Search
- Page Path
- HOME > Search
- The effects of gingival blood flow on pulpal blood flow detection using ultrasound Doppler flowmetry: animal study
- Dohyun Kim, Hyoung-Seok Ko, Soo-Yeon Park, Seung-Yeon Ryu, Sung-ho Park
- Restor Dent Endod 2023;48(1):e9. Published online January 30, 2023
- DOI: https://doi.org/10.5395/rde.2023.48.e9
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
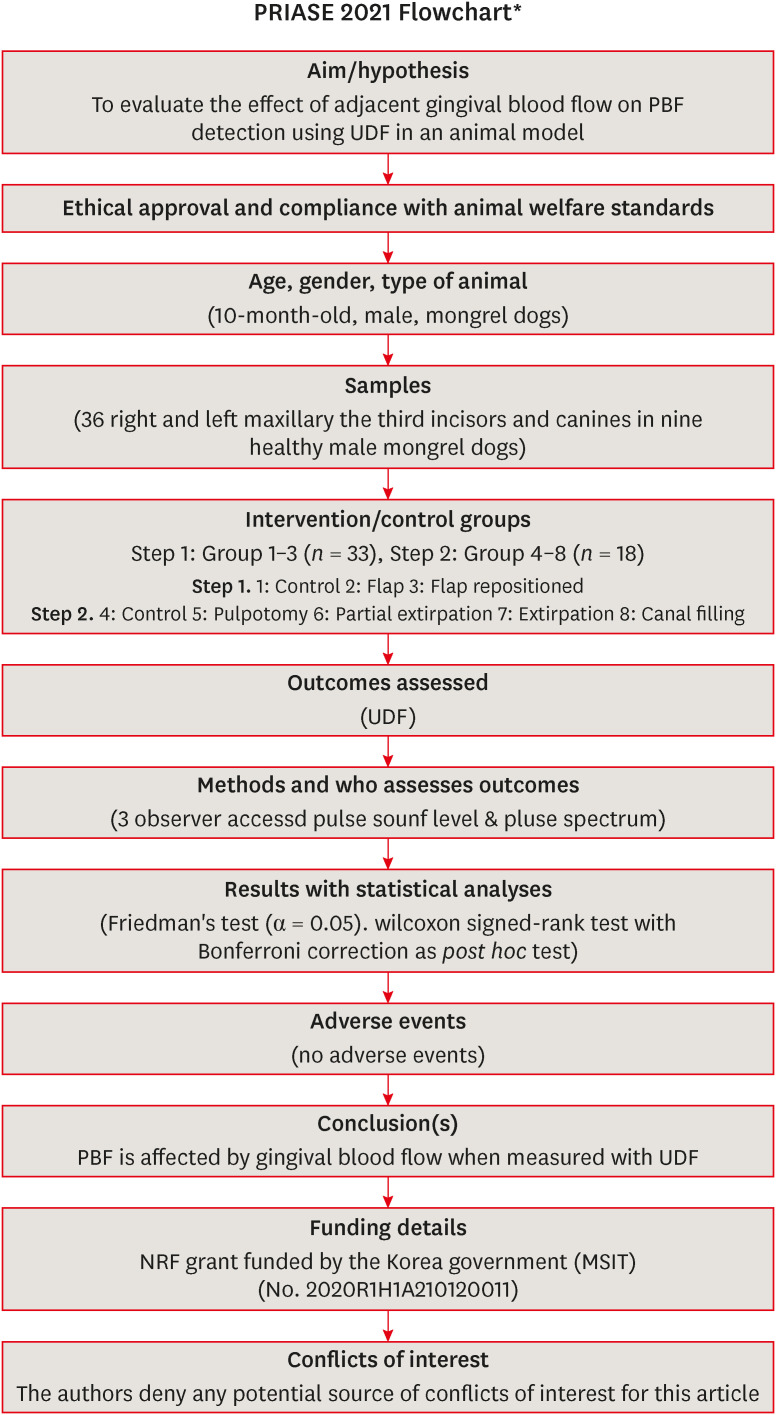
ePub Objectives This study evaluated the effect of adjacent gingival blood flow on detection of pulpal blood flow (PBF) using ultrasound Doppler flowmetry (UDF) through animal study.
Materials and Methods The study included 36 right and left maxillary the third incisors and canines in 9 experimental dogs. The study included 2 main steps: In the first step, the pulse sound level (PSL) was recorded on the cervical part of each tooth without flap elevation (Group 1), with flap elevation (Group 2), and after it was repositioned in place (Group 3). In the second step, the PSL was recorded on the cervical part of each tooth (Group 4), after pulpotomy (Group 5), after partial pulp extirpation (Group 6), after complete extirpation (Group 7), and after canal filling (Group 8). In Groups 5–8, the study was performed with and without flap elevation in the left and right teeth, respectively. The PSL was graded as follows: 0, inaudible; 1, heard faintly; and 2, heard well. The difference between each group was analyzed using Friedman’s test with Wilcoxon signed-rank tests (α = 0.05).
Results In step 1, the PSL results were Group 1 > 2 and 3. In step 2, there was no significant difference between the groups when the flap was not elevated, while PSL results were Group 4 > 5 ≥ 6 and 7 ≥ 8 when the flap was elevated.
Conclusions PBF is affected by gingival blood flow when measured with UDF. UDF measurements require isolation of gingiva from the tooth.
-
Citations
Citations to this article as recorded by- Modern aspects of the use of hardware methods for diagnosing pulp vitality (Part 2. Non-traditional diagnostic methods)
K. V. Shadrina, L. Yu. Orekhova, V. D. Goncharov, V. Yu. Vashneva, E. S. Silina, E. V. Kosova, A. A. Petrov
Endodontics Today.2025; 23(3): 423. CrossRef - Exploring approaches to pulp vitality assessment: A scoping review of nontraditional methods
Farzaneh Afkhami, Patricia Paule Wright, Philip Yuan‐Ho Chien, Chun Xu, Laurence James Walsh, Ove Andreas Peters
International Endodontic Journal.2024; 57(8): 1065. CrossRef
- Modern aspects of the use of hardware methods for diagnosing pulp vitality (Part 2. Non-traditional diagnostic methods)
- 2,442 View
- 39 Download
- 1 Web of Science
- 2 Crossref

- Use of ultrasound Doppler to determine tooth vitality in a discolored tooth after traumatic injury: its prospects and limitations
- Yong-Wook Cho, Sung-Ho Park
- Restor Dent Endod 2014;39(1):68-73. Published online January 20, 2014
- DOI: https://doi.org/10.5395/rde.2014.39.1.68
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub When a tooth shows discoloration and does not respond to the cold test or electric pulp test (EPT) after a traumatic injury, its diagnosis can be even more difficult due to the lack of proper diagnostic methods to evaluate its vitality. In these case reports, we hope to demonstrate that ultrasound Doppler might be successfully used to evaluate the vitality of the tooth after trauma, and help reduce unnecessary endodontic treatments. In all three of the present cases, the teeth were discolored after traumatic injuries and showed negative responses to the cold test and EPT. However, they showed distinctive vital reactions in the ultrasound Doppler test during the whole observation period. In the first case, the tooth color returned to normal, and the tooth showed a positive response to the cold test and EPT at 10 wk after the injury. In the second case, the tooth color had returned to its normal shade at 10 wk after the traumatic injury but remained insensitive to the cold test and EPT. In the third case, the discoloration was successfully treated with vital tooth bleaching.
-
Citations
Citations to this article as recorded by- Determination of Blood Flow in Superficial Arteries of Human Face using Doppler Ultrasonography in Young Adults
Nedal Iqbal, Khubaib Shahid, Muhammad Imtiaz, Faiqua Yasser, Ayesha Ashraf, Muhammad Zain ul Abdin
The International Journal of Frontier Sciences.2024;[Epub] CrossRef - The effects of gingival blood flow on pulpal blood flow detection using ultrasound Doppler flowmetry: animal study
Dohyun Kim, Hyoung-Seok Ko, Soo-Yeon Park, Seung-Yeon Ryu, Sung-ho Park
Restorative Dentistry & Endodontics.2023;[Epub] CrossRef - Evaluation of blood flow in superficial arteries of face by Doppler ultrasound in young adults
Izza Javaid, Anjum Tazeen, Syeda Khadija, Zareen Fatima, Muhammad Adeel Saleem, Mehreen Fatima, Umme Rubab
Pakistan BioMedical Journal.2022; : 165. CrossRef - Comparison of the Response to Pulpal Sensibility Tests in Well‐Controlled and Uncontrolled Type II Diabetes Mellitus Patients: A Cross‐Sectional Study
Fatemeh Owlia, Faezeh Zarezadeh, Sara Jambarsang, Maryam Kazemipoor, Giuseppe Minervini
International Journal of Dentistry.2022;[Epub] CrossRef - Detection of pulsed blood flow through a molar pulp chamber and surrounding tissue in vitro
S. Knörzer, K.-A. Hiller, M. Brandt, A. Niklas, J. Putzger, G. J. Monkman, S. N. Danilov, S. D. Ganichev, I. Schulz, G. Schmalz
Clinical Oral Investigations.2019; 23(3): 1121. CrossRef - Evaluation of microcirculation in the pulp of immature permanent teeth by ultrasound doppler after direct pulp capping with bioactive materials
N. U. Dmitrienko, L. R. Sarap, E. A. Kirienkova
Regional blood circulation and microcirculation.2018; 17(2): 26. CrossRef - Detection of atrial fibrillation during pulpal blood flow assessment using Doppler ultrasound: a case report
Chan-Hyun Lee, Euiseong Kim, Dohyun Kim
Dentomaxillofacial Radiology.2018; : 20170354. CrossRef - Long-term Prognosis of Pulpal Status of Traumatized Teeth Exhibiting Contradictory Results between Pulp Sensibility Test and Ultrasound Doppler Flowmetry: A Retrospective Study
So-Yeon Ahn, Dohyun Kim, Sung-Ho Park
Journal of Endodontics.2018; 44(3): 395. CrossRef
- Determination of Blood Flow in Superficial Arteries of Human Face using Doppler Ultrasonography in Young Adults
- 1,636 View
- 4 Download
- 8 Crossref

- Pulp vitality and coronal discoloration following traumatic injuries
- Tae-Sun Yoon, Hyung-Gyu Kong, Euiseong Kim
- J Korean Acad Conserv Dent 2010;35(6):492-496. Published online November 30, 2010
- DOI: https://doi.org/10.5395/JKACD.2010.35.6.492
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Coronal discoloration is a common sequela to traumatic injuries. In subluxation cases, although the injury is not strong enough to rupture the apical vessels, discoloration may appear by tearing thin walls or occluding small capillaries. In absence of infection pulpal regeneration can occur, and as a result discoloration may completely or partially subside. But judging pulpal status by coronal discoloration can be dangerous and it may lead to unnecessary treatment.
This case presents coronal discoloration and recovery following traumatic injury of maxillary anterior teeth. In diagnosing traumatized teeth routine cold tests or electric pulp tests are known to be unreliable, but with the aid of ultrasound doppler imaging, assessing pulp vitality of traumatized teeth can be more accurate.
-
Citations
Citations to this article as recorded by- Pulp necrosis following luxated injury to teeth in a patient with uncontrolled type II diabetes mellitus: a case report
Haneol Shin, Seung-Jong Lee, Il-Young Jung, Chan-Young Lee
Restorative Dentistry & Endodontics.2012; 37(1): 61. CrossRef
- Pulp necrosis following luxated injury to teeth in a patient with uncontrolled type II diabetes mellitus: a case report
- 1,502 View
- 13 Download
- 1 Crossref


 KACD
KACD

 First
First Prev
Prev


