Abstract
-
Objectives
This study evaluated alterations in neuronal conductivity related to calcium silicate cements (CSCs) by investigating compound action potentials (cAPs) in rat sciatic nerves.
-
Materials and Methods
Sciatic nerves were placed in a Tyrode bath and cAPs were recorded before, during, and after the application of test materials for 60-minute control, application, and recovery measurements, respectively. Freshly prepared ProRoot MTA, MTA Angelus, Biodentine, Endosequence RRM-Putty, BioAggregate, and RetroMTA were directly applied onto the nerves. Biopac LabPro version 3.7 was used to record and analyze cAPs. The data were statistically analyzed.
-
Results
None of the CSCs totally blocked cAPs. RetroMTA, Biodentine, and MTA Angelus caused no significant alteration in cAPs (p > 0.05). Significantly lower cAPs were observed in recovery measurements for BioAggregate than in the control condition (p < 0.05). ProRoot MTA significantly but transiently reduced cAPs in the application period compared to the control period (p < 0.05). Endosequence RRM-Putty significantly reduced cAPs.
-
Conclusions
Various CSCs may alter cAPs to some extent, but none of the CSCs irreversibly blocked them. The usage of fast-setting CSCs during apexification or regeneration of immature teeth seems safer than slow-setting CSCs due to their more favorable neuronal effects.
-
Keywords: Apical extrusion; Bioceramics; Calcium silicate cements; Neuronal conductivity; Neurotoxicity
INTRODUCTION
Bioceramics are calcium silicate cements (CSCs) that have been widely used in endodontic procedures such as perforation repair, vital pulp therapies, apexogenesis, apexification, retrograde filling, obturation, and regeneration procedures [
1]. ProRoot MTA, which has a gray color (Dentsply Tulsa Dental Specialties, Johnson City, TN, USA) and consists of 75% Portland cement, 20% bismuth oxide, and 5% gypsum, was the first commercial product for root repair, retrofilling, and regenerative purposes in the dental market [
2,
3]. As the tetracalcium aluminoferrite and bismuth oxide ingredients caused discoloration of the tooth structure, white MTA with a reduced amount of tetracalcium aluminoferrite was introduced [
4]. MTA Angelus is another form of MTA consisting of 80% Portland cement and 20% bismuth oxide. The increased amount of calcium carbonate, calcium silicate, and barium zinc phosphate allows the material to set faster [
4]. Biodentine (Septodont, Saint-Maur-des-Fossés, France) is another fast-setting aluminate-free CSC containing highly pure tricalcium silicate in its powder and calcium chloride in its liquid as an accelerator instead of distilled water [
5]. Its encapsulated form, which allows a consistent mix, and lower discoloration effects are other advantages over ProRoot MTA [
5,
6]. Endosequence RRM-Putty (Brasseler, Savannah, GA, USA) is a premixed CSC available in paste or putty form with similar physical properties, but better handling properties, than MTA [
7]. BioAggregate (Innovative Bioceramix, Vancouver, Canada) is a CSC modified with calcium phosphate that includes tantalum oxide instead of bismuth oxide as a radiopacifier. RetroMTA (BioMTA, Seoul, Korea) is a novel and fast-setting hydraulic bioceramic, which is not based on Portland cement. It contains zirconium oxide instead of bismuth oxide and causes less discoloration than ProRoot and MTA Angelus [
8].
Biocompatibility is a crucial factor for endodontic repair materials, which directly interact with pulpal and periodontal tissues, as it may affect the viability, repair, and regeneration capacity of the residual cells [
9,
10,
11]. Furthermore, unintentional extrusion of the repair materials during apexification procedures or repair of perforations is also possible [
11,
12,
13,
14]. Although MTA and other CSCs are known to be biocompatible and bioactive, the outcomes of apical extrusion may be favorable or unfavorable, requiring surgical intervention [
11,
12,
15]. Furthermore, the periapical extrusion of endodontic materials may cause neurotoxic damage related to mechanical, thermal, or chemical mechanisms. For example, some of the current calcium silicate-based sealers caused severe degradation of axons and myelin sheaths in nerve tissue as a result of an inflammatory response [
16]. Endodontic materials may alter nerve membrane potentials and inhibit action potential conduction, which may result in sensory disorders such as pain, hyperesthesia or hypoesthesia, anesthesia, dysesthesia, and paresthesia [
17]. The severity of neurotoxic damage is related to toxic content and the contact time of the material with the tissue [
18].
An action potential is a nerve signal caused by a sufficient stimulus at threshold level and defined as a rapid rise and subsequent fall in voltage or membrane potential across a cellular membrane with a characteristic pattern. When an action potential is generated by a group of nerve fibers, it is called a compound action potential (cAP) [
19]. Alterations in cAPs caused by dental materials, especially endodontic sealers, were previously evaluated to estimate their neurotoxic effects [
16,
20]. However, although the biocompatibility of CSCs has been demonstrated in numerous studies investigating their cytotoxicity on pulp or periodontal cells, there are limited studies regarding their neuronal effects [
10,
21,
22,
23]. The purpose of this study was to evaluate the potential neuronal effects of these commonly used commercial CSCs by investigating their effects on neuronal conductivity via cAP alterations in sciatic nerves in a rat model. The null hypothesis was that CSCs would not block neuronal conductivity.
MATERIALS AND METHODS
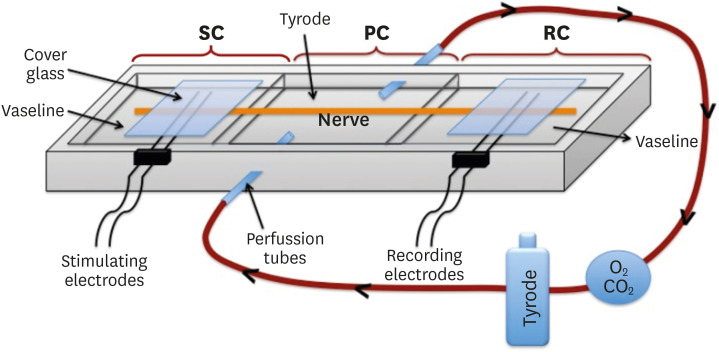
The CSCs tested in this study and their compositions are listed in
Table 1. In this study, a rat sciatic nerve experimental model was used, as previously described by Onur
et al. [
20]. Six sciatic nerves from 3 rats for each experimental group (18 rats in total) were used in this study in full accordance with the ethical principles and guidelines of the World Medical Association Declaration of Helsinki (2013). After receiving approval from the Ethics Board and Commission of Hacettepe University (2010/15-5 and 2018/35), locally bred female albino rats (
Wistar albino) weighing 300–340 g were anesthetized with intramuscular injections of Ketalar (50 mg/mL) and Rompun (2%) at a ratio of 90 to 10. Upon the administration of anesthesia, 1 of the sciatic nerves of each animal was dissected and desheathed under a microscope from adherent tissue. An intact nerve was longitudinally placed between 2 platinum electrodes in a 3-chambered Pyrex bath, which included stimulating, perfusion, and recording chambers. The perfusion chamber was full of Tyrode solution (8 g/L NaCl, 0.2 g/L KCl, 0.2 g/L CaCl
2, 0.1 g/L MgCl
2, 1 g/L NaHCO
3, 0.05 g/L NaH
2PO
4, 1 g/L glucose; pH 7.4) and continuously gassed with a mixture of 95% O
2 and 5% CO
2, and the nerve was perfused with fresh Tyrode solution at a flow rate of 2 mL/min at 37°C throughout the entire experimental process. The stimulating and recording chambers were electrically isolated using liquid Vaseline to prevent undesired environmental stimulations. The experimental set-up is shown in
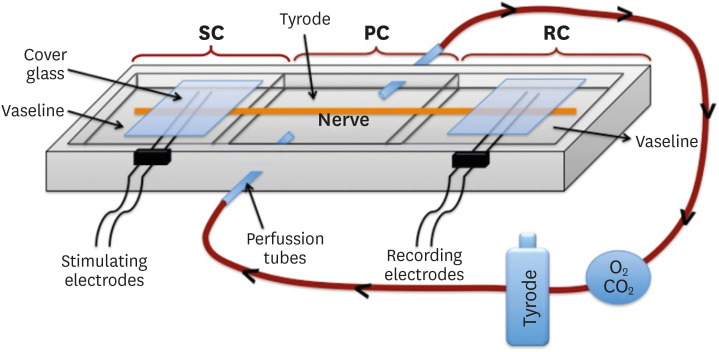
Figure 1.
Table 1 Calcium silicate-based cements tested in this study
|
Material |
Composition |
Manufacturer |
|
ProRoot MTA (grey) |
Powder: tricalcium silicate, dicalcium silicate, bismuth oxide, tricalcium aluminate, calcium sulfate dihydrate or gypsum |
Dentsply Tulsa Dental Specialties, Johnson City, TN, USA |
|
Liquid: distilled water |
|
MTA Angelus |
Powder: Silicon dioxide, potassium oxide, aluminum oxide, sodium oxide, iron oxide, sulfur trioxide, calcium oxide, bismuth oxide, magnesium oxide, insoluble residues of calcium oxide, potassium sulfate, sodium sulfate, and crystalline silica |
Angelus Londrina, Londrina, PR, Brazil |
|
Liquid: distilled water |
|
Biodentine |
Powder: tricalcium silicate, dicalcium silicate, calcium carbonate, zirconium oxide, calcium oxide, iron oxide |
Septodont, Saint-Maur-des-fossés, France |
|
Liquid: calcium chloride, a hydrosoluble (water-soluble) polymer, water |
|
Endosequence RRM-Putty |
Calcium silicates, zirconium oxide, tantalum pentoxide, calcium phosphate monobasic, and filler agents |
Brasseler, Savannah, GA, USA |
|
BioAggregate |
Powder: tricalcium silicate, dicalcium silicate, tantalum pentoxide, calcium phosphate monobasic, amorphous silicon oxide |
Innovative Bioceramix, Vancouver, Canada |
|
Liquid: deionized water |
|
RetroMTA |
Calcium carbonate, silicon dioxide, aluminum oxide, calcium zirconia complex |
BioMTA, Seoul, Korea |
Figure 1 Diagrammatic representation of the experimental set-up. A 3-chambered bath was used, consisting of a stimulating chamber (SC), a perfusion chamber (PC), and a recording chamber (RC). The sciatic nerve is placed through the bath, contacts stimulating electrodes, and passes through the perfusion chamber and reaches the recording electrodes. The Tyrode solution, O2, and CO2 flow in the direction of the arrows and perfuse the nerve.
A Biopac MP35 data acquisition unit (Biopac Systems Inc., Goleta, CA, USA) connected to platinum electrodes was used to create electrical stimuli and record cAP amplitudes of the nerve tissue. Before the experiments, the supramaximal stimulus level required to create a cAP with an amplitude of 0.05 ms was specifically determined for each nerve. The health status of the sciatic nerve was also checked by this application and those that could not be evoked were discarded. The nerve was stimulated every 10 seconds by using a BSLSTM Biopack system stimulator triggered by an MP35 unit, and existing action potentials were recorded on a computer with a sample rate of 100 kHz, an interval of 10 ms, and 5 ms acquisition length. Raw data were processed digitally by amplifying with a ×500 gain and a 2 kHz low pass, and Q = 0.707 filtering. Biopac LabPro version 3.7 software (Biopac Systems Inc.) was used to record and analyze data.
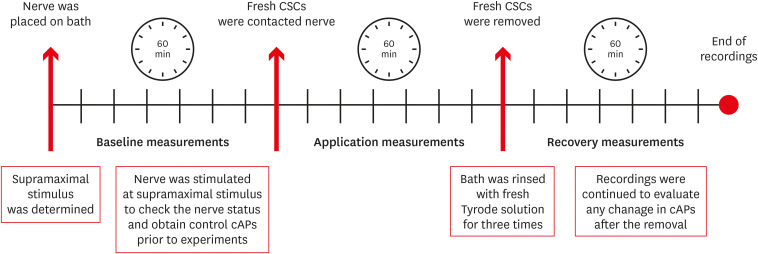
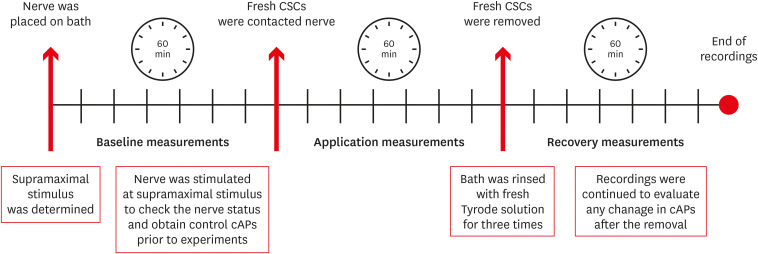
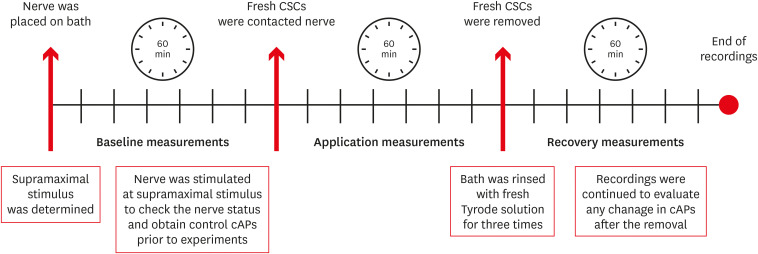
In this study, the data were recorded and assigned in 3 periods of 60 minutes each: baseline, application, and recovery, respectively. The baseline values recorded before the application of test material were used to compare the alterations during the experiments and served as a control. Each test material was prepared according to the recommendations of the manufacturer and applied directly onto a sciatic nerve as soon as it was prepared and the cAP amplitudes were recorded for 60 minutes. The test material was then removed, and sciatic nerve and bath was gently rinsed 3 times with fresh Tyrode solution to be sure that all remnants were removed. Immediately thereafter, cAP amplitudes were recorded for 60 additional minutes to evaluate post-application reactions and to evaluate recovery. The evoked cAP amplitudes were recorded every 10 minutes during each 60-minute experimental period, and the average of the recorded values was used as the mean cAP amplitude of the related period. As 2 nerves did not respond to stimulations during baseline measurements, Endosequence RRM-Putty was tested on 4 separate nerves (
n = 4) while the others were tested on 6 nerves (
n = 6). The experimental process is shown in
Figure 2.
Figure 2
Diagrammatic timetable of the experimental process, showing 3 measurement intervals: baseline, application, and recovery measurements.
cAP, compound action potential; CSC, calcium silicate cement.
The data were analyzed using SPSS version 21.0 (IBM Corp., Armonk, NY, USA). Repeated-measures 2-way analysis of variance was used for intra-material comparisons of cAPs versus time. The post hoc Tukey test was used for pairwise comparisons. The level of significance was set at p < 0.05.
RESULTS
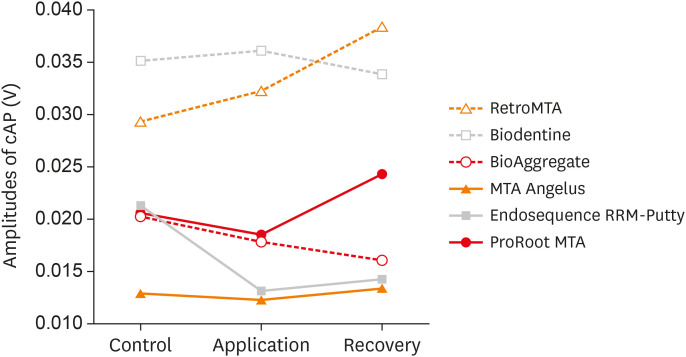
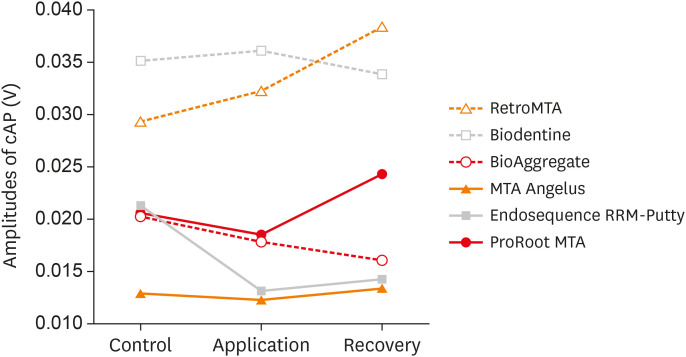
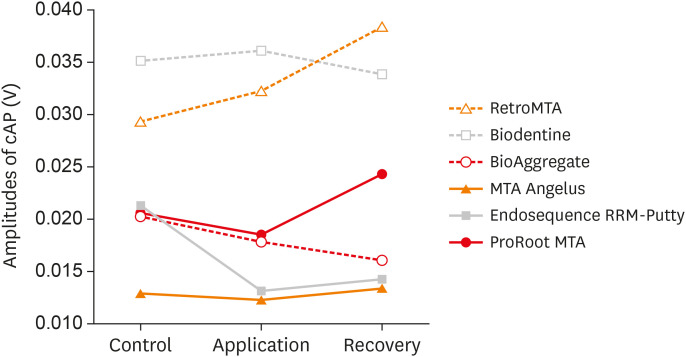
None of the test materials totally blocked the cAP amplitudes. When the cAPs of the baseline, application, and recovery measurements were compared, no significant differences were found for RetroMTA, Biodentine, and MTA Angelus (
p > 0.05). However, a significant difference was observed for BioAggregate, ProRoot MTA, and Endosequence RRM-Putty (
p < 0.05). Significantly lower cAPs were observed in the recovery measurements for BioAggregate compared to baseline (
p < 0.05). In the ProRoot MTA group, cAPs significantly decreased from baseline to application (
p < 0.05); however, there was no significant difference compared to the recovery values (
p > 0.05), meaning that the reduction was transient. Endosequence RRM-Putty significantly reduced cAPs (
p < 0.05). The mean, median, standard deviation, and minimum and maximum amplitudes of cAP for the test groups in the baseline, application, and recovery measurements are listed in
Table 2. Changes in the cAP amplitudes of test materials versus time are shown in
Figure 3.
Table 2 Means, medians, SDs, and minimum and maximum compound action potential (cAP) amplitudes (V) of the test groups for the control, application, and recovery measurements
|
Groups |
N |
Control cAP (V) |
Application cAP (V) |
Recovery cAP (V) |
|
ProRoot MTA |
6 |
Mean |
0.0206*
|
0.0184*
|
0.0243 |
|
Median |
0.0157 |
0.0145 |
0.0140 |
|
SD |
0.0114 |
0.0104 |
0.0209 |
|
Minimum |
0.0091 |
0.0083 |
0.0084 |
|
Maximum |
0.0390 |
0.0358 |
0.0623 |
|
MTA Angelus |
6 |
Mean |
0.0129 |
0.0123 |
0.0133 |
|
Median |
0.0132 |
0.0119 |
0.0126 |
|
SD |
0.0049 |
0.0055 |
0.0078 |
|
Minimum |
0.0052 |
0.0044 |
0.0030 |
|
Maximum |
0.0181 |
0.0187 |
0.0233 |
|
Biodentine |
6 |
Mean |
0.0352 |
0.0361 |
0.0339 |
|
Median |
0.0332 |
0.0266 |
0.0302 |
|
SD |
0.0182 |
0.0255 |
0.0221 |
|
Minimum |
0.0176 |
0.0140 |
0.0143 |
|
Maximum |
0.0662 |
0.0778 |
0.0739 |
|
Endosequence RRM-Putty |
4 |
Mean |
0.0211*
|
0.0130*
|
0.0142*
|
|
Median |
0.0157 |
0.0123 |
0.0137 |
|
SD |
0.0108 |
0.0121 |
0.0130 |
|
Minimum |
0.0126 |
0.0000 |
0.0000 |
|
Maximum |
0.0381 |
0.0298 |
0.0302 |
|
BioAggregate |
6 |
Mean |
0.0202*
|
0.0178 |
0.0162*
|
|
Median |
0.0193 |
0.0172 |
0.0140 |
|
SD |
0.0110 |
0.0097 |
0.0102 |
|
Minimum |
0.0068 |
0.0049 |
0.0038 |
|
Maximum |
0.0351 |
0.0304 |
0.0281 |
|
RetroMTA |
6 |
Mean |
0.0293 |
0.0323 |
0.0384 |
|
Median |
0.0275 |
0.0301 |
0.0375 |
|
SD |
0.0128 |
0.0170 |
0.0253 |
|
Minimum |
0.0148 |
0.0151 |
0.0101 |
|
Maximum |
0.0507 |
0.0603 |
0.0799 |
Figure 3 Changes in compound action potential (cAP) amplitudes of the tested calcium silicate cements versus time.
DISCUSSION
The extrusion of endodontic filling materials into anatomical landmarks, such as the mandibular canal, may cause undesired complications such as paresthesia when the materials come into direct contact with the inferior alveolar nerve (IAN) [
22,
24]. Even though the biocompatibility and bioactivity of CSCs have been demonstrated in numerous studies with pulp or periodontal cells, there are limited studies regarding their neurotoxic effects [
10,
21,
22,
23,
25].
In our study, the possible neuronal effects of CSCs were evaluated by measuring alterations in cAP amplitudes, a common electrical activity of each nerve fiber in the nerve trunk that is related to neuronal conductivity. Experiments were performed on rat sciatic nerve tissue, as it is a mixed nerve similar to the IAN and thick enough to allow creating and recording electrical stimulations. Furthermore, surgical dissection of the sciatic nerve without any damage is easy. This experimental model enables direct contact of the test material with the nerve and measurements of alterations in cAP amplitudes. Therefore, it simulates clinical cases where CSC extrudes into the mandibular canal and directly contacts the IAN.
Asrari and Lobner [
22] evaluated the effects of freshly prepared or set ProRoot MTA, amalgam, SuperEBA (Henry Schein, Melville, NY, USA), and Diaket (ESPE, Hessen, Germany) on cortical cell cultures containing both neuronal and glial cells prepared from fetal mice. They evaluated neurotoxicity by a quantitative assessment of lactate dehydrogenase released from damaged or destroyed cells. They found that neither fresh unset ProRoot MTA was toxic to neuronal or glial cells, while the other materials caused 50%–100% cell death. These results are in accordance with our results that cAPs significantly decreased from baseline to the application time in the ProRoot MTA group.
All the cements tested in this study were directly applied onto nerves immediately after preparation during the 60-minute application period. Biodentine, MTA Angelus, and Retro MTA are relatively fast-setting cements compared to ProRoot MTA, Endosequence RRM-Putty, and BioAggregate [
1,
26]. None of the fast-setting CSCs caused any significant reduction in cAPs during the application or recovery period, but the slow-setting CSCs reduced the cAPs. When compared to baseline, BioAggregate and ProRoot significantly reduced cAPs during the recovery and application periods, respectively. The mean application and recovery cAPs for Endosequence RRM-Putty were lower than the baseline cAPs.
In another study, Abbasipour
et al. [
23] evaluated the nociceptive and anti-nociceptive effects of white ProRoot MTA by subcutaneous injections in a rat animal model. They observed that ProRoot MTA did not irritate nerve tissues. Similarly, neither ProRoot MTA nor other CSCs tested in our study caused an irreversible blockage of cAPs.
As is widely known, most of the bioceramics used in endodontics are Portland cement-based. Although its biocompatibility has been recognized, Portland cement may contain some heavy metals and contaminants such as arsenic, lead, and chromium [
27,
28]. Arsenic is a metalloid encountered in nature in both organic and inorganic forms and in different oxidation states. The most toxic states are trivalent and pentavalent. It has been shown that arsenic toxicity may be related to renal, hepatic, respiratory, glandular, digestive, and skin problems, as well as nervous system disorders [
29]. According to this information, it is possible that CSCs may have some neurotoxic effects because of their arsenic content. However, none of the tested CSCs in this study caused irreversible nerve blockage, as discussed above. According to the ISO 9917-1 standard, dental cements should not contain more arsenic than 2 mg/kg [
30]. Monteiro Bramante
et al. [
28] investigated the amount of arsenic in some commercial MTA compositions by atomic absorption spectrophotometry and showed that the white forms of Portland cement, MTA Angelus, and ProRoot MTA contained less arsenic than the ISO limits, but gray ProRoot MTA contains more. However, Duarte
et al. [
27] showed that arsenic release from gray ProRoot MTA and white MTA Angelus was below the ISO limit. The ferric salts in gray ProRoot MTA [
4] may stabilize arsenic and reduce its release to acceptable values [
31]. Camilleri
et al. [
32] also showed very low levels of leaching of arsenic from BioAggregate and Biodentine.
To create an action potential, an electrical stimulus at the threshold level is required and this may vary among the nerve bundles through the nerve trunk. The nerve must be evoked with a supramaximal stimulus, enough to reach the highest threshold level through the nerve trunk, to create a cAP amplitude [
20]. After determining the optimal supramaximal stimulus level required for each sciatic nerve; cAP amplitudes created under these conditions were recorded during baseline, application, and recovery measurements. Although the same type of rats, with similar weight and age, was used in the experiments, the supramaximal stimulus levels and baseline cAP values of the sciatic nerves used for the experiments were variable. This variation, which is a limitation of the study, may be related to anatomic and physiologic differences of the nerve trunk upon which the material was applied.
Slight alterations, including both increases and decreases in cAP amplitudes, were observed in this study; however, they were not directly correlated to neurotoxicity. However, the fact that no irreversible blockage of cAPs was observed in this study may show that CSCs are safe in terms of neurotoxicity. To reach a more comprehensive conclusion about neurotoxicity, tests should be performed on live animal models and supported with histologic studies.
CONCLUSIONS
Within the limitations of this study, it can be concluded that none of the tested CSCs in this study irreversibly blocked neuronal conductivity. However, using fast-setting CSCs during apexification or regeneration of immature teeth, especially close to the mandibular canal, seems safer than slow-setting CSCs due to their more favorable neuronal effects.
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Daglı-Comert F, Deniz-Sungur D, Onur MA.
Data curation: Onur MA, Formal analysis.
Funding acquisition: Sayın TC, Daglı-Comert F.
Methodology: Onur MA.
Project administration: Sayın TC.
Resources: Onur MA, Daglı-Comert F.
Software: Deniz-Sungur D, Onur MA.
Supervision: Daglı-Comert F, Sayın TC.
Validation: Onur MA.
Visualization: Deniz-Sungur D.
Writing - original draft: Deniz-Sungur D.
Writing - review & editing: Onur MA, Sayın TC.
REFERENCES
- 1. Dawood AE, Parashos P, Wong RHK, Reynolds EC, Manton DJ. Calcium silicate-based cements: composition, properties, and clinical applications. J Investig Clin Dent 2017;8:e12195.ArticlePDF
- 2. Torabinejad M, Hong CU, McDonald F, Pitt Ford TR. Physical and chemical properties of a new root-end filling material. J Endod 1995;21:349-353.ArticlePubMed
- 3. Parirokh M, Torabinejad M. Mineral trioxide aggregate: a comprehensive literature review--part I: chemical, physical, and antibacterial properties. J Endod 2010;36:16-27.ArticlePubMed
- 4. Song JS, Mante FK, Romanow WJ, Kim S. Chemical analysis of powder and set forms of Portland cement, gray ProRoot MTA, white ProRoot MTA, and gray MTA-Angelus. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;102:809-815.ArticlePubMed
- 5. Malkondu Ö, Karapinar Kazandağ M, Kazazoğlu E. A review on biodentine, a contemporary dentine replacement and repair material. BioMed Res Int 2014;2014:160951.ArticlePubMedPMCPDF
- 6. Roberts HW, Toth JM, Berzins DW, Charlton DG. Mineral trioxide aggregate material use in endodontic treatment: a review of the literature. Dent Mater 2008;24:149-164.ArticlePubMed
- 7. Walsh RM, Woodmansey KF, Glickman GN, He J. Evaluation of compressive strength of hydraulic silicate-based root-end filling materials. J Endod 2014;40:969-972.ArticlePubMed
- 8. Kang SH, Shin YS, Lee HS, Kim SO, Shin Y, Jung IY, Song JS. Color changes of teeth after treatment with various mineral trioxide aggregate-based materials: an ex vivo study. J Endod 2015;41:737-741.PubMed
- 9. Torabinejad M, Pitt Ford TR. Root end filling materials: a review. Endod Dent Traumatol 1996;12:161-178.ArticlePubMed
- 10. Gomes Cornélio AL, Salles LP, Campos da Paz M, Cirelli JA, Guerreiro-Tanomaru JM, Tanomaru Filho M. Cytotoxicity of Portland cement with different radiopacifying agents: a cell death study. J Endod 2011;37:203-210.ArticlePubMed
- 11. Chang SW, Oh TS, Lee W, Cheung GS, Kim HC. Long-term observation of the mineral trioxide aggregate extrusion into the periapical lesion: a case series. Int J Oral Sci 2013;5:54-57.ArticlePubMedPMCPDF
- 12. Asgary S, Fayazi S. Endodontic surgery of a symptomatic overfilled MTA apical plug: a histological and clinical case report. Iran Endod J 2017;12:376-380.PubMedPMC
- 13. Comin Chiaramonti L, Cavalleri G. Effect of unintentionally extruded mineral trioxide aggregate in treatment of root perforation with periradicular lesion: a case report. Minerva Stomatol 2011;60:217-222.PubMed
- 14. Islam I, Chng HK, Yap AU. Comparison of the physical and mechanical properties of MTA and portland cement. J Endod 2006;32:193-197.ArticlePubMed
- 15. Asgary S, Eghbal MJ, Mehrdad L, Kheirieh S, Nosrat A. Surgical management of a failed internal root resorption treatment: a histological and clinical report. Restor Dent Endod 2014;39:137-142.ArticlePubMedPMC
- 16. Tuğ Kılkış B, Er K, Taşdemir T, Yildirim M, Taskesen F, Tümkaya L, Kalkan Y, Serper A. Neurotoxicity of various root canal sealers on rat sciatic nerve: an electrophysiologic and histopathologic study. Clin Oral Investig 2015;19:2091-2100.ArticlePubMedPDF
- 17. Ahlgren FK, Johannessen AC, Hellem S. Displaced calcium hydroxide paste causing inferior alveolar nerve paraesthesia: report of a case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003;96:734-737.ArticlePubMed
- 18. Pogrel MA. Damage to the inferior alveolar nerve as the result of root canal therapy. J Am Dent Assoc 2007;138:65-69.ArticlePubMed
- 19. He S, Teagle HFB, Buchman CA. The electrically evoked compound action potential: from laboratory to clinic. Front Neurosci 2017;11:339.ArticlePubMedPMC
- 20. Onur MA, Cehreli ZC, Tasman F, Gümrükçuoğlu A. Neurotoxic effects of fifth-generation dentin adhesives on rat sciatic nerve. J Endod 2001;27:676-678.ArticlePubMed
- 21. Damas BA, Wheater MA, Bringas JS, Hoen MM. Cytotoxicity comparison of mineral trioxide aggregates and EndoSequence bioceramic root repair materials. J Endod 2011;37:372-375.ArticlePubMed
- 22. Asrari M, Lobner D.
In vitro neurotoxic evaluation of root-end-filling materials. J Endod 2003;29:743-746.PubMed
- 23. Abbasipour F, Rastqar A, Bakhtiar H, Khalilkhani H, Aeinehchi M, Janahmadi M. The nociceptive and anti-nociceptive effects of white mineral trioxide aggregate. Int Endod J 2009;42:794-801.ArticlePubMed
- 24. González-Martín M, Torres-Lagares D, Gutiérrez-Pérez JL, Segura-Egea JJ. Inferior alveolar nerve paresthesia after overfilling of endodontic sealer into the mandibular canal. J Endod 2010;36:1419-1421.ArticlePubMed
- 25. Sarkar NK, Caicedo R, Ritwik P, Moiseyeva R, Kawashima I. Physicochemical basis of the biologic properties of mineral trioxide aggregate. J Endod 2005;31:97-100.ArticlePubMed
- 26. Sinkar RC, Patil SS, Jogad NP, Gade VJ. Comparison of sealing ability of ProRoot MTA, RetroMTA, and Biodentine as furcation repair materials: an ultraviolet spectrophotometric analysis. J Conserv Dent 2015;18:445-448.ArticlePubMedPMC
- 27. Duarte MA, De Oliveira Demarchi AC, Yamashita JC, Kuga MC, De Campos Fraga S. Arsenic release provided by MTA and Portland cement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005;99:648-650.ArticlePubMed
- 28. Monteiro Bramante C, Demarchi AC, de Moraes IG, Bernadineli N, Garcia RB, Spångberg LS, Duarte MA. Presence of arsenic in different types of MTA and white and gray Portland cement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008;106:909-913.ArticlePubMed
- 29. Hughes MF. Arsenic toxicity and potential mechanisms of action. Toxicol Lett 2002;133:1-16.ArticlePubMed
- 30. International Standardization Organization. Dentistry - water based cements part 1: powder/liquid acid-base cements. Geneva: International Standardization Organization; 2003. p. 1-22.
- 31. Kim JY, Davis AP, Kim KW. Stabilization of available arsenic in highly contaminated mine tailings using iron. Environ Sci Technol 2003;37:189-195.ArticlePubMed
- 32. Camilleri J, Kralj P, Veber M, Sinagra E. Characterization and analyses of acid-extractable and leached trace elements in dental cements. Int Endod J 2012;45:737-743.ArticlePubMed
 , Mehmet Ali Onur2
, Mehmet Ali Onur2 , Esin Akbay2
, Esin Akbay2 , Gamze Tan3
, Gamze Tan3 , Fügen Daglı-Comert1,4
, Fügen Daglı-Comert1,4 , Taner Cem Sayın1,5
, Taner Cem Sayın1,5


 KACD
KACD
 ePub Link
ePub Link Cite
Cite

