Articles
- Page Path
- HOME > Restor Dent Endod > Volume 37(3); 2012 > Article
- Case Report Diastema closure using direct bonding restorations combined with orthodontic treatment: a case report
- Soon-Kong Hwang, Jung-Hong Ha, Myoung-Uk Jin, Sung-Kyo Kim, Young-Kyung Kim
-
2012;37(3):-169.
DOI: https://doi.org/10.5395/rde.2012.37.3.165
Published online: August 29, 2012
Department of Conservative Dentistry, Kyungpook National University School of Dentistry, Daegu, Korea.
- Correspondence to Young-Kyung Kim, DDS, PhD. Associate Professor, Department of Conservative Dentistry, Kyungpook National University School of Dentistry, 2-188-1 Samduk-dong, Jung-gu, Daegu, Korea 700-412. TEL, +82-53-600-7601; FAX, +82-53-426-8958; wisekim@knu.ac.kr
• Received: February 3, 2012 • Revised: April 11, 2012 • Accepted: April 24, 2012
©Copyights 2012. The Korean Academy of Conservative Dentistry.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 1,924 Views
- 18 Download
- 11 Crossref
Abstract
- Closure of interdental spaces using proximal build-ups with resin composite is considered to be practical and conservative. However, a comprehensive approach combining two or more treatment modalities may be needed to improve esthetics. This case report describes the management of a patient with multiple diastemas, a peg-shaped lateral incisor and midline deviation in the maxillary anterior area. Direct resin bonding along with orthodontic movement of teeth allows space closure and midline correction, consequently, creating a better esthetic result.
Introduction
Tooth size discrepancy or inappropriate distribution of space in the anterior region of mouth is a major esthetic problem for patients.1 Amongst the suggested options for diastema closure such as orthodontic, restorative and prosthodontic treatment, the use of proximally applied resin composite seems to be more practical and conservative.2,3 Direct composite restoration has several distinct advantages, such as, conservation of tooth structure, reversibility of procedure, lower cost to patient and relative ease of addition or removal of materials when necessary.4 However, a number of clinical cases cannot be corrected or maintained by the restorative approach only. Therefore, an interdisciplinary approach that combines two or more treatment modalities may be required for better outcomes.5
The esthetic appearance of teeth forms a part of an overall picture, interacting closely with facial esthetics. Since a pleasant smile is governed largely by symmetry, asymmetry at the midline creates an unacceptable esthetic presentation for both patients and observers.6 When diastema closure is performed, dental midline as well as occlusal relationship and esthetic proportion of an individual tooth, must be considered and should coincide with the midline of face.7 This clinical case reports a patient with uneven interdental spaces and midline deviation in maxillary anterior region. The patient's esthetic expectations were successfully met through a comprehensive approach consisting of direct resin bonding and orthodontic movement to recontour the teeth and to correct the midline, respectively.
Case report
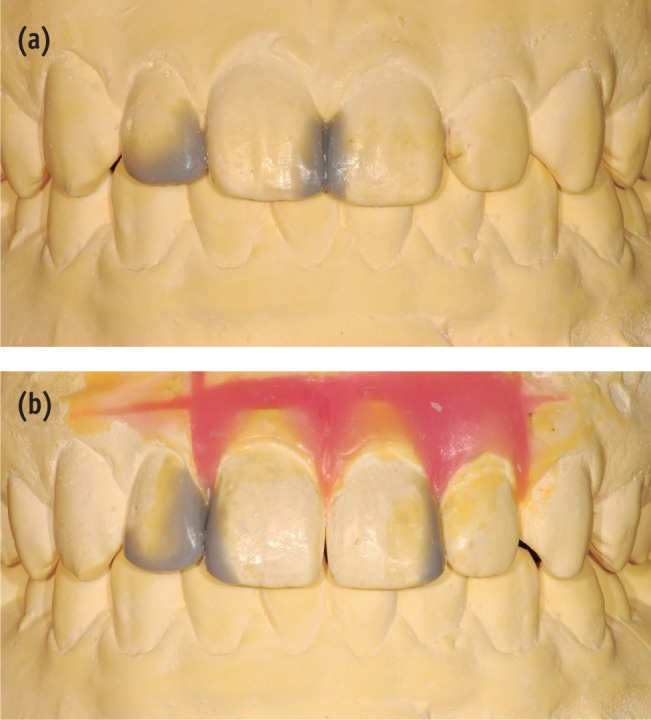
A 23-year-old male came to the Department of Conservative Dentistry, Kyungpook National University dental hospital, complaining about spaces among maxillary anterior teeth. Through a clinical examination, the esthetic problems of the patient in maxillary anterior part were uneven spaces among teeth from right lateral incisor to left canine, midline deviation to the right side and slightly pegshaped right lateral incisor (Figure 1). Meanwhile, there was no esthetic problem in mandibular anterior region. The widest interdental space was between two central incisors, approximately 1 mm. Maxillary midline had shifted 2 mm to the right side from facial midline. On the first visit, irreversible hydrocolloid impressions of both arches were taken to fabricate a diagnostic cast (Figure 2). The patient showed Angle class I malocclusion with normal overjet (2 mm) and overbite (2 mm). Since a proper size relationship in anterior teeth is very important to achieve an esthetic result, mesio-distal widths of anterior teeth of both arches were recorded to calculate intermaxillary tooth-size ratio.8 The sums of mesio-distal widths of maxillary and mandibular teeth were 46.0 and 36.8 mm, respectively. Tooth size ratio was then calculated according to the following formula:
Anterior Bolton ratio (%) = (sum of mesio-distal widths of mandibular anterior teeth/sum of mesio-distal widths of maxillary anterior teeth) × 100
When comparing the obtained value, the maxillary teeth appeared to be smaller (77.2%) than the average value (80.1%) and needed to be enlarged. Based on the analysis of the patient's face, tooth size discrepancy and the diagnostic cast, two different diagnostic wax-ups were made. One was a simple closure with composite addition on the right lateral incisor and the both central incisors (Figure 3a). The other was a set up model in which the interdental spaces were re-distributed from the right lateral incisor to the left canine and the midline was corrected through tooth movement. The spaces were then closed using direct resin composite (Figure 3b). Over the two diagnostic wax-ups, favorable results were predicted by the latter. Assuming the right central incisor would move to the left, the midline would be shifted to the left and harmonize with the facial midline. In addition, resin build-ups could be performed on the distal sides of the central incisors (Figure 3b). Since the tooth shape of the both central incisors was square, composite addition was needed on the distal side of the teeth rather than the mesial to provide an ideal tooth axis, slightly distal toward the apex. After a thorough consultation and review of the two options, the patient agreed to choose the second one. However, gingival level of the two central incisors was inharmonious and the right central incisor looked longer than the left central incisor. Although crown lengthening of the left central incisor was also considered during the presentation of the treatment plan to correct the gingival asymmetry and length discrepancy, the patient did not want a surgical procedure.
All preoperative data were collected and orthodontic treatment was initiated. The metal brackets (Gemini 018 Roth bracket, 3M Unitek, St. Paul, MN, USA) were bonded to the maxillary anterior teeth. A 0.16 × 0.22 inch TMA wire (TMA broad arch wire, Ormco Corp., Orange, CA, USA) was used, combined with an elastic chain (Super thread, Rocky Mountain Morita Corp., Tokyo, Japan) to move the left lateral incisor and the both central incisors toward the left side. After two weeks, the space between the left lateral incisor and the left canine was closed and the both central incisors moved to the left (Figure 4a), resulting in correcting the maxillary midline. To keep the space between the left central incisor and the left lateral incisor, a flowable resin (Unifil flow, GC Corp., Tokyo, Japan) was applied on the interdental space of the teeth. An open coil spring was then inserted between the right central incisor and the right lateral incisor in order to move the right central incisor in mesial direction (Figure 4b). The recall checks were carried out every other week.
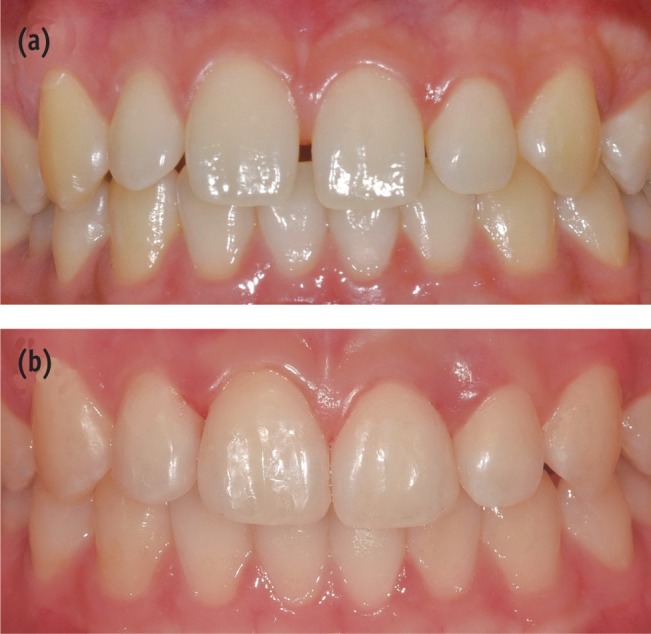
After six weeks of orthodontic treatment, the teeth were in proper positions. All brackets and wires were removed (Figure 5). An irreversible hydrocolloid impression of maxillary arch was taken and wax-up was performed again. A silicone index (Exafine Putty Type, GC Corp.) was obtained from the cast to guide the application of the first lingual composite layer. For direct resin bonding procedure of the left central incisor, tooth surfaces were cleaned with a slurry of fine pumice. Although the space of 1.5 mm or less can be successfully restored using a relatively translucent enamel shade, a mock-up with different shades/opacities of resin composites was done to accurately match not just single shade, but also the adjacent tooth structure.9 A superfine diamond bur was used to roughen the proximal enamel surfaces for optimal adhesion, extending from the facial line angle to the lingual line angle.10 With cotton rolls in place to isolate the operating field, a gingival retraction cord of size 00 was tucked in the gingival crevice to displace the tissue of interproximal gingival papilla. The adjacent tooth was separated by Teflon tape (P.T.F.E. thread seal tape, Chungku Industrial Co., Seoul, Korea). The enamel was etched with 32% phosphoric acid (Uni-Etch, BISCO Inc., Schaumburg, IL, USA) for 30 seconds. After rinsing and drying, bonding agent (One-Step, BISCO Inc.) was applied according to manufacturer's instructions and cured for 10 seconds using a LED curing unit (Sholuz, IV Tech., Seoul, Korea). A microhybrid resin composite, GRADIA DIRECT (GC Corp.) was used for the composite build-ups due to its good handling property and shade matching. The composite was placed and polymerized using a layering technique to simulate natural tooth color and translucency. Each layer was light-cured for 40 seconds each from facial and lingual directions. Once the putty index was placed, the first lingual composite layer of shade NT was applied. In order to avoid translucent 'shine through' effect, a small amount of an opaque dentin shade of resin (shade AO2) was added. The facial and incisal contours were then established by using A2, A1 and NT shade of resin composites in turn. Care was taken to achieve the desired proximal contour, especially in the gingival embrasure area. After closing the space between the left central incisor and the left lateral incisor, finishing and polishing of the restoration took place with Super Snap Discs (SHOFU Inc., Kyoto, Japan) in the sequence recommended by manufacturer (Figure 6). The other spaces were closed with the same technique as described previously and the incisal edge of the right lateral incisor was modified according to the shape of the left lateral incisor. After the restorative procedures, the final irreversible hydrocolloid impression of maxillary arch was taken to make a clear aligner which was used for retention of the both incisors from rotational or labial movement.11 The following check-ups of the patient were done for 3 months. As shown in Figure 6, it was possible to obtain an optimal esthetic result with a combination of restoration and minor tooth movement. Although the patient was satisfied with the appearance, a better result would be obtained if the gingival level of the central incisors had been corrected through a periodontal approach.
Discussion
In clinical cases wherein conservative, esthetic correction of the appearance of anterior teeth is indicated, direct bonded composite restorations may be preferable. However, for better esthetic results, an interdisciplinary approach is often required. In this case, through minor tooth movement, the deviated maxillary midline was corrected and harmonized with the facial midline. The use of conservative direct resin bonding, such as proximal build-ups and recontouring of tooth shape provided the symmetrical and harmonious arrangement of the teeth.
Conclusions
The comprehensive approach combining direct composite build-ups and orthodontic tooth movement resulted in more successful outcome and patient's satisfaction rather than simple closure with composite addition.
- 1. Wolff D, Kraus T, Schach C, Pritsch M, Mente J, Staehle HJ, Ding P. Recontouring teeth and closing diastemas with direct composite buildups: a clinical evaluation of survival and quality parameters. J Dent 2010;38:1001-1009.ArticlePubMed
- 2. Lenhard M. Closing diastemas with resin composite restorations. Eur J Esthet Dent 2008;3:258-268.PubMed
- 3. Kim YH, Cho YB. Diastema closure with direct composite: architectural gingival contouring. J Korean Acad Conserv Dent 2011;36:515-520.Article
- 4. Heymann HO, Hershey HG. Use of composite resin for restorative and orthodontic correction of anterior interdental spacing. J Prosthet Dent 1985;53:766-771.ArticlePubMed
- 5. Kuljic BL. Merging orthodontics and restorative dentistry: an integral part of esthetic dentistry. J Esthet Restor Dent 2008;20:155-163.ArticlePubMed
- 6. Zhang YF, Xiao L, Li J, Peng YR, Zhao Z. Young people's esthetic perception of dental midline deviation. Angle Orthod 2010;80:515-520.ArticlePubMedPMC
- 7. Brisman AS. Esthetics: a comparison of dentist's and patient's concepts. J Am Dent Assoc 1980;100:345-352.ArticlePubMed
- 8. Lasseigne TP, Chiche G, Tokutomi H, Wiltz II CP, Mendez AJ. Managing space in the anterior dentition. Am J Esthet Dent 2011;1:138-157.
- 9. Murchison DF, Roeters J, Vargas MA, Chan DCN. In: Summitt JB, Robbins JW, Hilton TJ, Schwartz RS, editors. Direct Anterior Restorations. Fundamentals of Operative Dentistry: A Contemporary Approach. 2006. 3rd ed. Chicago: Quintessence; p. 274-279.
- 10. Heymann HO. In: Roberson TM, Heymann HO, Swift EJ Jr, editors. Additional Conservative Esthetic Procedures. Sturdevant's Art and Science of Operative Dentistry. 2006. 5th ed. St. Louis: Mosby; p. 635.Article
- 11. Kim TW, Echarri P. Clear aligner: an efficient, esthetic, and comfortable option for an adult patient. World J Orthod 2007;8:13-18.PubMed
REFERENCES
Figure 1

Preoperative photograph. Note the unevenly distributed interdental spaces among maxillary anterior teeth and midline deviation of 2 mm to right side of maxillary arch.

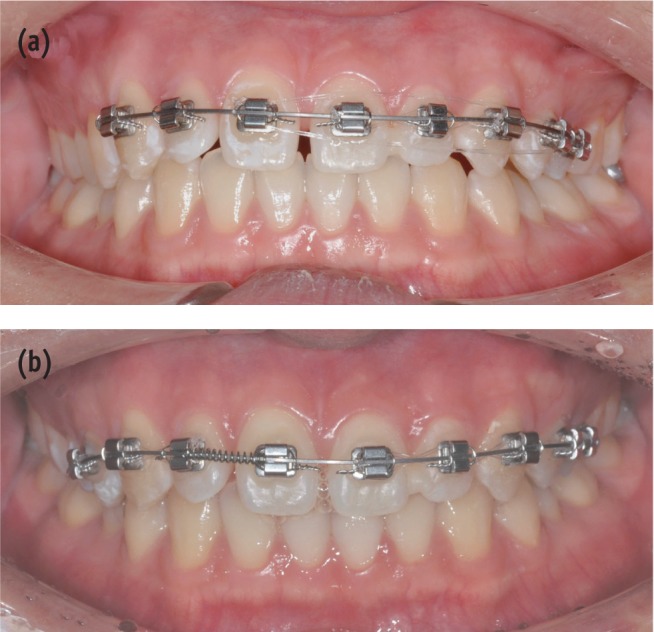
Figure 2
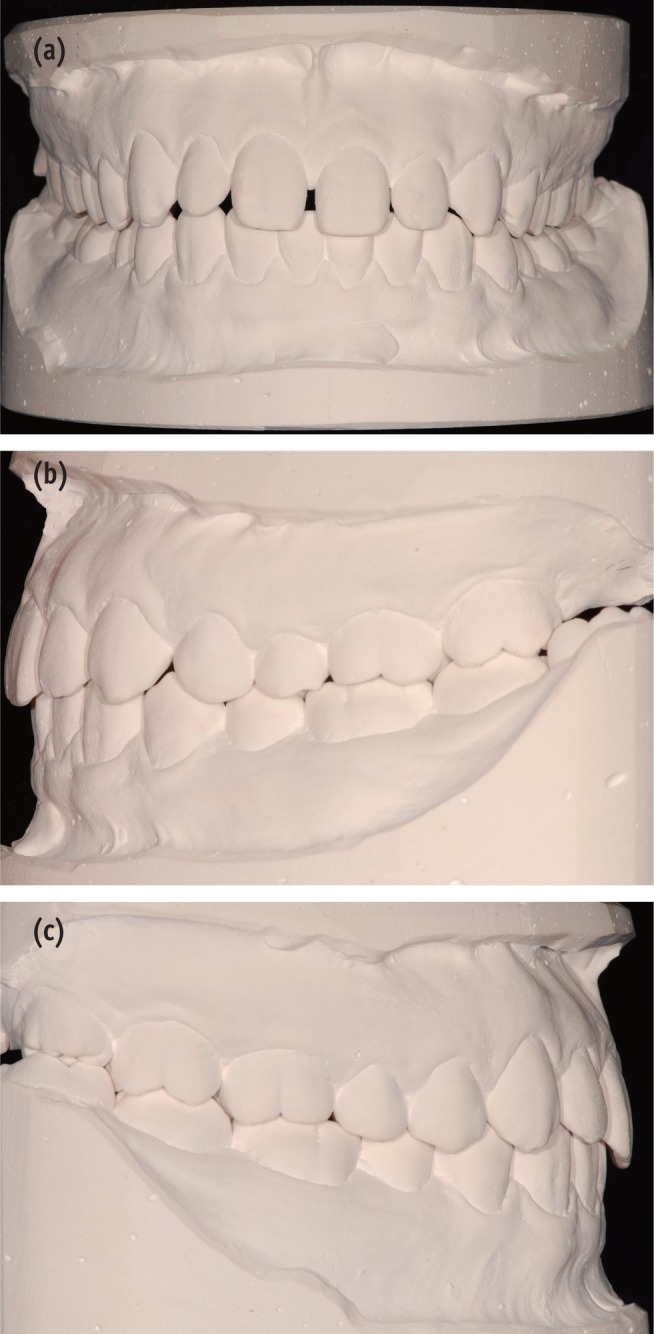
Diagnostic cast. (a) Frontal view; (b) Side view, left; (c) Side view, right; The patient showed Angle class I malocclusion with normal overjet (2 mm) and overbite (2 mm).
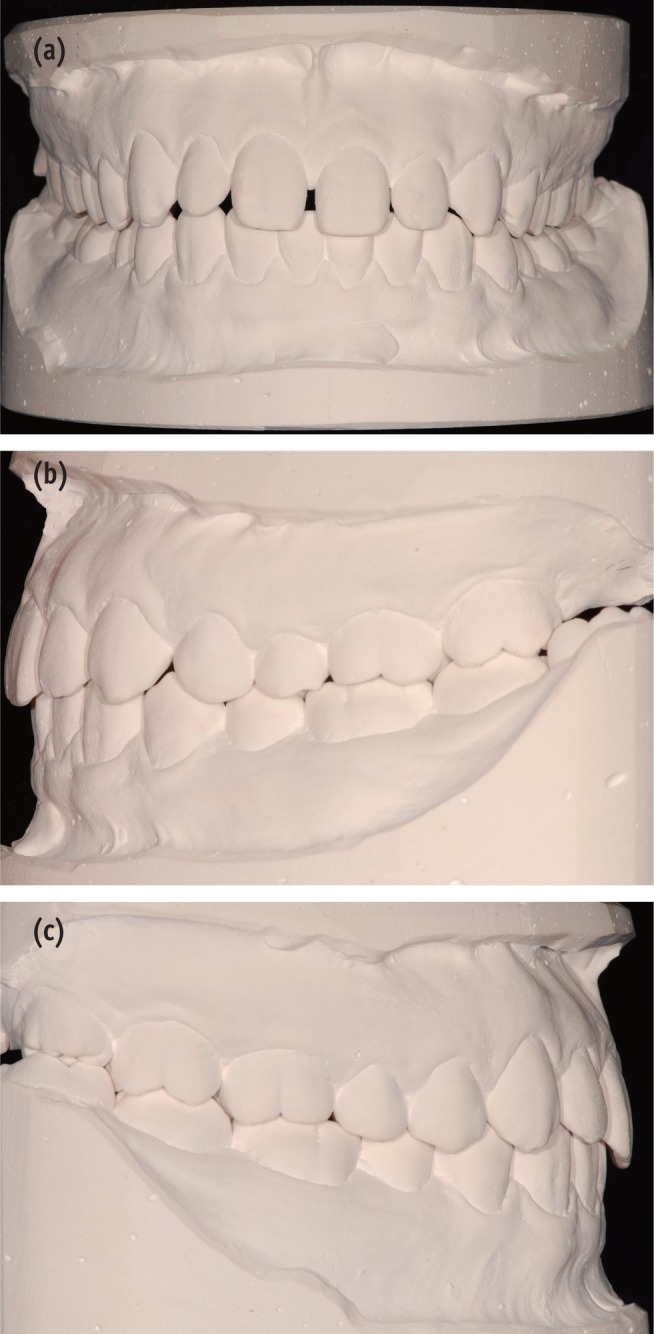
Figure 3
Two different diagnostic wax-ups. (a) Direct composite build-ups only; (b) Direct composite build-ups combined with orthodontic tooth movement.
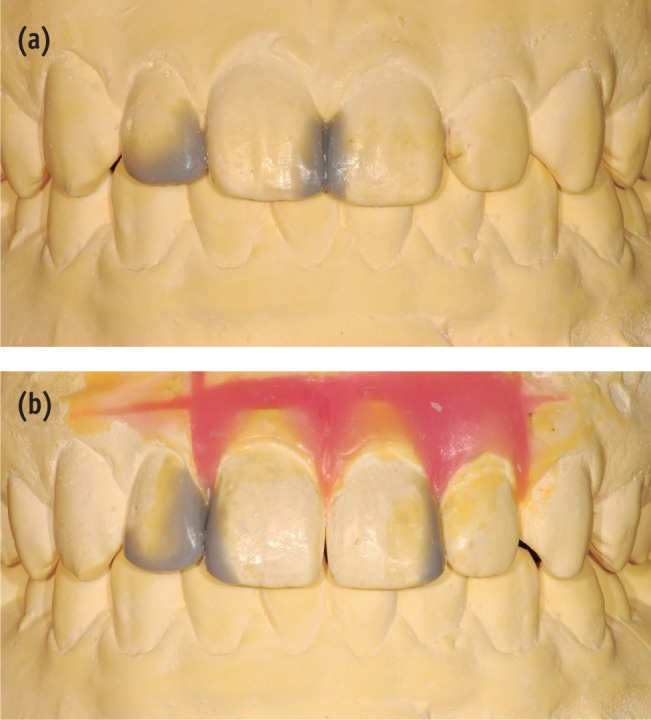
Figure 4
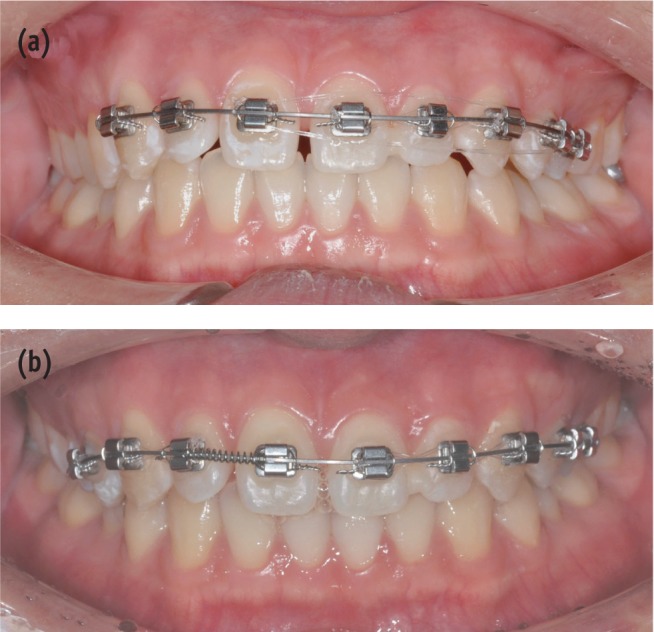
Orthodontic tooth movement. (a) A 0.16 × 0.22 inch TMA wire was used for arranging the teeth; (b) An open coil spring was inserted between right central incisor and right lateral incisor for mesial movement of right central incisor.
Tables & Figures
REFERENCES
Citations
Citations to this article as recorded by 

- Gingival Conditioning with Provisional Composite Veneer Prior to Final Dental Restoration: Three-year Follow-up
B Mueller, GB Rauber, LA Linhares, JK Bernardon, E Santini, LF Pottmaier
Operative Dentistry.2023; 48(3): 237. CrossRef - Effectiveness, longevity, and color stability of in-office bleaching (6% H2O2 gel/Violet LED) and diastema closure with direct composite: 3-year follow-up
Ikejiri Larissa Luri Almeida Amorim, Álamo Larissa , Galli Mateus Zamora , Bombonatti Juliana Fraga Soares , de Amoêdo Campos Velo Marilia Mattar , Mondelli Rafael Francisco Lia
Journal of Clinical Advances in Dentistry.2023; 7(1): 001. CrossRef - Ortodontik Tedavi Bitiminden Sonra Polidiastemanın Kompozit Rezin Ile Rehabilitasyonu: Olgu Sunumu
Rümeysa BATTAL, Hacer Deniz ARISU
Selcuk Dental Journal.2022; 9(4): 127. CrossRef - Multidisciplinary Approach to Treatment of Midline Diastema With Edge-to-Edge Bite
Sumukh Nerurkar, Ranjit Kamble, Japneet Kaiser, Jeni Mathew
Cureus.2022;[Epub] CrossRef - ÜST ANTERİOR DİŞLERDE BULUNAN ÇÜRÜKLERİN VE ESKİ RESTORASYONLARIN KOMPOZİT REZİNLER İLE ESTETİĞİNİN SAĞLANMASI: BİR VAKA SUNUMU
Abdulkadir HARMANKAYA, Hakan Yasin GÖNDER
Selcuk Dental Journal.2022; 9(4): 86. CrossRef - ANTERİOR DİASTEMALARIN DİREKT KOMPOZİT REZİN RESTORASYONLARLA ESTETİK REHABİLİTASYONU: 5 OLGU SUNUMU
Handan YILDIRIM, Esra ÖZYURT
Selcuk Dental Journal.2020; 7(2): 334. CrossRef - VAKUMLA ŞEKİLLENDİRİLEN ORTODONTİK PEKİŞTİRME APAREYLERİNİN KOMPOZİT RESTORASYONLARIN KLİNİK BAŞARISINA ETKİSİ
Serdar AKARSU, Sultan AKTUĞ KARADEMİR, Süleyman Kutalmış BÜYÜK
Atatürk Üniversitesi Diş Hekimliği Fakültesi Dergisi.2020; : 1. CrossRef - Aesthetic Smile Coming with Direct Composite Resin Laminate Restorations: Two Case Reports
Funda Demir, Elif Aybala Oktay, Numan Aydın, Fulya Toksoy Topçu, Ertürk Bilgeç
Ankara Medical Journal.2018;[Epub] CrossRef - Effects of Different Demineralization‐Inhibiting Methods on the Shear Bond Strength of Glass‐Ceramics
Erhan Dilber, Mehmet Akın, Tevfik Yavuz, Ali Erdem
Journal of Prosthodontics.2015; 24(5): 407. CrossRef - Correction of Mandibular Prognathism in Combination with Polydiastema Using Rectangular Body Ostectomy: Literature Review and Case Report
Metin Sencimen, Abdullah Tugrul Coskun, Gurkan Rasit Bayar, Handan Altug, Hasan Ayberk Altug, Tamer Zerener
Case Reports in Clinical Medicine.2014; 03(11): 601. CrossRef - Predictable interproximal tissue removal with a surgical stent
Fausto Frizzera, Suzane Cristina Pigossi, Mateus Rodrigues Tonetto, William Kabbach, Elcio Marcantonio
The Journal of Prosthetic Dentistry.2014; 112(4): 727. CrossRef
Diastema closure using direct bonding restorations combined with orthodontic treatment: a case report

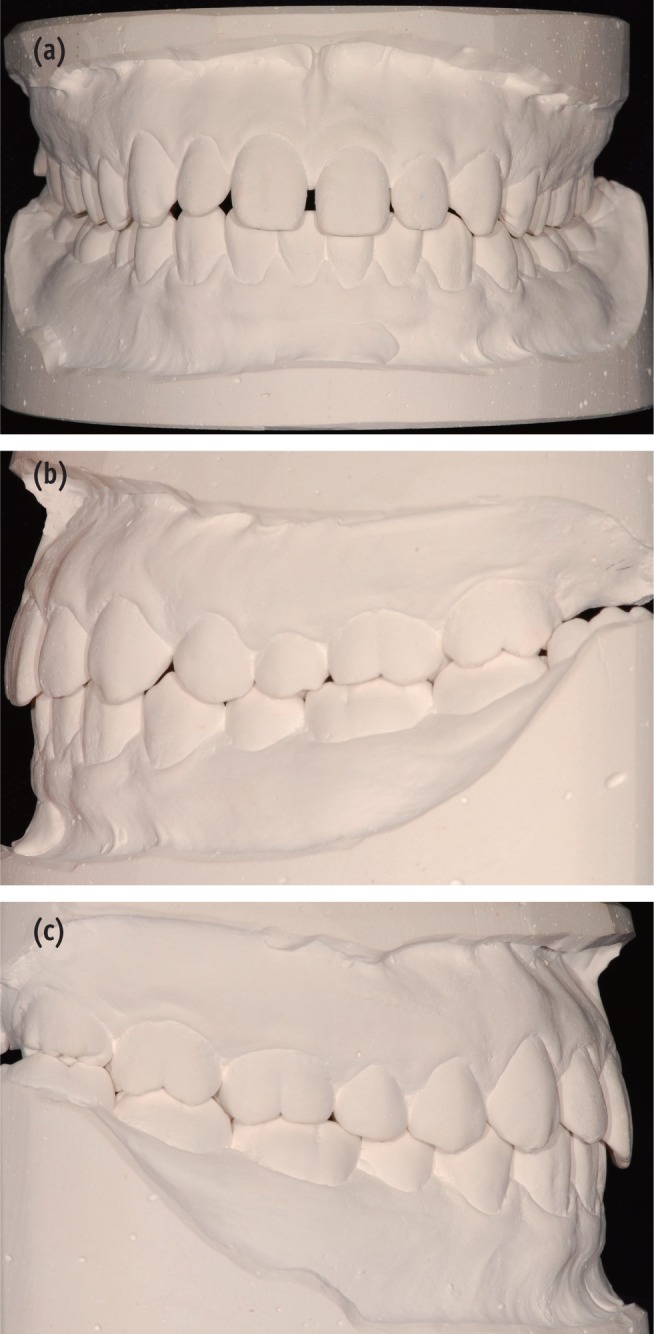
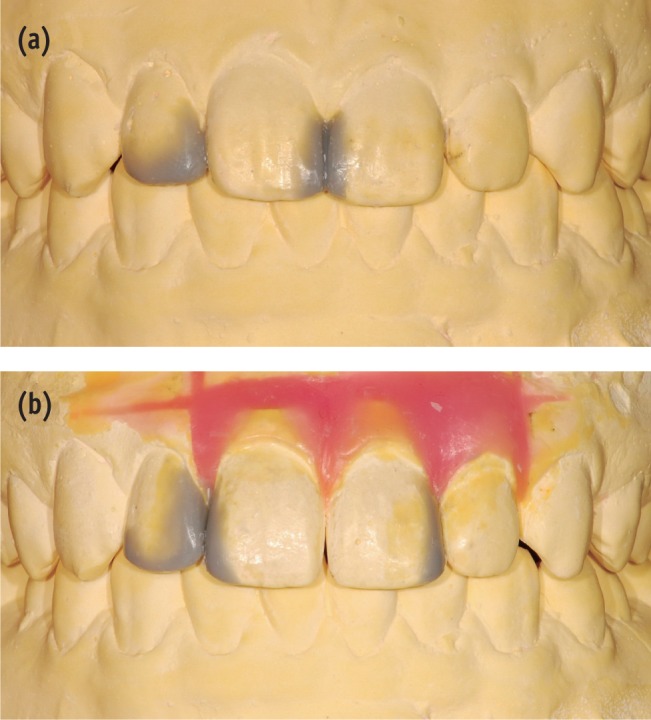
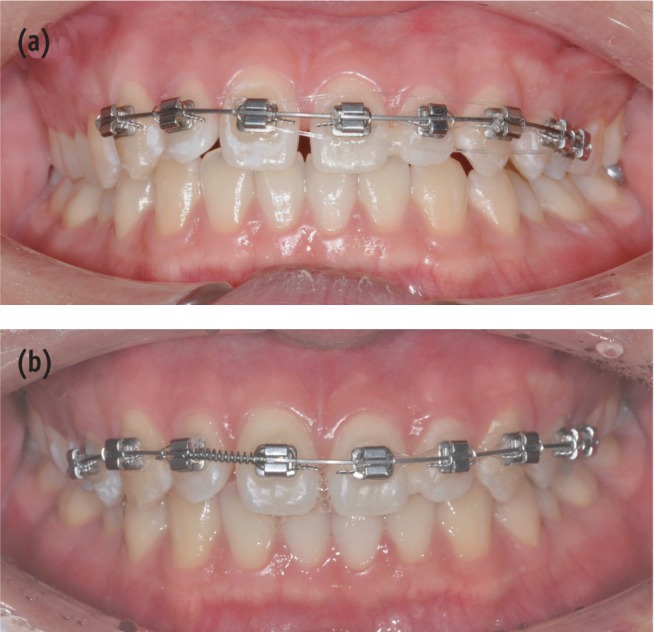

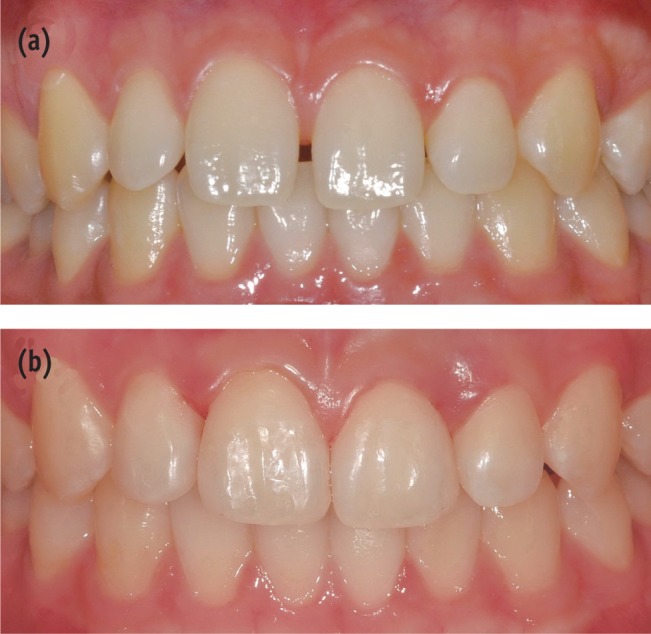
Figure 1 Preoperative photograph. Note the unevenly distributed interdental spaces among maxillary anterior teeth and midline deviation of 2 mm to right side of maxillary arch.
Figure 2 Diagnostic cast. (a) Frontal view; (b) Side view, left; (c) Side view, right; The patient showed Angle class I malocclusion with normal overjet (2 mm) and overbite (2 mm).
Figure 3 Two different diagnostic wax-ups. (a) Direct composite build-ups only; (b) Direct composite build-ups combined with orthodontic tooth movement.
Figure 4 Orthodontic tooth movement. (a) A 0.16 × 0.22 inch TMA wire was used for arranging the teeth; (b) An open coil spring was inserted between right central incisor and right lateral incisor for mesial movement of right central incisor.
Figure 5 Midline correction and re-distribution of interdental spaces after minor tooth movement. Through the movement of both central incisors to the left, midline was corrected and interdental spaces were re-distributed.
Figure 6 Diastema closure with an interdisciplinary approach. (a) Preoperative photograph; (b) Postoperative photograph. Interdental spaces were closed and maxillary midline was corrected with a combination of restoration and minor tooth movement.
Figure 1
Figure 2
Figure 3
Figure 4
Figure 5
Figure 6
Diastema closure using direct bonding restorations combined with orthodontic treatment: a case report

 KACD
KACD

 ePub Link
ePub Link Cite
Cite

