Abstract
-
Purpose
Intentional replantation (IR) is a suitable treatment option when nonsurgical retreatment and periradicular surgery are unfeasible. For successful IR, fracture-free safe extraction is crucial step. Recently, a new extraction method of atraumatic safe extraction (ASE) for IR has been introduced.
-
Patients and Methods
Ninety-six patients with the following conditions who underwent IR at the Department of Conservative Dentistry, Seoul National University Bundang Hospital, in 2010 were enrolled in this study: failed nonsurgical retreatment and periradicular surgery not recommended because of anatomical limitations or when rejected by the patient. Preoperative orthodontic extrusive force was applied for 2-3 weeks to increase mobility and periodontal ligament volume. A Physics Forceps was used for extraction and the success rate of ASE was assessed.
-
Results
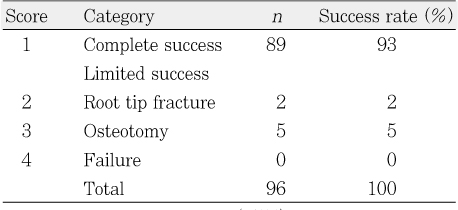
Ninety-six premolars and molars were treated by IR. The complete success rate (no crown and root fracture) was 93% (n = 89); the limited success rates because of partial root tip fracture and partial osteotomy were 2% (n = 2) and 5% (n = 5), respectively. The clinical and overall success rates of ASE were 95% and 100%, respectively; no failure was observed.
-
Conclusions
ASE can be regarded as a reproducible, predictable method of extraction for IR.
-
Keywords: Atraumatic safe extraction; Intentional replantation; Orthodontic extrusion; Physics forceps
INTRODUCTION
Intentional replantation (IR) is the final treatment option to save teeth when the conventional or nonsurgical root canal treatment fail and periradicular surgery is unfeasible. In IR, a safely extracted tooth is treated outside the oral cavity in a controlled environment and is replaced into its original alveolar socket.
1 Studies revealed that IR has a relatively high success rate, although differing according to the researcher, and is a predictable and reliable treatment option.
2-
4
Many authors emphasize that safe extraction without crown or root fracture is the primary prerequisite for successful IR.
1,
2,
4,
6 However, many teeth indicated for IR are weakened by repetitive root canal treatments and root canal post, etc.
6,
7 Moreover, molar teeth require a significant amount of load during extraction due to broad root surface; curved and divergent roots also make fracture-free safe extraction difficult.
8 Nonetheless, little is known about the practical extraction methods for IR, except that an elevator should not be used and the beak of the conventional extraction forceps should be placed on the crown above the cementoenamel junction.
5 Many clinicians regard IR difficult because of the scant information on specific extraction methods.
Atraumatic safe extraction (ASE) for IR using the newly developed Physics Forceps
9 along with preoperative orthodontic treatment has been introduced recently.
10 The aim of this study was to evaluate the clinical reliability of ASE for IR.
PATIENTS AND METHODS
This retrospective study was approved by the Institutional Review Board (IRB) of Seoul National University Bundang Hospital (IRB No. B-1011-115-103).
Patients
Ninety-six patients who underwent IR at the Department of Conservative Dentistry of the Seoul National University Hospital in 2010 were enrolled. Their average age was 41.5 ± 13.7 years (range, 14-75 years). There were 42 male patients and 54 female patients. Some had visited the hospital for periradicular disease treatment; the others were referred by private dental clinics for nonsurgical retreatment, periradicular surgery, or IR. None of the patients had a noticeable medical history, and all were in relatively good health. Patients with severe periodontal disease were excluded. Periradicular surgery was unfeasible in 79 patients in whom nonsurgical retreatment was ineffective and retrieval or bypass was impossible because of the presence of a fractured root canal instrument or calcified root canal. Periradicular surgery was not recommended in cases of proximity to anatomical structures such as the inferior alveolar nerve and maxillary sinus, the presence of thick cortical bone, or a combination of these two conditions. Some teeth had root perforation or cracks; in other cases, the patients rejected nonsurgical retreatment and periradicular surgery, whereas some wanted dental implants after extraction. The patients were informed about the IR procedure and gave their written consent.
The entire IR procedure, from extraction to periapical treatment and replantation, was performed by one endodontist with experience in surgical root canal treatment using conventional local anesthesia and the appropriate sterilized surgical environment.
ASE procedure
Orthodontic procedure
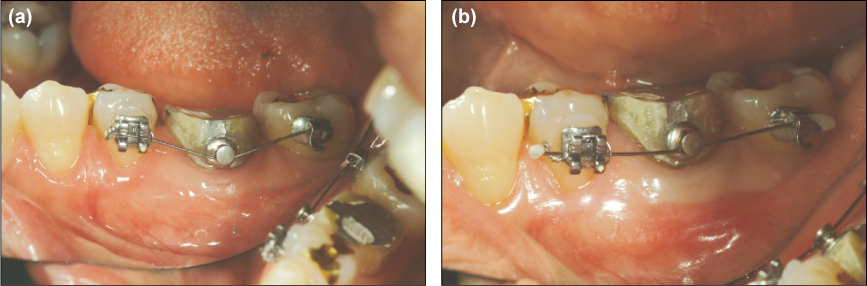
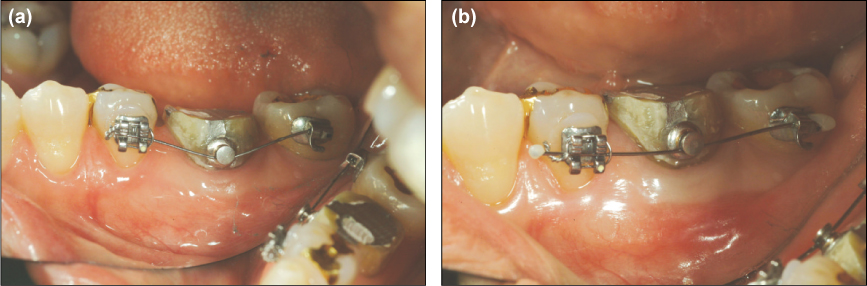
An orthodontic bracket was attached slightly toward the gingival side of the buccal surface of the tooth requiring IR. A .014 Ni-Ti round wire was then ligated, and 50 g of orthodontic extrusive force was applied onto the tooth for 2-3 weeks (
Figure 1a). Occlusal reduction was needed to ensure adequate space for extrusion. In general, no ankylosis was noted; increased mobility in addition to 1-2 mm extrusion could be observed (
Figure 1b). For the most posterior teeth, such as the second molars, a .016 × .022 TMA wire was applied by using the cantilever method to apply extrusive force. If necessary, an orthodontic micro-implant could be used (
Figures 2a and 2b).
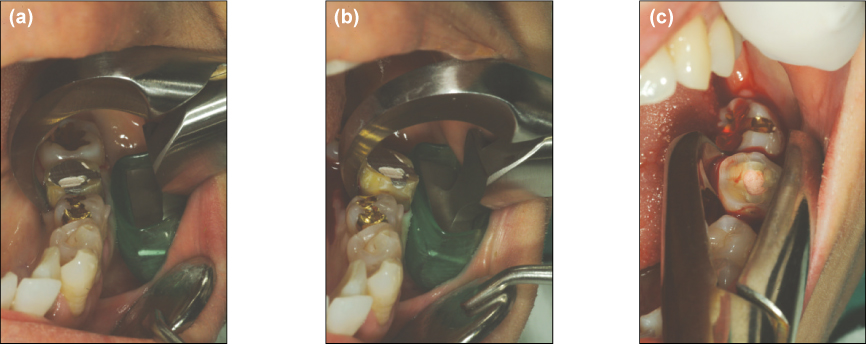
Surgical procedure
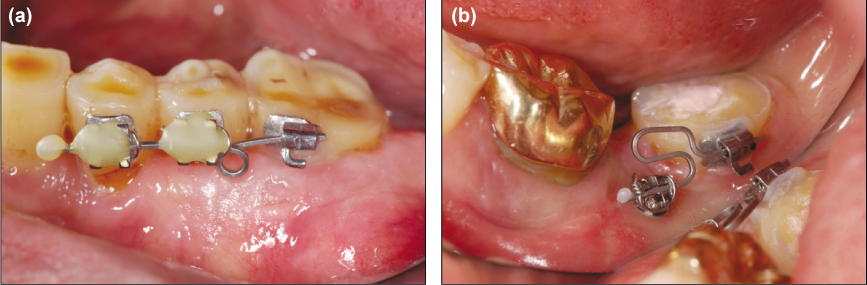
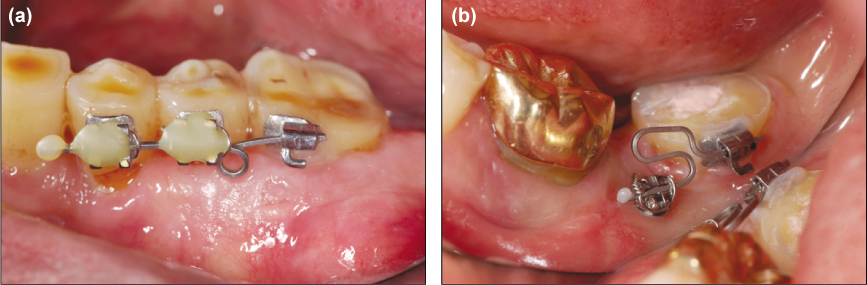
Under conventional local anesthesia, the beak of a Physics Forceps was placed against the lingual side or palatal root surface of the tooth. Thereafter, the buccal-side bumper of the forceps was placed at the mucogingival junction level of the buccal surface and firmly secured without squeezing the handle or movement. By using only the wrist, a steady, slow rotational force was applied (
Figure 3a). If the tooth rotated or elevation was observed, the rotational action was stopped and complete extraction was performed by using the conventional forceps (
Figures 3b and 3c).
The extraction time was measured in seconds from the moment of extraction force was applied until the tooth was completely removed from its socket. The extracted tooth was then observed under an operating microscope (OPMI Pico, Carl Zeiss, Oberkochen, Germany) to detect problems of root including crack, fracture and perforation, etc.
Assessment
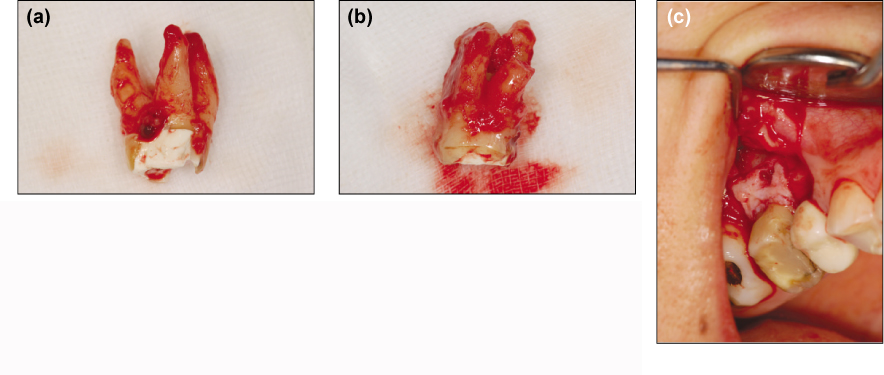
The success of extraction was based on the following criteria:
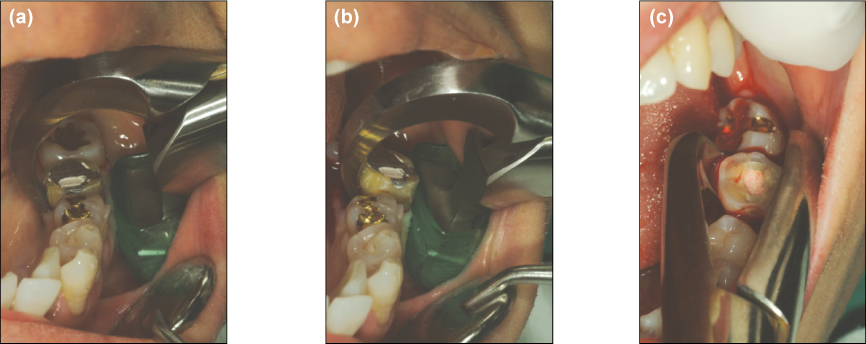
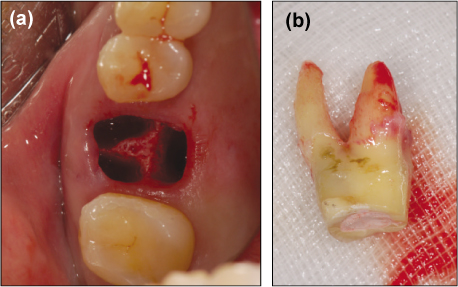
Complete success: extraction without crown and root fracture (Figure 4a)
Limited success with root tip fracture: extraction involving partial root tip fracture that did not hamper IR (Figure 4b)
Limited success with osteotomy: fracture-free extraction and partial osteotomy in case of divergent roots and thick cortical bone was present (Figure 4c)
Failure: extraction with crown or root fracture making IR impossible
Furthermore, the presence of a postoperative sensory disorder (paresthesia or hyperesthesia) was noted.
RESULTS
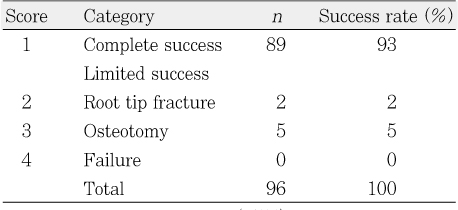
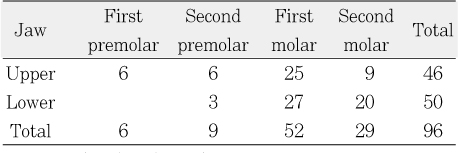
Table 1 presents the distribution of the teeth requiring IR. In most cases, the patients did not feel pain during orthodontic extrusion. When a patient complained of pain, the application of an excessive extrusive load was checked. The average extraction time was 4 minutes 8 seconds (range, 40 seconds-22 minutes 12 seconds). After orthodontic extrusion, increased mobility led to easier and faster extraction; the partial osteotomy cases required a relatively long time for extraction.
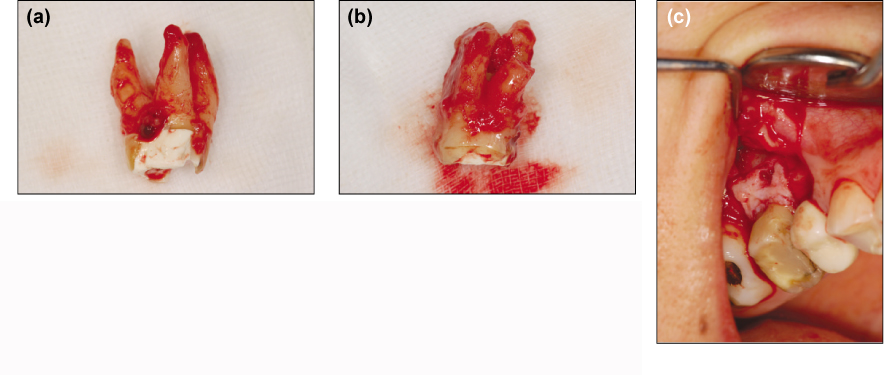
Table 2 presents the success rates of all the extracted teeth. With regard to limited success, root tip fracture occurred in two cases (mandibular second premolar and mandibular first molar;
Figure 4b) and osteotomy was performed on four maxillary first molars and one mandibular first molar (
Figure 4c). During extraction, greenstick fractures on the buccal side of the alveolar bone occurred in two mandibular first molars; although soft tissue suturing and postoperative finger compression were necessary in such cases, no concerns such as alveolar bone resorption occurred and healing was uneventful. Concurrent extraction and removal of the septal bone were performed on two mandibular second molars (
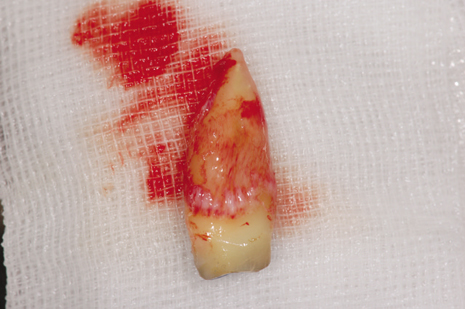
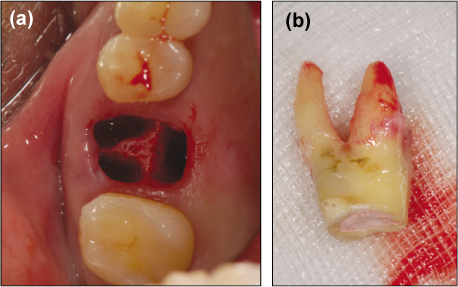
Figure 5). In most cases except those with osteotomy, almost no damage to the teeth and peripheral soft tissue was observed (
Figures 6a and 6b).
No patient complained of paresthesia or hyperesthesia. In addition, no cases of severe edema or systemic infection were observed. All the extracted teeth were replaced after apicoectomy outside the oral cavity. Currently, they are under observation to check their prognosis.
DISCUSSION
Some authors have reported high success rates after long-term observation of the prognosis of IR and low rates of adverse effects such as root resorption and alveolar bone loss. Moreover, they assert that IR should be considered as a treatment option that can be regarded concurrently with other treatment rather than as the final treatment.
2,
6 Despite the many positive studies on IR, however, there is hesitation to apply the method clinically, because a safe, repeatable extraction is unpredictable in most cases.
5 Posterior teeth for which IR is required, most cases are multi-rooted teeth. Furthermore, repetitive root canal treatments weakened the physical strength of the tooth, posing inevitable difficulty in safe extraction without fracture.
11 Choi et al.
10 introduced ASE for IR. In this method, preoperative orthodontic extrusion increase periodontal ligament volume and tooth mobility; and then, extraction using the Physics Forceps, even multirooted molars can be extracted safely without fracture.
Hayashi
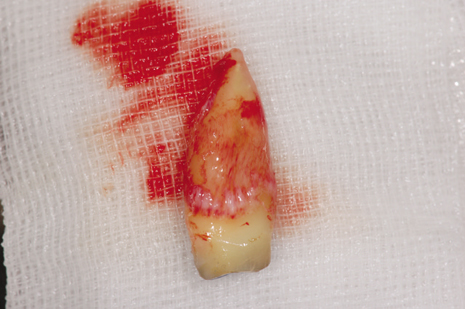
12 revealed that the use of orthodontic extrusion in autotransplantation of teeth facilitates extraction and increases periodontal ligament volume, ultimately promoting new or reattachment after transplantation (
Figure 7). In particular, the periodontal ligament on the root surface is crucial for the healing process: the bigger is its volume, the better is the prognosis.
13 In this study, most of the teeth with an extrusive load for 2-3 weeks showed increased mobility, which in turn enabled easier extraction. If the mobility does not increase, additional partial osteotomy can be used; the clinician can assess the level of difficulty of extraction in advance (
Figure 4c). Kany
14 reported successful prognosis after IR with accompanying osteotomy to protect the periodontal ligament.
Although an elevator should not be used and the forceps should be placed on the crown above the cementoenamel junction during extraction for IR. Therefore, damage to the periodontal ligament attached to the root is avoidable procedure, causing following damage to the marginal periodontal tissue (
Figure 8).
5 By gripping the root surface below the cementoenamel junction, however, fracture-free extraction is possible, although this damages the periodontal ligament.
14
Misch and Perez
9 developed the Physics Forceps for dental implant placement immediately after extraction to minimize damage to the root and especially marginal periodontal tissue. The bumper of the forceps acts as a fulcrum and prevents fracture of the buccal alveolar bone (
Figures 3a and 3b). In addition, by using the principle of a type 1 lever, force can be loaded vertically, facilitating safe extraction. The beak contacts only the lingual side, minimizing damage to the gingiva and alveolar bone, and significantly lowering the possibility of crown or root fracture. Actually, no case of tooth fracture occurred in this study.
The two cases of root tip fracture during extraction were caused by hypercementosis and a curved root tip (
Figure 4b). However, the broken root tip length was insignificant considering the amount resected during apicoectomy, eventually causing no impact on IR. Partial osteotomy was performed for extraction when mobility did not increase after preoperative orthodontic extrusion; lack of extraction despite weak, consistent force applied for a long time; and particularly, for cases with thick buccal bone. However, the osteotomy did not significantly affect the hard and soft tissue healing process.
In this retrospective study, a complete success rate of 93% was achieved, or 95% when limited success with root tip fracture was included. When cases of concurrent osteotomy with ASE were considered, the overall extraction success rate reached 100%. In conclusion, the ASE method should be considered as reliable extraction method for safe and successful IR; it is expected to contribute greatly to save natural teeth. However, long-term observation of its prognosis is required.
REFERENCES
- 1. Grossman LI. Intentional replantation of teeth: a clinical evaluation. J Am Dent Assoc. 1982;104: 633-639.ArticlePubMed
- 2. Kingsbury BC Jr, Wiesenbaugh JM Jr. Intentional replantation of mandibular premolars and molars. J Am Dent Assoc. 1971;83: 1053-1057.ArticlePubMed
- 3. Benenati FW. Intentional replantation of a mandibular second molar with long-term follow-up: report of a case. Dent Traumatol. 2003;19: 233-236.ArticlePubMedPDF
- 4. Peer M. Intentional replantation - a 'last resort' treatment or a conventional treatment procedure? nine case reports. Dent Traumatol. 2004;20: 48-55.ArticlePubMedPDF
- 5. Kratchman S. Intentional replantation. Dent Clin North Am. 1997;41: 603-617.ArticlePubMed
- 6. Bender IB, Rossman LE. Intentional replantation of endodontically treated teeth. Oral Surg Oral Med Oral Pathol. 1993;76: 623-630.ArticlePubMed
- 7. Assif D, Gorfil C. Biomechanical considerations in restoring endodontically treated teeth. J Prosthet Dent. 1994;71: 565-567.ArticlePubMed
- 8. Al-Shammari KF, Kazor CE, Wang HL. Molar root anatomy and management of furcation defects. J Clin Periodontol. 2001;28: 730-740.ArticlePubMedPDF
- 9. Misch CE, Perez HM. Atraumatic extractions: a biomechanical rationale. Dent Today. 2008;27: 98. 100-101.
- 10. Choi YH, Bae JH, Kim YK. Atraumatic safe extraction for intentional replantation. J Korean Dent Assoc. 2010;48: 531-537.ArticlePDF
- 11. Sorensen JA, Engelman MJ. Ferrule design and fracture resistance of endodontically treated teeth. J Prosthet Dent. 1990;63: 529-536.ArticlePubMed
- 12. Hayashi H. Ortho-transplantation. 2006;1st ed. Seoul: Narae Publishing Co.; 18-28.
- 13. Tsukiboshi M, Andreasen J, Asai Y. Autotransplantation of teeth. 2001;1st ed. Tokyo: Quintessence; 22-40.
- 14. Kany FM. Single-tooth osteotomy for intention replantation. J Endod. 2002;28: 408-410.ArticlePubMed
Figure 1(a) Orthodontic brackets and wire attached to a left mandibular first molar requiring IR. In this case, a button was used; however, any devices can be used as long as an extrusive force is applied. (b) Twenty-two days after orthodontic extrusive force was applied. Given the straightening of the wire, tooth extrusion was assumed to have occurred; concurrently, mobility increased.
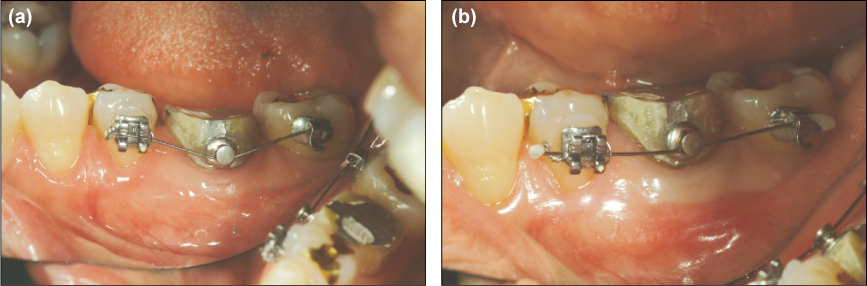
Figure 2(a) Extrusive force was applied on the most posterior tooth, using a .016 × .022 TMA wire as a coil spring. (b) If no appropriate anchor position is available, an orthodontic implant can be used for anchorage.
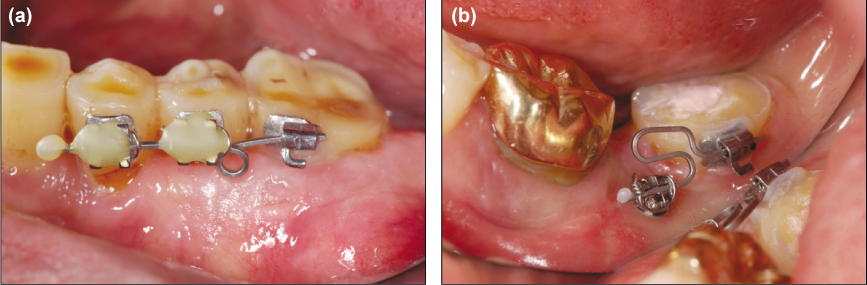
Figure 3(a) Positioning of the Physics Forceps. Ensure that the beak is placed only on the lingual root surface to significantly reduce the possibility of crown or root fracture. (b) Extraction procedure. A weak but consistent force was applied for extraction. The mandibular left 1st molar was extracted with rotational force. (c) Once the tooth rotated, then conventional forcep was used to extracted completely. The extraction time in this case was 1 minute 17 seconds. (photograph of another patient)
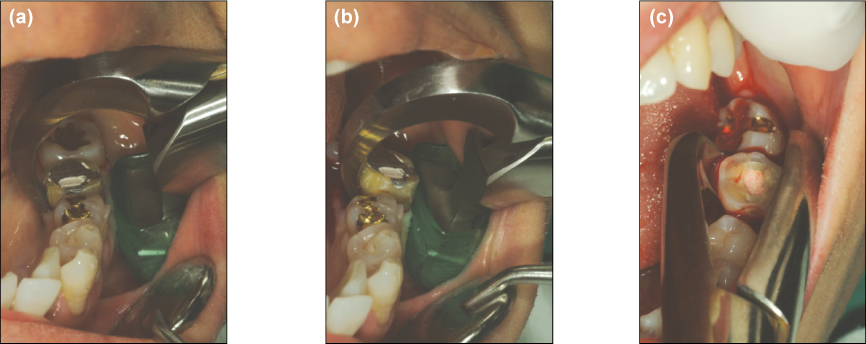
Figure 4(a) The maxillary first molar was successfully extracted by ASE. The extraction time was 5 minutes 17 seconds. (b) Limited success with root tip fracture. The curved distolingual root tip of the mandibular left molar fractured during extraction. The extraction time was 4 minutes. (c) Limited success with osteotomy. The maxillary first molar showed no increased mobility after orthodontic extrusion; its divergent buccal and palatal roots and particularly thick buccal cortical bone were possibly responsible. The extraction time including osteotomy was 10 minutes 31 seconds.
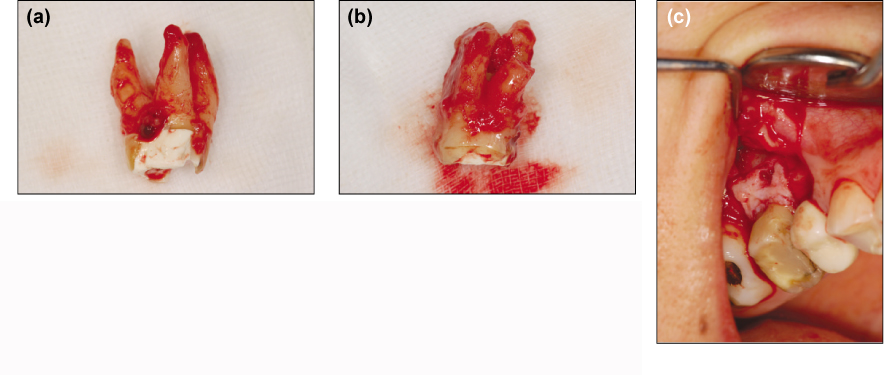
Figure 5The mandibular second molar was extracted concurrently with the septal bone. The extraction time was 15 minutes 46 seconds.

Figure 6(a) Extraction socket of a right maxillary first molar. No soft tissue damage is observable, and the alveolar bone is well preserved. (b) The extracted tooth. The extraction time was 3 minutes 30 seconds.
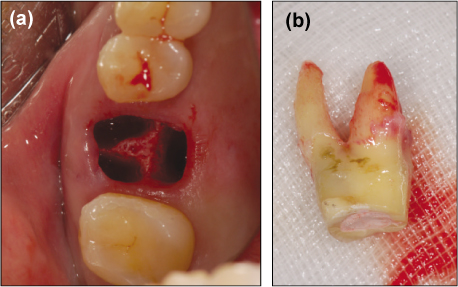
Figure 7An extracted right maxillary second premolar. The elongated periodontal ligament attached to the root area can be seen, helping the replanted tooth to heal uneventfully.
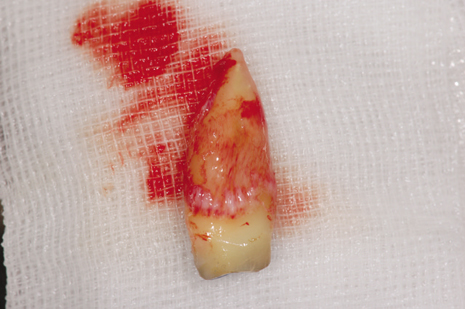
Figure 8A maxillary premolar extracted for orthodontic treatment. The beak of the forceps is located in the subgingival area, damaging the periodontal ligament, gingiva, and alveolar bone. The greater is the damage to the marginal tissue, the less likely is primary closure.

Table 1Tooth distribution for IR
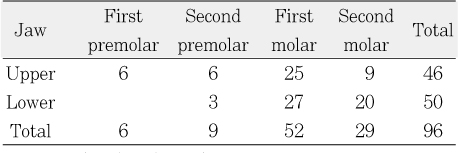
Table 2Scale for evaluating the clinical and overall success rates of ASE





 KACD
KACD

 ePub Link
ePub Link Cite
Cite

