Articles
- Page Path
- HOME > Restor Dent Endod > Volume 39(2); 2014 > Article
- Case Report Healing after horizontal root fractures: 3 cases with 2-year follow-up
- Yoorina Choi1, Sung-Ok Hong1, Seok-Ryun Lee1, Kyung-San Min2, Su-Jung Park1
-
2014;39(2):-131.
DOI: https://doi.org/10.5395/rde.2014.39.2.126
Published online: March 21, 2014
1Department of Conservative Dentistry, Wonkwang University School of Dentistry, Iksan, Korea.
2Department of Conservative Dentistry, Chonbuk National University School of Dentistry, Jeonju, Korea.
- Correspondence to Su-Jung Park, DDS, PhD. Assistant Professor, Department of Conservative Dentistry, Wonkwang University School of Dentistry, 895, Moowang-ro, Iksan, Korea 570-749. TEL, +82-63-850-6930; FAX, +82-63-859-2932; conspsj@wonkwang.ac.kr
• Received: October 24, 2013 • Accepted: January 9, 2014
©Copyights 2014. The Korean Academy of Conservative Dentistry.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 2,127 Views
- 18 Download
- 4 Crossref
Abstract
- Among dental traumas, horizontal root fractures are relatively uncommon injuries. Proper initial management and periodical evaluation is essential for the successful treatment of a root-fractured tooth. If pulpal necrosis develops, endodontic treatment is indicated, exclusively for the coronal fragment. Fragment diastases exert a great influence on healing at the fracture line and on pulpal necrosis. An adequately treated root-fractured tooth has a good prognosis. This case report describes the treatment and 2-yr follow up of 3 maxillary central incisors, first with horizontal root fracture, second with horizontal root fracture and avulsion, and third with horizontal root fracture and lateral luxation. All three cases were treated with mineral trioxide aggregate (ProRoot, Dentsply). During 2 yr of follow-up evaluation, the root-fractured teeth of the present patients were well retained in the arch, showing periodontal healing, even after endodontic treatment.
Introduction
Among dental traumas, horizontal root fractures are relatively uncommon injuries as they comprise only 0.5 - 7.0% of injured permanent teeth. These injuries involve various dental tissues such as the dental pulp, dentin, cementum, and supportive tissues (e.g., the periodontal ligament and alveolar bone).1,2
After adequate clinical management with repositioning and splinting, patient should be followed up periodically. In approximately 25% of patients, permanent pulpal necrosis occurs in the coronal fragment and requires endodontic treatment.2,3 Endodontic treatment is usually indicated, exclusively for the coronal fragment.3
The survival rate of a horizontally root-fractured tooth is reportedly to be relatively high (83%) for up to 10 years of observation.4 This case report illustrates 3 cases of healing and survival of root-fractured teeth.
Case reports
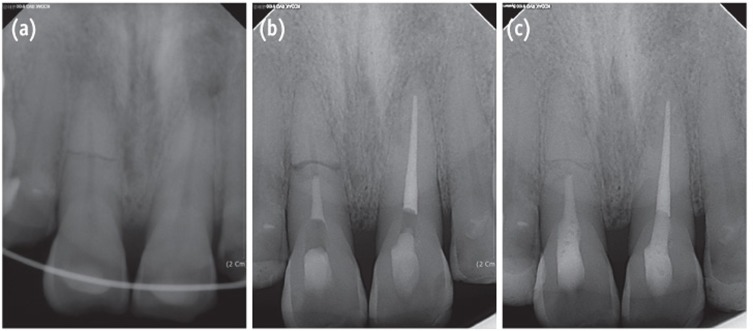
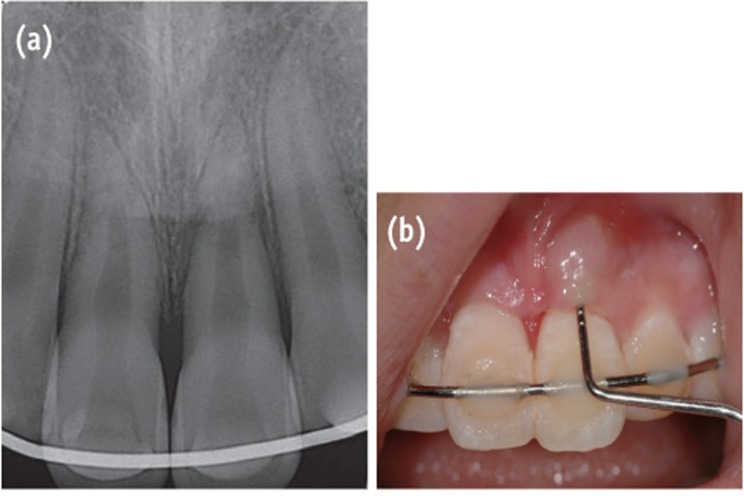
A 33-year-old man presented to the Department of Conservative Dentistry at the Wonkwang University Dental Hospital (Iksan, Korea) with a complaint of discomfort of the maxillary right central incisor during mastication. Two days before, the tooth had impacted against a rigid object. The patient's medical history was noncontributory. Radiographic examination showed a horizontal fracture in the middle third of the root of the tooth and a slight displacement of the apex (Figure 1a). Intraoral examination revealed that all maxillary teeth had normal responses to pulp vitality tests, no mobility, and no discolored crown. Since the maxillary central incisor showed no signs of mobility or pathology, the patient was followed up without any splint appliances. His occlusion was checked and adjusted to eliminate loading on the traumatized tooth during function.
Four weeks after the trauma, a radiolucent area appeared intra-canally on the apical portion of the coronal fragment and it continued to progress until 6 weeks of observation (Figures 1b and 1c). Root canal treatment was initiated on the coronal fragment with K-file and irrigated with 5% sodium hypochlorite. Working length was established with an apex locator (DentaPort ZX, Morita, Kyoto, Japan). Special care was taken to instrument within the coronal fragment. After 2 months of intracanal calcium hydroxide dressing, the canal was obturated with mineral trioxide aggregate (MTA, ProRoot, Dentsply, Tulsa, OK, USA) (Figure 2a).
At the 2-year follow-up evaluation, the patient did not report any clinical symptoms. Complete healing of the root fracture with the interposition of hard tissue between the fragments was observed on the periapical radiographs (Figure 2c).
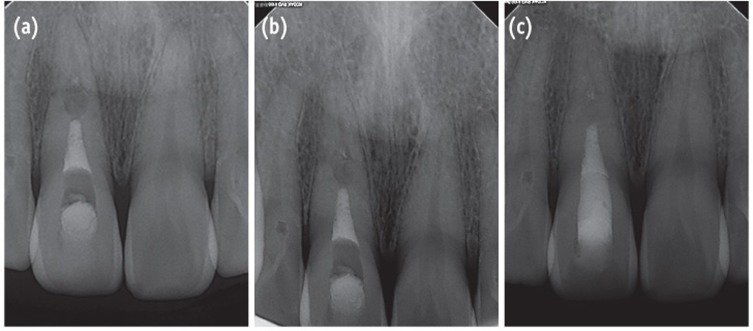
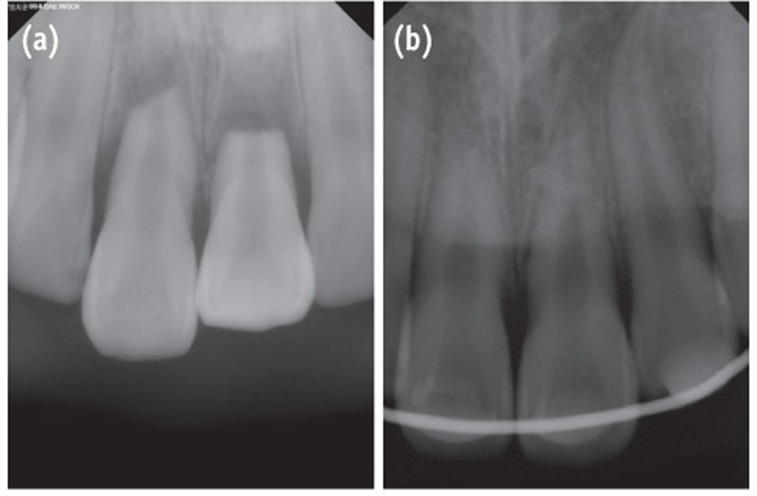
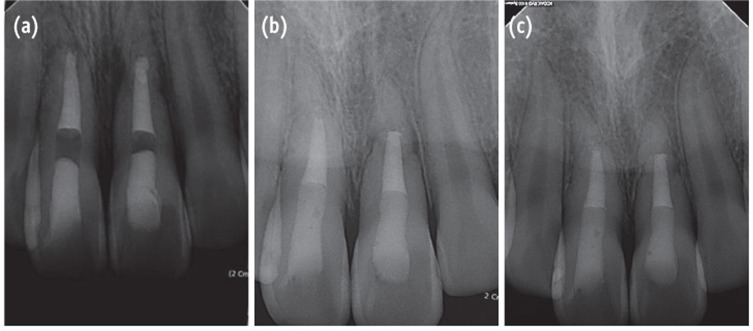
A 60-year-old male patient was referred to the Department of Conservative Dentistry at the Wonkwang University Dental Hospital (Iksan, Korea) for the evaluation of the maxillary anterior teeth. He had a history of trauma that had occurred 7 days previously. The patient's medical history was noncontributory. The initial diagnosis by the emergency dentist was horizontal root fracture on the maxillary right central incisor and avulsion on the maxillary left central incisor. According to the emergency note, a crown fragment of tooth #11 had been extruded with a large amount of diastases. The emergency dentist performed pulp extirpation on the crown fragment and the teeth were repositioned and splinted with a semi-rigid splint (Figure 3a). Root canal treatment was performed on coronal fragment of tooth #11 with K-file and irrigated with 5% sodium hypochlorite. Working length was established with an apex locator (DentaPort ZX). After 6 weeks of intracanal calcium hydroxide dressing, the canal was obturated with MTA (ProRoot) (Figure 3b).
At the 2-year follow-up evaluation, the patient had no complaints of pain or discomfort. Radiographic examination showed the root-fractured tooth was completely healed with hard and soft tissue between the fragments (Figure 3c).
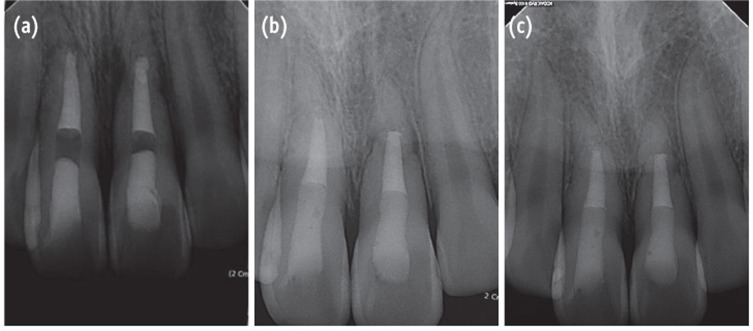
A 13-year-old female patient was referred to the Department of Conservative Dentistry at the Wonkwang University Dental Hospital (Iksan, Korea) for the evaluation of her maxillary anterior teeth. Seven days previously, the maxillary central incisors were traumatized when she slipped on the stairs and fell down. The coronal fragments of the incisors were luxated laterally, thereby showing the exposed labial surface of the root. The patient's medical history was noncontributory. The emergency dentist diagnosed the teeth as having horizontal root fractures with alveolar bone fractures. The teeth were repositioned with a rigid splint (Figure 4).
One week after the trauma, both teeth had a normal response to pulp vitality tests. Three weeks later, localized swelling was observed on the labial gingiva of the maxillary left central incisor, and a radiolucent lesion was present near the fracture line. Both teeth had no responses to the thermal and electronic pulp tests. The narrow and deep pocket (approximately 8 mm) were explored by a dental probe through the gingival sulcus to the swollen portion (Figure 5). Root canal treatment was initiated on both coronal fragments of the teeth with K-file and irrigated with 5% sodium hypochlorite. Working length was established with an apex locator (DentaPort ZX). Calcium hydroxide was applied into the canals between appointments. The deep pocket was debrided because of the possibility of the insertion of a foreign body at the time of the accident. At the 2-month follow-up evaluation, the swelling had disappeared and pocket depth was reduced to 3 mm. The canals were obturated with MTA (ProRoot) confined to the coronal fragment (Figure 6a).
At the 6-month and 1-year follow-up evaluation, she did not complain of any pain. However, she reported occasional swelling of the gingiva of the maxillary left central incisor. Clinically normal probing depth and normal response to percussion were observed on the teeth. Radiographic examination showed that the radiolucent area near the fracture line of the maxillary left central incisor had decreased, but the lesion remained (Figure 6b). At the 1½-year evaluation, a fragment of tooth-like material was observed in the gingival swelling area and the fragment was removed. At the 2-year follow-up evaluation, she reported no recurrence of gingival swelling since her last visit to the dental hospital. Slight mobility remained, but both teeth were retained well in the maxillary arch without any discomfort. Radiographic examination showed the teeth were healed with soft tissue between the fragments (Figure 6c).
Discussion
Horizontal root fractures, which frequently affect the upper incisors, usually result from a frontal impact. As a result, combined injuries occur in dental tissues such as the pulp, dentin, cementum, periodontal ligament, and alveolar bone.1,4,5,6 The coronal fragment of a root-fractured tooth frequently shows extrusion and displacement to the lingual region.1,6 Concussion, subluxation, extrusion, and lateral luxation with or without an alveolar bone fracture can occur on the coronal fragment, based on the severity of the trauma.7 In Case 1, there was no extrusion of the coronal fragment, which simulated a concussion injury. In Case 2, the coronal fragment was totally extruded, which simulated extrusive luxation. In Case 3, the fragment showed extrusion and severe displacement to the lingual region, and simulated lateral luxation and an alveolar bone fracture.
In an emergency visit for a horizontal root fracture, treatment involves repositioning the fragments as closely as possible.1,6 Applying a semi-rigid splint to the adjacent teeth for 3 - 4 weeks is recommended.1,8 A splint is not essential in cases of slight injury that simulate a concussion. However, a longer splinting time is often recommended in cases of coronal root fracture.5,8 Therefore, clinical and radiographic evaluation should be performed during periodic follow-up examinations.2,6,7 In the first month, the patients should be observed weekly. After the splinting period, the patients should be observed at 3 months, 6 months, and 12 months. Thereafter, they should be observed yearly for 5 - 10 years.6,9
Permanent pulpal necrosis of the coronal fragment occurs in approximately 25% of adult patients with a horizontal root fracture.7,10 The apical pulpal circulation is generally not disrupted because the apical fragment is not displaced.2 Root canal treatment should be confined to the coronal fragment because pulp necrosis in the apical fragment is extremely rare.9,11
In Case 1, internal resorption around the coronal fracture line was observed at approximately 4 weeks after the trauma. Andreasen et al. reported 3 types of resorption in patients with root fractures, (1) external surface resorption (ESR), (2) internal surface resorption (ISR), and (3) internal tunneling resorption (ITR).1 Andreasen stated that these root resorption processes are usually correlated with healing processes and therefore require no interceptive treatment. The pathogenesis of internal root resorption and subsequent healing following root fracture result from an interplay between the exposed dentin, a damaged but uninfected pulp, and the in-growth of vital tissue.1,7 In Case 1, the ISR type of root resorption was apparent on radiographic examination at approximately 4 weeks, and therefore a process of healing was expected. Root canal treatment was unfortunately initiated without a full knowledge of the healing process of root fractures. At the 2-year follow-up examination, the tooth showed complete healing on the radiograph. However, the tooth supposedly could have healed spontaneously, even without root canal treatment. For the successful management of root fractures, it is important to understand the healing patterns thoroughly.
In Case 3, a fragment of tooth-like material was observed on the gingival swelling area at 18 months after the trauma. After removing the fragment, gingival swelling disappeared and radiolucency around the fracture line was decreased, which indicated periodontal healing. Residual infected material can cause a persistent or new radiolucency, thereby interfering with the healing of periodontal tissue.1,3 A foreign body may act as an inflammatory source in the space between fragments.
Andreasen and Hjorting-Hansen classified the healing of root-fractured teeth into four groups, (1) healing with hard tissue, (2) healing with the interposition of hard and soft tissue, (3) healing with interposition of soft tissue, and (4) no healing.12 The factors influencing the healing of a root-fractured tooth include the patient's age, stage of root growth, mobility of the coronal fragment, and diastasis of the fragments.1 In the present patients, injury factors (e.g., fragment diastasis and mobility of the coronal fragment) exerted a strong influence on healing at the fracture line and on pulpal necrosis. Case 1 had small diastasis of less than 0.5 mm and no mobility, and the tooth healed with hard tissue and with the evidence of a spontaneous healing process such as ISR. Case 2 showed extrusive luxation of the crown fragment with a large amount of diastases. It was impossible to determine whether the pulp was vital because root canal treatment had been already initiated by the emergency dentist. The follow-up radiographs showed healing with hard and soft tissue. Case 3 showed lateral luxation of the crown fragment with a large amount of diastases. Interposition of soft tissue with pulp necrosis of coronal fragment was also observed. Increasing diastases between fragments reportedly increases the risk of pulp necrosis, and decreases the likelihood of hard tissue healing.13 According to a report, the frequency of pulp necrosis is stable with diastasis of up to 1 mm, whereas hard tissue healing shows stable values up to 0.5 mm.13
The patient in Case 2 had the unfavorable factors of age and a large amount of diastases, but showed a notably favorable treatment outcome with proper initial management and root canal treatment. Cvek et al. reported a high survival rate of root-fractured teeth for up to 10 years of observation, a high frequency of healing after endodontic treatment (79% of 95 treated teeth), and a healing frequency that was comparable to that of patients reported in previous endodontic studies.4 In the present report, the root-fractured teeth of the patients were retained well in permanent dentition during the 2-year follow-up evaluation. We propose that continuous follow-up evaluations should be performed on patients.
A root-fractured tooth requires proper initial management and periodic evaluation.1 Understanding the healing patterns of root fracture is essential for successful treatment.7 Diastasis between fragments exerts a great influence on healing at the fracture line and on pulpal necrosis.9 Adequately treated teeth with horizontal root fractures have a good prognosis.12
Conclusions
This case report highlights the good healing of various type of root fracture. Two years after the trauma, the root-fractured teeth in the present patients had a good prognosis with periodontal healing.
Acknowledgement
This paper was supported by Wonkwang University in 2012.
- 1. Andreasen FM, Andreasen JO. Root fractures. In: Andreasen JO, Andreasen FM, editors. Textbook and color atlas of traumatic injuries to the teeth. 3rd ed. Copenhagen: Munksgaard; 1994. p. 279-314.
- 2. Clark SJ, Eleazer P. Management of a horizontal root fracture after previous root canal therapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000;89:220-223.ArticlePubMed
- 3. Cvek M, Mejàre I, Andreasen JO. Conservative endodontic treatment of teeth fractured in the middle or apical part of the root. Dent Traumatol 2004;20:261-269.ArticlePubMed
- 4. Cvek M, Tsilingaridis G, Andreasen JO. Survival of 534 incisors after intra-alveolar root fracture in patients aged 7-17 years. Dent Traumatol 2008;24:379-387.ArticlePubMed
- 5. Andrade ES, de Campos Sobrinho AL, Andrade MG, Matos JL. Root healing after horizontal fracture: a case report with a 13-year follow up. Dent Traumatol 2008;24:e1-e3.ArticlePubMed
- 6. Versiani MA, de Sousa CJ, Cruz-Filho AM, Perez DE, Sousa-Neto MD. Clinical management and subsequent healing of teeth with horizontal root fractures. Dent Traumatol 2008;24:136-139.ArticlePubMed
- 7. Andreasen FM, Andreasen JO. Resorption and mineralization processes following root fracture of permanent incisors. Endod Dent Traumatol 1988;4:202-214.ArticlePubMed
- 8. Andreasen JO, Andreasen FM, Mejàre I, Cvek M. Healing of 400 intra-alveolar root fractures. 2. Effect of treatment factors such as treatment delay, repositioning, splinting type and period and antibiotics. Dent Traumatol 2004;20:203-211.ArticlePubMed
- 9. Hargreaves KM, Cohen S. Cohen's pathways of the pulp. 10th ed. St. Louis: Mosby Elsevier; 2010. p. 635-637.
- 10. Shin JH, Kim RJ. Management of horizontal root fractures by fabrication of canine protected occlusion using composite resin. Restor Dent Endod 2012;37:180-184.ArticlePubMedPMC
- 11. Wölner-Hanssen AB, von Arx T. Permanent teeth with horizontal root fractures after dental trauma. A retrospective study. Schweiz Monatsschr Zahnmed 2010;120:200-212.PubMed
- 12. Andreasen JO, Hjorting-Hansen E. Intra-alveolar root fractures: radiographic and histologic study of 50 cases. J Oral Surg 1967;25:414-426.PubMed
- 13. Andreasen JO, Andreasen FM, Mejàre I, Cvek M. Healing of 400 intra-alveolar root fractures. 1. Effect of preinjury and injury factors such as sex, age, stage of root development, fracture type, location of fracture and severity of dislocation. Dent Traumatol 2004;20:192-202.PubMed
REFERENCES
Figure 1
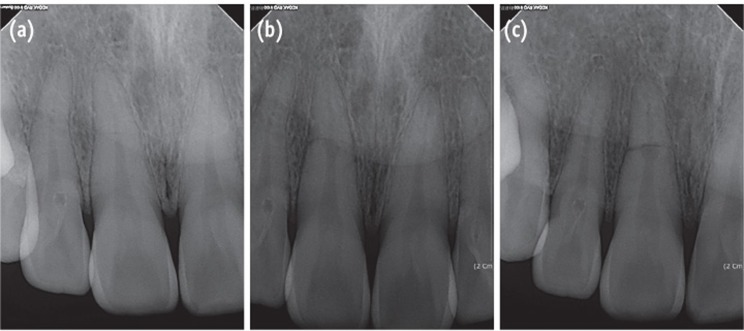
(a) The radiograph of the initial visit shows a horizontal root fracture line on the maxillary right central incisor; (b) The 4-week follow-up radiograph shows internal resorption around the fracture line; (c) The 6-week follow-up radiograph shows that the internal resorption site is larger and more distinct.
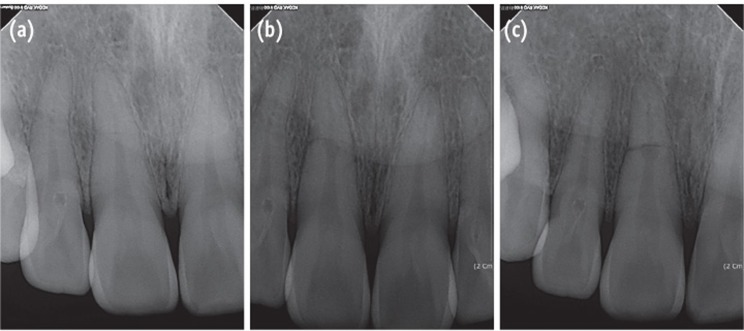
Figure 2
Radiograph of the tooth. (a) After root canal treatment; (b) At the 1-year follow-up evaluation; (c) At the 2-year follow-up evaluation. 2-year follow-up radiograph reveals healing with the interposition of hard tissue between the fragments.
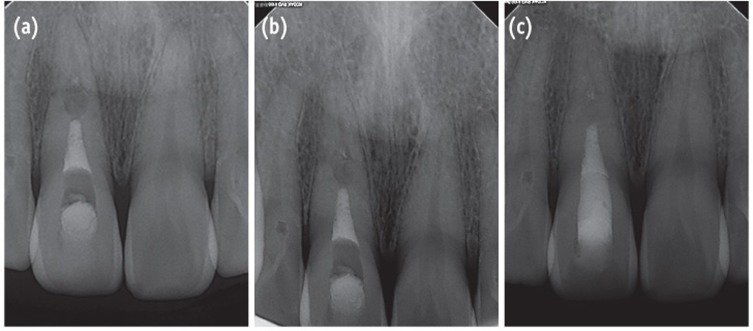
Figure 3
Radiograph of the right maxillary central incisor with horizontal root fracture. (a) After repositioning and applying a resin-wire splint; (b) After root canal treatment; (c) At the 2-year follow-up evaluation. 2-year follow-up radiograph reveals healing with the interposition of hard and soft tissue between the fragments.
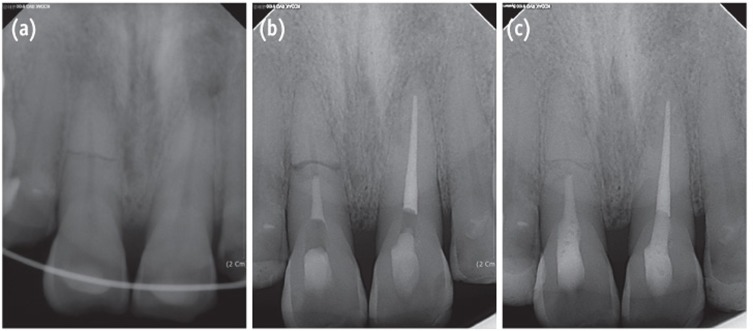
Figure 4
Radiographs of the emergency visit shows the teeth. (a) Before the application of the resin-wire splint; (b) After repositioning and the application of the resin-wire splint.
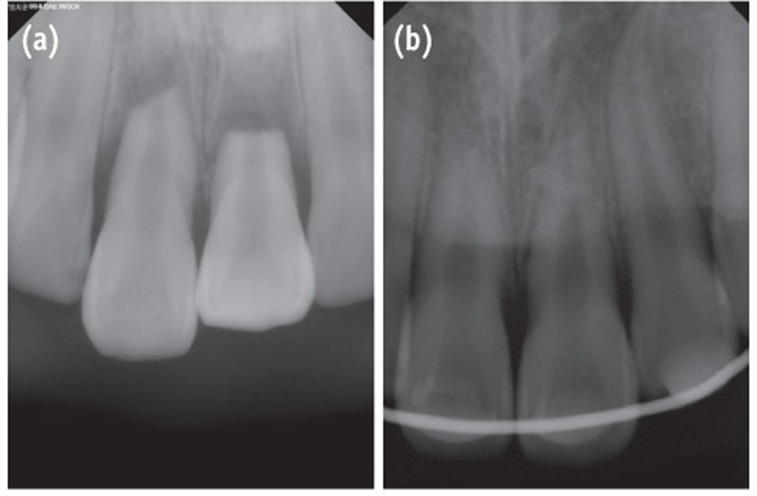
Figure 5
Images were obtained 3 weeks after the trauma. (a) The periapical radiograph shows a radiolucent lesion around the fracture line on tooth #21; (b) The clinical photograph shows narrow and deep pocket depth and gingival swelling on tooth #21.
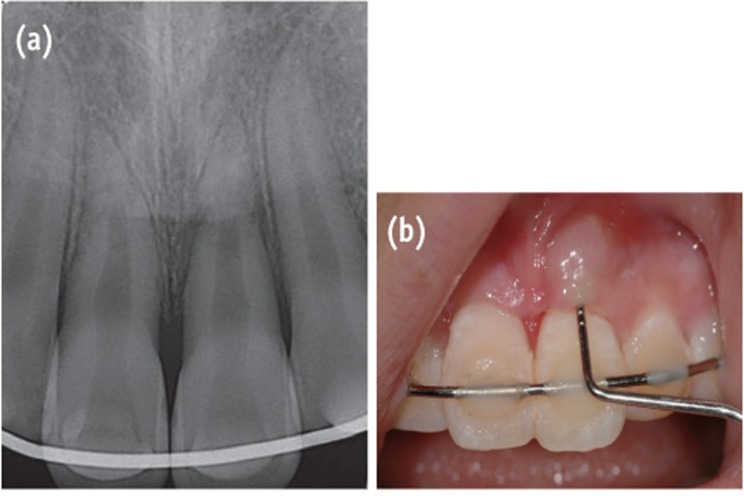
Figure 6
Radiograph of the teeth. (a) After the root canal treatment; (b) At the 1-year follow-up evaluation; (c) at the 2-year follow-up evaluation. The radiolucent lesion has disappeared on tooth #21. 2-year follow-up radiograph reveals healing with interposition of soft tissue between the fragments.
Tables & Figures
REFERENCES
Citations
Citations to this article as recorded by 

- Clinical applications of calcium silicate‐based materials: a narrative review
S Küçükkaya Eren
Australian Dental Journal.2023;[Epub] CrossRef - A three-dimensional finite element analysis of stress distribution in maxillary central incisor with a horizontal mid root fracture after various management protocols
Kavitha Anantula, Bhavana Vankayala, SarjeevSingh Yadav
Journal of Conservative Dentistry.2021; 24(5): 470. CrossRef - : The Use of Mineral Trioxide Aggregate in The Treatment of Horizontal Root Fractures: A Case Presentation and Literature Update
Elif BALLIKAYA, Hamdi GÜNGÖR
Selcuk Dental Journal.2021; 8(3): 850. CrossRef - Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview – part II: other clinical applications and complications
M. Torabinejad, M. Parirokh, P. M. H. Dummer
International Endodontic Journal.2018; 51(3): 284. CrossRef
Healing after horizontal root fractures: 3 cases with 2-year follow-up
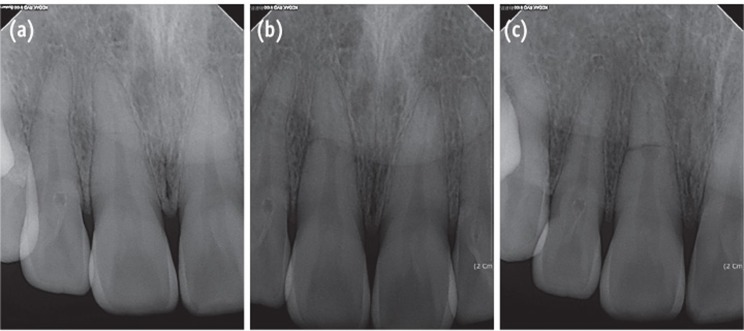
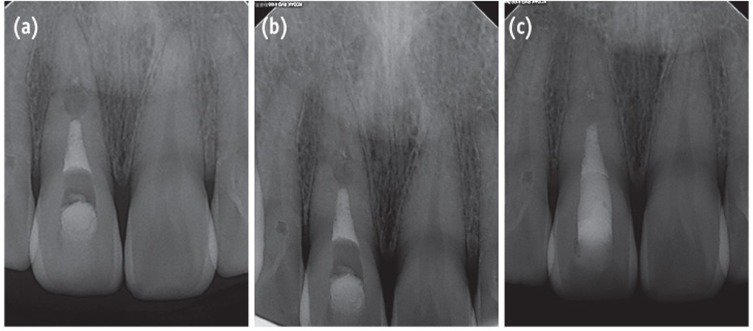
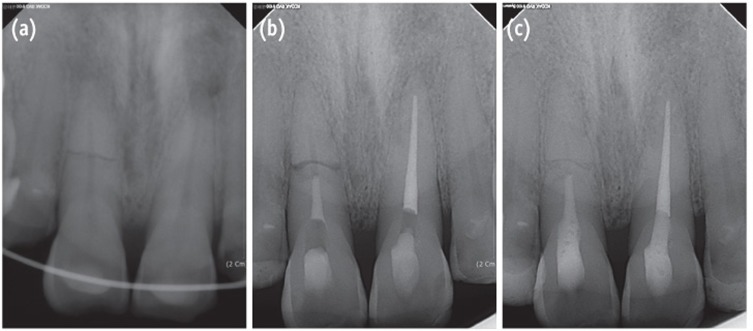
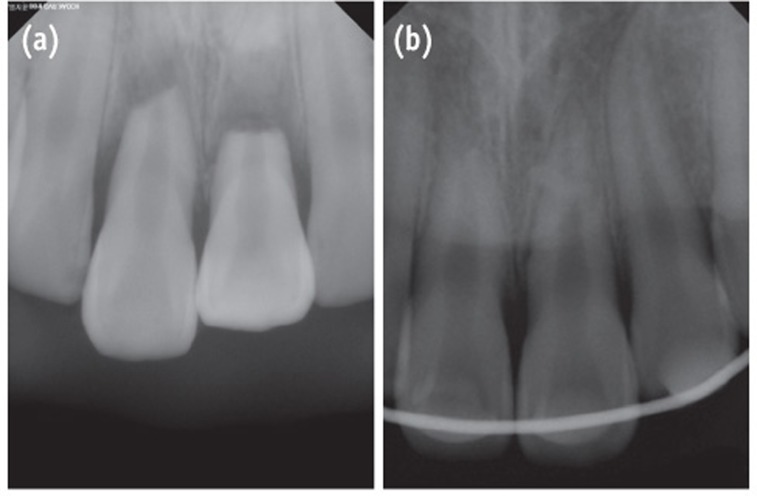
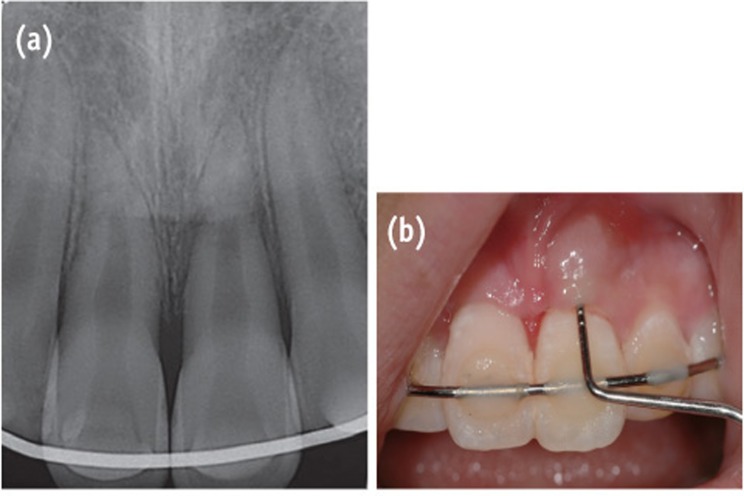
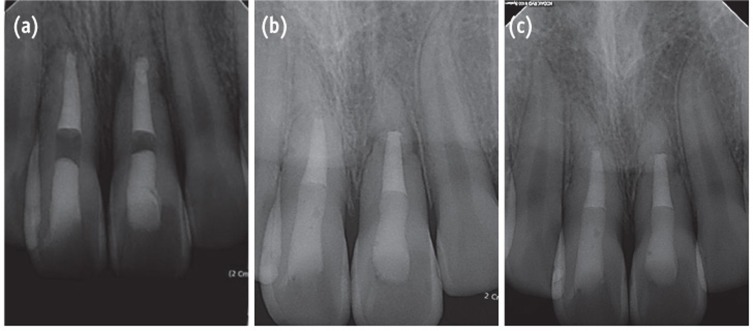
Figure 1 (a) The radiograph of the initial visit shows a horizontal root fracture line on the maxillary right central incisor; (b) The 4-week follow-up radiograph shows internal resorption around the fracture line; (c) The 6-week follow-up radiograph shows that the internal resorption site is larger and more distinct.
Figure 2 Radiograph of the tooth. (a) After root canal treatment; (b) At the 1-year follow-up evaluation; (c) At the 2-year follow-up evaluation. 2-year follow-up radiograph reveals healing with the interposition of hard tissue between the fragments.
Figure 3 Radiograph of the right maxillary central incisor with horizontal root fracture. (a) After repositioning and applying a resin-wire splint; (b) After root canal treatment; (c) At the 2-year follow-up evaluation. 2-year follow-up radiograph reveals healing with the interposition of hard and soft tissue between the fragments.
Figure 4 Radiographs of the emergency visit shows the teeth. (a) Before the application of the resin-wire splint; (b) After repositioning and the application of the resin-wire splint.
Figure 5 Images were obtained 3 weeks after the trauma. (a) The periapical radiograph shows a radiolucent lesion around the fracture line on tooth #21; (b) The clinical photograph shows narrow and deep pocket depth and gingival swelling on tooth #21.
Figure 6 Radiograph of the teeth. (a) After the root canal treatment; (b) At the 1-year follow-up evaluation; (c) at the 2-year follow-up evaluation. The radiolucent lesion has disappeared on tooth #21. 2-year follow-up radiograph reveals healing with interposition of soft tissue between the fragments.
Figure 1
Figure 2
Figure 3
Figure 4
Figure 5
Figure 6
Healing after horizontal root fractures: 3 cases with 2-year follow-up

 KACD
KACD
 ePub Link
ePub Link Cite
Cite

