Articles
- Page Path
- HOME > Restor Dent Endod > Volume 43(2); 2018 > Article
- Research Article Effect of ultrasonic agitation on push-out bond strength and adaptation of root-end filling materials
-
Murilo Priori Alcalde1
 , Rodrigo Ricci Vivan1
, Rodrigo Ricci Vivan1 , Marina Angélica Marciano2
, Marina Angélica Marciano2 , Jussaro Alves Duque1
, Jussaro Alves Duque1 , Samuel Lucas Fernandes1
, Samuel Lucas Fernandes1 , Mariana Bailo Rosseto1
, Mariana Bailo Rosseto1 , Marco Antonio Hungaro Duarte1
, Marco Antonio Hungaro Duarte1
-
Restor Dent Endod 2018;43(2):e23.
DOI: https://doi.org/10.5395/rde.2018.43.e23
Published online: April 27, 2018
1Department of Restorative Dentistry, Dental Materials and Endodontics, Bauru Dental School, University of São Paulo, Bauru, SP, Brazil.
2Department of Restorative Dentistry, School of Dentistry of Piracicaba, State University of Campinas, Piracicaba, SP, Brazil.
- Correspondence to: Jussaro Alves Duque, DDS, MS. PhD Student, Department of Restorative Dentistry, Dental Materials and Endodontics, Bauru Dental School, University of São Paulo, Al. Octávio Pinheiro Brisola No. 9-75 Bauru, SP 17012-901, Brazil. jussaroduque@usp.br
Copyright © 2018. The Korean Academy of Conservative Dentistry
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 1,699 Views
- 12 Download
- 10 Crossref
Abstract
-
Objectives This study evaluated the effect of ultrasonic agitation of mineral trioxide aggregate (MTA), calcium silicate-based cement (CSC), and Sealer 26 (S26) on adaptation at the cement/dentin interface and push-out bond strength.
-
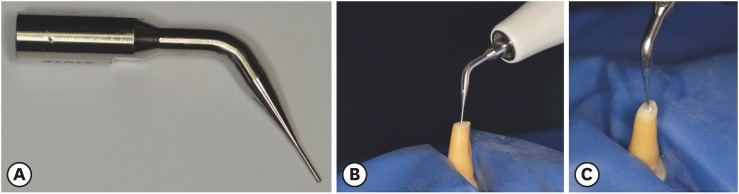
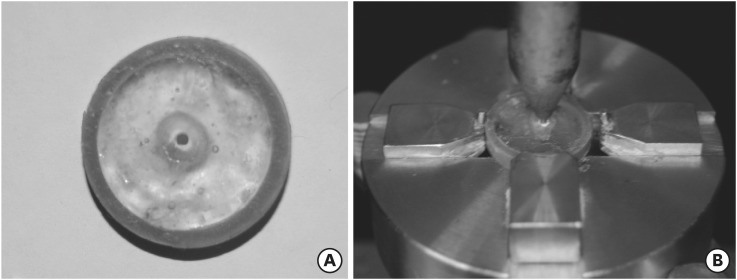
Materials and Methods Sixty maxillary canines were divided into 6 groups (n = 10): MTA, S26, and CSC, with or without ultrasonic activation (US). After obturation, the apical portions of the teeth were sectioned, and retrograde cavities were prepared and filled with cement by hand condensation. In the US groups, the cement was activated for 60 seconds: 30 seconds in the mesio-distal direction and 30 seconds in the buccal-lingual direction, using a mini Irrisonic insert coupled with the ultrasound transducer. After the materials set, 1.5-mm thick sections were obtained from the apexes. The presence of gaps and the bond between cement and dentin were analyzed using low-vacuum scanning electron microscopy. Push-out bond strength was measured using a universal testing machine.
-
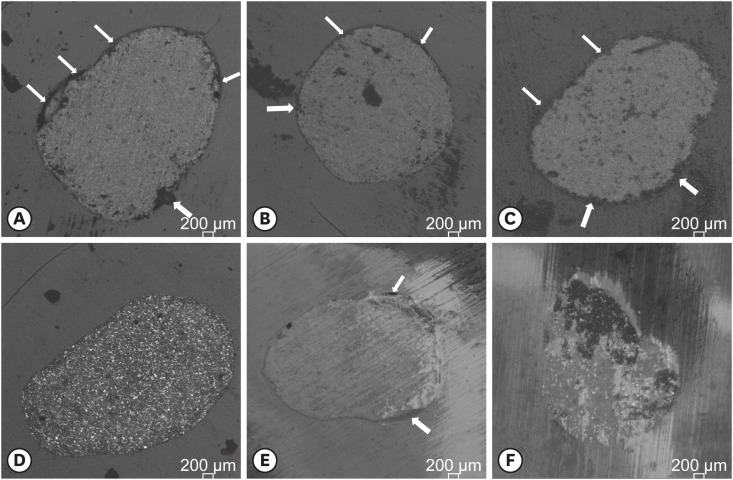
Results Ultrasonic agitation increased the interfacial adaptation of the cements. The S26 US group showed a higher adaptation value than MTA (p < 0.05). US improved the push-out bond strength for all the cements (p < 0.05).
-
Conclusions The US of retrograde filling cements enhanced the bond to the dentin wall of the root-end filling materials tested.
INTRODUCTION
MATERIALS AND METHODS
Mini Irrisonic tip used for ultrasonic activation (US) of the cements (A). US of the cement on retrograde cavity in the lateral (B) and top views (C). Images depicting agitation of the filling materials.
(A) Illustrative image of a specimen fixed in polyester resin and horizontally sectioned. (B) Illustrative image of a specimen fixed on the metal apparatus with a vertical force applied in the middle of the canal using the metal point of the test machine.
RESULTS
Median, minimum, and maximum values of interfacial adaptation (gaps in dentin/cement interface) and number of samples according to the type of failure
Representative images of interfacial adaptation at ×50 magnification by scanning electron microscope in the (A) mineral trioxide aggregate (MTA), (B) MTA/ultrasonic activation (US), (C) calcium silicate-based cement (CSC), (D) CSC/US, (E) Sealer 26 (S26), and (F) S26/US groups. The white arrows indicate the presence of interfacial gaps.
Push-out bond strength of the tested cements to dentin
| Group | Bond strength (MPa) |
|---|---|
| S26 | 2.264 ± 0.973a |
| S26 US | 4.072 ± 1.103b |
| MTA | 1.770 ± 1.114a |
| MTA US | 3.208 ± 0.674b |
| CSC | 2.241 ± 0.673a |
| CSC US | 4.018 ± 1.113b |
DISCUSSION
CONCLUSIONS
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Vivan RR, Duarte MAH.
Data curation: Alcalde MP, Fernandes SL, Rosseto MB.
Formal analysis: Alcalde MP, Fernandes SL, Rosseto MB.
Funding acquisition: Vivan RR, Duarte MAH.
Investigation: Alcalde MP, Fernandes SL, Rosseto MB.
Methodology: Alcalde MP, Fernandes SL, Rosseto MB.
Project administration: Vivan RR, Duarte MAH.
Resources: Vivan RR, Duarte MAH.
Software: Marciano MA, Duque JA.
Supervision: Vivan RR, Duarte MAH.
Validation: Vivan RR, Duarte MAH.
Visualization: Marciano MA, Duque JA.
Writing - original draft: Marciano MA, Duque JA.
Writing - review & editing: Marciano MA, Duque JA.
- 1. Friedman S, Rotstein I, Koren L, Trope M. Dye leakage in retrofilled dog teeth and its correlation with radiographic healing. J Endod 1991;17:392-395.ArticlePubMed
- 2. Lee SJ, Monsef M, Torabinejad M. Sealing ability of a mineral trioxide aggregate for repair of lateral root perforations. J Endod 1993;19:541-544.ArticlePubMed
- 3. Maroto M, Barbería E, Planells P, García Godoy F. Dentin bridge formation after mineral trioxide aggregate (MTA) pulpotomies in primary teeth. Am J Dent 2005;18:151-154.PubMed
- 4. Duarte MAH, Alves de Aguiar K, Zeferino MA, Vivan RR, Ordinola-Zapata R, Tanomaru-Filho M. Evaluation of the propylene glycol association on some physical and chemical properties of mineral trioxide aggregate. Int Endod J 2012;45:565-570.ArticlePubMed
- 5. Salem Milani A, Froughreyhani M, Charchi Aghdam S, Pournaghiazar F, Asghari Jafarabadi M. Mixing with propylene glycol enhances the bond strength of mineral trioxide aggregate to dentin. J Endod 2013;39:1452-1455.ArticlePubMed
- 6. Camilleri J. Hydration mechanisms of mineral trioxide aggregate. Int Endod J 2007;40:462-470.ArticlePubMed
- 7. Coomaraswamy KS, Lumley PJ, Hofmann MP. Effect of bismuth oxide radioopacifier content on the material properties of an endodontic Portland cement-based (MTA-like) system. J Endod 2007;33:295-298.ArticlePubMed
- 8. Marciano MA, Costa RM, Camilleri J, Mondelli RF, Guimarães BM, Duarte MAH. Assessment of color stability of white mineral trioxide aggregate angelus and bismuth oxide in contact with tooth structure. J Endod 2014;40:1235-1240.ArticlePubMed
- 9. Cutajar A, Mallia B, Abela S, Camilleri J. Replacement of radiopacifier in mineral trioxide aggregate; characterization and determination of physical properties. Dent Mater 2011;27:879-891.ArticlePubMed
- 10. Duarte MAH, de Oliveira El Kadre GD, Vivan RR, Guerreiro Tanomaru JM, Tanomaru Filho M, de Moraes IG. Radiopacity of portland cement associated with different radiopacifying agents. J Endod 2009;35:737-740.ArticlePubMed
- 11. Marciano MA, Duarte MAH, Camilleri J. Calcium silicate-based sealers: Assessment of physicochemical properties, porosity and hydration. Dent Mater 2016;32:e30-e40.ArticlePubMed
- 12. Camilleri J, Grech L, Galea K, Keir D, Fenech M, Formosa L, Damidot D, Mallia B. Porosity and root dentine to material interface assessment of calcium silicate-based root-end filling materials. Clin Oral Investig 2014;18:1437-1446.ArticlePubMedPDF
- 13. Camilleri J, Sorrentino F, Damidot D. Investigation of the hydration and bioactivity of radiopacified tricalcium silicate cement, Biodentine and MTA Angelus. Dent Mater 2013;29:580-593.ArticlePubMed
- 14. Bernardes RA, de Amorim Campelo A, Junior DS, Pereira LO, Duarte MAH, Moraes IG, Bramante CM. Evaluation of the flow rate of 3 endodontic sealers: Sealer 26, AH Plus, and MTA obtura. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010;109:e47-e49.Article
- 15. Duarte MAH, Demarchi AC, Giaxa MH, Kuga MC, Fraga SC, de Souza LC. Evaluation of pH and calcium ion release of three root canal sealers. J Endod 2000;26:389-390.ArticlePubMed
- 16. Siqueira JF, Roças IN, Valois CR. Apical sealing ability of five endodontic sealers. Aust Endod J 2001;27:33-35.ArticlePubMed
- 17. Tanomaru-Filho M, Luis MR, Leonardo MR, Tanomaru JM, Silva LA. Evaluation of periapical repair following retrograde filling with different root-end filling materials in dog teeth with periapical lesions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;102:127-132.ArticlePubMed
- 18. Harrison AJ, Chivatxaranukul P, Parashos P, Messer HH. The effect of ultrasonically activated irrigation on reduction of Enterococcus faecalis in experimentally infected root canals. Int Endod J 2010;43:968-977.ArticlePubMed
- 19. Huffaker SK, Safavi K, Spangberg LS, Kaufman B. Influence of a passive sonic irrigation system on the elimination of bacteria from root canal systems: a clinical study. J Endod 2010;36:1315-1318.ArticlePubMed
- 20. Duarte MAH, Balan NV, Zeferino MA, Vivan RR, Morais CA, Tanomaru-Filho M, Ordinola-Zapata R, Moraes IG. Effect of ultrasonic activation on pH and calcium released by calcium hydroxide pastes in simulated external root resorption. J Endod 2012;38:834-837.ArticlePubMed
- 21. Guimarães BM, Amoroso-Silva PA, Alcalde MP, Marciano MA, de Andrade FB, Duarte MAH. Influence of ultrasonic activation of 4 root canal sealer on the filling quality. J Endod 2014;40:964-968.PubMed
- 22. Aminoshariae A, Hartwell GR, Moon PC. Placement of mineral trioxide aggregate using two different techniques. J Endod 2003;29:679-682.ArticlePubMed
- 23. Yeung P, Liewehr FR, Moon PC. A quantitative comparison of the fill density of MTA produced by two placement techniques. J Endod 2006;32:456-459.ArticlePubMed
- 24. Bernabé PF, Gomes-Filho JE, Bernabé DG, Nery MJ, Otoboni-Filho JA, Dezan E Jr, Cintra LT. Sealing ability of MTA used as a root end filling material: effect of the sonic and ultrasonic condensation. Braz Dent J 2013;24:107-110.ArticlePubMed
- 25. Schneider SW. A comparison of canal preparations in straight and curved root canals. Oral Surg Oral Med Oral Pathol 1971;32:271-275.ArticlePubMed
- 26. Vivan RR, Guerreiro-Tanomaru JM, Bosso-Martelo R, Costa BC, Duarte MAH, Tanomaru-Filho M. Push-out bond strength of root-end filling materials. Braz Dent J 2016;27:332-335.ArticlePubMed
- 27. Basturk FB, Nekoofar MH, Günday M, Dummer PM. The effect of various mixing and placement techniques on the compressive strength of mineral trioxide aggregate. J Endod 2013;39:111-114.ArticlePubMed
- 28. Duque JA, Fernandes SL, Bubola JP, Duarte MAH, Camilleri J, Marciano MA. The effect of mixing method on tricalcium silicate-based cement. Int Endod J 2018;51:69-78.ArticlePubMedPDF
- 29. Xavier CB, Weismann R, de Oliveira MG, Demarco FF, Pozza DH. Root-end filling materials: apical microleakage and marginal adaptation. J Endod 2005;31:539-542.ArticlePubMed
- 30. Maltezos C, Glickman GN, Ezzo P, He J. Comparison of the sealing of Resilon, Pro Root MTA, and Super-EBA as root-end filling materials: a bacterial leakage study. J Endod 2006;32:324-327.ArticlePubMed
REFERENCES
Tables & Figures
REFERENCES
Citations

- Effect of ultrasonic activation on setting time, pH and calcium ion release, solubility, and chemical structure of calcium silicate sealers
Simone Argenta Scalabrin, Lina Naomi Hashizume, Theodoro Weissheimer, Gabriel Barcelos Só, Jefferson Ricardo Pereira, Milton Carlos Kuga, Ricardo Abreu da Rosa, Marcus Vinicius Reis Só
Brazilian Dental Journal.2024;[Epub] CrossRef - Impact of different disinfection protocols on the bond strength of NeoMTA 2 bioceramic sealer used as a root canal apical plug (in vitro study)
Nada Omar, Nihal Refaat Kabel, Muhammad Abbass Masoud, Tamer M. Hamdy
BDJ Open.2024;[Epub] CrossRef - Effect of Endo-Z bur or Bladesonic ultrasonic tip on the adaptation of filling material. A micro-CT study
Pedro Henrique Fiorin de Souza, Airton Oliveira Santos-Junior, Jáder Camilo Pinto, Karina Ines Medina Carita Tavares, Juliane Maria Guerreiro-Tanomaru, Mário Tanomaru-Filho
Brazilian Dental Journal.2023; 34(5): 29. CrossRef - Effect of Different Mixing Methods on Physicochemical Properties of Mineral Trioxide Aggregate: A Systematic Review
Amin Salem Milani, Faraz Radmand, Behrad Rahbani, Mahdi Hadilou, Farnaz Haji Abbas Oghli, Fatemeh Salehnia, Milad Baseri, Stefano Pagano
International Journal of Dentistry.2023; 2023: 1. CrossRef - Micro-CT comparative evaluation of porosity and dentin adaptation of root end filling materials applied with incremental, bulk, and ultrasonic activation techniques
Berkan Celikten, Aysenur Oncu, Mehrdad Koohnavard, Mert Ocak, Kaan Orhan
Proceedings of the Institution of Mechanical Engineers, Part H: Journal of Engineering in Medicine.2022; 236(8): 1209. CrossRef - Effect of ultrasonic activation of the adhesive system on dentin tubule penetration and the pushout bond strength of fiber posts
Isabel Verdum, Igor Abreu de Bem, Pedro Henrique Marks Duarte, Lucas Silveira Machado, Jefferson Ricardo Pereira, Marcus Vinícius Reis Só, Ricardo Abreu da Rosa
The Journal of Prosthetic Dentistry.2022; 127(2): 295. CrossRef - Influence of Ultrasonic Activation on the Physicochemical Properties of Calcium Silicate-Based Cements
Fredson Márcio Acris De Carvalho, Yara Teresinha Corrêa Silva-Sousa, Carlos Eduardo Saraiva Miranda, Paulo Henrique Miller Calderon, Ana Flávia Simões Barbosa, Luciana Martins Domingues De Macedo, Fuad Jacob Abi Rached-Junior, Boonlert Kukiattrakoon
International Journal of Dentistry.2021; 2021: 1. CrossRef - Micro-computed tomographic evaluation of the flow and filling ability of endodontic materials using different test models
Fernanda Ferrari Esteves Torres, Juliane Maria Guerreiro-Tanomaru, Gisselle Moraima Chavez-Andrade, Jader Camilo Pinto, Fábio Luiz Camargo Villela Berbert, Mario Tanomaru-Filho
Restorative Dentistry & Endodontics.2020;[Epub] CrossRef - Dental discoloration caused by Grey-MTAFlow cement: analysis of its physicochemical, biological and antimicrobial properties
Lauter Eston PELEPENKO, Flávia SAAVEDRA, Gabriela Fernanda BOMBARDA, Brenda Paula Figueiredo de Almeida GOMES, Adriana DE-JESUS-SOARES, Alexandre Augusto ZAIA, Marco Antonio Hungaro DUARTE, Mario TANOMARU-FILHO, Marina Angélica MARCIANO
Journal of Applied Oral Science.2020;[Epub] CrossRef - Effect of Ultrasonic Activation of Endodontic Sealers on Intratubular Penetration and Bond Strength to Root Dentin
Igor Abreu De Bem, Renata Aqel de Oliveira, Theodoro Weissheimer, Carlos Alexandre Souza Bier, Marcus Vinícius Reis Só, Ricardo Abreu da Rosa
Journal of Endodontics.2020; 46(9): 1302. CrossRef
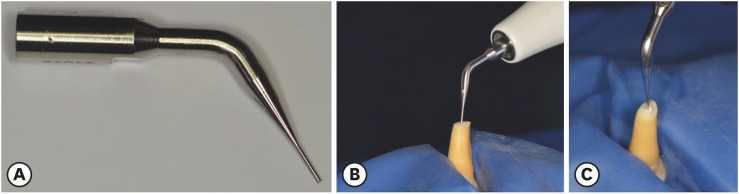
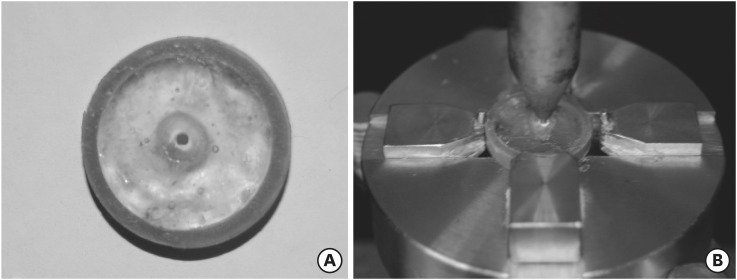
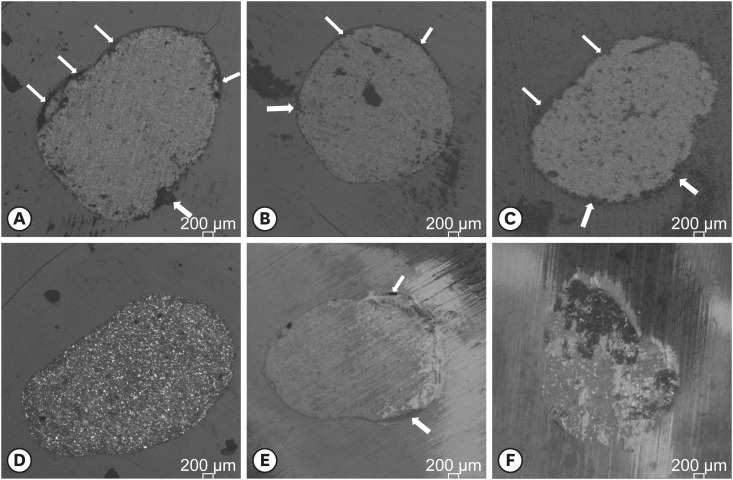
Figure 1
Figure 2
Figure 3
Median, minimum, and maximum values of interfacial adaptation (gaps in dentin/cement interface) and number of samples according to the type of failure
| Group | Gap (µm) | Failure | ||
|---|---|---|---|---|
| Adhesive | Cohesive | Mixed | ||
| MTA | 6.79 (0.00–27.10)a | 7 | 2 | 1 |
| MTA US | 1.90 (0.00–17.34)ab | 8 | 1 | 1 |
| S26 | 1.18 (0.00–8.40)ab | 7 | 1 | 2 |
| S26 US | 0.00 (0.00–4.75)b | 6 | 2 | 2 |
| CSC | 4.66 (0.00–15.08)ab | 7 | 1 | 2 |
| CSC US | 1.15 (0.00–13.04)ab | 8 | 0 | 2 |
Different lowercase superscript letters indicate statistically significant differences between groups (p < 0.05).
MTA, mineral trioxide aggregate; US, ultrasound activation; S26, Sealer 26; CSC, calcium silicate-based cement.
Push-out bond strength of the tested cements to dentin
| Group | Bond strength (MPa) |
|---|---|
| S26 | 2.264 ± 0.973a |
| S26 US | 4.072 ± 1.103b |
| MTA | 1.770 ± 1.114a |
| MTA US | 3.208 ± 0.674b |
| CSC | 2.241 ± 0.673a |
| CSC US | 4.018 ± 1.113b |
Data were presented in means ± standard deviations.
Different lowercase superscript letters represent signifcant differences among the groups (p < 0.05).
S26, Sealer 26; US, ultrasound activation; MTA, mineral trioxide aggregate; CSC, calcium silicate-based cement.
Different lowercase superscript letters indicate statistically significant differences between groups (
MTA, mineral trioxide aggregate; US, ultrasound activation; S26, Sealer 26; CSC, calcium silicate-based cement.
Data were presented in means ± standard deviations.
Different lowercase superscript letters represent signifcant differences among the groups (
S26, Sealer 26; US, ultrasound activation; MTA, mineral trioxide aggregate; CSC, calcium silicate-based cement.

 KACD
KACD
 ePub Link
ePub Link Cite
Cite

