Articles
- Page Path
- HOME > Restor Dent Endod > Volume 49(3); 2024 > Article
-
Research Article
Procedural errors detected by cone beam tomography in cases with indication for retreatment:
in vivo cross-sectional study -
Henry Paul Valverde Haro1,2
 , Carmen Rosa Garcia Rupaya2
, Carmen Rosa Garcia Rupaya2 , Flávio R. F. Alves3
, Flávio R. F. Alves3
-
Restor Dent Endod 2024;49(3):e26.
DOI: https://doi.org/10.5395/rde.2024.49.e26
Published online: June 24, 2024
1Postgraduate Program in Dentistry, University of Grande Rio (UNIGRANRIO), Rio de Janeiro, RJ, Brazil.
2Postgraduate Program in Dentistry, Cayetano Heredia University, Lima, Peru.
3Department of Dental Research, Faculty of Dentistry, Iguaçu University (UNIG), Nova Iguaçu, RJ, Brazil.
- Correspondence to Henry Paul Valverde Haro, DDS, MSc. Postgraduate Program in Dentistry, University of Grande Rio (UNIGRANRIO), Rua Professor José de Souza Herdy, 1160 Jardim Vinte e Cinco de Agosto, Duque de Caxias, RJ 25071-202, Brazil. endosolutionsec@gmail.com
Copyright © 2024. The Korean Academy of Conservative Dentistry
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Objectives This study aimed to investigate the frequency and type of endodontic procedural errors in cases indicated for retreatment through cone-beam computed tomography (CBCT) analysis.
-
Materials and Methods The sample consisted of 96 CBCT scans, encompassing 122 permanent teeth with fully formed roots. Errors included perforation, instrument fracture, canal transportation, missed canals, and inadequate apical limit of filling. Additionally, potential risk factors were analyzed and subjected to statistical modeling.
-
Results The most frequent procedural error observed was the inadequate apical limit of filling, followed by canal transportation, perforation, missed canal, and instrument fracture. Statistically significant associations were identified between various procedural errors and specific factors. These include canal transportation and root canal wall, with the buccal wall being the most commonly affected; missed canal and tooth type, particularly the palatine and second mesiobuccal canal canals; inadequate apical limit of filling and root curvature, showing a higher deviation to the mesial direction in severely curved canals; inadequate apical limit of filling and the presence of calcifications, with underfilling being the most frequent; canal transportation and periapical lesion, notably with deviation to the buccal direction; and the direction of perforation and periapical lesion, most frequently occurring to buccal direction.
-
Conclusions CBCT emerges as a valuable tool in identifying procedural errors and associated factors, crucial for their prevention and management.
INTRODUCTION
MATERIALS AND METHODS
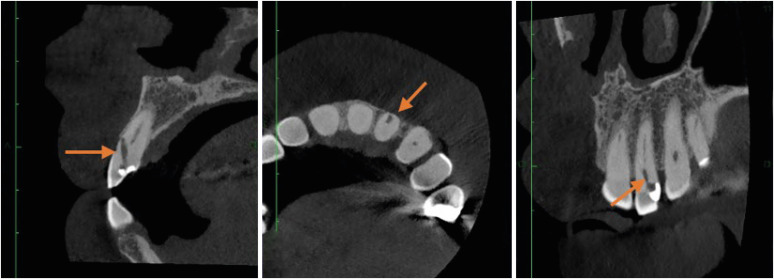
1. Perforation and direction
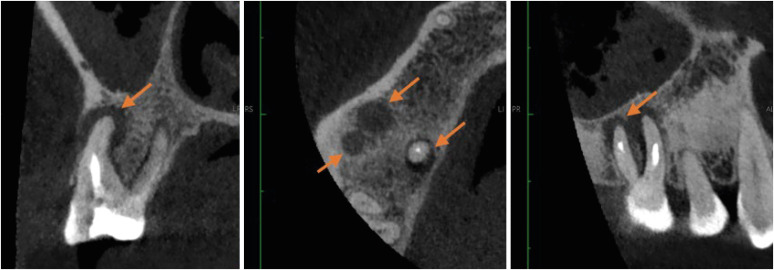
Dynamic cone-beam computed tomography analysis for identification of perforation in the right lateral incisor.
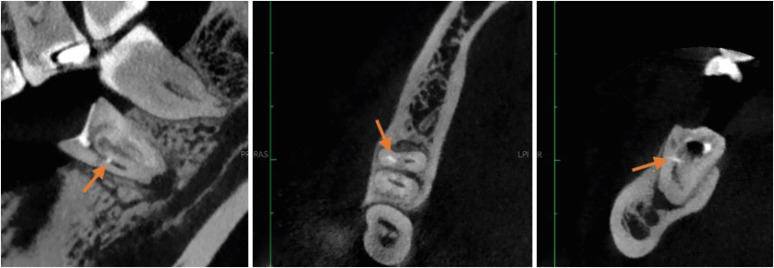
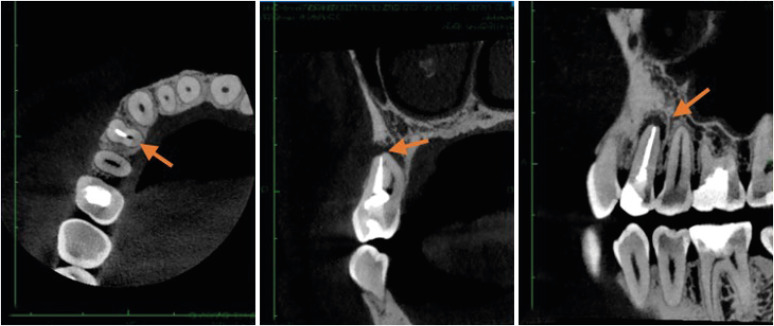
2. Instrument fracture
Dynamic cone-beam computed tomography analysis for identification of fractured instrument in lower left first molar.
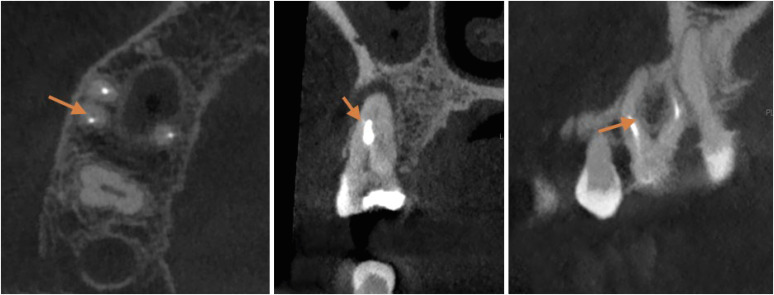
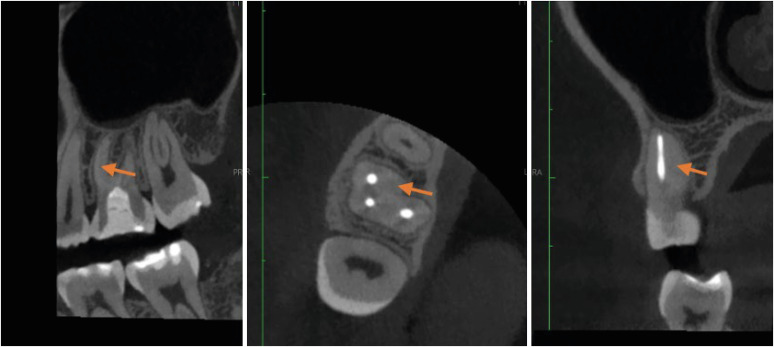
3. Canal transportation
Dynamic cone-beam computed tomography analysis for identification of canal transportation in upper right first molar.
4. Missed canal
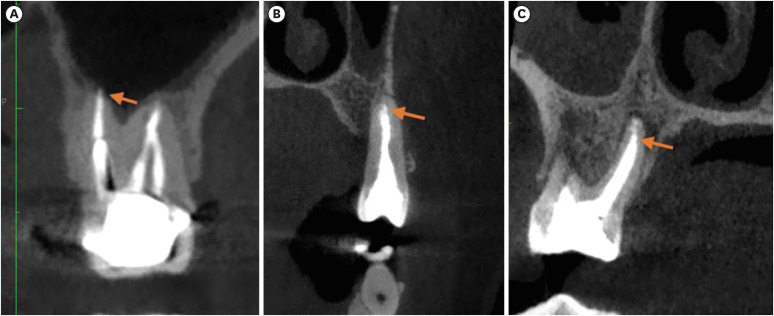
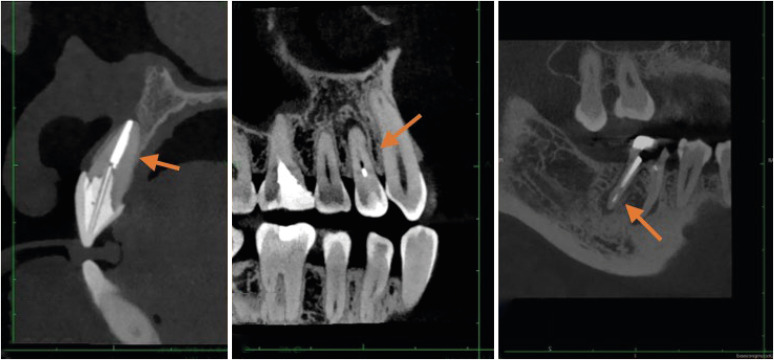
5. Apical limit of filling
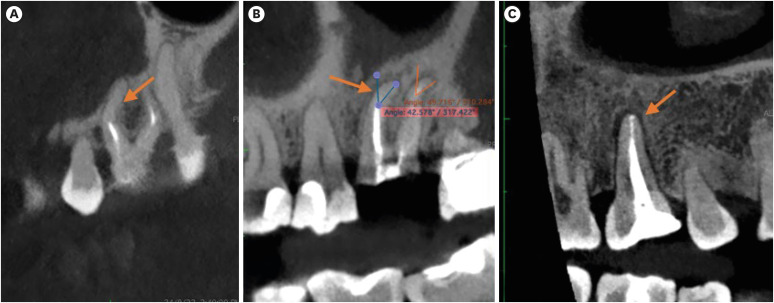
Identification of (A) molar with an overfilled canal, (B) premolar at the appropriate level and (C) palatal canal of an underfilled upper molar.
6. Associated factors
RESULTS
Type and frequency of endodontic procedural errors per canal (n = 227)
Procedural errors according to tooth type
Procedural errors according to the type of root curvature
Procedural errors according to the presence of calcifications
Endodontic procedure errors according to the presence of periapical reaction
Procedural errors according to dental quadrant
DISCUSSION
CONCLUSIONS
-
Funding: This study was supported by grants from Fundação Carlos Chagas Filho de Amparo à Pesquisa do Estado do Rio de Janeiro (FAPERJ) and Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Brazilian Governmental Institutions.
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Valverde Haro HP, Rupaya CR.
Data curation: Valverde Haro HP.
Formal analysis: Valverde Haro HP.
Funding acquisition: Valverde Haro HP.
Investigation: Valverde Haro HP.
Methodology: Rupaya CR.
Project administration: Rupaya CR.
Resources: Valverde Haro HP.
Software: Valverde Haro HP.
Supervision: Rupaya CR.
Validation: Alves FRF.
Visualization: Valverde Haro HP.
Writing - original draft: Valverde Haro HP, Alves FRF.
Writing - review & editing: Alves FRF.
- 1. Toia CC, Khoury RD, Corazza BJM, Orozco EIF, Valera MC. Effectiveness of 1-visit and 2-visit endodontic retreatment of teeth with persistent/secondary endodontic infection: a randomized clinical trial with 18 months of follow-up. J Endod 2022;48:4-14.ArticlePubMed
- 2. Gaêta-Araujo H, Fontenele RC, Nascimento EHL, Nascimento MDCC, Freitas DQ, de Oliveira-Santos C. Association between the root canal configuration, endodontic treatment technical errors, and periapical hypodensities in molar teeth: a cone-beam computed tomographic study. J Endod 2019;45:1465-1471.ArticlePubMed
- 3. Alamoudi RA, Alharbi AH, Farie GA, Fahim O. The value of assessing case difficulty and its effect on endodontic iatrogenic errors: a retrospective cross-sectional study. Libyan J Med 2020;15:1688916.ArticlePubMedPMC
- 4. Yagmoor M, Bakhsh A, Mandourah O, Alsofi L. Management of a radiopaque foreign body associated with a lower first premolar: a case report. Clin Case Rep 2022;10:e05465.ArticlePubMedPMCPDF
- 5. da Cunha LZV, Solda C, Padoin K, Rigo L. Endodontic procedural errors: analysis of images from cone beam computed tomography. Forensic Imaging 2022;28:200493.Article
- 6. Siqueira JF Jr, Rôças IN. Clinical implications and microbiology of bacterial persistence after treatment procedures. J Endod 2008;34:1291-1301.e3.ArticlePubMed
- 7. Peña-Bengoa F, Cáceres C, Niklander SE, Meléndez P. Association between second mesiobuccal missed canals and apical periodontitis in maxillary molars of a Chilean subpopulation. J Clin Exp Dent 2023;15:e173-e176.PubMedPMC
- 8. Ballikaya E, Koc N, Avcu N, Cehreli ZC. The quality of root canal treatment and periapical status of permanent teeth in Turkish children and teens: a retrospective CBCT study. Oral Radiol 2022;38:405-415.ArticlePubMedPDF
- 9. Nouroloyouni A, Salem Milani A, Etminan A, Noorolouny S, Tavakkol E, Mikaieli Xiavi H, et al. Cone-beam computed tomography assessment of quality of endodontic treatment and prevalence of procedural errors in mandibular molars. Int J Clin Pract 2023;2023:3558974.ArticlePubMedPMCPDF
- 10. Alghamdi NS, Algarni YA, Ain TS, Alfaifi HM, AlQarni AA, Mashyakhi JQ, et al. Endodontic mishaps during root canal treatment performed by undergraduate dental students: an observational study. Medicine (Baltimore) 2021;100:e27757.PubMedPMC
- 11. Fayad MI, Nair M, Levin MD, Benavides E, Rubinstein RA, Barghan S, et al. AAE and AAOMR joint position statement: use of cone beam computed tomography in endodontics 2015 update. Oral Surg Oral Med Oral Pathol Oral Radiol 2015;120:508-512.PubMed
- 12. Costa FF, Pacheco-Yanes J, Siqueira JF Jr, Oliveira ACS, Gazzaneo I, Amorim CA, et al. Association between missed canals and apical periodontitis. Int Endod J 2019;52:400-406.ArticlePubMedPDF
- 13. Karabucak B, Bunes A, Chehoud C, Kohli MR, Setzer F. Prevalence of apical periodontitis in endodontically treated premolars and molars with untreated canal: a cone-beam computed tomography study. J Endod 2016;42:538-541.ArticlePubMed
- 14. Schneider SW. A comparison of canal preparations in straight and curved root canals. Oral Surg Oral Med Oral Pathol 1971;32:271-275.ArticlePubMed
- 15. Nascimento EHL, Gaêta-Araujo H, Andrade MFS, Freitas DQ. Prevalence of technical errors and periapical lesions in a sample of endodontically treated teeth: a CBCT analysis. Clin Oral Investig 2018;22:2495-2503.ArticlePubMedPDF
- 16. Al Yahya RS, Al Attas MH, Javed MQ, Khan KI, Atique S, Abulhamael AM, et al. Root canal configuration and its relationship with endodontic technical errors and periapical status in premolar teeth of a Saudi sub-population: a cross-sectional observational CBCT study. Int J Environ Res Public Health 2023;20:1142.ArticlePubMedPMC
- 17. Jurič R, Vidmar G, Blagus R, Jan J. Factors associated with the outcome of root canal treatment-a cohort study conducted in a private practice. Int Endod J 2024;57:377-393.ArticlePubMed
- 18. Villa-Machado PA, Restrepo-Patiño DM, Calvo-Trejos JP, Restrepo-Restrepo FA, Tobón-Arroyave SI, Provenzano JC, et al. Cone-beam computed tomographic and micro-computed tomographic evaluations of the root apexes of teeth with posttreatment apical periodontitis. J Endod 2020;46:1695-1701.ArticlePubMed
- 19. Siqueira JF Jr, Rôças IN. Present status and future directions: microbiology of endodontic infections. Int Endod J 2022;55(Supplement 3):512-530.ArticlePubMedPDF
- 20. Pinto JC, de Faria-Vasconcelos K, Leite AF, Pedano MS, Guerreiro-Tanomaru J, Jacobs R, et al. Effect of foraminal enlargement on microcrack formation and apical transportation: a nano-CT assessment. Sci Rep 2023;13:4881.ArticlePubMedPMCPDF
- 21. Wu MK, Fan B, Wesselink PR. Leakage along apical root fillings in curved root canals. Part I: effects of apical transportation on seal of root fillings. J Endod 2000;26:210-216.ArticlePubMed
- 22. Hasheminia SM, Farhad A, Sheikhi M, Soltani P, Hendi SS, Ahmadi M. Cone-beam computed tomographic analysis of canal transportation and centering ability of single-file systems. J Endod 2018;44:1788-1791.ArticlePubMed
- 23. Wong J, Lee A, Zhang C. Diagnosis and management of apical fenestrations associated with endodontic diseases: a literature review. Eur Endod J 2021;6:25-33.ArticlePubMedPMC
- 24. Wu L, Ha WN, Decurcio DA, Estrela C, Rossi-Fedele G. Comparison of curvature severity between sagittal and coronal planes of mesiobuccal canals in permanent maxillary first molars using multiple complexity-risk criteria: a CBCT cross-sectional study of a Brazilian subpopulation. J Endod 2023;49:1682-1689.e4.ArticlePubMed
- 25. Wang FM, Rudman J, Walsh RM, Jalali P. A retrospective study of initial root canal treatment failure in maxillary premolars via using cone-beam computed tomography. J Am Dent Assoc 2023;154:471-478.ArticlePubMed
- 26. Ayatollahi F, Tabrizizadeh M, Razavi H, Mowji M. Diagnostic value of cone-beam computed tomography and digital periapical radiography in detection of separated instruments. Iran Endod J 2019;14:14-17.PubMedPMC
- 27. Özer SY, Özkan G, Çetin E, Özkan HD. A comparative study of cone-beam computed tomography and periapical radiographs in decision-making after endodontic instrument fractures. Int J Artif Organs 2017;40:510-514.ArticlePubMedPDF
REFERENCES
Tables & Figures
REFERENCES
Citations

- Repair of furcal perforations using different calcium silicate cements: An in vitro study
Ariana Esperanza Apolo Aguilar, Maria Soledad Peñaherrera Manosalvas, Henry Paul Valverde Haro
Journal of Conservative Dentistry and Endodontics.2025; 28(10): 1007. CrossRef - Impact of Downward Load and Rotational Kinematics on Root Canal Instrumentation with a Heat-Treated Nickel–Titanium Rotary Instrument
Risako Yamamoto, Keiichiro Maki, Shunsuke Kimura, Satoshi Omori, Keiko Hirano, Arata Ebihara, Yoshio Yahata, Takashi Okiji
Materials.2025; 19(1): 108. CrossRef - ANALYSIS OF THE QUALITY OF ROOT CANAL OBTURATION AND PREVALENCE OF APICAL PERIODONTITIS IN ENDODONTICALLY TREATED TEETH
Cristina Coralia Nistor, Ioana Suciu , Elena Zabrac , Ruxandra Ioana Bartok , Bogdan Dimitriu , Andreea Baluta
Romanian Journal of Oral Rehabilitation.2024; 16(4): 311. CrossRef
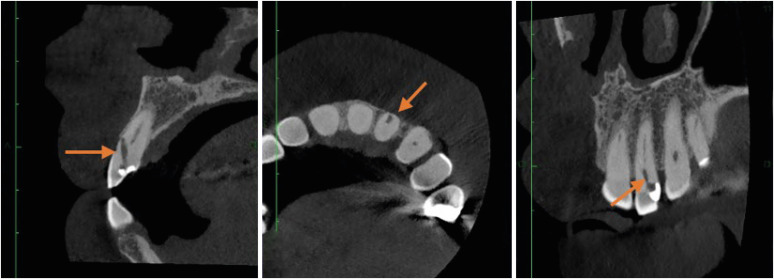
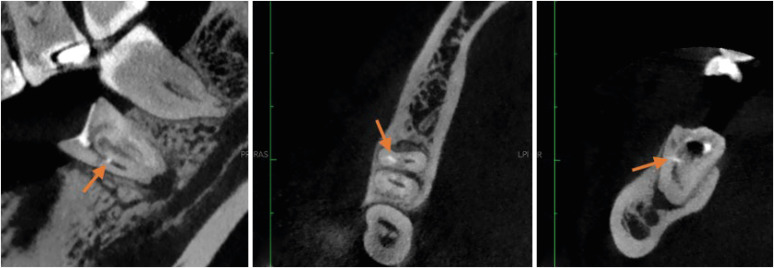
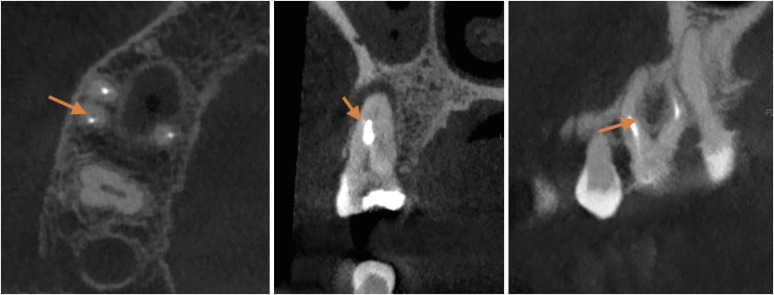
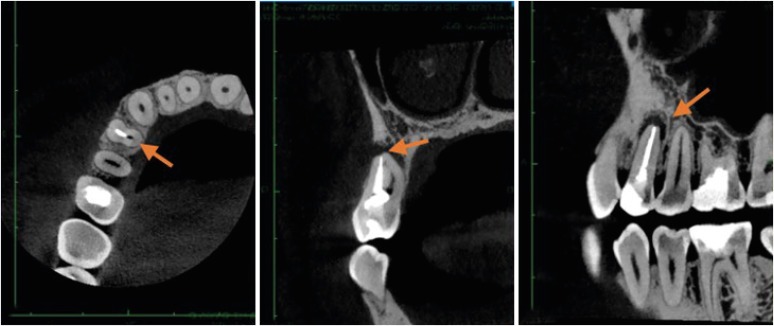
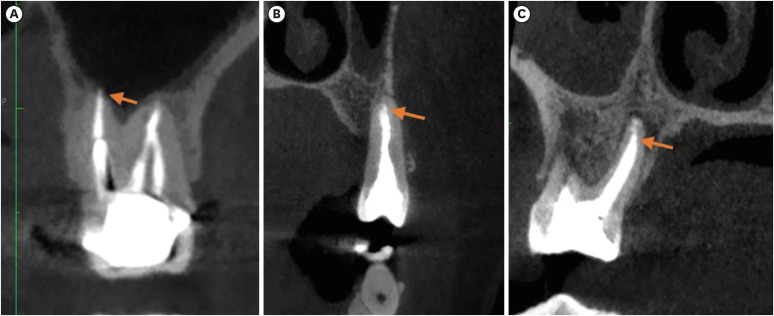
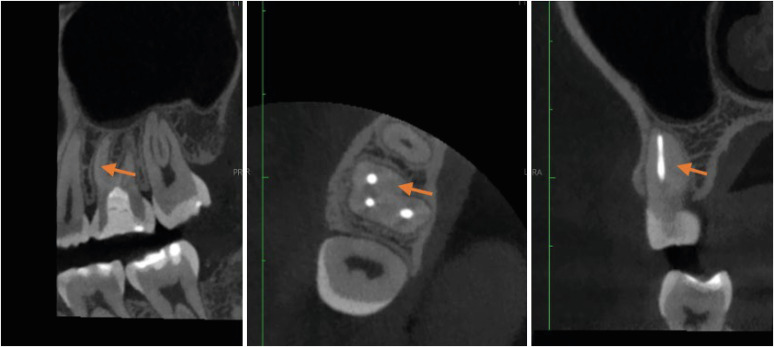
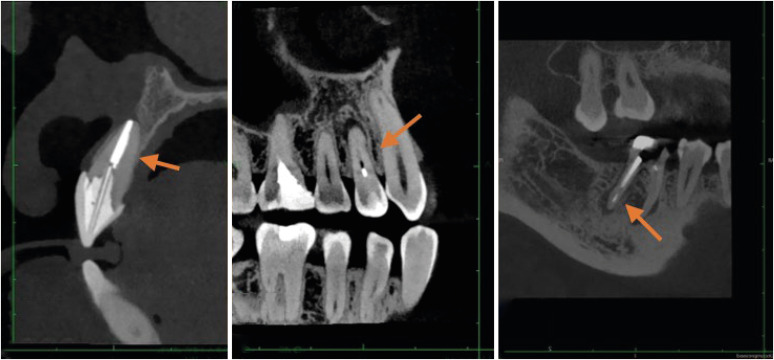
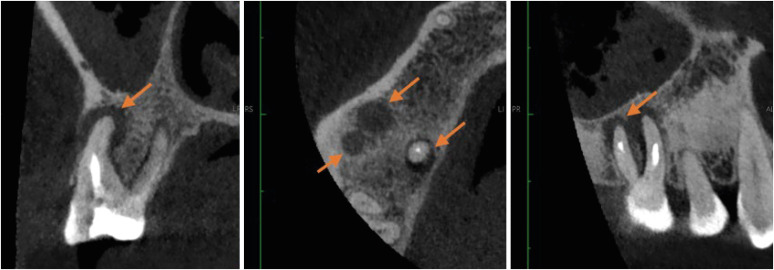
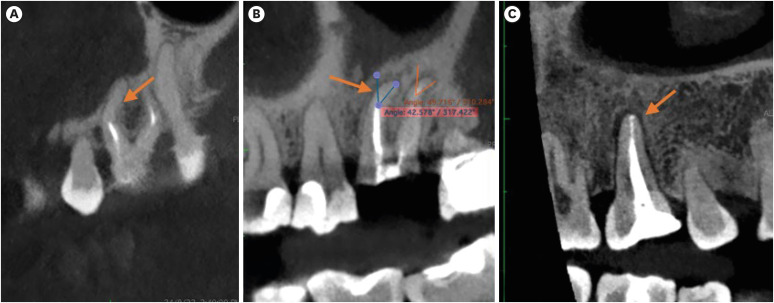
Figure 1
Figure 2
Figure 3
Figure 4
Figure 5
Figure 6
Figure 7
Figure 8
Figure 9
Type and frequency of endodontic procedural errors per canal (n = 227)
| Procedural errors | Values | |
|---|---|---|
| Perforation | ||
| Without perforation | 83 (36.56) | |
| Buccal | 54 (23.79) | |
| Distal | 27 (11.89) | |
| Mesial | 39 (17.18) | |
| Palatal | 24 (10.57) | |
| Root canal transportation | ||
| No transport | 71 (31.28) | |
| Buccal | 64 (28.19) | |
| Distal | 24 (10.57) | |
| Mesial | 42 (18.50) | |
| Palatal | 26 (11.45) | |
| Instrument fracture | ||
| No fracture | 223 (98.24) | |
| Middle third | 4 (1.76) | |
| Missed canals | ||
| No missed canal | 190 (83.70) | |
| Single canal | 1 (0.44) | |
| Mesiobuccal | 6 (2.64) | |
| Mesiolingual | 2 (0.88) | |
| MB2 | 9 (3.96) | |
| Distobuccal | 5 (2.20) | |
| Palatal | 10 (4.41) | |
| Buccal | 4 (1.76) | |
| Root filling extension | ||
| Underfilled | 114 (50.22) | |
| Overfilled | 33 (14.54) | |
| Adequate | 40 (17.62) | |
| Unfilled | 40 (17.62) | |
Values are presented as number (%).
Procedural errors according to tooth type
| Procedural errors | Tooth type | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Upper Incisors | Upper canines | Upper premolars | Upper molars | Lower incisors | Lower premolars | Lower molars | Total | ||
| Perforation | |||||||||
| Without perforation | 13 (5.73) | 2 (0.88) | 19 (8.37) | 34 (14.98) | 0 (0.00) | 1 (0.44) | 14 (6.17) | 83 (36.56) | |
| Buccal | 15 (6.61) | 3 (1.32) | 11 (4.85) | 15 (6.61) | 0 (0.00) | 2 (0.88) | 8 (3.52) | 54 (23.79) | |
| Distal | 2 (0.88) | 1 (0.44) | 3 (1.32) | 13 (5.73) | 1 (0.44) | 0 (0.00) | 7 (3.08) | 27 (11.89) | |
| Mesial | 9 (3.96) | 0 (0.00) | 4 (1.76) | 15 (6.61) | 0 (0.00) | 2 (0.88) | 9 (3.96) | 39 (17.18) | |
| Palatal | 3 (1.32) | 0 (0.00) | 2 (0.88) | 10 (4.41) | 0 (0.00) | 2 (0.88) | 7 (3.08) | 24 (10.57) | |
| Pearson χ2 (1) = 0.6996 Pr = 0.403 | |||||||||
| Root canal transportation | |||||||||
| No transport | 6 (2.64) | 0 (0.00) | 16 (7.05) | 33 (14.54) | 0 (0.00) | 1 (0.44) | 15 (6.61) | 71 (31.28) | |
| Buccal | 19 (8.37) | 4 (1.76) | 14 (6.17) | 16 (7.05) | 0 (0.00) | 2 (0.88) | 9 (3.96) | 64 (28.19) | |
| Distal | 2 (0.88) | 1 (0.44) | 2 (0.88) | 12 (5.29) | 1 (0.44) | 0 (0.00) | 6 (2.64) | 24 (10.57) | |
| Mesial | 11 (4.85) | 1 (0.44) | 4 (1.76) | 15 (6.61) | 0 (0.00) | 3 (1.32) | 8 (3.52) | 42 (18.50) | |
| Palatal | 4 (1.76) | 0 (0.00) | 3 (1.32) | 11 (4.85) | 0 (0.00) | 1 (0.44) | 7 (3.08) | 26 (11.45) | |
| Pearson χ2 (1) = 6.9223 Pr = 0.009 | |||||||||
| Instrument fracture | |||||||||
| Unfractured | 42 (18.50) | 6 (2.64) | 39 (17.18) | 85 (37.44) | 1 (0.44) | 7 (3.08) | 43 (18.94) | 223 (98.24) | |
| Middle third | 0 (0.00) | 0 (0.00) | 0 (0.00) | 2 (0.88) | 0 (0.00) | 0 (0.00) | 2 (0.88) | 4 (1.76) | |
| Fisher's exact = 1.000/1-sided Fisher's exact = 0.438 | |||||||||
| Missed canals | |||||||||
| Single canal | 1 (0.44) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 1 (0.44) | |
| Mesiobuccal | 0 (0.00) | 0 (0.00) | 0 (0.00) | 4 (1.76) | 0 (0.00) | 0 (0.00) | 2 (0.88) | 6 (2.64) | |
| Mesiolingual | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 2 (0.88) | 2 (0.88) | |
| MB2 | 0 (0.00) | 0 (0.00) | 0 (0.00) | 9 (3.96) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 9 (3.96) | |
| Distobuccal | 0 (0.00) | 0 (0.00) | 0 (0.00) | 4 (1.76) | 0 (0.00) | 0 (0.00) | 1 (0.44) | 5 (2.20) | |
| Palatal | 0 (0.00) | 0 (0.00) | 7 (3.08) | 3 (1.32) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 10 (4.41) | |
| Buccal | 0 (0.00) | 0 (0.00) | 2 (0.88) | 2 (0.88) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 4 (1.76) | |
| Pearson χ2 (1) = 7.3180 Pr = 0.007 | |||||||||
| Root filling extension | |||||||||
| Underfilled | 19 (8.37) | 4 (1.76) | 15 (6.61) | 47 (20.70) | 1 (0.44) | 2 (0.88) | 26 (11.45) | 114 (50.22) | |
| Overfilled | 13 (5.73) | 0 (0.00) | 6 (2.64) | 11 (4.85) | 0 (0.00) | 3 (1.32) | 0 (0.00) | 33 (14.54) | |
| Adequate | 9 (3.96) | 2 (0.88) | 10 (4.41) | 8 (3.52) | 0 (0.00) | 2 (0.88) | 9 (3.96) | 40 (17.62) | |
| Unfilled | 1 (0.44) | 0 (0.00) | 8 (3.52) | 21 (9.25) | 0 (0.00) | 0 (0.00) | 10 (4.41) | 40 (17.62) | |
| Pearson χ2 (1) = 0.5117 Pr = 0.474 | |||||||||
Values are presented as number (%).
Procedural errors according to the type of root curvature
| Procedural errors | Type of root curvature | |||||
|---|---|---|---|---|---|---|
| Straight (≤ 5°) | Mild (5°–10°) | Moderate (10°–20°) | Severe (25°–70°) | Total | ||
| Perforation | ||||||
| Without perforation | 60 (26.43) | 7 (3.08) | 5 (2.20) | 11 (4.85) | 83 (36.56) | |
| Buccal | 38 (16.74) | 8 (3.52) | 1 (0.44) | 7 (3.08) | 54 (23.79) | |
| Distal | 13 (5.73) | 4 (1.76) | 2 (0.88) | 8 (3.52) | 27 (11.89) | |
| Mesial | 19 (8.37) | 10 (4.41) | 1 (0.44) | 9 (3.96) | 39 (17.18) | |
| Palatal | 18 (7.93) | 3 (1.32) | 2 (0.88) | 1 (0.44) | 24 (10.57) | |
| Pearson χ2 (8) = 15.3963 Pr = 0.052 | ||||||
| Root canal transportation | ||||||
| No transport | 46 (20.26) | 9 (3.96) | 5 (2.20) | 11 (4.85) | 71 (31.28) | |
| Buccal | 49 (21.59) | 7 (3.08) | 1 (0.44) | 7 (3.08) | 64 (28.19) | |
| Distal | 11 (4.85) | 4 (1.76) | 2 (0.88) | 7 (3.08) | 24 (10.57) | |
| Mesial | 22 (9.69) | 9 (3.96) | 1 (0.44) | 10 (4.41) | 42 (18.50) | |
| Palatal | 20 (8.81) | 3 (1.32) | 2 (0.88) | 1 (0.44) | 26 (11.45) | |
| Pearson χ2 (8) = 13.7770 Pr = 0.088 | ||||||
| Instrument fracture | ||||||
| Unfractured | 146 (64.32) | 31 (13.66) | 11 (4.85) | 35 (15.42) | 223 (98.24) | |
| Middle third | 2 (0.88) | 1 (0.44) | 0 (0.00) | 1 (0.44) | 4 (1.76) | |
| Fisher's exact = 0.612/1-sided Fisher's exact = 0.434 | ||||||
| Missed canals | ||||||
| No missed canal | 131 (57.71) | 25 (11.01) | 7 (3.08) | 27 (11.89) | 190 (83.70) | |
| Single canal | 1 (0.44) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 1 (0.44) | |
| Mesiobuccal | 1 (0.44) | 3 (1.32) | 0 (0.00) | 2 (0.88) | 6 (2.64) | |
| Mesiolingual | 1 (0.44) | 1 (0.44) | 0 (0.00) | 0 (0.00) | 2 (0.88) | |
| MB2 | 1 (0.44) | 2 (0.88) | 0 (0.00) | 6 (2.64) | 9 (3.96) | |
| Distobuccal | 5 (2.20) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 5 (2.20) | |
| Palatal | 6 (2.64) | 1 (0.44) | 2 (0.88) | 1 (0.44) | 10 (4.41) | |
| Buccal | 2 (0.88) | 0 (0.00) | 2 (0.88) | 0 (0.00) | 4 (1.76) | |
| Pearson χ2 (1) = 7.2211 Pr = 0.007 | ||||||
| Root filling estension | ||||||
| Underfilled | 67 (29.52) | 18 (7.93) | 5 (2.20) | 24 (10.57) | 114 (50.22) | |
| Overfilled | 24 (10.57) | 6 (2.64) | 1 (0.44) | 2 (0.88) | 33 (14.54) | |
| Adequate | 37 (16.30) | 2 (0.88) | 1 (0.44) | 0 (0.00) | 40 (17.62) | |
| Unfilled | 20 (8.81) | 6 (2.64) | 4 (1.76) | 10 (4.41) | 40 (17.62) | |
| Pearson χ2 (6) = 23.7269 Pr = 0.001 | ||||||
Values are presented as number (%).
Procedural errors according to the presence of calcifications
| Procedural errors | Calcification | |||
|---|---|---|---|---|
| Yes | No | Total | ||
| Perforation direction | ||||
| Without perforation | 8 (3.52) | 75 (33.04) | 83 (36.56) | |
| Buccal | 3 (1.32) | 51 (22.47) | 54 (23.79) | |
| Distal | 3 (1.32) | 24 (10.57) | 27 (11.89) | |
| Mesial | 2 (0.88) | 37 (16.30) | 39 (17.18) | |
| Palatal | 2 (0.88) | 22 (9.69) | 24 (10.57) | |
| Pearson χ2 (1) = 0.5235 Pr = 0.469 | ||||
| Root canal transportation | ||||
| No transport | 9 (3.96) | 62 (27.31) | 71 (31.28) | |
| Buccal | 3 (1.32) | 61 (26.87) | 64 (28.19) | |
| Distal | 1 (0.44) | 23 (10.13) | 24 (10.57) | |
| Mesial | 1 (0.44) | 41 (18.06) | 42 (18.50) | |
| Palatal | 4 (1.76) | 22 (9.69) | 26 (11.45) | |
| Pearson χ2 (1) = 3.1882 Pr = 0.074 | ||||
| Instrument fracture | ||||
| Unfractured | 18 (7.93) | 205 (90.31) | 223 (98.24) | |
| Middle third | 0 (0.00) | 4 (1.76) | 4 (1.76) | |
| Fisher's exact = 1.000/1-sided Fisher's exact = 0.717 | ||||
| Missed canals | ||||
| No missed canal | 7 (3.08) | 183 (80.62) | 190 (83.70) | |
| Single canal | 1 (0.44) | 0 (0.00) | 1 (0.44) | |
| Mesiobuccal | 1 (0.44) | 5 (2.20) | 6 (2.64) | |
| Mesiolingual | 1 (0.44) | 1 (0.44) | 2 (0.88) | |
| MB2 | 6 (2.64) | 3 (1.32) | 9 (3.96) | |
| Distobuccal | 0 (0.00) | 5 (2.20) | 5 (2.20) | |
| Palatal | 1 (0.44) | 9 (3.96) | 10 (4.41) | |
| Buccal | 1 (0.44) | 3 (1.32) | 4 (1.76) | |
| Pearson χ2 (1) = 28.7759 Pr = 0.000 | ||||
| Root filling extension | ||||
| Underfilled | 5 (2.20) | 109 (48.02) | 114 (50.22) | |
| Overfilled | 2 (0.88) | 31 (13.66) | 33 (14.54) | |
| Adequate | 1 (0.44) | 39 (17.18) | 40 (17.62) | |
| Unfilled | 10 (4.41) | 30 (13.22) | 40 (17.62) | |
| Pearson χ2 (3) = 19.6993 Pr = 0.000 | ||||
Values are presented as number (%).
Endodontic procedure errors according to the presence of periapical reaction
| Procedural errors | Periapical reaction | |||
|---|---|---|---|---|
| Presence | Absence | Total | ||
| Fenestration direction | ||||
| Without perforation | 67 (29.52) | 16 (7.05) | 83 (36.56) | |
| Buccal | 40 (17.62) | 14 (6.17) | 54 (23.79) | |
| Distal | 26 (11.45) | 1 (0.44) | 27 (11.89) | |
| Mesial | 32 (14.10) | 7 (3.08) | 39 (17.18) | |
| Palatal | 11 (4.85) | 13 (5.73) | 24 (10.57) | |
| Pearson χ2 (4) = 20.6146 Pr = 0.000 | ||||
| Root canal transportation | ||||
| No transport | 56 (24.67) | 15 (6.61) | 71 (31.28) | |
| Buccal | 51 (22.47) | 13 (5.73) | 64 (28.19) | |
| Distal | 23 (10.13) | 1 (0.44) | 24 (10.57) | |
| Mesial | 34 (14.98) | 8 (3.52) | 42 (18.50) | |
| Palatal | 12 (5.29) | 14 (6.17) | 26 (11.45) | |
| Pearson χ2 (4) = 19.8368 Pr = 0.001 | ||||
| Instrument fracture level | ||||
| No fracture | 174 (76.65) | 49 (21.59) | 223 (98.24) | |
| Middle third | 2 (0.88) | 2 (0.88) | 4 (1.76) | |
| Fisher's exact = 0.219/1-sided Fisher's exact = 0.219 | ||||
| Omission of root canals | ||||
| No missed canal | 144 (63.44) | 46 (20.26) | 190 (83.70) | |
| Single canal | 0 (0.00) | 1 (0.44) | 1 (0.44) | |
| Mesiobuccal | 6 (2.64) | 0 (0.00) | 6 (2.64) | |
| Mesiolingual | 2 (0.88) | 0 (0.00) | 2 (0.88) | |
| MB2 | 9 (3.96) | 0 (0.00) | 9 (3.96) | |
| Distobuccal | 4 (1.76) | 1 (0.44) | 5 (2.20) | |
| Palatal | 8 (3.52) | 2 (0.88) | 10 (4.41) | |
| Buccal | 3 (1.32) | 1 (0.44) | 4 (1.76) | |
| Pearson χ2 (1) = 2.0343 Pr = 0.154 | ||||
| Root filling quality | ||||
| Underfilled | 89 (39.21) | 25 (11.01) | 114 (50.22) | |
| Overfilled | 25 (11.01) | 8 (3.52) | 33 (14.54) | |
| Adequate level | 27 (11.89) | 13 (5.73) | 40 (17.62) | |
| Unfilled | 35 (15.42) | 5 (2.20) | 40 (17.62) | |
| Pearson χ2 (3) = 4.6713 Pr = 0.198 | ||||
Values are presented as number (%).
Procedural errors according to dental quadrant
| Procedural errors | Dental quadrant | |||||
|---|---|---|---|---|---|---|
| Upper right | Upper left | Lower left | Lower right | Total | ||
| Fenestration direction | ||||||
| Without perforation | 35 (15.42) | 33 (14.54) | 6 (2.64) | 9 (3.96) | 83 (36.56) | |
| Buccal | 16 (7.05) | 28 (12.33) | 1 (0.44) | 9 (3.96) | 54 (23.79) | |
| Distal | 10 (4.41) | 9 (3.96) | 4 (1.76) | 4 (1.76) | 27 (11.89) | |
| Mesial | 11 (4.85) | 17 (7.49) | 7 (3.08) | 4 (1.76) | 39 (17.18) | |
| Palatal | 7 (3.08) | 8 (3.52) | 3 (1.32) | 6 (2.64) | 24 (10.57) | |
| Pearson χ2 (12) = 15.9915 Pr = 0.192 | ||||||
| Root canal transportation | ||||||
| No transport | 27 (11.89) | 28 (12.33) | 5 (2.20) | 11 (4.85) | 71 (31.28) | |
| Buccal | 20 (8.81) | 33 (14.54) | 2 (0.88) | 9 (3.96) | 64 (28.19) | |
| Distal | 10 (4.41) | 7 (3.08) | 4 (1.76) | 3 (1.32) | 24 (10.57) | |
| Mesial | 14 (6.17) | 17 (7.49) | 7 (3.08) | 4 (1.76) | 42 (18.50) | |
| Palatal | 8 (3.52) | 10 (4.41) | 3 (1.32) | 5 (2.20) | 26 (11.45) | |
| Pearson χ2 (12) = 11.7629 Pr = 0.465 | ||||||
| Instrument fracture | ||||||
| Unfractured | 78 (34.36) | 94 (41.41) | 21 (9.25) | 30 (13.22) | 223 (98.24) | |
| Middle third | 1 (0.44) | 1 (0.44) | 0 (0.00) | 2 (0.88) | 4 (1.76) | |
| Fisher's exact = 1.000/1-sided Fisher's exact = 0.566 | ||||||
| Missed canals | ||||||
| Single canal | 61 (26.87) | 81 (35.68) | 19 (8.37) | 29 (12.78) | 190 (83.70) | |
| Mesiobuccal | 0 (0.00) | 1 (0.44) | 0 (0.00) | 0 (0.00) | 1 (0.44) | |
| Mesiolingual | 3 (1.32) | 1 (0.44) | 1 (0.44) | 1 (0.44) | 6 (2.64) | |
| MB2 | 0 (0.00) | 0 (0.00) | 0 (0.00) | 2 (0.88) | 2 (0.88) | |
| Distobuccal | 5 (2.20) | 4 (1.76) | 0 (0.00) | 0 (0.00) | 9 (3.96) | |
| Palatal | 3 (1.32) | 1 (0.44) | 1 (0.44) | 0 (0.00) | 5 (2.20) | |
| Buccal | 6 (2.64) | 4 (1.76) | 0 (0.00) | 0 (0.00) | 10 (4.41) | |
| Single canal | 1 (0.44) | 3 (1.32) | 0 (0.00) | 0 (0.00) | 4 (1.76) | |
| Fisher's exact = 0.266 | ||||||
| Root filling extension | ||||||
| Underfilled | 43 (18.94) | 42 (18.50) | 13 (5.73) | 16 (7.05) | 114 (50.22) | |
| Overfilled | 10 (4.41) | 20 (8.81) | 0 (0.00) | 3 (1.32) | 33 (14.54) | |
| Adequate | 10 (4.41) | 19 (8.37) | 6 (2.64) | 5 (2.20) | 40 (17.62) | |
| Unfilled | 16 (7.05) | 14 (6.17) | 2 (0.88) | 8 (3.52) | 40 (17.62) | |
| Pearson χ2 (9) = 13.5785 Pr = 0.138 | ||||||
Values are presented as number (%).
Values are presented as number (%).
Values are presented as number (%).
Values are presented as number (%).
Values are presented as number (%).
Values are presented as number (%).
Values are presented as number (%).

 KACD
KACD
 ePub Link
ePub Link Cite
Cite

