Articles
- Page Path
- HOME > Restor Dent Endod > Volume 47(4); 2022 > Article
- Review Article Influence of the root canal filling technique on the success rate of primary endodontic treatments: a systematic review
-
Daniel Feijolo Marconi1
 , Giovana Siocheta da Silva1
, Giovana Siocheta da Silva1 , Theodoro Weissheimer1
, Theodoro Weissheimer1 , Isadora Ames Silva1
, Isadora Ames Silva1 , Gabriel Barcelos Só1
, Gabriel Barcelos Só1 , Leonardo Thomasi Jahnke1
, Leonardo Thomasi Jahnke1 , Jovito Adiel Skupien2
, Jovito Adiel Skupien2 , Marcus Vinicius Reis Só1
, Marcus Vinicius Reis Só1 , Ricardo Abreu da Rosa1
, Ricardo Abreu da Rosa1
-
Restor Dent Endod 2022;47(4):e40.
DOI: https://doi.org/10.5395/rde.2022.47.e40
Published online: October 11, 2022
1Department of Conservative Dentistry, School of Dentistry, Federal University of Rio Grande do Sul (UFRGS), Porto Alegre, RS, Brazil.
2Health and Life Sciences Master’s and Dental School, Franciscan University (UFN), Santa Maria, RS, Brazil.
- Correspondence to Theodoro Weissheimer, DDS, MSc. Department of Conservative Dentistry, Federal University of Rio Grande do Sul - UFRGS, 2492 Ramiro Barcelos Street, Porto Alegre, RS 90035-003, Brazil. theodoro.theo@hotmail.com
Copyright © 2022. The Korean Academy of Conservative Dentistry
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Objectives This study aimed to investigate the influence of different obturation techniques compared to cold lateral compaction on the success rate of primary non-surgical endodontic treatments.
-
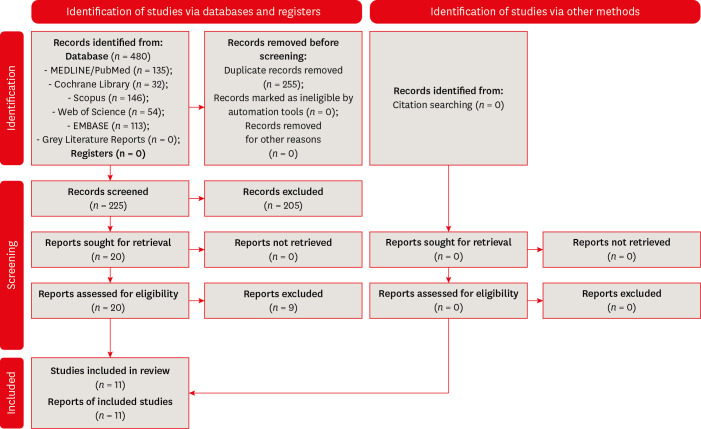
Materials and Methods Systematic searches were performed for studies published up to May 17th, 2022 in MEDLINE/PubMed, Cochrane Library, Web of Science, Scopus, EMBASE, and Grey Literature Reports. Randomized clinical trials and nonrandomized (nonrandomized clinical trials, prospective or retrospective) studies that evaluated the success rate of primary non-surgical endodontic treatments obturated with the cold lateral compaction (control) and other obturation techniques were included. The revised Cochrane risk of bias tools for randomized trials (RoB 2) and nonrandomized studies of interventions (ROBINS-I) were used to evaluate the risk of bias. The Grading of Recommendations Assessment, Development, and Evaluation (GRADE) tool was used to evaluate the certainty of evidence.
-
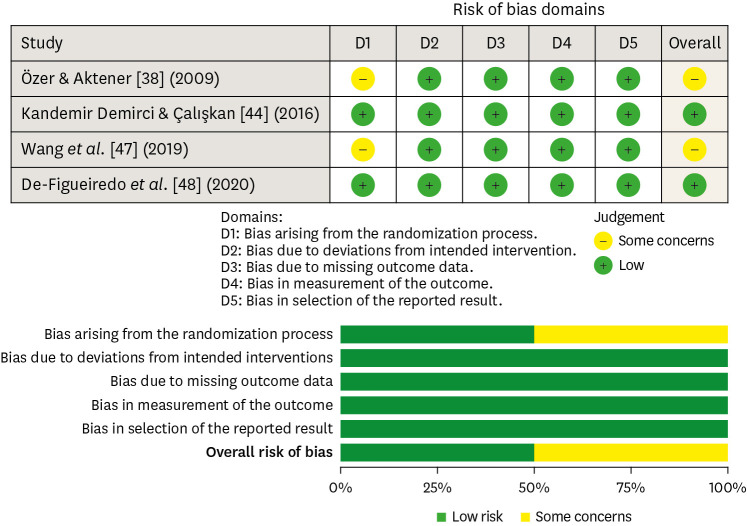
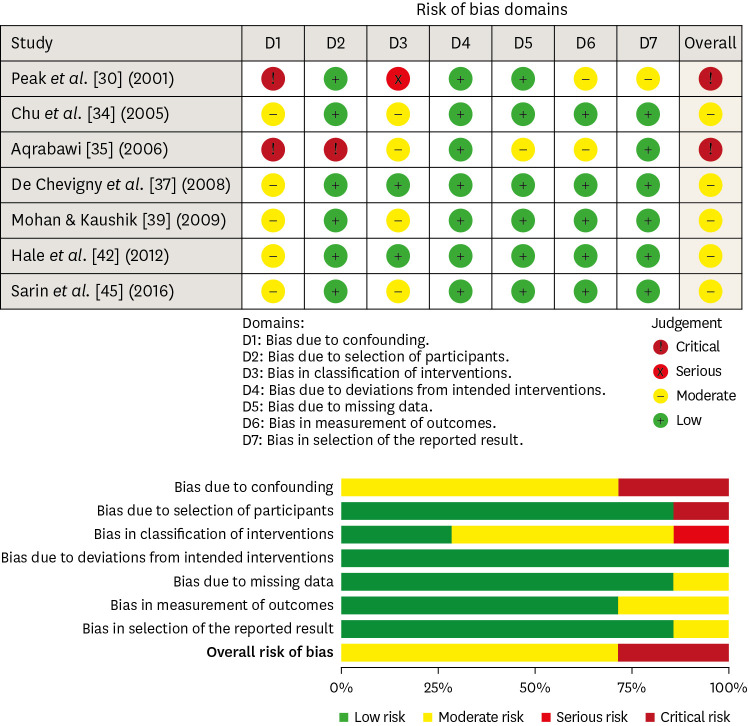
Results Eleven studies (4 randomized clinical trials (RCTs), 4 prospective, and 3 retrospectives) were included. Two RCTs were classified as having some concerns risk of bias and 2 as a low risk of bias. Two nonrandomized studies were classified as having a critical risk of bias and 5 as having a moderate risk of bias. The GRADE analysis demonstrated a very low to moderate certainty of evidence.
-
Conclusions This systematic review generally evidenced no differences in the success rate of primary non-surgical endodontic treatments when the cold lateral compaction technique and other obturation techniques are performed. Further well-designed studies are still necessary.
INTRODUCTION
MATERIALS AND METHODS
• Population (P) – adult patients undergoing primary non-surgical endodontic treatment;
• Intervention (I) – different obturation techniques;
• Comparison (C) – cold lateral compaction technique;
• Outcome (O) – clinical and radiographic success rate;
• Study design (S) – randomized clinical trials, nonrandomized clinical trials, and longitudinal (prospective and retrospective) studies.
1. Data extraction
2. Risk of bias analysis
1) Confounding factors: ‘Low’ risk of bias was considered when all possible confounding factors were checked in the design or the statistical analysis. ‘Moderate’ risk of bias when some possible confounding factors were controlled. ‘Serious’ risk of bias when no possible confounding factors were controlled. ‘Critical’ risk of bias when possible confounding factors were not even discussed.
2) Selection of participants: ‘Low’ risk of bias was considered when all eligible participants were included in the study. ‘Moderate’ risk of bias when the participant selection may have been related to intervention/outcome. ‘Serious’ risk of bias when participant selection was related to intervention/outcome. ‘Critical’ risk of bias when the selection process was not described.
3) Classification of interventions: ‘Low’ risk of bias was considered when the chemo-mechanical preparation and obturation techniques were well described. ‘Moderate’ risk of bias when the chemo-mechanical preparation and obturation techniques presented some missing information, but the missing data were not relevant to the purpose of the included study. ‘Serious’ risk of bias when the chemo-mechanical preparation and obturation techniques were not well described. ‘Critical’ risk of bias when the chemo-mechanical preparation and obturation techniques were not described.
4) Deviations from intended interventions: ‘Low’ risk of bias was considered when no differences occurred after the beginning of the study, or differences in one or both groups occurred after the beginning of the study, but the participant continued (for analysis purposes) to be part of the study. ‘Moderate’ risk of bias when differences occurred after the beginning of the study, but it does not seem to affect its outcome. ‘Serious’ risk of bias when few differences occurred after the beginning of the study and changes in the sample or intervention were required. ‘Critical’ risk of bias when several differences occurred after the beginning of the study.
5) Missing data: ‘Low’ risk of bias was considered when the number of teeth evaluated per group, type of teeth, preparation technique, number of visits, obturation technique, follow-up time, and parameters evaluated to determine success were well reported. ‘Moderate’ risk of bias when there were some missing data, but the missing data were not relevant to the purpose of the included study. ‘Serious’ risk of bias when there were some relevant missing data. ‘Critical’ risk of bias when there were several relevant missing data
6) Measurement of outcomes: ‘Low’ risk of bias was considered when valid parameters (clinical and radiographic) were used to determine success. ‘Moderate’ risk of bias when using a valid methodology, but the methodology was not well described. ‘Serious’ risk of bias when a valid methodology was not used, but the methodology was well described. ‘Critical’ risk of bias when a valid methodology was not used, not well described, or the methodology used was not described.
7) Selection of described results: ‘Low’ risk of bias was considered when all results were presented. ‘Moderate’ risk of bias when results were reported but not well described. ‘Serious’ risk of bias when there was a substantial difference in the description of the results of each intervention. ‘Critical’ risk of bias when information is not presented.
3. Certainty of evidence
RESULTS
Characteristics of the included studies
| Authors (year of publication) – study design | Number of teeth evaluated (per group) | Teeth evaluated | Diagnosis | Preparation technique | Number of visits | Obturation technique | Follow-up time | Parameters evaluated to determine success | Main findings |
|---|---|---|---|---|---|---|---|---|---|
| Peak et al. [30] (2001) – Retrospective | n = 406 (cold lateral compaction – n = 258; Single-cone technique – n = 85; Silver/titanium points technique – n = 76; Endomethasone only - n = 19) | Maxillary and mandibular anterior and posterior teeth | Necrotic teeth | NR | NR | Cold lateral compaction – sealer not reported; single-cone technique – sealer not reported; silver/titanium point technique – sealer not reported; Endomethasone only | 3 yr or more | No clinical signs or symptoms; no radiographic evidence of pathology | Success rate: |
| cold lateral compaction: 92%; single-cone technique: 68%; silver/titanium points technique: 73%; Endomethasone only: 89%; cold lateral compaction technique shown higher success rates than the other techniques; single-cone and silver/titanium points techniques were associated with a high failure rate in cases within 3 yr | |||||||||
| Chu et al. [34] (2005) – Prospective | n = 71 (cold lateral compaction – n = 34; carrier-based obturation – n = 37) | Maxillary and mandibular anterior and posterior teeth | Necrotic teeth | K-files + 5% NaOCl | Two visits or more (with calcium hydroxide paste or an antibiotic-corticosteroid paste) | Carrier-based obturation (Thermafil) + AH 26; cold lateral compaction + AH 26 | 3–4 yr | Tooth clinically sound and radiographic normal appearance of the surrounding bone structure | Success rate: |
| cold lateral compaction: 79%; carrier-based obturation: 81%; there was no difference in the success rate between the investigated techniques | |||||||||
| Aqrabawi [35] (2006) – Prospective | n = 340 (cold lateral compaction – n = 160; warm vertical compaction – n = 180) | NR | Necrotic teeth | NR | NR | Cold lateral compaction + AH26 sealer; warm vertical compaction + Kerr pulp canal sealer | 5 yr | Strindberg’s criteria; PAI ≤ 2 | Success rate: |
| cold lateral compaction: 79%; warm vertical compaction: 82%; there were no differences between techniques; a significantly higher success rate was observed for the warm vertical compaction in teeth presenting radiographically visible periapical lesions | |||||||||
| De Chevigny et al. [37] (2008) – Prospective* | n = 1,952 (cold lateral compaction – n = 820; warm vertical compaction – n = 1,074; single-cone technique or injectable gutta-percha – n = 58) | Maxillary and mandibular anterior and posterior teeth | Vital and necrotic teeth | Hand files and engine-drive nickel titanium instruments + 2.5% NaOCl and, occasionally, 2% chlorhexidine | One visit or more (with calcium hydroxide paste) | Cold lateral compaction – sealer not reported; warm vertical compaction – sealer not reported; single-cone technique + glass ionomer sealer or injectable gutta-percha | 4–6 yr | PAI ≤ 2; no clinical signs or symptoms | Success rate: |
| cold lateral compaction: 77%; warm vertical compaction: 87%; single cone technique or injectable gutta-percha: NR; warm vertical compaction was associated with a significant better outcome | |||||||||
| Mohan & Kaushik [39] (2009) – Prospective | n = 100 (cold lateral compaction – n = 50; carrier-based obturation – n = 50) | Maxillary incisors and mandibular molars | Vital and necrotic teeth | NR | NR | Cold lateral compaction + AH-26; carrier-based obturation + AH-26 | 1 yr | No clinical signs or symptoms; no radiographic evidence of pathology | Success rate: |
| cold lateral compaction: 90%; carrier-based obturation: 96%; there was no difference in the success rate between the investigated techniques | |||||||||
| Özer & Aktener [38] (2009) – RCT | n = 98 (cold lateral compaction – n = 49; carrier-based obturation – n = 49) | Mandibular first and second molars | Necrotic teeth | Quantec LX + NR | NR | Cold lateral compaction + Diaket; carrier-based obturation (Soft-Core) + Diaket | 3 yr | No clinical signs or symptoms; no radiographic evidence of pathology | Success rate: |
| cold lateral compaction: 80%; carrier-based obturation: 85%; there was no difference in the success rate between the investigated techniques | |||||||||
| Hale et al. [42] (2012) – Retrospective | n = 71 (cold lateral compaction – n = 36; carrier-based obturation – n = 35) | Maxillary and mandibular anterior and posterior teeth | Vital and necrotic teeth | ProFile rotary instrument + 3% NaOCl | One visit or more (with calcium hydroxide paste) | Cold lateral compaction + AH Plus; carrier-based obturation + AH Plus | 18–37 mon | No clinical signs or symptoms; no radiographic evidence of pathology or reduction of lesion’ size | Success rate: |
| cold lateral compaction: 81%; carrier-based obturation: 83%; there was no difference in the success rate between the investigated techniques | |||||||||
| Kandemir Demirci & Çalışkan [44] (2016) – RCT | n = 120 (cold lateral compaction – n = 60; carrier-based obturation – n = 60) | Maxillary anterior teeth | Necrotic teeth | Hand files + 2.5% NaOCl | Two-visits (with calcium hydroxide paste) | Cold lateral compaction + AH Plus; carrier-based obturation (Thermafill) + AH Plus | 2 yr | PAI ≤ 2; no clinical signs or symptoms | Success rate: |
| cold lateral compaction: 98.2%; carrier-based obturation: 96.4%; there was no difference in the success rate between the investigated techniques | |||||||||
| Sarin et al. [45] (2016) – Retrospective | n = 140 (cold lateral compaction – n = 70; carrier-based obturation – n = 70) | Anterior and posterior teeth | Vital and necrotic teeth | NR | NR | Cold lateral compaction + Apexit Plus; carrier-based obturation + Apexit Plus | 18–38 mon | Absence of hard or soft tissue pathology | Success rate: |
| cold lateral compaction: 80%; carrier-based obturation: 83%; there was no difference in the success rate between the investigated techniques | |||||||||
| Wang et al. [47] (2019) – RCT | n = 127 (cold lateral compaction – n = 60; warm vertical compaction – n = 67) | Anterior and posterior teeth | Vital and necrotic teeth | NiTi rotary instruments + 1% NaOCl and 2% CHX before gutta-percha insertion | NR | Cold lateral compaction – sealer not specified; warm vertical compaction – sealer not specified | 2 mon | No clinical signs or symptoms; no radiographic evidence of pathology | Success rate: |
| cold lateral compaction: 70.9%; warm vertical compaction: 98.2%; warm vertical compaction had a significantly improved success rate | |||||||||
| De-Figueiredo et al. [48] (2020) – RCT | n = 87 (cold lateral compaction – n = 42; single-cone technique – n = 45) | Maxillary and mandibular anterior teeth | Necrotic teeth | Hand files + 2.5% NaOCl; Reciproc + 2.5% NaOCl | One visit | Cold lateral compaction + AH Plus; single-cone + AH Plus | 1 yr | PAI ≤ 2; no clinical signs or symptoms | Success rate: |
| cold lateral compaction: 73%; single-cone technique: 78%; there was no difference in the success rate between the investigated techniques |
Quality assessment of the randomized clinical trials, according to the Cochrane Collaboration standard scheme for bias and RoB2 tool.
Quality assessment of the nonrandomized studies, according to the Cochrane Collaboration standard scheme for bias and ROBINS- I tool.
Certainty of the evidence of the included studies
DISCUSSION
CONCLUSION
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Marconi DF, Weissheimer T, da Rosa RA.
Data Curation: Marconi DF, da Silva GS, Weissheimer T.
Formal Analysis: Marconi DF, da Silva GS, Weissheimer T.
Investigation: Marconi DF, da Silva GS.
Methodology: Weissheimer T, Skupien JA, Só MVR, da Rosa RA.
Project administration: Weissheimer T, Skupien JA, Só MVR, da Rosa RA.
Supervision: Skupien JA, Só MVR, da Rosa RA.
Writing - original draft: Marconi DF, da Silva GS, Weissheimer T.
Writing - review & editing: Jahnke LT, Silva IS, Só GB, Skupien JA, da Rosa RA.
SUPPLEMENTARY MATERIAL
- 1. Olcay K, Ataoglu H, Belli S. evaluation of related factors in the failure of endodontically treated teeth: a cross-sectional study. J Endod 2018;44:38-45.ArticlePubMed
- 2. Chugal NM, Clive JM, Spångberg LS. Endodontic infection: some biologic and treatment factors associated with outcome. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003;96:81-90.ArticlePubMed
- 3. Kim S, Jung H, Kim S, Shin SJ, Kim E. The influence of an isthmus on the outcomes of surgically treated molars: a retrospective study. J Endod 2016;42:1029-1034.ArticlePubMed
- 4. Chybowski EA, Glickman GN, Patel Y, Fleury A, Solomon E, He J. Clinical outcome of non-surgical root canal treatment using a single-cone technique with Endosequence Bioceramic Sealer: a retrospective analysis. J Endod 2018;44:941-945.ArticlePubMed
- 5. Ng YL, Mann V, Rahbaran S, Lewsey J, Gulabivala K. Outcome of primary root canal treatment: systematic review of the literature -- Part 2. Influence of clinical factors. Int Endod J 2008;41:6-31.ArticlePubMed
- 6. Torabinejad M, Corr R, Handysides R, Shabahang S. Outcomes of nonsurgical retreatment and endodontic surgery: a systematic review. J Endod 2009;35:930-937.ArticlePubMed
- 7. Levitan ME, Himel VT, Luckey JB. The effect of insertion rates on fill length and adaptation of a thermoplasticized gutta-percha technique. J Endod 2003;29:505-508.ArticlePubMed
- 8. Naseri M, Kangarlou A, Khavid A, Goodini M. Evaluation of the quality of four root canal obturation techniques using micro-computed tomography. Iran Endod J 2013;8:89-93.PubMedPMC
- 9. Keleş A, Alcin H, Kamalak A, Versiani MA. Micro-CT evaluation of root filling quality in oval-shaped canals. Int Endod J 2014;47:1177-1184.PubMed
- 10. Li GH, Niu LN, Selem LC, Eid AA, Bergeron BE, Chen JH, Pashley DH, Tay FR. Quality of obturation achieved by an endodontic core-carrier system with crosslinked gutta-percha carrier in single-rooted canals. J Dent 2014;42:1124-1134.ArticlePubMedPMC
- 11. Nhata J, Machado R, Vansan LP, Batista A, Sidney G, Rosa TP, Leal Silva EJ. Micro-computed tomography and bond strength analysis of different root canal filling techniques. Indian J Dent Res 2014;25:698-701.ArticlePubMed
- 12. Selem LC, Li GH, Niu LN, Bergeron BE, Bortoluzzi EA, Chen JH, Pashley DH, Tay FR. Quality of obturation achieved by a non-gutta-percha-based root filling system in single-rooted canals. J Endod 2014;40:2003-2008.ArticlePubMed
- 13. Moinzadeh AT, Zerbst W, Boutsioukis C, Shemesh H, Zaslansky P. Porosity distribution in root canals filled with gutta percha and calcium silicate cement. Dent Mater 2015;31:1100-1108.ArticlePubMed
- 14. Ho ES, Chang JW, Cheung GS. Quality of root canal fillings using three gutta-percha obturation techniques. Restor Dent Endod 2016;41:22-28.ArticlePubMedPMCPDF
- 15. Jaworska M, Kierklo A. Use of microcomputed tomography for the evaluation of canal filling quality depending on the part of root canal. J Stomatol 2016;69:638-646.Article
- 16. Schilder H. Filling root canals in three dimensions. 1967. J Endod 2006;32:281-290.PubMed
- 17. Zhang W, Liu H, Wang Z, Haapasalo M, Jiang Q, Shen Y. Long-term porosity and retreatability of oval-shaped canals obturated using two different methods with a novel tricalcium silicate sealer. Clin Oral Investig 2022;26:1045-1052.ArticlePubMedPDF
- 18. De-Deus G, Reis C, Beznos D, de Abranches AM, Coutinho-Filho T, Paciornik S. Limited ability of three commonly used thermoplasticized gutta-percha techniques in filling oval-shaped canals. J Endod 2008;34:1401-1405.ArticlePubMed
- 19. Peng L, Ye L, Tan H, Zhou X. Outcome of root canal obturation by warm gutta-percha versus cold lateral condensation: a meta-analysis. J Endod 2007;33:106-109.ArticlePubMed
- 20. Whitworth J. Methods of filling root canals: principles and practices. Endod Topics 2005;12:2-24.Article
- 21. Pirani C, Camilleri J. Effectiveness of root canal filling materials and techniques for treatment of apical periodontitis: a systematic review. Int Endod J 2022;Jun 23 [Epub].ArticlePDF
- 22. Aminosharie A, Johnson WT, Kulild JC, Tay F. Chapter 9: Cohen’s pathways of the pulp. 12th ed. St. Louis, MO: Mosby Elsevier; 2020.
- 23. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann T, Mulrow CD, Shamseer L, Moher D. Mapping of reporting guidance for systematic reviews and meta-analyses generated a comprehensive item bank for future reporting guidelines. J Clin Epidemiol 2020;118:60-68.ArticlePubMed
- 24. Maia LC, Antonio AG. Systematic reviews in dental research. A guideline. J Clin Pediatr Dent 2012;37:117-124.ArticlePubMedPDF
- 25. Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA. PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015;4:1.PubMedPMC
- 26. Page MJ, Higgins JP, Sterne JA. Chapter 13: Assessing risk of bias due to missing results in a synthesis. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane handbook for systematic reviews of interventions version 6.2. Chichester: John Wiley & Sons; 2019.
- 27. Sterne JA, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng HY, Corbett MS, Eldridge SM, Emberson JR, Hernán MA, Hopewell S, Hróbjartsson A, Junqueira DR, Jüni P, Kirkham JJ, Lasserson T, Li T, McAleenan A, Reeves BC, Shepperd S, Shrier I, Stewart LA, Tilling K, White IR, Whiting PF, Higgins JP. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898.ArticlePubMed
- 28. Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan AW, Churchill R, Deeks JJ, Hróbjartsson A, Kirkham J, Jüni P, Loke YK, Pigott TD, Ramsay CR, Regidor D, Rothstein HR, Sandhu L, Santaguida PL, Schünemann HJ, Shea B, Shrier I, Tugwell P, Turner L, Valentine JC, Waddington H, Waters E, Wells GA, Whiting PF, Higgins JP. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355:i4919.ArticlePubMedPMC
- 29. Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, Norris S, Falck-Ytter Y, Glasziou P, DeBeer H, Jaeschke R, Rind D, Meerpohl J, Dahm P, Schünemann HJ. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 2011;64:383-394.ArticlePubMed
- 30. Peak JD, Hayes SJ, Bryant ST, Dummer PM. The outcome of root canal treatment. A retrospective study within the armed forces (Royal Air Force). Br Dent J 2001;190:140-144.ArticlePubMed
- 31. Friedman S, Abitbol S, Lawrence HP. Treatment outcome in endodontics: the Toronto Study. Phase 1: initial treatment. J Endod 2003;29:787-793.ArticlePubMed
- 32. Farzaneh M, Abitbol S, Lawrence HP, Friedman S. Toronto Study. Treatment outcome in endodontics-the Toronto Study. Phase II: initial treatment. J Endod 2004;30:302-309.ArticlePubMed
- 33. Peters OA, Barbakow F, Peters CI. An analysis of endodontic treatment with three nickel-titanium rotary root canal preparation techniques. Int Endod J 2004;37:849-859.ArticlePubMed
- 34. Chu CH, Lo EC, Cheung GS. Outcome of root canal treatment using Thermafil and cold lateral condensation filling techniques. Int Endod J 2005;38:179-185.ArticlePubMed
- 35. Aqrabawi JA. Outcome of endodontic treatment of teeth filled using lateral condensation versus vertical compaction (Schilder’s technique). J Contemp Dent Pract 2006;7:17-24.Article
- 36. Marquis VL, Dao T, Farzaneh M, Abitbol S, Friedman S. Treatment outcome in endodontics: the Toronto Study. Phase III: initial treatment. J Endod 2006;32:299-306.ArticlePubMed
- 37. de Chevigny C, Dao TT, Basrani BR, Marquis V, Farzaneh M, Abitbol S, Friedman S. Treatment outcome in endodontics: the Toronto study--phase 4: initial treatment. J Endod 2008;34:258-263.ArticlePubMed
- 38. Özer SY, Aktener BO. Outcome of root canal treatment using Soft-Core and cold lateral compaction filling techniques: a randomized clinical trial. J Contemp Dent Pract 2009;10:74-81.Article
- 39. Mohan SM, Kaushik SK. Root canal treatment using thermoplasticized carrier condensation technique. Med J Armed Forces India 2009;65:336-341.ArticlePubMedPMC
- 40. Fleming CH, Litaker MS, Alley LW, Eleazer PD. Comparison of classic endodontic techniques versus contemporary techniques on endodontic treatment success. J Endod 2010;36:414-418.ArticlePubMed
- 41. Prashanth MB, Tavane PN, Abraham S, Chacko L. Comparative evaluation of pain, tenderness and swelling followed by radiographic evaluation of periapical changes at various intervals of time following single and multiple visit endodontic therapy: an in vivo study. J Contemp Dent Pract 2011;12:187-191.ArticlePubMed
- 42. Hale R, Gatti R, Glickman GN, Opperman LA. Comparative analysis of carrier-based obturation and lateral compaction: a retrospective clinical outcomes study. Int J Dent 2012;2012:954675.ArticlePubMedPMCPDF
- 43. Krug R, Krastl G, Jahreis M. Technical quality of a matching-taper single-cone filling technique following rotary instrumentation compared with lateral compaction after manual preparation: a retrospective study. Clin Oral Investig 2017;21:643-652.ArticlePubMedPDF
- 44. Kandemir Demirci G, Çalışkan MK. A prospective randomized comparative study of cold lateral condensation versus core/gutta-percha in teeth with periapical lesions. J Endod 2016;42:206-210.ArticlePubMed
- 45. Sarin A, Gupta P, Sachdeva J, Gupta A, Sachdeva S, Nagpal R. Effect of different obturation techniques on the prognosis of endodontic therapy: a retrospective comparative analysis. J Contemp Dent Pract 2016;17:582-586.ArticlePubMed
- 46. de Figueiredo FE, Lima LF, Oliveira LS, Ribeiro MA, Correa MB, Brito-Junior M, Faria-E-Silva AL. Effectiveness of a reciprocating single file, single cone endodontic treatment approach: a randomized controlled pragmatic clinical trial. Clin Oral Investig 2020;24:2247-2257.ArticlePubMedPDF
- 47. Wang J, Du Y, Deng J, Wang X, He J. Efficacy of warm gutta-percha root canal filling in the treatment of dental pulpal and periapical diseases. Int J Clin Exp 2019;12:2738-2745.
- 48. de-Figueiredo FE, Lima LF, Lima GS, Oliveira LS, Ribeiro MA, Brito-Junior M, Correa MB, Sousa-Neto MD, Faria E Silva AL, Silva AL. Apical periodontitis healing and postoperative pain following endodontic treatment with a reciprocating single-file, single-cone approach: a randomized controlled pragmatic clinical trial. PLoS One 2020;15:e0227347.ArticlePubMedPMC
- 49. Swathi UB, Ramesh S, Antony DP. Comparative analysis of various obturation techniques in mandibular molars - a retrospective clinical outcome study. Int J Pharm Sci Res 2020;11(SPL3):172-178.ArticlePDF
- 50. McGuinness LA, Higgins JP. Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods 2021;12:55-61.ArticlePubMedPDF
- 51. Young GR, Parashos P, Messer HH. The principles of techniques for cleaning root canals. Aust Dent J 2007;52(Suppl):S52-S63.ArticlePubMed
- 52. Ricucci D, Siqueira JF Jr. Fate of the tissue in lateral canals and apical ramifications in response to pathologic conditions and treatment procedures. J Endod 2010;36:1-15.ArticlePubMed
- 53. American Association of Endodontists. Guide to clinical endodontics. Chicago, IL: American Association of Endodontists; 2013.
- 54. European Society of Endodontology. Quality guidelines for endodontic treatment: consensus report of the European Society of Endodontology. Int Endod J 2006;39:921-930.ArticlePubMed
- 55. Ørstavik D, Nordahl I, Tibballs JE. Dimensional change following setting of root canal sealer materials. Dent Mater 2001;17:512-519.ArticlePubMed
- 56. Sjogren U, Hagglund B, Sundqvist G, Wing K. Factors affecting the long-term results of endodontic treatment. J Endod 1990;16:498-504.ArticlePubMed
- 57. Azim AA, Griggs JA, Huang GT. The Tennessee study: factors affecting treatment outcome and healing time following nonsurgical root canal treatment. Int Endod J 2016;49:6-16.ArticlePubMed
- 58. Friedman S, Mor C. The success of endodontic therapy--healing and functionality. J Calif Dent Assoc 2004;32:493-503.ArticlePubMed
- 59. Orstavik D, Kerekes K, Eriksen HM. The periapical index: a scoring system for radiographic assessment of apical periodontitis. Endod Dent Traumatol 1986;2:20-34.ArticlePubMed
- 60. Strindberg LZ. The dependence of the results of pulp therapy on certain factors—An analytical study based on radiographic and clinical follow-up examination. Acta Odontol Scand 1956;14:1-175.
- 61. Siqueira JF Jr, Rôças IN, Favieri A, Lima KC. Chemomechanical reduction of the bacterial population in the root canal after instrumentation and irrigation with 1%, 2.5%, and 5.25% sodium hypochlorite. J Endod 2000;26:331-334.ArticlePubMed
- 62. Ulin C, Magunacelaya-Barria M, Dahlén G, Kvist T. Immediate clinical and microbiological evaluation of the effectiveness of 0.5% versus 3% sodium hypochlorite in root canal treatment: a quasi-randomized controlled trial. Int Endod J 2020;53:591-603.ArticlePubMedPDF
- 63. Gazzaneo I, Vieira GC, Pérez AR, Alves FR, Gonçalves LS, Mdala I, Siqueira JF Jr, Rôças IN. Root canal disinfection by single- and multiple-instrument systems: effects of sodium hypochlorite volume, concentration, and retention time. J Endod 2019;45:736-741.ArticlePubMed
- 64. Petridis X, Busanello FH, So MV, Dijkstra RJ, Sharma PK, van der Sluis LW. Factors affecting the chemical efficacy of 2% sodium hypochlorite against oral steady-state dual-species biofilms: exposure time and volume application. Int Endod J 2019;52:1182-1195.ArticlePubMedPMCPDF
- 65. Moreira MS, Anuar AS, Tedesco TK, Dos Santos M, Morimoto S. Endodontic treatment in single and multiple visits: an overview of systematic reviews. J Endod 2017;43:864-870.ArticlePubMed
- 66. Skelly AC, Dettori JR, Brodt ED. Assessing bias: the importance of considering confounding. Evid Based Spine Care J 2012;3:9-12.Article
- 67. Guyatt GH, Oxman AD, Vist G, Kunz R, Brozek J, Alonso-Coello P, Montori V, Akl EA, Djulbegovic B, Falck-Ytter Y, Norris SL, Williams JW Jr, Atkins D, Meerpohl J, Schünemann HJ. GRADE guidelines: 4. Rating the quality of evidence--study limitations (risk of bias). J Clin Epidemiol 2011;64:407-415.ArticlePubMed
- 68. Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, Alonso-Coello P, Glasziou P, Jaeschke R, Akl EA, Norris S, Vist G, Dahm P, Shukla VK, Higgins J, Falck-Ytter Y, Schünemann HJ. GRADE Working Group. GRADE guidelines: 7. Rating the quality of evidence--inconsistency. J Clin Epidemiol 2011;64:1294-1302.ArticlePubMed
- 69. Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, Alonso-Coello P, Falck-Ytter Y, Jaeschke R, Vist G, Akl EA, Post PN, Norris S, Meerpohl J, Shukla VK, Nasser M, Schünemann HJ. GRADE Working Group. GRADE guidelines: 8. Rating the quality of evidence--indirectness. J Clin Epidemiol 2011;64:1303-1310.ArticlePubMed
- 70. Murad MH, Mustafa RA, Schünemann HJ, Sultan S, Santesso N. Rating the certainty in evidence in the absence of a single estimate of effect. Evid Based Med 2017;22:85-87.ArticlePubMedPMC
- 71. Guyatt GH, Oxman AD, Sultan S, Glasziou P, Akl EA, Alonso-Coello P, Atkins D, Kunz R, Brozek J, Montori V, Jaeschke R, Rind D, Dahm P, Meerpohl J, Vist G, Berliner E, Norris S, Falck-Ytter Y, Murad MH, Schünemann HJ. GRADE Working Group. GRADE guidelines: 9. Rating up the quality of evidence. J Clin Epidemiol 2011;64:1311-1316.ArticlePubMed
- 72. Ackley BJ, Swan BA, Ladwig G, Tucker S. Evidence-based nursing care guidelines: medical-surgical interventions. 1st ed. St. Louis, MO: Mosby Elsevier; 2008. p. 7.
REFERENCES
Tables & Figures
REFERENCES
Citations

- Assessing Sealing Ability of C-Root SP Strontium Silicate Sealer With Different Obturation Techniques: An in vitro Study
Suixin Hu, Jianshe Li, Meng Xu, Laiqing Xu, Yangming Yin, Peng Xue, Liping Dong, Lin Wang, Huixia He, Ying Liu, Qiang Luo, Fei Chen
International Dental Journal.2026; 76(1): 109283. CrossRef - Comparative Analysis Of Obturation Techniques In Endodontics: Lateral Vs. Thermoplasticized. Thermoplasticized
Juan Esteban Díaz Pacheco , Rómulo Guillermo López Torres , Verónica Alejandra Salame Ortíz
Salud, Ciencia y Tecnología.2025; 5: 1626. CrossRef - Effect of ultrasonic activation of endodontic sealers on root canal filling quality during the single-cone obturation procedure: a systematic review and meta-analysis of laboratory-based studies
Shuting Feng, Weiqing Zhou, Xiaojun Chu, Shuaimei Xu, Xiongqun Zeng
Odontology.2025; 113(4): 1380. CrossRef - In Vitro and In Vivo Evaluation of a New Experimental Polydimethylsiloxane-Based Endodontic Sealer
Fabiola Cardoso Maldonado, Cesar Gaitan Fonseca, Carlos Bermudez Jimenez, Luis Alejandro Aguilera Galaviz, Margarita L. Martinez-Fierro, Lorena Troncoso Vazquez, Martha Eugenia Reyes Ortiz
Journal of Functional Biomaterials.2025; 16(11): 402. CrossRef - Evaluation of three obturation techniques in 3D-printed models of oval canals with standardized prepared morphology: a micro-CT study
Wenjun Xia, Qisheng Gu, Yingshuang Song, Yunjia Liu, Xuetao Deng, Wenhao Qian
BMC Oral Health.2025;[Epub] CrossRef - Clinical and Radiographic Failure of Nonsurgical Endodontic Treatment and Retreatment Using Single-cone Technique With Calcium Silicate-based Sealers: A Systematic Review and Meta-analysis
Mohammad A. Sabeti, Negah Karimpourtalebi, Arash Shahravan, Omid Dianat
Journal of Endodontics.2024; 50(6): 735. CrossRef - Method of microbial decontamination of endodontic absorbent paper points: a randomised experimental study
O. A. Pavlovskaya, O. A. Kachanova, V. V. Volobuev, M. N. Mitropanova, A. R. Gazarova, V. Y. Zobenko, A. G. Uvarova
Pediatric dentistry and dental prophylaxis.2024; 24(2): 157. CrossRef - The Push-Out Bond Strength, Surface Roughness, and Antimicrobial Properties of Endodontic Bioceramic Sealers Supplemented with Silver Nanoparticles
Karla Navarrete-Olvera, Nereyda Niño-Martínez, Idania De Alba-Montero, Nuria Patiño-Marín, Facundo Ruiz, Horacio Bach, Gabriel-Alejandro Martínez-Castañón
Molecules.2024; 29(18): 4422. CrossRef - Clinical outcome of non-surgical root canal treatment using different sealers and techniques of obturation in 237 patients: A retrospective study
Mateusz Radwanski, Krystyna Pietrzycka, Tan Fırat Eyüboğlu, Mutlu Özcan, Monika Lukomska-Szymanska
Clinical Oral Investigations.2024;[Epub] CrossRef
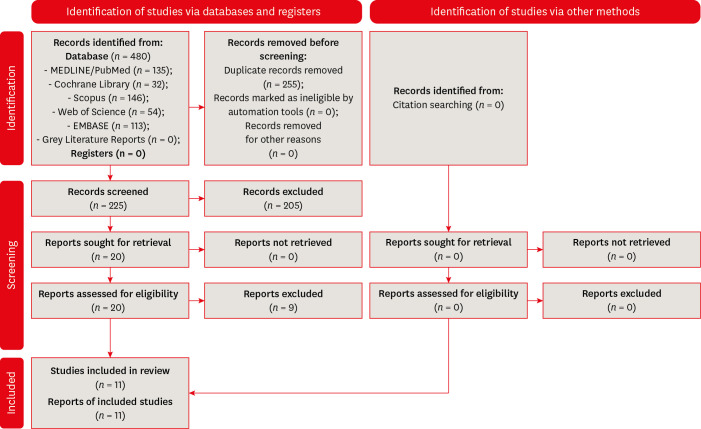
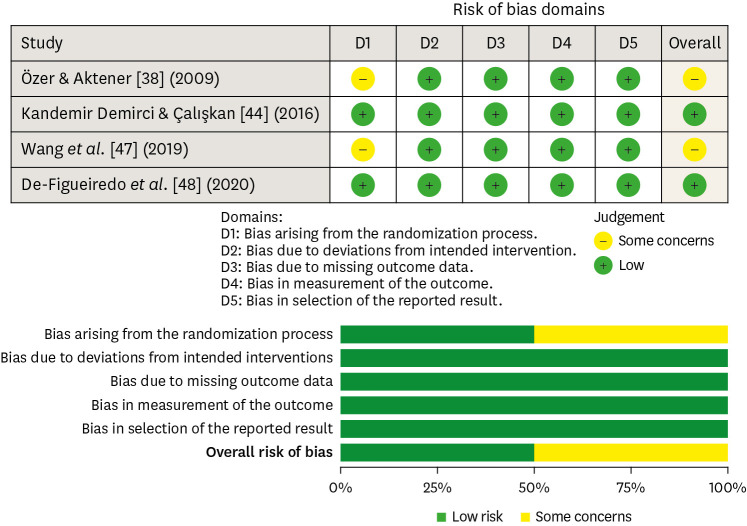
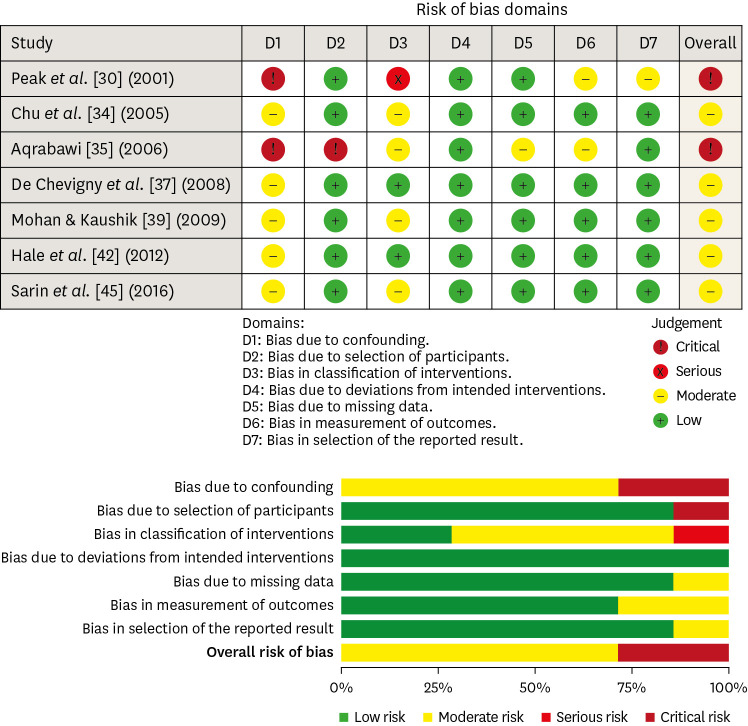
Figure 1
Figure 2
Figure 3
Characteristics of the included studies
| Authors (year of publication) – study design | Number of teeth evaluated (per group) | Teeth evaluated | Diagnosis | Preparation technique | Number of visits | Obturation technique | Follow-up time | Parameters evaluated to determine success | Main findings |
|---|---|---|---|---|---|---|---|---|---|
| Peak | Maxillary and mandibular anterior and posterior teeth | Necrotic teeth | NR | NR | Cold lateral compaction – sealer not reported; single-cone technique – sealer not reported; silver/titanium point technique – sealer not reported; Endomethasone only | 3 yr or more | No clinical signs or symptoms; no radiographic evidence of pathology | Success rate: | |
| cold lateral compaction: 92%; single-cone technique: 68%; silver/titanium points technique: 73%; Endomethasone only: 89%; cold lateral compaction technique shown higher success rates than the other techniques; single-cone and silver/titanium points techniques were associated with a high failure rate in cases within 3 yr | |||||||||
| Chu | Maxillary and mandibular anterior and posterior teeth | Necrotic teeth | K-files + 5% NaOCl | Two visits or more (with calcium hydroxide paste or an antibiotic-corticosteroid paste) | Carrier-based obturation (Thermafil) + AH 26; cold lateral compaction + AH 26 | 3–4 yr | Tooth clinically sound and radiographic normal appearance of the surrounding bone structure | Success rate: | |
| cold lateral compaction: 79%; carrier-based obturation: 81%; there was no difference in the success rate between the investigated techniques | |||||||||
| Aqrabawi [ | NR | Necrotic teeth | NR | NR | Cold lateral compaction + AH26 sealer; warm vertical compaction + Kerr pulp canal sealer | 5 yr | Strindberg’s criteria; PAI ≤ 2 | Success rate: | |
| cold lateral compaction: 79%; warm vertical compaction: 82%; there were no differences between techniques; a significantly higher success rate was observed for the warm vertical compaction in teeth presenting radiographically visible periapical lesions | |||||||||
| De Chevigny | Maxillary and mandibular anterior and posterior teeth | Vital and necrotic teeth | Hand files and engine-drive nickel titanium instruments + 2.5% NaOCl and, occasionally, 2% chlorhexidine | One visit or more (with calcium hydroxide paste) | Cold lateral compaction – sealer not reported; warm vertical compaction – sealer not reported; single-cone technique + glass ionomer sealer or injectable gutta-percha | 4–6 yr | PAI ≤ 2; no clinical signs or symptoms | Success rate: | |
| cold lateral compaction: 77%; warm vertical compaction: 87%; single cone technique or injectable gutta-percha: NR; warm vertical compaction was associated with a significant better outcome | |||||||||
| Mohan & Kaushik [ | Maxillary incisors and mandibular molars | Vital and necrotic teeth | NR | NR | Cold lateral compaction + AH-26; carrier-based obturation + AH-26 | 1 yr | No clinical signs or symptoms; no radiographic evidence of pathology | Success rate: | |
| cold lateral compaction: 90%; carrier-based obturation: 96%; there was no difference in the success rate between the investigated techniques | |||||||||
| Özer & Aktener [ | Mandibular first and second molars | Necrotic teeth | Quantec LX + NR | NR | Cold lateral compaction + Diaket; carrier-based obturation (Soft-Core) + Diaket | 3 yr | No clinical signs or symptoms; no radiographic evidence of pathology | Success rate: | |
| cold lateral compaction: 80%; carrier-based obturation: 85%; there was no difference in the success rate between the investigated techniques | |||||||||
| Hale | Maxillary and mandibular anterior and posterior teeth | Vital and necrotic teeth | ProFile rotary instrument + 3% NaOCl | One visit or more (with calcium hydroxide paste) | Cold lateral compaction + AH Plus; carrier-based obturation + AH Plus | 18–37 mon | No clinical signs or symptoms; no radiographic evidence of pathology or reduction of lesion’ size | Success rate: | |
| cold lateral compaction: 81%; carrier-based obturation: 83%; there was no difference in the success rate between the investigated techniques | |||||||||
| Kandemir Demirci & Çalışkan [ | Maxillary anterior teeth | Necrotic teeth | Hand files + 2.5% NaOCl | Two-visits (with calcium hydroxide paste) | Cold lateral compaction + AH Plus; carrier-based obturation (Thermafill) + AH Plus | 2 yr | PAI ≤ 2; no clinical signs or symptoms | Success rate: | |
| cold lateral compaction: 98.2%; carrier-based obturation: 96.4%; there was no difference in the success rate between the investigated techniques | |||||||||
| Sarin | Anterior and posterior teeth | Vital and necrotic teeth | NR | NR | Cold lateral compaction + Apexit Plus; carrier-based obturation + Apexit Plus | 18–38 mon | Absence of hard or soft tissue pathology | Success rate: | |
| cold lateral compaction: 80%; carrier-based obturation: 83%; there was no difference in the success rate between the investigated techniques | |||||||||
| Wang | Anterior and posterior teeth | Vital and necrotic teeth | NiTi rotary instruments + 1% NaOCl and 2% CHX before gutta-percha insertion | NR | Cold lateral compaction – sealer not specified; warm vertical compaction – sealer not specified | 2 mon | No clinical signs or symptoms; no radiographic evidence of pathology | Success rate: | |
| cold lateral compaction: 70.9%; warm vertical compaction: 98.2%; warm vertical compaction had a significantly improved success rate | |||||||||
| De-Figueiredo | Maxillary and mandibular anterior teeth | Necrotic teeth | Hand files + 2.5% NaOCl; Reciproc + 2.5% NaOCl | One visit | Cold lateral compaction + AH Plus; single-cone + AH Plus | 1 yr | PAI ≤ 2; no clinical signs or symptoms | Success rate: | |
| cold lateral compaction: 73%; single-cone technique: 78%; there was no difference in the success rate between the investigated techniques |
NR, not reported; PAI, Periapical index.
*Toronto study: phase IV – only information related to the pooled phases were considered.
Certainty of the evidence of the included studies
| Number of studies – study design | Certainty assessment | |||||
|---|---|---|---|---|---|---|
| Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | Overall certainty of evidence | |
| 4 randomized studies | Serious* | Not serious | Not serious | Not serious | None | ⨁⨁⨁○ |
| MODERATE | ||||||
| 7 nonrandomized studies | Very serious† | Serious‡ | Not serious | Not serious | None | ⨁◯◯◯ |
| VERY LOW | ||||||
*2/4 studies presented concerns regarding the randomization process; †5/7 studies did not control for all possible confounding factors; and 2/7 studies did not report for controlling of confounding factors at all; ‡Some heterogeneity was verified among studies.
NR, not reported; PAI, Periapical index.
*Toronto study: phase IV – only information related to the pooled phases were considered.
*2/4 studies presented concerns regarding the randomization process; †5/7 studies did not control for all possible confounding factors; and 2/7 studies did not report for controlling of confounding factors at all; ‡Some heterogeneity was verified among studies.

 KACD
KACD
 ePub Link
ePub Link Cite
Cite

