Search
- Page Path
- HOME > Search
- Effects of the cathepsin K inhibitor with mineral trioxide aggregate cements on osteoclastic activity
- Hee-Sun Kim, Soojung Kim, Hyunjung Ko, Minju Song, Miri Kim
- Restor Dent Endod 2019;44(2):e17. Published online April 23, 2019
- DOI: https://doi.org/10.5395/rde.2019.44.e17
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives Root resorption is an unexpected complication after replantation procedures. Combining anti-osteoclastic medicaments with retrograde root filling materials may avert this resorptive activity. The purpose of this study was to assess effects of a cathepsin K inhibitor with calcium silicate-based cements on osteoclastic activity.
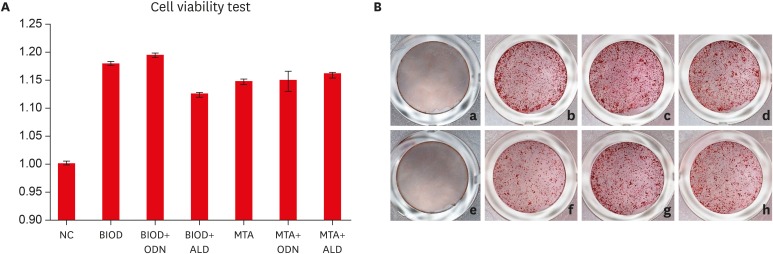
Methods MC3T3-E1 cells were cultured for biocompatibility analyses. RAW 264.7 cells were cultured in the presence of the receptor activator of nuclear factor-kappa B and lipopolysaccharide, followed by treatment with Biodentine (BIOD) or ProRoot MTA with or without medicaments (Odanacatib [ODN], a cathepsin inhibitor and alendronate, a bisphosphonate). After drug treatment, the cell counting kit-8 assay and Alizarin red staining were performed to evaluate biocompatibility in MC3T3-E1 cells. Reverse-transcription polymerase chain reaction, tartrate-resistant acid phosphatase (TRAP) staining and enzyme-linked immunosorbent assays were performed in RAW 264.7 cells to determine the expression levels of inflammatory cytokines, interleukin (IL)-1β, IL-6, tumor necrosis factor-α (TNF-α) and prostaglandin E2 (PGE2). Data were analyzed by one-way analysis of variance and Tukey's
post hoc test (p < 0.05).Results Biocompatibility results showed that there were no significant differences among any of the groups. RAW 264.7 cells treated with BIOD and ODN showed the lowest levels of TNF-α and PGE2. Treatments with BIOD + ODN were more potent suppressors of inflammatory cytokine expression (
p < 0.05).Conclusion The cathepsin K inhibitor with calcium silicate-based cement inhibits osteoclastic activity. This may have clinical application in preventing inflammatory root resorption in replanted teeth.
-
Citations
Citations to this article as recorded by- Root-filling materials for endodontic surgery: biological and clinical aspects
Andreas Koutroulis, Vasileios Kapralos, Dag Ørstavik, Pia Titterud Sunde
Biomaterial Investigations in Dentistry.2024; 11: 115. CrossRef - Effect of intra‐alveolar delivery of Frondoside A on inflammatory response of delayed tooth replantation
Lar Herr, Ju Ri Ye, Sang Wook Kang, Sang Tae Ro, Yong Kwon Chae, Ko Eun Lee, Mi Sun Kim, Myeong Kwan Jih, Chunui Lee, Sung Chul Choi, Ok Hyung Nam
Dental Traumatology.2024; 40(2): 178. CrossRef - Bone-targeting PLGA derived lipid drug delivery system ameliorates bone loss in osteoporotic ovariectomized rats
Youyun Zeng, Yiding Shen, Shuyi Wu, Lei Cai, Zhen Wang, Kexin Cai, Jiating Shen, Kendrick Hii Ru Yie, Hualin Zhang, Lihua Xu, Jinsong Liu
Materials & Design.2022; 221: 110967. CrossRef
- Root-filling materials for endodontic surgery: biological and clinical aspects
- 247 View
- 5 Download
- 3 Crossref

- Cytotoxicity and biocompatibility of Zirconia (Y-TZP) posts with various dental cements
- Hyeongsoon Shin, Hyunjung Ko, Miri Kim
- Restor Dent Endod 2016;41(3):167-175. Published online May 30, 2016
- DOI: https://doi.org/10.5395/rde.2016.41.3.167
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives Endodontically treated teeth with insufficient tooth structure are often restored with esthetic restorations. This study evaluated the cytotoxicity and biological effects of yttria partially stabilized zirconia (Y-TZP) blocks in combination with several dental cements.
Materials and Methods Pairs of zirconia cylinders with medium alone or cemented with three types of dental cement including RelyX U200 (3M ESPE), FujiCEM 2 (GC), and Panavia F 2.0 (Kuraray) were incubated in medium for 14 days. The cytotoxicity of each supernatant was determined using 3-(4,5-dimethylthiazole-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assays on L929 fibroblasts and MC3T3-E1 osteoblasts. The levels of interleukin-6 (IL-6) mRNA were evaluated by reverse transcription polymerase chain reaction (RT-PCR), and IL-6 protein was evaluated by enzyme-linked immunosorbent assays (ELISA). The data were analyzed using one-way ANOVA and Tukey
post-hoc tests. Ap < 0.05 was considered statistically significant.Results The MTT assays showed that MC3T3-E1 osteoblasts were more susceptible to dental cements than L929 fibroblasts. The resin based dental cements increased IL-6 expression in L929 cells, but reduced IL-6 expression in MC3T3-E1 cells.
Conclusions Zirconia alone or blocks cemented with dental cement showed acceptable biocompatibilities. The results showed resin-modified glass-ionomer based cement less produced inflammatory cytokines than other self-adhesive resin-based cements. Furthermore, osteoblasts were more susceptible than fibroblasts to the biological effects of dental cement.
-
Citations
Citations to this article as recorded by- Digital light processing 3D printing of yttria stabilized zirconia ceramics: microstructures, characterizations, and cytocompatibility
Luke Wadle, Mena Asha Krishnan, Ryan Wall, Lanh Trinh, Bin Duan, Bai Cui
Emergent Materials.2024;[Epub] CrossRef - Doping of casted silk fibroin membranes with extracellular vesicles for regenerative therapy: a proof of concept
Sandra Fuest, Amanda Salviano-Silva, Cecile L. Maire, Yong Xu, Christian Apel, Audrey Laure Céline Grust, Arianna Delle Coste, Martin Gosau, Franz L. Ricklefs, Ralf Smeets
Scientific Reports.2024;[Epub] CrossRef - 3D printing of ceramics: Advantages, challenges, applications, and perspectives
Susmita Bose, Enver Koray Akdogan, Vamsi K. Balla, Sushant Ciliveri, Paolo Colombo, Giorgia Franchin, Nicholas Ku, Priya Kushram, Fangyong Niu, Joshua Pelz, Andrew Rosenberger, Ahmad Safari, Zachary Seeley, Rodney W. Trice, Lionel Vargas‐Gonzalez, Jeffrey
Journal of the American Ceramic Society.2024; 107(12): 7879. CrossRef - A Review on Biocompatibility of Dental Restorative and Reconstruction Materials
Pune Nina Paqué, Mutlu Özcan
Current Oral Health Reports.2024; 11(1): 68. CrossRef - Enhancement of Human Gingival Fibroblasts Bioactivity and Proliferation on Plasma Sprayed Yttria-Stabilised Zirconia/TiO2 Surface Coating of Titanium Alloys: An In-Vitro Study
Afida Jemat, Masfueh Razali, Yuichi Otsuka, Mariyam Jameelah Ghazali
Coatings.2023; 13(10): 1746. CrossRef - Material extrusion-based additive manufacturing of zirconia toughened alumina: Machinability, mechanical properties and biocompatibility
Tianyu Yu, Xiaolong Zhu, Hongwei Yu, Pan Wu, Chun Li, Xiaoxiao Han, Mingjun Chen
Journal of Manufacturing Processes.2023; 94: 120. CrossRef - Green synthesis and characterization of zirconium nanoparticlefor dental implant applications
Mohammad Asaduzzaman Chowdhury, Nayem Hossain, Md. Golam Mostofa, Md. Riyad Mia, Md. Tushar, Md. Masud Rana, Md. Helal Hossain
Heliyon.2023; 9(1): e12711. CrossRef - The role of Y2O3 in the bioactivity of YSZ/PLLA composites
Elia Marin, Giada Bassi, Orion Yoshikawa, Francesco Boschetto, Wenliang Zhu, Arianna Rossi, Alex Lanzutti, Huaizhong Xu, Monica Montesi, Silvia Panseri, Giuseppe Pezzotti
Journal of Materials Science.2023; 58(27): 11218. CrossRef - Nano-β-tricalcium phosphate incorporated root dentin adhesive in the bonding interface of yttria-stabilized tetragonal zirconia polycrystalline post
Amal S. Al-Qahtani, Huda I. Tulbah, Mashael Binhasan, Mai M. Alhamdan, Imran Farooq, Fahim Vohra, Tariq Abduljabbar
Applied Nanoscience.2022; 12(11): 3489. CrossRef - Outcome of teeth restored with CAD/CAM zirconium dioxide post-cores: a retrospective study with a follow-up period of 3–6 years
Shunv Ying, Song Chen, Siyuan Wang, Lingli Xu, Xiaofeng Wang, Fuming He, Wei Liu
BMC Oral Health.2022;[Epub] CrossRef - Review of Physical, Mechanical, and Biological Characteristics of 3D-Printed Bioceramic Scaffolds for Bone Tissue Engineering Applications
Mahendran Thangavel, Renold Elsen Selvam
ACS Biomaterials Science & Engineering.2022; 8(12): 5060. CrossRef - Comparison of Regular and Speed Sintering on Low-Temperature Degradation and Fatigue Resistance of Translucent Zirconia Crowns for Implants: An In Vitro Study
Suchada Kongkiatkamon, Chaimongkon Peampring
Journal of Functional Biomaterials.2022; 13(4): 281. CrossRef - Cytotoxicity and Bonding Property of Bioinspired Nacre-like Ceramic-Polymer Composites
Hui Sun, Kefeng Gao, Zhe Yi, Chengwei Han, Zengqian Liu, Qiang Wang, Qing Zhou, Zhefeng Zhang
Frontiers in Bioengineering and Biotechnology.2022;[Epub] CrossRef - Characterisation of Selected Materials in Medical Applications
Kacper Kroczek, Paweł Turek, Damian Mazur, Jacek Szczygielski, Damian Filip, Robert Brodowski, Krzysztof Balawender, Łukasz Przeszłowski, Bogumił Lewandowski, Stanisław Orkisz, Artur Mazur, Grzegorz Budzik, Józef Cebulski, Mariusz Oleksy
Polymers.2022; 14(8): 1526. CrossRef - Adhesive bond integrity of Y‐TZP post with calcium fluoride infiltrated resin dentin adhesive: An SEM, EDX, FTIR and micro‐Raman study
Eman M. AlHamdan, Samar Al‐Saleh, Mohammad H. AlRefeai, Imran Farooq, Eisha Abrar, Fahim Vohra, Tariq Abduljabbar
Surface and Interface Analysis.2021; 53(11): 956. CrossRef - Additive Manufacturing (3D PRINTING) Methods and Applications in Dentistry
Elif DEMİRALP, Gülsüm DOĞRU, Handan YILMAZ
Clinical and Experimental Health Sciences.2021; 11(1): 182. CrossRef - Interleukin-1β activity in gingival crevicular fluid of abutment teeth with temporary fixed restorations versus final fixed restorations: Prospective observational study
Amal Abdallah A. Abo-Elmagd, Dina Sabry, Ebtehal Mohammed
The Saudi Dental Journal.2021; 33(6): 322. CrossRef - Change in the Microhardness of Composite Ceramics at the CaO–ZrO2/CaO–ZrO2 + Al2O3 Interface
A. A. Dmitrievskiy, D. G. Zhigacheva, G. V. Grigoriev, P. N. Ovchinnikov
Journal of Surface Investigation: X-ray, Synchrotron and Neutron Techniques.2021; 15(S1): S137. CrossRef - Cytotoxicity of two self-adhesive flowable composites on bovine dental pulp-derived cells
Firdevs KAHVECİOĞLU, Türkay KÖLÜŞ, Fatma SAĞ GÜNGÖR, Hayriye Esra ÜLKER
Journal of Health Sciences and Medicine.2021; 4(2): 209. CrossRef - Cytotoxicity and biocompatibility of high mol% yttria containing zirconia
Gulsan Ara Sathi Kazi, Ryo Yamagiwa
Restorative Dentistry & Endodontics.2020;[Epub] CrossRef - Cytotoxic effects of different self-adhesive resin cements: Cell viability and induction of apoptosis
Soner Şişmanoğlu, Mustafa Demirci, Helmut Schweikl, Gunes Ozen-Eroglu, Esin Cetin-Aktas, Serap Kuruca, Safa Tuncer, Neslihan Tekce
The Journal of Advanced Prosthodontics.2020; 12(2): 89. CrossRef - Effects of nano-zirconia fillers conditioned with phosphate ester monomers on the conversion and mechanical properties of Bis-GMA- and UDMA-based resin composites
Jiaxue Yang, Jiadi Shen, Xinyi Wu, Feng He, Haifeng Xie, Chen Chen
Journal of Dentistry.2020; 94: 103306. CrossRef - Effect of APTES- or MPTS-Conditioned Nanozirconia Fillers on Mechanical Properties of Bis-GMA-Based Resin Composites
Jiaxue Yang, Mengyuan Liao, Gaoying Hong, Shiqi Dai, Jiadi Shen, Haifeng Xie, Chen Chen
ACS Omega.2020; 5(50): 32540. CrossRef - In Vitro Cytotoxicity of Self-Adhesive Dual-Cured Resin Cement Polymerized Beneath Three Different Cusp Inclinations of Zirconia
Chang-Yuan Zhang, Yi-Ling Cheng, Xin-Wen Tong, Hao Yu, Hui Cheng
BioMed Research International.2019; 2019: 1. CrossRef - Investigations on the corrosion behaviour and biocompatibility of magnesium alloy surface composites AZ91D-ZrO2 fabricated by friction stir processing
R. Vaira Vignesh, R. Padmanaban, M. Govindaraju, G. Suganya Priyadharshini
Transactions of the IMF.2019; 97(5): 261. CrossRef - Microwave assisted synthesis and antimicrobial activity of Fe3O4-doped ZrO2 nanoparticles
M. Imran, Saira Riaz, Ifra Sanaullah, Usman Khan, Anjum N. Sabri, Shahzad Naseem
Ceramics International.2019; 45(8): 10106. CrossRef - Additive manufacturing of ceramics for dental applications: A review
Raquel Galante, Celio G. Figueiredo-Pina, Ana Paula Serro
Dental Materials.2019; 35(6): 825. CrossRef - Reinforcement of dental resin composite via zirconium hydroxide coating and phosphate ester monomer conditioning of nano-zirconia fillers
Xinyi Wu, Shiqi Dai, Ying Chen, Feng He, Haifeng Xie, Chen Chen
Journal of the Mechanical Behavior of Biomedical Materials.2019; 94: 32. CrossRef - Effects of TiO2 on microstructural, mechanical properties and in-vitro bioactivity of plasma sprayed yttria stabilised zirconia coatings for dental application
A. Jemat, M.J. Ghazali, M. Razali, Y. Otsuka, A. Rajabi
Ceramics International.2018; 44(4): 4271. CrossRef - In vitro evaluation of cytotoxicity of different self-adhesive resin cements
Necla Demir, Firdevs Kahvecioğlu, Muhammet Karcı, Hayriye Esra Ülker, Nuray Günaydın
Acta Odontologica Turcica.2017;[Epub] CrossRef
- Digital light processing 3D printing of yttria stabilized zirconia ceramics: microstructures, characterizations, and cytocompatibility
- 317 View
- 3 Download
- 30 Crossref

- The effects of bone morphogenetic protein-2 and enamel matrix derivative on the bioactivity of mineral trioxide aggregate in MC3T3-E1cells
- Youngdan Jeong, Wonkyung Yang, Hyunjung Ko, Miri Kim
- Restor Dent Endod 2014;39(3):187-194. Published online June 19, 2014
- DOI: https://doi.org/10.5395/rde.2014.39.3.187
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives The effects of bone morphogenetic protein-2 (BMP-2) and enamel matrix derivative (EMD) respectively with mineral trioxide aggregate (MTA) on hard tissue regeneration have been investigated in previous studies. This study aimed to compare the osteogenic effects of MTA/BMP-2 and MTA/EMD treatment in MC3T3-E1 cells.
Materials and Methods MC3T3-E1 cells were treated with MTA (ProRoot, Dentsply), BMP-2 (R&D Systems), EMD (Emdogain, Straumann) separately and MTA/BMP-2 or MTA/EMD combination. Mineralization was evaluated by staining the calcium deposits with alkaline phosphatase (ALP, Sigma-Aldrich) and Alizarin red (Sigma-Aldrich). The effects on the osteoblast differentiation were evaluated by the expressions of osteogenic markers, including ALP, bone sialoprotein (BSP), osteocalcin (OCN), osteopontin (OPN) and osteonectin (OSN), as determined by reverse-transcription polymerase chain reaction analysis (RT-PCR, AccuPower PCR, Bioneer).
Results Mineralization increased in the BMP-2 and MTA/BMP-2 groups and increased to a lesser extent in the MTA/EMD group but appeared to decrease in the MTA-only group based on Alizarin red staining. ALP expression largely decreased in the EMD and MTA/EMD groups based on ALP staining. In the MTA/BMP-2 group, mRNA expression of OPN on day 3 and BSP and OCN on day 7 significantly increased. In the MTA/EMD group, OSN and OCN gene expression significantly increased on day 7, whereas ALP expression decreased on days 3 and 7 (
p < 0.05).Conclusions These results suggest the MTA/BMP-2 combination promoted more rapid differentiation in MC3T3-E1 cells than did MTA/EMD during the early mineralization period.
-
Citations
Citations to this article as recorded by- Elucidating epigenetic mechanisms governing odontogenic differentiation in dental pulp stem cells: an in-depth exploration
Lei Huang, Xuan Chen, Xiaoxia Yang, Yinchun Zhang, Yiyun Liang, Xiaoling Qiu
Frontiers in Cell and Developmental Biology.2024;[Epub] CrossRef - Evaluation of the genotoxicity, cytotoxicity, and bioactivity of calcium silicate-based cements
Merve Esen, Yeliz Guven, Mehmet Fatih Seyhan, Handan Ersev, Elif Bahar Tuna-Ince
BMC Oral Health.2024;[Epub] CrossRef - GelMA‐based hydrogel biomaterial scaffold: A versatile platform for regenerative endodontics
Lei Huang, Xuan Chen, XiaoXia Yang, Yinchun Zhang, Xiaoling Qiu
Journal of Biomedical Materials Research Part B: Applied Biomaterials.2024;[Epub] CrossRef - Experimental Validation of Antiobesogenic and Osteoprotective Efficacy of Ginsenoside CK via Targeting Lipid and Atherosclerosis Pathways
Md. Niaj Morshed, Reshmi Akter, Imran Mahmud, Ah-Yeong Gwon, Jin Woo Jeang, Yeong-Geun Lee, Dae Won Park, Deok Chun Yang, Yeon Ju Kim, Se-Chan Kang
Life.2024; 15(1): 41. CrossRef - Anti-osteoporosis effects of triterpenoids from the fruit of sea buckthorn (Hippophae rhamnoides) through the promotion of osteoblast differentiation in mesenchymal stem cells, C3H10T1/2
Da Eun Lee, Kun Hee Park, Joo-Hyun Hong, Seon Hee Kim, Ki-Moon Park, Ki Hyun Kim
Archives of Pharmacal Research.2023; 46(9-10): 771. CrossRef - In Silico and In Vitro Evaluation of Antiobesogenic and Osteoprotective Effect of Pomegranate Juice Fermented by Tannin Acyl Hydrolase and Lactobacillus vespulae DCY75 via the Wnt/β-Catenin Pathway
Reshmi Akter, Vinothini Boopathi, Muhammad Awais, Juha Park, Byoung Man Kong, Se-Woung Oh, Ji-Hyung Oh, Jong Chan Ahn, Deok Chun Yang
ACS Food Science & Technology.2023; 3(11): 1975. CrossRef - Early induction of Hes1 by bone morphogenetic protein 9 plays a regulatory role in osteoblastic differentiation of a mesenchymal stem cell line
Chang‐Hwan Seong, Norika Chiba, Mardiyantoro Fredy, Joji Kusuyama, Kiyohide Ishihata, Toshiro Kibe, Muhammad Subhan Amir, Ryohei Tada, Tomokazu Ohnishi, Norifumi Nakamura, Tetsuya Matsuguchi
Journal of Cellular Biochemistry.2023; 124(9): 1366. CrossRef - Effects of Fucoidan Powder Combined with Mineral Trioxide Aggregate as a Direct Pulp-Capping Material
Mijoo Kim, Marc Hayashi, Bo Yu, Thomas K. Lee, Reuben H. Kim, Deuk-Won Jo
Polymers.2022; 14(12): 2315. CrossRef - Nerve growth factor promotes osteogenic differentiation of MC3T3-E1 cells via BMP-2/Smads pathway
Xuming Yang, Donggang Mou, Qunying Yu, Jimei Zhang, Ying Xiong, Zhimin Zhang, Shan Xing
Annals of Anatomy - Anatomischer Anzeiger.2022; 239: 151819. CrossRef - Anti-Osteoporosis Effects of the Fruit of Sea Buckthorn (Hippophae rhamnoides) through Promotion of Osteogenic Differentiation in Ovariectomized Mice
Kun Hee Park, Joo-Hyun Hong, Seon-Hee Kim, Jin-Chul Kim, Ki Hyun Kim, Ki-Moon Park
Nutrients.2022; 14(17): 3604. CrossRef - Oroactive dental biomaterials and their use in endodontic therapy
Ebrahim Patel, Priyamvada Pradeep, Pradeep Kumar, Yahya E. Choonara, Viness Pillay
Journal of Biomedical Materials Research Part B: Applied Biomaterials.2020; 108(1): 201. CrossRef - BMP-2 and type I collagen preservation in human deciduous teeth after demineralization
Nina Bono, Paolo Tarsini, Gabriele Candiani
Journal of Applied Biomaterials & Functional Materials.2019;[Epub] CrossRef - An assessment of the overexpression of BMP‐2 in transfected human osteoblast cells stimulated by mineral trioxide aggregate and Biodentine
E. M. Rodrigues, A. L. Gomes‐Cornélio, A. Soares‐Costa, L. P. Salles, M. Velayutham, C. Rossa‐Junior, J. M. Guerreiro‐Tanomaru, M. Tanomaru‐Filho
International Endodontic Journal.2017;[Epub] CrossRef - Sandblasting and fibronectin-derived peptide immobilization on titanium surface increase adhesion and differentiation of osteoblast-like cells (MC3T3-E1)
Samdharu Pramono, Kamolparn Pugdee, Jintamai Suwanprateep, Sittichai Koontongkaew
Journal of Dental Sciences.2016; 11(4): 427. CrossRef - Combined Effects of Growth Hormone and Mineral Trioxide Aggregate on Growth, Differentiation, and Angiogenesis in Human Dental Pulp Cells
Hyung-Mun Yun, Seok-Woo Chang, Kyung-Ran Park, Lan Herr, Eun-Cheol Kim
Journal of Endodontics.2016; 42(2): 269. CrossRef - Combined effects of mineral trioxide aggregate and human placental extract on rat pulp tissue and growth, differentiation and angiogenesis in human dental pulp cells
Seok-Woo Chang, Ji-Youn Kim, Mi-Joo Kim, Ga-Hyun Kim, Jin-Kyu Yi, Deok-Won Lee, Kee-Yeon Kum, Eun-Cheol Kim
Acta Odontologica Scandinavica.2016; 74(4): 298. CrossRef - Mineral trioxide aggregate induces osteoblastogenesis via Atf6
Toyonobu Maeda, Atsuko Suzuki, Satoshi Yuzawa, Yuh Baba, Yuichi Kimura, Yasumasa Kato
Bone Reports.2015; 2: 36. CrossRef - Locally controlled delivery of TNFα antibody from a novel glucose-sensitive scaffold enhances alveolar bone healing in diabetic conditions
Qi Wang, Hao Li, Yu Xiao, Shuan Li, Bo Li, Xiaowen Zhao, Lin Ye, Bin Guo, Xinmin Chen, Yi Ding, Chongyun Bao
Journal of Controlled Release.2015; 206: 232. CrossRef
- Elucidating epigenetic mechanisms governing odontogenic differentiation in dental pulp stem cells: an in-depth exploration
- 209 View
- 1 Download
- 18 Crossref

-
Tissue response of Pro-Root® MTA with
rh BMP-2 in pulpotomized rat teeth - Kyungtae Park, Wonkyung Yang, Hyunjung Ko, Miri Kim
- J Korean Acad Conserv Dent 2007;32(5):403-410. Published online September 30, 2007
- DOI: https://doi.org/10.5395/JKACD.2007.32.5.403
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub The purpose of this study was to investigate whether
rh BMP-2 (BMP2) could induce synergistic effect with Pro-Root® MTA (MTA) in pulpotomized teeth in the rats. Healthy upper first molars from thirty-two, 10 weeks old, Sprague-Dawley rats were used for this investigation. The molars were exposed with round bur, and light pressure was applied with sterilized cotton to control hemorrhage. 1.2 grams of MTA cement was placed in right first molars as a control group. In left first molars, 1 µg of BMP2 was additionally placed on exposed pulps with MTA. All cavities were back-filled with light-cured glass-ionomer cements. The rats were sacrificed after 2 weeks and 7 weeks, respectively. Then histologic sections were made and assessed by light microscopy. Data were statistically analyzed via student t-test with SPSSWIN 12.0 program (p < 0.05).Inflammation observed in 2 weeks groups were severe compared to the 7 weeks groups. But the differences were not statistically significant. BMP2-addition groups had less inflammation than MTA groups in both periods, though these differences were also not statistically significant. In conclusion, the combination of BMP2 and MTA showed no differences with MTA only for pulpotomy of rat teeth.
-
Citations
Citations to this article as recorded by- A bioactivity study of Portland cement mixed with β-glycerophosphosphate on human pulp cell
Young-Hwan Oh, Young-Joo Jang, Yong-Bum Cho
Journal of Korean Academy of Conservative Dentistry.2009; 34(5): 415. CrossRef
- A bioactivity study of Portland cement mixed with β-glycerophosphosphate on human pulp cell
- 189 View
- 0 Download
- 1 Crossref


 KACD
KACD

 First
First Prev
Prev


