Articles
- Page Path
- HOME > Restor Dent Endod > Volume 40(2); 2015 > Article
- Case Report Surgical management with intentional replantation on a tooth with palato-radicular groove
- Jorge Forero-López1, Luis Gamboa-Martínez1, Laura Pico-Porras1, Javier Laureano Niño-Barrera1,2
-
2014;40(2):-171.
DOI: https://doi.org/10.5395/rde.2015.40.2.166
Published online: December 22, 2014
1Department of Endodontics, Universidad El Bosque School of Dentistry, Bogotá, Colombia.
2Universidad Nacional de Colombia School of Dentistry, Bogotá, Colombia.
- Correspondence to Javier Laureano Niño-Barrera, DDS, MSc. Professor, Department of Endodontics, Universidad El Bosque School of Dentistry and Universidad Nacional de Colombia School of Dentistry, Calle 135 #58b-21 Interior 2 Apartamento 302. Bogotá, Colombia. TEL, +57-300-3195998; FAX, +571 3165000; jlninob@unal.edu.co
• Received: August 4, 2014 • Accepted: November 7, 2014
©Copyrights 2015. The Korean Academy of Conservative Dentistry.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 2,159 Views
- 11 Download
- 22 Crossref
Abstract
- A palato-radicular groove (PRG) is a developmental anomaly primarily found in the maxillary lateral incisors. It is a potential communication path between the root canal and the periodontium that decreases the survival prognosis of the affected tooth, therefore compromising the stability of the dental structure in the oral cavity. The aim of this case report is to present an original technique where a PRG was treated by means of intracanal disinfection, PRG sealing with glass ionomer, replantation with intentional horizontal 180 degree rotation of the tooth, and an aesthetic veneer placed to provide adequate tooth morphology. The clinical and biological benefits of this novel technique are presented and discussed.
Introduction
A palato-radicular groove (PRG) is a developmental abnormality primarily found in the maxillary lateral incisor.1,2 This irregularity, which is considered a potential communication path between the root canal and the periodontium, clearly decreases the survival rate of the affected tooth.2 As a consequence of this connection, the PRG acts as an expedient route for nutrients to reach bacteria in the root canal and surrounding tissues. These bacteria colonize the tooth surface to form biofilms, and eventually lead to bone loss, thus compromising the stability of the dental structure in the mouth.1,2,3
From the embryological point of view, the PRG has been developed as a consequence of the alteration in the growth of the inner enamel epithelium and Hertwig's epithelial root sheath. It has also been considered the result of a failed attempt to form a dens invaginatus or an unsuccessful trial of the body to develop another root of the altered tooth.3,4,5,6 This anatomical aberration usually starts at the cingulum, advances distoapically, and ends at different levels on the root. The clinical relevance of this situation is that it influences the prognosis of the tooth, as it is directly related to the length, depth, and the time of development.3,7,8,9
The incidence of PRG ranges from 2.8% to 18%, with the latter corresponding to reports on Chinese population, who have a particularly high incidence.5,10 In 1991 Goon et al. classified PRG into two main categories, simple and complex grooves.3 While a simple groove partially communicates the root canal with the periodontium and does not extend lengthwise in depth, a complex groove communicates the root canal with the periodontium directly and extends lengthwise through the root. The aim of PRG treatment is to achieve adequate root surface sealing in order to prevent communication between the periodontium and the root canal.6,9,11,12,13,14,15,16
The purpose of this case report is to present a novel technique where a PRG was treated by means of intracanal disinfection, PRG sealing with glass ionomer, replantation with intentional horizontal 180 degree rotation, and an aesthetic veneer placed to provide adequate tooth anatomy. The clinical and biological benefits of the technique are presented and discussed as well.
Case Report
A 25 year-old male patient presented to the Department of Endodontics at the Universidad El Bosque School of Dentistry in Bogotá, Colombia with the chief complaint of acute pain, inflammation, and purulent exudate of the upper right lateral incisor since three days ago. Inquiry into the patient's medical history showed that he was an otherwise healthy person who had been taking Amoxicillin and Ibuprofen for the past few days. Dental history revealed that he had finished orthodontic treatment 30 days before presenting to the Department of Endodontics.
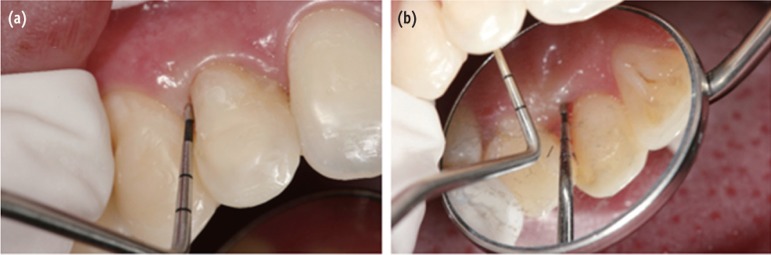
Intra-oral examination revealed a moderate swelling on the gingival papilla between the upper right lateral incisor and the ipsilateral canine, localized bleeding on probing, subgingival calculus, and tooth mobility of grade II. Additionally, a 12 mm probing depth at the distopalatal area of the upper right lateral incisor associated to a PRG was documented. Pulp vitality tests were within normal limits. A periapical radiograph showed a radiolucent area on the distal surface of the crown associated to a PRG found in the lateral incisor (Figure 1a). A single root canal and a distal alveolar bone loss at the level of the periodontium were observed in the root, showing approximately 10 mm radiolucent image at the apical 1/3 of the root (Figure 1b). Clinical and radiographic findings were consistent with apical periodontitis associated to a PRG. Prognosis was regarded as poor.
Based on the clinical, radiographic, and expectations of the patient, the following treatment plan was proposed: 1) Scaling and root planing (SRP) to eliminate subgingival calculi, 2) Initial intracanal antibiotic medication followed by conventional root canal therapy (RCT) to eliminate bacteria, 3) Minimally-invasive extraction of the upper right lateral incisor, 4) Sealing of the PRG, 5) Replantation with intentional horizontal 180 degree rotation of the tooth, and 6) An aesthetic veneer placed to provide an adequate tooth anatomy.17 The procedures were carefully explained to the patient, who understood the benefits and risks of the proposed treatment plan.
After informed consent, the hygienic phase took place under local anesthesia with 2% lidocaine (Ropsohn Laboratorios, Bogotá, Colombia). Root canal instrumentation was performed using the crown down technique up to the size 25 endodontic K-file (Dentsply Maillefer, Ballaigues, Switzerland). The tooth was filled with a provisional material (Coltosol F, Coltène/Whaledent AG, Switzerland). On the next appointment, removal of the provisional filling material and root canal irrigation with 5.25% sodium hypochlorite was performed. Manual instrumentation followed to reach the master apical file (MAF) of size 35 (Figure 1c). Intracanal medication consisting of a composite paste of two antibiotics and a steroid (Clindamycin, Metronidazole, and Clobetasol) was placed. This medication was maintained for a month. Finally, a cotton swab and a provisional filling material (Coltosol F) were placed to provide adequate sealing. The patient returned after 30 days in order to have the PRG sealed. This was accomplished by minimally-invasive extraction of the upper right lateral incisor under the local anesthesia.
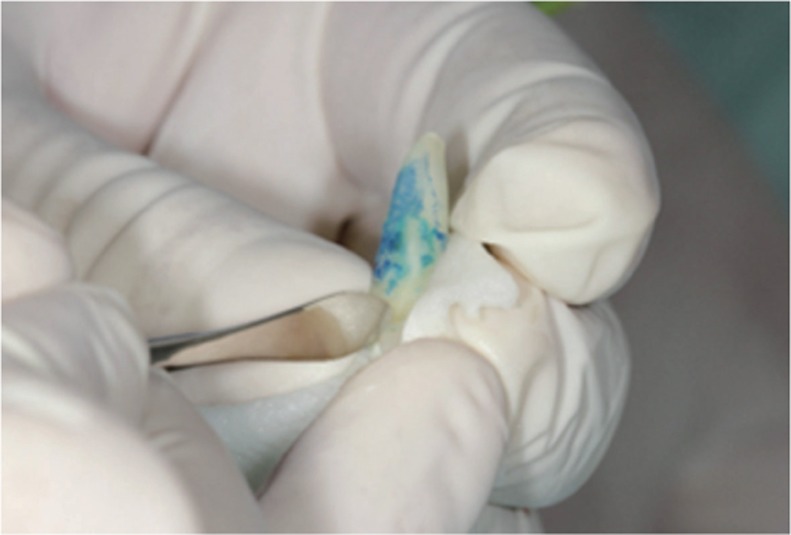
In order to have a better visualization of the PRG, the tooth was stained with methylene blue and observed under a light microscope (Seiler 202 ENT Surgical Microscope, Seiler Instruments, St. Louis, MO, USA). While holding the stained tooth firmly, the PRG was prepared as conservatively as possible using a tapered diamond bur, dried with paper tips, and sealed with Vitremer (3M ESPE, St. Paul, MN, USA) as depicted in Figure 2. The tooth, which remained outside of the socket for 8 minutes, was then replanted with a 180 degree rotation using mild digital pressure. The alveolus did not require any special preparation (Figure 3a).
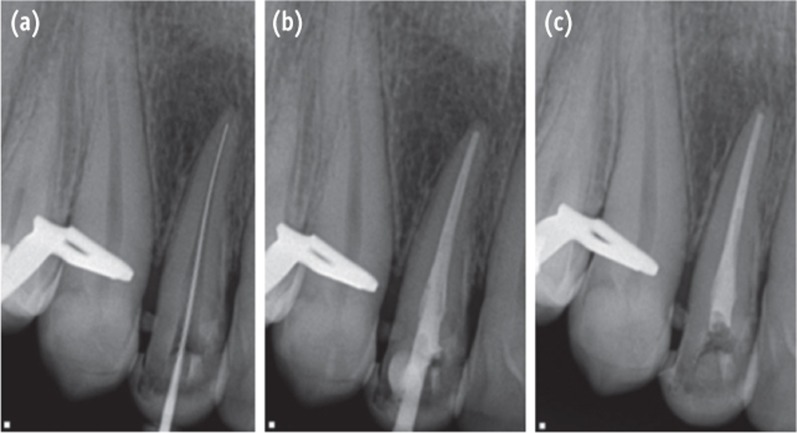
The aesthetic details were completed by performing a slight incisal reduction and restored with composite resin to reconstruct the facial morphology, followed by a vestibular nylon semi-rigid splint from the central incisor to the canine (Figure 3b). Three hundred mg of Clindamycin and 500 mg of Acetaminophen were prescribed. The patient, who healed uneventfully, returned to our Department after 15 days for splint removal. Two months later, a scaling and root planing (SRP) was performed. At the following appointment, the final, conventional RCT was performed (Figures 4a and 4b).
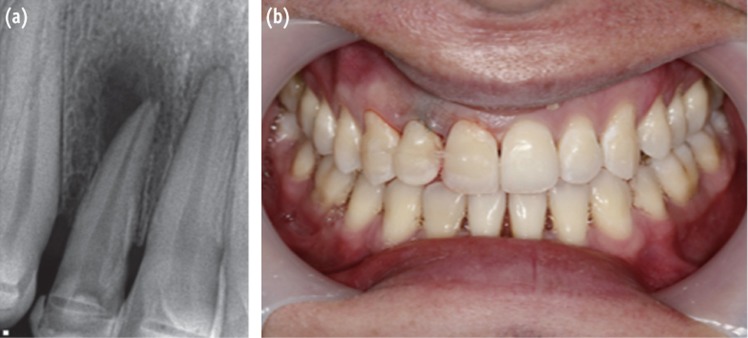
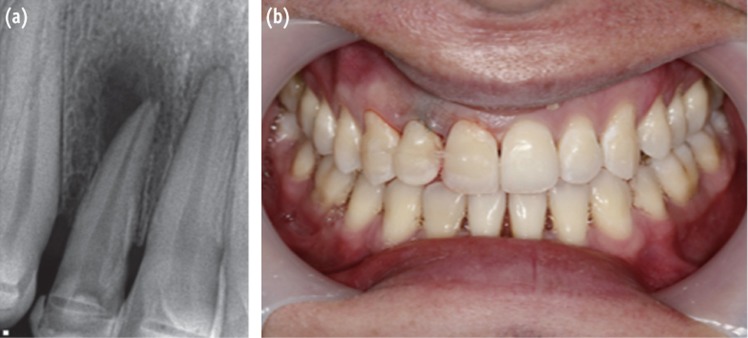
The canal was prepared with the Reciproc System (VDW, Munich, Germany), and the access cavity was sealed with a sealing material (Roekoseal, Coltène/Whaledent AG). The tooth was restored with a composite resin veneer (Filtek P60 Posterior Restorative System, 3M ESPE, Figure 4c). After 3 months, the patient was asymptomatic and did not show either periodontal pocket or evidence of recurrence of the apical lesion. He was satisfied with the functional and esthetic results (Figures 5a and 5b). He was placed on a 3 month follow-up schedule.
Discussion
In this case report we presented an original method for treating PRG by way of intracanal disinfection, PRG sealing with glass ionomer, replantation with intentional horizontal 180 degree rotation, and an aesthetic veneer placed to provide adequate tooth anatomy. To the best of our knowledge, this is the first time this combination of techniques is reported in the scientific literature. The current philosophy for PRG treatment is based on surgical procedures that allow defect sealing9,11,12,13,14,15,16 either by performing an intentional replantation and repairing the defect of the extracted tooth or by a decision made during the surgical procedure and repairing under direct observation.9,11,12,13,14,15,16 None of such reports, however, have considered intentional 180 degree rotation, which is performed to put the healthy side of the tooth in contact with the bone defect and the repaired wall with glass ionomer in contact with the healthy alveolar bone.
In 2001 Sugaya et al. and Kawanami et al. successfully demonstrated the reliability of the intentional replantation of a rotated tooth for the treatment of endo-periodontal lesions in which the defect extended to the apex17,18 They explained that rapid reinsertion achieved inhibition of the formation of the long junctional epithelium and its subsequent periodontal pocket when the tooth is rotated. This tissue exhibited adequate bone healing with recovery of the alveolar bone height due to the absence of bacteria. By doing this rotating replantation, the remaining healthy periodontal ligament (PDL) approximated the alveolus with connective tissue at the site where periodontal breakdown took place. The biological result was that prompt attachment of the tissues occurred, preventing apical migration of the gingival epithelium during the early stage of healing. Another advantage is that the clinician can debride the morbid parts of the root thoroughly by performing extraorally and under direct vision.18
Based on the literature, an intentional replantation with 180 degree horizontal rotation of a tooth with a complete vertical root fracture was performed using resin adhesive to join the fragments.17,18,19 The tooth was asymptomatic after the 18 month follow-up period, and an increase in the alveolar bone density was shown with a decrease in the depth of the periodontal pockets. Kawai et al., on the other hand, reported two cases of vertical fracture in which the fragments were joined together with resin adhesive and subsequently replanted with 180 degree rotation, showing bone regeneration after 3 year follow-up period.20 The success of intentional replantation is mainly based on adequate vascular supply and proper healing of the PDL.21,22,23,24 In 1982, Polson et al. found that the connective tissue reattachment occurred to its initial level after the normal root surface had been transplanted into the reduced periodontium, which indicated that the gingival supracrestal connective tissue had retained certain potential to bond with attached collagen fibers on the root surface.25 They theorized that a linkage between the supracrestal connective tissue fibers and the fibers retained on the root surface had occurred.25
The biological rationale behind the 180 degree rotation we performed is that the repaired PRG was put in direct contact with the healthy bony wall that had not been affected by the periodontal defect, which aided in bone growth at the contact area between the bone defect from the PRG and the unaffected radicular wall. By rotating the tooth, the remnants of the healthy PDL on the root faced the connective tissue in the alveolus at the sites that were initially compromised, which effectively reduced the defective diseased area by half.26,27,28 Based on the literature, we expected expedited reattachment of the tissues during the early stage of the healing process after the replantation.26 Current research supports the principle of placing the healthy root surface in areas that previously had bone destruction and pocketing allows for quick attachment after replantation, thus inhibiting gingival epithelial down growth and pocket formation.18,26,27,28,29
Given the fact that we performed a technique-sensitive new procedure, many precautions to improve the prognosis of the tooth were taken. One such precaution was the staining of the tooth with methylene blue which, theoretically, would enhance the visibility by showing how far the PRG extend into dentin.30 Recent evidence, however, suggests that staining may not necessarily enhance the detection of cracks because the dye cannot flow into craze lines unless there is a break on the surface. Once a crack propagates into a fissure or fracture, these can be stained with dyes.7,31 Another precaution we took was the use of intracanal corticosteroids (Clobetasol MK, Tecnoquímicas, Santiago de Cali, Colombia) to manipulate the inflammatory response after tooth replantation and minimize the risk of ankylosis and internal root resorption.32
Our case is in agreement with previous case reports where rapid insertion is sought by putting the wall of the tooth repaired with glass ionomer in contact with the healthy alveolar bone and by putting the healthy wall of the tooth into contact with the bone defect that caused the formation of the periodontal pocket.17,18,27,28 We confirm that maxillary lateral incisor teeth frequently have unusual morphology of the root canal system. Therefore, clinicians must be aware of the many variations in the root canal morphology of the tooth.7,30 The success of the technique we implemented rests on proper infection elimination, adequate bone formation, disappearance of the underlying pocket, regaining of form and function, and patient's comfort.
Conclusions
In conclusion, this new technique represents a reliable alternative with great utility for the management of PRG, showing satisfactory results in terms of providing adequate physiology, anatomy, and quality of life. However, additional cases are needed to evaluate the long-term benefits of the therapy.
Acknowledgment
The authors would like to thank Dr. Jaime CastroNúñez for the invaluable assistance provided during the preparation of this manuscript. We also offer a special word of gratitude to Mrs. Kathryn Pope and to Dr. David Tripp at Antioch University (Bridge Program) in Los Angeles, CA.
- 1. Ennes JP, Lara VS. Comparative morphological analysis of the root developmental groove with the palatogingival groove. Oral Dis 2004;10:378-382.ArticlePubMed
- 2. Withers JA, Brunsvold MA, Killoy WJ, Rahe AJ. The relationship of palato-gingival grooves to localized periodontal disease. J Periodontol 1981;52:41-44.ArticlePubMed
- 3. Goon WW, Carpenter WM, Brace NM, Ahlfeld RJ. Complex facial radicular groove in a maxillary lateral incisor. J Endod 1991;17:244-248.ArticlePubMed
- 4. Gandhi A, Kathuria A, Gandhi T. Endodontic-periodontal management of two rooted maxillary lateral incisor associated with complex radicular lingual groove by using spiral computed tomography as a diagnostic aid: a case report. Int Endod J 2011;44:574-582.ArticlePubMed
- 5. Everett FG, Kramer GM. The disto-lingual groove in the maxillary lateral incisor; a periodontal hazard. J Periodontol 1972;43:352-361.ArticlePubMed
- 6. Ballal NV, Jothi V, Bhat KS, Bhat KM. Salvaging a tooth with a deep palatogingival groove: an endo-perio treatment-a case report. Int Endod J 2007;40:808-817.ArticlePubMed
- 7. Kogon SL. The prevalence, location and conformation of palato-radicular grooves in maxillary incisors. J Periodontol 1986;57:231-234.ArticlePubMed
- 8. Storrer CM, Sanchez PL, Romito GA, Pustiglioni FE. Morphometric study of length and grooves of maxillary lateral incisor roots. Arch Oral Biol 2006;51:649-654.ArticlePubMed
- 9. Schwartz SA, Koch MA, Deas DE, Powell CA. Combined endodontic-periodontic treatment of a palatal groove: a case report. J Endod 2006;32:573-578.ArticlePubMed
- 10. Hou GL, Tsai CC. Relationship between palato-radicular grooves and localized periodontitis. J Clin Periodontol 1993;20:678-682.ArticlePubMed
- 11. Brunsvold MA. Amalgam restoration of a palatogingival groove. Gen Dent 1985;33:244.PubMed
- 12. Jeng JH, Lu HK, Hou LT. Treatment of an osseous lesion associated with a severe palato-radicular groove: a case report. J Periodontol 1992;63:708-712.ArticlePubMed
- 13. Attam K, Tiwary R, Talwar S, Lamba AK. Palatogingival groove: endodontic-periodontal management-case report. J Endod 2010;36:1717-1720.ArticlePubMed
- 14. Johns DA, Shivashankar VY, Shobha K, Johns M. An innovative approach in the management of palatogingival groove using Biodentine™ and plateletrich fibrin membrane. J Conserv Dent 2014;17:75-79.ArticlePubMedPMC
- 15. Mittal M, Vashisth P, Arora R, Dwivedi S. Combined endodontic therapy and periapical surgery with MTA and bone graft in treating palatogingival groove. BMJ Case Rep 2013;2013:pii: bcr2013009056. doi: 10.1136/bcr-2013-009056.Article
- 16. Al-Hezaimi K, Naghshbandi J, Simon JH, Rotstein I. Successful treatment of a radicular groove by intentional replantation and Emdogain therapy: four years follow-up. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;107:e82-e85.ArticlePubMed
- 17. Sugaya T, Kawanami M, Noguchi H, Kato H, Masaka N. Periodontal healing after bonding treatment of vertical root fracture. Dent Traumatol 2001;17:174-179.ArticlePubMedPDF
- 18. Kawanami M, Sugaya T, Gama H, Tsukuda N, Tanaka S, Kato H. Periodontal healing after replantation of intentionally rotated teeth with healthy and denuded root surfaces. Dent Traumatol 2001;17:127-133.ArticlePubMedPDF
- 19. Kudou Y, Kubota M. Replantation with intentional rotation of a complete vertically fractured root using adhesive resin cement. Dent Traumatol 2003;19:115-117.ArticlePubMedPDF
- 20. Kawai K, Masaka N. Vertical root fracture treated by bonding fragments and rotational replantation. Dent Traumatol 2002;18:42-45.ArticlePubMedPDF
- 21. Loe H, Waerhaug J. Experimental replantation of teeth in dogs and monkeys. Arch Oral Biol 1961;3:176-184.ArticlePubMed
- 22. Fong C, Morris M, Grant T, Berger J. Experimental tooth transplantation in the rhesus monkey. J Dent Res 1967;46:492-496.ArticlePubMedPDF
- 23. Andreasen JO. A time-related study of periodontal healing and root resorption activity after replantation of mature permanent incisors in monkeys. Swed Dent J 1980;4:101-110.PubMed
- 24. Andreasen JO. Periodontal healing after replantation and autotransplantation of incisors in monkeys. Int J Oral Surg 1981;10:54-61.ArticlePubMed
- 25. Polson AM, Caton J. Factors influencing periodontal repair and regeneration. J Periodontol 1982;53:617-625.ArticlePubMed
- 26. Proye MP, Polson AM. Repair in different zones of the periodontium after tooth reimplantation. J Periodontol 1982;53:379-389.ArticlePubMed
- 27. Fariniuk LF, Ferreira EL, Soresini GC, Cavali AE, Baratto Filho F. Intentional replantation with 180 degrees rotation of a crown-root fracture: a case report. Dent Traumatol 2003;19:321-325.ArticlePubMed
- 28. Kim DS, Shin DR, Choi GW, Park SH, Lee JW, Kim SY. Management of complicated crown-root fractures using intentional replantation: two case reports. Dent Traumatol 2013;29:334-337.ArticlePubMed
- 29. Lim JH, Lee JH, Shin SJ. Diagnosis and treatment of teeth with primary endodontic lesions mimicking periodontal disease: three cases with long-term follow ups. Restor Dent Endod 2014;39:56-62.ArticlePubMedPMC
- 30. Lee MH, Ha JH, Jin MU, Kim YK, Kim SK. Endodontic treatment of maxillary lateral incisors with anatomical variations. Restor Dent Endod 2013;38:253-257.ArticlePubMedPMC
- 31. von Arx T, Kunz R, Schneider AC, Bürgin W, Lussi A. Detection of dentinal cracks after root-end resection: an ex vivo study comparing microscopy and endoscopy with scanning electron microscopy. J Endod 2010;36:1563-1568.ArticlePubMed
- 32. Kirakozova A, Teixeira FB, Curran AE, Gu F, Tawil PZ, Trope M. Effect of intracanal corticosteroids on healing of replanted dog teeth after extended dry times. J Endod 2009;35:663-667.ArticlePubMed
REFERENCES
Figure 1
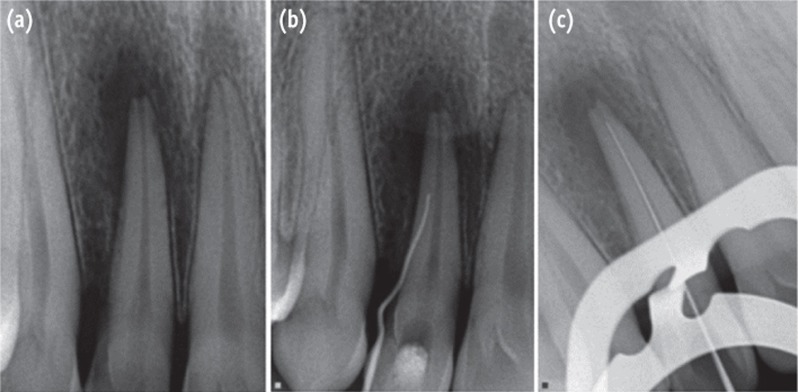
(a) Periapical lesion in the right maxillary lateral incisor; (b) Gutta-percha cone through the gingival sulcus; (c) Periapical radiographic image with initial apical file for determintation of working length.
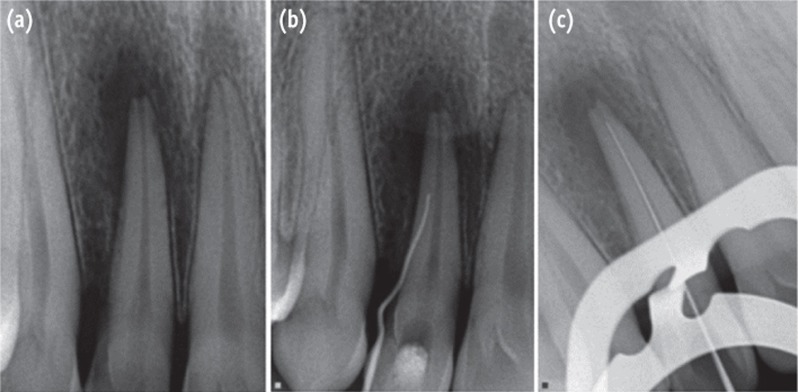
Figure 3
(a) Tooth replantation with 180 degree rotation; (b) Aesthetic restoration of the upper right lateral incisor, after replantation.
Tables & Figures
REFERENCES
Citations
Citations to this article as recorded by 

- Retrospective Analysis of Clinical Characteristics and Therapeutic Effect of Intentional Replantation
Jiani Zhu, Xiangfen Li, Qin Su
Journal of Endodontics.2026;[Epub] CrossRef - A classification of radicular grooves from the perspective of periodontology
Huxiao Li, Zhaowei Tai, Jiachen Dong, Zhongchen Song
BMC Oral Health.2025;[Epub] CrossRef - Diagnostic Approaches of Palatogingival Groove: A Systematic Review
Greta Venskutė
Journal of Dental Health and Oral Research.2024; : 1. CrossRef - Palatogingival Groove: A Plaque Trap Leading to Bone Loss in a Maxillary Lateral Incisor – A Rare Case Report
Gayathri Priyadharshini Elangovan, Indra Kumar Periyasamy, Saravana Kumar R, Gopinath Vivekanandhan
Dental Journal of Indira Gandhi Institute of Medical Sciences.2024; 3: 104. CrossRef - Palatogingival Groove: The Known–unknown Devourer
Sandeep Tandon, Rinku Mathur, Ambika S Rathore, Tripti S Rai, Kanchan Kumari Dhaker, Sumedha Gupta
International Journal of Clinical Pediatric Dentistry.2024; 17(S1): S95. CrossRef - Palatal groove associated with periodontal lesions: a systematic review illustrated by a decisional tree for management
Yvan Gaudex, Vianney Gandillot, Isabelle Fontanille, Philippe Bouchard, Stephane Kerner, Maria Clotilde Carra
BMC Oral Health.2024;[Epub] CrossRef - Prevalence of palatogingival groove affecting maxillary anterior teeth in Saudi subpopulation: A cone-beam computed tomographic study with literature review
Ali Ibrahim Aljuailan, Roqayah Aljuailan, Rahul N. Gaikwad, Shaul Hameed Kolarkodi, Nasser Rufaydan Alamri
The Saudi Dental Journal.2023; 35(8): 1039. CrossRef - Interdisciplinary approach for diagnosis and management of the tooth with type III palatogingival groove
Harakh Chand Baranwal, Jyoti Yadav
Saudi Endodontic Journal.2023; 13(2): 211. CrossRef - Management of Palatogingival Groove in Maxillary Lateral Incisor: A Report of a Rare Case With a Brief Review of Literature
Irfan Ansari, Sanjay Miglani, Vijay Yadav, Shamimul Hasan
Cureus.2023;[Epub] CrossRef - Intentional replantation combined root resection therapy for the treatment of type III radicular groove with two roots: A case report
Dan Tan, Shi-Ting Li, Hao Feng, Zhong-Chao Wang, Cai Wen, Min-Hai Nie
World Journal of Clinical Cases.2022; 10(20): 6991. CrossRef - The incidence of radicular groove on maxillary lateral incisors of Saudi population: CBCT evaluation
Sarah M. Alkahtany, Fatemah Alrwais, Asma Altamimi, Sundus M. Bukhary, Amani Mirdad
BMC Oral Health.2022;[Epub] CrossRef - Retrospective Study of Intentional Replantation for Type IIIb Dens Invaginatus with Periapical Lesions
Na Li, Huihui Xu, Cunhui Kan, Jing Zhang, Song Li
Journal of Endodontics.2022; 48(3): 329. CrossRef - Combined Periodontal and Endodontic Management of Palatal Radicular Groove with Platelet‐Rich Fibrin and Biodentine®
Arjun Hari Rijal, Bhageshwar Dhami, Pratistha Ghimire, Konstantinos Michalakis
Case Reports in Dentistry.2022;[Epub] CrossRef - Intentional Replantation of Single-Rooted and Multi-Rooted Teeth: A Systematic Review
Massimo Pisano, Federica Di Spirito, Stefano Martina, Giuseppe Sangiovanni, Francesco D’Ambrosio, Alfredo Iandolo
Healthcare.2022; 11(1): 11. CrossRef - Management of the palato-radicular groove with a periodontal regenerative procedure and prosthodontic treatment: A case report
Dan-Hua Ling, Wei-Ping Shi, Yan-Hong Wang, Dan-Ping Lai, Yan-Zhen Zhang
World Journal of Clinical Cases.2022; 10(17): 5732. CrossRef - Prevalence and Periodontal Conditions of Developmental Grooves in an Italian School of Dentistry and Dental Hygiene: A Cross-Sectional Study
Giovanna Laura Di Domenico, Simone Fabrizi, Paolo Capparè, Maria Teresa Sberna, Massimo de Sanctis
International Journal of Environmental Research and Public Health.2022; 19(7): 4047. CrossRef - Clinical Observation and Research Progress of Comprehensive Treatment of Palatogingival Groove
华姣 胡
Advances in Clinical Medicine.2021; 11(03): 846. CrossRef - Palato-gingival groove: A silent nidus. Recognition and an innovative management approach: A report of 3 cases
Purushothama Rangaswamy, Sri Harsha Tummala, Samrat R Magarvalli, Sujith Ramachandra, Kavitha Govindappa, Shwetha E
IP Indian Journal of Conservative and Endodontics.2021; 6(2): 114. CrossRef - Periodontal Regenerative Treatment of Intrabony Defects Associated with Palatal Grooves: A Report of Two Cases
Stefano Corbella, Alice Alberti, Beatrice Zotti, Luca Francetti, Jiiang H. Jeng
Case Reports in Dentistry.2019;[Epub] CrossRef - Recognition and management of palatogingival groove for tooth survival: a literature review
Hee-Jin Kim, Yoorina Choi, Mi-Kyung Yu, Kwang-Won Lee, Kyung-San Min
Restorative Dentistry & Endodontics.2017; 42(2): 77. CrossRef - The use of Intentional Replantation to Repair an External Cervical Resorptive Lesion not am Enable to Conventional Surgical Repair
Kreena Pa Tel, Federico Foschi, Ioana Pop, Shanon Patel, Francesco Mannocci
Primary Dental Journal.2016; 5(2): 78. CrossRef - Management of apicomarginal defect in esthetic region associated with a tooth with anomalies
Vinayak Venkoosa Meharwade, Dipali Yogesh Shah, Pradyna Prabhakar Mali, Vidya Vinayak Meharwade
Restorative Dentistry & Endodontics.2015; 40(4): 314. CrossRef
Surgical management with intentional replantation on a tooth with palato-radicular groove
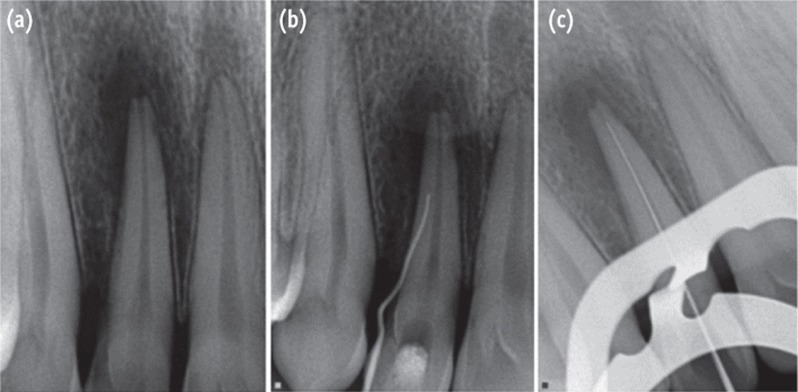
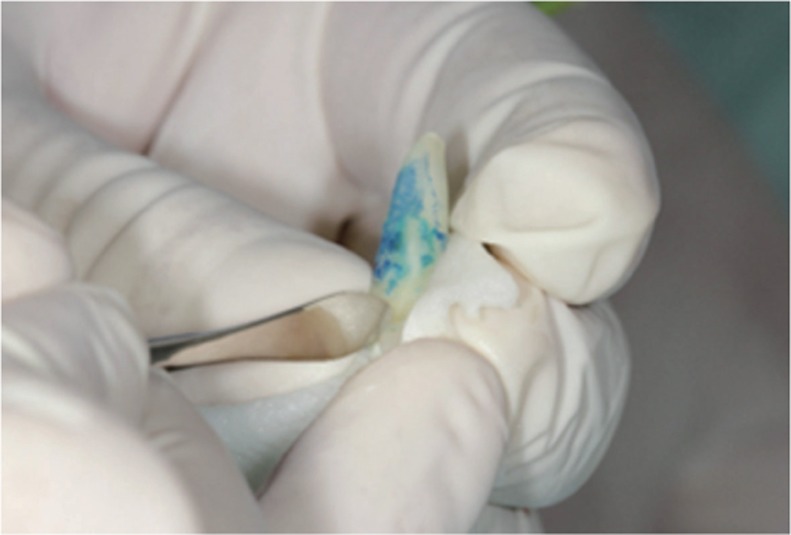
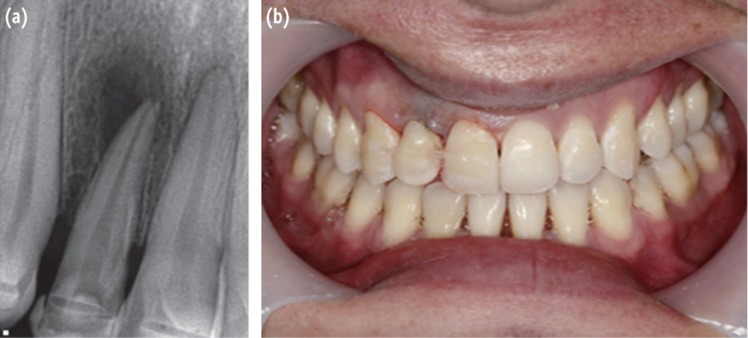
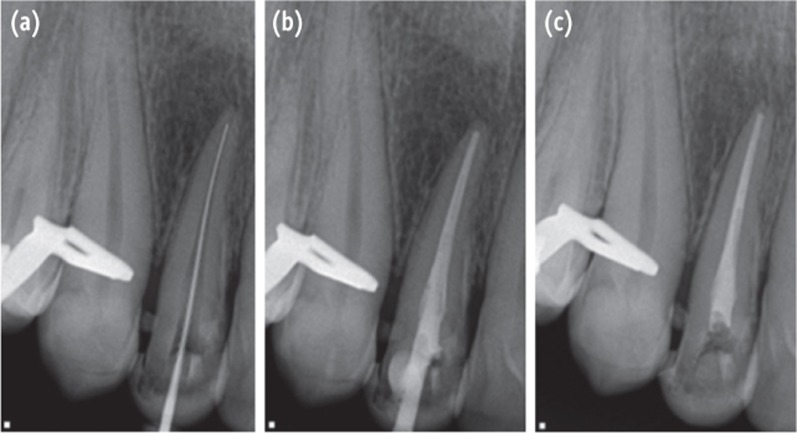
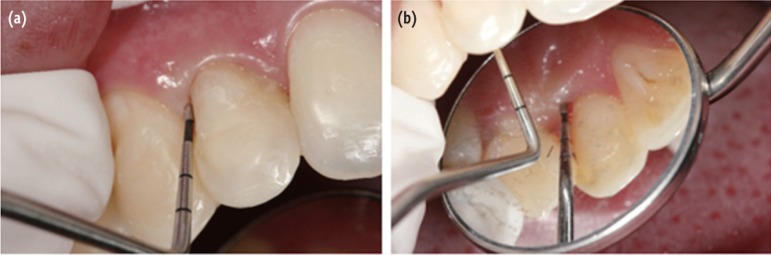
Figure 1 (a) Periapical lesion in the right maxillary lateral incisor; (b) Gutta-percha cone through the gingival sulcus; (c) Periapical radiographic image with initial apical file for determintation of working length.
Figure 2 Extraoral observation of the tooth after methylene blue staining.
Figure 3 (a) Tooth replantation with 180 degree rotation; (b) Aesthetic restoration of the upper right lateral incisor, after replantation.
Figure 4 (a) New length measurement of 22 mm after replantation of the tooth; (b) Final endodontic obturation; (c) Follow-up radiograph one year after the procedure, developing healing process.
Figure 5 (a) and (b) Absence of periodontal pocket and gingival bleeding.
Figure 1
Figure 2
Figure 3
Figure 4
Figure 5
Surgical management with intentional replantation on a tooth with palato-radicular groove

 KACD
KACD
 ePub Link
ePub Link Cite
Cite

