Abstract
Endodontic microsurgery is a predictable treatment option when orthograde treatment or retreatment is unsuccessful or unfeasible. However, when there is a gross compromise of periapical bone, achievement of bone regeneration after the surgical procedure may be hampered. In such cases, the application of guided tissue regeneration principles, with adjunctive use of leukocyte platelet-rich fibrin to fill the bone defect as a bone substitute and as a membrane to cover the site, provides a cost-effective solution with the benefits of accelerated physiological healing and reduced post-surgical pain and discomfort. This case report presents 2 cases of endodontic microsurgery of the upper lateral incisors with loss of buccal cortical plate, where platelet-rich fibrin was successfully applied.
-
Keywords: Endodontics; Guided tissue regeneration; Microsurgery; Leukocyte-platelet-rich fibrin
INTRODUCTION
One of the main goals of root canal treatment is to conduct chemo-mechanical debridement of the root canal system space [
1] to reduce the intracanal microbial load to a level that is insufficient to induce a pathological response [
2]. Following proper cleaning and shaping of the root canal system, a 3-dimensional root canal obturation prevents re-contamination [
3] and allows the reestablishment of periapical health. Nonetheless, in a small group of treated teeth, root canal treatment may fail, with persistent periapical pathology and, possibly, associated symptoms [
4]. In such cases, endodontic microsurgery (EMS) may be a valid and predictable treatment option, with reported success rates over 90% [
5,
6].
Radiographic confirmation of bone repair in cases of apical periodontitis is expected after successful EMS [
7]. However, clinical conditions such as large bony crypts or the absence of cortical marginal bone may reduce the success rate [
8]. Guided tissue regeneration (GTR) techniques have been comprehensively studied in periodontology and may be adjunctively applied in EMS [
9,
10] in order to overcome preoperative bone defects. The use of leukocyte platelet-rich fibrin (L-PRF) is one of these techniques. L-PRF is easily and quickly obtained by centrifuging a patient’s blood without mixing with any additives, providing a stable and resistant membrane rich in growth factors, from which wound healing can rapidly take place [
11]. The literature shows a considerable reduction in early postoperative pain levels and swelling, with a positive impact on patients’ quality of life after an EMS procedure [
12]. However, contradictory results have been reported on the actual effects and benefits of autologous platelet concentrates in bone healing [
11,
13].
The present case report documents 2 cases of EMS involving 2 maxillary lateral incisors with unsuccessful root canal treatment, in which L-PRF was applied as an osseous filler and barrier membrane of large preoperative bone defects.
CASE REPORT
General root canal treatment procedures
In both cases, the medical history was reviewed and considered non-contributory. An intra-oral examination was conducted to assess periodontal pocket depth and mobility, which were considered within physiological limits prior to the radiographic investigation. A pulpal and periapical diagnosis was made for both cases, combining the examination findings, pulpal tests (in case 1), and periapical radiographs. Endodontic therapy was recommended as a treatment plan to both patients, who accepted the plan and signed informed consent forms. The treatments were performed after local anesthesia with 1.8 mL of 4% articaine with 1:200.000 epinephrine (Artinibsa, Inibsa, Spain), and rubber dam placement. Prior to mechanical instrumentation of the canals, a manual glide path was established with an ISO size 10 K-file (K-File; Dentsply, Ballaigues, Switzerland). Full debridement was performed under copious irrigation with 5.25% sodium hypochlorite (Denta Flux; J. Ripoll SL, Murcia, Spain) using a 5 mL syringe and a 27G notched needle (CanalPro Slotted-End Tips, Coltene, Lezzenes, France). The working length was established using an electronic apex locator (miniRoot Zx; Morita, Irvine, CA, USA), with additional confirmation via periapical radiography. Mechanical instrumentation was performed using a VDW Silver motor (VDW, Munich, Germany). The final irrigation protocol also included 1 minute of irrigation with 10% citric acid prior to a final sodium hypochlorite rinse under sonic agitation with EndoActivator (Dentsply Maillefer, Ballaigues, Switzerland), after which the canals were dried with 4% tapered paper points (Zipperer; VDW) and obturated with gutta-percha and sealer (AH Plus Jet; Dentsply DeTrey, Konstanz, Germany) using the continuous-wave condensation technique performed with the B&L system (Biotech, Seoul, Korea). After canal obturation, the pulp chambers were rinsed with alcohol, the canal orifices were sealed with Ionoseal (VOCO GmbH, Cuxhaven, Germany), and the access cavities were temporarily filled with Cavit (Cavit W; 3M ESPE, Seefeld, Germany). The patients were referred for a restorative appointment for definitive restoration of the endodontic accesses.
Case 1
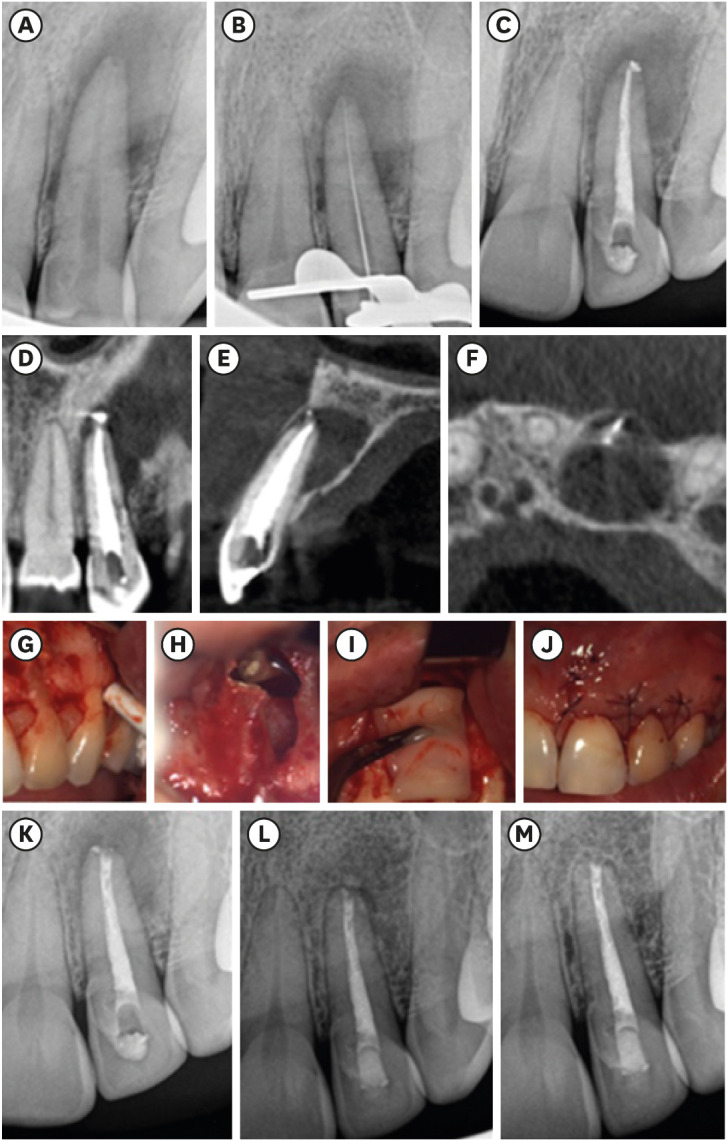
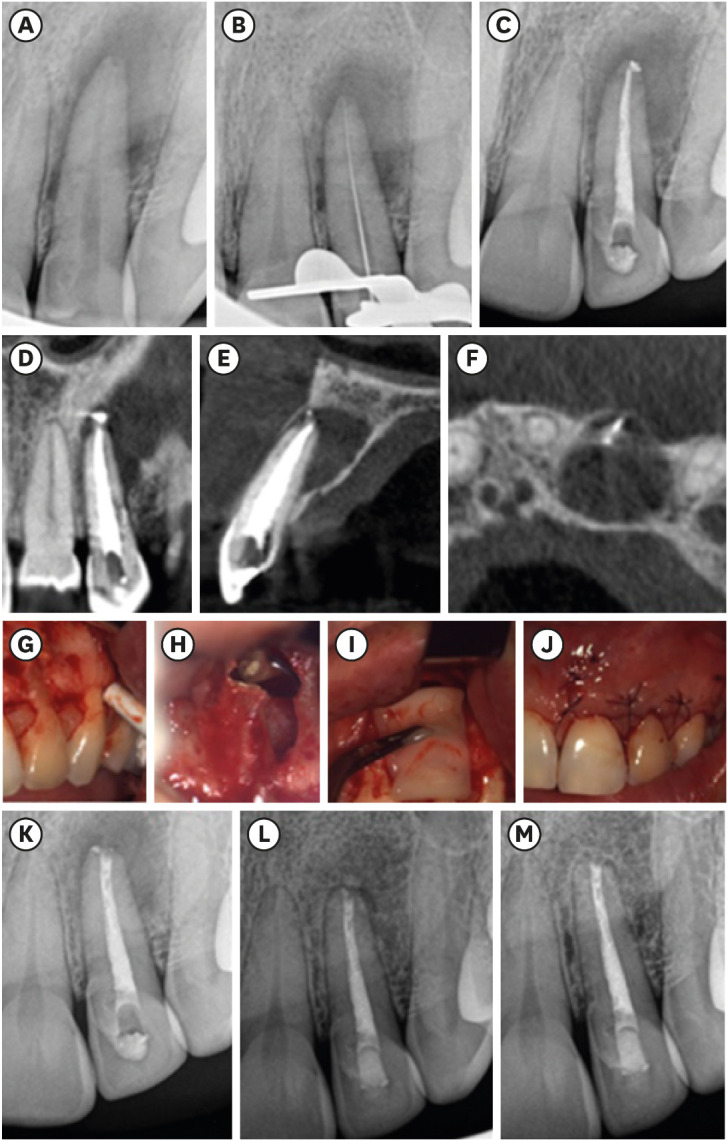
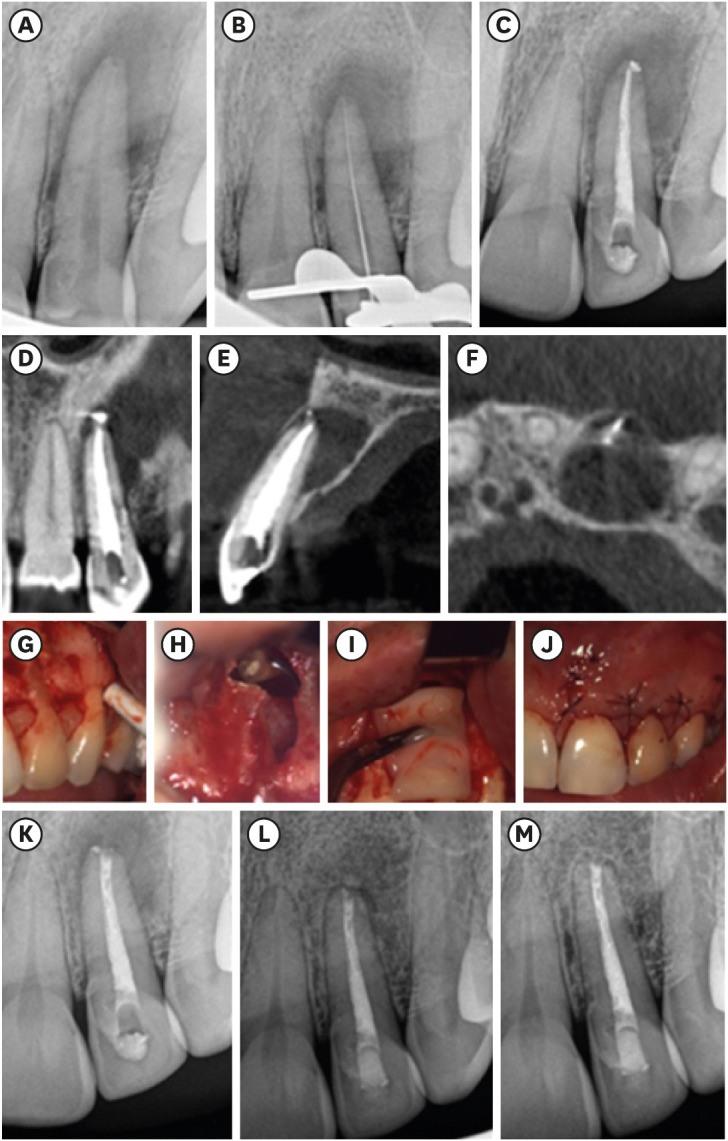
A 43-year-old female patient was referred to an endodontic appointment at a private practice after an incidental radiographic finding of a periapical radiolucency associated with the maxillary left lateral incisor (tooth #22), which presented with a sound crown (no caries or restorations) (
Figure 1A). The patient reported a history of dental trauma with an impact to the upper anterior teeth about 20 years earlier. There was pain to buccal palpation over tooth #22, and vertical percussion also elicited a painful response. There was no response to cold (Endo cold spray; Henry Schein, Hessen, Germany), with normal responses on both adjacent teeth. A diagnosis of necrotic pulp, probably of traumatic origin, and symptomatic apical periodontitis was established. The endodontic access was prepared using a round diamond bur (Komet Medical, Lemgo, Germany) and refined using an Endo Z bur (Dentsply Maillefer). After determining the working length (
Figure 1B), the Reciproc (R25 and R40; VDW) system was chosen for instrumentation. Due to time limitations, the root canal treatment was not concluded at the first appointment. A dressing of calcium hydroxide (UltraCal; Ultradent, South Jordan, UT, USA) was applied as an intracanal medication between appointments. At the second visit 2 weeks later, the tooth was asymptomatic, and the root canal treatment was completed (
Figure 1C). At 3 months post-treatment, the patient developed an acute apical abscess. An additional periodontal examination was done, and cone-beam computed tomography (CBCT) was performed to fully ascertain the dimensions and extension of the periapical lesion (
Figure 1D-1F) in order to establish a proper treatment plan. EMS was then recommended and accepted, and the patient signed a written consent form. After the EMS procedure (
Figure 1G-1K), with the details of the general procedures explained below, a follow-up radiographic examination was performed at 6 months (
Figure 1L), showing good progression of osseous healing. At 12 months (
Figure 1M) there was complete resolution of the periapical lesion.
Figure 1Chronological documentation of case 1: (A) initial periapical radiograph of tooth #22; (B) working length confirmation; (C) periapical radiograph showing the final root canal treatment; (D, E, F) axial, sagittal, and coronal views of cone-beam computed tomography prior to endodontic microsurgery; (G) mucoperiosteal flap; (H) apicoectomy, retrograde preparations, and obturation with MTA; (I) previously prepared leukocyte platelet-rich fibrin membranes used to fill and cover the surgical bone defect; (J) repositioned flap; (K) post-surgical periapical radiograph; (L) radiograph from a 6-month follow-up visit; (M) radiograph from a 12-month follow-up after endodontic microsurgery.
Case 2
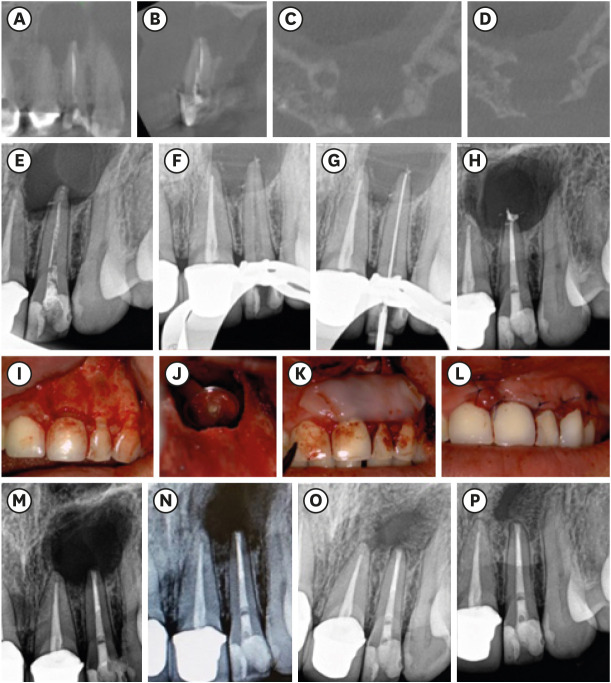
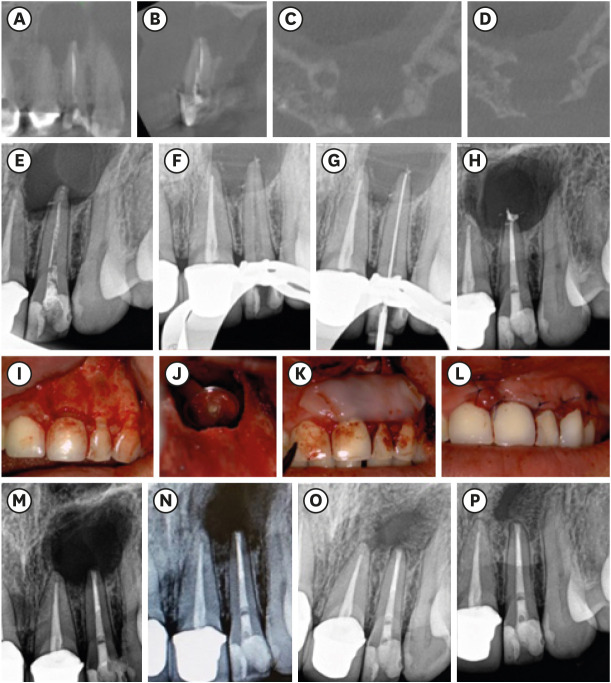
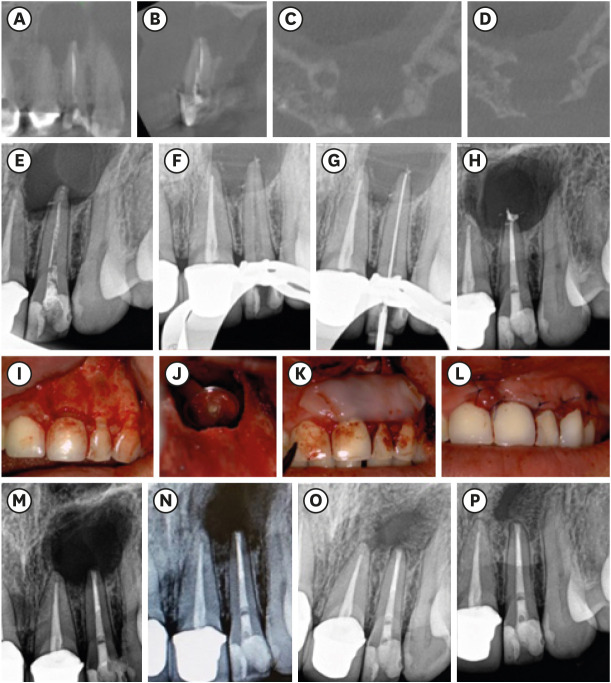
A 32-year-old female patient was sent for an appointment at the endodontics post-graduate clinic at the University of Lisbon, with a previously initiated root canal treatment on the maxillary left lateral incisor (tooth #22). The referring clinician reported an inability to dry the canal after several rounds of intracanal medication. The tooth presented with mesial and distal composite restorations and a provisional filling over the palatal access. There was pain on palpation and percussion, while the periodontal probing was normal. A CBCT scan was requested, and it revealed an extensive lesion involving both buccal and palatal cortical plates. Considering the clinical and imaging data (
Figure 2A-2E), root canal retreatment was advised. The treatment was performed under magnification through a dental operating microscope (M320; Leica, Wetzlar, Germany). After removing the provisional filling, the endodontic access was refined with Start-X 3 ultrasonic tip (Dentsply Maillefer USA, Los Angeles, CA, USA). The intracanal dressing was rinsed with copious irrigation (
Figure 2F) and the working length was determined (
Figure 2G). The WaveOne Gold system (Primary, Medium and Large; Dentsply Maillefer) was chosen for instrumentation and the treatment was completed in a single session (
Figure 2H). Two months after the appointment, the patient reported spontaneous, continuous dull pain over the periapical area of the treated tooth. After clinical observation, EMS was advised, and the patient signed a consent form. The microsurgical procedures (
Figure 2I-2L) are described below. Radiographic examinations at 2, 4 and 6 months (
Figure 2M-2O) showed a gradual increase in bone trabeculation. At a 1-year follow-up (
Figure 2P) there was considerable ossification of the periapical area with an apparent residual scar tissue area.
Figure 2Chronological documentation of case 2: (A, B, C, D) Axial, sagittal, and coronal views of cone-beam computed tomography before root canal treatment; (E) initial periapical radiograph of tooth #22; (F) cleaned root canal after irrigation; (G) working length confirmation; (H) periapical radiograph showing the final root canal treatment; (I) mucoperiosteal flap; (J) apicoectomy, retrograde preparations, and obturation with mineral trioxide aggregate; (K) leukocyte platelet-rich fibrin membranes filling the bone defect; (L) repositioning of the surgical flap; (M) radiograph from a 2-month follow-up; (N) radiograph from a 4-month follow-up; (O) radiograph from a 6-month follow-up; (P) and radiograph from a 12-month follow-up after endodontic microsurgery.
General EMS procedures
The L-PRF was obtained using the IntraSpin system (BioHorizons, Birmingham, AL, USA). The patient’s blood was drawn by a nurse practitioner on-site immediately before surgery into 9 mL plastic tubes without anticoagulant agents. The collected blood samples were immediately centrifuged for 15 minutes at 2,700 rpm. The produced clots were extracted from the container using thin sterile forceps and placed in a specially designed kit to compress L-PRF clots into L-PRF membranes with a consistent thickness of 1 mm.
The surgical procedures were done under magnification through a dental operating microscope (M320; Leica) at the university clinic. Local anesthesia was achieved with buccal and palatal infiltrations of 4% articaine with 1:100,000 epinephrine. A full-thickness mucoperiosteal flap was raised with a microblade scalpel (SybronEndo, Orange, CA, USA) through a papilla-based incision extending from the mesial aspect of tooth 21 to the distal aspect of tooth 23 and supported by 2 vertical releasing incisions (
Figures 1G and
2I). The cortical buccal plates over the intended osteotomy sites were very thin, and access to the apices of both teeth was gained with the aid of a surgical curette (Hu-Friedy, Chicago, IL, USA). High-speed osteotomy tungsten carbide round burs (Dentsply Sirona, Philadelphia, PA, USA) were used under irrigation to refine the bony margins. All granulomatous tissues were removed by manual curettage and hemostasis was obtained with the aid of Telfa pads (Covidien, Cascais, Portugal). Apical root resection (3 mm) was performed with a Zekrya (Dentsply Sirona) surgical bur, and the retrograde preparation was accomplished with JT-2B ultrasonic tip (Biotech). After drying the root-end preparation with paper points, an apical plug of MTA (ProRoot MTA; Dentsply Tulsa Dental, Tulsa, OK, USA) was placed (
Figures 1H and
2J). L-PRF was used to fill the bone defect in both cases and also cover the cortical bone as a membrane (
Figures 1I and
2K). The flap was repositioned with the aid of non-resorbable sutures with 5.0 silk (Braun, Tuttlingen, Germany) (
Figure 1J and
2K) and 0.2% chlorhexidine gel (Elugel; Pierre Fabre Oral Care, Castres, France) was applied with a sterile cotton gauze pad over the area that received the intervention. The patients were medicated with systemic antibiotics (875 mg of amoxicillin + 125 mg of clavulanic acid, 1 pill every 12 hours for 8 days), a non-steroidal anti-inflammatory drug (600 mg of ibuprofen, 1 pill every 8–12 hours for 3 to 5 days) and pain medication (300 mg of clonixin, up to 2 pills a day to manage symptoms) along with dedicated post-surgical instructions. Sutures were removed 5 days after the procedure, with good tissue healing and no major discomfort.
DISCUSSION
Failure of nonsurgical endodontic treatment is commonly associated with the persistence of intraradicular contamination [
14]. When endodontic treatment is performed according to a high standard of care and symptoms still persist symptoms, surgical endodontic retreatment is a viable option. Modern EMS encompasses the use of magnification, dedicated micro-instruments, ultrasonic tips, and biocompatible root-end filling materials (such as mineral trioxide aggregate [MTA]), and it has been associated with long term survival rates of over 95% [
8,
15,
16].
The ultimate goal of an endodontic surgical procedure is to help regenerate the periapical tissues that were affected by the infectious process, including the alveolar bone, cementum, and periodontal ligament [
17]. In both presented cases, there was a considerable loss of marginal buccal bone after the surgical procedure. Previous studies have suggested a correlation between the mesiodistal dimension of the bony crypt [
18] and the height of the remaining buccal bone plate [
8] with the outcomes of EMS.
The application of GTR principles in EMS in such cases is based on the need to create a stable and sealed space for bone regeneration to occur, without ingrowth of undesired connective tissue [
9]. The advantage of L-PRF over other available options for membranes and bone substitutes is the fact that it is an autologous easily obtained material, that serves not only as a physical barrier but also as a source of all the blood constituents essential for the physiological osseous healing process. It is a cost-effective biomaterial that efficiently and locally directs and accelerates the healing process by serving as a stable network for migration of cells for neo-angiogenesis and as a provider of all the molecular and cellular intervening factors, while protecting the open wound from epithelial ingrowth [
19].
There is a general consensus on the positive effect of autologous platelet concentrates on postoperative quality of life, with lower levels of pain and swelling [
12,
13]. However, it is far more difficult to ascertain whether there is in fact a significant difference in bone healing. A study assessed periapical healing following EMS on 1-year postoperative CBCT scans and concluded that the addition of L-PRF did not significantly improve the results in terms of bone density and volume change when compared to MTA [
13]. Furthermore, evaluating the effect of these adjunctive techniques would require a histological assessment of the intervened-upon areas after healing in comparison with areas where no L-PRF was applied. Nonetheless, a systematic review on the advantages of autologous platelet concentrates on the healing of endodontic lesions following microsurgery concluded that autologous platelet concentrates, specifically L-PRF, showed benefits in terms of bone regeneration, although only 3 of the 4 included studies formally quantified bone formation [
12].
Radiographic and clinical follow-up examinations of the presented cases were performed regularly up to 1 year after EMS. Case 2 was considered radiographically as showing incomplete healing, presenting with a considerable improvement of periapical osseous density in a pattern typical of lesions affecting both buccal and palatal cortical plates—a “through-and-through” lesion [
20]. This pattern of healing can be considered stable and successful, without the need for prolonged follow-up intervals and with a good correlation with longer-term follow-up examines [
6,
8]. Other reports have suggested that, for through-and-through lesions, the use of membranes (either resorbable or expanded polytetrafluoroethylene) and xenografts may reduce the risk of scar tissue formation [
21,
22].
CONCLUSIONS
From the cases reported herein, the use of autologous L-PRF as an osseous filler and barrier membrane following EMS is a beneficial and viable option for achieving a successful outcome. However, there was evidence of scar tissue formation in 1 of the cases.
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Pires MD, Ginjeira A.
Data curation: Pires MD.
Formal analysis: Martins JNR.
Investigation: Pires MD, Pereira B, Baruwa AO.
Methodology: Pires MD, Pereira B.
Project administration: Martins JNR, Pereira B.
Resources: Pereira B.
Software: Baruwa AO.
Supervision: Martins JNR, Ginjeira A.
Validation: Martins JNR, Baruwa AO.
Visualization: Ginjeira A.
Writing - original draft: Pires MD, Pereira B.
Writing - review & editing: Martins JNR, Baruwa AO, Ginjeira A.
REFERENCES
- 1. Haapasalo M, Endal U, Zandi H, Coil JM. Eradication of endodontic infection by instrumentation and irrigation solutions. Endod Topics 2005;10:77-102.Article
- 2. Siqueira JF Jr, Rôças IN. Clinical implications and microbiology of bacterial persistence after treatment procedures. J Endod 2008;34:1291-1301.e3.ArticlePubMed
- 3. Schilder H. Filling root canals in three dimensions. 1967. J Endod 2006;32:281-290.PubMed
- 4. Nair PN. On the causes of persistent apical periodontitis: a review. Int Endod J 2006;39:249-281.ArticlePubMed
- 5. Kang M, In Jung H, Song M, Kim SY, Kim HC, Kim E. Outcome of nonsurgical retreatment and endodontic microsurgery: a meta-analysis. Clin Oral Investig 2015;19:569-582.ArticlePubMedPDF
- 6. Tsesis I, Rosen E, Taschieri S, Telishevsky Strauss Y, Ceresoli V, Del Fabbro M. Outcomes of surgical endodontic treatment performed by a modern technique: an updated meta-analysis of the literature. J Endod 2013;39:332-339.ArticlePubMed
- 7. European Society of Endodontology. Quality guidelines for endodontic treatment: consensus report of the European Society of Endodontology. Int Endod J 2006;39:921-930.ArticlePubMed
- 8. Song M, Kim SG, Shin SJ, Kim HC, Kim E. The influence of bone tissue deficiency on the outcome of endodontic microsurgery: a prospective study. J Endod 2013;39:1341-1345.ArticlePubMed
- 9. von Arx T, Cochran DL. Rationale for the application of the GTR principle using a barrier membrane in endodontic surgery: a proposal of classification and literature review. Int J Periodontics Restorative Dent 2001;21:127-139.PubMed
- 10. Del Fabbro M, Corbella S, Sequeira-Byron P, Tsesis I, Rosen E, Lolato A, Taschieri S. Endodontic procedures for retreatment of periapical lesions. Cochrane Database Syst Rev 2016;10:CD005511.PubMed
- 11. Karan NB, Aricioğlu B. Assessment of bone healing after mineral trioxide aggregate and platelet-rich fibrin application in periapical lesions using cone-beam computed tomographic imaging. Clin Oral Investig 2020;24:1065-1072.ArticlePubMedPDF
- 12. Meschi N, Castro AB, Vandamme K, Quirynen M, Lambrechts P. The impact of autologous platelet concentrates on endodontic healing: a systematic review. Platelets 2016;27:613-633.ArticlePubMed
- 13. Del Fabbro M, Ceresoli V, Lolato A, Taschieri S. Effect of platelet concentrate on quality of life after periradicular surgery: a randomized clinical study. J Endod 2012;38:733-739.ArticlePubMed
- 14. Song M, Kim HC, Lee W, Kim E. Analysis of the cause of failure in nonsurgical endodontic treatment by microscopic inspection during endodontic microsurgery. J Endod 2011;37:1516-1519.ArticlePubMed
- 15. de Chevigny C, Dao TT, Basrani BR, Marquis V, Farzaneh M, Abitbol S, Friedman S. Treatment outcome in endodontics: the Toronto study--phases 3 and 4: orthograde retreatment. J Endod 2008;34:131-137.ArticlePubMed
- 16. Huang S, Chen NN, Yu VS, Lim HA, Lui JN. Long-term success and survival of endodontic microsurgery. J Endod 2020;46:149-157.e4.ArticlePubMed
- 17. Pecora G, Baek SH, Rethnam S, Kim S. Barrier membrane techniques in endodontic microsurgery. Dent Clin North Am 1997;41:585-602.ArticlePubMed
- 18. von Arx T, Hänni S, Jensen SS. Correlation of bone defect dimensions with healing outcome one year after apical surgery. J Endod 2007;33:1044-1048.ArticlePubMed
- 19. Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, Dohan SL, Dohan AJ, Mouhyi J, Dohan DM. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part IV: clinical effects on tissue healing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;101:e56-e60.ArticlePubMed
- 20. Molven O, Halse A, Grung B. Incomplete healing (scar tissue) after periapical surgery--radiographic findings 8 to 12 years after treatment. J Endod 1996;22:264-268.ArticlePubMed
- 21. Pecora G, Kim S, Celletti R, Davarpanah M. The guided tissue regeneration principle in endodontic surgery: one-year postoperative results of large periapical lesions. Int Endod J 1995;28:41-46.ArticlePubMed
- 22. Taschieri S, Corbella S, Tsesis I, Bortolin M, Del Fabbro M. Effect of guided tissue regeneration on the outcome of surgical endodontic treatment of through-and-through lesions: a retrospective study at 4-year follow-up. Oral Maxillofac Surg 2011;15:153-159.ArticlePubMedPDF
 , Jorge N. R. Martins1,2
, Jorge N. R. Martins1,2 , Abayomi Omokeji Baruwa1
, Abayomi Omokeji Baruwa1 , Beatriz Pereira1
, Beatriz Pereira1 , António Ginjeira1,2
, António Ginjeira1,2


 KACD
KACD
 ePub Link
ePub Link Cite
Cite

