Abstract
-
Objectives
This study evaluated the effect of ProTaper Next (PTN), ProTaper Universal Retreatment (PTR) and hybrid instrumentation (HI) for canal filling removal on the fracture resistance (FR), mode of failure (MoF), and filling removal time.
-
Materials and Methods
Ninety-six, mandibular premolars were decoronated and randomly divided into 6 groups (n = 16), as follows: sound (S), untreated canals; prepared teeth (P), canals only prepared to ProTaper Universal finishing instrument (F4); endodontically-treated (ET), prepared and obturated canals using the single-cone technique; and groups PTN, PTR, and HI where filling was removed using PTN, PTR, or HI respectively. FR under vertical loading; MoF and time were assessed. Data were analyzed (Significance level [α] = 0.05).
-
Results
There was a significant difference in FR among all groups (p < 0.001) (HI < P < PTN < S < ET < PTR). HI showed lower FR than S, ET and PTR, and P showed lower FR than PTR (p < 0.05). For experimental groups, there was a significant difference between every group pair (p < 0.05) No significant difference was found regarding MoF distribution (p > 0.05). HI required the highest filling removal time, while PTR required the least (p < 0.05 between every group pair).
-
Conclusions
The effect of filling removal on FR may depend on the filling removal technique/system used. PTR could be faster and protect against fracture followed by PTN; HI could adversely affect FR. FR may be associated with filling removal time.
-
Keywords: Fracture; Instrumentation; Manual; Retreatment; Root canal preparation
INTRODUCTION
Root fracture is one of the most common reasons for the extraction of endodontically-treated (ET) teeth [
1]. According to the American Association of Endodontists, vertical root fracture (VRF) is defined as a fracture in the root whereby the fractured segments are incompletely separated; it may occur buccolingually or mesiodistally [
2]. It can be complete or incomplete starting at any level of the root of a given tooth, usually in a buccolingual (BL) direction [
3]. Following endodontic therapy, VRF is one complication with the poor prognosis being one of the main reasons for extraction, where its prevalence in extracted ET ranges from 4.3% to 25.3% [
1,
4,
5,
6,
7,
8].
VRF is a time-dependent, cumulative, multifactorial phenomenon with factors being either predisposing (non-iatrogenic) or contributory (iatrogenic) [
7,
9]. Dentine loss has been designated as the primary iatrogenic cause for fracture of ET, and root canal and root anatomy as primary non-iatrogenic causes. Iatrogenic induction of microcracks was designated as a secondary iatrogenic cause; this makes prevention challenging [
4,
9,
10].
On endodontic failure, non-surgical retreatment, which involves filling removal followed by cleaning, shaping, and re-obturation, is usually the preferred treatment option [
11,
12,
13,
14]. Given the probability of more dentin loss and possibly more microcracks, endodontic retreatment can have more unfavorable effects on tooth fracture resistance (FR) than primary treatment; this has been clinically detectable where a tooth subjected to endodontic retreatment has an 8-to-12-fold higher risk of developing a VRF than a tooth with primary treatment [
4,
11,
15].
Several methods have been used for root canal filling removal including physical (heat, laser), chemical and mechanical methods; the latter are the most commonly used through using manual, rotary, and/or reciprocating instruments [
11,
12,
16,
17]. The main advantage of using engine-driven instruments is the easier and faster removal [
12,
13,
18]. Various NiTi rotary system brands, designed specifically for retreatment procedures, are available. ProTaper Universal retreatment system (PTR; Dentsply Maillefer, Ballaigues, Switzerland), is one of the most commonly used NiTi retreatment systems which has 3 files with different lengths and progressively-increasing tapers [
11,
14,
16,
19].
So far, various instruments/systems initially designed for initial root canal preparation, became used to remove filling materials [
13,
16,
18,
19]. One of these systems is ProTaper Next (PTN; Dentsply Maillefer), an ‘off-centered’ file system of 5 instruments with variable tapers intended to reduce the torsional stress on the instrument; such design facilitates the removal of debris and filling with little apically-extruded debris [
12,
13,
16,
20]. To date, there is only limited
ex vivo evidence suggesting an adverse effect of filling removal on the FR of roots; the low number of studies combined with their heterogeneity implicated the need for more coherent laboratory studies to support or refute such conclusions [
15]. Several studies have assessed the effect of filling removal on the FR of teeth, of which few made direct, head-to-head comparisons among different retreatment techniques/systems, with fewer comparing the hand/hybrid instrumentation with PTR, and none investigating the effect of canal-preparation systems used for filling removal,
e.g. PTN, in comparison [
14,
17,
21,
22,
23,
24,
25]. The aim of this study, thus, was to assess the effect of retreatment on the FR of ET, and to compare the effect of PTN, PTR and hybrid instrumentation (HI) regarding FR, mode of failure (MoF) and filling removal time. The null hypotheses were that: first, there is no adverse effect of filling removal on FR and MoF of roots, and, second, there is no difference among the different used filling-removal techniques on the same outcomes.
MATERIALS AND METHODS
The protocol of this ex vivo study was submitted to and approved by the Research Ethics Committee, Faculty of Dentistry, Cairo University; the approval number is (19-9-10).
Sample size calculation
Based on the study by Yiğit
et al. [
14], the mean and standard deviation of the FR in the control retreatment group was 718.2 ± 58.23 Newtons (N). The sample size was calculated with an alpha (α) level of 0.05 (5%), a power of 80%, and an estimated mean difference of 25 N of mean FR where a minimum of 15 specimens were required per experimental or control group.
Ninety-six, single-rooted, single-canalled mandibular premolars, freshly extracted due to orthodontic or periodontal problems, were collected. Included premolars had straight canals (< 10° according to Schneider’s technique), mature root apices, and lengths between 18–21 mm; those with calcified canals, root cracks, fractures, resorption and/or decay were excluded. Pre-operative radiographs were taken to confirm patency. Mesiodistal (MD) and BL dimensions of the root at the level of cementoenamel junction were measured using a digital caliper [
26].
Teeth surfaces were thoroughly washed and carefully cleaned using scalers. Teeth were disinfected in 5.25% sodium hypochlorite (NaOCl; Clorox, Household cleaning products of Egypt, Cairo, Egypt) for 30 minutes then stored in distilled water and then stored in saline until use. Specimens were horizontally decoronated using a diamond disc (Abrasive technology, Lewis Center, Ohio, Canada), under copious coolant to obtain standardized root lengths of 14 mm (± 1 mm) [
6,
17,
25].
Canals were checked for patency using #10 K-file size (Mani, Inc., Tochigi, Japan) then 1mm was subtracted to determine the working length. Canals were prepared using ProTaper Universal rotary Instruments (PTU; Dentsply Maillefer) mounted in an endodontic motor (E-cube endo, SAESHIN, Daegu, Korea) at a speed of 300 rpm and torque of 2 N.cm up to finishing file F4 (#40/0.06) according to manufacturer’s instructions [
25]. Each file was used for 5 canals.
Irrigation was done using 2 mL 2.6% NaOCl between every 2 successive instruments using 30-gauge, side-vented needles. Final irrigation was done using 5 mL of 2.6% NaOCl followed by 5 mL of 17% ethylenediaminetetraacetic acid (META BIOMED CO.LTD, Cheongju, Korea) for 1 minute then a final flush using 10 mL of distilled water. Size-matched paper points were used for canal dryness, then obturation was done using the single-cone (SC) technique with size-matched gutta-percha cones and epoxy-resin sealer (AH-Plus sealer, Dentsply Detrey GmbH, Konstanz, Germany). The excess filling was removed, and the canal orifice was sealed using temporary filling (Coltosol F, Coltene, Germany). Specimens were stored at 100% humidity and 37°C for 1 month to ensure a complete sealer setting.
Randomization and blinding
A sequence generation was performed using a computer random-sequence generator (
https://www.random.org). The allocated sequence was concealed using numbered, opaque, sealed containers. Randomization was performed by an investigator not involved in the endodontic procedures. The study was assessor- and statistician-blinded.
A drop of solvent (Endosolv R; SeptoDent, Cedex, France) was introduced into the canal orifice for one minute to help facilitate penetration into the filling [
21]. Ninety-six specimens were randomly divided into 6 groups (
n = 16), 3 control and 3 experimental, as follows: group sound (S), had sound teeth in which canals received no instrumentation; group prepared teeth (P), where canals were only prepared by PTU without obturation; group (ET), where canals were prepared then obturated simulating ET teeth; group (PTN), where filling of obturated canals was removed using PTN so that instruments were used at a speed of 300 rpm and torque of 2 N.cm in continuous rotation using X2 through to X5 to the full WL in a brushing motion according to manufacturer’s instructions; group (PTR), where filling was removed using PTR according to the manufacturer’s instructions so that instruments were used at a speed of 500 rpm and torque 2 N.cm [
32]. D1 was inserted in the canal followed by D2 to remove canal filling from the coronal and middle thirds, then D3 was used at the apical third in a brushing action reaching the full WL. Additional preparation was done by PTU rotary instruments till F5 (#50/0.05); and, finally, group (HI), where filling was removed by hybrid instrumentation using Gates-Glidden (GG) burs #2 and #3 and H-files #15 through to #50 to the full WL in a circumferential, quarter-turn, push-pull motion [
14]. Filling removal was considered completed when no filling debris was observed between the flutes of the file, the final irrigant appeared clear, and the canal walls felt smooth [
16,
17,
19].
For experimental groups, each instrument was used to remove root canal filling material from 5 root canals and irrigation was done as previously described for initial canal preparation. All specimens were re-obturated by the SC technique and were stored at 100% humidity and 37°C for 1 week. All endodontic procedures were done by a single, trained operator [
6,
14,
17].
The total filling removal time (T
tot) was recorded from introducing the first instrument into the canal until the removal of the last instrument from the canal. A stopwatch was used to record the time required for root canal filling removal where T
1 was the time to reach the WL, and T
2 was the time to complete filling removal. T
tot is the sum of both T
1 and T
2; the time needed for changing instruments and irrigating solutions was excluded [
11,
13].
To simulate the bony socket, specimens were vertically embedded in self-cured acrylic resin in prefabricated plastic molds (16 mm in diameter and 26 mm in height) to a level of 2 mm apical to the coronal end of the specimen [
17]. For periodontal ligament simulation, roots were dipped in blue molten wax to achieve a 0.2-0.3 mm coating, leaving 2 mm apical to the coronal end of the specimen before embedding [
26,
27]. After polymerization started, roots were removed from the resin and the wax was eliminated using a warm water bath, then sockets were filled with condensation silicone impression, roots were re-inserted and excess material was removed by a scalpel.
Acrylic blocks were mounted in the lower jig of the Universal Testing Machine Model 334 (Instron, Wycombe, UK). A spherical tip (5 mm in diameter) attached to the upper jig of the machine contacted the circumference of the orifice of each specimen contacting the flat root face on both mesial and distal sides to evenly distribute the load on the root surface, as an antagonistic tooth [
1,
28]. Continuous, static, vertical compressive loading along the long axis of the root was applied at a loading rate of 1 mm/min until fracture. The force at which the fracture occurred was recorded in N. Fracture was defined as the point at which a sharp, instantaneous drop in load. A computer software (BlueHill Universal, Instron) attached to the machine recorded and verified the force.
After FR testing, the root surfaces were inspected for fracture lines using a stereomicroscope up to 70X magnification (MA 100 NIKON, Tokyo, Japan). The failure mode of each specimen was assessed according to classifications by Al-Hiyasat
et al. [
26] and Lin
et al. [
1] Failure mode was either a split vertical fracture that goes along the long axis of the root or a comminuted fracture that shatters the root into more than 2 fragments [
26]. Failure mode was, also, scored as follows: type 1: complete crack extends across the root dentine surface; type 2: incomplete crack extends from the outer root dentine surface on one side to approximately half on the other side; type 3: incomplete crack extends to half of the root dentin surface on one side only; type 4: incomplete crack confines to the inner root dentine surface without reaching external surface [
1]. Fracture-line(s) direction at the coronal root surface was classified as BL, MD or compound, a combination of both as in comminuted or/and oblique fractures [
1,
3]. All images were presented as a Microsoft Office PowerPoint presentation and displayed in slide format on an liquid-crystal display monitor. Two blinded, calibrated observers assessed the patterns of failure independently; disagreements were resolved by discussion.
Descriptive statistics were calculated for each group. Data were explored for normality using Kolmogorov-Smirnov and Shapiro-Wilk tests. Normally distributed data were analyzed using 1-way analysis of variance (ANOVA), followed by a Tukey post hoc test for pair-wise comparisons. Categorical data were analyzed using χ2 test and Fisher’s exact test whenever applicable. An interobserver agreement analysis using the Intraclass correlation coefficient was performed to determine consistency among observers regarding the evaluation of the MoF. Pearson’s coefficient was calculated to correlate numerical variables. The significance level was set at α = 0.05. Statistical analysis was performed using IBM SPSS statistics version 20.0 for Windows (SPSS Inc., IBM Corporation, Armonk, NY, USA).
RESULTS
Data of the MD and BL dimensions are summarized in
Table 1. One-way ANOVA showed no significant difference among groups regarding MD (
p = 0.109) or BL dimensions (
p = 0.305).
Table 1 The mean ± standard deviation (SD), minimum (Min) and maximum (Max) values of the mesiodistal (MD) and buccolingual (BL) dimensions of the different groups
|
Groups |
MD |
BL |
|
Mean ± SD |
Min–Max |
Mean ± SD |
Min–Max |
|
Group (PTN) |
5.09a ± 0.29 |
4.48–5.52 |
7.08a ± 0.28 |
6.68–7.78 |
|
Group (HI) |
5.12a ± 0.29 |
4.60–5.67 |
6.92a ± 0.48 |
6.14–7.80 |
|
Group (PTR) |
4.87a ± 0.30 |
4.05–5.16 |
6.87a ± 0.39 |
6.21–7.64 |
|
Group (ET) |
5.05a ± 0.31 |
4.56–5.56 |
7.11a ± 0.37 |
6.54–7.73 |
|
Group (S) |
5.09a ± 0.34 |
4.35–5.68 |
7.14a ± 0.43 |
6.40–7.73 |
|
Group (P) |
4.89a ± 0.40 |
4.19–5.43 |
6.99a ± 0.37 |
6.45–7.56 |
|
p value |
0.190 |
0.305 |
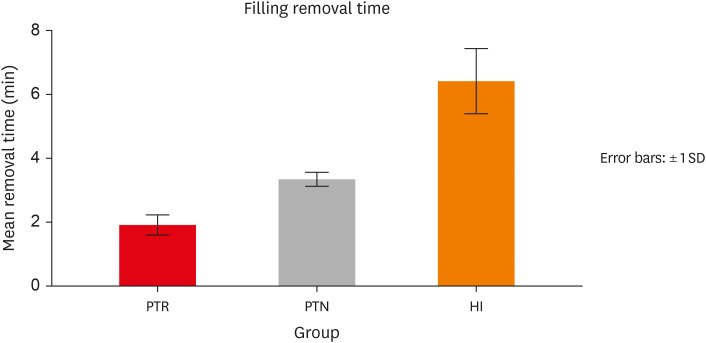
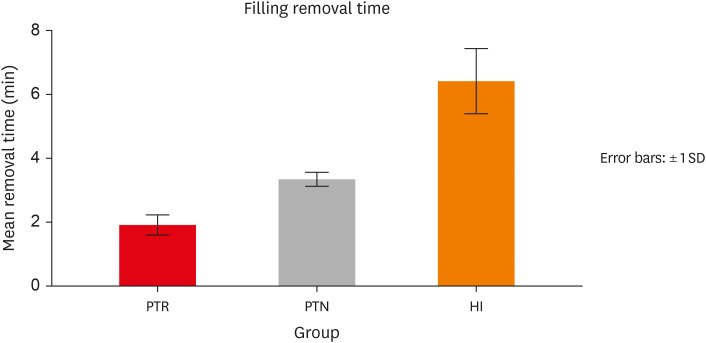
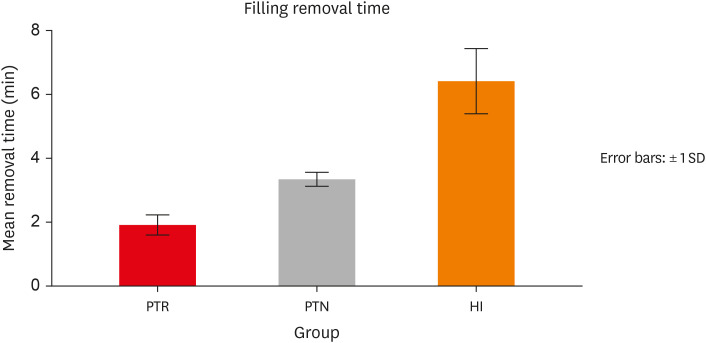
Data of the filling removal time are presented in
Table 2 and
Figure 1. One-way ANOVA test showed a significant difference among groups for T
1, T
2, and T
tot (
p < 0.05). Tukey
post hoc test revealed a significant difference between every group pair (
p = 0.000) where group PTR showed the shortest time, while group HI showed the longest time.
Table 2 The mean ± standard deviation (SD), minimum (Min) and maximum (Max) values of filling removal time (minutes) of the experimental groups till reach working length (T1), to complete filling removal (T2) and the total time (Ttot)
|
Groups |
T1
|
T2
|
Ttot
|
|
Mean ± SD |
Min–Max |
Mean ± SD |
Min–Max |
Mean ± SD |
Min–Max |
|
Group (PTN) |
2.30b ± 0.24 |
1.87–3.00 |
1.04b ± 0.14 |
0.83–1.33 |
3.34b ± 0.22 |
3.03–3.83 |
|
Group (PTR) |
1.30c ± 0.26 |
0.90–1.80 |
0.60c ± 0.08 |
0.50–0.73 |
1.92c ± 0.31 |
1.43–2.53 |
|
Group (HI) |
4.74a ± 1.04 |
3.00–6.53 |
1.67a ± 0.41 |
1.00–2.35 |
6.41a ± 1.01 |
4.40–7.53 |
|
p value |
< 0.001*
|
< 0.001*
|
< 0.001*
|
Figure 1
Filling removal time for experimental groups.
PTN, ProTaper Next; HI, hybrid instrumentation; PTR, ProTaper Universal retreatment.
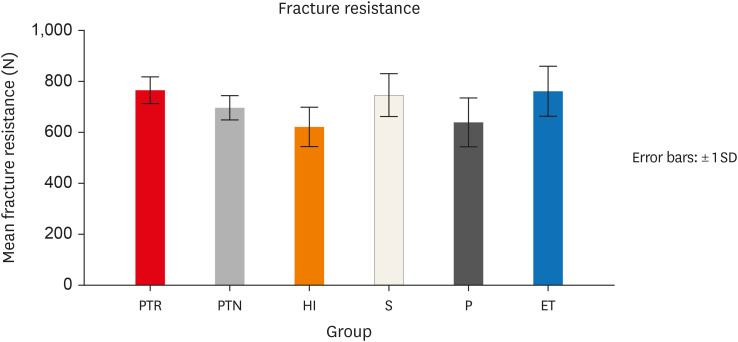
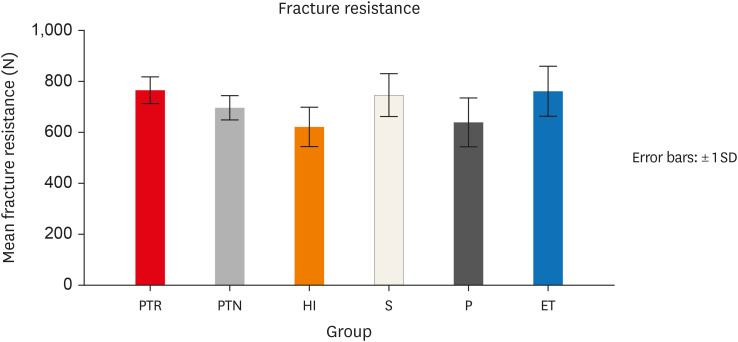
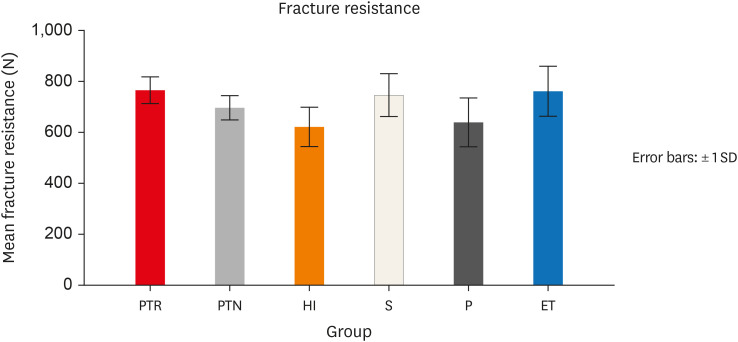
Data of the FR are presented in
Table 3 and
Figure 2. One-way ANOVA test showed a significant difference among all groups (
p < 0.001). Tukey
post hoc test revealed a significant difference between group HI and each of the ET and S groups as well as between PTR and P groups (
p = 0.000). Considering the experimental groups only, one-way ANOVA test showed a significant difference among groups (
p < 0.001). Tukey
post hoc test revealed a significant difference between every group pair (
p < 0.05) where group PTR showed the highest resistance, while group HI showed the least resistance.
Table 3 The mean ± standard deviation (SD), minimum (Min) and maximum (Max) values of fracture resistance of the different groups
|
Groups |
Fracture resistance |
|
Mean ± SD |
Min–Max |
|
Group (PTN) |
696.81abB ± 47.69 |
605.46–762.57 |
|
Group (HI) |
621.92bC ± 76.74 |
511.88–783.06 |
|
Group (PTR) |
766.42aA ± 52.22 |
696.28–873.56 |
|
Group (ET) |
762.39a ± 97.77 |
614.17–898.87 |
|
Group (S) |
747.08a ± 83.94 |
599.20–872.10 |
|
Group (P) |
640.56b ± 95.59 |
444.14–790.88 |
|
p value |
< 0.001*
|
Figure 2
Fracture resistance for different groups.
PTN, ProTaper Next; HI, hybrid instrumentation; PTR, ProTaper Universal; ET, endodontically treated; S, sound; P, prepared teeth.
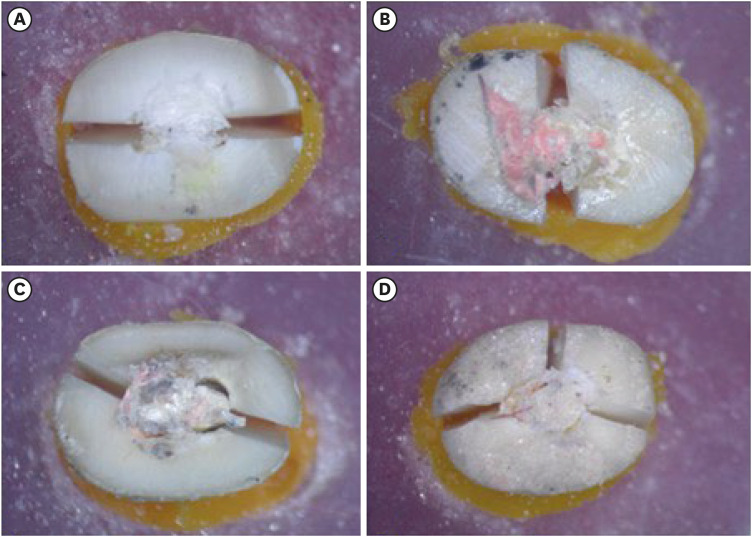
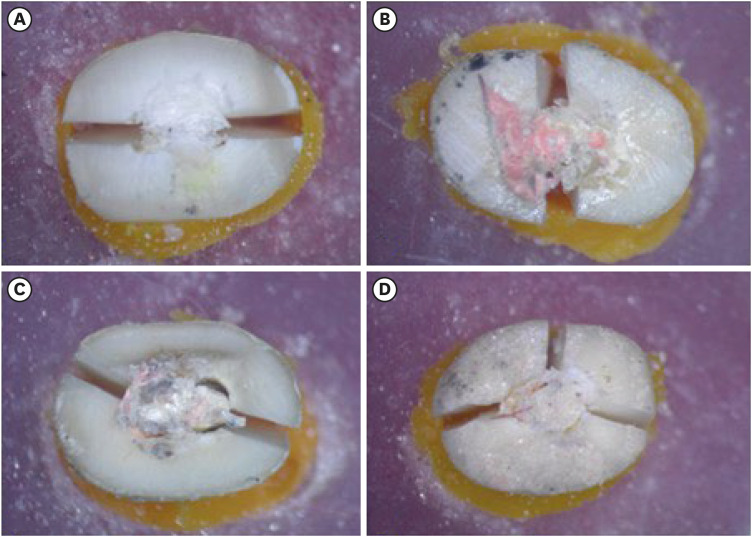
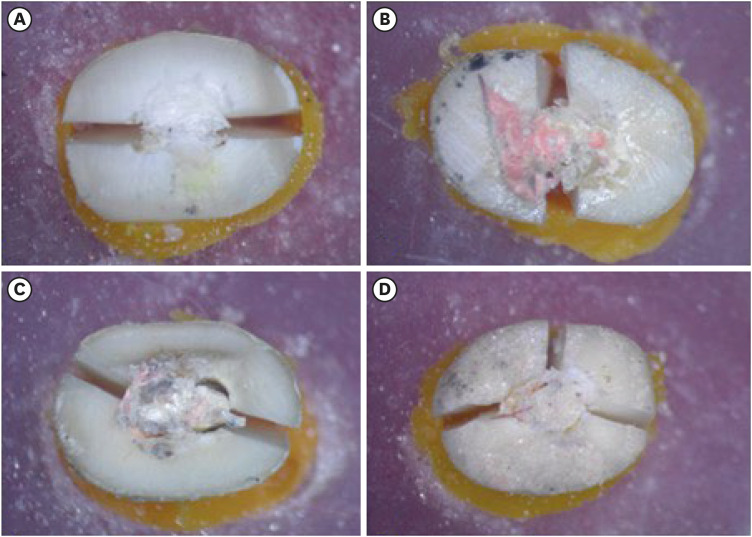
Failure mode findings are presented in
Table 4. There was no difference among groups regarding the failure mode according to both classifications (
p > 0.05). Regardless of groups, 48 of 96 (50%) of the specimens showed split vertical fracture mode and 50% showed comminuted fracture mode. Overall, the direction of the fracture line was combined in most specimens (59.4%) followed by the BL direction (36.5%) and then the MD direction (4.1%). Representative specimens of the modes of failure and their directions are presented in
Figure 3. Type 1 crack propagation was the most frequent (92 out of 96 [95.8%];
Table 4) which is considered the most catastrophic. The interobserver agreement was κ = 0.94 (
p < 0.001), 95% confidence interval (0.87–1.00) indicating almost perfect agreement [
29].
Table 4 The values of types of failure modes according to Al-Hiyasat et al. [26] and Lin et al. [1] classifications of the different groups
|
Groups |
Al-Hiyasat et al. (2021) |
Lin et al. (2022) |
|
Type |
Values |
Type |
Values |
|
Group (PTN) |
Split |
7 (43.80) |
Type 1 |
16 (100.00) |
|
Comminuted |
9 (56.30) |
Type 2 |
0 (00.00) |
|
|
Type 3 |
0 (00.00) |
|
|
Type 4 |
0 (00.00) |
|
Group (HI) |
Split |
7 (43.80) |
Type 1 |
15 (93.80) |
|
Comminuted |
9 (56.30) |
Type 2 |
0 (00.00) |
|
|
Type 3 |
1 (6.30) |
|
|
Type 4 |
0 (00.00) |
|
Group (PTR) |
Split |
7 (43.80) |
Type 1 |
15 (93.80) |
|
Comminuted |
9 (56.30) |
Type 2 |
0 (00.00) |
|
|
Type 3 |
1 (6.30) |
|
|
Type 4 |
0 (00.00) |
|
Group (ET) |
Split |
11 (31.30) |
Type 1 |
16 (100.00) |
|
Comminuted |
5 (68.80) |
Type 2 |
0 (00.00) |
|
|
Type 3 |
0 (00.00) |
|
|
Type 4 |
0 (00.00) |
|
Group (S) |
Split |
8 (50.00) |
Type 1 |
15 (93.80) |
|
Comminuted |
8 (50.00) |
Type 2 |
0 (00.00) |
|
|
Type 3 |
1 (6.30) |
|
|
Type 4 |
0 (00.00) |
|
Group (P) |
Split |
8 (50.00) |
Type 1 |
15 (93.80) |
|
Comminuted |
8 (50.00) |
Type 2 |
0 (00.00) |
|
|
Type 3 |
1 (6.30) |
|
|
Type 4 |
0 (00.00) |
|
p value |
0.912 |
0.840 |
Figure 3 Representative specimens of the modes of failure according to Al-Hiyasat et al. [26] and their directions after fracture testing. (A) Split buccolingual fracture; (B) split mesiodistal fracture; (C) split oblique fracture (compound direction); and (D) comminuted fracture (compound direction).
FR was moderately inversely correlated to each of the filling removal times (p < 0.001, r = −0.616) and fairly inversely correlated MD dimension of the specimen (p = 0.024, r = −0.326), but it was not significantly correlated with BL dimension (p = 0.691, r = −0.059).
DISCUSSION
Dentin loss is a primary iatrogenic risk factor and dentinal defects are secondary ones for VRF; both are more pronounced in endodontic retreatment than in primary treatment making their effects more likely clinically detectable [
4,
9]. If the efficacy of filling removal is similar across different techniques/systems then other factors
e.g., removal time, cost and/or FR become more relevant for clinical decision-making [
20]. A recent systematic review and meta-analysis of
ex vivo studies have highlighted the need for more laboratory studies to ascertain such effects and compare different systems [
14,
15,
21,
22,
24]. Only 2 studies have compared hand or hybrid instrumentation with PTR on FR, yet, none have investigated the effects of canal-preparation systems used for filling removal,
e.g. PTN, in comparison [
14,
21].
Canal instrumentation significantly increases the risk of fracture of mandibular premolars compared to other single-rooted teeth, possibly due to the much narrower MD compared to the BL dimension [
3,
4]. Mandibular second premolars were among the most commonly extracted teeth for VRF, and the most commonly used in FR studies [
3,
15]. Their root length shows little variation, so is less likely to confound results [
5].
In the present study, standardization of the specimens and conditions was sought to enhance study validity. Randomization was done to minimize confounding. A single operator performed all the endodontic procedures [
8,
11]. SC technique has minimal effect on initiating or propagating dentinal defects and can be less likely to adversely affect root strength; thus, it was used [
1,
6,
11,
30,
31].
The use of solvent during canal filling removal can be controversial. Some studies use it to facilitate screwing in of NiTi instruments, and reduce instrument separation, apically-extruded debris and retreatment time; however, it may affect the cleanliness of root canal [
11,
18]. It is, nevertheless, regarded as a matter of personal preference and still frequently used by clinicians [
32,
33]. Most studies assessing the effect of filling removal on FR used solvents [
15,
21,
22,
23,
24]. In this study, EndoSolv R, a solvent particularly effective for the removal of resin-based sealers, has been used [
11]. In retreatment procedures, the final apical size should generally be larger than that of initial preparation to reduce residual filling materials [
11,
14,
16,
19,
20].
In the present study, an artificial socket model was used to mimic the cushioning effect of the healthy teeth attachment regarding the stress distribution [
1,
11,
21,
26,
27].
There are 2 types of loading on testing FR: the static and the dynamic [
34]. Static-loading tests are ‘destructive’ where teeth are fractured above the maximum physiological bite force, thus, more relevant to failures caused by accidentally high forces. Dynamic-loading tests simulate better the mastication forces, however, are rarely used in endodontic experiments as take a long duration and might not affect results [
25,
34,
35]. Despite their limitations, laboratory models are necessary for the development and testing of new restorative modalities as well as for understanding failure mechanisms and confounding variables [
5,
11,
15,
34,
36]. Most previous retreatment studies, however, have used the static approach [
15,
17,
22,
23,
24]. In the present study, a static-loading test allows comparison across studies.
When extracted teeth are used, factors such as MD and BL widths and lengths should be standardized [
11,
28]. In the present study, similar MD and BL dimensions were obtained for all groups indicating proper randomization and helping minimize the allocation bias.
The simplest way to determine the ease of removal is by measuring the filling removal time [
11]. Removal time findings in this study were in accordance with most literature where hand/HI instrumentation takes longer than NiTi rotary instrumentation [
12,
13,
18,
20,
32,
37,
38]. Such difference could have been accentuated in this study due to the use SC obturation technique with an adhesive sealer in oval canals where a large amount of sealer is expected making it more difficult to remove with the less-aggressive movements of hand files; increased removal time could affect the number of cracks in canal dentin as well [
11,
31,
39].
In this study, PTR revealed faster filling removal than PTN; this was in accordance with 1 study, and in disagreement with others where PTN was faster or both were similar [
12,
13,
16,
37,
38]. Differences could be attributed to differences in canal size and curvature, and/or the speed used for PTR. Two studies have assessed the 3 techniques in this study showing partial agreement with this study where both showed shorter time with rotary NiTi systems than hand/hybrid instrumentation; PTR, however, showed longer removal time than PTN in 1 study, yet both systems showed similar results in the other [
12,
38]. One study used PTR in mandibular premolars at the speed of 300 rpm and 3 N.cm, while the other used curved mesial canals of mandibular molars [
12,
38]. The difference in design features, cutting efficiency and activation parameters could explain the results [
20]. The more rigid alloy, D1’s active tip and convex triangular cross-section in PTR, with sharper blade angles than the rectangular cross-section in PTN, could explain the results [
13,
19].
In this study, canal preparation with the ProTaper Universal system (P group) adversely affected root FR compared to S roots (S group); the latter showed similar FR to ET roots (ET group). This agreed with previous studies, yet, partially agreed with others [
6,
17,
24,
25,
28,
40]. Some of these studies showed less FR for ET compared to S and some showed similar FR for ET and P [
6,
17,
40]. Differences could be attributed to tooth type, obturation technique, sealer type and/or methodological differences. The adverse effect of canal preparation could be attributed to the loss of radicular dentin and increased dentinal defects [
6,
9,
28]. A similar FR of ET and S could be attributed to the reinforcing effect of epoxy-resin sealers [
8,
24,
25,
28]. When using an adhesive obturation technique, particularly if in a corporation with an adhesive-based restorative approach, any critical defect could possibly be filled up [
8,
15]. AH Plus sealer has desired properties,
e.g. formation of a covalent bond between the open epoxide ring and exposed amino acids in the collagen, excellent penetration ability into the surface micro-irregularities which could provide micromechanical retention, long-term dimensional stability, low solubility and greater film thickness than other sealers; all such properties, in addition to expected thick layers of sealers on using SC technique in oval canals, can explain its reinforcing capabilities [
6,
8,
11,
39,
40].
Both PTR and PTN showed similar FR to ET and S groups, whereas only PTR showed higher FR than the P group. These findings agreed with some studies, yet, disagreed with others [
14,
15,
17,
21,
22,
23,
24,
25]. Differences in findings could be attributed to differences in tooth types, endodontic procedural steps and/or methodological differences. Some studies have used incisors and canines, while others used mandibular premolars [
14,
17,
22,
23,
24]. Some studies used cold lateral compaction technique (CLC) for initial obturation, while others used warm vertical compaction (WVC); in the present study, the SC technique was used [
14,
17,
22,
23,
24]. In some studies, no additional preparation was done after filling removal, while additional preparation was done using 2 sizes larger than the initial preparation in others; in the present study, additional preparation was one size larger [
17,
22,
24]. PDL simulation was done in the present study, but it was not done in others [
17,
23,
24]. For some studies, vertical loading was done using a cone tip or a tip with a smaller diameter,
e.g. 2 mm, than the tip used in this study; such differences could lead to differences in the type and amount of stresses induced within roots [
14,
17]. The findings of this study could be attributed to the sealer’s reinforcing effects and the SC obturation technique which could induce fewer microcracks compared to CLC and WVC [
6,
7,
8,
30,
31,
40].
An adverse effect of HI on FR was reported in this study compared to the S and ET groups. These findings agreed with a previous study where HI showed less resistance than ET, yet, disagreed with another where HI and ET were similar [
14,
21]. The differences in the rigidity, design, rotational speed, and number of the instruments used with HI compared to the NiTi instruments could explain such effects [
41,
42]. The use of GG burs may have significantly contributed to these findings due to their possible effects on dentin loss, particularly in teeth with thinner proximal walls
e.g. mandibular premolars, dentinal-defects initiation as well as the final longitudinal canal configuration which is hourglass in shape with GG burs compared to the continuously tapered format with NiTi instruments; the hourglass format may not enable uniform load distribution along the root canal walls [
42].
Comparing filling removal techniques only, PTR showed higher FR than PTN which showed higher FR than HI in this study. These findings disagree with previous studies that reported similar FR with PTR and HI on filling removal in maxillary anterior teeth and mandibular premolars; no previous study within the authors’ search scope has, yet, assessed PTN’s effect on FR on filling removal [
14,
21]. Differences could be attributed to differences in tooth types, initial preparation size, obturation technique, the use of solvent, the presence or absence of additional preparations as well as methodological differences
e.g. the tip used for load application [
14,
21]. In the present study, the difference in the FR among the experimental groups could be explained by differences in rotational speed, design and alloys of instruments, and the specific protocol for each technique which can affect filling removal time, the amount of dentin removed and the incidence of defects [
31,
41]. In this study, there was an inverse correlation between FR and filling removal time where the longer time, the less FR.
In the present study, the overall MoF was equally distributed between split and comminuted fracture patterns where the direction of the fracture line was compound in most specimens followed by the BL direction and then the MD direction. These findings partially agreed with 1 study, yet, disagreed with other studies [
1,
14,
43]. Yiğit
et al. [
14] reported 55.6% overall incidence of comminuted fracture and 44.4% of split fracture in maxillary anterior teeth; the direction of the fracture line(s) was compound in most specimens (55.6%) followed by BL (37.8%) then MD (6.6%). Tavanafar
et al. [
43] and Lin
et al. [
1] reported a majority of BL fractures (80% and 62.5% respectively) followed by MD fractures (17.5% and 31.25% respectively), then compound fractures (2.5% and 6.25% respectively). Differences could be attributed to variations in tooth type and chronological age, the existence of the butterfly effect, the type of intervention tested, the obturation technique as well as methodological differences [
44].
Most VRFs occur in root-filled teeth and usually run buccolingually [
1,
3,
5,
7,
44]. The direction of fracture line in VRF is associated with several factors including the occurrence of the butterfly effect as well as anatomical factors,
e.g., canal shape, root shape, and dentin thickness [
5,
14,
36,
44]. The butterfly effect is an optical phenomenon that occurs in some transverse cross-sections of root canals attributed to dentinal tubular sclerosis that differs in the MD and BL directions producing a characteristic butterfly shape caused by different shades of dentin observed in teeth from all age groups and at all levels making teeth more prone to have cracks at a BL rather than a MD direction which is associated with harder, more brittle sclerotic dentin [
1,
5,
36,
44]. In this study, the majority of fractures showed a compound direction. The prevalence of the butterfly effect in lower premolars can reach an average value of 40.28% and variations in prevalence have been attributed to the patient’s tooth age, patient’s ethnic origin, degree of dentine sclerosis and the tubule density; the butterfly effect may be more likely in the apical than the coronal thirds [
5]. Taken together and given that the load application in this
ex vivo study occurred on the coronal root face, it can be justifiable that the fracture line may not be predominantly BL. A clinical study has shown that only 57.4% of the VRFs that occurred cervically were BL in orientation [
10]. A recent study has, also, shown that compound fractures were observed in both young and older teeth when there is either the absence of sclerotic dentin or the presence of complete sclerosis implying dissipation of forces rather than their BL concentration [
36].
This study, however, has some limitations. The age of the patients from which the teeth were obtained is unknown; this could limit the ability to correlate the FR values with age which could be a point of interest for future research. Randomization, however, can allow balancing known (
e.g. root BL and MD dimensions) as well as unknown confounders (
e.g. Patients’ age, degree of sclerosis) across groups [
11,
25]. The use of mandibular premolars could limit generalizing the results to other tooth types, thus, future studies are required using different tooth types and root configurations. The use of cyclic-fatigue tests could provide findings that better match clinical conditions, yet static-loading tests still provide a valid tool for comparative purposes [
5,
36]. On the other hand, sample-size calculation and randomization can be considered among this study’s strengths to provide a sufficiently powered sample and minimize selection bias respectively.
CONCLUSIONS
Within the conditions of the present study, it could be concluded that the use of PTR for root canal filling removal could protect against VRF followed by PTN after SC obturation with an epoxy-resin sealer in mandibular premolars; HI, on the other hand, may adversely affect the FR of mandibular premolar roots. FR may be associated with filling removal time.
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Hanafy HH, Amin SAW.
Formal analysis: Hanafy HH, Bedier MM, Amin SAW.
Funding acquisition: Hanafy HH.
Investigation: Hanafy HH, Bedier MM, Amin SAW.
Methodology: Hanafy HH, Bedier MM, Amin SAW.
Resources: Hanafy HH, Bedier MM, Amin SAW.
Supervision: Bedier MM, Amin SAW.
Writing - original draft: Hanafy HH.
Writing - review & editing: Bedier MM, Amin SAW.
REFERENCES
- 1. Lin GSS, Singbal KP, Noorani TY, Penukonda R. Vertical root fracture resistance and dentinal crack formation of root canal-treated teeth instrumented with different nickel-titanium rotary systems: an in-vitro study. Odontology 2022;110:106-112.ArticlePubMedPDF
- 2. American Association of Endodontists (AAE). Glossary of endodontic terms (Tenth Edition). updated March, 2020]. cited May 24, 2024]. Available from: https://www.aae.org/specialty/clinical-resources/glossary-endodontic-terms.
- 3. von Arx T, Bosshardt D. Vertical root fractures of endodontically treated posterior teeth: a histologic analysis with clinical and radiographic correlates. Swiss Dent J 2017;127:14-23.ArticlePubMedPDF
- 4. García-Guerrero C, Mendoza-Beltrán W, Roldan-Roldan M, Villa-Machado P, Restrepo-Restrepo F. Vertical root fractures: a time-dependent clinical condition. A case-control study in two colombian populations. J Clin Exp Dent 2021;13:e1104-e1111.PubMedPMC
- 5. Sodvadiya UB, Bhat GS, Shetty A, Hegde MN, Shetty P. The “Butterfly Effect” and its correlation to the direction of the fracture line in root dentin. J Endod 2021;47:787-792.ArticlePubMed
- 6. Mandhane SA, Mattigatti S, Dsouza VV, Nahar S, Chauhan UB, Shah A. Evaluation of fracture resistance of mandibular premolar canals filled with four different obturation techniques: an in vitro study. J Clin Diagn Res 2021;15:ZC24-ZC28.
- 7. Patel S, Bhuva B, Bose R. Present status and future directions: vertical root fractures in root filled teeth. Int Endod J 2022;55(Supplement 3):804-826.ArticlePubMedPMCPDF
- 8. Uzunoglu-Özyürek E, Küçükkaya Eren S, Karahan S. Effect of root canal sealers on the fracture resistance of endodontically treated teeth: a systematic review of in vitro studies. Clin Oral Investig 2018;22:2475-2485.PubMed
- 9. Kishen A. Biomechanics of fractures in endodontically treated teeth. Endod Topics 2015;33:3-13.Article
- 10. Sugaya T, Nakatsuka M, Inoue K, Tanaka S, Miyaji H, Sakagami R, et al. Comparison of fracture sites and post lengths in longitudinal root fractures. J Endod 2015;41:159-163.ArticlePubMed
- 11. Ajina MA, Shah PK, Chong BS. Critical analysis of research methods and experimental models to study removal of root filling materials. Int Endod J 2022;55(Supplement 1):119-152.ArticlePubMedPDF
- 12. Dhanyakumar NM, Shivanna V, Sharma S.
Ex vivo evaluation of endodontic retreatment using four rotary file systems and hand Hedstrom files in the removal of gutta-percha and MTA-based salicylate resin sealer. CODS J Dent 2018;10:29-34.
- 13. Özlek E, Gündüz H. Effectiveness of different rotary file systems in removing the root canal filling material: a micro-computed tomography study. J Dent Res Dent Clin Dent Prospect 2021;15:273-278.ArticlePubMedPMCPDF
- 14. Yiğit DH, Yilmaz A, Saridağ S, Avcu E, Yildiran Y. Vertical fracture resistance of roots retreated using different instrumentation techniques. Turkish Endod J 2016;1:1-6.Article
- 15. Schestatsky R, Dartora G, Felberg R, Spazzin AO, Sarkis-Onofre R, Bacchi A, et al. Do endodontic retreatment techniques influence the fracture strength of endodontically treated teeth? A systematic review and meta-analysis. J Mech Behav Biomed Mater 2019;90:306-312.ArticlePubMed
- 16. Özyürek T, Demiryürek EÖ. Efficacy of different nickel-titanium instruments in removing gutta-percha during root canal retreatment. J Endod 2016;42:646-649.ArticlePubMed
- 17. Kamalak A, Uzun I, Arslan H, Keleş A, Doğanay E, Keskin C, et al. Fracture resistance of endodontically retreated roots after retreatment using self-adjusting file, passive ultrasonic irrigation, photon-induced photoacoustic streaming, or laser. Photomed Laser Surg 2016;34:467-472.ArticlePubMed
- 18. Rossi-Fedele G, Ahmed HMA. Assessment of root canal filling removal effectiveness using micro-computed tomography: a systematic review. J Endod 2017;43:520-526.ArticlePubMed
- 19. Delai D, Jardine AP, Mestieri LB, Boijink D, Fontanella VRC, Grecca FS, et al. Efficacy of a thermally treated single file compared with rotary systems in endodontic retreatment of curved canals: a micro-CT study. Clin Oral Investig 2019;23:1837-1844.ArticlePubMedPDF
- 20. Azevedo MAD, Silva TGD, Fernandes Â, Piasecki L, Fariniuk LF, Silva Neto UXD. Endodontic retreatment using a single instrument from four nickel-titanium systems - a micro-CT study. Braz Dent J 2020;31:605-610.ArticlePubMed
- 21. Aydemir S, Arukaslan G. Comparison of the fracture resistance of the roots retreated using different techniques with or without Guttasolv. Turkiye Klinikleri J Dent Sci 2018;24:169-174.Article
- 22. Er K, Tasdemir T, Siso SH, Celik D, Cora S. Fracture resistance of retreated roots using different retreatment systems. Eur J Dent 2011;5:387-392.ArticlePubMedPMC
- 23. Ganesh A, Venkateshbabu N, John A, Deenadhayalan G, Kandaswamy D. A comparative assessment of fracture resistance of endodontically treated and re-treated teeth: an in vitro study. J Conserv Dent 2014;17:61-64.ArticlePubMedPMC
- 24. Khalap ND, Hegde V, Kokate S. Fracture resistance exhibited by endodontically treated and retreated teeth shaped by ProTaper NEXT versus WaveOne: an in vitro study. J Conserv Dent 2015;18:453-456.ArticlePubMedPMC
- 25. Missau T, De Carlo Bello M, Michelon C, Mastella Lang P, Kalil Pereira G, Baldissara P, et al. Influence of endodontic treatment and retreatment on the fatigue failure load, number of cycles for failure, and survival rates of human canine teeth. J Endod 2017;43:2081-2087.PubMed
- 26. Al-Hiyasat AS, El-Farraj HS, Alebrahim MA. The effect of calcium hydroxide on dentine composition and root fracture resistance of human teeth: an in vitro study. Eur J Oral Sci 2021;129:e12798.PubMed
- 27. Soares CJ, Pizi ECG, Fonseca RB, Martins LRM. Influence of root embedment material and periodontal ligament simulation on fracture resistance tests. Braz Oral Res 2005;19:11-16.ArticlePubMed
- 28. Sagsen B, Er O, Kahraman Y, Akdogan G. Resistance to fracture of roots filled with three different techniques. Int Endod J 2007;40:31-35.ArticlePubMed
- 29. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159-174.ArticlePubMed
- 30. Aydinbelge HA, Azmaz NT, Yilmaz MO. Dentinal crack formation after different obturation techniques. Saudi J Oral Sci 2019;6:3-7.Article
- 31. Çapar ID, Saygili G, Ergun H, Gok T, Arslan H, Ertas H. Effects of root canal preparation, various filling techniques and retreatment after filling on vertical root fracture and crack formation. Dent Traumatol 2015;31:302-307.ArticlePubMed
- 32. Duncan HF, Chong BS. Removal of root filling materials. Endod Topics 2011;19:33-57.Article
- 33. Scardini IL, Sarra G, Braga MM, Dos Santos M, Freire LG. The effect of number of visits, use of solvent and gutta-percha removal technique on postoperative pain following nonsurgical endodontic retreatment; a systematic review and meta-analysis. Iran Endod J 2023;18:71-84.PubMedPMC
- 34. Ordinola-Zapata R, Lin F, Nagarkar S, Perdigão J. A critical analysis of research methods and experimental models to study the load capacity and clinical behaviour of the root filled teeth. Int Endod J 2022;55(Supplement 2):471-494.ArticlePubMedPMCPDF
- 35. Lin F, Ordinola-Zapata R, Xu H, Heo YC, Fok A. Laboratory simulation of longitudinally cracked teeth using the step-stress cyclic loading method. Int Endod J 2021;54:1638-1646.ArticlePubMedPMCPDF
- 36. Jaganathan V, Kumar R, Nawal RR, Talwar S. Comparison of dentin microstructure and its correlation to the direction of fracture line in mandibular molars of young and older individuals: in vitro study. J Endod 2023;49:1508-1513.PubMed
- 37. Obeid MF, Elgendy AA. Efficacy of three Ni-Ti rotary systems for removal of filling materials from root canal system of extracted teeth. Tanta Dent J 2015;12:259-264.Article
- 38. Özyürek T, Ozsezer-Demiryurek E. Efficacy of ProTaper Next and ProTaper Universal Retreatment systems in removing gutta-percha in curved root canals during root canal retreatment. J Istanb Univ Fac Dent 2017;51:7-13.PubMedPMC
- 39. De-Deus G, Santos GO, Monteiro IZ, Cavalcante DM, Simões-Carvalho M, Belladonna FG, et al. Micro-CT assessment of gap-containing areas along the gutta-percha-sealer interface in oval-shaped canals. Int Endod J 2022;55:795-807.ArticlePubMedPDF
- 40. Almohaimede A, Almanie D, Alaathy S, Almadi E. Fracture resistance of root filled with bioCeramic and epoxy resin-based sealers: in vitro study. Eur Endod J 2020;5:134-137.PubMedPMC
- 41. Arslan H, Karataş E, Çapar ID, Özsu D, Doğanay E. Effect of ProTaper Universal, Endoflare, Revo-S, HyFlex coronal flaring instruments, and Gates Glidden drills on crack formation. J Endod 2014;40:1681-1683.ArticlePubMed
- 42. Harandi A, Mohammadpour Maleki F, Moudi E, Ehsani M, Khafri S. CBCT assessment of root dentine removal by Gates-Glidden Drills and two engine-driven root preparation systems. Iran Endod J 2017;12:29-33.PubMedPMC
- 43. Tavanafar S, Karimpour A, Karimpour H, Mohammed Saleh A, Hamed Saeed M. Effect of different instrumentation techniques on vertical root fracture resistance of endodontically treated teeth. J Dent (Shiraz) 2015;16:50-55.PubMedPMC
- 44. Russell AA, Chandler NP, Friedlander LT. Crack formation following root-end preparation in roots with the butterfly effect. Eur Endod J 2018;3:107-112.ArticlePubMedPMC
 , Marwa Mahmoud Bedier
, Marwa Mahmoud Bedier , Suzan Abdul Wanees Amin
, Suzan Abdul Wanees Amin


 KACD
KACD
 ePub Link
ePub Link Cite
Cite

