B0-field distortion resulting in extensive signal voids, Zr implants were clearly depicted with only minor distortions. | Excellent contrast, limited artifacts, radiation-free and accurate implant assessment indicate that MRI is a valuable imaging alternative for Zr implants. |
| 16 | Fang et al. (2014) [ | 6 casting alloy post & cores (Zr post & core – control). All 7 types of post & cores were of same the size & shape | T1-weighted SE imaging (SE-T1WI), T2-weighted turbo spin-echo imaging (TSE-T2WI), and DWI. | Co-Cr alloy post & core generated severe artifacts, whereas Au-Pd alloy post & core generated no obvious artifacts, & no difference was seen between the Zr & Au-Pd alloy post & cores. Pure Ti alloy post & core produced mild artifacts. Post & cores of Ti, Ni-Cd, & Au-Pt alloys generated moderate artifacts. | Different metal post & cores had different influences on MRI. With exception of that generated by Co-Cr alloy, the artifacts generated by single-alloy post & core did not influence normal head & neck imaging. |
| [Article in Chinese] | |||||
| 17 | Sinkiewicz et al. (2013) [ | Orthodontic appliances | - | - | This review article gave recommendations for the removal or retention of orthodontic appliances during MR imaging. |
| 18 | Tymofiyeva et al. (2013) [ | A series of standard dental materials was studied & their magnetic susceptibility was estimated | 1.5 T MRI system using SE and GRE pulse sequences. | Materials were classified as fully compatible (material can be present even in tooth of interest), compatible I, & non-compatible (material should not be present in patient's mouth for any dental MRI applications). | A material classification that complies with the standard grouping of materials according to their magnetic susceptibility can serve as a guideline in future dental MRI research. |
| 19 | Taniyama et al. (2010) [ | Non-magnetic metal (type-4 gold alloy ring) that was intact or cut | 2 T MRI; excitation RF field was along the x-axis, with RF-receiver coil in the y-z plane. T1 (spin-lattice relaxation time)-weighted images. | For the intact gold ring, a portion around the ring disappeared. It was nearly restored with a cut ring. Artifacts appeared when the circumferential surface of the ring was placed perpendicular to the RF field of MRI. However, in other directions or with a cut ring, the artifact disappeared. | This demonstrated the characteristics and cause of artifacts by non-magnetic dental metals. An alternating magnetic field was shown to induce a surface current that interfered with the field on the continuous gold ring. |
| 20 | Costa et al. (2009) [ | Retrospective study of 1,200 medical records of epileptics who underwent MRI. 70 MR images with artifacts were retrieved & reviewed | MRI acquisition parameters were: 1) sagittal T1 SE; 2) coronal images, T1-weighted inversion recovery; 3) axial images, T1-weighted GRE. | The artifact image plane was given a score of 0 or 1 (0 = distinguishable for diagnosis; 1 = not distinguishable). 78% of artifacts were caused by orthodontic appliances (the highest scores in all planes), followed by dental Ti implants (18%) & metallic crowns (4%). | It is difficult to avoid the effects of metallic artifacts in maxillofacial regions on brain scans. Removing the metallic parts of orthodontic appliance should ensure diagnostically useful scans. |
| Metallic objects were dental (Au) crowns, dental Ti implants, & metallic orthodontic appliances (bands, brackets, arch wires) | a) T1-weighted GRE; b) FLAIR. | ||||
| 21 | Hunt et al. (2009) [ | - | - | - | In this letter to the editor, the authors contemplated the use of Essix trays to fit over bonded canine-to-canine retainers or other fixed attachments prior to MRI to prevent appliance dislodgement. They also suggested the use of TMA wire for fixed retainers. |
| 22 | Elison et al. (2008) [ | 10 subjects received 5 consecutive cranial MR scans. A control scan was conducted with Essix trays fitted over the maxillary & mandibular teeth. 4 experimental head MR scans were done with plastic, ceramic, Ti, & S.S. brackets incorporated into Essix tray material | Each MR scan consisted of 4 sequences: sagittal T1-weighted SE (T1 sagittal), axial T2-weighted SE (T2 axial), GRE & DWI. | Statistically significant difference between the distortion scores of S.S. brackets & those of other experimental MR scans. | Plastic, ceramic & Ti brackets caused minimal distortion of cranial MR images. However, S.S. brackets caused significant distortion (cranial regions were non-diagnostic). The areas with the most distortion were the mandible body, hard palate, base of tongue, globes, nasopharynx & frontal lobes. The closer the S.S. appliance was to a specific anatomic region, the greater MR image distortion was found. |
| 23 | Hu et al. (2008) [ | - | - | - | This review article concluded that FPDs produced artifacts in MRI, thus reducing image quality when patients with a metallic prosthesis in mouth undergo head & neck MRI. However, these FPDs cannot be removed arbitrarily. |
| [Article in Chinese] | |||||
| 24 | Destine et al. (2008) [ | 1 pre-fabricated magnetic keeper and 4 clinical dental alloys (Au-Ag-Pa, casting Au alloy type 3, Co-Cr, Au porcelain alloy); in total, 2 metal crowns & 5 magnetic keepers were analyzed | 1.5 T MRI apparatus; in axial, coronal, & sagittal planes; T1-weighted SE sequence (TR/TE) & T2-weighted TSE sequence were used. | Co-Cr showed greater signal intensity, up to 40 mm in coronal T2WI images & 70 mm in axial T1WI images for the magnetic keeper. The signal intensities of Au-Ag-Pa & casting Au alloy type 3 were similar to the control. The signal intensity of Au-porcelain alloy was different from the control at 0 mm & 5 mm in coronal T1, T2WI & in sagittal T1WI at 0 mm. | The artifacts generated by the magnetic keeper and Co-Cr crown when they were used in a second molar could disturb MR images of the TMJ. |
| 25 | Starčuková et al. (2008) [ | Magnetic susceptibility, electrical conductivity and artifacts were evaluated for 45 cylindrical standardized samples of dental alloys and amalgam. | Artifact sizes were measured in SE and GRE images at 1.5 T according to the standards of the American Society for Testing and Materials. | Short-echo-time GRE imaging is possible even at very close distances from dental devices made of amalgam, precious alloys & Ti alloys. Ni-Cr & Co-Cr artifacts were still acceptable, but large restorations of Al-bronzes preclude orofacial imaging. Influence of electrical conductivity on artifact size was negligible. | Dental materials differ considerably in their magnetic susceptibility, electrical conductivity and artifacts. For dental devices, magnetic susceptibility differences are of little clinical importance for diagnostic SE/GRE imaging of the neck and brain, but are significant for orofacial imaging. MRI is possible even close to dental devices if they are made of dental materials with low magnetic susceptibility. Not all materials in current use meet this requirement. |
| Magnetic susceptibility and electrical conductivity were determined. | |||||
| 26 | Blankenstein et al. (2006) [ | 5 standard dental magnet attachments with volumes of 6.5–31.4 mm3: NdFeB magnet with open magnetic field, NdFeB magnet with closed magnetic field, SmCo magnet with open magnetic field, S.S. keeper (AUM-20) & PdCo piece | 1.5 T & 3 T MRI; gradient-echo and T1- & T2-weighted SE sequence. | In gradient-echo images, artifacts were substantially larger and symmetrically adjusted around the object. Areas with total signal loss were mushroom-like. In SE images, the signal loss areas were smaller, but not centered. Different ferromagnetic attachments had no clinically relevant influence on the signal loss in either 1.5 T or 3 T MRI. | Ferromagnetic materials used in dentistry are not intraorally standardized. To ensure that the area of interest is not affected by artifacts, the maximum extent of the signal loss area should be assumed: a radius of up to 7 cm in 1.5 & 3 T MRI by T1 & T2 sequences, and a radius of up to 10 cm in T2 sequences. To decide whether magnet attachments have to be removed before MRI, physicians should consider both the intact retention of keepers and safety distance between ferromagnetic objects and the area of interest. |
| [Article in German] | |||||
| 27 | Hubálková et al. (2006) [ | - | - | - | This review article concluded that MRI causes movement or heating of metal objects (with positive magnetic properties) present in the body, which can lead to health risks. The safety & MRI compatibility of dental alloys must always be considered prior to MRI. |
| 28 | Harris et al. (2006) [ | A patient undergoing orthodontic treatment who required repeated MRI scans on a regular basis | - | S.S. & other metallic orthodontic appliances created substantial artifacts & obliterated details in the facial area. Ceramic brackets & directly-bonded metal tubes did not affect MRI scan diagnostic quality. | The authors concluded that metallic orthodontic appliances in the head & neck region can distort MR images, thus reducing their value. Aesthetic brackets (no metal components and arch wires removed) do not distort MRI scans. |
| 29 | Shafiei et al. (2003) [ | 11 dental casting or implant materials were imaged | 1.5 T MRI apparatus with 3 different sequences. | A variety of artifacts with different magnitudes was observed. Only 1 sample, composed mainly of Pa, In, & antimony (Sb), showed no artifacts in any imaging sequences. | Selecting specific dental casting alloys according to their elemental compositions can minimize metal artifacts in MRI; however, Ti alloys currently pose a problem with respect to causing MRI artifacts. |
| 30 | Okano et al. (2003) [ | MR imaging was performed in 20 TMJs before and after insertion of 6 kinds of orthodontic appliances (ceramic/metal brackets; directly-bonded tube/band tube; +/− S.S. arch wires) | - | For disk position, diagnostic accuracy was 70%–80% (ceramic/metal brackets with no S.S. arch wires), & 60%–70% with S.S. arch wires. For condylar configurations, accuracy was 80% (ceramic brackets & directly-bonded tube), 55% (metal brackets & directly-bonded tube), 40% (metal brackets & band tube), reduced to 10%–40% in the presence of S.S. arch wires. No significant changes were found in the condylar head marrow signals. | MRI should preferably be performed in orthodontic patients by using ceramic brackets in the front teeth & direct bonding tubes in molars, while removing arch wires. |
| 31 | Hubálková et al. (2002) [ | 15 dental alloys, 4 dental implants, 1 surgical splint & 2 wires for fixation of maxillofacial fractures | - | Artifacts were significant: for surgical splints, a spherical artifact of 55 mm in diameter; for wires, up to 22 mm; & for the dental blade implant, a 28 × 20 mm artifact. | Although the selected dental appliances are safe when present in patients undergoing MRI, artifacts can substantially influence MRI results. |
| 32 | Savane et al. (2001) [ | Ti implants | 1.5 T MR unit, with 2 commonly used sequences (SE,GRE) | Minor artifacts, without distortions | In order to minimize ‘ghost images’, Ti and its alloys should be an alternative. |
| [Article in French] | |||||
| 33 | Abbaszadeh et al. (2000) [ | Dental Au, amalgam, S.S., Ti, Ag-Pa, & vitallium | T1-weighted MR imaging. | All metallic objects produced artifacts. Artifacts were most pronounced in the central plane of the object. Au produced the greatest artifacts; amalgam produced the least. | Because metals commonly used in the maxillofacial region produce artifacts on MR images, avoidance measures should be used to minimize these artifacts. |
| 34 | Tetsumura et al. (1999) [ | Minute metallic particles deposited during surgery may cause artifacts — 4 types of cutting instruments were used to cut an extracted tooth: a diamond bur attached to a rotor handpiece, a steel bur & bone bur attached to a micromotor handpiece & a bone file | 1.5 T; 6 MR sequences: SE, 2 TSE sequences, fast low angle short, turbo gradient SE, turbo inversion recovery sequences. | MR artifacts seen in tooth samples using the bone bur & bone file, but not the diamond & steel burs. | Artifacts seen on postoperative MRI were derived from minute metal particles from the bone bur or file used for condylar arthroplasty. Metal artifacts should be considered when interpreting postoperative MR images. |
| 35 | Borris et al. (1999) [ | Large ferromagnetic MRI artifacts were seen in the area of a previous mandibular osteotomy | - | MRI revealed multiple non-uniform halo-appearing teardrop-shaped areas associated with the mandibular ramus in the osteotomy area, visible in axial & coronal views. Surgical exploration revealed several minute hard & soft tissue specimens (foreign bodies). | Even tiny particles distort MR images leading to halo artifacts. Surgeons must be aware of foreign bodies implanted during surgery, and recognize their appearance. Dental restorations usually do not cause artifacts. |
| 36 | Devge et al. (1997) [ | Implants from the Brånemark System were tested | The ferromagnetic properties of implant materials are seldom described by the manufacturer. Important factors are alloy composition, size & shape of the metallic material, and its position in body. | Artifacts caused by implants were minor and did not jeopardize scan evaluation. However, magnet keepers attached to implants caused major artifacts. | Magnet keepers attached to implants must be removed before an implant patient is referred for MRI examination |
| 37 | Behr et al. (1996) [ | Cylindrical samples of 13 alloys & 14 pure substances (in plaster & water-filled acrylic resin phantom-representing disc & TMJ condyle were investigated) | SE & GRE sequence. | Metallic artifacts appeared on SE technique as distortions, and on gradient-echo technique signal loss could be observed. Precious alloys were diamagnetic. Non-precious alloys investigated were paramagnetic. | Paramagnetic alloys produce clinically relevant artifacts. |
| 38 | Beuf et al. (1994) [ | Cylindrical dental alloy samples incorporating gold, silver, and palladium (placed in a Pyrex beaker filled with distilled water) | 0.13 T using 2-dimensional Fourier transformation and projection reconstruction at 360° imaging methods. | Only palladium-based alloys were detected to be paramagnetic. One of the silver-based alloys did not induce detectable distortion because its susceptibility was very close to that of distilled water. | Use of this material may be recommended for applications involving MRI evaluation. |
| 39 | Iimuro (1994) [ | Specimens of each material were prepared as spheres & cylinders. Sphere samples with diameters of 1, 2, and 3 mm and 4 mm cylinders of 0.2, 0.3, 0.4, 0.6, 0.8 diameter and 1 mm height were prepared | 0.2 T; 3 sequences: short SE (TR-300, TE-38), long SE (TR-500, TE-110) and GRE (TR-200, TE-23, flip angle 60) were used. Images were taken in the coronal, sagittal & transverse planes. | During MRI, artifacts were not caused by the magnet itself, but by the S.S. keeper (ferromagnetic). Short & long SE sequences resulted in the same artifact range (distortion; further from the specimen, distortion was attenuated); the gradient-echo sequence caused a larger image artifact (signal loss/blackout). The image around the most severely deformed area was quite distorted, but the structures could be distinguished. | The higher the magnetic permeability, the greater the artifact produced. The size and volume of the material directly influence the artifact produced. Artifact size can be attenuated by the sequence used to obtain images. In vitro and in vivo results suggest that even in patients with a magnetic attachment system, MRI is the diagnostic method of choice. Possible solutions to reduce the artifact range are to find alternative keeper materials with a lower magnetic permeability; or to design the keeper in such a manner that it can be removed easily. |
| 40 | Oikarinen et al. (1993) [ | 4 samples of different sizes of fractured tooth crown, pieces of amalgam, glass, asphalt, composite, dry wood, and stone (embedded in soft tissue) | 1 T; T1 and T2 weighted and proton-density images. | MRI was the least suitable imaging method, as particles with a metallic content gave rise to artifacts. Foreign body particles in soft tissue were better defined in form & size with CT & ultrasonography than with MRI or plain radiography. | When plain radiographs, history, and clinical examination fail to reveal the presence of superficial foreign bodies, ultrasonography or CT can serve as an alternative method that is preferable to MRI. |
| 41 | Laurell et al. (1989) [ | 8 types of prosthetic magnet keepers of the disc and bar type | 1.5 T, with partial saturation pulse sequence. | Image artifacts present in all 8 samples (160–280 mm diameter). Artifacts obliterated vital cranio-cervical areas. For bar keepers & Jackson disc keepers, artifacts partially/totally obliterated eye & brain images. Other disc keepers degraded eye images, but not brain or cervical spine images. | The ferromagnetic potential of magnetic keepers caused sufficient localized alterations of the magnetic field, leading to signal loss. Patients with magnetic keepers requiring comprehensive head & neck MRI must have them removed. |
| 42 | Sadowsky et al. (1988) [ | 5 patients with fixed appliances in maxillary & mandibular arches undergoing MRI scans of brain & TMJ | T1-weighted scan; transverse multi-echo sequence of the brain. | Orthodontic appliances produced MR artifacts in the facial region (mouth & maxillary sinus). The frontal & temporal lobes of the brain were most affected, but the degree of the artifact varied from patient to patient. Artifacts were not severe enough to alter the diagnostic scan quality. On TMJ scans, no degradation was detected. | Phantom studies indicated that orthodontic arch wires increased distortion & artifacts. All banded & bonded attachments should be checked for firm attachment to the teeth or passively ligated with elastic chains for added safety. Eliminating all removable components of appliances (arch wires) ensures a diagnostic scan. Complete removal of metallic appliances is not needed unless the region of interest is close to the mouth. |
T, tesla; S.S., stainless steel; Ti, titanium; Co-Cr, cobalt-chromium; Zr, zirconium; CT = computed tomography; CBCT, cone-beam computed tomography; SPACE, sampling perfection with application optimized contrasts using different flip angle evolution; TSE, turbo spin-echo; T1W1, T1-weighted; T2W1, T2-weighted; TMJ, temporomandibular joint; Au, gold; Ag, silver; Pd, palladium; Pt, platinum; Cd, cadmium; NdFeB magnet, neodymium iron boron magnet; SmCo magnet, samarium cobalt magnet; PdCo, palladium cobalt magnet; GRE, gradient echo; PFM, porcelain-fused-to-metal; GRASS, gradient-recalled acquisition in steady state; SPGR, spoiled GRASS; Al, aluminum; Ni-Cr, nickel-chromium alloy; FSPGR, fast SPGR; SE, spin-echo; UTE, ultrashort-echo time; TE, echo time; EPI, echoplanar imaging; DWI, diffusion-weighted imaging; RF, radiofrequency; FLAIR, fluid attenuated inversion recovery; FPD, fixed partial denture; TR, repetition time; FIESTA, fast imaging employing steady state; EPI, echo planar imaging.
Recommendations for the removal of orthodontic appliances based on the type of material
| Appliance type | Magnitude of artifact | Recommendations for appliance removal |
|---|---|---|
| Ceramic brackets with metal slot and titanium brackets | Very limited or no artifacts | Removal is only necessary if the area under investigation is close to fixed appliances (i.e., in the oral cavity). |
| Fixed retainers containing steel | Poor image quality in the area of the oral cavity only | Removal is only necessary ahead of an MRI scan if the area under investigation is within the oral cavity. |
| Stainless steel brackets | Extensive artifacts in the oral cavity and other areas (TMJ, posterior cerebral fossa, maxillary sinus), images uninterpretable | Removal is always necessary before MRI images of the head and neck area are taken. |
MRI, magnetic resonance imaging; TMJ, temporomandibular joint.
MRI, magnetic resonance imaging; χ, magnetic susceptibility (synonym = magnetizability); µ, magnetic permeability, µ = 1 + χ.
χ, magnetic susceptibility (synonym = magnetizability); SE, spin-echo; GRE, gradient-echo; compatible I, 3 < Δx < 200 ppm; material produces noticeable distortions, acceptability depends on application.
MRI, magnetic resonance imaging; GRE, gradient echo; SE, spin-echo.
T, tesla; S.S., stainless steel; Ti, titanium; Co-Cr, cobalt-chromium; Zr, zirconium; CT = computed tomography; CBCT, cone-beam computed tomography; SPACE, sampling perfection with application optimized contrasts using different flip angle evolution; TSE, turbo spin-echo; T1W1, T1-weighted; T2W1, T2-weighted; TMJ, temporomandibular joint; Au, gold; Ag, silver; Pd, palladium; Pt, platinum; Cd, cadmium; NdFeB magnet, neodymium iron boron magnet; SmCo magnet, samarium cobalt magnet; PdCo, palladium cobalt magnet; GRE, gradient echo; PFM, porcelain-fused-to-metal; GRASS, gradient-recalled acquisition in steady state; SPGR, spoiled GRASS; Al, aluminum; Ni-Cr, nickel-chromium alloy; FSPGR, fast SPGR; SE, spin-echo; UTE, ultrashort-echo time; TE, echo time; EPI, echoplanar imaging; DWI, diffusion-weighted imaging; RF, radiofrequency; FLAIR, fluid attenuated inversion recovery; FPD, fixed partial denture; TR, repetition time; FIESTA, fast imaging employing steady state; EPI, echo planar imaging.
MRI, magnetic resonance imaging; TMJ, temporomandibular joint.

 KACD
KACD
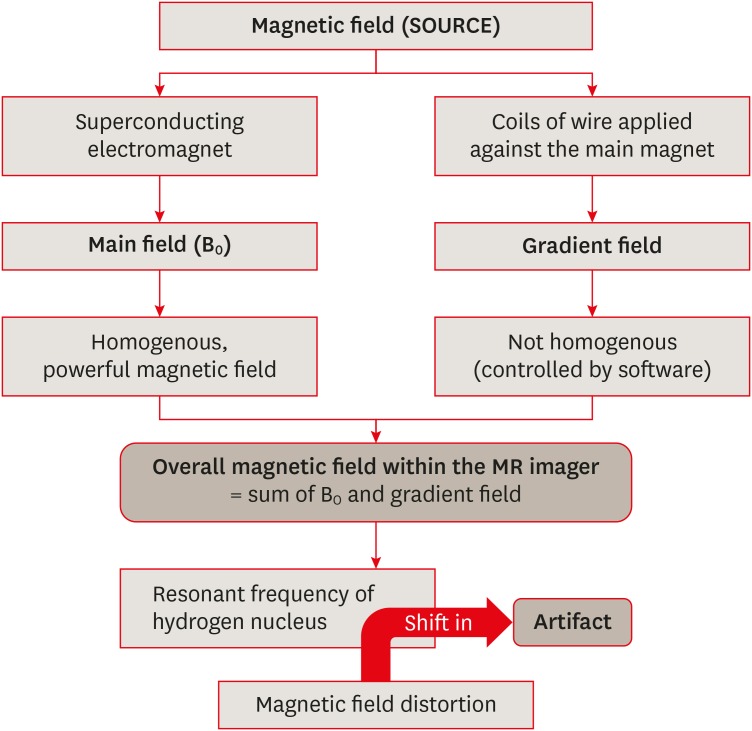
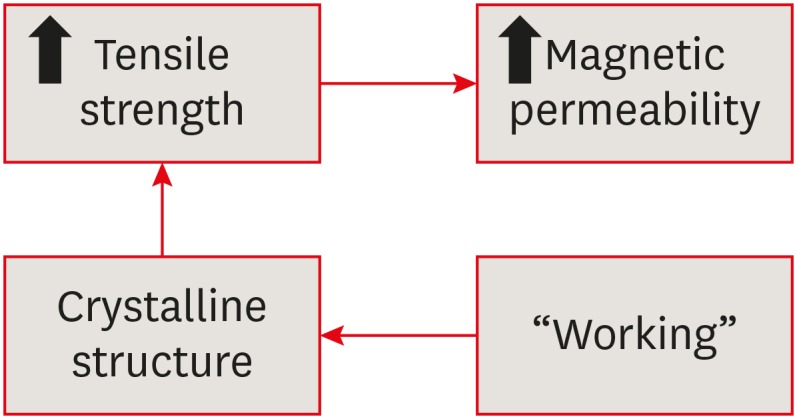
 ePub Link
ePub Link Cite
Cite

