Abstract
This case report introduces a straightforward, noninvasive approach for the esthetic rehabilitation of malformed anterior teeth in adolescents using direct composite restorations. The universal composite resin restorations are applied within a transparent 3-dimensionally printed rigid-resin index, which is individually customized from a digital wax-up. Compared to other methods, this technique streamlines the restoration process, significantly reducing chairside time while enhancing the predictability, accuracy, and patient acceptance of the aesthetic outcome.
-
Keywords: Adolescent; Case report; Computer aided design; Dental restoration; 3D printing
INTRODUCTION
Direct composite restorations are a mainstay in esthetic dentistry, serving as a cornerstone for addressing a range of anterior tooth imperfections [
1]. Beyond restoring carious lesions, direct composites are instrumental in treating crown fractures, hypoplasia, discoloration, and anomalies in tooth size and shape. They are particularly useful for augmenting the mesio-distal width of undersized teeth, especially in aesthetically conscious adolescent patients [
2]. This demographic presents unique challenges, including heightened esthetic expectations and the need for conservative treatment modalities to accommodate the growing nature of their teeth and jaws [
3]. While freehand composite application remains commonplace, achieving consistently predictable and satisfying esthetic outcomes can prove demanding, often relying heavily on the clinician’s artistry and experience.
This case report introduces a straightforward technique utilizing a custom 3-dimensionally (3D)-printed resin index to transfer digital wax-up designs directly to anterior teeth, enhancing predictability and simplifying the placement of direct composite restorations. The use of indices for replicating wax-up designs has been well-documented in various restorative applications. Studies have demonstrated their benefits in fabricating interim restorations, creating guides for tooth preparation, and aiding in the placement of fiber-reinforced composite prostheses [
4,
5,
6,
7,
8].
Existing techniques often employ silicone-based indices, ranging from the traditional palatal index to more recent innovations involving injectable composite resin and transparent silicone materials [
9,
10,
11,
12,
13,
14]. While these approaches offer certain advantages, they also present limitations. This report aims to address these limitations by utilizing a rigid, transparent resin index—fabricated using readily available digital technologies—for direct composite restorations in an adolescent patient with tooth shape and size anomalies.
CASE REPORT
A 16-year-old male adolescent with a noncontributory medical history presented to the educational dental clinic at Qassim University Dental Hospital. His dental history included a previous class V composite resin restoration in the maxillary right central incisor, an irregular tooth-brushing habit, and no history of dental trauma. His chief complaint was dissatisfaction with the esthetics of his maxillary anterior teeth and concern about the appearance of his smile.
Upon clinical examination, peg-shaped maxillary lateral incisors and malformed maxillary central incisors were observed. A midline diastema was present between the maxillary central incisors, along with noticeable spacing between the left central and lateral incisors. A deep cervical carious lesion was identified in the left maxillary lateral incisor (tooth #22). Additionally, hypocalcification was noted on the cervical areas of the anterior teeth. An occlusal analysis indicated Angle Class I, an overjet of 2 mm, a normal overbite of 3 mm, and a canine-guided occlusal scheme (
Figure 1).
Figure 1 Preoperative intraoral retracted view, displaying malformed central incisors and microdont lateral incisors with atypical ‘peg’ shape.

The patient and his parents expressed a desire to enhance the shape of his maxillary anterior teeth, close the spaces, and improve the esthetics of his smile using a conservative treatment modality. After considering various treatment options, the patient and the dental team decided on direct composite resin restorations (veneers) for the 4 anterior teeth, considering factors such as the patient’s age, financial treatment modifiers, and the patient’s request for a quick esthetic result. Written informed consent was obtained from the patient's legal guardian, and assent was obtained from the adolescent patient prior to treatment.
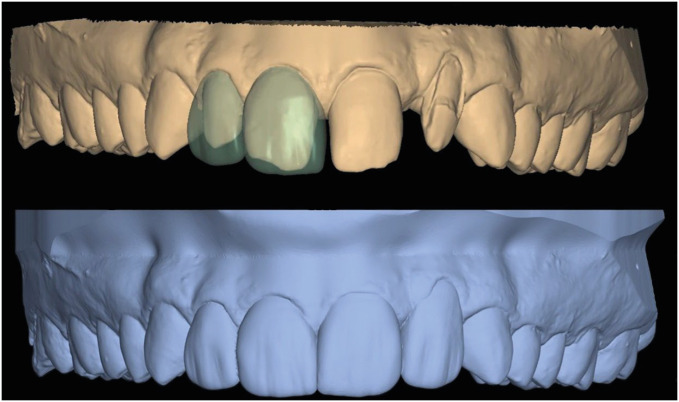
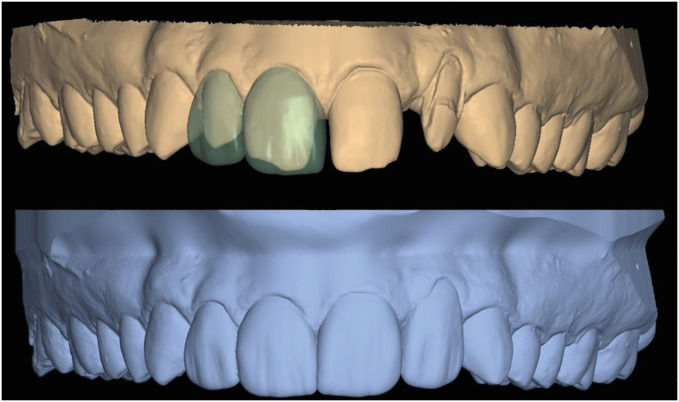
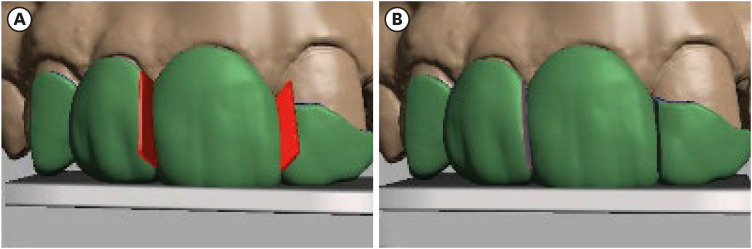
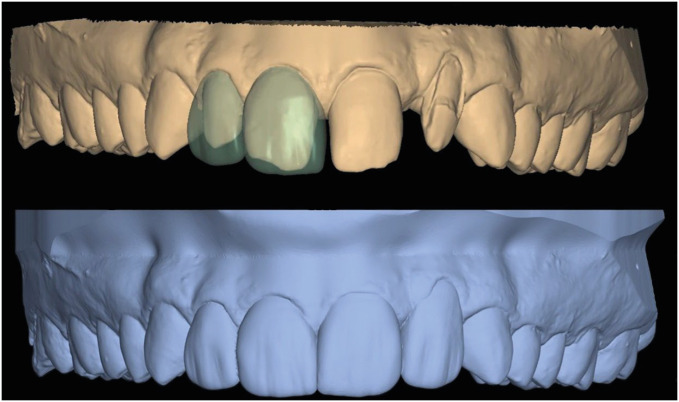
The dental team opted to use a clear resin-based 3D-printed index to accurately replicate a diagnostic wax-up in the final direct composite restorations. The process began with a virtual wax-up design using a dental Computer-Aided Design (CAD) software program (Dental Cad 3.0 Galway; Exocad GmbH, Darmstadt, Germany). The approved design was then exported as Standard Tessellation Language (STL) files: the first one for the wax-up of the right central and lateral incisors only, and the second one for the wax-up of all 4 maxillary anterior teeth (
Figure 2). The STL files were imported into a 3D modeling software program (Meshmixer; Autodesk, Inc., San Rafael, CA, USA), an open-source software, to design the custom indices. To facilitate manipulation and resin composite build-up and index removal, 2 indices were designed—one for the right side and the other for the left side—using the 2 imported virtual wax-up files. It was ensured that both indices extended to partially cover at least 1 tooth before and 1 tooth after those intended to be restored, for accurate indexing and verification of seating.
Figure 2 Digital representation of virtual wax-up designs within dental software.
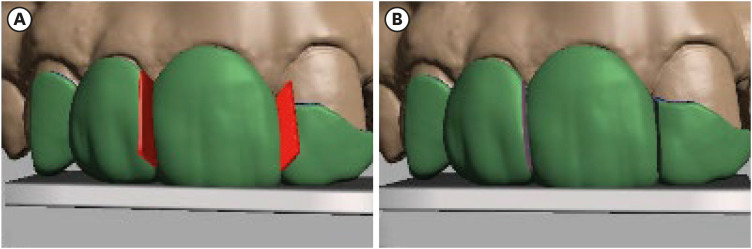
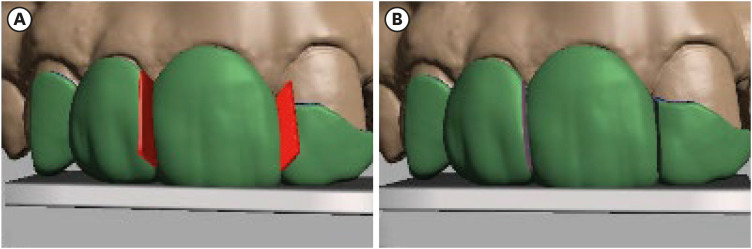
Once the designs were completed in the software, virtual sheets with a thickness of 0.1 mm were imported and placed inter-proximally adjacent to the teeth to be restored on both sides. The size (height and width) of the sheets was adjusted according to the corresponding interproximal space. Proper alignment was achieved, and the Boolean difference function was performed in the software program one by one in each designed index (
Figure 3).
Figure 3 Dental software depiction of the designed index. (A) The virtual sheet correctly positioned interproximally; (B) The index after applying the Boolean difference function to create space for metal matrices.
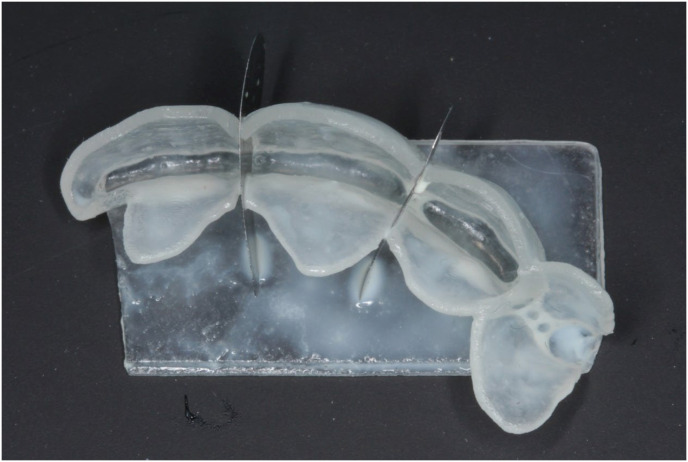
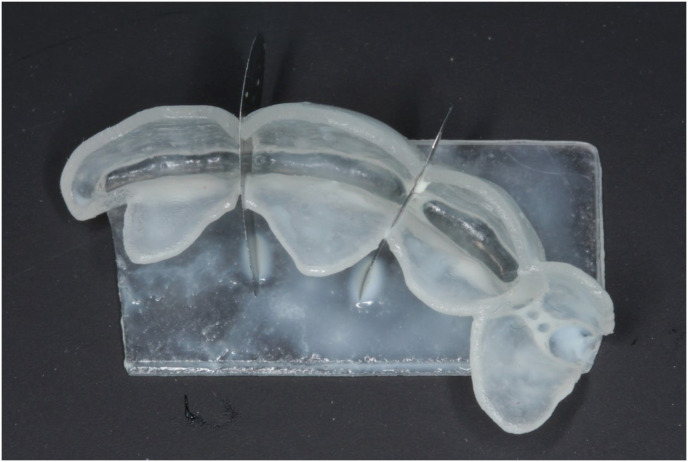
The designed indices were 3-dimensionally printed using a clear biocompatible resin (NextDent Ortho Clear; NextDent B.V., Soesterberg, Netherlands) compatible with photopolymerizing 3D printing technology, such as stereolithography (SLA) and digital light processing (DLP). In this case report, a 3D printer (NextDent 5100; NextDent B.V.) was used. The 3D-printed indices were disinfected with a 70% ethanol solution spray and allowed to remain wet for 10 minutes before being thoroughly rinsed with distilled water to remove any residual ethanol. Starting with the right side restorations, appropriately sized metal matrices were selected and placed in the corresponding spaces created inter-proximally in the right index. The patency of the spaces for the metal matrix segments was first verified by inserting the matrix segment. Any closed spaces due to adhesion of their borders during the 3D printing process, due to their small size, were reopened using an ultra-thin diamond-impregnated disc.
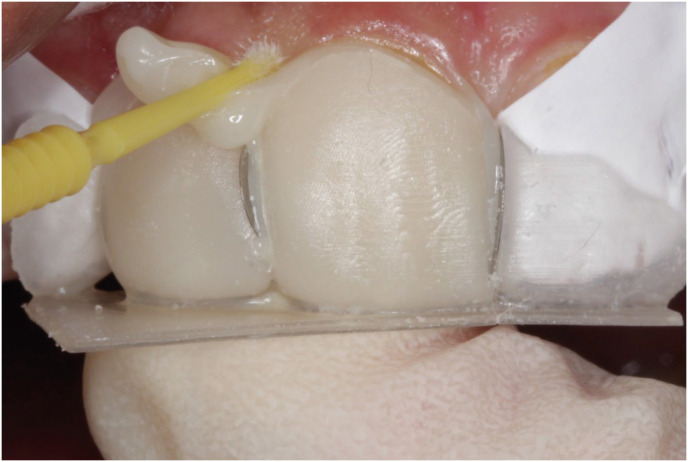
Proper seating of the index with the incorporation of the metal matrix segments was then verified in the patient’s mouth by checking for optimal fit, using the index engagement with adjacent teeth as a guide (
Figure 4). Any necessary trimming of the matrices or index was performed to achieve a proper fit.
Figure 4 Three-dimensional-printed index with integrated metal matrices in place for fit evaluation.

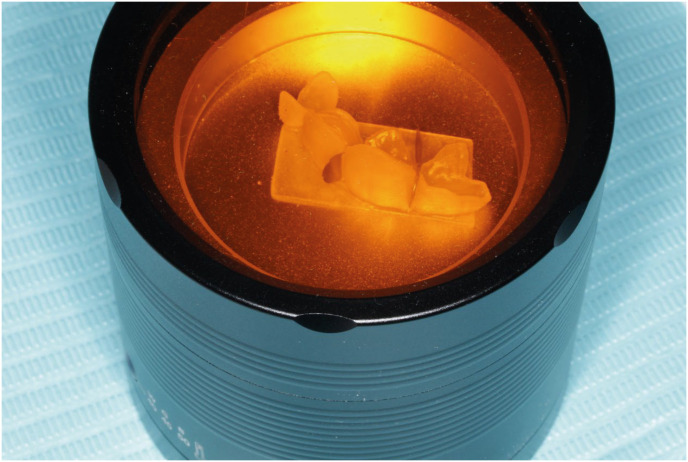
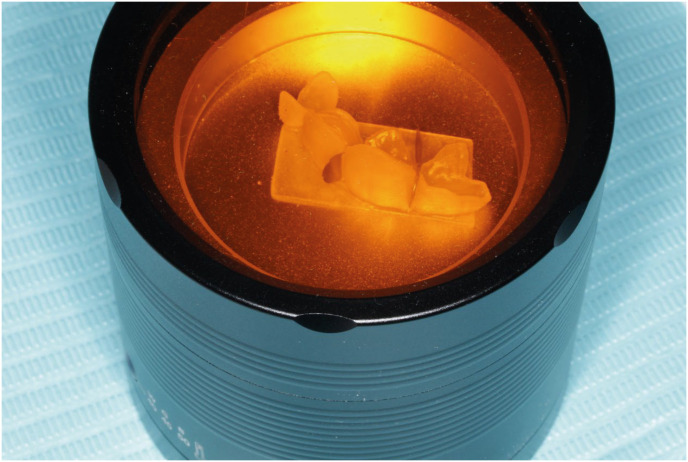
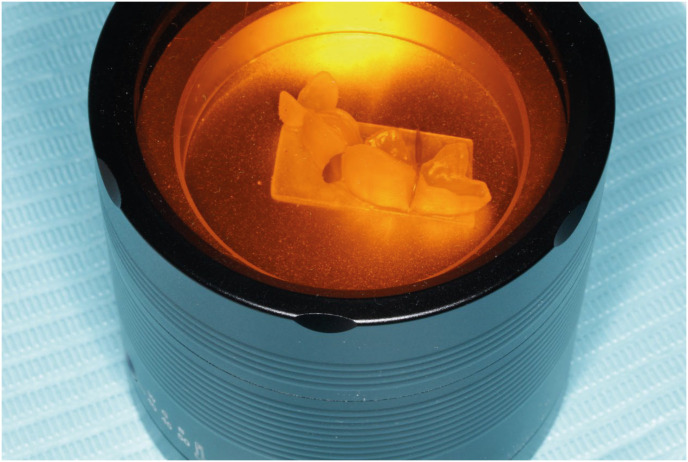
The index was then coated with a separating medium (Siliform; Trigroup Technologies, Sunnyvale, TX, USA) by fully submerging it for 15 seconds, allowing it to dry for 10 minutes, and repeating the coating process once more (
Figure 5). The index was filled with a heated conventional composite (Filtek Z250 Universal Restorative Compules, A2 shade; 3M Dental, St Paul, MN, USA) by injecting it from the compule using a composite gun. The composite was adapted to the intaglio surface of the index using a Teflon-coated, non-stick plastic composite instrument, and the index was placed in a covered composite heater (Azdent Dental Resin Composite Warmer; Henan Baistra Industries Corp., Zhengzhou, China) until use (
Figure 6).
Figure 5 Three-dimensional-printed index coated with separating medium.
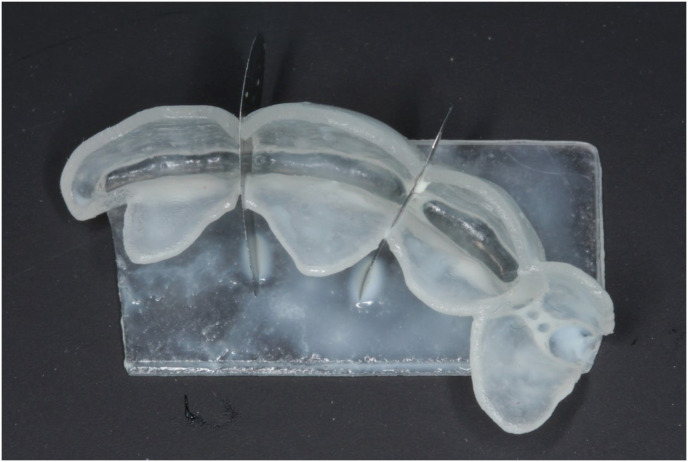
Figure 6 Three-dimensional-printed index loaded with composite resin and placed into composite heater.
Partial isolation was applied using cotton rolls and a lip and cheek retractor (OptiView; Kerr Corp, Pomona, CA, USA). The adjacent teeth were isolated using polytetrafluoroethylene (PTFE) tape. No preparation was done to the teeth to be restored except for rounding the sharp line angles. The enamel surfaces were etched with 37% phosphoric acid (Scotchbond Universal Etchant; 3M Dental) for 15 seconds. Single Bond Universal Adhesive (3M Dental) was applied to the pre-etched surfaces using a regular-sized microbrush for 20 seconds. The bonding agent-coated enamel was gently air-blown for 5 seconds and then polymerized with a dental light-emitting diode (LED) light-polymerizing unit (Mini LED; Acteon Group, Mérignac, France) for 10 seconds, following the manufacturer’s instructions.
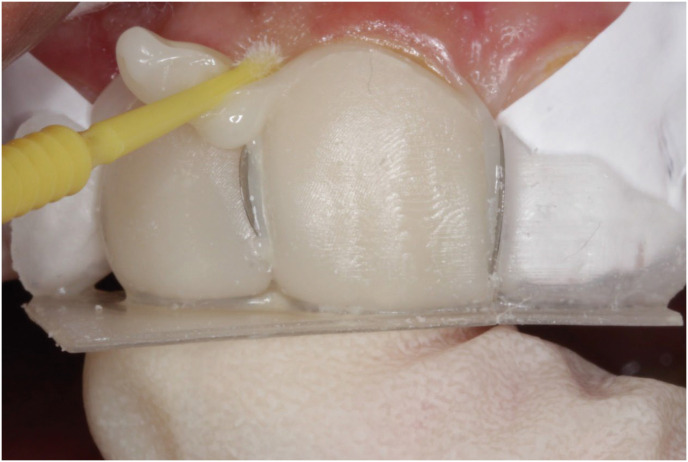
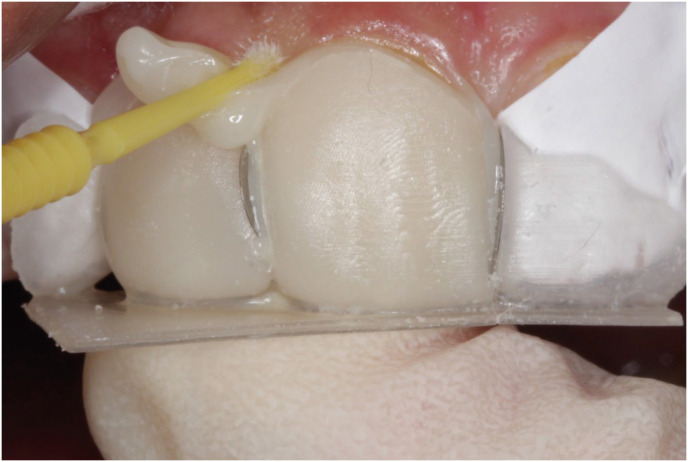
The heated, composite-filled index was seated onto the teeth
in situ and stabilized by hand. Excess filling material at the margins was removed. Once adjusted to mouth temperature, the composite’s high consistency facilitated easy removal (
Figure 7). The composite restoration was fully polymerized using a dental light-polymerizing unit, applying light on each surface according to manufacturer instructions. The index was carefully removed to prevent fracturing the restoration. The proper application of a separating medium facilitated a clean release between the index and the composite resin, and the metal matrices were removed inter-proximally.
Figure 7 Removal of excess composite at the index margins after verification of full seating.
The restorations were inspected for proper contour to ensure adherence to the intended design from the wax-up. If necessary, adjustments to add or remove excess material were made, and static and dynamic occlusal contact was checked. The restorations were finished and polished as follows: excess 3D-printed resin and surplus resin composite were initially removed using a sickle hand scaler and a number 12 blade. A tapered ultrafine finishing Tapered Shoulder diamond bur (847KREF FG.016; Komet, Rock Hill, SC, USA) was employed to refine the restoration, and for the interproximal areas, a mosquito-shaped diamond finishing bur (8392SU.FG.016; Komet) was used to refine the embrasure areas. Interproximal contours were finished using flexible and malleable medium and fine-grain stainless steel and polyester finishing strips (Microdont, São Paulo, SP, Brazil).
The polishing process continued with stones and impregnated silicone polishers, both cup-type and cone-shaped (Composite Polishing Kit CA; SHOFU Dental, San Marcos, CA, USA). For the final touch, polishing discs (Sof-Lex contouring and polishing Discs, Coarse/Medium, Fine/Super Fine; 3M Dental) were utilized, completing the polishing procedure for the right side restorations (
Figure 8). The left side index was then tried, metal matrices were then fitted, and the same steps were repeated to complete the left side, finalizing the restorations for the 4 anterior teeth. This gave the patient his new optimal smile, taking into account the clinical circumstances and modifiers of his case. The patient was satisfied with the final results (
Figure 9).
Figure 8 Postoperative view of finished right side restorations, after completion of finishing and polishing.

Figure 9 Postoperative view of the completed restorations on both sides, following finishing and polishing.

DISCUSSION
One of the challenges when restoring multiple adjacent teeth is the potential for restorations to bond together after composite resin polymerization. This affects the establishment of proper contact points and contours, which in turn impacts access to oral hygiene and aesthetic outcomes. The inability to print ultra-thin resin barriers, similar to metal matrices, coupled with concealed interproximal contours in the wax-up or 3D-printed resin base cast or conventional gypsum-based casts, complicates this process. Several studies have attempted to address this issue [
15,
16,
17]. In the present case, the incorporation of interproximal metal strips within the index has been proposed.
Innovations in digital dentistry and CAD software make it possible to design spaces to accommodate thin metal matrix segments between adjacent teeth. The proper design of the wax-up contours, embrasure areas, and a snugly fitting index that extends and copies contours and surface details of the interproximal and embrasure areas, all in the presence of ultra-thin metal matrix segments placed within the index in the interproximal areas, will ensure the formation of precise interproximal contours and contacts. Furthermore, these metal matrices can be easily removed independently before or after index removal, either withdrawn in the buccal or lingual/palatal direction after resin polymerization, similar to metal matrix bands used in conventional restorative procedures. This approach prevents inadvertent composite fusion between adjacent teeth and reduces the time required for finishing and polishing.
The index’s scalloped margin, closely following the gingival contour, facilitates the easy removal of excess composite material before polymerization, promoting a seamless marginal seal and reducing finishing time. The index design also allows for proper seating in the presence of a rubber dam, which is generally considered the most effective means of isolation for optimizing bonding procedures. Due to its concise design, the seating of the index is not impaired by either the rubber dam or clamps. However, in the presented case, the high zenith of the left lateral incisor made it difficult to apply effective rubber dam isolation. Consequently, appropriate non-rubber dam isolation was used. Furthermore, the rigidity of the resin material provides stability during the placement and sculpting of high-viscosity composite resins, enhancing control and predictability throughout the restorative procedure.
The proposed approach not only streamlines the restoration process but also has the potential to enhance both adolescent patient and dentist satisfaction with the final outcome. By simplifying the technique and reducing reliance on freehand artistry, the technique may lead to more consistent and predictable aesthetic results. Additionally, the reduced chairside time and simplified finishing procedures translate into a more efficient workflow for the dentist. Importantly, the use of a rigid index may minimize the need for specialized, highly filled, flowable composites, which can be more technique-sensitive [
11]. Moreover, the reliance on widely available 3D printers and clear resin materials allows for the seamless integration of this technique into everyday dental practice.
Despite its advantages, this technique requires careful consideration of certain limitations. The rigidity of the resin index, while advantageous during placement, necessitates cautious removal to prevent fracture of either the index or the restoration. This is because if there are undercuts in the composite restoration, it will be difficult to withdraw the rigid matrix intact. This is similar to conventional prefabricated cellulose acetate crowns, which frequently need to be cut and stripped from the tooth after polymerization of the resin composite. Sectioning the index may be necessary in some cases, precluding reuse.
To mitigate this, a balance between rigidity and ease of removal is achieved by designing the index with a thickness of approximately 1 mm. Additionally, it may be possible to reduce or eliminate the undercut in the wax-up design or offset it in the index design; however, this will affect the esthetically proper and anatomically correct contours and transitional line angles of the teeth. Therefore, this is not recommended despite its possibility. Furthermore, the use of a separating medium specifically formulated for 3D-printed resins is crucial to prevent bonding between the index and the composite [
18]. This separating medium is a silicone-based separator coating for 3D-printed resin dental appliances, specifically designed to be compatible with dental bonding procedures. It has a very low film thickness and its hydrophobic nature will not lead to any discoloration of the composite resin or bonding resin [
19,
20]. The application technique of the separating medium makes the coating of the index more uniform, which facilitates easy and clean separation and removal of the index while slightly affecting the surface roughness of the resultant composite restoration [
18]. This can be improved through proper finishing and polishing of the restorations to achieve a smooth and well-finished surface. Finally, warming the composite resin to reduce its viscosity before placement is recommended to minimize the risk of index fracture and facilitate smoother adaptation.
CONCLUSIONS
Malformed incisors were aesthetically restored using direct universal composite restoration. This approach used a transparent resin index, precisely customized from a digital wax-up, enabling a predictable and straightforward application of the restoration. This workflow not only streamlined the process and significantly improved the precision of the restorative technique but also reduced chairside time and assured a predictable and optimal aesthetic outcome. The index is custom-fabricated for each patient, ensuring an accurate fit and optimal adaptation to the individual tooth morphology.
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Farah R.
Data curation: Farah R, Al-Haj Ali S, Alharbi A, Alresheedi B.
Formal analysis: Farah R, Al-Haj Ali S.
Investigation: Farah R, Alharbi A, Alresheedi B.
Methodology: Farah R, Alharbi A, Alresheedi B.
Resources: Farah R, Alharbi A, Alresheedi B.
Software: Farah R.
Supervision: Farah R.
Validation: Farah R, Al-Haj Ali S.
Visualization: Farah R, Al-Haj Ali S.
Writing - original draft: Farah R, Al-Haj Ali S.
Writing - review & editing: Al-Haj Ali S.
REFERENCES
- 1. Izgi AD, Ayna E. Direct restorative treatment of peg-shaped maxillary lateral incisors with resin composite: a clinical report. J Prosthet Dent 2005;93:526-529.ArticlePubMed
- 2. Dean VA, Avery DR, McDonald RE. McDonald and Avery’s dentistry for the child and adolescent. 11th ed. St. Louis, MO: Elsevier; 2022.
- 3. American Academy of Dentistry. Adolescent oral health care. The reference manual of dentistry. Buena Park, CA: American Academy of Dentistry; 2021. p. 267-276.
- 4. Raigrodski AJ. Multipurpose application of custom, rigid, clear matrix for fabricating trial restorations, tooth preparation guides, and interim veneers. J Prosthet Dent 2022;128:560-565.ArticlePubMed
- 5. Revilla-León M, Sánchez-Rubio JL, Besné-Torre A, Özcan M. A report on a diagnostic digital workflow for esthetic dental rehabilitation using additive manufacturing technologies. Int J Esthet Dent 2018;13:184-196.PubMed
- 6. Revilla-León M, Besné-Torre A, Sánchez-Rubio JL, Fábrega JJ, Özcan M. Digital tools and 3D printing technologies integrated into the workflow of restorative treatment: a clinical report. J Prosthet Dent 2019;121:3-8.ArticlePubMed
- 7. Revilla-León M, Fountain J, Piedra-Cascón W, Özcan M, Zandinejad A. Workflow of a fiber-reinforced composite fixed dental prosthesis by using a 4-piece additive manufactured silicone index: a dental technique. J Prosthet Dent 2021;125:569-575.ArticlePubMed
- 8. Hosaka K, Tichy A, Hasegawa Y, Motoyama Y, Kanazawa M, Tagami J, et al. Replacing mandibular central incisors with a direct resin-bonded fixed dental prosthesis by using a bilayering composite resin injection technique with a digital workflow: a dental technique. J Prosthet Dent 2021;126:150-154.ArticlePubMed
- 9. Ammannato R, Ferraris F, Allegri M. The “index cutback technique”: a three-dimensional guided layering approach in direct class IV composite restorations. Int J Esthet Dent 2017;12:450-466.PubMed
- 10. Gao Y, Li J, Dong B, Zhang M. Direct composite resin restoration of a class IV fracture by using 3D printing technology: a clinical report. J Prosthet Dent 2021;125:555-559.ArticlePubMed
- 11. Terry DA, Powers JM. A predictable resin composite injection technique, Part I. Dent Today 2014;33:96. 98-101.PubMed
- 12. Hosaka K, Tichy A, Yamauti M, Watanabe K, Kamoi K, Yonekura K, et al. Digitally guided direct composite injection technique with a bi-layer clear mini-index for the management of extensive occlusal caries in a pediatric patient: a case report. J Adhes Dent 2023;25:211-218.PubMed
- 13. Geštakovski D. The injectable composite resin technique: biocopy of a natural tooth - advantages of digital planning. Int J Esthet Dent 2021;16:280-299.PubMed
- 14. Watanabe K, Tichy A, Kamoi K, Hiasa M, Yonekura K, Tanaka E, et al. Restoration of a microdont using the resin composite injection technique with a fully digital workflow: a flexible 3D-printed index with a stabilization holder. Oper Dent 2023;48:483-489.ArticlePubMedPDF
- 15. Zhang Y, Zhang J, Fan L, Yu H. Closing post-orthodontic spaces between anterior teeth using sequential 3D-printed direct composite injection guides. Oper Dent 2022;47:612-619.ArticlePubMedPDF
- 16. Hosaka K, Tichy A, Motoyama Y, Mizutani K, Lai WJ, Kanno Z, et al. Post-orthodontic recontouring of anterior teeth using composite injection technique with a digital workflow. J Esthet Restor Dent 2020;32:638-644.ArticlePubMedPDF
- 17. Xia J, Li Y, Cai D, Shi X, Zhao S, Jiang Q, et al. Direct resin composite restoration of maxillary central incisors using a 3D-printed template: two clinical cases. BMC Oral Health 2018;18:158.ArticlePubMedPMCPDF
- 18. Farah RI, Elzeky M, Alresheedi B, Al-Haj Ali SN. Evaluation of separating media for autopolymerizing acrylic resin fabricated on 3D-printed acrylate-based resin dental casts. J Prosthet Dent 2023;130:110.e1-110.e5.ArticlePubMed
- 19. Wood BF, Sorensen SE, Ortman HR. Denture mold separators as a cause of staining around porcelain denture teeth. J Prosthet Dent 1967;17:149-154.ArticlePubMed
- 20. Zani D, Vieira DF. A comparative study of silicone as a separating medium for denture processing. J Prosthet Dent 1979;42:386-391.ArticlePubMed
 , Sanaa Najeh Al-Haj Ali2
, Sanaa Najeh Al-Haj Ali2 , Abdullah Alharbi3
, Abdullah Alharbi3 , Bandar Alresheedi1
, Bandar Alresheedi1










 KACD
KACD
 ePub Link
ePub Link Cite
Cite

