Abstract
-
Objectives
The purpose of present study was to evaluate the internal adaptation of composite restorations using different adhesive systems.
-
Materials and Methods
Typical class I cavities were prepared in 32 human third molars. The teeth were divided into the following four groups: 3-step etch-and-rinse, 2-step etch-and-rinse, 2-step self-etch and 1-step self-etch system were used. After the dentin adhesives were applied, composite resins were filled and light-cured in two layers. Then, silver nitrate solution was infiltrated, and all of the samples were scanned by micro-CT before and after thermo-mechanical load cycling. For each image, the length to which silver nitrate infiltrated, as a percentage of the whole pulpal floor length, was calculated (%SP). To evaluate the internal adaptation using conventional method, the samples were cut into 3 pieces by two sectioning at an interval of 1 mm in the middle of the cavity and they were dyed with Rhodamine-B. The cross sections of the specimens were examined by stereomicroscope. The lengths of the parts where actual leakage was shown were measured and calculated as a percentage of real leakage (%RP). The values for %SP and %RP were compared.
-
Results
After thermo-mechanical loading, all specimens showed significantly increased %SP compared to before thermo-mechanical loading and 1-step self-etch system had the highest %SP (p < 0.05). There was a tendency for %SP and %RP to show similar microleakage percentage depending on its sectioning.
-
Conclusions
After thermo-mechanical load cycling, there were differences in internal adaptation among the groups using different adhesive systems.
-
Keywords: Dentin adhesive; Internal adaptation; Micro-CT; Microleakage
Introduction
While composite resins are aesthetically pleasing, and they adhere to tooth material, the resin polymerization process can cause gaps at tooth-resin interfaces. Microleakage can occur either on the outer surface of the tooth or inside it. Poor internal adaptation can result in hypersensitivity to cold or pain on mastication.
1,
2 For these reasons, several methods have been attempted for evaluating internal adaptation at the interface of the inside of the tooth.
To evaluate the internal adaptation caused by polymer shrinkage, dye and tracer penetration methods have been used.
3 These methods require soaking the specimens in various kinds of solutions, sectioning through the restorations, and assessing the leakage that has been occurred by light microscope. Tracers, such as methylene blue, rhodamine, erythrosine, and silver nitrate, can be used for infiltration. These methods are very simple; however, the specimens must be cut to be examined. Dyed samples can only be examined on the plane through which they were sectioned, and they cannot be evaluated again. The resin-dentin interface can also be examined by SEM after sectioning specimens. However, this method is very technique-sensitive, and it has limitations in quantitative assessment.
4,
5 In addition, it is impossible for traditional methods, which require sectioning and dye infiltration, to compare internal adaptation before and after thermo-mechanical loading. Another method for assessing internal adaptation is to measure the flow of fluid from the pulp to a sealed dentin surface.
6,
7 Microleakage can also be detected by submerging the restored tooth in water and subjecting the tooth to air pressure. If bubbles appear, there could be gaps that have permitted the passage of gas. The specimens can be examined longitudinally because of this method's non-destructive nature. However, a problem is that the nominal values are too low, so the actual leakage path is sometimes unclear.
8 Leakage can occur through the dental substrate itself, which can lead to a false increase of interfacial leakage values.
Micro-CT has recently been introduced to evaluate the internal adaptation of restorations.
9,
10 X-rays from micro-CT pass through the specimen along a single plane for the entire interface. This two-dimensional information can be processed into 3D reconstruction. For the evaluation of internal adaptation in composite resin filling, several studies with micro-CT have been performed.
11-
13 However, dentin adhesives were not applied in these studies, and the cavities were prepared in simple, round shapes, which has little correlation with practical situations. Recently, Kwon and Park proposed a method, in which a silver nitrate solution was penetrated from the pulp space through the dentinal tubules and the amount of silver nitrate penetration in micro-gap areas was assessed by micro-CT, and they reported that it may provide a new measure for evaluating the internal adaptation non-destructively.
14 In addition, specimens could be evaluated repeatedly with micro-CT. They compared Sandwich technique, using resin-modified glass ionomer cement (RMGIC) as a base material, with direct resin filling in the cavity. The infiltrated quantity of silver nitrate on micro-CT imaging was analyzed to evaluate the internal adaptation. Internal adaptation was poorer when the cavity was based with glass ionomer cement, but the change in internal adaptation between before and after mechanical loading was greater when the cavity was restored with composite without an RMGIC base. Silver ions from silver nitrate, which can penetrate the interface between a restoration and the tooth, precipitate as small inclusions, which can be easily detected by the X-rays from micro-CT.
9 Silver nitrate has a low molecular weight, and it has the ability to penetrate into gaps.
10
Today's adhesive techniques usually follow either an 'etch-and-rinse' or a 'self-etch' approach. Etch-and-rinse systems have definite effects on enamel etching, but they have shown technique sensitivity in dentin bonding.
15 Self-etch systems can reduce the excessive etching on dentin, but their etching effect on enamel is insufficient.
16 So-called 1-step self-etch adhesives are composed of intricate mixes of hydrophilic and hydrophobic components. It has been reported that the immediate bond strength of 1-step self-etch adhesives is inferior to that of multi-step adhesives, and any kind of aging process renders their long-term bonding effectiveness ever poorer.
17,
18 In addition, nanoleakage was increased at the interface because of 2-Hydroxyethyl methacrylate (HEMA), which was one of the components. 1-step self-etch adhesives showed greater water sorption from host dentin than 2- or 3-step adhesives.
19
The purpose of present study was to evaluate the internal adaptation of composite restorations that used different adhesive systems. For this purpose, a newly introduced method of analysis was applied, using silver nitrate and micro-CT. Another purpose of this study was to compare the results of micro-CT to those of conventional method that needed sectioning the specimens. Former researches did not use dentin adhesive for resin bonding, however, this study was performed including resin bonding with different kinds of adhesives. This study can be applicable for clinical choice of dentin adhesives.
The null hypotheses were that there would be no difference in internal adaptation among the groups in which different adhesive systems were used and that there would be no difference in internal adaptation between the new non-destructive and conventional evaluation methods.
Materials and Methods
This study was approved by the IRB committee for use of human extracted teeth for analysis of internal adaptation of adhesive restorations using micro-CT (2-2012-0060).
Specimen preparation
Thirty-two intact human molars, extracted within one month, were used. Class I cavities were prepared, with dimensions of 1/2 the length of bucco-lingual (B-L) and 1/2 the length of the mesio-distal (M-D) cuspal distance. The cavity depth was 4 mm. The cavities were prepared with diamond burs and with the help of digital radiography and metal gauge, until the thickness of the remaining dentin was 1 mm at the top of the pulp roof. The pulpal floor base length can be defined as the length from the left vertical wall endpoint to the right vertical wall endpoint.
The 32 specimens were randomly divided into four groups. For each group, different kinds of dentin adhesives were applied as follows:.
1. 3-step etch-and-rinse system group (group 1)
Scotchbond multipurpose system (3M ESPE, St Paul, MN, USA) was used. The enamel and exposed dentin of the cavities were etched with 37% phosphoric acid (3M ESPE, USA) for 15 seconds, washed with water, and air-dried. Scotchbond primer and Scotchbond adhesive were applied according to the manufacturer's recommendations, and then the specimens were light cured for 20 seconds using an LED-type light curing unit (Bluephase, Ivoclar Vivadent, Schaan, Liechtenstein).
2. 2-step etch-and-rinse system group (group 2)
Single Bond 2 system (3M ESPE,USA) was used. The interior parts of the cavities were etched with 37% phosphoric acid (3M ESPE, USA) for 15 seconds. The cavities were washed with water and blot dried. Taking care not to dry the cavity completely, Single Bond 2 adhesive was applied with agitation for 15 seconds and was air-dried, according to the manufacturer's recommendations. Then, light-curing was performed for 20 seconds using the same LED-type light-curing unit with that used in the Group 1.
3. 2-step self-etch system group (group 3)
AdheSE (Ivoclar Vivadent, Liechtenstein) was used for priming and bonding. The interior parts of the cavities were treated, from the enamel to the dentin, with AdheSE primer for 20 seconds. The cavities were dried with strong air blasts. AdheSE bond was applied from the dentin to the enamel, according to the manufacturer's recommendations. After the bonding application, it was dried with weak air. Light-curing was performed for 10 seconds using the same light-curing unit with that used in the Group 1.
4. 1-step self-etch system group (group 4)
Xeno V (Dentsply Caulk, Milford, DE, USA) was used for priming and bonding. The interior parts of the cavities were treated with Xeno V adhesive and were agitated for 20 seconds. The cavities were dried with blown air for more than 5 seconds, until there was no movement of the liquid. Light-curing was performed for 10 seconds using the same light-curing unit with that used in the Group 1.
After light curing of each adhesive, the cavities were incrementally filled with composite resin (Tetric N-Ceram, Ivoclar Vivadent, Liechtenstein), 2 mm at a time. With each increment, the composite was light cured for 20 seconds using the same light-curing unit with that used for the adhesives.
Silver nitrate solution application and micro-CT
Using high-speed diamond burs, the roots were resected at 1 mm below the CEJ. The pulp chambers of the specimens were soaked with 17% ethylenediamine tetraacetic acid (EDTA) for 5 minutes. Then, they were washed with saline. The teeth were immersed in 25% silver nitrate solution and were placed under pressure of 3.75 kPa for 3 days, according to Kwon and Park.
14 High-resolution micro-CT (Model 1076, Skyscan, Aartselaar, Belgium) was used to obtain images under the conditions of 100 kV of acceleration voltage, 100 µA of beam current, a 0.5 mm Al filter, 18 µm of resolution and 360° rotation in 0.5° steps. To see the specimen overall, two-dimensional 550-560 sagittal and coronal images of each specimen were obtained from the mesial to distal surfaces of the tooth. From sagittal images, the image at the center of the resin filling was chosen. Then 50 mesial images from the center at the interval of 40 µm and 50 distal images from the center at the same interval were selected. Coronal images were not used for the evaluation directly. During this procedure, each tooth specimen was mounted in a special template, which had been created only for that specimen. This template minimized the changes in the position of the specimen during repeated processes. The 2D images were analyzed using the CTAn (Skyscan, Belgium) computer program.
A CS-4.8 chewing simulator (SD Mechatronik, Feldkirchen-Westerham, Germany) was used. Under thermodynamic conditions (5 - 55℃), a mechanical load of 5 kgf (49 N) was applied 600,000 times with continuous water flow. The cone-shaped opposing plunger, which was made of nickel chromium, was initially positioned at the center of the restorations. Vertical force, approximately 2 mm above the restoration, and horizontal movement, of roughly 1 mm, were applied laterally. After thermo-mechanical loading, the samples were placed again in the silver nitrate solution, and micro-CT images were obtained using the same methods described above.
Analysis of internal adaptation
The special templates that were used for micro-CT before thermo-mechanical loading were re-used to hold the specimens. These templates minimized changes in the positions of the specimens during repeated processes.
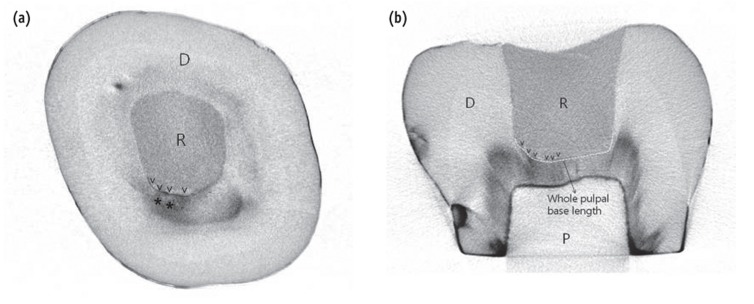
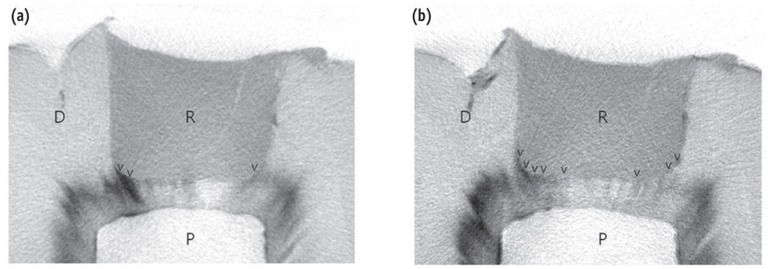
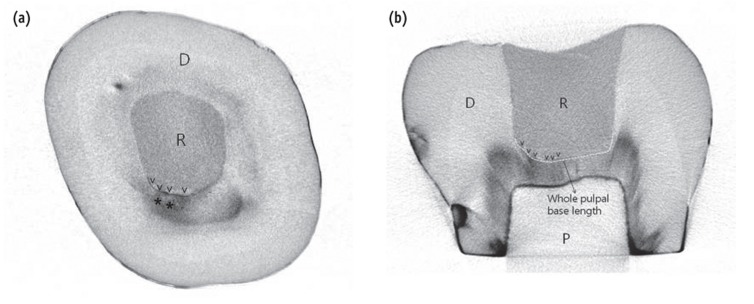
Among the 2D images of each specimen of before thermo-cycling, 100 sagittal images were selected in the center of the cavity at the same interval. For the same specimen, a selection of 2D images after mechanical loading which were corresponding with those berfore thermo-cycling was obtained at equal intervals for each group. Silver nitrate penetration into the microgap between the tooth and restorative materials was considered to be valid when the density was more than 141 indices, which was based on the observation that the areas that were clearly penetrated by the silver nitrate solution had densities > 141 on the index, when the sagittal and coronal images were compared for the same phase (
Figure 1). For each specimen, the width of the margin of the pulpal floor showing a microgap or intact margin was calculated on each image. All of the data were collected and totaled. The silver nitrate penetration into the microgap between the tooth and restoration, as a percentage of the entire length of the pulpal floor, was calculated for each specimen (%SP,
Figure 1b):
%SP (silver nitrate penetration%) = (the length that was penetrated by silver nitrate / the pulpal floor base length) × 100.
In this manner, 100 measurements were collected for each specimen, and the mean %SP values were calculated.
Stereomicroscope examination after tooth sectioning (Conventional method)
To evaluate the internal adaptation using conventional method, the tooth specimens, which had been used for thermo-mechanical loading and micro-CT analysis, were embedded in acrylic clear resin. Using a low-speed diamond disc (500 rpm), two M-D directional sections were obtained at an interval of 1 mm at the center of the cavity. Then, the specimens were infiltrated with 1% rhodamine-B for 24 hours. Next, they were examined with a regular stereomicroscope (Leica S8APO, Leica Microsystems, Wetzlar, Germany) at ×120 magnification to measure the infiltrated length of the rhodamine-B.
3 The sum was then divided by the total length of the cavity base to calculate the percentage, which was called %RP:
%RP (rhodamine-B penetration) = (the length infiltrated by rhodamine-B) / (pulpal floor base length) × 100.
Statistical analysis
One-way ANOVA was used to compare the %SP among the groups before and after loading. A paired t-test was used to compare the %SP before and after thermo-mechanical loading. Duncan's analysis was used for post hoc analysis. All statistical inferences made were within a 95% confidence interval. Values for %RP were compared with one-way ANOVA at the 95% significance level. Duncan's analysis was used for post hoc analysis. Values for %SP and %RP after mechanical loading were compared with a paired t-test.
Results
Silver nitrate infiltration
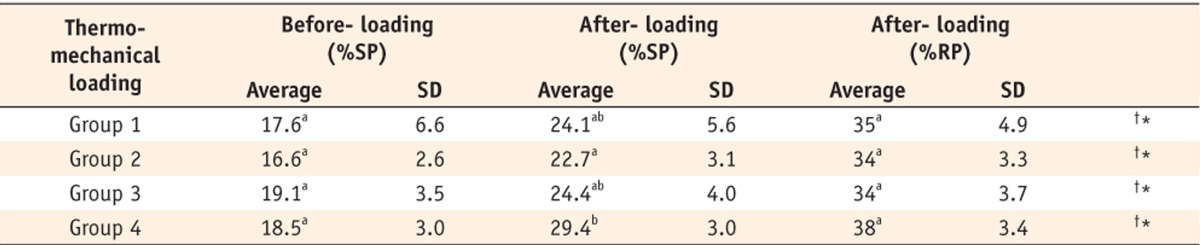
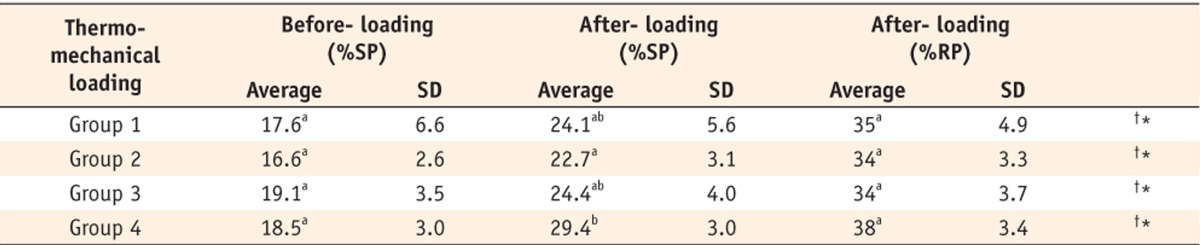
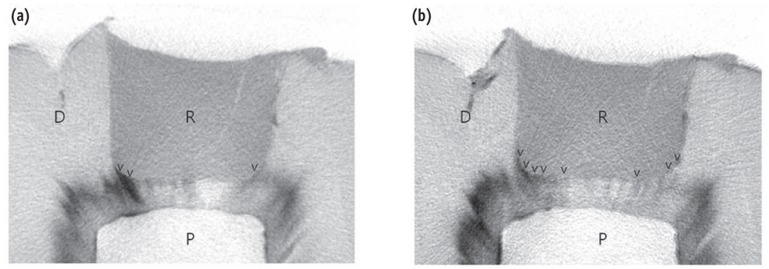
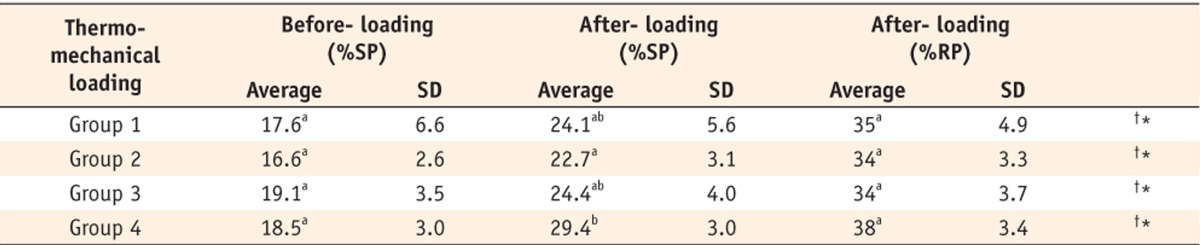
Figures 2a and 2b show the micro CT images of silver nitrate penetration before and after thermo-mechanical loading. Silver nitrate penetrated from the pulp chamber space through the dentinal tubules to the spaces between the composite and the cavity floor. Generally, penetration occurred more frequently in the cavity corners. When %SP values were compared, there were significant differences between before and after loading in all of the groups (
p < 0.05). Before loading, there were no differences in %SP among the groups. After loading, %SP was higher in group 4 than group 2 (
Table 1). On CT images, it was at the axio-pulpal line angles that more discernible infiltration of silver nitrate appeared. Also, thick layers of adhesive were observed along the axio-pulpal line angles (
Figures 2a and 2b).
The results of stereoscopic examination after sectioning and dyeing
The values for %RP were greater than the after-loading %SP values in all of the groups (
p < 0.05). However, there were no significant differences in %RP among the groups (
Table 1).
Discussion
Hydrolysis, thermal changes, and occlusal loading stress can cause the bonding between resin and tooth cavities to deteriorate.
20 To examine the changes at the interface between resins and tooth cavities, three kinds of artificial aging technique can be used; 1) aging by water storage; 2) aging by thermo-cycling; and 3) aging by thermo-mechanical load cycling.
21-
23 Whereas storage in water or thermo-cycling might have little effect on artificial aging, thermo-mechanical load cycling can effectively cause artificial aging.
5,
8,
24,
25 For these reasons, both thermal and mechanical stimulation were applied in the present study.
Internal adaptation can differ depending on the shapes of tooth cavities. C-factors, as well as tooth size and shape, can affect the results of the microleakage. In previous reports, the effects of the polymerization shrinkage were evaluated in standardized cylindrical cavities.
11-
13 In this study, the cavities were prepared just as in clinical situations for composite resin filling. The cavities were typical class I cavities, the dimension of which was 1/2 of the intercuspal distance. They were 3.5 - 4.8 mm in depth, depending on the tooth. In this experiment, the C-factor was about 6.
Before thermo-mechanical loading, no statistical differences were found in %SP among the groups. The null hypothesis was accepted. However, after 600,000 thermo-mechanical loadings, %SP increased significantly in all of the groups. For the results after loading, the null hypothesis was rejected. This result was consistent with those of previous studies.
14,
26,
27 After thermo-mechanical loading, %SP in group 2 was statistically less than that in group 4. In group 2, Single Bond 2 which has ethanol as a solvent is very sensitive to the wetness of the dentin. Despite its technical sensitivity, the etch-and-rinse technique provides stable and promising results, compared with 1-step self-etching system.
8 It has been documented that 1-step self-etch adhesives have several shortcomings, such as increased nanoleakage, limited bond durability, enhanced water sorption, and phase separation.
17,
28,
29 Any kinds of 'aging' result in lowering long-term bonding effectiveness.
30,
31 Other studies have reported increased interfacial nanoleakage.
32,
33 1-step self-etch adhesives that are rich in HEMA show increased water resorption from the dentin;
19 in contrast, self-etch primers without HEMA demonstrate phase separation in their composition.
34 Xeno V is a HEMA-free 1-step self-etch adhesive. The effects of phase separation might have been a reason for the higher %SP in groups using Xeno V than in other groups after thermo-mechanical loading.
In group 1, there was greater diversity in %SP, which resulted in a high standard deviation in the statistical analysis. One of the reasons for this outcome might have been the difference in the effects of etching on dentin. Etching on dentin can leave dissolved calcium phosphate that is not rinsed away. This embedded calcium phosphate is very unstable. Moreover, excessive etching cannot keep hydroxyapatite crystals around the collagen fibrils.
35 Exposed dentinal collagen is very vulnerable to internal hydrolytic degradation.
35 Another possible reason might have been the technical difficulties with proper bonding using etch-and-rinse systems.
35,
36 Differences in wetness on the dentin surface can result in greater deviations in bonding. Because Scotchbond Multipurpose is a water-based dentin primer, water can remain even after drying, which can cause a decrease in its ability to bond to dentin.
37
The value of %SP in group 3 did not show any difference from the values in groups 1, 2, and 4. Self-etch dentin primers can demonstrate weakness in enamel etching.
16 Peripheral enamel seals are important to long-term durability.
38,
39 When mechanical load is applied, the enamel sealing of self-etching systems can be broken easily, and cyclic strains can be applied onto hybrid layers and adhesive layers, which can result in the acceleration of weakening of layers. With AdheSE, the functional monomers of self-etching adhesives, such as phenyl-P and HEMA phosphate, will initially bond to the calcium of in hydroxyapatite, but they can also readily de-bond.
35
With %RP, the actual measurements by stereoscope were obtained by 2 sections from each tooth, and the gap measured for a selective area could not represent the entire sample. Other studies have reported that there were no differences in microleakage among dental adhesives if the specimens were dyed and sectioned.
40 With tooth sectioning, damage to specimens can affect the resin-dentin interface, which might constitute a limitation of traditional destructive techniques. In many cases in which silver nitrate had previously penetrated the gap, it was very difficult to detect the rhodamine penetration because the intense black shade of the silver nitrate could prevent the detection of the red rhodamine shade. To validate the results obtained from the micro-CT (%SP), all specimens were sectioned and evaluated by stereomicroscope (%RP). %RP showed significantly higher microleakage that those of micro-CT (%SP). Though a statistical correlation between %SP and %RP could not be found, there was a tendency for %SP and %RP to show similar microleakage percentage depending on its sectioning.
Conclusions
After thermo-mechanical loading, all of the specimens showed significantly increased %SP compared to before thermo-mechanical loading. After thermo-mechanical loading, the 1-step self-etch system showed a higher %SP than the 2-step etch-and-rinse system. The recently introduced methods for internal adaptation measurement, using micro-CT and silver nitrate adaptation can be used for evaluation of internal adaptation.
Acknowledgement
This study was supported in part by the program of the College of Dentistry of Yonsei University (2011).
-
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1. Bausch JR, de Lange K, Davidson CL, Peters A, de Gee AJ. Clinical significance of polymerization shrinkage of composite resins. J Prosthet Dent 1982;48:59-67.ArticlePubMed
- 2. Eick JD, Welch FH. Polymerization shrinkage of posterior composite resins and its possible influence on postoperative sensitivity. Quintessence Int 1986;17:103-111.PubMed
- 3. Hilton TJ. Can modern restorative procedures and materials reliably seal cavities? In vitro investigations. Part 2. Am J Dent 2002;15:279-289.PubMed
- 4. Alani AH, Toh CG. Detection of microleakage around dental restorations: a review. Oper Dent 1997;22:173-185.PubMed
- 5. Heintze S, Forjanic M, Cavalleri A. Microleakage of Class II restorations with different tracers-comparison with SEM quantitative analysis. J Adhes Dent 2008;10:259-267.PubMed
- 6. Bouillaguet S, Duroux B, Ciucchi B, Sano H. Ability of adhesive systems to seal dentin surfaces: an in vitro study. J Adhes Dent 2000;2:201-208.PubMed
- 7. Del-Nero MO, Escribano N, de la Macorra JC. Analysis of sealing vs tensile bond strength of eight adhesive restorative material systems. J Adhes Dent 2000;2:117-127.PubMed
- 8. De Munck J, Van Landuyt K, Peumans M, Poitevin A, Lambrechts P, Braem M, Van Meerbeek B. A critical review of the durability of adhesion to tooth tissue: methods and results. J Dent Res 2005;84:118-132.ArticlePubMedPDF
- 9. De Santis R, Mollica F, Prisco D, Rengo S, Ambrosio L, Nicolais L. A 3D analysis of mechanically stressed dentin-adhesive-composite interfaces using X-ray micro-CT. Biomaterials 2005;26:257-270.ArticlePubMed
- 10. Eden E, Topaloglu-Ak A, Cuijpers V, Frencken JE. Micro-CT for measuring marginal leakage of Class II resin composite restorations in primary molars prepared in vivo. Am J Dent 2008;21:393-397.PubMed
- 11. Sun J, Eidelman N, Lin-Gibson S. 3D mapping of polymerization shrinkage using X-ray micro-computed tomography to predict microleakage. Dent Mater 2009;25:314-320.ArticlePubMed
- 12. Kakaboura A, Rahiotis C, Watts D, Silikas N, Eliades G. 3D-marginal adaptation versus setting shrinkage in light-cured microhybrid resin composites. Dent Mater 2007;23:272-278.ArticlePubMed
- 13. Zeiger DN, Sun J, Schumacher GE, Lin-Gibson S. Evaluation of dental composite shrinkage and leakage in extracted teeth using X-ray microcomputed tomography. Dent Mater 2009;25:1213-1220.ArticlePubMedPMC
- 14. Kwon OH, Park S. Evaluation of internal adaptation of dental adhesive restorations using Micro-CT. Restor Dent Endod 2012;37:41-49.Article
- 15. De Munck J, Van Meerbeek B, Yoshida Y, Inoue S, Vargas M, Suzuki K, Lambrechts P, Vanherle G. Four-year water degradation of total-etch adhesives bonded to dentin. J Dent Res 2003;82:136-140.ArticlePubMedPDF
- 16. Devarasa GM, Subba Reddy VV, Chaitra NL, Swarna YM. Self-etching adhesive on intact enamel, with and without pre-etching. Microsc Res Tech 2012;75:650-654.ArticlePubMed
- 17. Van Landuyt KL, Mine A, De Munck J, Jaecques S, Peumans M, Lambrechts P, Van Meerbeek B. Are one-step adhesives easier to use and better performing? Multifactorial assessment of contemporary one-step self-etching adhesives. J Adhes Dent 2009;11:175-190.PubMed
- 18. Sadek FT, Goracci C, Cardoso PE, Tay FR, Ferrari M. Microtensile bond strength of current dentin adhesives measured immediately and 24 hours after application. J Adhes Dent 2005;7:297-302.PubMed
- 19. Tay FR, Pashley DH, Suh B, Carvalho R, Miller M. Single-step, self-etch adhesives behave as permeable membranes after polymerization. Part I. Bond strength and morphologic evidence. Am J Dent 2004;17:271-278.PubMed
- 20. Hashimoto M, Ohno H, Kaga M, Endo K, Sano H, Oguchi H. In vivo degradation of resin-dentin bonds in humans over 1 to 3 years. J Dent Res 2000;79:1385-1391.ArticlePubMedPDF
- 21. Shono Y, Terashita M, Shimada J, Kozono Y, Carvalho RM, Russell CM, Pashley DH. Durability of resin-dentin bonds. J Adhes Dent 1999;1:211-218.PubMed
- 22. Leloup G, D'Hoore W, Bouter D, Degrange M, Vreven J. Meta-analytical review of factors involved in dentin adherence. J Dent Res 2001;80:1605-1614.ArticlePubMedPDF
- 23. Nikaido T, Kunzelmann KH, Chen H, Ogata M, Harada N, Yamaguchi S, Cox CF, Hickel R, Tagami J. Evaluation of thermal cycling and mechanical loading on bond strength of a self-etching primer system to dentin. Dent Mater 2002;18:269-275.ArticlePubMed
- 24. Abdalla AI, Davidson CL. Effect of mechanical load cycling on the marginal integrity of adhesive Class I resin composite restorations. J Dent 1996;24:87-90.ArticlePubMed
- 25. Mitsui FH, Bedran-de-Castro AK, Ritter AV, Cardoso PE, Pimenta LA. Influence of load cycling on marginal microleakage with two self-etching and two one-bottle dentin adhesive systems in dentin. J Adhes Dent 2003;5:209-216.PubMed
- 26. Krejci I, Häusler T, Sägesser , Lutz F. New adhesives in Class V restorations under combined load and simulated dentinal fluid. Dent Mater 1994;10:331-335.ArticlePubMed
- 27. Frankenberger R, Strobel WO, Krämer N, Lohbauer U, Winterscheidt J, Winterscheidt B, Petschelt A. Evaluation of the fatigue behavior of the resin-dentin bond with the use of different methods. J Biomed Mater Res B Appl Biomater 2003;67:712-721.ArticlePubMed
- 28. Van Meerbeek B, Van Landuyt K, De Munck J, Hashimoto M, Peumans M, Lambrechts P, Yoshida Y, Inoue S, Suzuki K. Technique-sensitivity of contemporary adhesives. Dent Mater J 2005;24:1-13.ArticlePubMed
- 29. Van Landuyt KL. Optimization of the chemical composition of dental adhesives: towards a simplified and durable, universal enamel/dentin adhesives. KU Leuven; 2008. Thesis dissertation.
- 30. Shirai K, De Munck J, Yoshida Y, Inoue S, Lambrechts P, Suzuki K, Shintani H, Van Meerbeek B. Effect of cavity configuration and aging on the bonding effectiveness of six adhesives to dentin. Dent Mater 2005;21:110-124.ArticlePubMed
- 31. Walter R, Swift EJ Jr, Nagaoka H, Chung Y, Bartholomew W, Braswell KM, Pereira PN. Two-year bond strengths of "all-in-one" adhesives to dentine. J Dent 2012;40:549-555.ArticlePubMed
- 32. Tay FR, King NM, Chan KM, Pashley DH. How can nanoleakage occur in self-etching adhesive systems that demineralize and infiltrate simultaneously? J Adhes Dent 2002;4:255-269.PubMed
- 33. Tay FR, Pashley DH, Yoshiyama M. Two modes of nanoleakage expression in single-step adhesives. J Dent Res 2002;81:472-476.ArticlePubMedPDF
- 34. Van Landuyt KL, De Munck J, Snauwaert J, Coutinho E, Poitevin A, Yoshida Y, Inoue S, Peumans M, Suzuki K, Lambrechts P, Van Meerbeek B. Monomer-solvent phase separation in one-step self-etch adhesives. J Dent Res 2005;84:183-188.ArticlePubMedPDF
- 35. Van Meerbeek B, Yoshihara K, Yoshida Y, Mine A, De Munck J, Van Landuyt KL. State of the art of self-etch adhesives. Dent Mater 2011;27:17-28.ArticlePubMed
- 36. Pashley DH, Tay FR, Breschi L, Tjäderhane L, Carvalho RM, Carrilho M, Tezvergil-Mutluay A. State of the art etch-and-rinse adhesives. Dent Mater 2011;27:1-16.ArticlePubMed
- 37. Zheng L, Pereira PN, Nakajima M, Sano H, Tagami J. Relationship between adhesive thickness and microtensile bond strength. Oper Dent 2001;26:97-104.PubMed
- 38. Loguercio AD, Moura SK, Pellizzaro A, Dal-Bianco K, Patzlaff RT, Grande RH, Reis A. Durability of enamel bonding using two-step self-etch systems on ground and unground enamel. Oper Dent 2008;33:79-88.ArticlePubMedPDF
- 39. Gamborgi GP, Loguercio AD, Reis A. Influence of enamel border and regional variability on durability of resin-dentin bonds. J Dent 2007;35:371-376.ArticlePubMed
- 40. Banomyong D, Palamara JE, Messer HH, Burrow MF. Sealing ability of occlusal resin composite restoration using four restorative procedures. Eur J Oral Sci 2008;116:571-578.PubMed
Figure 1Coronal (a) and sagittal (b) sections of micro-CT image. (a) In coronal section, 'v' marks indicate silver nitrate penetrated into microgap between tooth and restoration. '*' mark indicates silver nitrate which infiltrated into dentinal tubules; (b) The percentage of the silver nitrate penetration length into the microgap between the tooth and restoration with regard to the entire length of the pulpal floor (white dotted line) was calculated for each micro CT image (% SP). R, Resin; D, Dentin; P, Pulp.
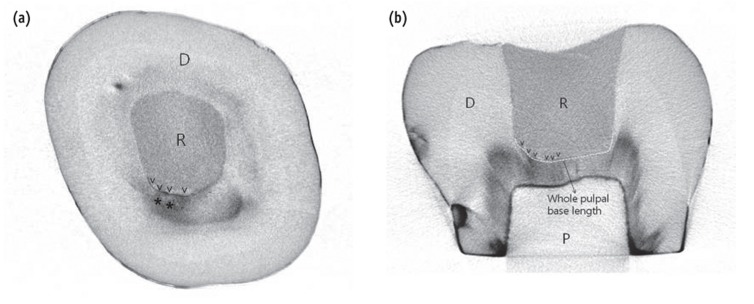
Figure 2Sagittal section of micro-CT image. (a) before thermo-mechanical loading; (b) after thermo-mechanical loading. 'v' marks indicate that silver nitrate penetrated into microgap between tooth and restoration. R, Resin; D, Dentin; P, Pulp.
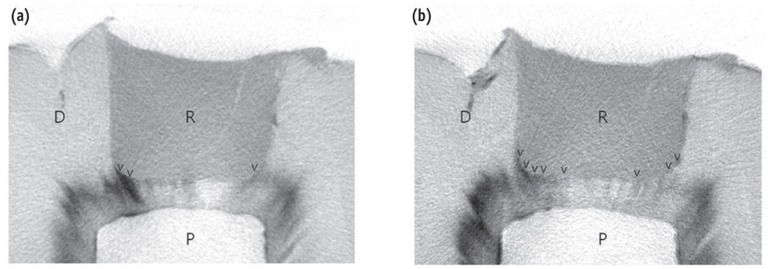
Table 1Mean percentage of silver nitrate penetration length to the whole pulpal floor (%SP)


 KACD
KACD
 ePub Link
ePub Link Cite
Cite

